Abstract
Several recent national initiatives have called for increased efforts to integrate social determinants of health (SDH) into health care settings using health information technology (HIT). However, there is limited evidence to guide the implementation of these recommendations in practice. Research is needed to understand what SDH information is most important to collect, how SDH information can be used to inform clinical care and referrals, and ultimately, whether and how integrating SDH screening and action into primary care affects individual and population health. We recently proposed a conceptual framework to illustrate how HIT can be used to bring SDH information into primary care. In this paper, we describe how we are putting this conceptual model into practice within the OCHIN network of community health centers by highlighting examples of ongoing research, identifying knowledge gaps, and outlining a roadmap of future research to move the field forward.
Keywords: Social determinants of health, electronic health records, health information technology, primary care
Social determinants of health (SDH), the conditions in which people are born, grow, work, live, and age,1 profoundly impact the health of individuals and populations. A large body of scientific literature shows that SDH affect morbidity and mortality across the life course; some estimates suggest that up to 60% of preventable deaths are caused by modifiable SDH factors.2 Research also shows that SDH are critical drivers of persistent health inequities.
Several recent national initiatives have called for increased efforts to integrate SDH into health care settings using health information technology (HIT).3–7 In 2014, a National Academy of Medicine (formerly the Institute of Medicine) panel of experts recommended standardized documentation of a set of SDH domains in electronic health records (EHRs).3 The Medicare Access & Children’s Health Insurance Program Reauthorization Act of 2015 (MACRA), the Centers for Medicare and Medicaid Services (CMS) 2016 National Quality Strategy, and the Office of the National Coordinator for Health Information Technology also emphasize the importance of health care providers identifying and addressing patients’ SDH-related needs, and using EHRs to support these efforts.4–6 Moreover, as part of their Accountable Healthcare Communities Model, CMS recently developed a 10- item screening tool for use in the clinical setting that identifies patient needs in five SDH domains that can be addressed by community services.7
Primary care is uniquely positioned to identify and address SDH.8–11 Integrating the collection of SDH data into primary care could enable providers to take into account a broader array of factors that influence health and may facilitate referrals to resources that can help to address identified needs. National health care organizations and initiatives, such as those highlighted above, have taken the first step of recognizing the importance of addressing SDH and identifying priority SDH domains to capture in EHRs. However, there is limited evidence to guide the implementation of these recommendations in practice. Research is needed to understand who should be screened for SDH needs and which domains are the most important to focus on, barriers and facilitators to collecting this information in clinical settings, how SDH information can be used to inform clinical care and referrals, and ultimately, whether and how integrating SDH screening and action into primary care affects individual and population health.12–15 We recently introduced a conceptual framework outlining ways that HIT could be used to identify and address SDH in primary care. This follow-up paper describes how we are applying our framework to guide a body of primary care research within the OCHIN* network of community health centers (CHCs) and identifies knowledge gaps and areas of future research needed to move the field forward.
Developing a Strategic Portfolio of SDH Research in the OCHIN Community Laboratory
