Abstract
Leptospirosis is a widespread worldwide zoonosis. Human leptospirosis was first identified in the Korea in 1984 as the cause of “epidemic pulmonary hemorrhagic fever of unknown etiology” that occurred sporadically or in outbreaks. The major outbreaks, leading to some deaths, mainly involved rice field farmers who worked in wet and muddy rice paddies following floods or heavy rainfalls. Leptospirosis was designated a nationally notifiable disease in 1987. The Korean government introduced a supplementary immunization program to control the disease from 1988 to 1997, which provided people at risk in endemic areas with the inactivated vaccine prepared from a local strain Leptospira interrogans serovar Lai. In addition, the continuous promotion of education and awareness in the media played a role in improving personal hygiene management. Since then, the reported incidence of leptospirosis has been low. Leptospirosis is currently considered in the differential diagnosis of acute febrile illnesses occurring in fall. This study historically reviews clinical and epidemiological publications, scientific reports, and public health policies for recognition, identification, and infection control of human leptospirosis in the Korea.
Keywords: Leptospira, Leptospirosis, Korea, Communicable diseases, History
Introduction
Leptospirosis is a re-emerging zoonosis worldwide. The incidence of human leptospirosis, as a nationally notifiable disease, has decreased in recent years in the Korea, although the outbreaks of the disease were a serious public health challenge in the 1980s. While sporadic leptospirosis cases have occurred annually in endemic areas, concern about potential epidemics remains because of the persistence of animal leptospiral carriers as natural reservoirs, people at risk, and favorable environmental and climate conditions. Therefore, a comprehensive review of the literature on our existing knowledge and experience for recognition, identification, and infection control of human leptospirosis in the Korea would be able to take advantages for the future challenges.
Herein, the author provides the historical review of human leptospirosis in the Korea between 1945 and 2015, with a reference source of information for those interested in Leptospira and leptospirosis. There were many more articles on leptospirosis than those cited in this review. Some of them were not included due to overlapping findings or unavailability. The author apologizes to those whose works might be inadequately recognized in this review.
1. Occurrence and epidemics
1) Early history of discovery of leptospirosis in other countries
In beginning the historical review of leptospirosis in the Korea, it is necessary to look back briefly on the early history of the disease in other countries. Since leptospirosis was first described as Weil's disease, by physician Adolf Weil in 1886 in Germany, a characteristic infectious disease accompanied by splenomegaly, jaundice, and nephritis [1], leptospirosis was recognized as a new disease differentiated from other diseases with similar symptoms. After that, many cases and epidemics were reported in the army and other general populations in Western Europe. When Weil's disease spread among coal miners in Japan in 1914 – 1915, Inada et al. at Kyushu University successfully isolated the bacteria from blood of guinea pigs that were transmitted the infection [2]. The disease was recognized as an entity in ancient times as well, and was referred to as “rice-harvest jaundice” in ancient Chinese language and as “7-day fever” or “autumn fever” in Japanese language, with names associated with the season, occupation, and duration of symptoms. Since the causative bacteria, animal reservoirs, and the importance of environmental conditions were identified between 1920 and 1960, it became known that the disease transmission by working in dangerous environmental conditions rather than occupational exposure. Japanese researchers also described that rats served as carriers, opening the important way for understanding the epidemiological principles transmitted by carrier animals, and their management. Several years later, wide-ranging zoonotic characteristics involving wild and domestic animals were determined. The important basic knowledge of leptospirosis and Leptospira species was largely described in the early 1920s. Many Leptospira species were isolated from host animals worldwide, and more than 180 serovars were identified with description of the associated clinical aspects and geographical distribution until the early 1950s [3].
2) Lack of evidence for human leptospirosis (1945 – 1969)
Historically, the presence of leptospirosis in Korea had long been a subject of debate before the liberation of Korea from Japanese occupation in 1945. Although a case with Leptospira isolation from blood was reported in Japanese literature, which was not accepted by the medical society at that time, due to lack of serological test and animal experiment. In the period of Korean War (1951 – 1952), there were the number of cases of Korean hemorrhagic fever and infectious hepatitis occurred. Korean and American medical scientists studied extensively on leptospirosis for those with fever, jaundice, and hemorrhagic manifestation, but failed to prove the presence of the disease. Several Leptospira strains were isolated from house rats in Busan (a temporary capital city during the Korean War) and wild rats (Apodemus agrarius) in the Demilitarized Zone. Two leptospiral isolates were serologically very close to L. icterohaemorrhagica [4]. Therefore, leptospirosis was recognized their existence among animals, but human cases had not been confirmed [5].
3) First epidemic described as “hemorrhagic pneumonitis-like disease of unknown etiology” (1970 – 1980)
Twenty-five years after the Korean War, in October 1975, there was an epidemic of “hemorrhagic pneumonitis-like disease” or “epidemic pulmonary hemorrhagic fever” of unknown etiology in the central part of the Korea, particularly in Yeoju and Icheon in the Gyeonggi Province. The ill people showed fever, cough, and hemoptysis, and some of them died with rapid progression of symptoms. As reported to public health authorities as well as across mass media, the epidemic became a social issue and gained academic attention. Subsequent cases occurred in Chungbuk Province, Paju in Gyeonggi Province, and army bases in Gangwon Province. Accordingly, the Korean Society of Infectious Diseases (KSID) held a symposium on this epidemic of pneumonitis-like disease of unknown etiology at the 14th annual conference on November 29, 1975, presenting the epidemiological investigation and patterns, clinical pictures and progression, X-ray findings, and autopsy and pathological findings of the disease. The Korean Medical Association (KMA) also held a panel discussion on the “epidemic of pneumonitis-like disease from the year's fall” on December 1, 1975 to understand the specifics of the epidemic [6]. All the presentations from the KSID symposium were published later as special articles in the Journal of the KMA in April, 1976 [7,8,9,10,11,12,13,14]. Based on the epidemiological investigation conducted in 121 patients in Yeoju and Icheon in Gyeonggi Province, many cases occurred during the rice harvesting seasons, and the majority of them were young men (n = 108, 89.3%) working in agriculture (n = 114, 94.2%). Many patients performed rice reaping (n = 101, 83.5%) and threshing (n = 95, 78.5%), and some cases worked for more than 10 hours per day (n = 71, 58.7% and n = 64, 38.0%, respectively). The case fatality rate of 5.7% (n = 7) was lower compared to 17% reported to public health centers. Cases developed mild to severe symptoms. While most patients complained of fever and chills, headache, and malaise, more than half cases had cough, myalgia, and hemoptysis. The illness lasted for 3–10 days [7]. The radiological findings of the 151 patients analyzed revealed lung involvement (n = 137, 91.7%). Based on these findings, primary atypical pneumonia or viral pneumonia was suggested as a potential cause of the disease [10,11,12]. The autopsy findings of four patients aged 21 - 24 years who died of hemoptysis indicated systemic infection characterized by cardiac, pulmonary, hepatic, adrenal, gastric, and cerebral hemorrhage and monocyte infiltrations, especially with hemorrhagic interstitial pneumonia [14]. In addition, the Korean Armed Forces Capital Hospital reported 20 patients with acute febrile hemorrhagic lung disease of unknown cause who were young and previously healthy [15]; some cases developed rapid progressive acute pulmonary edema, dyspnea, and death, others recovered completely within short periods of time despite relatively widespread pulmonary involvement. There was no person-to-person transmission within groups, alternatively considering for investigation of environmental hygiene in the involved areas. Therefore, multiple speculations were made regarding the cause of this disease, such as pesticide poisoning, pulmonary allergic condition, and idiopathic viral pneumonia; however, the etiology of the disease remained undetermined. Two studies reported later in February 1980 that the disease had occurred every year before as well as after the epidemic in 1975, on the basis of a retrospective review of patients admitted to Wonju Presbyterian Hospital [16,17]. Nevertheless, the condition had no longer gained a widespread public interest since the epidemic in 1975.
