Abstract
Objective:
The current study examined whether variations in patient weight and eating-disorder behavior frequency influenced the recognition of bulimia nervosa (BN) and the perception that it is a serious mental health concern.
Method:
Participants (N=320) were randomly assigned to one of six conditions in which they read a vignette describing a young woman with BN. Each vignette was identical except for the variables of interest: weight status (underweight, healthy-weight, overweight), and symptom frequency (daily or weekly binge-eating episodes and purging).
Results:
Participants were more likely to have negative attitudes toward and blame the patient with overweight. Participants were less likely to believe that the patient with overweight was experiencing mental illness and that her problems were too serious to handle on her own. There were no significant differences by symptom frequency.
Conclusion:
Findings suggest the presence of weight stigma and that overweight might impede the recognition of eating disorders.
Keywords: bulimia nervosa, eating disorders, obesity, treatment barriers, stigma
Introduction
Bulimia nervosa (BN) is a serious mental health problem associated with physical health complications and impaired psychosocial functioning in home, work, personal, and social environments (Marques et al., 2011; Sheehan, Harnett-Sheehan, & Raj, 1996; Udo & Grilo, 2018). Estimates suggest that less than two-thirds of patients with BN seek treatment for their eating disorder (Coffino, Udo, & Grilo, 2019). While individuals with BN may recognize that they have a problem, barriers to treatment such as shame and fear of change can prevent them from seeking help on their own (Hepworth & Paxton, 2007; Innes, Clough, & Casey, 2017; Rodgers et al., 2015). BN, as a psychiatric disorder, also carries mental health stigma. BN can go undetected by friends and family because individuals may not display severe external symptoms, such as those that are characteristic of anorexia nervosa (AN; e.g., emaciation). In fact, individuals with BN are more likely be healthy-weight or overweight with median BMI around 27 (Masheb & White, 2012; Udo & Grilo, 2018), and may be less likely to receive treatment if they are not underweight (Bulik, Marcus, Zerwas, Levine, & La Via, 2012). Additionally, the social desirability of weight loss and belief that it enhances appearance, a belief that stigmatizes excess weight, can make treatment aimed at stopping extreme weight-control behaviors aversive (Star, Hay, Quirk, & Mond, 2015). Eating-disordered behaviors, including binge eating and extreme weight-control behaviors, can be secretive (Boggiano, Turan, Maldonado, Oswald, & Shuman, 2013) due to associated feelings of embarrassment or guilt (American Psychiatric Association, 2013). Health providers can also fail to detect BN if they do not screen for eating disorders or if patients do not disclose symptoms during appointments; these barriers to detection could also interrelate, for example, if patients are less likely to disclose behaviors that they are not asked about directly (Anderson, Accurso, Kinasz, & Le Grange, 2017; Mond, Hay, Rodgers, & Owen, 2007; Thompson-Brenner, Satir, Franko, & Herzog, 2012). Individuals can appear healthy at medical appointments, but more thorough clinical interviewing and medical testing (e.g., electrolyte imbalances) can identify signs of BN. Taken together, failure to identify BN by individuals themselves, friends and family, and health care providers, suggests a need for increased awareness about BN, as well as increased familiarity with appropriate referrals to facilitate treatment when indicated.
Stigma in any form can be a barrier to seeking treatment; individuals with BN experience mental health stigma and, if they also have excess weight, weight stigma (Puhl & Suh, 2015). Stigma includes attribution of negative personal characteristics to the individual, blaming the individual (e.g., perceiving symptoms as “choices”), and maintaining social distance from that individual (Hinshaw & Stier, 2008). Obesity and eating disorders are stigmatized when negative personal characteristics are attributed to an individual because of obesity (weight stigma) or an eating disorder (mental health stigma), or when the individual is blamed or held personally responsible for obesity (weight stigma) or an eating disorder (mental health stigma) (Puhl & Suh, 2015). Mental health stigma is associated with psychological distress, weaker social support networks (Hackler, 2010; Hinshaw & Stier, 2008), exacerbated feelings of shame (Puhl & Suh, 2015), and negative treatment-seeking attitudes (Seamark & Gabriel, 2018), all of which could impede proper management of eating disorders. Likewise, weight stigma is associated with poorer psychological functioning, shame, and inconsistent health care providers (Puhl & Heuer, 2010; Puhl, Peterson, & Luedicke, 2013; Puhl & Suh, 2015). Moreover, weight stigma and eating disorder stigma can interact: weight stigma is associated with eating-disordered behaviors, and both forms of stigma can be internalized as self-blame (Puhl & Suh, 2015). The notable difference between mental health and weight stigma is that weight cannot be easily masked or hidden, thus an individual may be more vulnerable to experiencing weight discrimination than experiencing discrimination related to mental health.
