ABSTRACT
Policy-makers worldwide are increasingly interested in scaling up evidence-based interventions (EBIs) to larger populations, and implementation scientists are developing frameworks and methodologies for achieving this. But scaling-up does not always produce the desired results. Why not? We aimed to enhance awareness of the various pitfalls to be anticipated when planning scale-up. In lower- and middle-income countries (LMICs), the scale-up of health programs to prevent or respond to outbreaks of communicable diseases has been occurring for many decades. In high-income countries, there is new interest in the scaling up of interventions that address communicable and non-communicable diseases alike. We scanned the literature worldwide on problems encountered when implementing scale-up plans revealed a number of potential pitfalls that we discuss in this paper. We identified and discussed the following six major pitfalls of scaling-up EBIs: 1) the cost-effectiveness estimation pitfall, i.e. accurate cost-effectiveness estimates about real-world implementation are almost impossible, making predictions of economies of scale unreliable; 2) the health inequities pitfall, i.e. some people will necessarily be left out and therefore not benefit from the scaled-up EBIs; 3) the scaled-up harm pitfall, i.e. the harms as well as the benefits may be amplified by the scaling-up; 4) the ethical pitfall, i.e. informed consent may be a challenge on a grander scale; 5) the top-down pitfall, i.e. the needs, preferences and culture of end-users may be forgotten when scale-up is directed from above; and 6) the contextual pitfall, i.e. it may not be possible to adapt the EBIs to every context. If its pitfalls are addressed head on, scaling-up may be a powerful process for translating research data into practical improvements in healthcare in both LMICs and high-income countries, ensuring that more people benefit from EBIs.
KEYWORDS: Scaling-up, evidence-based intervention, harms, equity, cost-effectiveness, ethics, health
Background
In lower- and middle-income countries (LMICs), the scale-up of health interventions is not a new concept, although it has been often called by other names. For many decades, through international and national agencies, small-scale interventions have been scaled up to larger populations in LMICs to prevent or respond to outbreaks of communicable diseases [1]. Preventable noncommunicable diseases are now becoming as much of a burden in LMICs as in high-income countries [2]. But not all scaling-up efforts produce the desired results. There is thus a shared interest in knowing the pitfalls of scaling-up, and addressing them on a global scale.
Evidence-based interventions (EBIs) are interventions that have been proven effective, efficacious and ready for dissemination [3]. For example, motivational interviewing is a reproducible intervention that has been shown to be effective for the primary and secondary prevention of disease by improving health behaviors such as medication adherence [4], smoking cessation [5], and physical activity [6]. However, this and other EBIs often stay at the research level and fail to reach the people who should benefit from them. To get better value for their investments in research, policy-makers are taking a new interest in scaling-up, defined by the World Health Organization (WHO) as ‘deliberate efforts to increase the impact of successfully tested health innovations so as to benefit more people and to foster policy and program development on a lasting basis’ [7,8].
Two examples of scaling up demonstrate very different processes. In Ghana, a successful community-based health services experiment was scaled up to 104 out of 110 districts [9]. The process included piloting, field demonstrations, resource assessment, leadership development, building and equipping facilities and assigning health staff, training counterparts and deploying volunteers. Authors credit its success to consensus building, a sense of ownership among the targeted communities, the presence of change agents, credibility of the change and demonstration of feasibility in the communities. They also credit the involvement of all levels of bureaucracy in the change.
In another example in British Columbia, Canada, a program to integrate physical education and healthy eating in schools was scaled up to reach 500,000 students and 81,000 teachers [10]. Scale-up involved establishing action zones, a central support team, school facilitators and stakeholder teams, a planning guide and resource directory, and bins filled with exercise equipment. This program credits its success at the micro-level to training and resourcing teachers, supportive school policies and sustained implementation. At the macro-level, they credit their success to multisectorial partnerships and embedded knowledge exchange mechanisms.
In high-income countries, the science of scaling-up is still in its infancy. Various frameworks have been proposed for guiding researchers and policy-makers in designing the scale-up of an EBI [7,11–19]. Researchers are also proposing methods for evaluating the scalability of interventions, using indicators such as coverage, impact and setting, to prepare researchers to include them in the earliest stages of their study designs [20]. While these frameworks appear convincing and the evolving discourse on scaling-up is enthusiastic, a brief scan of the literature for problems encountered during scale-up revealed a number of potential pitfalls.
The members of a multidisciplinary group in implementation science performed a brainstorming on potential pitfalls on the scaling-up of EBIs. This diverse team, including healthcare providers, a scale-up scientist, patient-oriented research specialists, graduate students, postdoctoral fellows, an information specialist, a biostatistician, research assistants, research coordinators, and a caregiver-research partner began to focus on knowledge translation over 15 years ago [21]. They have developed and validated a number of knowledge translation tools (e.g. decision aids, health provider training programs) in the field of shared decision making that they are planning to scale up. To anticipate points of concern, the team was presented with the notion of scaling up and several examples (in low- to high-income countries). They were asked to identify pitfalls they could predict in their own fields (i.e. what elements, in their experiences, readings or observations, could compromise the success of scaling up in those contexts). They debated these and reached consensus on the most important pitfalls. They then performed a literature scan (including low- to high-income countries) by searching PubMed for literature on the identified pitfalls using the snowball approach and a search of the grey literature (Google Scholar and WHO websites). Finally, they met again to discuss the literature and select the most relevant pitfalls (see Figure 1).