4) Identification of leptospirosis during the second epidemic (1984)
On September 1984, there was the second epidemic of the disease following a flood. Many patients engaged in post-flood restoration of rice plants. The epidemic spread beyond the areas affected by the previous epidemic to Jeonnam, Jeonbuk, Gyeongbuk, and Chungnam Provinces, with the increasing numbers of deaths. With the efforts of the public health authority and specialists in academia, the disease was finally confirmed as leptospirosis. Briefly, Jungsoon Kim, an epidemiologist in Seoul National University, established a hypothesis based on the findings of the previous studies and described the disease as follows: a systemic infection, no person-to-person transmission, occurrence in association with rice harvesting in fall, having epidemiological setting of wet rice fields with mud, the causative agent to be maintained its lifecycle in carriers, with incidentally infecting humans, and prolonged survival outside of reservoirs, and rodents which were abundant in rice fields in fall, serving as carriers. The differential diagnoses included endemic typhus, scrub typhus, other rickettsioses, Korean hemorrhagic fever, new viral disease, and leptospirosis. Leptospirosis was chosen to be the most likely diagnosis. Furthermore, epidemiological investigations could identify the environmental exposure among residents of Gangwon Province (Wonju, Hongchun, Wonsung, and Hoengsung) and military personnel in Gwangju in Jeonnam Province, supporting of the hypothesis [18]. Accordingly, the research team in the Korea National Institute of Health (KNIH) successfully isolated Leptospira strains from clinical samples (blood, cerebrospinal fluid, and urine) of two patients with the hemorrhagic pneumonitis-like disease in Wonju Presbyterian Hospital, and from wild rats caught in the epidemic areas (Wonju, Hoengsung, Hongchun, and Gwangju). The Leptospira isolates were further confirmed for a causative-relationship using guinea pigs according to the four criteria of Koch's postulates [19]. In addition, a research team in the Yonsei University also reported the isolation of Leptospira strains from two patients in Hongchun Hospital as well as from wild rats caught in Gwangju [20].
In a retrospective view, the confirmation of the first epidemic of leptospirosis occurred in the Korea was delayed by at least 10 years, probably due to unusual clinical presentation characterized by pulmonary hemorrhage and dyspnea leading to death in early stage, in contrast to the well-known traditional manifestations of Weil's disease accompanied by jaundice and kidney renal failure.
5) Yearly trends in the occurrence of leptospirosis (1987 – 2015)
The exact number of cases of “hemorrhagic pneumonitis-like disease” occurred was unknown before the first epidemic of 121 cases in 1975. The 1976 report of the KNIH described 80 cases (6 deaths, 7.5%) with the disease occurred in Gyeonggi, Gangwon Chungbuk, and Chungnam provinces in 1976 [21]. As already described, two retrospective studies identified clinically the cases admitted to the hospital, including 18 patients (6 deaths) between 1970 and 1974 [16], 11 (2 deaths) in 1977, 13 (5 deaths) in 1978, 3 in 1979, 7 in 1980, 2 in 1981, and 6 in 1982 [17]. These studies also indicated that the disease had been endemic in the Korea.
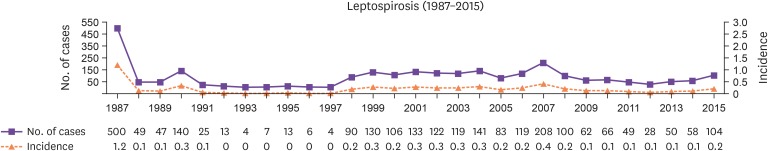
Since serological diagnosis of leptospirosis was available at the KNIH in 1985, approximately 200 cases (only some cases were confirmed serologically) in 1984, 264 cases in 1985, and 50 cases in 1986 were estimated based on the results of the microscopic agglutination test. In 1987, 562 cases were reported mostly from Jeonnam and Jeonbuk Provinces affected in the large epidemic. The reported cases then decreased significantly after 1991 [22]. According to the National Notifiable Disease Surveillance System from the Korea Centers for Disease Control and Prevention (KCDC) (http://is.cdc.go.kr/nstat), the annual incidence rate ranged from 0.01 to 1.2 per 100,000 population from 1987 to 2015, depending on the presence of the epidemic in sizes (Fig. 1). In a surveillance system constructed in the Yangpyeong Gun (county level) in Gyeonggi Province by Choi et al., the attack rate of leptospirosis from September to December, 1989 was 1.12 - 3.35 per 10,000 people in 1989, and increased to 3.63 - 9.85 per 10,000 people (projected to the population of the county) in 1990 following a flood. This study indicated that the incidence rates revealed approximately 50-fold higher than the number of cases reported nationally [23].
Figure 1. Annual number of reported cases of leptospirosis and incidence per 100,000 population (1987 – 2015).
6) Estimation of leptospirosis by seroepidemiological studies (1985 – 1990)
(1) Serologic tests of “leptangamushi diseases” for acute febrile illnesses
With the confirmation of epidemics of leptospirosis and scrub typhus in the Korea in 1984 and 1987, respectively, Ho Wang Lee, an expert in Hantaan virus, introduced the need for serology-based differential diagnosis of the acute febrile illnesses referred as “leptangamushi diseases” (leptospirosis, Hantaan virus infection, and tsutsugamushi disease) especially in seasons when the diseases were commonly prevalent. The reasons were included as follows: the diseases were febrile illnesses that showed early symptoms similar to hemorrhagic fever with renal syndrome (HFRS), which had been endemic in the Korea; natural reservoirs were rodents; the diseases occurred each year; people at risk were soldiers, farmers, or outdoor workers. He reported the results of serological tests for “leptangamushi diseases” among the serum samples requested to the Viral Disease Laboratory at Korea University for antibody tests of HFRS between 1985 and 1987. Based on the serological diagnostic criteria alone, 697 of 2,135 patients (33%) tested in 1985 were diagnosed with HFRS, 435 of 1,554 cases (28%) with leptospirosis, and 129 of 1,230 (11%) with scrub typhus. The remaining 41% of patients had undetermined causes. In 1986, 34% (706/2,068), 4% (64/1,593), 31% (215/692), and 52% (1,083/2,068) of patients were diagnosed with HFRS, leptospirosis, scrub typhus, and undetermined causes, respectively [24]. Since some residents in endemic areas could retain residual antibodies of the diseases over long periods of time after asymptomatic infections, he emphasized the observance of extreme caution when performing serological differential diagnosis, and described the possibility of combined infections where antibodies of two diseases might be present in a small number of cases. The seroepidemiological view on “leptangamushi disease” was once introduced in Harrison's textbook, with providing an important approach currently in serological differential diagnosis of patients with febrile illnesses in fall.
