Abstract
Objectives.
We sought to better understand the tools used by public health officials in the control of tuberculosis (TB).
Methods.
We conducted a series of in-depth interviews with public health officials at the local, state, and federal levels to better understand how health departments around the country use isolation measures to control TB.
Results.
State and local public health officials’ use of social distancing tools in infection control varies widely, particularly in response to handling noncompliant patients. Judicial and community support, in addition to financial resources, impacted the incentives and enablers used to maintain isolation of infectious TB patients.
Conclusions.
Instituting social distancing requires authorities and resources and can be impacted by evidentiary standards, risk assessments, political will, and community support. Awareness of these factors, as well as knowledge of state and local uses of social distancing measures, is essential to understanding what actions are most likely to be instituted during a public health emergency and to target interventions to better prepare health departments to utilize the best available tools necessary to control the spread of disease.
Introduction
The 2014–2015 Ebola outbreak in West Africa and subsequent cases in the United States reinvigorated a national debate about the use of isolation and quarantine measures in the control of a communicable disease. Policy-makers, faced with a frightened public and limited options for pharmaceutical interventions to control Ebola, moved quickly to institute isolation and quarantine measures. Social distancing policies, however, varied greatly across the country.1
Whereas quarantine has been used only sparingly in the United States over the past 50 years2, public health officials utilize isolation and other social distancing measures regularly for the control of communicable diseases. We sought to better understand how local, state, and federal health officials around the nation use isolation and other social distancing measures by documenting how these measures are used for the control of tuberculosis (TB). Our intent was to learn from the existing processes in place to address TB in the United States and to then apply this understanding to inform policy recommendations to broader considerations around the use of quarantine and isolation. Instead of waiting for public health emergencies that may require quarantine, we hypothesized that there were lessons to be learned from the somewhat regular application of isolation to control TB that could inform social distancing policies.
The World Health Organization 2015 Tuberculosis Report identified TB as a leading cause of death worldwide. In 2014, TB killed 1.5 million people around the world, and approximately one-third of the global population is infected.3 In the United States, there were 9421 new cases of TB reported in 2014, a slight 1.5% decrease from 2013. The US incidence of TB, however, varies significantly between US-born (1.2 per 100,000) and foreign-born (15.4 per 100,000) individuals. In 2014, 66% of TB cases in the United States were in foreign-born individuals, and in 11 states – Colorado, Maine, Maryland, Massachusetts, Nebraska, New Jersey, New York, Utah, Virginia, Washington, and Wisconsin – at least 80% of cases occurred among foreign-born individuals. Approximately 1% of all new cases in the United States are multi-drug resistant.4
Per guidance from the Centers for Disease Control and Prevention (CDC), active TB disease is treated with a combination of antibiotics, most often with 4 drugs for 2 months, and a continuation of 2 of those drugs for 4 to 7 months.5 Patients with smear–positive active TB should be isolated for the first 2 to 4 weeks of therapy, until they have 3 negative sputum smears and show clinical improvement. All patients with active TB receiving treatment should undergo directly observed therapy to ensure that no antibiotic doses are missed.6,7 Ensuring patients are isolated for appropriate periods of time and taking medication as prescribed can create a burden on health care and public health infrastructures, particularly when patients are noncompliant.
This study aimed to better understand national variation in implementing isolation measures through an examination of how health departments isolated TB patients in a series of select cases. We expected the case studies to demonstrate how past experience, local (and sometimes ultra-local) politics, financial constraints, and the legal/regulatory environment impacted decision-making around isolation. We also expected that these findings could be extracted to the larger category of social distancing measures.
Methods
We compiled a list of 41 recent tuberculosis cases and outbreaks that occurred between 2004 and 2014 by using Morbidity and Mortality Weekly Report, Google News searches, and newsletters from Stop TB USA. From that list, we selected 16 to use as case studies, aiming to capture variety in geographic region, level of government (local, state, or federal), size of population served, and specific population or issue. For each case study, we identified primary and secondary contacts based on the health department officials identified in any media coverage or health department reports of the case or outbreak, and corresponded with the state tuberculosis control officer for additional contact information when needed. Of the 16 case studies identified, we were able to successfully complete interviews for 12 case studies. Four case studies were not successfully completed owing to difficulties identifying the correct contact and to not receiving a response from contacted health officials. Basic information about the 12 completed case studies is listed in Table 1.
