Abstract
Pain is prevalent among individuals with overweight or obesity but few studies have examined the mechanism linking pain with excess body weight. Because there is evidence that social and physical pain may be processed through similar physiological mechanisms, weight-stigma may potentiate the experience of physical pain through shared neuroanatomical pathways. This study evaluated the relationship between perceived weight stigma and self-reported bodily pain in a sample of overweight and obese adult women. Sixty-one women with a body mass index (BMI) between 25–35 completed self-report questionnaires assessing perceived stigma, internalized weight stigma, and self-reported pain. Height and weight were measured and participants completed a demographic and health history questionnaire. Hierarchical regression analyses were utilized to predict self-reported pain from perceived stigma, adjusting for demographic variables associated with self-reported pain as well as pain-related conditions. Perceived stigma was associated with pain F(6, 54)=6.10, p<.001) as was internalized stigma. Perceived stigma mediated the relationship between BMI and bodily pain among individuals with a BMI in the overweight range but not among individuals with a BMI in the obese range. Weight-related stigma among women with overweight or obesity appears to be associated with greater experience of physical pain. These results underscore the need to evaluate multiple mechanisms that might explain the relationship between bodily pain and body weight and to determine how the relationship may vary across different subgroups of individuals.
Keywords: Obesity, pain, bodily pain, obesity stigma, internalized weight bias
Introduction
Obesity continues to be a preeminent threat to public health (Ogden, Carroll, Kit, & Flegal, 2014). One in three adults in the United States have a body mass index (BMI) in the obese range, significantly increasing the risk for medical and psychiatric morbidity among those individuals. Increasingly, obesity is linked with bodily pain and chronic pain. Although estimates of pain in the general population vary widely due to differing foci and measurement of pain (Kennedy, Roll, Schraudner, Murphy, & McPherson, 2014), individuals with overweight or obesity are disproportionately affected by pain, with rates of chronic pain increasing across BMI categories (Okifuji & Hare, 2015). The comorbidity of pain and obesity may exacerbate the negative consequences of both conditions, contributing to further reduction in quality of life and increased medical costs.
Accumulating evidence suggests that obesity is prospectively associated with increased risk of pain later in life (Hitt, McMillen, Thornton-Neaves, Koch, & Cosby, 2007), and weight loss has been shown to attenuate reported pain. However, pain also has been linked to poor weight management outcomes (Masheb et al., 2015). Therefore, bodily pain is a costly comorbidity (Gaskin & Richard, 2012) that may also be a barrier to successful weight loss, thereby perpetuating both conditions. It is currently accepted that multiple factors and pathways likely contribute to the relationship between pain and obesity. Recent data suggest that dietary factors linked to inflammation may be one mechanism (Emery, Olson, Bodine, Lee, & Habash, 2017). Historically, physical/mechanical factors (e.g., biomechanical loading on joints) have been studied in the relationship of pain and obesity while psychosocial factors have been studied to a lesser degree (Janke, Collins, & Kozak, 2007).
Emerging research suggests that emotional pain may be processed through the same neuroanatomical and physiological mechanisms as physical pain (Eisenberger & Lieberman, 2004), indicating that the biological ‘foot print’ of physical pain and psychological pain may overlap. Perhaps the strongest evidence comes from research evaluating social rejection, a specific type of psychological pain, which has been consistently associated with increased physical pain (Eisenberger, Lieberman, & Williams, 2003). Weight-related stigma, a form of social rejection experienced by individuals with overweight or obesity, is highly prevalent and may contribute to the relationship between obesity and pain through shared physiological mechanisms. Pearl and colleagues (2014) found that internalized weight bias was associated with bodily pain among a sample of individuals diagnosed with and seeking treatment for binge eating disorder. However, the relationship between perceived stigma and bodily pain remains unexplored. Also, it is not clear that internalized weight bias is associated with bodily pain among individuals without binge eating disorder. The current study was designed to evaluate the hypotheses that (1) greater experience of stigma would be associated with higher levels of self-reported pain among women with overweight or obesity who were entering a weight management study; and (2) that stigma would mediate the relationship between BMI and pain.