Aims and Hypotheses
The purpose of the current study was to determine whether variations in patient weight status (underweight, healthy-weight, overweight) and symptom frequency (daily, weekly) influenced the recognition of BN and its classification as a serious mental health concern. We hypothesized that participants who read the vignette about a patient with more frequent BN behaviors (daily binge eating and purging rather than weekly) would perceive a more serious medical problem and be less likely to view the symptoms as voluntary or controllable even though both daily and weekly symptom frequencies meet criteria for BN (American Psychiatric Association, 2013). We also hypothesized that participants who read the vignette about a patient whose weight was in the overweight range would report more negative attitudes about the patient than participants who read the vignettes about patients with healthy-weight or underweight, because of the stigma associated with excess weight. Finally, we hypothesized that participants who read the vignette about a patient whose weight was in the underweight range would be more likely to recommend intervention because of the consistency of underweight with traditional stereotypes of eating disorders.
Methods
Participants
Participants (N=320) were recruited through Amazon’s Mechanical Turk website, which is an online labor market that advertises, among other tasks, research surveys to potential workers. Mechanical Turk provides convenient and reliable data that are generally more demographically-diverse than both college student samples and samples recruited by traditional methods such as listservs or in-person recruitment (Behrend, Sharek, Meade, & Wiebe, 2011; Buhrmester, Kwang, & Gosling, 2011). Participants recruited from Mechanical Turk also provide higher quality data compared to other online recruitment methods (Behrend et al., 2011). In part, this is because Mechanical Turk allows for quality control from the platform as well as validity checks for the research team to review response quality. In the current study, we required approval ratings to exceed 85%, and also included three items throughout the survey to assess effort and attention in line with recommendations (Buhrmester et al., 2011), and two questions at the end of the vignettes that checked for attention to the vignette content (“what was the name of the patient in the story you just read” and “what kind of information did you read about the patient”). Participants were excluded if they did not provide a correct answer to validity items.
Participants were between 21 and 70 years old (M=35.5, SD=12.0) and included both women (n=221, 69.1%) and men (n=97, 30.3%). Participants self-identified their race as White (n=251, 78.4%), Asian (n=27, 8.4%), Black (n=17, 5.3%), or other (n=25, 7.8%). Ethnicity was Hispanic (n=15, 4.7%) and not Hispanic (n=305, 95.3%). Participants were highly educated on average: high school or less (n=45, 14.1%), some college (n=101, 31.5%), or college degree or higher (n=174, 54.4%). This study received approval from our university’s research ethics review board. All participants provided electronic informed consent. The data that support the findings of this study are available from the corresponding author upon reasonable request.
Materials
Vignettes were created describing the results of a recent annual physical for “Emily,” a fictitious patient with BN, in the style of a primary care provider’s medical note. For the text of the vignettes, please see Online Supplemental Materials. Vignette experiments provide reliable data about public attitudes toward mental health (Link, Yang, Phelan, & Collins, 2004). Our vignettes described a 21-year-old female college student who met diagnostic criteria for BN as specified by DSM-5. Each vignette included a vitals table (weight, BMI, heart rate, temperature, blood pressure), with columns indicating the normal range, the patient’s result, and whether the result was outside the normal range. A short description of the patient’s presentation followed the vitals table and included thoughts, behaviors, and functioning. There were three weight conditions and two symptom frequency conditions for a total of six vignettes. The weight conditions varied the BMI of the fictitious patient: underweight (BMI=17.7 kg/m2), healthy-weight (BMI=21.5 kg/m2), and overweight (BMI=25.2 kg/m2). For the underweight and overweight conditions, we selected weights that produced BMIs only slightly below or above the healthy-weight range. Frequency conditions varied the concluding statement of the health care provider’s note about the frequency of binge-eating and purging episodes (daily or weekly).
Procedure
Participants were randomly assigned to one of six vignettes (underweight-daily; healthy-weight-daily; overweight-daily; underweight-weekly; healthy-weight-weekly; overweight-weekly). After reading the vignette, participants made treatment recommendations as though they were the patient’s health care provider and rated how much they agreed with statements about the patient’s condition and character.
Measures
MacArthur Mental Health Module.
Participants’ attitudes about mental health were assessed using items from the 1996 MacArthur Mental Health Module, a mental health stigma survey that is available for public use (Martin, Pescosolido, & Tuch, 2000; Pescosolido, Monahan, Link, Stueve, & Kikuzawa, 1999). Items were scored from −2 (strongly disagree) to +2 (strongly agree). Items have been used to evaluate mental health stigma across populations and conditions (Pescosolido, Medina, Martin, & Long, 2013; Phelan, Link, Stueve, & Pescosolido, 2000). The current study assessed attitudes toward the condition (e.g., “Emily is experiencing a mental illness”), including its consequences (e.g., “Emily’s eating and weight concerns could cause her to be more impulsive and make poorer decisions”). Items also evaluated participants’ attitudes towards the patient (e.g., “Emily is lazy”). Items from this scale have demonstrated good internal reliability in a variety of epidemiological studies measuring attitudes toward mental illness (Link et al., 2004). All attitude/belief items are included in Table 1. In the current study, the items used from the scale yielded internally consistent scores (α=.88).