Table 1:
Completed Case Studies on Tuberculosis (TB)a
| Government Level and Population Size | Geographic Region | Population Impacted and Topic | Year(s) of TB Cases/Outbreak | |
|---|---|---|---|---|
| 1 | State – medium | Southwest | Immigrants | 2006–2008 |
| 2 | Local – small metropolitan area | Midwest | Extensive outbreak | 2012–2014 |
| 3 | Local – large central metropolitan area | Northeast | Health care facility | 2013 |
| 4 | State – small | Northeast | College | 2014 |
| 5 | Local – Multi-county, serves micropolitan, small, and medium metropolitan areas | Southeast | Port | 2014 |
| 6 | Federal | Cross-border | 2010 | |
| 7 | State – medium | Southeast | Correctional facility | 2014 |
| 8 | Local – large fringe metropolitan area | Southeast | High school | 2012–2013 |
| 9 | Local – medium metropolitan area | West | Law enforcement involvement | 2014 |
| 10 | Local – small metropolitan area | Midwest | Extensive outbreak | 2013 |
| 11 | Local – large central metropolitan area | Midwest | Homeless | 2014 |
| 12 | Local – large central metropolitan area | West | Homeless | 2007–2013 |
Notes: State population sizes are categorized as follows: small, < 3 million; medium, between 3 and 10 million; large, > 10 million.
Local population size classifications follow the National Center for Health Statistics 2013 Urban-Rural Classification Scheme for Counties: 1, large central metro; 2, large fringe metro; 3, medium metro; 4, small metro; 5, micropolitan; 6, noncore.b Geographic regions are defined as follows: West is California, Colorado, Idaho, Montana, Nevada, Oregon, Utah, Washington, Wyoming; Southwest is Arizona, New Mexico, Oklahoma, Texas; Midwest is Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, Wisconsin; Southeast is Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, Mississippi, North Carolina, Tennessee, South Carolina, Virginia, West Virginia; and Northeast is Connecticut, Delaware, District of Columbia, Maine, Maryland, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, Vermont.
Source: Ingram DD, Franco SJ. 2013 NCHS Urban-Rural Classification Scheme for Counties. National Center for Health Statistics; 2014. https://www.cdc.gov/nchs/data/series/sr_02/sr02_166.pdf.
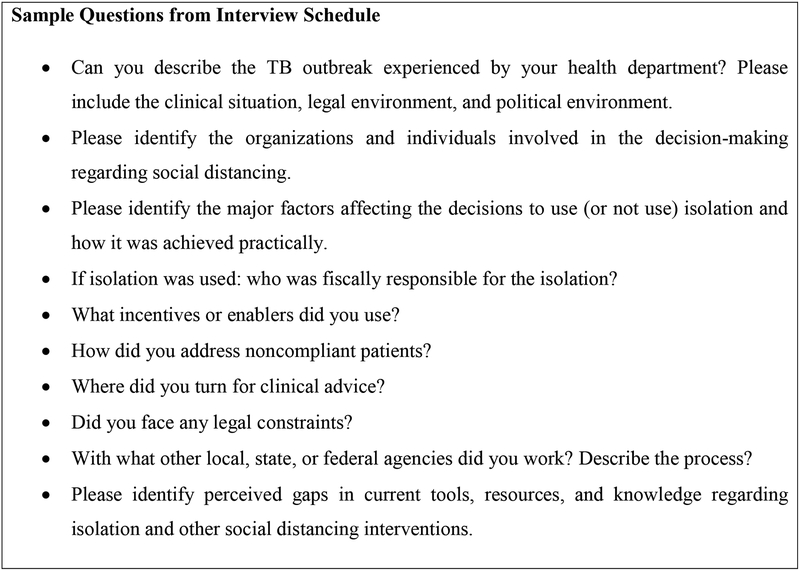
Between December 2014 and February 2015, we conducted 30- to 60-minute semi-structured interviews via telephone with public health officials who were involved in the response to the identified case or outbreak. The interviews were based on an interview schedule with open-ended questions about the specific case (See Figure 1), as well as the general protocols for isolation of infectious tuberculosis patients, noncompliance, legal issues, working with state and federal agencies, and working with foreign partners. Often the interviews ended up covering the selected case study as well as the public health official’s relevant experiences with TB in recent history. An interviewer and 2 note takers were present for each interview. Audio recording was not utilized. Interview notes were then coded for major categories and findings were reviewed by 2 researchers independently.
Figure 1:
Sample Questions from Interview Schedule.
The George Washington University Office of Human Research Institutional Review Board approved the study (IRB# 031401). All aspects of the study were approved by the Institutional Review Board, including communication to potential respondents.
Results
Although we found some consistencies in the way that public health officials from across the country respond to and mitigate outbreaks of TB, and the tools they have available to do so, the variation in methods used by public health officials due to varying resources was striking. Below, we describe our findings, categorized by housing, enablers and incentives, workforce, costs and responsibilities for payment, cross-border relationships, community awareness of TB, and the legal landscape around noncompliance.