Methods
Women interested in weight loss were recruited from a large Midwestern metropolitan area to participate in the Logging Exercise And Nutrition (LEAN) into Health Study, an 8-week randomized, controlled weight loss pilot intervention. Eligible women were identified as over the age of 25 with BMI ≥25 and <35 (although a few participants were enrolled with a BMI>35 due to under-reporting during screening). All eligible participants completed an individual baseline assessment including both objective and self-report measurements. Height and weight were measured by study staff. Participants were given a paper packet of psychosocial questionnaires to complete after all physical measurements were recorded. This study was approved by The Ohio State University Institutional Review Board (Protocol Number: 2015B0077) and all participants provided written consent to all study procedures prior to enrollment in the study.
Measures
Self-report of demographic and medical history information included age, race, level of education and employment, and health history. As part of the medical history questionnaire, participants were given a list of medical conditions and directed to indicate presence or absence of the condition (including a history of the condition). The pain-related conditions (arthritis, joint pain, or headache) were included in analyses as covariates.
Body Mass Index Height (meters) and weight (kilograms) were measured and used to calculate each participant’s BMI (kg/m2).
Bodily Pain Subscale (BP, Ware & Sherbourne, 1992) is a two-item subscale of the Medical Outcomes Study-Short Form-36 (SF-36). The BP subscale assesses pain presence (‘how much bodily pain have you had’) and interference (‘how much did pain interfere with normal work’) during the previous 4 weeks. Inter-correlation of the two-item subscale in this sample was r=0.88. Higher scores reflect lower levels of pain. This subscale is widely used to assess self-reported pain across diverse samples and in the context of overall health (Hawker, Mian, Kendzerska, & French, 2011).
Stigma Impact Scale (SIS; Fife & Wright, 2000) The SIS is a 24-item questionnaire developed to examine facets of stigma and assess the impact of perceived stigma among individuals with chronic illnesses. This measure was modified to prompt participants to consider each of the 24 experiences “that people who are overweight or obese may have from time to time,” and rate them on a 5-point likert scale. The questionnaire includes four subscales representing social rejection, financial insecurity, internalized shame, and social isolation. The term ‘illness’ was changed to ‘condition’ throughout the scale to increase applicability of item content for the current sample, and internal reliability was excellent (Cronbach’s alpha=0.94).
Weight Bias Internalization Scale (WBIS; Durso & Latner, 2008) is an 11-item questionnaire designed to assess the degree to which an individual believes negative weight-related attributes are accurate and applicable to him/herself, thereby providing a measure of internalized stigma. Items are scored on a 7-point likert scale with higher scores indicating greater internalized weight bias. The first item of the WBIS (“As an overweight person, I feel that I am just as competent as anyone”) was removed due to low inter-correlation with other items which is consistent with common use of the measure (Hilbert, et al. 2014). Cronbach’s alpha for the remaining ten items was 0.89.
Data Analysis
All participants were included in analyses, regardless of level of self-reported pain. Correlational and linear regression analyses were conducted to evaluate the relationship between stigma and bodily pain utilizing Statistical Analysis Software (SAS 9.2). The PROCESS (Hayes, 2013) macro in SAS 9.2 was then used to evaluate the hypothesis that stigma and internalized weight bias mediate the relationship between BMI and self-reported bodily pain. Stigma variables associated with bodily pain in regression analyses were tested as mediators, with BMI as a predictor of self-reported bodily pain. Covariates were included in the models using 10,000 bootstrap samples with 95% bias-corrected confidence intervals to test direct and indirect effects among the predictor, BMI, and the bodily pain outcome variable.
Results
Sixty-one women completed the baseline study assessment (see Table 1 for sample demographics). As shown in Table 1, the mean bodily pain score for the total sample (as well as within each BMI class) was in the mid-60s, reflecting less bodily pain than the general population. However, only seven individuals (out of 61) reported no bodily pain in the past four weeks. Perceived stigma was associated with greater bodily pain (r=−.29, p=0.02), and the relationship remained significant when controlling for potential demographic/health correlates of pain (age, race, BMI) as well as pain-related conditions (arthritis, joint pain, and headaches; F(6, 54)=6.10, p<.001; β:−0.43, p=0.04). Analyses of the four SIS subscales were conducted to identify facets of perceived stigma associated with pain. Internalized shame emerged as the only significant correlate (β: −1.46, p=0.04). Controlling for the demographic and pain condition covariates in the SIS analyses, WBIS also was associated with self-reported pain (β: −4.19, t=−2.06, p=0.05).
