Abstract
Purpose
Post-hepatectomy liver failure (PHLF) is a severe complication in hepatocellular carcinoma (HCC) patients who have undergone hepatectomy. This research aimed to investigate the combination of albumin–bilirubin (ALBI) score and aspartate aminotransferase-platelet ratio index (APRI) as a novel approach in predicting PHLF risk in hepatitis B virus (HBV)-related HCC patients.
Patients and methods
HBV-related HCC patients who underwent hepatectomy from January 2006 to October 2013 were enrolled in this study. A novel model was constructed using a combination of ALBI and APRI scores to predict PHLF risk, and the prognostic value of the model was evaluated and compared with Child-Pugh (C-P) grade, ALBI score and APRI score.
Results
A total of 1,055 HCC patients were retrospectively studied, which included 151 experienced PHLF. Univariable and multivariate analyses showed that the ALBI and APRI scores were independent predictors of PHLF. The area under the ROC curve (AUC) of the ALBI score, APRI score, and C-P grade was 0.717, 0.720, and 0.602, respectively, with AUC (ALBI) > AUC (C-P) (P <0.001) and AUC (APRI) > AUC (C-P) (P <0.001). After ALBI was associated with APRI, the AUC (ALBI-APRI) was 0.766, and AUC (ALBI-APRI) > AUC (ALBI) (P <0.001), AUC (ALBI-APRI) > AUC (APRI) (P =0.047). Our results indicated that ALBI and APRI scores had higher discriminatory abilities than C-P grade in predicting the risk of PHLF, and the ALBI-APRI model could enhance the capability of predicting PHLF compared to ALBI or APRI alone.
Conclusion
ALBI-APRI score is a novel and effective predictive model of PHLF for HBV-related HCC patients, and its accuracy in predicting the risk of PHLF is better than that of C-P, ALBI and APRI scores.
Keywords: HCC, PHLF, ALBI, APRI, combination of ALBI and APRI
Introduction
Surgical resection is the most effective method for patients with resectable hepatocellular carcinoma (HCC).1–4 Nevertheless, most HCC patients have chronic liver disease,5 including hepatitis B and C, alcoholic and nonalcoholic liver disease, which can lead to liver cirrhosis and hepatic dysfunction. Patients with cirrhosis are at greater risk for post-hepatectomy liver failure (PHLF), which is a severe complication after hepatectomy and can lead to postoperative mortality.5,6 Despite improvements in surgical techniques and management the postoperative outcomes,7 PHLF remains a challenge for patients undergoing hepatectomy.8,9 Accurate preoperative evaluation of liver function and prediction of PHLF are thus essential for the determination of the feasibility of liver resection.6
Child-Pugh (C-P) grade has been incorporated into surgical management for HCC patients.2,5 However, the C-P grading system has specific deficiencies such as inclusion of ascites and encephalopathy.10–13 Recently, Johnson12 reported an albumin–bilirubin (ALBI) model to evaluate hepatic function in HCC patients, which was developed based on statistical evidence and eliminating subjective observation, and an important factor in this model is that the estimation of albumin and bilirubin is objectively conducted and can be assessed as a simple heat map or nomogram. Our previous study was the first to demonstrate that a preoperative ALBI score could predict PHLF more accurately than the C-P score in HCC patients who underwent hepatectomy.14 Subsequently, Toyoda and Hiraoka reported15,16 similar findings. However, ALBI score only includes serum albumin and bilirubin, and these two variables have no “ceiling effect.” Furthermore, serum albumin and bilirubin are not ideal direct indicators of the severity of liver cirrhosis.14 Normally, liver biopsy (LB) remains the “golden standard” in evaluating the severity of cirrhosis. However, this invasive approach usually poses a heavy burden on patients. Thus, appropriate evaluation of liver cirrhosis often fails in many HCC patients before hepatectomy. The aspartate aminotransferase to platelet ratio index (APRI) was reported by Wai17 is an effective tool for assessing the severity of cirrhosis and was determined to be comparable to LB. Castéra18 verified that APRI score could be a noninvasive, rapid, and reliable model for evaluating liver cirrhosis, even to the point of replacing LB, and supported the conclusion that this model was effective for assessing liver function. Subsequently, Ichikawa19 reported that preoperative APRI score is effective for independently predicting PHLF after hepatectomy in HCC patients. We also verified that preoperative APRI score can be effective predictor of PHLF, especially in patients with high hepatitis-B virus (HBV) DNA load or cirrhosis.20 However, APRI score also only includes serum AST and PLT levels, and these two quantitative variables have no “ceiling effect.” In addition, serum AST and PLT levels are not ideal direct indicators of liver function. Thus, the efficacy of APRI scores for evaluating liver function reserve and predicting PHLF remains controversial. Liver function reserve and the severity of cirrhosis must be considered simultaneously when predicting PHLF.