Figure 1.
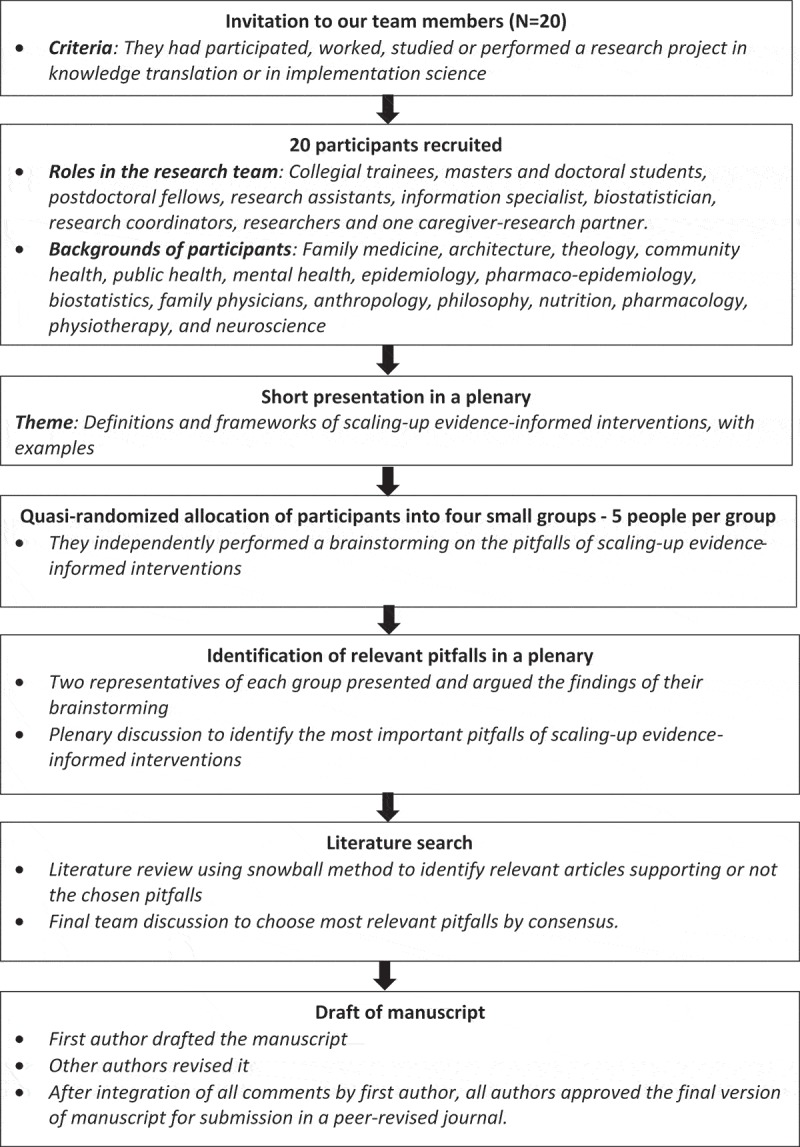
Flowchart of the pitfall identification process.
This debate paper is meant as a stimulant to further discussion on the topic of scaling up, as well as an advance warning. Scaling up is still a young science (although an old practice) and we focused on the pitfalls so that as the knowledge develops, researchers can be aware of them early on.
Six potential pitfalls of the scaling-up of EBIs were identified and considered relevant by our multidisciplinary group. They related to cost-effectiveness, equity, harms, ethics, bottom-up/top-down scaling-up, and the context in which the EBI was scaled up (see Figure 2). To discuss them, we identified 45 scaling-up studies that raised these difficulties, of which 13 were on cost-effectiveness estimates or cost-analysis models [22–34], 14 on equity [35–48], four on harms [16,49–52], three on ethics [53–55], six on top-down implementation [42,56–60], and eight on contextual problems [40,43,61–66]. Four out of the 45 studies identified covered more than one pitfall [40,42,43,47].
Figure 2.
