Abstract
Objective
to identify the predicting factors and sensitivity, specificity, positive and negative related value of nursing diagnosis Ineffective Breathing Pattern among patients of an intensive care unit.
Method
cross-sectional study. A logistic regression was fitted to assess the simultaneous effects of related factors.
Results
among the 120 patients, 67.5% presented Ineffective Breathing Pattern. In the univariate analysis, the related factors were: group of diseases, fatigue, obesity and presence of bronchial secretion, and the defining characteristics were: changes in respiratory depth, auscultation with adventitious sounds, dyspnea, reduced vesicular murmurs, tachypnea, cough and use of the accessory musculature to breathe. The mean age of patients with was higher than those without this diagnosis. The defining characteristics reduced murmurs had high sensitivity (92.6%), specificity (97.4%), negative related value (86.4%) and positive related value (98.7%). The related factors of Ineffective Breathing Pattern were the related factors fatigue, age and group of diseases.
Conclusion
fatigue, age and patients with a group of diseases were related factors of Ineffective Breathing Pattern in this study. Reduced vesicular murmurs, auscultation with adventitious sounds and cough may be defining characteristics to be added in the international classification, as well as the related factors bronchial secretion and group of diseases.
Keywords: Risk Factors; Signs and Symptoms; Nursing Diagnosis, Respiratory System; Classification; Nursing
Abstract
Objetivo
identificar os fatores preditores e a sensibilidade, especificidade, valores preditivos positivo e negativo do diagnóstico de enfermagem Padrão respiratório ineficaz em pacientes de uma unidade de terapia intensiva.
Método
estudo transversal. Foi realizada a regressão logística para avaliar os efeitos simultâneos dos fatores relacionados.
Resultados
dos 120 pacientes, 67,5% apresentaram padrão respiratório ineficaz. Na análise univariada, os fatores relacionados foram: grupo de doenças, fadiga, obesidade e a secreção nos brônquios, e as características definidoras foram: alteração na profundidade respiratória, ausculta com ruídos adventícios, dispneia, murmúrios vesiculares diminuídos, taquipneia, tosse e uso da musculatura acessória para respirar. A média de idade dos pacientes com este diagnóstico foi superior ao daqueles sem este diagnóstico. A característica definidora murmúrios vesiculares diminuídos teve alta sensibilidade (92,6%), especificidade (97,4%), valor preditivo negativo (86,4%) e valor preditivo positivo (98,7%). Os fatores relacionados de padrão respiratório ineficaz foram a fadiga, a idade e o grupo de doenças.
Conclusão
a fadiga, a idade e pacientes com grupo de doenças foram fatores preditores do diagnóstico padrão respiratório ineficaz neste estudo. Os murmúrios vesiculares diminuídos, a ausculta com ruídos adventícios e a tosse podem ser características definidoras a serem acrescentadas na classificação internacional, assim como os fatores relacionados secreção nos brônquios e grupo de doenças.
Keywords: Fatores de Risco, Sinais e Sintomas, Diagnóstico de Enfermagem, Sistema Respiratório, Classificação, Enfermagem
Abstract
Objetivo
identificar los factores predictores y la sensibilidad, especificidad, valores predictivos positivo y negativo del diagnóstico de enfermería padrón respiratorio ineficaz en pacientes de una unidad de terapia intensiva.
Método
estudio transversal. Se ajustó una regresión logística para evaluar los efectos simultáneos de factores relacionados.
Resultados
de los 120 pacientes, 67,5% presentaron padrón respiratorio ineficaz. En el análisis univariado, los factores relacionados que se asociaron con este diagnóstico fueron: grupo de enfermedades, fatiga, obesidad y la secreción en los bronquios y las características definitorias que se asociaron fueron alteración en la profundidad respiratoria, ausculta con ruidos adventicios, disnea, murmullo vesicular disminuido, taquipnea, tos y uso de la musculatura accesoria para respirar. El promedio de edad de los pacientes con padrón respiratorio ineficaz fue superior al de aquellos sin padrón respiratorio ineficaz. Las características definitorias redujeron los soplos con alta sensibilidad (92.6%), especificidad (97.4%), valor negativo relacionado (86.4%) y valor positivo relacionado (98.7%). Los factores relacionados con el patrón de respiración ineficaz fueron los factores relacionados con la fatiga, la edad y el grupo de enfermedades.