(2) Seropositivity of Leptospira antibody among patients with acute febrile illness and residents in endemic areas
The KNIH performed a seroepidemiological study using the macroslide agglutination test for Leptospira antibody among residents of 17 Guns in 5 provinces (Gyeonggi, Gangwon, Chungbuk, Gyeongbuk, and Jeonnam) between February 1985 and July 1986. The overall seropositive rate was 11.69% (113/967). The percent frequency by region was 17.06% in Gangwon, 16.18% in Gyeonggi, 10.17% in Chungbuk, and 6.17% in Gyeongbuk. There was no notable sex difference, but the rates were significantly higher in people aged between 41 - 50 years (19.8%) and 51–60 years (19.2%). In the seroepidemiological study performed among residents of 17 cities and Guns in 9 provinces between February and May 1987, the seropositive rate was 5.9% (68/1162), and the regional positive rate was 14% in Chungbuk, 12% in Jeonbuk, and 8% in Jeonnam, reflecting the decreased number of cases of leptospirosis in 1986 compared to those reported in 1985. In the meantime, the study using the microscopic agglutination test (MAT) conducted in 1,141 patients with suspected leptospirosis in Seoul, Gyeonggi, Gangwon, Chungbuk, Gyeongbuk, Jeonbuk, and Jeonnam between the spring of 1986 and June 1987, 132 patients (11.6%) showed titers above 1:80 [25,26]. Subsequently, between 1986 and 1990, several research laboratories and institutes analyzed and reported the yearly, monthly, and regional occurrence of leptospirosis in local residents as well as the patients with acute febrile illness through seroepidemiological investigation [27,28,29,30,31].
2. Disease characteristics
1) Identification of the causative Leptospira serovars
Leptospira, belonging to the family Leptospiraceae, is a thin (width: 0.1 μm, length: 6 - 20 μm) and coiled aerobic Spirocheta. Leptospires can be observed under the dark-field microscope or phase-contrast microscope. Its end is hooked, and is extremely active motility when bent or rotating. Leptospires requires specialized media for culture and takes several weeks to months to grow. The genus Leptospira is characterized by antigenic and genetic heterogeneity and can be further classified genetically according to phylogeny and virulence or serologically. Serovar is defined as a leptospire whose homologous rabbit antiserum agglutinates it, but cannot be defined to a single isolate [3]. Serovar identification of isolated leptospires in a given region is necessary for development of diagnostic reagents and vaccines and is vital for research on changes in antigenicity or pathogenicity. When the cross-agglutination absorption test (CAAT) of two strains shows significant differences in antigen (residual titer >10%), they belong to different serovars [32]. Standard strains represent each serovar, and more than 250 serovars were found in 26 serogroups. Since CAAT takes a great deal of time and effort, it is limited for timely identification and epidemiological investigation of strains causing epidemics, and the test may also fail to show subtle but important antigenic differences between strains. Since the early 1980s, relatively quick and accurate tests, such as antigen agglutination assay using monoclonal antibodies [33], and restriction enzyme DNA analysis, have been available to complement CAAT [34].
During the initial stage of serovar identification, the researchers in KNIH performed CAAT for 15 strains isolated in 1985 (11 from patients and 4 from rats) using 17 reference strains and their respective antisera obtained from the American CDC, Japanese NIH, and Ehime University. HM3 and HV8 strains were initially reported as serogroup icterohaemorrhagica serovar Mwogolo, and HS7 as serogroup canicola serovar Canicola, respectively. The remaining strains were found to be similar to Mwogolo or Birkini or could not be clearly identified [35]. The American CDC also determined that these strains were serovar Mwogolo. In the meantime, MJ Kim reported that three strains isolated from patients in Yeoju (HY-1, HY-2, and HY-10) were clearly different from serovar Mwogolo or Birkini in analyses using shiromizu, RGA, and smithi monoclonal antibodies produced by Kobayashi in Japan [36]. She also informed that the pulmonary hemorrhage observed in these patients were similar to those observed in leptospirosis epidemics in China and that the major serovar responsible for the Chinese epidemics was serovar Lai [37,38]. Subsequently, Jang et al. compared the DNA restriction fragments of 21 Korean isolates belonging to the icterhemorrhagiae serogroup and reported that they showed a restriction fragment pattern identical to serovar Lai isolated from China, except a band of difference caused by a point mutation [39]. Jang et al. also analyzed 29 Korean leptospiral isolates for reactivity patterns to monoclonal antibodies produced from the WH-20 strain isolated in Wonju area. Of them, 23 isolates were identified as serovar Lai and 3 were possibly new serovars [40,41]. Cho et al. also analyzed the serovars of 24 strains isolated from patients and 68 strains isolated from rats using CAAT and the monoclonal antibody assay. They reported that most strains were serovar Lai and 5 strains, including HM-3 and 18R, may be new serovars [42,43]. In conclusion, Oh et al. successfully proved that HM3 and 18R were new serovars, named as serovar Yeonchon and serovar Hongchon; these serovars were internationally registered as new serovars [44].
2) Epidemiology aspects
(1) Natural reservoirs and routes of transmission
Wild rats are known to be the most important reservoir for leptospirosis, and other domestic animals, including sheep, goats, pigs, and cattle, are also known as reservoirs. As anti-leptospiral antibodies existed in dogs, cattle, and pigs in Korea, it is likely that animals have acted as reservoirs of leptospires for a very long time [45,46]. Leptospires are excreted in an infected animals' urine and can survive for several weeks in humid conditions, soil with neutral pH, or water. Human infections occur when skin with small abrasions is exposed to an environment contaminated with Leptospira species, or when contaminated aerosol or droplets come into contact with the nose, mouth, or eyes. However, human to human transmission can occur very rarely.
Researchers in KNIH isolated 69 Leptospira strains from rats between 1984 and 1987 in Wonsung, Hongchun, Yangju, Wonju, Cheolwon, and Gwangsan in Gangwon Province; from Gwangju in Jeonnam Province; and in Paju, Yeoju, and Yeoncheon in Gyeonggi Province. In particular, 64 strains were isolated from A. agrarius, 2 from Rattus norvegicus, 1 from Cricetulus tritonnestor, and 1 from Crocidura lasiura. The carriage rate of Leptospira species from wild rats was 15.5% (7/45) in 1984, 14.9% (44/295) in 1985, 1.6% (4/247) in 1986, and 30.9% (13/42) in late 1987 in Yeoju and Paju, demonstrating notable regional differences [19,25,26]. In 292 native Korean cattle and 226 pigs in Gyeonggi, Chungcheong, Gangwon, and Gyeongsang Provinces, the seropositivity rate was 4.1–8.6% in cattle from Gyeonggi Province and 5.7% in pigs from Gyeonggi and Chungnam Provinces (17.6% in Cheongyang and Dangjin, Chungnam Province) [26,47]. These results demonstrated that wild rats, particularly A. agrarius, are important natural reservoirs of Leptospira species in the Korea and that a correlation was found between years with epidemics and carrier rates in wild rats.