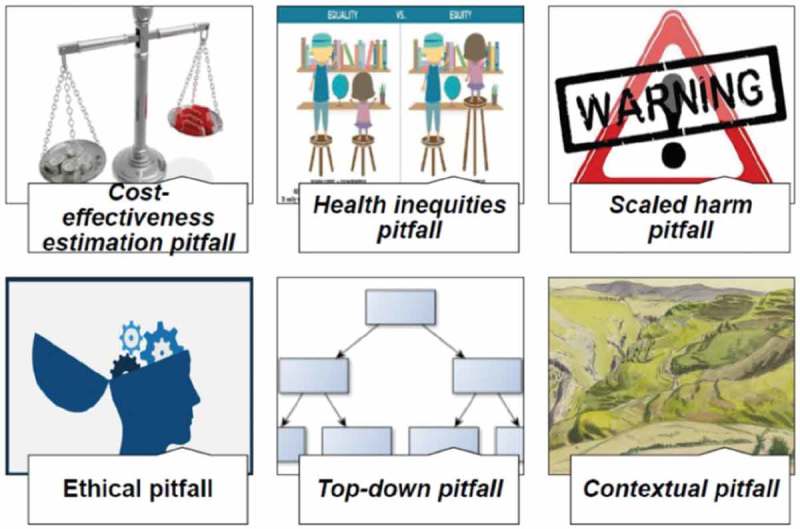
Pitfalls of scaling up evidence-based interventions.
The cost-effectiveness estimate pitfall: accurate cost-effectiveness estimates about real-world implementation are almost impossible
One of the incentives for promoting scaling up is the expectation of economies of scale, i.e. a decrease in costs proportionate to increased implementation. For example, the assumption that an increase in patient volume in a hospital service will reduce costs per patient in that service. However, unlike on factory production lines, economies of scale cannot be taken for granted in health services because of their heterogeneity. In the hospital example, increased volume in one service increased the costs per patient of other services in the hospital [67]. Planners may address this heterogeneity by using mathematical models to compare the cost-effectiveness of a variety of EBIs. One study, for example, compared the cost-effectiveness of scaling-up two service models for reducing maternal, fetal, and neonatal deaths in LMICs, and found that scaling-up midwifery services was almost twice as cost-effective as scaling-up obstetrics services [22].
However, cost-effectiveness estimates based on mathematical models are highly complex, contain inherent uncertainties, and depend on numerous assumptions not always based on evidence. A systematic review by Gomez et al. [25] showed that unfounded assumptions about such critical factors as cost, coverage and impact can substantially influence cost-effectiveness estimates. Cost-effectiveness estimates need to consider the size of the targeted population, the incidence or prevalence of the disease or risk factor, the significance of the intervention’s efficacy, and the amount spent or available [29].
Thus while many modelling studies show scaling-up EBIs to be cost-effective [22–24,26,27,30–34], they may not reflect the multi-factorial complexity of the real world. Categorical universal statements about the cost-effectiveness of scaling-up are thus difficult to justify. Further methodological work is needed to better approximate the cost-effectiveness of scaling-up EBIs.
The health inequities pitfall: some people will necessarily be left out
Many studies highlight equity as a motive for scaling-up effective healthcare interventions: an EBI that is delivered only to a small population constitutes a health inequity, as others are deprived of its proven health benefits [36,38–40,42,43,46–48].
Others point out the importance of ensuring the process of scale-up itself occurs in an equitable way [36,38–40,42,43,46–48], notwithstanding the challenge this represents [37,38,40,45]. A study in Zambia, for example, used equity measures when evaluating a scaling-up model for integrating HIV/AIDS treatment into primary care services [46]. The process not only improved the efficient use of staff time and clinic space but also the equitable delivery of care to HIV/AIDS and non-HIV/AIDS patients alike [46].
However, ensuring equitable access to the EBIs for a target population that includes poor and vulnerable groups, while maintaining its quality within a given budget, can be difficult [35,41], especially because sufficient material, financial and/or human resources are rarely available to these groups [44,45]. For example, during a similar campaign to scale up the distribution of insecticide-treated mosquito nets Africa-wide, equitable access to malaria treatment was reached in only 30% of studied countries, and the urban and richest quintile of households were the beneficiaries in most cases [45]. Considerations of equity must be integrated into scaling-up strategies and health equity metrics need further exploration.
The scaled-up harm pitfall: harms as well as benefits may be amplified by the scaling-up
Scaling-up EBIs risks amplifying their harms as well as their benefits [49–51]. For example, in their study about scaling-up male circumcision in the context of HIV prevention, Kilima et al. reported severe bleeding, delayed wound healing, and wound sepsis as the most frequent adverse effects [49]. These are the known risks of male circumcision, but they were amplified by the scaling-up. Indeed, the risks were disproportionally increased in the larger targeted population because of insufficient equipment or skills for sterilizing the circumcision tools, inadequate training of the healthcare providers, and lack of resources for monitoring the circumcised persons.
Evidence of the risks, feasibility and acceptability of an intervention in one context may not be sufficient to support its implementation on a wider scale [52]. Health authorities planning to scale up EBIs must explicitly predict harmful effects and risks, closely monitor them at the implementation phase, and take immediate steps to reduce or mitigate them.