To date, neither ALBI nor APRI scores have been extensively used due to their limitations. The advantages of ALBI and APRI scores include their ability to compensate for each other’s limitations, and the new model that combines these two variables may enhance PHLF prediction. However, these results require confirmation using other measures. This research aimed to investigate the efficacy of the combination of ALBI and APRI (ALBI-APRI) scores to predict the risk of PHLF in HBV-related HCC patients who underwent hepatectomy via a retrospective study involving a large population.
Materials And Methods
Patients
In this research, patients diagnosed with HCC who were initially treated with hepatectomy from January 2006 to October 2013 at the Guangxi Medical University Cancer Hospital were enrolled. This research was approved by the Clinical Research Ethics Committee of the Guangxi Medical University Cancer Hospital. And all patients provided written informed consent. Our inclusion criteria were as follows: 1) pre-operative C-P grade A or B; 2) infected with HBV; and 3) postoperative pathology confirmed HCC and liver cirrhosis. The exclusion criteria were: 1) received other anticancer treatments for HCC before hepatectomy such as transcatheter arterial chemoembolization, ablation, and radiofrequency; 2) had other concurrent malignancies; and 3) have renal, cerebral, or cardiopulmonary dysfunction.
Definitions
Resection of three or more Couinaud liver segments was considered as major liver resection.21 The existence of gastroesophageal varices or splenomegaly with a PLT count <100 × 109/L was considered as clinically significant portal hypertension (CSPH).22 Based on the criteria of the International Study Group of Liver Surgery, patients with an increased serum TBil and INR level on postoperative day 5 are considered as PHLF.8 The postoperative mortality was determined by death within 3 months after surgery.
Calculation Of Score Values
The ALBI score = 0.660 × log10 [TBil (µmol/L)] − 0.085 × (ALB [g/L]).12 The APRI score = [(AST (U/L)/ULN)/PLT count (109/L)] × 100.17 Furthermore, based on the odds ratios (OR) of ALBI and APRI scores from multivariate analysis results in our study, the ALBI-APRI score = 5.280 × ALBI + 1.583 × APRI. All parameters of the above formulae were analyzed within 1 week before hepatectomy to ensure that the patients did not receive albumin supply and platelet infusion or others before the test.
Treatment And Follow-Up
Surgeries were carried out by experienced surgeons. Type and extent of resection were determined before surgery based on tumor size, number, location, and hepatic functional reserve. The indications of liver resection and details of surgery procedures are as described in the previous studies.20,23
After discharge, all patients underwent regular follow-up. Routine reexamination included serum AFP levels, serum biochemistry, abdominal ultrasound scan, and CT or MRI.
Statistical Analysis
The continuous variables with normal distribution are represented as the mean ± SD, whereas the non-normal distribution was represented as the median (range), and the categorical parameters were presented as frequencies.
To determine independent risk factors of PHLF, variables with P < 0.100 in the univariate logistic analysis were included in the multivariate logistic regression. The discriminatory ability of the C-P, ALBI, APRI, and ALBI-APRI scores to predict PHLF risk was estimated by the area under the ROC curve (AUC) analysis. SPSS version 19.0 was used for statistical analyses, and P <0.05 was considered statistically significant.
Results
This study enrolled a total of 1,629 HCC patients who underwent curative hepatectomy. Of these, 574 patients (35.2%) were excluded for the following reasons: 207 patients (12.7%) were not infected with HBV; 24 patients (1.5%) were infected with HCV; 301 patients (18.5%) had received other anti-HCC treatments before operation; 27 patients (1.7%) had other simultaneous malignant tumors; and 15 patients (0.9%) had renal, cardiopulmonary, or cerebral dysfunction. Finally, 1,055 HCC patients met the inclusion criteria were included in this research.
Baseline Characteristics
Baseline characteristics of the 1,055 HCC patients are shown in Table 1. All participating patients had associated HBV and liver cirrhosis, which was confirmed by postoperative histological examination. Most patients (95.5%) had C-P grade A, whereas the other 47 patients had C-P grade B. Approximately 835 patients underwent minor resection, whereas the remaining 220 patients underwent major resection.
Table 1.