(2) Epidemiological characteristics of epidemics in the Republic of Korea
Human leptospirosis can be classified into water-borne infections or those associated with domestic animals. Cases related to domestic animals occur often in dairy workers in the United Kingdom, United States, New Zealand, Australia, and Israel. Miners, sewage disposal workers, fishers, and soldiers have a high risk of infection. Farmers may become infected from contact with contaminated fields or crops. Leptospirosis can occur throughout the year, but usually fluctuates with season. Climate factors such as periods of heavy rainfall and crop-raising cycles may be associated with seasonal fluctuation of cases [48].
The epidemiological characteristics of leptospirosis in the Korea were described during the epidemics in 1975 and 1984 [7,8,49]. Most cases were actively working farmers rather than seniors. Occurrence of cases was associated with rice threshing or long periods of rice reaping during harvesting season, or with post-flooding restoration of rice plants. A significant number of cases had skin abrasions or injuries on their hands or legs. The incubation period was between 2 and 15 days (average: 5 days). Many soldiers also contracted the disease after they participated in the group work of tying fallen rice plants following flooding; therefore, soldiers belonged to a high-risk group [8,49,50,51,52]. According to the field investigation on geographical characteristics of some areas, rain-fed rice fields resembling stairs between rice field ridges in mountainous valleys in Gangwon Province were found to provide an environment enabling for long-term survival of leptospires. Moreover, the presence of multiple rat holes in rice field ridges with rice grains scattered around indicated that these acted like a good habitat for rats [49].
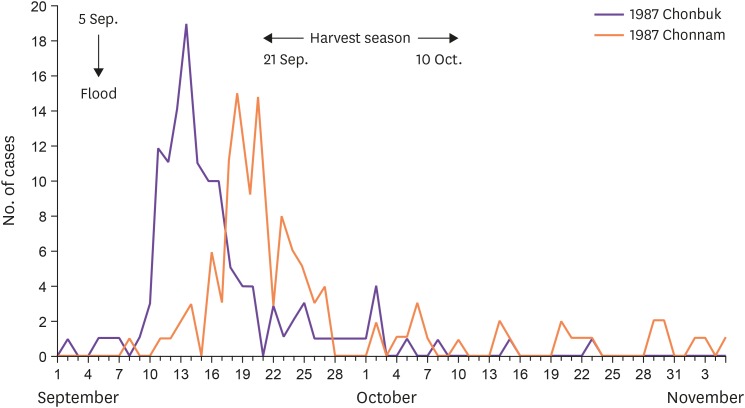
Occurrence of cases showed a seasonal pattern that started in early August, peaked in September and October, and decreased in November. In particular, the past epidemics were associated with localized heavy rain, flooding, or typhoons just before the harvesting season [53]. In relation to the 1984 and 1987 epidemics, flooding occurred across the country around the harvesting season, which brought disaster and severe crop damages. Localized torrential downpours with 200 - 300 mm of daily precipitation were recorded in Wonju in Gangwon Province between September 1 and 3, 1984. In Jeonra Provinces, the daily precipitation was 100 - 200 mm between September 5 and 6, 1987. These numbers were much higher than the monthly precipitation of 63 - 96 mm and 41 - 71 mm in September and October of the previous year, respectively. Occurrence of cases following a flood during the harvest season in Jeonnam and Jeonbuk Provinces have been shown well in the epidemic curves in 1987 (Fig. 2). In Yeoju, Gyeonggi Province, rain continued from mid-September in 1985, delaying rice harvesting until October. Nonetheless, there was a typhoon and heavy rain on October 5 during the harvest, followed by localized heavy rainfalls between October 10 and 13.
Figure 2. The epidemic curve of cases with leptospirosis following a flood in Chunbuk and Chunnam area of the 1987 epidemic, Korea (Adapted from Proceedings of Leptospirosis Research Conference 1990).
When there was heavy rainfall in the central part of the country between September 8 and 11, 1990, with a total precipitation of 500 mm, an epidemic of leptospirosis was anticipated; an epidemiologic study was conducted in Yangpyeon-gun, Gyeonggi Province, where soldiers participated in post-flooding restoration of rice fields. When the participated 446 soldiers underwent primary and secondary serological tests, the rate of infection was 11.2% [95% confidence interval (CI), 8.3% – 14.1%], the rate of symptomatic infection 1.8% (95% CI, 0.7% – 3.1%), and pathogenicity 16.0% (95% CI, 6.0% – 26.0%). The relative risk of attack rate revealed to depend on the type of work performed; 3.5-fold higher in those tied fallen rice plants for 3 days or longer, 2.7-fold higher in those tied fallen rice plants for 1–2 days, and 2.1-fold higher in those with other tasks [51]. Another study showed that two occurrences of typhoons and the floods during September 2000 were associated with occurrence of leptospirosis in 12 auxiliary police officers who worked in post-flooding restoration across the country, with one additional fatal case [54].
3) Clinical aspects
Leptospirosis shows various clinical manifestations, ranging from mild flu-like illness to fatal Weil's disease. Clinical severity depends on virulence of the serovar causing the infection, the size of bacterial inoculum into the body, the host susceptibility, and the organs involved. Even cases caused by an identical serovar may show different clinical manifestations by the region. Therefore, the term “serovar-specific syndrome” is no longer used. Clinical course of leptospirosis may show a biphasic pattern comprising the leptospiremic and immune phases. In the leptospiremic phase, leptospires are present in the blood, cerebrospinal fluid, and most other tissues, causing flu-like illness (high fever, headache, conjunctival edema, myalgia, nausea, and vomiting) for 4–7 days. When the disease enters the immune phase following 1–2 afebrile days, the patients show fever, accompanied by meningeal symptoms, uveitis, and myalgia. In general, 90% of patients develop mild anicteric infections and recover spontaneously, whereas 5%–10% progress to Weil's disease [3,48].