Housing
We found that when possible, health departments isolated TB patients in their homes while they were infectious; however, homeless patients and noncompliant patients posed unique challenges. The interviewed public health officials in state and local health departments often struggled to find adequate housing situations for these patients and other patients who were unable to be isolated in their homes because of family situations.
In most of the studied jurisdictions, we found that homeless patients were isolated in a hospital until they were noninfectious. Then, they may have been transferred to a long-term care facility (which may have been in another part of the state or even in another state), motel, or apartment or house in the community, depending on the resources available. Some localities were more accustomed to dealing with this and already had facilities identified and relationships with staff to facilitate the process; others struggled to find appropriate facilities in the community. Some localities didn’t have the resources to provide housing for homeless patients, which meant that if the patients truly had nowhere else to go, they would stay in the hospital for the duration of their treatment to ensure that treatment was fully completed – a costly solution that was seldom satisfactory to any of the involved parties. Other localities had no choice but to send homeless patients back into the shelters with guidance to stay close to windows and as far away from other residents as possible.
The states and localities studied varied in their resources, options, and attitudes regarding housing noncompliant patients. In some localities, jail was the only option with negative pressure isolation and appropriate security for noncompliant patients; however, several public health officials expressed that jail was not appropriate for building a relationship with the patient and “taking a patient-centered approach to care.” Two of the large central metropolitan areas included in our study were the only jurisdictions with consistent access to secure hospital wards in which they could isolate noncompliant patients. Where jail was not a legal option and there was no designated hospital with lockdown capabilities, officials were left with few options for removing noncompliant patients from the community.
Enablers and Incentives
The term enablers refers to the services and items that “make it possible for the patients to receive treatment by overcoming barriers,” whereas incentives are “small rewards given to patients to encourage them to either take their own medicines or keep their clinic or field directly observed therapy appointments.”8 We found that health departments provided a varying range of services to enable or incentivize compliance with isolation measures, including providing housing, paying patients’ rent, providing groceries or grocery gift cards, paying for utilities, and providing cell phones. Some of the health departments that we studied were unable to provide any enablers due to funding constraints, yet many pointed to the importance of using enablers to facilitate completion of treatment and the need to be flexible and accommodating in meeting patients’ needs in order to ensure compliance with what can be a long and difficult treatment. As one public health official pointed out, “…the hardest part is that TB doesn’t happen regularly with people that have the funds to support themselves.” Enablers were meant to ease the burden and therefore enable patients to successfully complete treatment.
In some of the states and localities studied, health departments only provided enabling services while patients were infectious and isolated and therefore unable to work. In other jurisdictions, the health department continued to provide enablers even after the patient was no longer isolated, particularly for homeless patients, in order to facilitate compliance with treatment. Other health departments expected patients to rely on their social networks and families, or the public health officials connected the patients to community resources including food pantries.
The health departments studied also provided incentives to patients to encourage patients to comply with their treatment regimen. Again, the health departments were limited by the funding available and the sources of that funding. The incentives included gift cards for common items like fast food and bus tickets. In some cases, the line between incentives and enablers was blurred, due to patients’ needs and the public health officials’ perceptions of what it would take to successfully get the patient to complete treatment and allow the health department to continue monitoring the patient.
Workforce Cooperation and Challenges
In most places that we studied, with the exception of the large central and fringe metropolitan areas, the state and local health departments worked closely together on TB control. Those localities that were not accustomed to seeing many TB cases relied on the assistance of their state partners and local health care organizations to help them perform contact tracing and test large numbers of individuals. The larger local health departments experienced TB cases with more regularity, and even when they struggled with resources they seldom relied upon assistance from the state.
Almost all of the TB control programs at the state and local level that we studied were understaffed. TB control officers often performed multiple roles, and in many cases they pulled in staff from other health department programs and relied on assistance from the CDC in the event of an outbreak. Public health officials also reported needing a vast range of skills to (1) track down infectious individuals who didn’t want to be found, (2) understand social and cultural factors to enable treatment compliance, and (3) negotiate with local businesses and school boards. One official remarked, “I should have a private detective license.” Many also pointed to the importance of building rapport with local communities, which is essential for working with populations that may not trust the government or authorities, including immigrant communities and Native Americans.
Costs and Responsibilities for Payment
Across the country, we found that public health officials were faced with the challenge of budgeting for the unknown. This was particularly true when they were trying to respond to and mitigate TB outbreaks; localities with very low annual case rates suddenly found themselves facing extensive outbreaks requiring massive resources.