Baseline Characteristics Of The Included 1055 Patients With HBV-Related HCC
| Variables | Patient Population (n = 1055) |
|---|---|
| Age (≥60/<60 yrs) | 162 (15.4%)/893 (84.6%) |
| Sex (male/female) | 921 (87.3%)/134 (12.7%) |
| Total bilirubin (μmol/L) | 12.4 (2.7 ~66.8) |
| Albumin (g/L) | 40.9 (24.9 ~54.4) |
| Aspartate aminotransferase (U/L) | 42 (14 ~459) |
| Platelet count (109/L) | 172 (12 ~668) |
| Prothrombin time (sec) | 12.9 (9.4 ~22.4) |
| AFP (≥400/<400 ng/mL) | 432 (40.9%)/623 (59.1%) |
| CSPH | 219 (20.8%) |
| Ascites | 183 (17.3%) |
| C-P grade (A/B/C) | 1008 (95.5%)/47 (4.5%)/0 (0%) |
| C-P score | 5 (5–9) |
| ALBI score | −2.77 (−3.91 ~ −1.14) |
| APRI score | 0.64 (0.11 ~23.75) |
| Tumor size (cm) | 6.0 (1.0 ~25.0) |
| Tumor number (≥3/<3) | 128 (12.1%)/927 (87.9%) |
| Extent of resection (major/minor) | 220 (20.9%)/835 (79.1%) |
| Blood loss (>400/≤400 mL) (n) | 338 (32.0%)/717 (68.0%) |
Abbreviations: AFP, alpha fetoprotein; CSPH, clinically significant portal hypertension; C-P, Child-Pugh; ALBI, albumin–bilirubin; APRI, aspartate aminotransferase to platelet ratio index; HBV, hepatitis B virus; HCC, hepatocellular carcinoma.
Morbidity And Mortality
Of the 1,055 patients, 579 (54.9%) had at least one or more postoperative complications. The most common complication was pleural effusion (17.8%), followed by ascites (16.0%), PHLF (14.3%), and others (6.8%). Grade A PHLF occurred in 54 patients (5.1%), grade B in 84 (8.0%), and grade C in 13 (1.2%). Besides, the postoperative 3-months mortality rate was 1.0% (11 patients). 9 patients died of PHLF, and 2 patients died of acute cardiopulmonary failure.
Univariable And Multivariable Analyses Of PHLF
According to univariable analysis, CSPH, tumor size, C-P score, ALBI score, APRI score, blood loss ≥ 400 mL and major liver resection were determined as independent predictors for PHLF (Table 2). Multivariable logistic analysis covered CSPH, ALBI score, APRI score, blood loss ≥ 400 mL and major liver resection (Table 2). Based on the multivariate analysis results, the odds ratio (OR) of ALBI score was 5.280 (2.763–10.086, 95% CI; P <0.001), and the OR of APRI score was 1.583 (1.275–1.964, 95% CI; P <0.001). Thus, ALBI-APRI scores were calculated as follows: 5.280 × ALBI + 1.583 × APRI; median (range): −13.41 (−20.03 to 27.76).
Table 2.
Univariable And Multivariable Analyses For PHLF
| Variable | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Age (≥60 years) | 1.450 (0.934–2.252) | 0.098 | 1.054 (0.902–2.059) | 0.118 |
| Sex (female) | 0.345 (0.165–0.721) | 0.005 | 0.332 (0.149–0.737) | 0.007 |
| AFP (≥400 ng/mL) | 1.005 (0.708–1.427) | 0.976 | – | – |
| CSPH | 5.208 (3.614–7.505) | < 0.001 | 3.573 (2.298–5.556) | < 0.001 |
| C-P score | 2.102 (1.647–2.681) | < 0.001 | 0.940 (0.665–1.329) | 0.726 |
| ALBI score | 8.501 (5.244–13.781) | < 0.001 | 5.280 (2.763–10.086) | < 0.001 |
| APRI score | 2.156 (1.777–2.617) | < 0.001 | 1.583 (1.275–1.964) | < 0.001 |
| Tumor size (cm) | 1.069 (1.025–1.114) | 0.002 | 0.989 (0.934–1.047) | 0.696 |
| Tumor number (≥3) | 1.438 (0.889–2.327) | 0.139 | - | - |
| Major liver resection | 2.566 (1.769–3.722) | < 0.001 | 2.986 (1.845–4.835) | < 0.001 |
| Blood loss (>400 mL) | 3.423 (2.404–4.874) | < 0.001 | 2.294 (1.503–3.502) | < 0.001 |
Abbreviations: AFP, alpha fetoprotein; CSPH, clinically significant portal hypertension; C-P, Child-Pugh; ALBI, albumin–bilirubin; APRI, aspartate aminotransferase to platelet ratio index; PHLF, post- hepatectomy liver failure.