Conclusión
la fatiga, la edad y los pacientes con grupo de enfermedades relacionadas con el trauma, cardiocirculatorio y otros grupos de enfermedades fueron factores predictores del diagnóstico padrón respiratorio ineficaz en esta unidad. Los murmullos vesiculares disminuidos, la auscultación con ruidos adventicios y la tos pueden ser características definitorias a ser añadidas en la clasificación internacional, así como los factores relacionados de secreción en los bronquios y grupo de enfermedades.
Keywords: Factores de Riesgo, Signos y Síntomas, Diagnóstico de Enfermería, Sistema Respiratório, Clasificación, Enfermería
Introduction
The evaluation of the breathing pattern is essential to define nursing interventions and care plan to meet the patients’ needs. This evaluation is performed through a physical examination, monitoring the physiological functions of chest examination, palpation, pulmonary percussion and auscultation, which provide objective data on the use of respiratory muscles, respiratory rate and lung sounds1-2.
In normal conditions, the breathing pattern satisfies the need for oxygenation of the body. However, situations where there is fatigue, airway impairment due to secretion and decreased pulmonary expansion characterize the nursing diagnosis (ND) ineffective breathing pattern (IBP)3.
The ND ineffective breathing pattern (IBP) was first defined in 1980 and revised in 1996, 1998, 2010 and 2017. In 2017, this diagnosis was modified and included associated conditions. This diagnosis focuses on problem and belongs to domain 4, class 4, activity/rest of the NANDA International, Inc. (NANDA-I). IBP is defined as an inspiration and/or expiration pattern that does not provide sufficient ventilation4.
This diagnosis has often been identified in adult individuals and in several units. In trauma patients treated at an university hospital in the city of São Paulo, Brazil, it was observed that 82.4% presented IBP5 and 85.7% in adults who receive care in emergency rooms6. In adult patients with heart disease, it was observed that this diagnosis was present in 70.6% and that 100.0% of them presented fatigue as a related factor (RF) and dyspnea as a defining characteristic (DC)7.
The first American survey identified the Nursing Diagnosis IBP in 81.0% of intensive care patients8. In the city of Rio Branco, Acre (AC), Brazil, a prevalence of 64.4% of IBP was identified in an Intensive Care Unit (ICU) patients9 however, these studies evaluated only the prevalence, did not identify the measures of accuracy and also did not evaluate the predicting factors of the IBP nursing diagnosis. Thus, it is observed that the nursing diagnosis IBP is very frequent in ICUs. Due to the importance of early identification and the establishment of a care plan for these patients, the objective of the present study was to identify the predicting factors and sensitivity, specificity, positive and negative related value of nursing diagnosis Ineffective Breathing Pattern among patients of an intensive care unit.
Method
This is an observational, cross-sectional, analytical study. The research was performed at the ICU of the Urgency and Emergency Hospital of the city of Rio Branco, AC, Brazil, from September 2015 to April 2016. The sample size was calculated by the formula for finite populations, using a 95% confidence coefficient; a random error of 5%; IBP prevalence of 64.4%, according to a study carried out at an ICU of the city of Rio Branco9, and the population of 180 individuals, according to the number of conscious and oriented patients hospitalized at this unit, over a period of one year. This profile of patients considered the need to perform the manovacuometry test. Thus, the sample size was 109 patients. Considering a 10% probability of loss, data were collected from 120 patients.
The inclusion criteria were: adult patients over 18 years of age, conscious and oriented, without neuromuscular disease identified by the medical and nurse evaluation and recorded in the medical record, with spontaneous breathing, which accepted and were able to undergo the manovacuometry test. Patients with hemodynamic instability that could interfere with the manovacuometry test were excluded10-11.