Originally known as the Oregon Community Health Information Network, then just OCHIN as other states joined, OCHIN is a non-profit health center-controlled network that hosts and manages an Epic© EHR for 440 primary care CHCs, with over 6,300 providers serving more than 714,000 adult patients across 18 states—united by a single EHR with one master patient index.16–17 As the nation’s largest CHC network on a single EHR, OCHIN pioneered EHR tool development in CHCs, hosts a centrally managed EHR research data warehouse, and has a strong research infrastructure and a record of participating in projects funded by multiple federal agencies. With 22 active research studies, OCHIN is committed to building the nation’s foremost community laboratory for health outcomes, policy, and primary care research with vulnerable and underserved populations. Current and past studies use the OCHIN community laboratory to understand health disparities, evaluate the impact of changes in policy and practice on health outcomes, develop and test practice-based HIT interventions, and understand the barriers and facilitators to the dissemination and implementation of evidence-based strategies.17–21
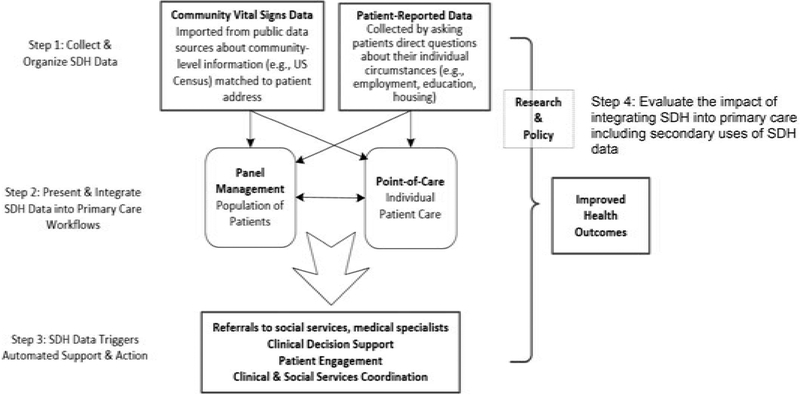
We developed our conceptual framework (Figure 1) as a roadmap to guide the strategic development of an SDH-related research portfolio at OCHIN.8 A key feature of our framework is the integration of two types of SDH data into clinical care: patient-reported SDH data collected from individuals at the point of care (e.g., information on food security, housing status, household income) and geocoded community-level SDH data from publicly available sources (median household income in a given geographic area, availability of fresh foods, or accessibility of safe recreation spaces).22 The framework traces the path of these data through the clinical workflow, providing the scaffolding of a research agenda that addresses: collecting and organizing patient-reported and community-level SDH data (step 1); presenting and integrating SDH data into primary care workflows (step 2); and developing clinical decision support (CDS) systems that trigger automated support and action based on SDH data, such as suggestions for adapting clinical care or treatment plans and/or providing referrals to community resources to address identified SDH needs (step 3). In addition to developing approaches for integrating SDH into primary care, we identified a fourth step of evaluating the impact of these efforts on the triple aim23 of enhancing patient and health care provider experiences, improving population health, and reducing costs (step 4). Using the framework as a guide, we outlined key implementation questions that could be targeted for future research (see Box 1).
Figure 1.
Conceptual framework for using health information technology to integrate SDH into primary care.a
a Adapted from: DeVoe JE, Bazemore AW, Cottrell EK, Likumahuwa-Ackman S, Grandmont J, Spach N, Gold R. Perspectives in primary care: a conceptual framework and a path for integrating social determinants of health into primary care practice. Ann Fam Med. 2016;14(2):104–8. https://doi.org/10.1370/afm.1903
PMid: 26951584
Box 1. CONCEPTUAL FRAMEWORK FOR USING HEALTH INFORMATION TECHNOLOGY TO INTEGRATE SDH INTO PRIMARY CARE: KNOWLEDGE GAPS AND AREAS FOR FUTURE RESEARCH.
| Step in framework | Knowledge Gaps: Areas for future research |
|---|---|
| Step 1. Collect and Organize Patient-reported and Community-level SDH Data. |
|
| Step 2. Present and integrate SDH data into primary care workflows. |
|
| Step 3. Trigger EHR-based automated support and action based on SDH data. |
|
| Step 4. Evaluate the impact of integrating SDH into primary care, including secondary uses of SDH data. |
|
Our portfolio of research projects is designed to address key implementation questions within this framework. Current projects are focused primarily on developing and testing HIT approaches for integrating SDH information into primary care (steps 1–3) and address the integration and use of both patient-reported and community-level SDH data (see Box 2 for a details on current projects). For example, building on the NAM’s recommendations for integrating SDH into EHRs, we worked collaboratively with OCHIN stakeholders to develop and pilot test EHR-based SDH screening tools for documenting patient-reported SDH information and summarizing areas of identified need (Act on Social Determinants Using EHR Tools in Safety Net Settings, or ASSESS). The EHR-based SDH screening tools—which include a flow-sheet with the SDH questions, a summary tool highlighting areas of identified need, and an optional patient portal survey that can be sent to patients prior to a visit—were made available to all OCHIN clinics in June 2016. Our research team used a mixed-methods approach, including qualitative interviews and site visits, to evaluate the feasibility and acceptability of using these tools in three pilot CHC sites.24
Box 2. PORTFOLIO OF SDH RESEARCH PROJECTS IN THE OCHIN COMMUNITY LABORATORY.