Several public health officials stated that one of the challenges they faced was inflexible funding mechanisms that made it difficult for them to provide housing and other enablers they felt were necessary for ensuring a patient stays in isolation to complete treatment. Funding was based on predictions for the year ahead, but the number of cases, particularly the number requiring costly isolation (voluntary or involuntary), was unpredictable. One official from a medium-sized state also spoke of the need for more flexibility in carrying over federal funds from previous years or sharing funds between states.
Cases requiring court-ordered isolation were identified as an additional cost seldom included in annual budgets. One local health department official stated that low funding made it difficult for her health department to comply with a changing legal atmosphere that emphasized civil liberties and more rigorous legal guidance for addressing noncompliance.
Cross-Border Relationships
We found that states often worked together when patients or outbreaks crossed political jurisdiction lines, when cases occurred close to state borders, or when patients identified contacts in bordering states. States that bordered either Canada or Mexico also coordinated with their neighboring cross-border jurisdiction if they were concerned that an outbreak would cross the international border. States also worked with US Customs and Border Patrol, US Immigration and Customs Enforcement, and the US Coast Guard as necessary.
We found, though, that local health departments along the Mexico border seldom coordinated directly with local health departments across the border, relying instead on state health departments that typically worked directly with cross-border states and through the CDC Division of Global Migration and Quarantine. While formal processes for sharing disease information across the border with Mexico seemed well ingrained, the process seemed more informal for localities along the Canadian border; respondents described direct communication between local health officials across the border with limited involvement of state or federal officials.
Legal System and Non-compliance
In our interviews, we confirmed that TB control regulations, which dictate the legal means for handling noncompliant cases, were generally codified in state statute. The regulations range from non-legally-binding home isolation agreements to written orders to cooperate with treatment protocols, and they tend to culminate in court-ordered isolation away from the community for noncompliant patients. Public health officials in all states and localities emphasized that noncompliant patients were very rare, but all health officials we spoke with were aware of the processes available to them in the case of a noncompliant patient.
Judges’ awareness of noncompliance and health orders, however, varied by jurisdiction, largely related to the caseload in the region. Jurisdictions with regular cases often had a set procedure, and health officials worked with the same judge or judges who were familiar with TB compliance concerns and other public health issues. In one extensive outbreak, public health officials stated that the judges were “quite befuddled” when faced with noncompliant patients. In contrast, a public health official in a large central metropolitan area stated that the judges understood the public health concerns, and that the jurisdiction was almost always successful in getting court-ordered isolation. In other jurisdictions, public health officials indicated that the judges were sympathetic to public health officials owing to their fear of TB.
In some states, judges were very willing to send patients to jail for noncompliance, while in others they were much more hesitant. We found that handling noncompliance was a simpler process for jurisdictions with the appropriate facilities for court-ordered isolation in a local hospital, when compared with the process for jurisdictions in which the only option for isolation was a correctional facility.
In some states there was very little health officials could do, legally, to remove noncompliant patients from the community. Many of the public health officials we interviewed spoke to the need for flexibility in handling noncompliant cases, remarking that there may be incentives or enablers that make a certain patient more likely to comply, or ways of enforcing isolation without resorting to jail (i.e., video monitoring, security guard, or electronic anklet monitoring).
Community Awareness of Tuberculosis
Almost all of the public health officials that we interviewed mentioned a general lack of awareness among the public, policy-makers, and some health care workers that TB is still a public health concern in the United States. In jurisdictions with low TB incidence rates, the officials stated that individuals can go undiagnosed for months, during which time they may transmit TB into the community and to health care workers. In one extensive outbreak, the index case had remained undiagnosed even though the patient had seen multiple providers over a 9-month period while experiencing TB symptoms.
Several public health officials spoke of the importance of policy-makers understanding the burden of TB in the country and in their communities. While policymakers may simply see case counts falling, the public health officials we interviewed argued that those decreases will not be sustained if funding also falls.
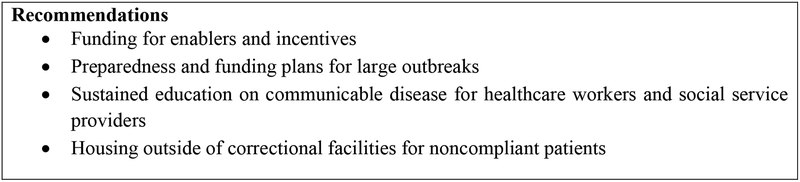
Discussion
We found great variation in how health departments around the country operationalize response to TB outbreaks, but we were also able to collect and assess a series of best practices. We have compiled a series of policy recommendations that would enable public health professionals to have the necessary resources and flexibility to adequately respond to and mitigate the consequences of a TB outbreak (Figure 2). Although these best practices are specific to TB, we believe they are also applicable to improving the planning for and implementation of all social distancing measures that may be necessary to mitigate any communicable disease.