Discriminatory Performance Of ALBI And APRI Scores In Predicting PHLF As Compared To The C-P Grade
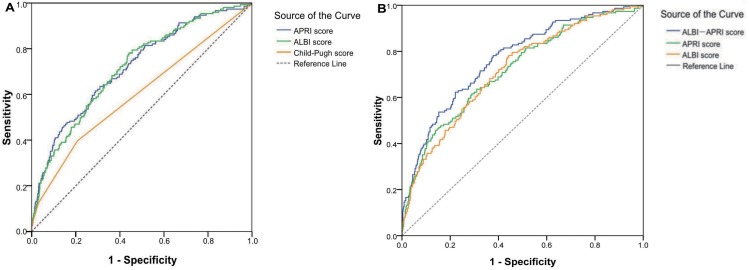
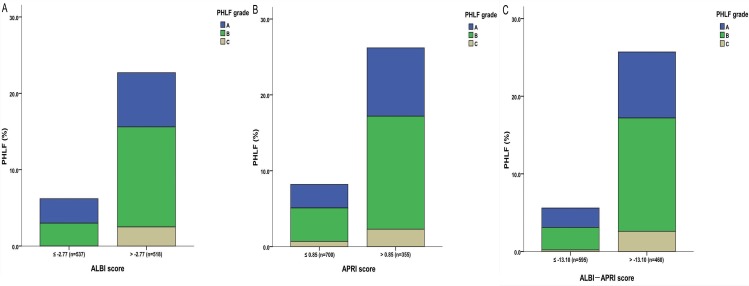
AUC analysis revealed that the ALBI score (AUC 0.717, 95% CI 0.689–0.744) and APRI score (AUC 0.720, 95% CI 0.692–0.747) for predicting the risk of PHLF were higher than the C-P grade (AUC 0.602, 95% CI 0.572–0.632) (P <0.001) (Figure 1A). There was no significant discrepancy between ALBI and APRI scores (P = 0.940). With an optimal cut-off value of −2.77, the ALBI score had a sensitivity of 78.1% and a specificity of 55.8% for predicting the risk of PHLF. The optimal cut-off value of the APRI score was 0.85, with a sensitivity of 61.6% and a specificity of 71.0% for predicting the risk of PHLF. Patients with ALBI scores > −2.77 had a higher incidence of PHLF than those patients with ALBI scores ≤ −2.77: 118 (22.8%) of 518 and 33 (6.1%) of 537, respectively (P <0.001). When the ALBI scores > −2.77, grade A PHLF was observed in 37 patients (7.1%), grade B in 68 (13.1%), and grade C in 13 (2.5%). In contrast, when the ALBI score was ≤ −2.77, grade A PHLF only developed in 17 patients (3.2%), grade B in 16 (3.0%), and grade C in 0 (0%) (Table 3, Figure 2A). Similarly, patients with APRI scores > 0.85 also had a higher incidence of PHLF than those patients with APRI scores ≤ 0.85: 93 (26.2%) of 355 and 58 (8.3%) of 700, respectively (P <0.001). When the APRI scores > 0.85, grade A PHLF was observed in 32 patients (9.0%), grade B in 53 (14.9%), and grade C in 8 (2.3%). By contrast, when the APRI score ≤ 0.85, grade A PHLF only developed in 22 patients (3.1%), grade B in 31 (4.4%), and grade C in 5 (0.7%) (Table 3, Figure 2B).
Figure 1.
(A) ROC curves for C-P grade, ALBI and APRI scores for predicting PHLF; (B) ROC curve for ALBI and APRI, combination of ALBI and APRI scores for predicting PHLF.
Abbreviations: PHLF, post-hepatectomy liver failure; C-P, Child-Pugh; ALBI, albumin–bilirubin; APRI, aminotransferase-platelet ratio index; ALBI-APRI, combination of ALBI and APRI.
Table 3.
Incidence And Severity Of ALBI, APRI And Combination ALBI-APRI Scores For Predicting PHLF
| ALBI Score | APRI Score | ALBI-APRI Score | |||||||
|---|---|---|---|---|---|---|---|---|---|
| ≤ −2.77 (n=537) | > −2.77 (n=518) | P Value | ≤ 0.85 (n=700) | > 0.85 (n=355) | P Value | ≤ −13.10 (n=595) | > −13.10 (n=460) | P Value | |
| PHLF | 33 (6.1%) | 118 (22.8%) | < 0.001 | 58 (8.3%) | 93 (26.2%) | < 0.001 | 33 (5.5%) | 118 (25.7%) | < 0.001 |
| PHLF A | 17 (3.2%) | 37 (7.1%) | < 0.001 | 22 (3.1%) | 32 (9.0%) | < 0.001 | 15 (2.5%) | 39 (8.5%) | < 0.001 |
| PHLF B | 16 (3.0%) | 68 (13.1%) | < 0.001 | 31 (4.4%) | 53 (14.9%) | < 0.001 | 17 (2.9%) | 67 (14.6%) | < 0.001 |
| PHLF C | 0 (0%) | 13 (2.5%) | < 0.001 | 5 (0.7%) | 8 (2.3%) | < 0.001 | 1 (0.2%) | 12 (2.6%) | < 0.001 |
Abbreviations: ALBI, albumin–bilirubin; APRI, aspartate aminotransferase to platelet ratio index; ALBI-APRI, combination of ALBI and APRI; PHLF, post-hepatectomy liver failure.