| Project Summary | Step in framework / Knowledge gap |
|---|---|
|
ASSESS: Act on Social Determinants Using EHR Tools in Safety Net Settings. Building on the Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE), a national effort to help health centers collect the data needed to better understand an act on their patients social needs, OCHIN is collaborating with Kaiser Permanente Center for Health Researchb to demonstrate the feasibility of creating EHR-based SDH data collection and presentation tools that can be used to document patient-reported SDH data, and facilitate and track referrals to community resources; and to evaluate uptake, use, and impact of the SDH tools in 3 pilot sites. Funder: National Institutes of Diabetes and Digestive and Kidney Diseases (09/01/2015 – 08/31/2017) |
Step 1: (i) Understand which patient-reported SDH have the biggest impact on health are most important to collect in primary care settings; (iv) Identify the most effective workflows to facilitate the collection of patient- reported SDH information. Step 2: (i) Develop EHR-based tools for presenting and summarizing patient-reported SDH information; (ii) Assess whether, how, and where to present community-level data in EHRs; (iii) Identify where in the workflow these data are available and who on the primary care team should have access to this information. Step 3: (iii) Develop tools to facilitate referrals to community resources based on patient-reported SDH needs; (iv) Develop strategies to help primary care practices integrate up-to-date information on community resources into their EHRs. |
|
ASCEND: Approaches to CHC Implementation of SDH Data Collection and Action OCHIN is collaborating with Kaiser Permanente Center for Health Researchb on a follow-up study that builds on the important pilot work conducted through ASSESS (described above). This study will test a set of implementation support strategies for helping community health centers (CHCs) routinely identify and take action on the SDH-related needs of patients with or at risk of diabetes, using a pragmatic, stepped-wedge, cluster-randomized design across 30 CHCs. Funder: National Institutes of Diabetes and Digestive and Kidney Diseases (09/01/2015 – 08/31/2017) |
Step 1: (iv) Identify the most effective workflows to facilitate the collection of patient-reported SDH information; (v) Understand whether tools such as patient EHR portals, tablets, or other technologies can be leveraged to enable patients to self-report their SDH needs; Step 2: (iii) Identify where in the workflow these data are available and who on the primary care team should have access to this information; (iv) Determine whether and how primary care teams can and should use information on patient-reported or community-level SDH data to inform clinical decision-making; (v) Determine whether and how primary care teams should use information on patient-level SDH needs to prompt referrals to community resources. Step 3: (i) Identify which staffing models and training resources best represent how diverse clinic staff can act on patient-reported and/or community-level SDH data;(ii) Understand whether and how to create EHR-based triggers or alerts that recommend specific clinical actions based on patient-reported SDH n; (iii) Develop tools to facilitate referrals to community resources based on patient-reported SDH needs; (iv) Develop strategies to help primary care practices integrate up-to-date information on community resources into their EHRs. |
|
CLINCH-IT: Clinical Information Needs of CHCs for Health Information Technology Care. OCHIN is collaborating with Oregon Health & Science University (OHSU)b to identify clinician/clinical care team HIT needs for complex patients (including SDH complexity) & methods for integrating this information into EHRs to inform clinical decision making. Funder: Agency for Healthcare Research and Quality (05/01/2015 – 04/30/2019) |
Step 1: (i) Understand the information needs of care teams and which patient-reported SDH are most important to collect in primary care settings; (iii) Assess how providers feel about integrating the collection of these data into primary care workflows; (iv) Identify the most effective workflows to facilitate the collection of patient-reported SDH information. Step 2: (i) Develop EHR-based tools for presenting and summarizing patient-reported SDH information; (iv) Determine whether and how primary care teams can and should use information on patient- reported or community-level SDH data to inform clinical decision-making; (v) Determine whether and how primary care teams should use information on patient-level SDH needs to prompt referrals to community resources. * Researchers will identify design principles to rapidly develop and test HIT tools |
|
CATCH-UP: Community-based Health Information Technology (HIT) Tools for Cancer Screening and Health Insurance Promotion. OHSUb and OCHIN are collaborating to build and test EHR tools to improve insurance coverage and thereby increase cancer screening and prevention care in uninsured patients at community health centers. Funder: National Cancer Institute (07/01/2014 – 06/30/2019) |