Table 1.
Beliefs and attitudes by vignette weight condition.
|
Underweight (n=104) |
Healthy-weight (n=104) |
Overweight (n=112) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | F | p | ηp2 | |
| Emily’s problems are serious. | 1.34 | 0.96 | 1.22 | 1.00 | 1.02 | 1.15 | 2.54 | .080 | .016 |
| Emily needs help. | 1.55 OW | 0.82 | 1.38 | 0.97 | 1.19 UW | 1.08 | 3.72 | .025 | .023 |
| These problems are too serious for Emily to handle on her own. | 0.99 OW | 1.10 | 0.88 | 1.11 | 0.58 UW | 1.34 | 3.35 | .036 | .021 |
| Emily is experiencing the usual ups and downs. | −0.54 | 1.34 | −0.42 | 1.25 | −0.29 | 1.23 | 1.00 | .369 | .006 |
| Emily is experiencing a physical illness. | 0.15 | 1.33 | 0.00 | 1.30 | −0.11 | 1.23 | 1.09 | .336 | .007 |
| Emily is experiencing a mental illness. | 1.23 OW | 0.93 | 1.03 | 1.18 | 0.74 UW | 1.22 | 5.18 | .006 | .032 |
| A friend, family member, or important community member could help Emily. | 0.94 | 1.09 | 0.72 | 1.16 | 0.82 | 1.10 | 1.00 | .370 | .006 |
| Emily would get better if she just gave it some time. | −0.89 | 1.25 | −0.76 | 1.14 | −0.58 | 1.17 | 1.91 | .150 | .012 |
| Emily should not need help with these problems | −1.06 | 1.20 | −1.05 | 1.08 | −0.95 | 1.11 | 0.33 | .719 | .002 |
| Emily’s eating and weight concerns could affect her relationships with others. | 1.27 OW | 0.78 | 0.93 | 0.99 | 0.99 UW | 0.92 | 4.15 | .017 | .026 |
| Emily’s eating and weight concerns could cause her to be more impulsive and make poorer decisions. | 1.12 | 0.90 | 0.97 | 0.98 | 0.85 | 0.90 | 2.24 | .108 | .014 |
| Emily’s eating and weight concerns may make it difficult to go to work or school. | 1.05 OW | 0.95 | 0.77 | 1.00 | 0.63 UW | 1.07 | 4.67 | .010 | .029 |
| Emily’s eating and weight concerns may prevent her from achieving her full potential. | 1.13 | 0.91 | 1.10 | 0.96 | 0.99 | 1.01 | 0.65 | .521 | .004 |
| Emily would be leading a better life if she put in more effort. | −0.47 | 1.12 | −0.58 OW | 1.06 | −0.13 HW | 1.24 | 4.40 | .013 | .027 |
| Emily is lazy. | −1.50 | 0.82 | −1.49 | 0.79 | −1.26 | 0.90 | 2.88 | .058 | .018 |
| Emily is to blame for her situation. | −1.06 OW | 0.94 | −1.03 OW | 0.92 | −0.63 UW, HW | 1.15 | 6.01 | .003 | .037 |
Note. Positive scores indicate greater agreement or recommendation. Mean scores for attitudes and beliefs could range from −2 to 2. Post-hoc comparisons used a Tukey HSD correction for multiple comparisons.
p<.05 difference from underweight vignette;
p<.05 difference from healthy-weight vignette;
p<.05 difference from overweight vignette.
Participants also reported their own mental health experience by answering questions about their contact with mental health treatments and providers (e.g., “Have any of your friends or family members experienced a mental health problem?”). Items assessing mental health experience were also taken from the 1996 Macarthur Mental Health Module (Pescosolido et al., 1999). In the current study, the items used from the scale yielded internally consistent scores (α=.86).
Treatment Recommendations.
Participants reported whether they would recommend various treatments if they were the patient’s health care provider. Recommendations were coded yes (1), maybe (0), or no (−1). Treatment recommendations ranged from seeing “Emily” at her next annual physical, to suggesting that she eat right and exercise more, to referring her to a personal trainer; all recommendations are listed in Table 2.
Table 2.