The ethical pitfall: informed consent may be a challenge on a grander scale
Ensuring that all ethical requirements, such as informed consent, are met at the population level can be a challenge in scaling-up EBIs. For example, the United Nations Programme on HIV/AIDS and the WHO recommended in 2004 that for scaling-up ethical HIV/AIDS testing: 1) the results must be confidential; 2) the intervention must be accompanied by an appropriate counseling; and 3) consent to be tested must be given in an informed, specific and voluntary way by the person to be tested [53,55]. However, counselling and informed consent are slow and costly, and in reality may slow down the achievement of universal access to testing and to urgently needed treatment.
Sometimes, indeed, scaling-up itself is the ethical imperative, for example, the scale-up of community mental health services in countries where families and health professionals sometimes resort to deception, coercion and restraints in caring for people with debilitating mental illnesses. Yet scaling-up effective mental health services is difficult in a situation where resources are limited, the human rights of the mentally ill are routinely denied, and the legislative framework is weak [54].
The top-down pitfall: the needs, preferences and culture of end-users may be forgotten
When scaling-up takes place as a result of a decision from above, population-wide interventions may not reflect the specific needs, preferences, or values of the targeted end-users. Local communities may be disempowered, and the distance (geographical and/or cultural) between policy-makers, health authorities and those implementing the EBI on the ground may result in deformation of the original EBI. The alignment of EBIs with local end-user priorities and contexts, or a bottom-up approach, is essential for the success of scaling-up [47,57,59,60,68]. On the other hand, a top-down approach to scaling-up is likely to have more financial resources at hand and to prioritize interventions that address population-level risk factors and diseases. In addition, political will is a main facilitator of scaling-up EBIs [47,57,59,60,68]. EBIs that are scaled up using a bottom-up approach, which usually involves communities, patients and participatory methodologies, may lose their effectiveness as they demand a certain level of local engagement which is difficult to replicate at scale. However, some eras and political climates are more favorable for this kind of approach, such as the scaling up of the Jyorei community health insurance system in nineteenth-century Japan [42].
Ultimately, both bottom-up and top-down approaches seem to be necessary to optimize the success of scaling-up EBIs [58]. Those responsible for scaling-up EBIs need to collaborate closely with policy-makers and system managers as well as maintain close association with end-users such as clinicians, patients, caregivers and communities.
The contextual pitfall: inadequate knowledge of the context
The contextual factors that affect scaling-up can be social, physical, regulatory, political or economic [62]. They can be at the micro-, meso- or macro- scale. Lack of knowledge or understanding of these factors can be a major obstacle to effective scaling up [43,61,62,64–66]. At the micro-scale, for example, Chopra et al. assessed the infant feeding components of a scaled-up program to prevent mother-to-child HIV transmission in four African countries [61]. They observed that health workers almost universally believed (mistakenly) that an HIV positive mother who breastfeeds will always infect her child and that breastfeeding avoidance by a mother indicates she is HIV positive [61]. Providing additional financial resources may not be enough to change healthcare providers’ old clinical habits, beliefs, or their personal motivation to adopt new behaviors. The lack of the required number of qualified human resources to conduct the intervention can also limit scaling-up [40]. On the meso-level, scaling-up an EBI successfully also depends on the health system’s capacity to effectively deliver the EBI, including having the appropriate infrastructure, management, and leadership to make it possible [63]. And on the macro-level, success depends on efforts by regulatory, political and economic sectors to ensure the feasibility of the process [66]. Ultimately, it may not be possible to adapt the EBI to every context.
Conclusion
Scaling-up can be a powerful process for reducing evidence-practice gaps and spreading the benefits of EBIs to those who most need them, but there are significant pitfalls. Although this study did not survey the entire literature on scaling-up, it showed that in designing scale-up studies, investigators need to develop rigorous methods for addressing pitfalls related to cost-effectiveness, equity, ethical standards, amplification of potential harms, top-down implementation, and contextual appropriateness.
Responsible Editor Stig Wall, Umeå University, Sweden
Funding Statement
This work was funded by the Quebec SPOR-SUPPORT Unit [#SU1-139759] and the Canada Research Chair in Shared Decision Making and Knowledge Translation [#950-231200]. The Quebec SPOR-SUPPORT Unit is funded by the Canadian Institutes of Health Research (CIHR) and provincial partners including the Ministère de la Santé et des Services Sociaux (MSSS) du Québec and the Fonds de recherche du Québec – Santé (FRQ-S). The Canada Research Chair is also supported by the CIHR. Only the authors are responsible for the information provided or views expressed in this paper.
Acknowledgments
We thank Roxane Lepine, scientific librarian, for assistance in our literature search; and Louisa Blair, English-language scientific editor, for her kind help with the manuscript.
Author contributions
HTVZ, ABC and FL initiated the project. All authors contributed to the draft, and approved the final version of the manuscript.
Disclosure statement
No potential conflict of interest was reported by the authors.
Ethics and consent
Not applicable.