Step 2: (i) Develop EHR-based tools for presenting and summarizing patient-reported SDH information. Step 3: (iii) Develop tools to facilitate referrals to community resources based on patient-reported SDH needs. * The tools for this study focus on insurance coverage, an important SDH factor. |
|
ADVANCE: Accelerating Data Value Across a National Community Health Center Network. ADVANCE Clinical Data Research Network, one of thirteen clinical data research networks (CDRNs) in the National Patient- Centered Clinical Research Network. OCHINb is collaborating with Health Choice Network and Fenway Health to create a Research Data Warehouse with patient- level EHR data from 2.6 million safety net patients across United States. As part of this effort, we are working with the Robert Graham Center and HealthLandscape to link geocoded with community- level SDH data with primary care clinical data and integrate this information into the ADVANCE Research Data Warehouse. Funder: Patient Centered Outcomes Research Institute (03/01/2016 – 08/01/2018) |
Step 1: (vi) Understand how primary care practices can obtain and integrate data on patients’ community-level SDH data into EHRs; (vii) Identify which community-level SDH are most relevant to patient health and most important to include in EHRs. |
|
Patient Complexity: The Impact of Patient Complexity on Healthcare Utilization. OCHINb is leading a collaboration between the ADVANCE and OneFlorida CDRNs to examine whether adding community vital signs to indices of clinical complexity (e.g., Charlson co-morbidity score) better predicts clinic-level risk for over-and under-utilization of services. Funder: Patient-Centered Outcomes Research Institute (09/01/2016 – 08/31/2017) |
Step 1: (vii) Identify which community-level SDH are most relevant to patient health and most important to include in EHRs. Step 4: (v) Integrate patient- reported and/or community- level SDH data into risk prediction and health care utilization models; (vi) Understand how SDH data collected in primary care settings could be used to identify gaps in needed local resources and trigger policy and advocacy. |
|
Enhance Care: Integrating Public Health Data into Primary Care Using Innovative Approaches. OCHIN is collaborating with OHSUb to describe and summarize past and current research on how community-level SDH have been used in primary care settings to support clinical decision-making to influence patient health. Funder: Pisacano Leadership Foundation |
Step 1: (vii) Identify which community-level SDH are most relevant to patient health and most important to include in EHRs. Step 2: (iv) Determine whether and how primary care teams can and should use information on patient-reported or community-level SDH data to inform clinical decision-making. |
Organization that received the grant award
As an extension of this work, in September 2017 we received funding for a sub-sequent project (Approaches to CHC Implementation of SDH Data Collection and Action, or ASCEND) to study the implementation of the EHR-based SDH tools across OCHIN’s national network of CHCs, understand barriers and facilitators associated with implementing the changes needed to collect and act on SDH data, and evaluate the effectiveness of a set of scalable, pragmatic implementation strategies designed to support SDH- related practice changes. Other projects that are planned and under review would examine patient and provider perspectives on the collection of SDH information in clinical settings and evaluate the utility and effectiveness of using tablets and other new HIT approaches for collecting patient-reported SDH data.
Also included in our current portfolio are studies that focus on the use of HIT to facilitate care coordination and insurance continuity for vulnerable populations. For example, CHCs provide care for complex patients who may have several concurrent physical, mental, and substance use comorbidities; many of these patients also face multiple SDH (e.g., food security, housing status) that affect their care. Yet little is known about the range of information that care teams need when caring for complex patients. To address this gap, researchers are conducting a mixed-methods study (Clinical Information Needs of CHCs for Health Information Technology Care, or CLINCH-IT) in 10 OCHIN CHCs to identify how care teams use EHRs and other HIT tools to coordinate care for complex patients. Based on these findings, the research team will work with EHR programmers to create prototypes of HIT tools to improve care delivery for this vulnerable population. Another project (Community-based Health Information Technology (HIT) Tools for Cancer Screening and Health Insurance Promotion, or CATCH-UP) is evaluating the utility and effectiveness of leveraging the EHR as a way for clinics to help improve insurance coverage and continuity, an important SDH, for their patient population. In response to needs identified by CHC staff, researchers worked with CHC stakeholders to develop an EHR-based tool that would flag uninsured patients who were eligible for coverage or alert front desk staff of an approaching insurance lapse.25 The CATCH-UP study is evaluating the effectiveness of this tool in 23 OCHIN clinics, by measuring the impact on rates of insurance coverage and utilization of cancer screening and prevention services.