Figure 2:
Policy Recommendations for State and Local Health Departments for Social Distancing Preparedness.
We also found variation in the cultural atmosphere around what health departments are willing to provide to patients. In some states and localities, the health department was very willing to provide enablers and incentives, whereas in others the health department was hesitant to provide such resources for fear of being seen as giving handouts.
Policy Recommendations
This study suggests that enablers and incentives are vital for patients to comply with isolation and treatment measures. Therefore, funding for these programs should not be considered optional and should be integrated into annual budgeting. Health departments need procedures and policies to ensure that funds will be available during large outbreaks. Education for health care workers and social service providers must be maintained, because identifying cases of TB (or other diseases) early diminishes transmission rates. Health care workers and social service providers need to know what to look for and always consider TB as a possibility. Finally, health departments need access to facilities other than jails in which to place noncompliant patients, so they can work with individuals to contain disease in a constructive manner.
Most importantly, it appears that access to resources, careful planning, engagement with the community as partners, and doing everything possible to reduce the feeling of punishment associated with isolation have enabled health departments to successfully contain outbreaks of TB. These are lessons that can and should be applied to preparedness planning for quarantine and other social distancing measures.
Limitations
This study was limited by the number of jurisdictions represented (n = 12); this is not representative of all health departments in the United States, and the number of TB cases represented by the case studies amounts to a little over 1.5% of all individual cases of TB in the United States in 2014. The findings may also be limited by recall bias, because public health officials were asked about cases and outbreaks that may have occurred several years prior to the interview. We believe, however, that the findings are useful in providing greater understanding of how public health officials work to control TB in the United States and the challenges they face and could be used as a basis for further study.
Conclusions
Effective implementation of isolation and quarantine is an essential core capacity for health departments faced with an emerging or unknown infectious disease threat. The lessons we learn from effectively controlling TB in the context of varying state laws and policies, resources, and social/political environments are lessons we must capture to better understand the state of preparedness in the country. There is much we can learn from the community of public health professionals around the country working diligently to control the spread of TB.
We must also not forget about the burden of TB in the United States. Even though the case count and case rate for TB continue to decline each year, continued investment, both financial and staffing, is necessary to reach the goal of TB elimination.
Acknowledgments
The project described was supported by Grant Number 105738 from NIAID. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIAID.
Contributor Information
Rebecca Katz, International Health, Center for Global Health Science and Security, Georgetown University,Georgetown University Medical Center, Washington, DC 20037.
Andrea Vaught, Center for Global Health Science and Security, Georgetown University, Georgetown University Medical Center, Washington, DC 20037.
References
- 1.Kraemer JD, Siedner MJ, Stoto MA. Analyzing Variability in Ebola-Related Controls Applied to Returned Travelers in the United States. Health Secur. 2015;13(5):295–306. 10.1089/hs.2015.0016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cetron M, Landwirth J. Public health and ethical considerations in planning for quarantine. Yale J Biol Med. 2005;78(5):329–334. [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Global Tuberculosis Report 2015. World Health Organization; 2015. [Google Scholar]
- 4.Centers for Disease Control and Prevention. Reported Tuberculosis in the United States, 2014. Atlanta, GA: U.S. Department of Health and Human Services, CDC; 2015. [Google Scholar]
- 5.Centers for Disease Control and Prevention. Treatment of tuberculosis, American Thoracic Society, CDC, and Infectious Diseases Society of America. MMWR Recomm Rep. 2003;52(RR-11):1–77. [PubMed] [Google Scholar]
- 6.Herchline TE. Tuberculosis treatment and management. Medscape website. http://emedicine.medscape.com/article/230802-treatment. Updated October 22, 2015. Accessed January 19, 2016. [Google Scholar]
- 7.Centers for Disease Control and Prevention. Tuberculosis (TB) fact sheet: infection control in health-care settings. CDC website. http://www.cdc.gov/tb/publications/factsheets/prevention/ichcs.htm. Accessed January 17, 2016.
- 8.Centers for Disease Control and Prevention. Self-Study Modules on Tuberculosis: Module 9: Patient Adherence to Tuberculosis Treatment Reading Material. 2012; http://www.cdc.gov/tb/education/ssmodules/module9/ss9reading3.htm. Accessed 12 May, 2016.