In the Korea, the earlier description of the diseases before the causative agent was not identified focused on pulmonary manifestations titled as “hemorrhagic pneumonitis-like disease” or “epidemic pulmonary hemorrhagic fever”; patients often showed dyspnea, hemoptysis, or blood-tinged sputum, and severe cases died of asphyxiation due to massive hemoptysis from pulmonary hemorrhage and acute respiratory failure within 4 days. Although many patients recovered without sequelae, studies included more severe cases with pulmonary involvement reported a higher case fatality (average of 15.2%) [55]. In addition, pathological findings of pulmonary hemorrhage were reported [13,14,15]. The chest X-ray findings were characterized in detail [11,12]; lung infiltration either bilateral or more prominent on the right; more prominent on the lateral lung fields; diffuse interstitial infiltrations or alveolar lesions. The chest X-ray findings worsened on day 3, as was the case for clinical symptoms; further worsened within several hours or 1–2 days; and peaked within 5–6 days. The pulmonary findings then improved rapidly like pulmonary edema, which was a clear difference from other types of pneumonia [55]. The pulmonary hemorrhage finding in leptospirosis had been already described in China between 1959 and 1960, which might be associated with serovar Lai as a major causative strain reported in both countries [56]. Since the late 1990s, leptospirosis has regained attention as an emerging infectious disease in several countries, and severe pulmonary form of leptospirosis (SPFL) in epidemic or sporadic cases has also been reported in Brazil, Nicaragua, Thailand, India, and Seychelles [57,58,59,60]. SPFL may appear in both anicteric and icteric leptospirosis. Even after 2000, sporadic cases of SPFL continued to occur in the endemic areas in the Korea [61]. In the meantime, the pulmonary involvement was observed in many areas, caused by various serovars, therefore, it is not a serovar-specific [62]. Korean researches have also investigated the pathogenic mechanism and pathophysiology of pulmonary hemorrhage, including direct toxicity of Leptospira species [63], toxin-induced damages to endothelial cells of alveolar capillaries [64], and cytotoxicity of pore-forming toxin [65,66].
Since serological diagnosis of leptospirosis was provided in the Korea, various clinical manifestations were reported, depending on the organs involved and disease severity: Weil's disease, pulmonary hemorrhage, acute kidney failure, influenza-like illness, and acute hepatitis. Regional differences in clinical manifestations were also described [56]. The earlier studies included severe cases referred to tertiary hospitals showed more severe clinical findings in frequency; hemoptysis (89%), oliguria (37%), jaundice (63%), and skin rash (18%) [67,68].
In terms of regional differences in clinical findings, of the 52 patients reported in Yeoju area in Gyeonggi Province, in 1985, 34.6% had hemoptysis; 65.4% and 48.1%, respectively, had elevated serum AST and ALT levels; 57.7% had lung infiltration; and 53.8% had abnormal urinary sediments. Jaundice, skin rash, kidney failure, central nervous system damage, and thrombocytopenia were relatively rare. More than 90% of patients were anicteric, and improved within 1 – 2 weeks, except two fatal cases [37]. In Chungnam Province, 6 cases with rashes were reported in 1984 and 1985 [69]. Of the 18 cases reported in 1985, 27.8% showed skin rashes, none of the patients experienced hemoptysis, and a few showed meningitis symptoms and jaundice [70]. In Chuncheon, Gangwon Province, 62.5% and 75% of 18 cases in 1985 showed pulmonary edema and congestion without hemoptysis and hypoalbuminemia, respectively [71]. Of the 13 cases reported in 1986, 90% or more showed anicteric hepatitis, demonstrating differences in clinical manifestations in the same area [72]. Of the 93 cases reported in Jeonbuk Province in the 1987 epidemic, hemoptysis, dyspnea, and hypotension were relatively common at 40%, 47%, and 41%, respectively, and 5 died of massive pulmonary hemorrhage [73]. Moreover, of the 127 cases from Jeonnam Province in the same epidemic, hemoptysis (46%) was more common in this area, along with dyspnea (22%) and hypotension (34%) [22]. As such, most patients had overlapped clinical findings based on the organs involved, and the frequency of blood-tinged sputum, dyspnea, and skin rash differed regionally.
3. Prevention and infection control
As the epidemic of leptospirosis was confirmed nationwide in the fall of 1984, health authorities subsequently discussed prevention and management strategies; systematic research on clinical microbiology of leptospirosis in the Korea (determination of the causative serovars, major serogroups responding to patient sera, regional statistics on incidence and prevalence, and clinical-epidemiological characteristics), animal reservoirs (wild rodents and domestic animals) and routes of transmission, investigation of antibody titer in residents (seropositivity rate and epidemiological investigation through surveys), and development of serological diagnosis (improved passive hemagglutination). Vaccine development was also planned for 2 years from August 1985. With support by the Ministry of Science and Technology and cooperation, all these works were actively performed in collaboration with hospitals across the country; the findings of these research efforts were described in detail in reports from the KNIH [25,47].
1) Detailed investigation of the occurrence
Differential diagnosis of leptospirosis from other febrile illnesses common during fall was difficult due to nonspecific clinical symptoms, and many people infected might be asymptomatic or have mild symptoms. Farmers were often financially unstable, and the disease occurred in the busiest season of harvesting, which may prevent them from seeking medical attention. Therefore, a prospective nationwide seroepidemiological investigation was performed to determine symptomatic and asymptomatic infections occurring among the patients who visited the hospitals. Six university hospitals in Gyeonggi, Gangwon, Chungbuk, Gyeongsang, and Jeonnam Provinces as well as Shinchon Hospital, Cheongju Hospital, Korean Armed Forces Capital Hospital, and Seoul National University Hospital, formed a collaborative network in 1985. Bacterial cultures and serological tests were taken from 1,313 patients with suspected leptospirosis, resulting in diagnoses of leptospirosis in 264 cases. Clinical and epidemiological characteristics of the patients were analyzed to confirm the timing and national distribution of infection, followed by surveys to determine the risk factors, including occupation, outdoor activities, and other environmental conditions.
2) Designation as a notifiable communicable disease and surveillance of occurrence
Leptospirosis was designated as a notifiable communicable disease in 1987 (belonged to the communicable diseases designated by the Minister of Health and Welfare for surveillance to assess epidemics). In December 1993, leptospirosis was designated again as a group 2 legal communicable disease (belonged to the communicable diseases that are included in the national vaccination program as they can be managed and prevented through vaccination). In 2001, leptospirosis was further designated as a group 3 notifiable communicable disease, which requires continued surveillance and establishment of prevention strategies. When a patient is diagnosed or an autopsy is performed, the case should be reported without delay.
3) Prevention and management strategies
Preventive measures for leptospirosis can be divided into management of reservoirs, management of contaminated environment, and management of humans. It is impossible to eradicate wild rats that are leptospiral carriers. Therefore, it is necessary to prevent rats from penetrating potential access points by maintaining the environment clean. Management of humans can be divided into personal hygiene and vaccination.
(1) Development of Leptospira vaccine and a supplementary immunization
For the control of leptospirosis, the KNIH developed a formalin-killed cell vaccine using serovar Lai (HY-10 strain) isolated from a patient with fatal leptospirosis. The safety and immunogenicity of this vaccine in humans were confirmed. The government then introduced a supplementary immunization program in 1988; every year, 400,000 vials were produced by national pharmaceutical companies (Green Cross, CheilJedang, Dongsin, and Boryung Pharmaceutical) and were administered to residents and soldiers in areas with endemic areas. Consequently, the number of cases decreased significantly between 1991 and 1997. Leptospirosis was excluded from the supplementary immunization program in 1997, based on the following reasons: Inactivated vaccines lack cross-immune responses among various Leptospira species and offer only short-term protection. Moreover, the protective immunity are sometimes incomplete, and side effects may arise from contamination of media; therefore, the inactivated leptospirosis vaccine was discontinued.