Figure 2.
Correlation of incidence and severity of PHLF and (A) ALBI score; (B) APRI score; (C) ALBI-APRI score.
Abbreviations: PHLF, post-hepatectomy liver failure; ALBI, albumin–bilirubin; APRI, aminotransferase-platelet ratio index; ALBI-APRI, combination of ALBI and APRI.
Discriminatory Performance Of ALBI-APRI Score For Predicting PHLF
The AUC of the ALBI-APRI model (AUC 0.766, 95% CI 0.739–0.791) for predicting the risk of PHLF was significantly higher than either the ALBI score (P < 0.001) or APRI score (P = 0.047) (Figure 1B). The ALBI-ARPI score cut-off value of −13.10 had a sensitivity of 78.1% and a specificity of 62.2% for predicting the risk of PHLF. Patients with ALBI-APRI scores > −13.10 had a higher incidence of PHLF than those patients with ALBI-APRI scores ≤ −13.10: 118 (25.7%) of 460 and 33 (5.5%) of 595, respectively (P < 0.001). When the ALBI-APRI scores > −13.10, grade A PHLF was observed in 39 patients (8.5%), grade B in 67 (14.6%), and grade C in 12 (2.6%). In contrast, when the ALBI-APRI scores ≤ −13.10, grade A PHLF was observed in only 15 patients (2.5%), grade B in 17 (2.9%), and grade C in 1 (0.2%) (Table 3, Figure 2C).
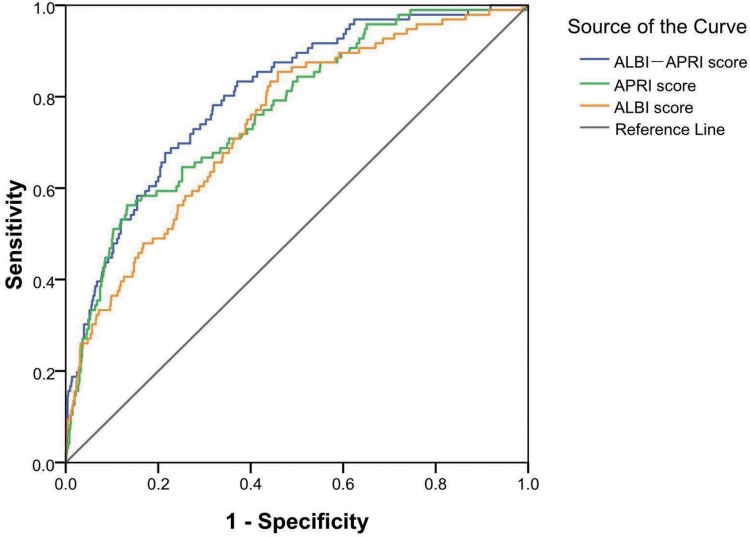
We then performed stratified analysis to evaluate the efficacy of ALBI-APRI model in predicting the risk of PHLF in HCC patients who underwent major and minor hepatectomy. Our results showed that ALBI-APRI score for predicting the risk of PHLF in HCC patients who underwent major hepatectomy was significantly greater than the ALBI score (0.683 vs 0.616; P < 0.001) and APRI score (0.683 vs 0.658; P <0.001) (Figure Supplement). After eliminating the effect of small remnant liver volume after major resection on PHLF, the AUC of the ALBI-APRI model for predicting the risk of PHLF in HCC patients who underwent minor hepatectomy was also significantly greater than that of the ALBI (0.805 vs 0.743; P < 0.001) and APRI (0.805 versus 0.770; P = 0.217) scores (Figure 3).
Figure 3.
ROC curves for ALBI, APRI, and ALBI-APRI scores for predicting the risk of PHLF for subjects who underwent minor resection.