Paper context
This current debate paper is written in a context in which policy-makers worldwide are increasingly interested in scaling up evidence-based interventions (EBIs) to larger populations. Although the scaling-up of EBIs has the great potential to reduce the gap between EBIs and practices, major pitfalls need to be anticipated. This paper discusses these pitfalls to permit to investigators to better plan their scaling-up of EBIs.
References
- [1].Simmons R, Fajans P, Ghiron L, Organization WH . ExpandNet. Scaling up health service delivery: from pilot innovations to policies and programmes. Geneva (Switzerland): World Health Organization; 2007. [Google Scholar]
- [2].Gaziano TA, Pagidipati N.. Scaling up chronic disease prevention interventions in lower- and middle-income countries. Annu Rev Public Health. 2013;34:317–8. Epub 01/07. PubMed PMID: 23297660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Flay BR, Biglan A, Boruch RF, et al. Standards of evidence: criteria for efficacy, effectiveness and dissemination. Prev Sci. 2005;6:151–175. PubMed PMID: 16365954. [DOI] [PubMed] [Google Scholar]
- [4].Zomahoun HT, Guenette L, Gregoire JP, et al. Effectiveness of motivational interviewing interventions on medication adherence in adults with chronic diseases: a systematic review and meta-analysis. Int J Epidemiol. 2016. PubMed PMID: 27864410 DOI: 10.1093/ije/dyw273. [DOI] [PubMed] [Google Scholar]
- [5].Lundahl B, Moleni T, Burke BL, et al. Motivational interviewing in medical care settings: a systematic review and meta-analysis of randomized controlled trials. Patient Educ Couns. 2013;93:157–168. PubMed PMID: 24001658. [DOI] [PubMed] [Google Scholar]
- [6].O’Halloran PD, Blackstock F, Shields N, et al. Motivational interviewing to increase physical activity in people with chronic health conditions: a systematic review and meta-analysis. Clin Rehabil. 2014;28:1159–1171. PubMed PMID: 24942478. [DOI] [PubMed] [Google Scholar]
- [7].World Health Organization (WHO) Nine steps for developing a scaling-up strategy. Geneva: WHO; 2010. [Google Scholar]
- [8].Milat AJ, King L, Bauman A, et al. Scaling up health promotion interventions: an emerging concept in implementation science. Health Promot J Austr. 2011;22: 238 PubMed PMID: 22497071. [DOI] [PubMed] [Google Scholar]
- [9].Nyonator FK, Awoonor-Williams JK, Phillips JF, et al. The Ghana community-based health planning and services initiative for scaling up service delivery innovation. Health Policy Plan. 2005;20:25–34. PubMed PMID: 15689427. [DOI] [PubMed] [Google Scholar]
- [10].McKay HA, Macdonald HM, Nettlefold L, et al. Action schools! BC implementation: from efficacy to effectiveness to scale-up. Br J Sports Med. 2015;49:210–218. Epub 2014/ 10/15. PubMed PMID: 25312876. [DOI] [PubMed] [Google Scholar]
- [11].Milat AJ, Newson R, King L, et al. A guide to scaling up population health interventions. Public Health Res Pract. 2016;26:e2611604 Epub 2016/ 02/11. PubMed PMID: 26863167. [DOI] [PubMed] [Google Scholar]
- [12].Barker PM, Reid A, Schall MW. A framework for scaling up health interventions: lessons from large-scale improvement initiatives in Africa. Implement Sci. 2016;11:12 PubMed PMID: 26821910; PubMed Central PMCID: PMCPMC4731989 DOI: 10.1186/s13012-016-0374-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Milat AJ, King L, Newson R, et al. Increasing the scale and adoption of population health interventions: experiences and perspectives of policy makers, practitioners, and researchers. Health Res Policy Syst. 2014;12:18 Epub 2014/ 04/17. PubMed PMID: 24735455; PubMed Central PMCID: PMCPMC3996855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Adamou B, Curran J, Wilson L, et al. Guide for monitoring scale-up of health practices and interventions. 2013. Available from: https://www.cpc.unc.edu/measure/prh
- [15].Cooley L, Ved RR. Scaling up—from vision to large-scale change: a management framework for practitioners. Washington (DC): Management Systems International; 2012. [Google Scholar]
- [16].Yamey G. Scaling up global health interventions: a proposed framework for success. PLoS Med. 2011;8:e1001049 PubMed PMID: 21738450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Bhandari N, Kabir AK, Salam MA. Mainstreaming nutrition into maternal and child health programmes: scaling up of exclusive breastfeeding. Matern Child Nutr. 2008;4:5–23. PubMed PMID: 18289156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Simmons R, Fajans P, Ghiron L. Scaling up health service delivery: from pilot innovations to policies and programmes. 20 Avenue Appia, 1211 Geneva 27, Switzerland: World Health Organization; 2007. [Google Scholar]