Table 1.
Demographic characteristics of study sample and key study constructs
| Total Sample (n=61) | Overweight (n=26) (BMI range=25–29.9) | Obese (n=35) (BMI range=30–36.8) | |
|---|---|---|---|
| Age (mean, SD) | 41.76 (10.7) | ||
| BMI (mean, SD) | 30.67 (3.0) | ||
| Race | 77% white | ||
| Education | 70% Bachelor’s degree or higher | ||
| Bodily Pain (mean, SD) | 66.56 (23.8) | 66.42 (22.7) | 66.66 (24.9) |
| Perceived Stigma (mean, SD) | 38.58 (12.5) | 38.5 (12.3) | 38.63 (12.8) |
| Internalized Weight Stigma (mean, SD) | 4.22 (1.22) | 4.30 (1.1) | 4.16 (1.3) |
Note. BMI=Body Mass Index; Bodily pain evaluated with the SF-36 Bodily Pain Subscale (BP); Perceived Stigma evaluated with the Stigma Impact Scale (SIS); Internalized Weight Stigma evaluated with the Weight Bias Internalization Scale (WBIS).
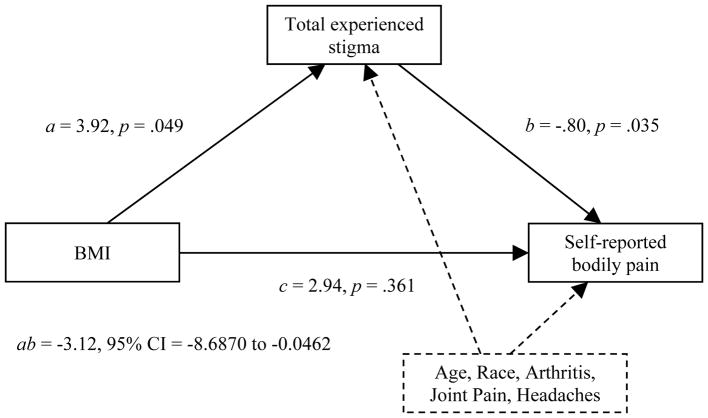
Results of the mediation analyses indicated no mediation effect for total experienced stigma, the internalized shame subscale (SIS), or internalized weight bias. Epidemiological studies consistently demonstrate a relationship between BMI category and differential risk for disease (Eggers et al., 2016). This is especially the case for pain symptoms, diagnoses, and severity (Janke, Collins, & Kozak, 2007). Therefore a post hoc exploratory subgroup analysis was conducted to evaluate the mediation models within each BMI group. Accordingly, the perceived and internalized stigma mediation models were conducted among overweight (n=26) and obese (n=35) participants. Perceived stigma mediated the relationship between BMI and bodily pain among overweight (25 < BMI < 30; ab = −3.12; 95% CI = −8.6870 to −0.0462: see Figure 1) but not obese (BMI > 30) participants. Neither of the internalized stigma variables were mediators.
Figure 1.
Mediation model: Among non-obese participants, total stigma mediates the relationship between BMI and self-reported bodily pain when controlling for potential demographic and pain-related confounds.