Abbreviations: PHLF, post-hepatectomy liver failure; ALBI, albumin–bilirubin; APRI, aminotransferase-platelet ratio index; ALBI-APRI, combination of ALBI and APRI.
Discussion
Accurate preoperative evaluation of liver function reserve and cirrhosis are crucial to predicting PHLF and determining the feasibility of liver resection.1–4,6 Most HCC patients develop liver cirrhosis and liver dysfunction attributable to chronic liver disease, which are major risk factors for PHLF.5,6 PHLF is a severe complication after hepatectomy that can cause postoperative death.5,6 Even though the C-P grade remains the most frequently used model for evaluating preoperative liver function, its limitations have been extensively discussed.10,11 Besides, although LB is the golden standard for evaluating liver cirrhosis and fibrosis, it places a heavy burden on patients. Thus, many HCC patients do not undergo appropriate assessment of the liver reserves function and the severity of cirrhosis before liver resection, leading to high incidence of PHLF. In turn, there is a need to develop novel, reliable, noninvasive means of evaluating liver function and cirrhosis and in predicting the risk of PHLF before liver resection.
Our previous study14 demonstrated that ALBI score can more accurately predict PHLF risk in HCC patients after liver resection than C-P scores. Subsequent studies by Kuo15 and Hiraoka16 further supported our findings. The ALBI score has specific advantages in that it was founded based on statistical evidence that eliminated subjective observation.12 In this study, univariable and multivariable logistic analyses showed that ALBI score is an independent predictor of PHLF. And the discriminatory ability of ALBI score for predicting the risk of PHLF was better than the C-P grade (P < 0.001) (Figure 1A). With an optimal cut-off value of −2.77, the ALBI score had a sensitivity of 78.1% and a specificity of 55.8% for predicting the risk of PHLF, which was similar to the results of our previous study.14 Besides, patients with ALBI scores > −2.77 had a greater incidence and severity of PHLF than those patients with ALBI scores ≤ −2.77 (P < 0.001) (Figure 2A). In the present research, we excluded those patients without HBV and cirrhosis. Consistent with our analyses, the efficacy of ALBI score in predicting the risk of PHLF in HCC patients has again been confirmed. However, the ALBI score also have limitations. ALBI score includes only two indicators and have no “ceiling effect”, and bilirubin and albumin cannot be used to directly evaluate liver cirrhosis. Thus, using the ALBI model instead of the C-P grade to predict PHLF in HCC patients has not been widely accepted.
Consistent with the limitations of ALBI score, we investigated another method for assessing liver cirrhosis and PHLF, one reported by Wai17 in 2003 and called the APRI score and had power in assessing the severity of cirrhosis and fibrosis comparable to that of LB. The results of a study conducted by Castéra18 were consistent with those reported by Wai and indicated that the APRI score could be a rapid, reliable, and noninvasive model to estimate the status of liver cirrhosis and suitable for replacing LB. Subsequently, Ichikawa19 reported that a preoperative APRI score could be used to independently predict PHLF in HCC patients. We also demonstrated that preoperative APRI score can act as an effective predictor of PHLF, especially in patients with high HBV-DNA load or cirrhosis.20 In this research, the AUC values of the APRI score used to predict PHLF risk were greater than the C-P grade (P < 0.001) (Figure 1A). The cut-off value of the APRI score was 0.85, with a sensitivity of 61.6% and a specificity of 71.0% for predicting the risk of PHLF. Importantly, patients with APRI scores >0.85 had greater PHLF values than patients with scores of ≤0.85 (P < 0.001) (Figure 2B). Even though the APRI score has advantages with respect to evaluating liver cirrhosis and fibrosis, AST and PLT counts are not ideal direct variables suitable for evaluating liver dysfunction. For this reason, APRI score has not been well accepted as a replacement of C-P grade to predict PHLF in HCC patients.