Treatment recommendations by vignette weight condition.
|
Underweight (n=104) |
Healthy-weight (n=104) |
Overweight (n=112) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | F | p | ηp2 | |
| Self-help (magazine, book) | 0.00 | 0.75 | −0.19 | 0.76 | 0.00 | 0.71 | 2.41 | .091 | .015 |
| Fad/Crash Diet (cabbage soup, liquid diets, etc.) | −0.82 | 0.54 | −0.81 | 0.48 | −0.71 | 0.61 | 1.43 | .240 | .009 |
| Supervised Program (Wt Watchers, Jenny Craig, OA) | −0.58 OW | 0.63 | −0.42 OW | 0.69 | −0.03 UW, HW | 0.80 | 17.28 | <.001 | .099 |
| Prescribed Diet Pills (Amphet, Redux, Fen-phen) | −0.83 OW | 0.47 | −0.84 OW | 0.42 | −0.61 UW, HW | 0.63 | 6.79 | .001 | .041 |
| Dietician/Nutritionist-Lsed Program | 0.49 | 0.72 | 0.41 | 0.65 | 0.51 | 0.68 | 0.61 | .543 | .004 |
| Psychologist/Psychiatrist/Other Mental Health | 0.78 OW | 0.48 | 0.67 | 0.61 | 0.52 UW | 0.63 | 5.53 | .004 | .034 |
| See her at her next annual physical | 0.45 | 0.83 | 0.55 | 0.75 | 0.47 | 0.80 | 0.43 | .651 | .003 |
| Have a mid-year check-up | 0.71 | 0.62 | 0.67 | 0.58 | 0.56 | 0.71 | 1.56 | .212 | .010 |
| Referral to a mental health professional | 0.67 OW | 0.55 | 0.49 | 0.72 | 0.46 UW | 0.72 | 3.19 | .042 | .020 |
| Referral to a dietician | 0.44 | 0.75 | 0.40 | 0.74 | 0.54 | 0.66 | 1.01 | .366 | .006 |
| Prescription for psychiatric medication | −0.35 OW | 0.72 | −0.53 | 0.64 | −0.56 UW | 0.67 | 3.15 | .044 | .020 |
| Referral to a personal trainer/exercise plan | −0.40 OW | 0.76 | −0.38 OW | 0.71 | 0.02 UW, HW | 0.76 | 11.19 | <.001 | .067 |
| Suggest eating right and exercising more | 0.12 OW | 0.84 | 0.19 OW | 0.81 | 0.65 UW, HW | 0.63 | 15.65 | <.001 | .091 |
| Prescription for weight-loss medication | −0.83 | 0.49 | −0.80 | 0.51 | −0.70 | 0.66 | 1.69 | .186 | .011 |
Note. Positive scores indicate greater average endorsement of the recommendation (scored as −1=no, 0=maybe, 1=yes).
p<.05 difference from underweight vignette;
p<.05 difference from healthy-weight vignette;
p<.05 difference from overweight vignette.
Statistical Analyses
Analyses of variance (ANOVAs) evaluated participants’ attitudes about the patient with BN by symptom severity (daily, weekly) and body weight (underweight, healthy-weight, overweight). Post-hoc tests used a Tukey correction for multiple comparisons. Pearson product-moment correlations examined relations between mental health experiences and perceptions of the patient. Statistical analyses were considered significant at p < .05.
Results
Participants’ beliefs about Emily’s presenting problems are summarized in Table 1. Participants were more likely to believe the following in the underweight than overweight conditions but healthy-weight did not differ significantly from other groups: “Emily needs help”; “These problems are too serious for Emily to handle on her own”; and “Emily is experiencing a mental illness.” Notably, mean scores reflected participants in all conditions believed that Emily needed help.
Participants’ attitudes about Emily are also summarized in Table 1. Participants were more likely to hold the following attitudes in the underweight condition than overweight: “Emily’s eating and weight concerns may make it difficult to go to work or school” and “Emily’s eating and weight concerns could affect her relationships with others.” “Emily would be leading a better life if she put in more effort” showed stronger disagreement for healthy-weight than overweight. “Emily is to blame for her situation” showed stronger disagreement in both healthy-weight and underweight conditions than overweight. Mean scores reflected that participants across conditions disagreed with the idea that Emily was “lazy.”
Results for treatment recommendations by vignette weight condition are presented in Table 2. Participants were more likely to recommend that Emily attend a supervised weight-loss program or receive a prescription for diet pills when binge/purge behaviors were portrayed with overweight than underweight and healthy-weight. Participants were also more likely to recommend a personal trainer or suggest eating right and exercising more when weight status was overweight compared with underweight and healthy-weight. Participants were more likely to recommend a mental health professional and psychiatric medication when BN was portrayed with underweight than overweight.
There was one significant interactions for treatment recommendations: dietician-led program, F(2,314)=3.33, p=.037, ηp2=021 (see Figure 1). Whereas a dietician-led program was more likely to be recommended for BN portrayed with underweight when binge/purge behaviors were daily (p=.042), recommendations for a dietician-led program did not significantly differ by binge/purge frequency when BN was portrayed with healthy-weight (p=.352) or overweight (p=270).