The independent study variables (DC, RF and associated conditions) were identified in the NANDA-I, classification for the Nursing diagnosis IBP4 and in a literature review (age, smoking, group of diseases, bronchial secretion, cough, reduce vesicular murmurs and auscultation with adventitious sounds)12. These selected variables were evaluated only by the main investigator of the study through interviews and physical examinations in the patients’ bed, according to the conceptual and operational definition of each variable, in which some were previously validated13-15and others were adapted for the adult population, such as assumption of three-point position to breathe, bradypnea/tachypnea values. The conceptual and operational definitions of the variables that have not been validated in other studies were elaborated by the researchers, according to the literature2,16-21.
All DC and RF were categorized as present or absent only by the main investigator, except for the group of diseases that were categorized according to the group diagnosed by the physician. The main groups of diseases identified were trauma (wound caused by gunshot and melee weapon, femur fracture and traumatic brain injury); cardiocirculatory diseases (acute myocardial infarction, atrioventricular block and ischemic or hemorrhagic stroke); diseases of the respiratory system (acute pulmonary edema and pneumonia); and other groups of diseases (acute abdomen, sepsis, snakebite, drowning, convulsion, exogenous intoxication, exploratory laparotomy, systemic lupus erythematosus, leptospirosis, pancreatitis and pregnancy-specific hypertension).
The defining characteristics of IBP evaluated were: changes in respiratory depth when assuming a three-point position to breathe, nose wing beats, bradypnea, increased anteroposterior chest diameter, decreased inspiratory pressure, decreased expiratory pressure, dyspnea, altered chest excursion, prolonged expiratory phase, orthopnea, abnormal breathing pattern, pursed-lip breathing, tachypnea, use of accessory muscles to breathe, decreased minute ventilation, cough12, auscultation with adventitious sounds12, and reduced vesicular murmurs4,12.
The related factors of IBP evaluated were: anxiety, pain, fatigue, respiratory muscle fatigue, hyperventilation, obesity, position of the body that prevents lung expansion, and bronchial secretion4,12. The RF age, smoking and a group of diseases were also included12.
The associated conditions of IBP evaluated were: chest wall deformity, bone deformity, musculoskeletal damage and hypoventilation syndrome4The associated conditions neurological damage, neurological immaturity, spinal cord injury and neuromuscular dysfunction were excluded because in these situations’ patients could not undergo the manovacuometry and the impossibility to perform this test was an exclusion criterion in the present study. The DC decreased vital capacity was not evaluated because there was no ventilator or spirometer in the unit, hindering the evaluation of the maximum percentage level of exhaled gas after maximal inspiration. These were limiting factor of the study. The outcome variable (dependent) studied was the presence of the nursing diagnosis IBP, defined as “inspiration and/or expiration that does not provide adequate ventilation”4. To have this diagnosis, patients should have three or more DC and maximal inspiratory pressure less than 80 cmH2O for men and less than 60 cmH2O for women22. The maximum inspiratory pressure was obtained through manovacuometry10 and is a simple way to measure maximum respiratory pressures, and a quantitative measure of respiratory muscle function and strength, which indicates if ventilation is adequate.
The DC decreased inspiratory pressure evaluated by the manovacuometer was chosen to confirm the presence of IBP because a study conducted in 2015 and 2016 with 626 adult ICU patients showed that this DC and the RF fatigue were the ones that had the greatest sensitivity for the IBP diagnosis in these patients23.
The nurse responsible for this research collected the data with aid of a standardized collection instrument prepared for this purpose. Collection was performed every day in the morning with patients who met the inclusion criteria in the ICU. After the data collection, the patients presenting and not presenting the IBP nursing diagnosis were compared to the causality of IBP nursing diagnosis.
For manovacuometry, the subjects were evaluated in the seated position (90º), using a nasal clip and semi-rigid rubber, diver type, with a internal hole of 2 mm diameter, in which the patient was asked to seal his lips firmly around the mouthpiece. In order to measure the maximal inspiratory pressure (MIP), the patient was asked to exhale, and at that moment the researcher occluded the orifice of the device and then the patient made a maximal inspiratory effort against the occluded airway, which was recorded on the manovacuometer. Patients would maintain the inspiratory pressure for at least 1.5 seconds and the highest sustained negative pressure was recorded. This same process was repeated three times, with one-minute intervals in each evaluation, and only the highest value was used11. It is emphasized that if differences of values greater than 10% were obtained between measurements, they were discarded.