It is notable that liver function reserve and severity of cirrhosis must be considered simultaneously when predicting PHLF. Although ALBI and APRI scores have their own limitations, interestingly, consistent with their advantages, they probably may have a moderate ability to supplement each other, and using the two in concert may increase their discriminatory power in predicting PHLF. In this research, when ALBI score was used in combination with APRI score, the ALBI-APRI model was found to have greater discriminatory power for the prediction of PHLF than either ALBI score (P < 0.001) or APRI score (P = 0.047) alone (Figure 1B). Patients with ALBI-APRI scores exceeding −13.10 had more PHLF than those with scores below this threshold (P <0.001) (Figure 2C). Furthermore, major liver resection was a risk factor for inadequate postoperative liver function reserve and PHLF.24 We executed stratified analysis to assess the accuracy of the ALBI-APRI model to predict PHLF risk in HCC patients who underwent major and minor resection. Although our results showed that the ALBI-APRI model for predicting the risk of PHLF in HCC patients who underwent major resection was significantly better than ALBI score (0.683 vs 0.616; P <0.001) and APRI score (0.683 vs 0.658; P < 0.001) (Figure Supplement), the AUC of the ALBI, APRI, and ALBI-APRI scores was all <0.7, which indicated that they have poor discriminatory power to predict PHLF risk in HCC patients who underwent major hepatectomy. Obviously, major resection has significant negative influence on the residual liver function. In this way, it has been well accepted that for any serum indocyanine green (ICG) clearance text, CT volumetry using three-dimensional reconstruction should be comprehensively considerate for precise evaluation of hepatic function reserve in HCC patients who underwent major resection.24 After eliminating the effect of major resection, the AUC of the ALBI-APRI model for predicting the risk of PHLF was significantly higher than the ALBI score (AUC 0.805 vs 0.743; P < 0.001) and APRI score (AUC 0.805 vs 0.770; P = 0.217) (Figure 3). The ALBI-APRI model could increase the discriminatory power to predict PHLF in patients with HBV-related HCC who underwent minor resection.
Here, we again confirmed that ALBI and APRI scores have greater discriminatory power than C-P grade for predicting the risk of PHLF in HBV-related HCC. With increasing ALBI and APRI scores, the incidence and severity of PHLF also increased. Importantly, our study is the first to show that ALBI-APRI model is a novel, rapid, and reliable tool for predicting PHLF in HBV-related HCC patients, and the combination of ALBI and APRI scores could enhance the discriminatory power in predicting PHLF as compared to ALBI or APRI score alone. However, this study still has some limitations. First of all, the main cause of HCC was chiefly HBV. More populations with different etiologies such as alcoholic liver disease or HCV must be studied in the future. Also, long-term survival analysis was not performed because HCC was not stratified by recurrence risk factors, including tumor capsule invasion, satellite nodules, and vascular invasion. Hence, the relationship between ALBI-APRI model and other risks of PHLF requires further prospective study in larger population. Furthermore, the capability of the ALBI-APRI model to predict PHLF risk in HCC patients who underwent major hepatectomy requires further evaluation.
Conclusion
ALBI-APRI score is a novel and effective predictive model of PHLF for HBV-related HCC patients, and its accuracy in predicting the risk of PHLF is better than that of C-P, ALBI and APRI scores.
Acknowledgments
This study was supported by the National Science Foundation of China Youth Fund Project (No. 81803007), Guangxi Natural Science Foundation Youth Fund Project (No. 2018GXNSFBA281030) and the National Natural Science Foundation of China (No. 81460426).
Abbreviations
HBV, hepatitis B virus; HCC, hepatocellular carcinoma; PHLF, post-hepatectomy liver failure; C-P, Child-Pugh; ALBI, albumin–bilirubin; APRI, aminotransferase-platelet ratio index; ALBI-APRI, combination of ALBI and APRI; AUC, area under the ROC curve.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67(1):358–380. doi: 10.1002/hep.29086 [DOI] [PubMed] [Google Scholar]
- 2.Galle PR, Forner A, Llovet JM, et al. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69(1):182–236. doi: 10.1016/j.jhep.2018.03.019 [DOI] [PubMed] [Google Scholar]