- [19].Kohl R, Cooley L. Scaling up – A conceptual and operational framework MacArthur Foundation’s program on population and reproductive health. Washington (DC): 2005. [Google Scholar]
- [20].Ben Charif A, Hassani K, Wong ST, et al. Assessment of scalability of evidence-based innovations in community-based primary health care: a cross-sectional study. CMAJ Open. 2018;6:E520–E527. PubMed PMID: 30389751; PubMed Central PMCID: PMCPMC6221806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].France Légaré Canada research chair on shared decision making and knowledge translation, Quebec city, Canadan.d. [cited 2019 August21]. Available from: http://www.decision.chaire.fmed.ulaval.ca/accueil-en
- [22].Bartlett L, Weissman E, Gubin R, et al. The impact and cost of scaling up midwifery and obstetrics in 58 low- and middle-income countries. PloS One. 2014;9:e98550 Epub 2014/06/19. PubMed PMID: 24941336; PubMed Central PMCID: PMCPmc4062394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Brooker S, Kabatereine NB, Fleming F, et al. Cost and cost-effectiveness of nationwide school-based helminth control in Uganda: intra-country variation and effects of scaling-up. Health Policy Plan. 2008;23:24–35. Epub 2007/ 11/21. PubMed PMID: 18024966; PubMed Central PMCID: PMCPmc2637386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Cleary SM, McIntyre D, Boulle AM. Assessing efficiency and costs of scaling up HIV treatment. AIDS. 2008;22:S35–S42. Epub 2008/ 08/02. PubMed PMID: 18664951. [DOI] [PubMed] [Google Scholar]
- [25].Gomez GB, Borquez A, Case KK, et al. The cost and impact of scaling up pre-exposure prophylaxis for HIV prevention: a systematic review of cost-effectiveness modelling studies. PLoS Med. 2013;10:e1001401 Epub 2013/ 04/05 PubMed PMID: 23554579; PubMed Central PMCID: PMCPmc3595225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Goodchild M, Sahu S, Wares F, et al. A cost-benefit analysis of scaling up tuberculosis control in India. Int J Tuberculosis Lung Dis. 2011;15:358–362. Epub 2011/ 02/22.PubMed PMID: 21333103. [PubMed] [Google Scholar]
- [27].Marseille E, Jiwani A, Raut A, et al. Scaling up integrated prevention campaigns for global health: costs and cost-effectiveness in 70 countries. BMJ Open. 2014;4:e003987 Epub 2014/06/28. PubMed PMID: 24969782; PubMed Central PMCID: PMCPmc4078786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Marseille E, Larson B, Kazi D, et al. Thresholds for the cost-effectiveness of interventions: alternative approaches. Bull World Health Organ. 2015;93:118–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Musgrove P, Fox-Rushby J. Cost-effectiveness analysis for priority setting In: Jamison DT, Breman JG, Measham AR, et al, editors. Disease control priorities in developing countries. Washington (DC): World Bank; 2006; p. 271–285. [Google Scholar]
- [30].Scott N, McBryde ES, Thompson A, et al. Treatment scale-up to achieve global HCV incidence and mortality elimination targets: a cost-effectiveness model. Gut. 2016. Epub 2016/ 05/20. PubMed PMID: 27196586 DOI: 10.1136/gutjnl-2016-311504 [DOI] [PubMed] [Google Scholar]
- [31].Strand KB, Chisholm D, Fekadu A, et al. Scaling-up essential neuropsychiatric services in Ethiopia: a cost-effectiveness analysis. Health Policy Plan. 2016;31:504–513. Epub 2015/ 10/23 PubMed PMID: 26491060; PubMed Central PMCID: PMCPmc4986243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Tromp N, Siregar A, Leuwol B, et al. Cost-effectiveness of scaling up voluntary counselling and testing in West-Java, Indonesia. Acta Med Indones. 2013;45:17–25. Epub 2013/04/16.PubMed PMID: 23585404. [PubMed] [Google Scholar]
- [33].Turner HC, Truscott JE, Fleming FM, et al. Cost-effectiveness of scaling up mass drug administration for the control of soil-transmitted helminths: a comparison of cost function and constant costs analyses. Lancet Infect Dis. 2016;16:838–846. Epub 2016/ 02/22 PubMed PMID: 26897109. [DOI] [PubMed] [Google Scholar]
- [34].Yamamoto N, Mori R, Jacklin P, et al. Introducing HPV vaccine and scaling up screening procedures to prevent deaths from cervical cancer in Japan: a cost-effectiveness analysis. BJOG. 2012;119:177–186. Epub 2011/ 07/29. PubMed PMID: 21794070. [DOI] [PubMed] [Google Scholar]
- [35].Bennett S. Alternative approaches to extending health services to the poorest In: Bennett S, Gilson L, Mills A, editors. Health economic, development and household poverty: from understanding to action. London: Routledge; 2007; p. 117–133. [Google Scholar]