Figure 1.
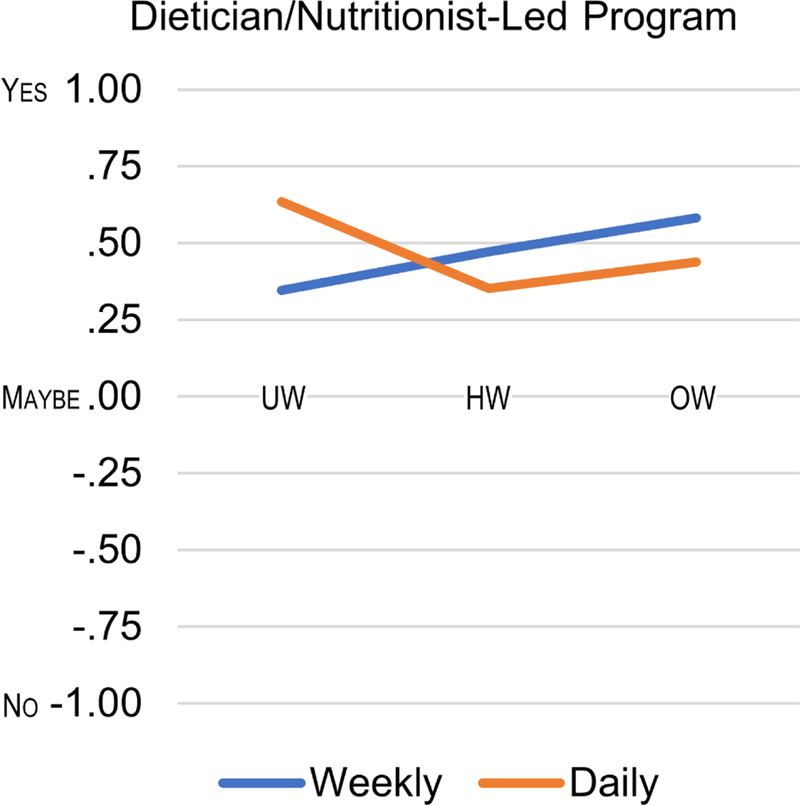
Recommendations to refer patient to a dietician-led program.
Note. Dietician-led program more likely to be recommended for bulimia nervosa portrayed with underweight when binge/purge behaviors were daily (p=.042); recommendations did not significantly differ by binge/purge frequency when bulimia nervosa was portrayed with healthy-weight (p=.352) or overweight (p=.270). UW = underweight, HW = healthy-weight, and OW=overweight.
Interactions were not significant for any other attitude, belief, or treatment recommendation variables. Symptom frequency was not significantly associated with any of the attitude, belief, or treatment recommendations.
Discussion
The current study used a vignette experimental design to provide new insight into how people may perceive individuals with BN. Weight, but not binge/purge frequency, influenced participants’ perceptions of BN. The overall pattern of results suggested that participants viewed BN as a serious psychiatric condition when the patient with BN had underweight but viewed the patient with BN as having a weight problem when she had overweight. Moreover, stigmatizing items (e.g., “Emily is to blame for her situation”) were endorsed more in the overweight condition than healthy-weight or underweight conditions, which provides more evidence of weight stigma than mental health stigma. As predicted, participants were more likely to assign blame toward the fictitious patient with BN if portrayed with overweight than if BN was portrayed with healthy-weight or underweight. Participants also perceived greater impairment (relational, work/school) for BN portrayed with underweight than overweight. However, contrary to expectations and to severity specifiers in the DSM-5, participants’ perceptions of the patient with BN did not significantly differ by the frequency of binge/purge episodes.