In addition to understanding how to collect and use patient-reported SDH data, we are exploring how best to leverage publicly available data on community-level SDH data to provide additional context on the neighborhoods where our patients live. The Accelerating Data Value across a National Community Health Center Network (ADVANCE) clinical data research network (CDRN), led by OCHIN, was one of 13 CDRNs funded by the by the Patient Centered Outcomes Research Institute (PCORI) to build capacity for using data routinely collected in health care settings for clinical research.21 Per the recommendation of our stakeholders, we utilized a portion of this infrastructure funding to integrate a set of community-level SDH (geocoded at the county, ZIP Code Tabulation Area, and census tract level) with patient-level clinical data in our research data warehouse, using information on patient address.22 Leveraging this unique data resource, we received additional PCORI funding to assess whether community-level SDH factors contribute to variation in health care utilization and/or measures of clinic-level quality and performance (The Impact of Patient Complexity on Healthcare Performance, or Patient Complexity). In this project, we are investigating whether incorporating information on the social, economic and environmental characteristics of the neighborhoods where patients live into traditional quality of care metrics helps to explain variation in outcomes across settings. Despite the large body of research demonstrating the impact of SDH on health, clinical quality metrics typically emphasize disease specific, clinical outcomes and do not include SDH factors. Bringing together community-level SDH and clinical data in this way could provide health systems with additional information to organize and mobilize the resources needed to care for and improve the health of the populations they serve. This approach could also inform clinical quality measures and risk adjustment, especially as models of value-based reimbursement gain more prominence in the health care landscape.
We are also exploring approaches for incorporating community-level SDH data into EHR interfaces for use in panel management or at the point of care (Integrating Public Health Data into Primary Care Using Innovative Approaches, or Enhance Care). As described above, efforts to collect SDH information from individual patients require workflow changes and considerable effort on the part of clinics. On the other hand, information on the community-level SDH providing context on the neighborhoods where these patients live is available from public sources and could be integrated into EHRs so that the care team has information on a patient’s community vital signs, alongside their clinical vital signs, at their fingertips.22 In additional to providing valuable context on the factors that shape the health of individual patients, bringing community-level SDH information into the EHR could also inform efforts to identify critical needs in the community and/or target outreach efforts to particularly vulnerable sub-populations. Despite this promise, many questions remain about how to utilize community-level SDH data within primary care as well as the relative value of community vs. patient-level SDH information in a clinical setting. Future studies will continue to explore which community- level SDH are most important to consider as well as the best approaches for presenting community vital signs information within EHRs.
Conclusions and Next Steps
Emergent community laboratories16–21 provide new opportunities for conducting pragmatic research that could lead to substantial advances in building the processes and infrastructure needed for primary care settings to obtain and use SDH data. This paper outlines a research agenda (Box 1) to inform implementation of EHR-based tools and other HIT that include patient-reported and community-level SDH. As shown in Box 2, we have started to implement studies in the OCHIN community laboratory that address key components of this agenda.
Studies to date focus primarily on developing and testing approaches for integrating SDH using HIT (steps 1–3 of the framework). As outlined in Box 1, steps 1–3 of the framework focus on the process of collecting and organizing, presenting and integrating, and taking action to address identified SDH needs through referrals to community services, CDS, patient engagement, or care coordination. There are numerous questions across this span of activities that warrant continued research, including understanding the relationship between patient-reported and community-level SDH (and the relative value of including each in EHRs), whether and how care teams should use SDH data to inform clinical decision-making and/or target referrals to community resources, what workflows and staffing structures are needed to ensure successful integration of SDH into primary care, and how best to utilize HIT and EHRs to facilitate these efforts. Building on the studies described above, we will continue to move this body of science forward within the OCHIN network and through partnerships with other institutions and research networks.