Discussion
Weight-related stigma was associated with self-reported bodily pain. As pain is a burdensome comorbidity of excess body weight that may interfere with weight management treatment, understanding the elevated prevalence of pain in this population is essential. The association of stigma with pain is especially concerning as stigma occurs in a variety of overt and covert ways, increasing the potential impact of stigma among individuals with overweight or obesity. Internalized weight bias (as measured by the WBIS and in the subscale analyses) appears to be particularly relevant in the relationship between stigma and bodily pain. These findings extend previous work documenting a relationship between internalized weight stigma and bodily pain among individuals with binge eating disorder (Pearl et al 2014). However, internalized stigma accounted for a small amount of variability in bodily pain in their sample while, in this study, bodily pain was more strongly associated with internalized weight stigma than with perceived stigma. This may reflect, in part, differences in the study samples, as Pearl et al. included men and women with Binge Eating Disorder, and average BMI (39kg/m2) was much higher. Nevertheless, obesity stigma emerges across disparate groups as a correlate of bodily pain, requiring further consideration in both research and clinical settings.
Perceived stigma mediated the relationship between BMI and bodily pain among individuals with a BMI in the overweight range but not among individuals in the obese range. Post hoc comparison of individuals with overweight versus obesity revealed no differences in stigma (perceived or internalized) or in bodily pain. This suggests that the results are not confounded by group differences in symptom severity or distribution. Pain experience among overweight women may be linked to social factors such as stigma, whereas pain among obese women may be better explained by biological or biomechanical factors, or perhaps social factors other than stigma.
Previous research has identified gender-related differences in the correlates of pain among individuals with a BMI greater than or equal to 25 (Masheb, White, & Grilo, 2016). Among individuals with binge eating disorder, Masheb and colleagues found that women reported greater pain and more pain-related interference compared to men, but pain was associated with metabolic and behavioral risk factors only among men. It is important to explore the relationship of stigma and pain in larger, more diverse samples.
These data are cross-sectional in nature, thus the direction of the relationship between stigma and pain is unknown. Activation of pain processing pathways due to physical pain may sensitize individuals to emotional pain, and vice versa. Alternatively, common psychological factors known to influence pain (i.e., catastrophizing) also may increase the likelihood of perceiving and internalizing stigmatizing encounters or negative societal messages about body weight. Given the biopsychosocial nature of pain, weight stigma and bodily pain may be related through an interaction of factors. However, weight-related stigma appears to be a relevant contributor. Because perceptions of stigma may be modifiable (e.g., internalized weight bias reduced following both cognitive behavioral and acceptance-based interventions (Levin, Potts, Haeger, & Lillis, 2017; Pearl, Hopkins, Berkowitz, & Wadden, 2016)), these data underscore the growing demand for interventions that better address psychosocial aspects of obesity.
In advancing this area of research, it will be important to replicate these effects in a larger, more diverse sample including both men and women. Further, the current findings suggest that the social stress of stigma may influence pain among overweight individuals, but other factors may become important for pain among obese individuals. It will be important to consider additional explanatory factors (e.g., inflammatory factors) within larger and more diverse samples to explore further the relationship of body fat to pain. As the hypotheses of this study were based on findings from social neuropsychology, expanding the methodology from self-report assessment to integrate biological and neuroanatomical assessment will enhance our ability to clarify these relationships. As this area advances, collaboration between pain researchers and obesity researchers will be essential for facilitating methodologically rigorous research.
Acknowledgments
This research was supported in part by grants from the Society for Health Psychology Graduate Student Research Award; American Psychological Association Graduate Dissertation Award; The Ohio State University (OSU) Alumni Grant for Graduate Research and Scholarship; OSU Presidential Fellowship; OSU Arts and Sciences Undergraduate Research Scholarship; and Award Number Grant UL1TR001070 from the National Center for Advancing Translational Sciences, NIH.