- [36].Bergh AM, Allanson E, Pattinson RC. What is needed for taking emergency obstetric and neonatal programmes to scale? Best Pract Res Clin Obstetrics Gynaecol. 2015;29:1017–1027. Epub 2015/04/30 PubMed PMID: 25921973. [DOI] [PubMed] [Google Scholar]
- [37].Byrne A, Morgan A, Soto EJ, et al. Context-specific, evidence-based planning for scale-up of family planning services to increase progress to MDG 5: health systems research. Reprod Health. 2012;9:27 Epub 2012/ 11/13 PubMed PMID: 23140196; PubMed Central PMCID: PMCPMC3563623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Cleary S. Equity and efficiency in scaling up access to HIV-related interventions in resource-limited settings. Curr Opin HIV AIDS. 2010;5:210–214. Epub 2010/06/12 PubMed PMID: 20539076. [DOI] [PubMed] [Google Scholar]
- [39].Hirschhorn LR, Talbot JR, Irwin AC, et al. From scaling up to sustainability in HIV: potential lessons for moving forward. Global Health. 2013;9:57 Epub 2013/ 11/10. PubMed PMID: 24199749; PubMed Central PMCID: PMCPMC3826849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Mangham LJ, Hanson K. Scaling up in international health: what are the key issues? Health Policy Plan. 2010;25:85–96. Epub 2010/ 01/15 PubMed PMID: 20071454. [DOI] [PubMed] [Google Scholar]
- [41].Mulholland E, Smith L, Carneiro I, et al. Equity and child-survival strategies. Bull World Health Organ. 2008;86:399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Ogawa S, Hasegawa T, Carrin G, et al. Scaling up community health insurance: Japan’s experience with the 19th century Jyorei scheme. Health Policy Plan. 2003;18: 270–278. Epub 2003/ 08/15.PubMed PMID: 12917268. [DOI] [PubMed] [Google Scholar]
- [43].Rollins N, Chanza H, Chimbwandira F, et al. Prioritizing the PMTCT implementation research agenda in 3 African countries: INtegrating and scaling up PMTCT through implementation REsearch (INSPIRE). J Acquir Immune Defic Syndr. 2014;67:S108–S113. Epub 2014/10/14 PubMed PMID: 25310115. [DOI] [PubMed] [Google Scholar]
- [44].Scott VE, Chopra M, Conrad L, et al. How equitable is the scaling up of HIV service provision in South Africa? S Afr Med J. 2005;95: 109–113. Epub 2005/ 03/09.PubMed PMID: 15751205. [PubMed] [Google Scholar]
- [45].Steketee RW, Eisele TP. Is the scale up of malaria intervention coverage also achieving equity? PLoS One. 2009;4:e8409 Epub 2009/ 12/23 PubMed PMID: 20027289; PubMed Central PMCID: PMCPMC2791860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Topp SM, Chipukuma JM, Chiko MM, et al. Integrating HIV treatment with primary care outpatient services: opportunities and challenges from a scaled-up model in Zambia. Health Policy Plan. 2013;28:347–357. Epub 2012/07/14 PubMed PMID: 22791556; PubMed Central PMCID: PMCPMC3697202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Victora CG, Barros FC, Assuncao MC, et al. Scaling up maternal nutrition programs to improve birth outcomes: a review of implementation issues. Food Nutr Bull. 2012;33: S6–26. PubMed PMID: 22913105. [DOI] [PubMed] [Google Scholar]
- [48].Wolkon A, Vanden Eng JL, Morgah K, et al. Rapid scale-up of long-lasting insecticide-treated bed nets through integration into the national immunization program during child health week in Togo, 2004. Am J Trop Med Hyg. 2010;83:1014–1019. Epub 2010/11/03 PubMed PMID: 21036829; PubMed Central PMCID: PMCPMC2963961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Kilima SP, Shayo EH, Msovela J, et al. The potential of involving traditional practitioners in the scaling up of male circumcision in the context of HIV prevention in Tanzania. Tanzan J Health Res. 2012;14:48–60; Epub 2012/01/01 PubMed PMID: 26591747. [DOI] [PubMed] [Google Scholar]
- [50].Ndlovu K, Littman-Quinn R, Park E, et al. Scaling up a mobile telemedicine solution in Botswana: keys to sustainability. Front Public Health. 2014;2:275 Epub 2015/01/08 PubMed PMID: 25566520; PubMed Central PMCID: PMCPMC4269123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Oyibo WA, Agomo CO. Scaling up of intermittent preventive treatment of malaria in pregnancy using sulphadoxine-pyrimethamine: prospects and challenges. Matern Child Health J. 2011;15:542–552. Epub 2010/ 04/29 PubMed PMID: 20425139. [DOI] [PubMed] [Google Scholar]
- [52].Schmidt WP, Cairncross S. Household water treatment in poor populations: is there enough evidence for scaling up now? Environ Sci Technol. 2009;43: 986–992. Epub 2009/ 03/27.PubMed PMID: 19320147. [DOI] [PubMed] [Google Scholar]
- [53].Csete J, Elliott R. Scaling up HIV testing: human rights and hidden costs. HIV AIDS Policy Law Rev. 2006;11: 1, 5–10. Epub 2006/ 06/30.PubMed PMID: 16805001. [PubMed] [Google Scholar]