Beyond these important questions of process and implementation, an integral area for future research will be to assess the impact of integrating SDH into primary care on the triple aim23 of enhancing patient experience of care, improving population health, and reducing costs (step 4 of the framework). It is essential that we evaluate the impact of integrating new initiatives to implement SDH screening in health care settings and the effectiveness of different mechanisms for taking action to address identified SDH needs. Towards this end, a critical next step is to develop a common framework for evaluating the impact of interventions to identify and address SDH in health settings, including primary care. The Social Interventions Research and Evaluation Network (SIREN), an inter-disciplinary group of practitioners and researchers, was formed recently to do just that.26 This group is working collaboratively to develop a conceptual framework that defines the boundaries, inputs, and outcomes of interventions to address SDH within the health care setting, with the goal of guiding future research and informing our collective efforts to improve the health of our patients. In sum, although there is a large body of literature documenting the relationship between SDH and health, future research is needed to understand whether and how to integrate identification of and action to address SDH into health care settings and to evaluate the impact of interventions. A stronger evidence base in this area will inform decision-making and best practices, and contribute to the effectiveness and sustainability of efforts to address SDH within the health care setting.
Acknowledgments
Funding: CLINCH-IT (R01 HS023324), ADVANCE (CDRN-1306–04716), ASSESS (R18 DK105463), PCORnet Health Systems Demonstration (HSD-1603–34987), CATCH-UP (R01 CA181452)
Footnotes
OCHIN is not an acronym, but was once.
References
- 1.World Health Organization. Social determinants of health. Genever, SUI: World Health Organization, 2016. Available at: www.who.int/social_determinants/en/. [Google Scholar]
- 2.McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff (Millwood). 2002. Mar-Apr;21(2):78–93. 10.1377/hlthaff.21.2.78 [DOI] [PubMed] [Google Scholar]
- 3.Institute of Medicine of the National Academies Committee on the recommended social and behavioral domains and measures for electronic health records. Capturing social and behavioral domains in Electronic Health Records: phase 2. Washington, DC: The National Academies Press; 2014. [PubMed] [Google Scholar]
- 4.Centers for Medicare & Medicaid Services. CMS quality strategy 2016. Baltimore, MD: Centers for Medicare & Mediciad Services, 2016. Available at: https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/qualityinitiativesgeninfo/downloads/cms-quality-strategy.pdf. [Google Scholar]
- 5.Centers for Medicare & Medicaid Services. MACRA: Delivery System Reform, Medicare Payment Reform. Baltimore, MD: Centers for Medicare & Mediciad Services, 2018. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.html. [Google Scholar]
- 6.Office of the National Coordinator for Health Information Technology. HITPC meaningful use stage 3 final recommendations. Washington, DC: United States Department of Health and Human Services, 2014. April 1 Available at: https://www.healthit.gov/facas/sites/faca/files/HITPC_MUWG_Stage3_Recs_2014-04-01.pdf. [Google Scholar]
- 7.Billioux A, Verlander K, Anthony S, et al. Standardized screening for health-related social needs in clinical settings: the accountable health communities screening tool. Washington, DC: National Academy of Medicine, 2017. May 30 Available at: https://nam.edu/wp-content/uploads/2017/05/Standardized-Screening-for-Health-Related-Social-Needs-in-Clinical-Settings.pdf. [Google Scholar]
- 8.DeVoe JE, Bazemore AW, Cottrell EK, et al. Perpsectives in primary care: a conceptual framework and a path for integrating social determinants of health into primary care practice. Ann Fam Med. 2016. Mar-Apr;14(2):104–8. 10.1370/afm.1903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garg A, Jack B, Zuckerman B. Addressing the social determinants of health within the patient-centered medical home: lessons learned from pediatrics. JAMA. 2013. May 15;309(19):2001–2. 10.1001/jama.2013.1471 [DOI] [PubMed] [Google Scholar]
- 10.Kaufman A Theory vs. practice: should primary care practice take on social determinants of health now? yes. Ann Fam Med. 2016. Mar-Apr;14(2):100–1. 10.1370/afm.1915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Academy of Family Physicians Social Determinants of Health Policy. Available at: https://www.aafp.org/about/policies/all/social-determinants.html. Accessed June 2018.