The manovacuometer used was for single-use, of analog type, Wika manufacturer, model 611.10.063L, +120/-120, calibrated according to the internal procedure PRP-04-re.13, from NBR-ISO-10012, part 1. After the evaluation, the patients were allocated into two groups, with and without IBP.
This project was submitted to the Research Ethics Committee (REC) of the Federal University of São Paulo (UNIFESP) and approved under Opinion no 1,290,590, CAAE: 39185814.9.0000.5505, 21/10/2015. This research followed the guidelines of the Resolution of the National Council of Ethics in Research (CONEP) nº 466/2012, of the National Health Council (NHC) of Brazil and all the patients who were interviewed were informed and signed an Informed Consent Term authorizing the research.
Data were analyzed using the Statistical Package for Social Sciences (SPSS), Microsoft Office, University of Chicago, version 20.0. An initial descriptive analysis of the data was performed. Absolute and relative frequencies were used for the categorical variables and summary measures (mean, quartiles, minimum, maximum, and standard deviation) were used for the numerical variables.
The association between two categorical variables was verified using the Chi-square test, or the Fisher’s exact test in cases of small samples. When differences were observed in the distributions, standardized adjusted residues were used to identify local differences. Comparison of means between two groups was performed using Student’s t-test for independent samples.
For all defining characteristics and related factors of dichotomous nature, accuracy measurements were presented through sensitivity, specificity, positive related value (PPV) and negative related value (NPV). Logistic regressions were fitted to evaluate the simultaneous effects of RF on the presence of IBP. Due to the large number of variables that predicted the size of the sample, the variables whose associations with the dependent variable were significant at 20% in the univariate analysis were selected for the initial models. Then the non-significant variables at 5% were excluded one by one in order of significance (backward method).
The Hosmer and Lemes how test was used to analyze the goodness of fit of the final model, considering the RF as related variables. Sensitivity and specificity were calculated based on the ROC curve, which allowed the definition of a cutoff point in the probabilities of occurrence of IBP estimated from the adjusted final regression model. A significance level of 5% was used for all statistical tests.
Results
From the 120 patients in the sample, 30.0% were elderly, with a mean age of 47 years, 60.8% were males, 59.2% were brown and 61.7% had primary schooling. The main groups of diseases identified were trauma (wound caused by gunshot and melee weapon, femur fracture and traumatic brain injury); cardiocirculatory diseases (acute myocardial infarction, atrioventricular block and ischemic or hemorrhagic stroke); diseases of the respiratory system (acute pulmonary edema and pneumonia); and other groups of diseases (acute abdomen, sepsis, snakebite, drowning, convulsion, exogenous intoxication, exploratory laparotomy, systemic lupus erythematosus, leptospirosis, pancreatitis and pregnancy-specific hypertension).
Among the evaluated patients, 67.5% presented the nursing diagnosis IBP. The Table 1 shows that IBP was associated with the following DC: changes in respiratory depth, auscultation with adventitious sounds, dyspnea, reduced vesicular murmurs, tachypnea, cough and use of accessory muscles to breathe. It was noted that 100% of the patients with these DC, except reduced vesicular murmurs, presented IBP.
Table 1. Defining characteristics according to the presence or absence of the Nursing diagnosis Ineffective Breathing Pattern. Rio Branco, AC, Brazil, 2015-2016.