References
- Durso LE, Latner JD. Understanding self-directed stigma: development of the weight bias internalization scale. Obesity. 2008;16(S2) doi: 10.1038/oby.2008.448. [DOI] [PubMed] [Google Scholar]
- Eggers S, Remington PL, Ryan K, Nieto FJ, Peppard P, Malecki K. Obesity Prevalence and Health Consequences: Findings From the Survey of the Health of Wisconsin. WMJ. 2016;115:238–243. [PMC free article] [PubMed] [Google Scholar]
- Eisenberger NI, Lieberman MD. Why rejection hurts: a common neural alarm system for physical and social pain. Trends in cognitive sciences. 2004;8(7):294–300. doi: 10.1016/j.tics.2004.05.010. [DOI] [PubMed] [Google Scholar]
- Eisenberger NI, Lieberman MD, Williams KD. Does rejection hurt? An fMRI study of social exclusion. Science. 2003;302(5643):290–292. doi: 10.1126/science.1089134. [DOI] [PubMed] [Google Scholar]
- Emery CF, Olson KL, Bodine A, Lee V, Habash DL. Dietary intake mediates the relationship of body fat to pain. Pain. 2017;158(2):273–277. doi: 10.1097/j.pain.0000000000000754. [DOI] [PubMed] [Google Scholar]
- Fife BL, Wright ER. The dimensionality of stigma: A comparison of its impact on the self of persons with HIV/AIDS and cancer. Journal of health and social behavior. 2000:50–67. [PubMed] [Google Scholar]
- Gaskin DJ, Richard P. The economic costs of pain in the United States. The Journal of Pain. 2012;13(8):715–724. doi: 10.1016/j.jpain.2012.03.009. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: The Guilford Press; 2013. [Google Scholar]
- Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual analog scale for pain (vas pain), numeric rating scale for pain (nrs pain), mcgill pain questionnaire (mpq), short-form mcgill pain questionnaire (sf-mpq), chronic pain grade scale (cpgs), short form-36 bodily pain scale (sf-36 bps), and measure of intermittent and constant osteoarthritis pain (icoap) Arthritis care & research. 2011;63(S11) doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- Hilbert A, Baldofski S, Zenger M, Löwe B, Kersting A, Braehler E. Weight Bias Internalization Scale: psychometric properties and population norms. PLoS One. 2014;9(1):e86303. doi: 10.1371/journal.pone.0086303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hitt HC, McMillen RC, Thornton-Neaves T, Koch K, Cosby AG. Comorbidity of obesity and pain in a general population: results from the Southern Pain Prevalence Study. The Journal of Pain. 2007;8(5):430–436. doi: 10.1016/j.jpain.2006.12.003. [DOI] [PubMed] [Google Scholar]
- Janke EA, Collins A, Kozak AT. Overview of the relationship between pain and obesity: What do we know? Where do we go next? J Rehabil Res Dev. 2007;44:245–262. doi: 10.1682/jrrd.2006.06.0060. [DOI] [PubMed] [Google Scholar]
- Kennedy J, Roll JM, Schraudner T, Murphy S, McPherson S. Prevalence of persistent pain in the US adult population: new data from the 2010 national health interview survey. The Journal of Pain. 2014;15(10):979–984. doi: 10.1016/j.jpain.2014.05.009. [DOI] [PubMed] [Google Scholar]
- Levin ME, Potts S, Haeger J, Lillis J. Delivering acceptance and commitment therapy for weight self-stigma through guided self-help: Results from an open pilot trial. Cognitive and Behavioral Practice 2017 [Google Scholar]
- Masheb RM, Lutes LD, Kim HM, Holleman RG, Goodrich DE, Janney CA, … Damschroder LJ. Weight loss outcomes in patients with pain. Obesity. 2015;23(9):1778–1784. doi: 10.1002/oby.21160. [DOI] [PubMed] [Google Scholar]
- Masheb RM, White MA, Grilo CM. Sex differences and correlates of pain in patients with comorbid obesity and binge eating disorder. European Eating Disorders Review. 2016;24(3):247–250. doi: 10.1002/erv.2432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. Jama. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okifuji A, Hare BD. The association between chronic pain and obesity. Journal of pain research. 2015;8:399. doi: 10.2147/JPR.S55598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearl RL, Hopkins CH, Berkowitz RI, Wadden TA. Group cognitive behavioral treatment for internalized weight stigma: a pilot study. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity. 2016:1–6. doi: 10.1007/s40519-016-0336-y. [DOI] [PubMed] [Google Scholar]
- Pearl RL, White MA, Grilo CM. Weight bias internalization, depression, and self-reported health among overweight binge eating disorder patients. Obesity. 2014;22(5) doi: 10.1002/oby.20617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF 36):I. Conceptual framework and item selection. Medical care. 1992:473–483. [PubMed] [Google Scholar]