- 12.Gottlieb LM, Ackerman S, Wing H, et al. Evaluation Activities and Influences at the Intersection of Medical and Social Services. JHCPU. 2017. August 3;28(3):e162521 10.1353/hpu.2017.0089 [DOI] [PubMed] [Google Scholar]
- 13.Gottlieb LM, Tirozzi KJ, Manchanda R, et al. Moving electronic medical records upstream: incorporating social determinants of health. Am J Prev Med. 2015. February;48(2):215–8. 10.1016/j.amepre.2014.07.009 [DOI] [PubMed] [Google Scholar]
- 14.Institute for Alternative Futures. Community health centers leveraging the social determinants of health. Alexandria, VA: Institute for Alternative Futures, 2012. March Available at: http://www.altfutures.org/pubs/leveragingSDH/IAF-CHCsLeveragingSDH.pdf. [Google Scholar]
- 15.Matthews KA, Adler NE, Forrest CB, et al. Collecting psychosocial “vital signs” in electronic health records: why now? what are they? what’s new for psychology? Am Psychol. 2016. September;71(6):497–504. 10.1037/a0040317 [DOI] [PubMed] [Google Scholar]
- 16.Oregon Community Health Information Network (OCHIN). About us. Portland, OR: OCHIN, Inc., 2016. Available at: http://www.ochin.org/about-us/. [Google Scholar]
- 17.DeVoe JE, Gold R, Spofford M, et al. Developing a network of community health centers with a common electronic health record: description of the safety net west practice-based research network (SNW-PBRN). J Am Board Fam Med. 2011. Sep-Oct;24(5):597–604. 10.3122/jabfm.2011.05.110052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DeVoe JE, Likumahuwa S, Eiff MP, et al. Lessons learned and challenges ahead: report from the OCHIN Safety Net West practice-based research network (PBRN). J Am Board Fam Med. 2012. Sep-Oct;25(5):560–4. 10.3122/jabfm.2012.05.120141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DeVoe JE, Sears A. The OCHIN community information network: bringing together community health centers, information technology, and data to support a patient-centered medical village. J Am Board Fam Med. 2013. May-Jun;26(3):271–8. 10.3122/jabfm.2013.03.120234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Likumahuwa S, Song H, Singal R, et al. Building research infrastructure in community health centers: a Community Health Applied Research Network (CHARN) report. J Am Board Fam Med. 2013. Sep-Oct;26(5):579–87. 10.3122/jabfm.2013.05.130025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.DeVoe JE, Gold R, Cottrell E, et al. The ADVANCE network: accelerating data value across a national community health center network. J Am Med Inform Assoc. 2014. Jul-Aug;21(4):591–5. 10.1136/amiajnl-2014-002744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bazemore AW, Cottrell EK, Gold R, et al. “Community vital signs”: incorporating geocoded social determinants into electronic records to promote patient and population health. J Am Med Inform Assoc. 2016. March;23(2):407–12. 10.1093/jamia/ovc088 [DOI] [PubMed] [Google Scholar]
- 23.Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff. 2008. May-Jun;27(3):759–69. 10.1377/hlthaff.27.3.759 [DOI] [PubMed] [Google Scholar]
- 24.Gold R, Cottrell EK, Bunce A, Middendorf M, Hollombe C, Cowburn S, Mahr P, Melgar G. Developing Electronic Health Record (EHR) strategies related to health center patients’ social determinants of health. J Am Board Fam Med. 2017. Jul-Aug;30(4):428–47. 10.3122/jabfm.2017.04.170046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.DeVoe JE, Huguet N, Likumahuwa-Ackman S, et al. Testing health information technology tools to facilitate health insurance support: a protocol for an effectiveness-implementation hybrid randomized trial. Implement Sci. 2015. August 25;10:123 10.1186/s13012-015-0311-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gottlieb L, Fichtenberg C, Adler N. Introducing the Social Interventions Research and Evaluation Network. San Francisco, CA: SIREN, 2017. February 27 Available at: https://sirenetwork.ucsf.edu/sites/sirenetwork.ucsf.edu/files/SIREN_Issue_Brief_Updt.pdf. [Google Scholar]