- [54].Patel V, Bloch S. The ethical imperative to scale up health care services for people with severe mental disorders in low and middle income countries. Postgrad Med J. 2009;85:509–513. Epub 2009/ 10/01 PubMed PMID: 19789188. [DOI] [PubMed] [Google Scholar]
- [55].World Health Organization (WHO) UNAIDS/WHO policy statement on HIV testing. Geneva (Switzerland): WHO; 2004. [Google Scholar]
- [56].Curry L, Taylor L, Pallas SW, et al. Scaling up depot medroxyprogesterone acetate (DMPA): a systematic literature review illustrating the AIDED model. Reprod Health. 2013;10:39 Epub 2013/08/07 PubMed PMID: 23915274; PubMed Central PMCID: PMCPMC3737048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Ledikwe JH, Nyanga RO, Hagon J, et al. Scaling-up voluntary medical male circumcision - what have we learned? HIV AIDS (Auckl). 2014;6:139–146. Epub 2014/ 10/23 PubMed PMID: 25336991; PubMed Central PMCID: PMCPMC4199973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Meslin EM. The value of using top-down and bottom-up approaches for building trust and transparency in biobanking. Public Health Genomics. 2010;13:207–214. PubMed PMID: 20395689; PubMed Central PMCID: PMCPMC2865393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Milat AJ, Bauman A, Redman S. Narrative review of models and success factors for scaling up public health interventions. Implement Sci. 2015;10:113 Epub 2015/08/13. PubMed PMID: 26264351; PubMed Central PMCID: PMCPMC4533941 DOI: 10.1186/s13012-015-0301-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Perez-Escamilla R, Curry L, Minhas D, et al. Scaling up of breastfeeding promotion programs in low- and middle-income countries: the “breastfeeding gear” model. Advances in Nutrition (Bethesda, Md). 2012;3:790–800. Epub 2012/11/17 PubMed PMID: 23153733; PubMed Central PMCID: PMCPMC3648703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Chopra M, Rollins N. Infant feeding in the time of HIV: rapid assessment of infant feeding policy and programmes in four African countries scaling up prevention of mother to child transmission programmes. Arch Dis Child. 2008;93:288–291. Epub 2007/08/10 PubMed PMID: 17686796. [DOI] [PubMed] [Google Scholar]
- [62].Gupta A, Thorpe C, Bhattacharyya O, et al. Promoting development and uptake of health innovations: the nose to tail tool. F1000Res. 2016;5:361 Epub 2016/ 05/31 PubMed PMID: 27239275; PubMed Central PMCID: PMCPMC4863676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Hanson K, Ranson M, Oliveira-Cruz V, et al. Expanding access to priority health intervention: a framework for understanding the constraints to scaling-up. J Int Dev. 2003;15:1–14. [Google Scholar]
- [64].Ikpeazu A, Momah-Haruna A, Madu Mari B, et al. An appraisal of female sex work in Nigeria–implications for designing and scaling up HIV prevention programmes. PLoS One. 2014;9:e103619 Epub 2014/08/15 PubMed PMID: 25118691; PubMed Central PMCID: PMCPMC4131880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Yamey G. What are the barriers to scaling up health interventions in low and middle income countries? A qualitative study of academic leaders in implementation science. Global Health. 2012;8:11 Epub 2012/ 05/31 PubMed PMID: 22643120; PubMed Central PMCID: PMCPMC3514334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Yothasamut J, Putchong C, Sirisamutr T, et al. Scaling up cervical cancer screening in the midst of human papillomavirus vaccination advocacy in Thailand. BMC Health Serv Res. 2010;10:S5 Epub 2010/07/16 PubMed PMID: 20594371; PubMed Central PMCID: PMCPMC2895749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Freeman M, Savva N, Scholtes S. Economies of scale and scope in hospitals: an empirical study of volume spillovers. History. 2019. Available from: http://faculty.london.edu/nsavva/ScaleAndScope.pdf [Google Scholar]
- [68].Pallas SW, Minhas D, Perez-Escamilla R, et al. Community health workers in low- and middle-income countries: what do we know about scaling up and sustainability? Am J Public Health. 2013;103:e74–e82. Epub 2013/ 05/18 PubMed PMID: 23678926; PubMed Central PMCID: PMCPMC3682607. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Adamou B, Curran J, Wilson L, et al. Guide for monitoring scale-up of health practices and interventions. 2013. Available from: https://www.cpc.unc.edu/measure/prh
- France Légaré Canada research chair on shared decision making and knowledge translation, Quebec city, Canadan.d. [cited 2019 August21]. Available from: http://www.decision.chaire.fmed.ulaval.ca/accueil-en