(2) Public health projects on management of acute febrile illnesses common in fall
Each year, with monthly plans for management of infectious diseases, establishment and delivery of prevention and management strategies have been achieved through provincial, municipal, gun, and gu public health centers in August. In September, advertisement on prevention of acute febrile illnesses common in fall has been emphasized.
(3) Advertisement and education on personal hygiene through media
Leptospirosis cases have been continuously monitored in endemic areas, and prevention strategies through personal hygiene have been taught and advertised every fall through the media. These education and advertisement efforts were based on the findings of the epidemiological investigation of individuals that participated in local volunteering programs (soldiers, auxiliary police officers, and university students). Since pre-task education on the disease and systematic post-task management can be achieved in group work settings, it is possible to prevent the occurrence of diseases and their complications [52]. While local residents working in post-flood restoration of rice plants have adequate knowledge about leptospirosis, volunteers, public servants, and soldiers lack such knowledge and often work without suitable personal protective equipment. Therefore, prevention efforts were once again emphasized as below (refer to press release from September 1999):
- Since leptospirosis is common among individuals who work in rice fields after heavy rain during the harvesting season, individuals involved in post-flood restorations should pay attention.
- If the protective equipment is not worn, leptospires present in contaminated water may enter the body through skin abrasions or mucosa while working, causing leptospirosis.
- Therefore, when working in potentially contaminated water, protective equipment, such as gloves and boots, should be worn. If high fever, headache, and myalgia persist for more than 1 day after participating in restoration of rice plants, seek medical attention at nearby clinics, hospitals, or public health centers.
Footnotes
Conflict of Interest: No conflicts of interest.
- Conceptualization: MJK.
- Data curation: MJK.
- Formal analysis: MJK.
- Investigation: MJK.
- Methodology: MJK.
- Project administration: MJK.
- Writing - original draft: MJK.
- Writing - review & editing: MJK.
References
- 1.Inada R, Ido Y, Hoki R, Kaneko R, Ito H. The etiology, mode of infection, and specific therapy of Weil's disease (Spirochaetosis icterohemorrhagica) J Exp Med. 1916;23:377–402. doi: 10.1084/jem.23.3.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weil A. On a strange, acute infectious disease, accompanied by swelling of the spleen, icterus, and nephritis. Dtsch Arch Klin Med. 1886;39:209–232. [German] [Google Scholar]
- 3.Fain S. Leptospira and leptospirosis. Boca Raton: CRC press; 1994. pp. 1–19. [Google Scholar]
- 4.Chun C. An overview of acute infectious diseases in South Korea. Seoul: Newest Medical Publisher; 1975. pp. 155–156. [Google Scholar]
- 5.Chun CH. Zoonotic contagious disease in Korea. Korean J Infect Dis. 1975;7:37–42. [Google Scholar]
- 6.Kang SY, Park SC, Bahk YW, Chun C, Choi I. Panel discussion: A pneumonitis-like disease epidemic during this autumn. J Korean Med Assoc. 1975;18:1095–1102. [Google Scholar]
- 7.Park SC, Lee JH, Kim M, Park HC, Min SH, Lee BH, Kim CS. An epidemiological study on the epidemic pneumonitis, occurred in Ryeo Ju and I Cheon, central area of Korea, 1975. J Korean Med Assoc. 1976;19:263–268. [Google Scholar]
- 8.Nam SD. Epidemiological pattern of acute endemic respiratory diseases. J Korean Med Assoc. 1976;19:269–273. [Google Scholar]
- 9.Kim KH, Hong SJ, Lee HS, Kang MW, Kim HY, Chung KW, Chung HY, Chun CH, Kim SM, Lee CM, Kim JJ. Clinical pictures of the hemorrhagic pneumonia like disease which occurred epidemically in the central area of Korea in autumn, 1975. J Korean Med Assoc. 1976;19:274–286. [Google Scholar]
- 10.Chae IS, Shim BS, Chin CJ, Shin KC, Choi KO. An epidemiological, clinical, and radiological study of the epidemic pneumonitis, occurred in the central area of Korea in autumn, 1975. J Korean Med Assoc. 1976;19:287–292. [Google Scholar]
- 11.Bahk YW, Kim CY, Park SH, Suk YK. Radiologic manifestation of pneumonia-like disease occurred in the central area of Korea in autumn, 1975. J Korean Med Assoc. 1976;19:293–297. [Google Scholar]
- 12.Kim KS. On the radiologic findings. J Korean Med Assoc. 1976;19:298–302. [Google Scholar]
- 13.Han WS, Kim DS. Autopsy and postmortem needle biopsy findings of pneumonitis-like disease. J Korean Med Assoc. 1976;19:303–306. [Google Scholar]
- 14.Moon GJ. The gross and histopathological findings. J Korean Med Assoc. 1976;19:307–309. [Google Scholar]
- 15.Ro YM, Yuk SJ, Yoon HJ, Choi JS, Cho HK, Hahn BS, Kim KS, Park CI, Han HS. Acute febrile hemorrhagic lung disease of unknown cause – A report of 20 cases in the epidemic of October through November in 1975. J Korean Med Assoc. 1976;19:315–323. [Google Scholar]
- 16.Choe KH, Kim DS, Shin KC, Lee KY, Ro SK, Kim JJ, Lee JT, Shim BS, Shim YH, Chai IS. Epidemic pulmonary hemorrhagic fever: II. Retrospective study (1970-1974) J Korean Med Assoc. 1980;23:145–150. [Google Scholar]
- 17.Shim YH, Shim BS, Choe KH, Kim DS, Shin KC, Lee KY, Lee YW, Kim YJ, Chin CJ, Lee JT, Chai IS. Epidemic pulmonary hemorrhagic fever: I. Epidemiological and clinical observation. J Korean Med Assoc. 1980;23:131–144. [Google Scholar]
- 18.Kim JS, Lee CW, Oh DK, In SD, Lee YH, Cho WH, Lee WY, Kim SO. An analytic epidemiological study to test the hypothesis, leptospirosis as the cause of epidemic pulmonary hemorrhagic fever in Korea. Korean J Epidemiol. 1984;6:8–15. [Google Scholar]