- 3.Zhou J, Sun H, Wang Z, et al. Guidelines for diagnosis and treatment of primary liver cancer in China (2017 edition). Liver Cancer. 2018;7:235–260. doi: 10.1159/000488035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Omata M, Cheng AL, Kokudo N, et al. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol Int. 2017;11(4):317–370. doi: 10.1007/s12072-017-9799-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hernaez R, Solà E, Moreau R, Ginès P. Acute-on-chronic liver failure: an update. Gut. 2017;66(3):541–553. doi: 10.1136/gutjnl-2016-312670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Den Broek MA, Olde DSW, Dejong CH, et al. Liver failure after partial hepatic resection: definition, pathophysiology, risk factors and treatment. Liver Int. 2008;28(6):767–780. doi: 10.1111/j.1478-3231.2008.01777.x [DOI] [PubMed] [Google Scholar]
- 7.Dimick JB, Wainess RM, Cowan JA, Upchurch GR, Knol JA, Colletti LM. National trends in the use and outcomes of hepatic resection. J Am Coll Surg. 2004;199(1):31–38. doi: 10.1016/j.jamcollsurg.2004.03.005 [DOI] [PubMed] [Google Scholar]
- 8.Rahbari NN, Garden OJ, Padbury R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011;149(5):713–724. doi: 10.1016/j.surg.2010.10.001 [DOI] [PubMed] [Google Scholar]
- 9.Schreckenbach T, Liese J, Bechstein WO, Moench C. Posthepatectomy liver failure. Dig Surg. 2012;29(1):79–85. doi: 10.1159/000335741 [DOI] [PubMed] [Google Scholar]
- 10.Durand F, Valla D. Assessment of the prognosis of cirrhosis: child-Pugh versus MELD. J Hepatol. 2005;42(Suppl1):S100–S107. doi: 10.1016/j.jhep.2004.11.015 [DOI] [PubMed] [Google Scholar]
- 11.Management consensus guideline for hepatocellular carcinoma. 2016 updated by the Taiwan Liver Cancer Association and the Gastroenterological Society of Taiwan. J Formos Med Assoc. 2018;117(5):381–403. doi: 10.1016/j.jfma.2017.09.007. [DOI] [PubMed] [Google Scholar]
- 12.Johnson PJ, Berhane S, Kagebayashi C, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol. 2015;33(6):550–558. doi: 10.1200/JCO.2014.57.9151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wiesner R, Edwards E, Freeman R, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124(1):91–96. doi: 10.1053/gast.2003.50016 [DOI] [PubMed] [Google Scholar]
- 14.Wang YY, Zhong JH, Su ZY, et al. Albumin-bilirubin versus child-pugh score as a predictor of outcome after liver resection for hepatocellular carcinoma. Br J Surg. 2016;103(6):725–734. doi: 10.1002/bjs.10095 [DOI] [PubMed] [Google Scholar]
- 15.Kuo YH, Wang JH, Hung CH, et al. The ALBI grade predicts the prognosis of patients with advanced hepatocellular carcinoma received sorafenib. J Gastroenterol Hepatol. 2017;32(12):1975–1981. doi: 10.1111/jgh.13783 [DOI] [PubMed] [Google Scholar]
- 16.Hiraoka A, Kumada T, Michitaka K, et al. Usefulness of albumin-bilirubin grade for evaluation of prognosis of 2584 Japanese patients with hepatocellular carcinoma. J Gastroenterol Hepatol. 2016;31(5):1031–1036. doi: 10.1111/jgh.13250 [DOI] [PubMed] [Google Scholar]
- 17.Wai CT, Greenson JK, Fontana RJ, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology. 2003;38(2):518–526. doi: 10.1053/jhep.2003.50346 [DOI] [PubMed] [Google Scholar]
- 18.Castéra L, Vergniol J, Foucher J, et al. Prospective comparison of transient elastography, Fibrotest, APRI, and liver biopsy for the assessment of fibrosis in chronic hepatitis C. Gastroenterology. 2005;128(2):343–350. doi: 10.1053/j.gastro.2004.11.018 [DOI] [PubMed] [Google Scholar]
- 19.Ichikawa T, Uenishi T, Takemura S, et al. A simple, noninvasively determined index predicting hepatic failure following liver resection for hepatocellular carcinoma. J Hepatobiliary Pancreat Surg. 2009;16(1):42–48. doi: 10.1007/s00534-008-0003-4 [DOI] [PubMed] [Google Scholar]
- 20.Mai RY, Ye JZ, Long ZR, et al. Preoperative aspartate aminotransferase-to-platelet-ratio index as a predictor of posthepatectomy liver failure for resectable hepatocellular carcinoma. Cancer Manag Res. 2019;11:1401–1414. doi: 10.2147/CMAR.S186114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pol B, Campan P, Hardwigsen J, Botti G, Pons J, Le TYP. Morbidity of major hepatic resections: a 100-case prospective study. Eur J Surg. 1999;165(5):446–453. doi: 10.1080/110241599750006686 [DOI] [PubMed] [Google Scholar]
- 22.Berzigotti A, Reig M, Abraldes JG, Bosch J, Bruix J. Portal hypertension and the outcome of surgery for hepatocellular carcinoma in compensated cirrhosis: a systematic review and meta-analysis. Hepatology. 2015;61(2):526–536. doi: 10.1002/hep.27431 [DOI] [PubMed] [Google Scholar]
- 23.Zhong JH, Xiang BD, Gong WF, et al. Comparison of long-term survival of patients with BCLC stage B hepatocellular carcinoma after liver resection or transarterial chemoembolization. PLoS One. 2013;8(7):e68193. doi: 10.1371/journal.pone.0068193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ge PL, Du SD, Mao YL. Advances in preoperative assessment of liver function. Hepatobiliary Pancreat Dis Int. 2014;13(4):361–370. [DOI] [PubMed] [Google Scholar]