| Ineffective Breathing Pattern | Total | ODDS RATIO | p-value* | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Absent | Present | |||||||
|
| ||||||||
| n | % | n | % | n | % | |||
| Changes in respiratory depth | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | <0.001* | |
| Absent | 39 | 44.8% | 48 | 55.2% | 87 | 100.0% | 1.00 | |
| Present | 0 | 0.0% | 33 | 100.0% | 33 | 100.0% | (1)† | |
| Auscultation with adventitious sounds | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | <0.001* | |
| Absent | 39 | 62.9% | 23 | 37.1% | 62 | 100.0% | 1.00 | |
| Present | 0 | 0.0% | 58 | 100.0% | 58 | 100.0% | (1)† | |
| Nose wing beats | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | 0.172‡ | |
| Absent | 39 | 33.9% | 76 | 66.1% | 115 | 100.0% | 1.00 | |
| Present | 0 | 0.0% | 5 | 100.0% | 5 | 100.0% | (1)† | |
| Bradypnea | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | - | |
| Absent | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | - | |
| Increased anteroposterior chest diameter | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | 0.172‡ | |
| Absent | 39 | 33.9% | 76 | 66.1% | 115 | 100.0% | 1.00 | |
| Present | 0 | 0.0% | 5 | 100.0% | 5 | 100.0% | (1)† | |
| Dyspnea | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | <0.001* | |
| Absent | 39 | 41.9% | 54 | 58.1% | 93 | 100.0% | 1.00 | |
| Present | 0 | 0.0% | 27 | 100.0% | 27 | 100.0% | (1)† | |
| Altered chest excursion | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | 0.052‡ | |
| Absent | 39 | 34.8% | 73 | 65.2% | 112 | 100.0% | 1.00 | |
| Present | 0 | 0.0% | 8 | 100.0% | 8 | 100.0% | (1)† | |
| Abnormal breathing pattern | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | 0.328‡ | |
| Absent | 3 | 60.0% | 2 | 40.0% | 5 | 100.0% | 1.00 | |
| Present | 36 | 31.3% | 79 | 68.7% | 115 | 100.0% | 3.29 | |
| Prolonged expiratory phase | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | 1.000‡ | |
| Absent | 39 | 32.8% | 80 | 67.2% | 119 | 100.0% | 1.00 | |
| Present | 0 | 0.0% | 1 | 100.0% | 1 | 100.0% | (1)† | |
| Pursed-lip breathing | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | 1.000‡ | |
| Absent | 39 | 33.1% | 79 | 66.9% | 118 | 100.0% | 1.00 | |
| Present | 0 | 0.0% | 2 | 100.0% | 2 | 100.0% | (1)† | |
| Reduced vesicular murmurs | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | <0.001* | |
| Absent | 38 | 86.4% | 6 | 13.6% | 44 | 100.0% | 1.00 | |
| Present | 1 | 1.3% | 75 | 98.7% | 76 | 100.0% | 475.00 | |
| Orthopnea | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | 1.000‡ | |
| Absent | 39 | 32.8% | 80 | 67.2% | 119 | 100.0% | 1.00 | |
| Present | 0 | 0.0% | 1 | 100.0% | 1 | 100.0% | (1)† | |
| Decreased expiratory pressure | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | - | |
| Present | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | - | |
| Decreased inspiratory pressure | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | 0.325‡ | |
| Absent | 1 | 100.0% | 0 | 0.0% | 1 | 100.0% | (2)§ | |
| Present | 38 | 31.9% | 81 | 68.1% | 119 | 100.0% | ||
| Assumption of a three-point position | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | 0.172‡ | |
| Absent | 39 | 33.9% | 76 | 66.1% | 115 | 100.0% | 1.00 | |
| Present | 0 | 0.0% | 5 | 100.0% | 5 | 100.0% | (1)† | |
| Tachypnea | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | <0.001* | |
| Absent | 39 | 40.2% | 58 | 59.8% | 97 | 100.0% | 1.00 | |
| Present | 0 | 0.0% | 23 | 100.0% | 23 | 100.0% | (1)† | |
| Cough | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | 0.001* | |
| Absent | 39 | 40.6% | 57 | 59.4% | 96 | 100.0% | 1.00 | |
| Present | 0 | 0.0% | 24 | 100.0% | 24 | 100.0% | (1)† | |
| Use of accessory muscles to breathe | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | <0.001* | |
| Absent | 39 | 39.0% | 61 | 61.0% | 100 | 100.0% | 1.00 | |
| Present | 0 | 0.0% | 20 | 100.0% | 20 | 100.0% | (1)† | |
| Decreased minute ventilation | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | 1.000‡ | |
| Absent | 39 | 33.1% | 79 | 66.9% | 118 | 100.0% | 1.00 | |
| Present | 0 | 0.0% | 2 | 100.0% | 2 | 100.0% | (1)† | |
*p-value = descriptive level of Chi-Square; †(1) OR not presented = absence of negative IBP cases in the presence of the defining characteristic; ‡Fisher’s exact test; §(2) OR not presented = absence of positive IBP cases in the absence of the defining characteristic
Table 2 shows the sensitivity, specificity and positive and negative related values of DC of patients with IBP. It is notable that only the defining characteristic reduced vesicular murmurs showed high sensitivity (92.6%), high specificity (97.4%) and PPV and NPV above 86%. Auscultation with adventitious sounds also showed high sensitivity (71.6%), specificity (100.0%) and PPV (100.0%), but moderate NPV (62.9%). The other characteristics, except abnormal breathing pattern and decreased inspiratory pressure, presented high specificity, but low sensitivity. An inverse pattern was observed for abnormal breathing pattern and maximal inspiratory pressure.