- 19.Cho MK, Paik SB, Oh HB, Song C. Bacteriological studies on leptospirosis in Korea (1984) Korean J Epidemiol. 1984;6:16–26. [Google Scholar]
- 20.Lee WY, Lee BK, Kim JD, Kim JS, Kim SO. Leptospira interrogans “Korea” isolated from patients with epidemic pulmonary hemorrhagic fever. Korean J Epidemiol. 1984;6:36–46. [Google Scholar]
- 21.Paik SB, Shin YO, Chung IB, Kim KH, Chai IS. Isolation and identification of pathogen for pneumonitis-like disease epidemic in South Korea. Korea National Institute of Health Annual Report. 1976;13:127–134. [Google Scholar]
- 22.Kim MJ. Infectious diseases occurring in autumn season in South Korea: Clinical and epidemiological characteristics of leptospirosis. J Korean Med Assoc. 1994;37:1408–1414. [Google Scholar]
- 23.Choi BY, Kang SM, Lee SJ, Park HB, Kim DW, Oh SJ, Kim JS. The surveillance and management system of leptospirosis in a rural community of Korea, 1989 and 1990. Korean J Epidemiol. 1993;15:74–84. [Google Scholar]
- 24.Lee HW. Seroepidemiologic studies of acute hemorrhagic diseases in Korea from 1985 to 1987 (hemorrhagic fever with renal syndrome, leptospirosis and scrub typhus) J Korean Med Assoc. 1988;31:581–593. [Google Scholar]
- 25.National Institute of Health. Studies on the Epidemiology of Leptospirosis in Korea (I). Final report from year 1. 1986. pp. 109–127. [Google Scholar]
- 26.Cho MK. Characterization of Leptospira interrogans isolated in Korea and seroepidemiological study on leptospirosis (1984-1987) J Korean Med Assoc. 1988;31:612–622. [Google Scholar]
- 27.Cho MK, Min CH, Kim YW, Yoon CS. Serological studies on leptospirosis in Kangwondo area (1985) J Korean Soc Microbiol. 1986;21:205–210. [Google Scholar]
- 28.Chang WH, Choi MS, Park KH, Lee WK, Kim SY, Choi IH, Choe KW, Woo JH, Song YW, Choi DH, Lee JH, Kim WY, Kee JI, Park YS, Kang SK, Park SK, Yoon SY, Kim JW, Chung SS, Kim SY. Seroepidemiological study of leptospirosis in Korea, 1987. Korean J Infect Dis. 1988;20:179–186. [Google Scholar]
- 29.Chang WH, Choi MS, Kee SH, Kim IS, Park CS, Kim IJ, Choi SB, Choe KW, Woo JH, Kang JS, Choi DH, Kim JW, Kim SH, Lee JH, Kim SY, Kee JI, Kim SY, Park KH, Yoon SY, Kim MC, Kang SK, Lee YK, Lee WK, Choi IH, Kim BC. Seroepidemiological survey of leptospirosis in Korea, 1988 and 1989. J Korean Soc Microbiol. 1990;25:341–346. [Google Scholar]
- 30.Kim YW, Cho MK, Kim HS, Yoon CS, Yoo KS, Lee JH, Min CH. Patterns of acute febrile illness (murine typhus, scrub typhus, leptospirosis and hemorrhagic fever with renal syndrome) from 1986 to 1990 in Korea. J Korean Soc Microbiol. 1991;26:431–441. [Google Scholar]
- 31.Chang WH, Kim IS, Choi MS, Kee SH, Hahn MJ, Seong SY, Uhm KH, Lee JH, Kang JS, Kim SY, Park KH, Kim IJ. Seroepidemiological survey of the leptospirosis in Korea, 1986-1991. J Korean Soc Microbiol. 1993;28:13–22. [Google Scholar]
- 32.Dikken H, Kmety E. Serological typing method for leptospires. In: Bergan T, Norris Jr, editors. Methods in Microbiology. Vol. 11. New York: Academic Press; 1978. pp. 259–309. [Google Scholar]
- 33.Kobayashi Y, Tamai T, Oyama T, Hasegawa H, Sada E, Kusaba T, Hamaji M. Characterization of monoclonal antibodies against etiological agents of Weil's disease. Microbiol Immunol. 1984;28:359–370. doi: 10.1111/j.1348-0421.1984.tb00687.x. [DOI] [PubMed] [Google Scholar]
- 34.Marshall RB, Wilton BE, Robinson AJ. Identification of leptospira serovars by restriction-endonuclease analysis. J Med Microbiol. 1981;14:163–166. doi: 10.1099/00222615-14-1-163. [DOI] [PubMed] [Google Scholar]
- 35.Oh HB, Park KS, Cho MK. Serological analysis of Leptospira interrogans isolated in Korea by cross-agglutinin adsorption method (1985) J Korean Soc Microbiol. 1986;21:337–343. [Google Scholar]
- 36.Kim MJ. Serovar identification of Korean leptospiral strains with monoclonal antibodies. Korean J Med. 1987;32:571–579. [Google Scholar]
- 37.Kim MJ, Park SC, Oh HB. Clinical features of serologically proven leptospirosis in Korea and changes in leptospiral agglutinin titer. Korean J Med. 1987;32:188–197. [Google Scholar]
- 38.Chen T. Development and present status of leptospiral vaccine and technology of vaccine production in China. Jpn J Bacteriol. 1985;40:755–762. doi: 10.3412/jsb.40.755. [DOI] [PubMed] [Google Scholar]
- 39.Chang WH, Kim SY, Seo JS. Restriction endonuclease DNA analysis of leptospiral field isolates from Korea. J Korean Soc Microbiol. 1987;22:463–471. [Google Scholar]
- 40.Chang WH, Park KH, Lee JB. Serological analysis of Leptospira interrogans isolated in Korea by monoclonal antibodies. J Korean Soc Microbiol. 1988;23:277–292. [Google Scholar]
- 41.Chang WH, Kim SY, Chun SW, Kee SH, Park KH, Kim IS. Restriction endonuclease DNA analysis and monoclonal antibody analysis of Leptospira interrogans isolated in Korea. J Korean Soc Microbiol. 1989;24:71–79. [Google Scholar]
- 42.Cho MK, Kim YW, Min CH, Oh HB. Serovar Determination of Leptospira interrogans isolated in Korea by cross-agglutinin absorption method (1984-1987) J Korean Soc Microbiol. 1988;23:169–177. [Google Scholar]
- 43.Cho MK, Lee JH, Yoon CS, Kim YW, Min CH, Kim YS, Park KS, Oh HB. Serological analysis of Leptospira Interrogans in Korea using monoclonal antibodies and cross-agglutinin absorption test. J Korean Soc Microbiol. 1989;24:539–548. [Google Scholar]
- 44.Oh HB, Chang WH, Cho MK, Seong WK, Park KS. Identification of new serovar yeonchon and hongchon belonging to Leptospira interrogans icterohemorragiae seogroup. J Korean Soc Microbiol. 1991;26:253–262. [Google Scholar]
- 45.Sekiguchi I. Leptospirosis on Kyonsang-buck-do. Saikingaku Zasshi. 1942;553:164–172. [Japaness] [Google Scholar]