When participants were asked to imagine they were the patient’s health care provider, participants were most likely to recommend weight loss strategies after reading the vignette portraying BN with overweight than healthy-weight or underweight, although most of the weight-loss recommendations were not highly endorsed. On the other hand, participants were more likely to recommend mental health treatment and psychiatric medication for BN with underweight than overweight. This coincides with the stronger belief in the underweight than in the overweight condition that the patient with BN was “experiencing a mental illness.” Together, this suggests that overweight may have changed participants’ prioritization of binge/purge behaviors as a serious mental health issue. This finding is important to consider in light of the fact that the condition in which BN was portrayed with overweight just met criteria for having a BMI in the overweight range. It is possible that an even higher BMI (e.g., a BMI in the “severe obesity” range) could have resulted in even higher weight stigma and/or recommendation of weight-loss strategies. However, it is also possible that the “overweight” label attached to weight and BMI in the vignettes garnered participants’ attention rather than an evaluation of how much the weight and BMI were outside of the normal range that was also listed in the vignette. Similarly, the condition in which BN was portrayed with underweight was just under the normal range (103 lbs compared to 108 lbs), however, it is possible that participants responded to the “underweight” label and viewed the condition as similar to anorexia nervosa binge/purge subtype, even in the absence of other key features of anorexia nervosa such as dietary restraint, fear of weight gain, and/or weight loss. As vignettes and questions did not name eating disorders by their diagnostic label, we were unable to assess how participants may or may not have categorized “Emily’s” condition. Further research should test these labels experimentally. While it is promising that participants recognized the need for patients with BN and underweight to receive mental health treatment, formal recommendations for mental health treatment are independent of weight and recommended for all individuals with BN (American Psychiatric Association, 2013; National Institute for Health and Care Excellence, 2017). This highlights the need for increased mental health literacy efforts, such as eating-disorder awareness campaigns in schools or other communities, helping increase public awareness of evidence-based treatments for eating disorders and other mental illnesses across the weight spectrum.
Weight status also affected participants’ perceptions of potential impairment related to the patient’s binge/purge behaviors. Participants who read the vignettes portraying BN with overweight were less likely to view the patient’s problems as leading to difficulties with relationships or work/school, particularly compared with BN and underweight. These findings suggest that weight status might, potentially, be interpreted as a severity marker in the sense that patients who are lower weight might be viewed as being more “successful” at purging. Thus, it appears that weight status in the overweight vignettes was a salient factor, whereas the eating-disorder behaviors were more evident in the absence of overweight, when the vignette patient was portrayed as more consistent with the eating-disorder stereotype (underweight). These results further suggest a need for an increase in mental health literacy regarding the presence of BN across the weight spectrum.
The finding that attitudes did not differ by symptom frequency was unexpected. It is possible that participants, who each viewed only one vignette, did not notice the frequency level, but rather the presence of binge/purge behaviors. Additionally, it is unlikely that a large proportion of participants were health care providers, thus they may have had little expertise in eating-disorder diagnostic criteria. As such, it is possible that participants did not understand that daily or weekly binge/purge behaviors might mark a meaningful difference. Without an anchor or reference to other severity levels, participants may have perceived similar severity across conditions.
There are several strengths and limitations to consider when interpreting the results of the present study. Mechanical Turk provides data from participants who tend to be internally motivated, which has been shown to produce high-quality data with greater diversity in age and geography than other recruitment sources, such as undergraduate research pools (Behrend et al., 2011; Buhrmester et al., 2011), and has been used with vignette methodology (Ohan, Ellefson, & Corrigan, 2015). Our study sample was predominately White and highly educated, thus limiting the generalizability of the study findings to more diverse samples. It is also important to note that while the vignette experiment design has been frequently and reliably used in studies measuring mental health stigma, results they yield do not necessarily reflect people’s attitudes or thoughts about a person with BN that they may encounter in their lives (Link et al., 2004). In a vignette experiment, the person described remains an abstract idea because participants are told that the patient is fictitious, and thus are unlikely to be as emotionally invested in the patient’s wellbeing as they would be in a person in their lives. While the current study presents important preliminary findings on the effect of weight status on attitudes toward individuals with eating disorders, more research is needed to understand the link between weight status and perception of eating-disorder symptoms and seriousness. For example, we do not know why participants selected the recommendations they made; qualitative research exploring perceptions and motivations would complement the current work. Further research is also needed to test whether weight impacts how people perceive other types of patients with BN, such as males, older or younger patients, or patients from specific racial/ethnic groups. Additionally, this work should be replicated among health care providers to evaluate whether their perceptions of BN are similarly influenced by weight status.
Despite these limitations, our findings are important because they provide some insight as to how people may view a person with BN when weight varies. Little research has been done to investigate how a person’s attitude toward someone engaging in eating-disorder behaviors may differ based on this person’s weight status, and none of this research has been experimental. These results demonstrate the need for increased public awareness of eating disorders, specifically, that eating disorders are serious illnesses that require evidence-based treatment regardless of weight. People with BN can fail to receive treatment because they often have a BMI in the normal weight range (e.g., Bulik et al., 2012). Increased public awareness could potentially increase help-seeking among those with BN, as more knowledge may lead to more treatment-seeking personally or suggesting seeking help to family or friends (Cusack, 2004; Dew, 1991). In addition to efforts to increase awareness that BN occurs across the weight spectrum, public health efforts could seek to foster more positive (less stigmatizing) attitudes toward excess weight, which could facilitate seeking treatment for eating and weight concerns (Griffiths, Rossell, Mitchison, Murray, & Mond, 2018; Kelly, Jorm, & Wright, 2007).