- 46.Cha Y, Lee T. Study on leptospirosis, I. Seroepidemiological investigation of cattle. Domestic Animal Farming Hygiene Reports. 1959;6:53–59. [Google Scholar]
- 47.National Institute of Health. Studies on the Epidemiology of Leptospirosis in Korea (II). Final report from year 2. 1987. pp. 110–147. [Google Scholar]
- 48.Faine S World Health Organization (WHO) Guidelines for the control of leptospirosis. Vol. 67. Geneva: WHO; 1982. pp. 21–23. [Google Scholar]
- 49.Kim JS, Lee JW, Oh DK, In SD, Lee YH, Cho WH. An epidemiological study on identification of cause for epidemic pulmonary hemorrhagic fever. J Korean Med Assoc. 1985;28:77–78. [Google Scholar]
- 50.Chun HJ, Kim TY, Choi BK, Ahn CH, Oh JH, Kim YO, Lee WG, Kim JY, Byun HG, Lee HC, Park YJ. Clinical, roentgenological and pathological evaluation of hemorrhagic pulmonary fever. J Korean Military Med Assoc. 1985;16:154–166. [Google Scholar]
- 51.Choi BY, Chung DE, Lee SJ, Park HB, Park JB, Lee KH, Kim JS. An epidemiologic study on the leptospiral infection in the period of an anticipated epidemic - for soldiers stationed in a rural area. Korean J Epidemiol. 1992;14:91–101. [Google Scholar]
- 52.Lee HJ. A sero-epidemiologic study on leptospiros is among military personnel mobilized for harvesting in ricefield after flood [dissertation] Seoul: Seoul National University; 1993. [Google Scholar]
- 53.Kim MJ, Kang SK, Choi IS. Kobayashi YZ. Leptospirosis in Korea: clinical and epidemiologic study; Proceedings of Leptospirosis Research Conference 1990, Japanese Leptospirosis Research Society; Tokyo: Hokusen-sha pub; 1991. pp. 88–103. [Google Scholar]
- 54.Chang WG, Song MJ, Cha YH, Kim KG, Paik UH, Kim YK, Kim SY, Kim YJ, Cho MK, Lee GJ. An epidemiological and clinical study of leptospirosis acquired by twelves combat policemen in september, 2000. Korean J Med. 2001;61:553–561. [Google Scholar]
- 55.Choi KW. Clinical characteristics of epidemic pulmonary hemorrhagic fever summarized from papers published. Korean J Epidemiol. 1984;6:3–7. [Google Scholar]
- 56.Kim MJ. Clinical characteristics of leptospirosis in Korea. J Korean Med Assoc. 1988;31:623–627. [Google Scholar]
- 57.Silva JJ, Dalston MO, Carvalho JE, Setúbal S, Oliveira JM, Pereira MM. Clinicopathological and immunohistochemical features of the severe pulmonary form of leptospirosis. Rev Soc Bras Med Trop. 2002;35:395–399. doi: 10.1590/s0037-86822002000400017. [DOI] [PubMed] [Google Scholar]
- 58.Seijo A, Coto H, San Juan J, Videla J, Deodato B, Cernigoi B, Messina OG, Collia O, de Bassadoni D, Schtirbu R, Olenchuk A, de Mazzonelli GD, Parma A. Lethal leptospiral pulmonary hemorrhage: an emerging disease in Buenos Aires, Argentina. Emerg Infect Dis. 2002;8:1004–1005. doi: 10.3201/eid0809.010499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yersin C, Bovet P, Mérien F, Wong T, Panowsky J, Perolat P. Human leptospirosis in the Seychelles (Indian Ocean): a population-based study. Am J Trop Med Hyg. 1998;59:933–940. doi: 10.4269/ajtmh.1998.59.933. [DOI] [PubMed] [Google Scholar]
- 60.Dolhnikoff M, Mauad T, Bethlem EP, Carvalho CR. Pathology and pathophysiology of pulmonary manifestations in leptospirosis. Braz J Infect Dis. 2007;11:142–148. doi: 10.1590/s1413-86702007000100029. [DOI] [PubMed] [Google Scholar]
- 61.Kang SJ, Lee KJ, Park KH, Jung SI. Clinical features of leptospirosis experienced in a university hospital between 2001 and 2007. Korean J Med. 2009;77:453–460. [Google Scholar]
- 62.Kim MJ. Clinical relevance of pulmonary involvement in leptospirosis. Korean J Med. 2009;77:450–452. [Google Scholar]
- 63.Chang W, Kim I, Lee W, Park K, Lee J, Chi J, Lee J. Microbiological and pathological features of experimentally induced leptospirosis in guinea pigs. J Korean Soc Microbiol. 1986;21:211–226. [Google Scholar]
- 64.Woo JH. An experimental study of the pathogenesis of pulmonary hemorrhagic lesions in leptospirosis. Korean J Med. 1990;38:644–655. [Google Scholar]
- 65.Lee SH, Kim KA, Park YG, Seong IW, Kim MJ, Lee YJ. Identification and partial characterization of a novel hemolysin from Leptospira interrogans serovar lai. Gene. 2000;254:19–28. doi: 10.1016/s0378-1119(00)00293-6. [DOI] [PubMed] [Google Scholar]
- 66.Lee SH, Kim S, Park SC, Kim MJ. Cytotoxic activities of Leptospira interrogans hemolysin SphH as a pore-forming protein on mammalian cells. Infect Immun. 2002;70:315–322. doi: 10.1128/IAI.70.1.315-322.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lee JS, Yoon SC, Lee HY, Ahn KR, Kim SK, Chi JK. Clinical features of the case identified as leptospirosis. Korean J Epidemiol. 1984;6:47–51. [Google Scholar]
- 68.Lee JS, Ahn C, Oh HY, Kim S, Choi KW, Lee M, Chi JG, Kim YI, Sul DS, Park JM, Park YH. Clinical studies on leptospirosis in Korea. J Korean Med Assoc. 1986;29:537–547. [Google Scholar]
- 69.Kim SY, Yoon SJ, Kim JO, Lee BH. The leptospirosis associated with fever and rash. Korean J Infect Dis. 1986;18:19–23. [Google Scholar]
- 70.Kim SJ, Kim JM, Hyun CO, Hong SY, Song BS, Rhu HK, Park SC. A clinical study of leptospirosis in Chung Nam area. Korean J Infect Dis. 1987;19:33–37. [Google Scholar]
- 71.Kim WY, Han SY, Kim SK, Suh JE, Joo SA, Kim KM. The 16 cases of leptospirosis in Chuncheon area. Korean J Med. 1986;30:745–750. [Google Scholar]
- 72.Lee YC, Lee SH, Kwak ST, Hong KI, Choi MK, Kim YK, Kim KM, Kim YW, Cho MK. The 13 cases of confirmed leptospirosis in Chun Cheon area, by the culture and isolation of leptospira, in 1986. Korean J Med. 1987;32:580–587. [Google Scholar]
- 73.Park SK, Lee SH, Rhee YK, Kang SK, Kim KJ, Kim MC, Kim KW, Chang WH. Leptospirosis in Chonbuk Province of Korea in 1987: a study of 93 patients. Am J Trop Med Hyg. 1989;41:345–351. [PubMed] [Google Scholar]