Overall, results from the current study indicate that participants’ beliefs about and treatment recommendations for BN differ based on weight status. Participants were more likely to have negative attitudes toward and blame patients when BN was portrayed with overweight, and were more likely to perceive BN portrayed with underweight as having a serious mental illness that impairs functioning. Results highlight the need for increased awareness as to how clinical characteristics can influence perceptions or detection of BN. Proper use of knowledge can motivate action toward increasing mental health literacy, thereby potentially increasing treatment-seeking rates and potentially prognoses of individuals with BN.
Supplementary Material
Acknowledgments
Funding: This research was supported, in part, by National Institutes of Health grant K24 DK070052. Funders played no role in the content of this paper.
Footnotes
Potential conflicts of interest: The authors report no conflicts of interest. Dr. Grilo reports several broader interests which did not influence this research or paper. Dr. Grilo’s broader interests include: Consultant to Sunovion and Weight Watchers; Honoraria for lectures, CME activities, and presentations at scientific conferences and Royalties from Guilford Press and Taylor & Francis Publishers for academic books.
References
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Anderson K, Accurso EC, Kinasz KR, & Le Grange D (2017). Residents’ and Fellows’ Knowledge and Attitudes About Eating Disorders at an Academic Medical Center. Acad Psychiatry, 41, 381–384. doi: 10.1007/s40596-016-0578-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behrend TS, Sharek DJ, Meade AW, & Wiebe EN (2011). The viability of crowdsourcing for survey research. Behav Res Methods, 43, 800–813. doi: 10.3758/s13428-011-0081-0 [DOI] [PubMed] [Google Scholar]
- Boggiano MM, Turan B, Maldonado CR, Oswald KD, & Shuman ES (2013). Secretive food concocting in binge eating: Test of a famine hypothesis. Int J Eat Disord, 46, 212–225. doi: 10.1002/eat.22077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buhrmester M, Kwang T, & Gosling SD (2011). Amazon’s Mechanical Turk: A new source of inexpensive, yet high-quality, data? Perspect PsycholSci, 6, 3–5. doi: 10.1177/1745691610393980 [DOI] [PubMed] [Google Scholar]
- Bulik CM, Marcus MD, Zerwas S, Levine MD, & La Via M (2012). The changing “weightscape” of bulimia nervosa. Am J Psychiatry, 169, 1031–1036. doi: 10.1176/appi.ajp.2012.12010147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffino JA, Udo T, & Grilo CM (2019). Rates of Help-seeking in U.S. adults with Lifetime DSM-5 Eating Disorders: Prevalence Across Diagnoses and Sex and Ethnic/Racial Differences. Mayo Clin Proc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cusack J, Deane FP, Wilson CJ, & Ciarrochi J . (2004). Who influence men to go to therapy? Reports from men attending psychological services. . Int J Adv Couns(26), 271–283. [Google Scholar]
- Dew MA, Bromet EJ, Schulberg HC, Parkinson DK, & Curtis EC . (1991). Factors affecting service utilization for depression in a white collar population. Soc Psychiatry Psychiatr Epidemiol, 26(5), 230–237. [DOI] [PubMed] [Google Scholar]
- Griffiths S, Rossell SL, Mitchison D, Murray SB, & Mond JM (2018). Pathways into treatment for eating disorders: A quantitative examination of treatment barriers and treatment attitudes. Eat Disord, 26, 556–574. doi: 10.1080/10640266.2018.1518086 [DOI] [PubMed] [Google Scholar]
- Hackler AH, Vogel DL, & Wade NG (2010). Attitudes toward seeking professional help for an eaing disorder: The role of stigma and anticipated outcomes. Journal of Counseling & Development, 88(4), 424–431. doi: 10.1002/j.1556-6678.2010.tb00042.x [DOI] [Google Scholar]
- Hepworth N, & Paxton SJ (2007). Pathways to help-seeking in bulimia nervosa and binge eating problems: a concept mapping approach. Int J Eat Disord, 40, 493–504. doi: 10.1002/eat.20402 [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, & Stier A (2008). Stigma as related to mental disorders. Annu Rev Clin Psychol, 4, 367–393. doi: 10.1146/annurev.clinpsy.4.022007.141245 [DOI] [PubMed] [Google Scholar]
- Innes NT, Clough BA, & Casey LM (2017). Assessing treatment barriers in eating disorders: A systematic review. Eat Disord, 25, 1–21. doi: 10.1080/10640266.2016.1207455 [DOI] [PubMed] [Google Scholar]
- Kelly CM, Jorm AF, & Wright A (2007). Improving mental health literacy as a strategy to facilitate early intervention for mental disorders. Med J Aust, 187(7 Suppl), S26–30. [DOI] [PubMed] [Google Scholar]
- Link BG, Yang LH, Phelan JC, & Collins PY (2004). Measuring mental illness stigma. Schizophr Bull, 30, 511–541. [DOI] [PubMed] [Google Scholar]
- Marques L, Alegria M, Becker AE, Chen CN, Fang A, Chosak A, & Diniz JB (2011). Comparative prevalence, correlates of impairment, and service utilization for eating disorders across US ethnic groups: Implications for reducing ethnic disparities in health care access for eating disorders. Int J Eat Disord, 44, 412–420. doi: 10.1002/eat.20787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin JK, Pescosolido BA, & Tuch SA (2000). Of Fear and Loathing: The Role of ‘Disturbing Behavior,’ Labels, and Causal Attributions in Shaping Public Attitudes toward People with Mental Illness. J Health Soc Behav, 41, 208–223. doi: doi: 10.2307/2676306 [DOI] [Google Scholar]
- Masheb R, & White MA (2012). Bulimia nervosa in overweight and normal-weight women. Comprehensive Psychiatry, 53(2), 181–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mond JM, Hay PJ, Rodgers B, & Owen C (2007). Health service utilization for eating disorders: Findings from a community-based study. Int J Eat Disord, 40, 399–408. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence. (2017). Eating disorders: recognition and treatment. NICE Guideline (NG69). [PubMed] [Google Scholar]
- Ohan JL, Ellefson SE, & Corrigan PW (2015). Brief Report: The Impact of Changing from DSM-IV ‘Asperger’s’ to DSM-5 ‘Autistic Spectrum Disorder’ Diagnostic Labels on Stigma and Treatment Attitudes. Rev J Autism Dev Disord, 45(10), 3384–3389. doi: 10.1007/s10803-015-2485-7 [DOI] [PubMed] [Google Scholar]
- Pescosolido BA, Medina TR, Martin JK, & Long JS (2013). The “backbone” of stigma: identifying the global core of public prejudice associated with mental illness. Am J Public Health, 103, 853–860. doi: 10.2105/AJPH.2012.301147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pescosolido BA, Monahan J, Link BG, Stueve A, & Kikuzawa S (1999). The public’s view of the competence, dangerousness, and need for legal coercion of persons with mental health problems. Am J Public Health, 89(9), 1339–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan JC, Link BG, Stueve A, & Pescosolido BA (2000. ). Public conceptions of mental illness in 1950 and 1996: What is mental illness and is it to be feared? J Health Soc Behav, 188–207. [Google Scholar]
- Puhl RM, & Heuer CA (2010). Obesity stigma: important considerations for public health. Am J Public Health, 100, 1019–1028. doi: 10.2105/AJPH.2009.159491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhl RM, Peterson JL, & Luedicke J (2013). Motivating or stigmatizing? Public perceptions of weight-related language used by health providers. Int J Obes, 37, 612–619. doi: 10.1038/ijo.2012.110 [DOI] [PubMed] [Google Scholar]
- Puhl RM, & Suh Y (2015). Stigma and eating and weight disorders. Curr Psychiatry Rep, 17. doi: 10.1007/s11920-015-0552-6 [DOI] [PubMed] [Google Scholar]
- Rodgers RF, Paxton SJ, McLean SA, Massey R, Mond JM, Hay PJ, & Rodgers B (2015). Stigmatizing attitudes and beliefs toward bulimia nervosa: The importance of knowledge and eating disorder symptoms. J Nerv Ment Dis, 203, 259–263. doi: 10.1097/nmd.0000000000000275 [DOI] [PubMed] [Google Scholar]
- Seamark D, & Gabriel L (2018). Barriers to support: a qualitative exploration into the help-seeking and avoidance factors of young adults. Br J Guid Couns, 46, 120–131. doi: 10.1080/03069885.2016.1213372 [DOI] [Google Scholar]
- Sheehan DV, Harnett-Sheehan K, & Raj BA (1996). The measurement of disability. Int Clin Psychopharmacol, 11 Suppl 3, 89–95. [DOI] [PubMed] [Google Scholar]
- Star A, Hay P, Quirk F, & Mond J (2015). Perceived discrimination and favourable regard toward underweight, normal weight and obese eating disorder sufferers: implications for obesity and eating disorder population health campaigns. BMC Obes, 2, 4. doi: 10.1186/s40608-014-0032-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson-Brenner H, Satir DA, Franko DL, & Herzog DB (2012). Clinician reactions to patients with eating disorders: a review of the literature. Psychiatr Serv, 63(1), 73–78. doi: 10.1176/appi.ps.201100050 [DOI] [PubMed] [Google Scholar]
- Udo T, & Grilo CM (2018). Prevalence and correlates of DSM-5-defined eating disorders in a nationally representative sample of US adults. Biol Psychiatry, 84, 345–354. doi: 10.1016/j.biopsych.2018.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