Table 2. Sensitivity, specificity and positive and negative related values of the defining characteristics of Ineffective Breathing Pattern. Rio Branco, AC, Brazil, 2015-2016.
| Defining characteristics | Sensitivity (%) | Specificity (%) | Related value (%) | |
|---|---|---|---|---|
|
| ||||
| Positive | Negative | |||
| Reduced vesicular murmurs | 92.6 (84.6 - 97.2) | 97.4 (86.5 - 99.9) | 98.7 (92.9-100.0) | 86.4 (72.6 - 94.8) |
| Auscultation with adventitious sounds | 71.6 (60.5 - 81.1) | 100.0 (91.0 - 100.0) | 100 (93.8-100.0) | 62.9 (49.7 - 74.8) |
| Abnormal breathing pattern | 97.5 (91.4 - 99.7) | 7.7 (1.6 - 20.9) | 68.7 (59.4-77.0) | 60.0 (14.7 - 94.7) |
| Decreased inspiratory pressure | 100.0 (95.5- 100) | 2.6 (0.1 - 13.5) | 68.1 (58.9-76.3) | 100.0 (2.5-100.0) |
| Decreased expiratory pressure | 100.0 (-)* | 0.0 (-)* | 67.5 (-) | - |
| Changes in respiratory depth | 40.7 (29.9 - 52.2) | 100.0 (91.0 - 100.0) | 100 (89.4 -100.0) | 44.8 (34.1 - 55.9) |
| Dyspnea | 33.3 (23.2 - 44.7) | 100.0 (91.0 - 100.0) | 100.0 (87.2-100.0) | 41.9 (31.8 - 52.6) |
| Cough | 29.6 (20.0 - 40.8) | 100.0 (91.0 - 100.0) | 100 (85.8 - 100.0) | 40.6 (30.7 - 51.1) |
| Tachypnea | 28.4 (18.9 - 39.5) | 100.0 (91.0 - 100.0) | 100.0 (85.2-100.0) | 40.2 (30.4 - 50.7) |
| Use of accessory muscles to breathe | 24.7 (15.8 - 35.5) | 100.0 (91.0 - 100.0) | 100.0 (83.2-100.0) | 39.0 (29.4 - 49.3) |
| Altered chest excursion | 9.9 (4.4 - 18.5) | 100.0 (91.0 - 100.0) | 100.0 (63.1-100.0) | 34.8 (26.1 - 44.4) |
| Increased anteroposterior chest diameter | 6.2 (2.0 - 13.8) | 100.0 (91.0 - 100.0) | 100.0 (47.8-100.0) | 33.9 (25.3 - 43.3) |
| Nose wing beats | 6.2 (2.0 - 13.8) | 100.0 (91.0 - 100.0) | 100.0 (47.8-100.0) | 33.9 (25.3 - 43.3) |
| Assumption of a three-point position | 6.2 (2.0 - 13.8) | 100.0 (91.0 - 100.0) | 100.0 (47.8-100.0) | 33.9 (25.3 - 43.3) |
| Decreased minute ventilation | 2.5 (0.3 - 8.6) | 100.0 (91.0 - 100.0) | 100.0 (15.8-100.0) | 33.1 (24.7 - 42.3) |
| Pursed-lip breathing | 2.5 (0.3 - 8.6) | 100.0 (91.0 - 100.0) | 100.0 (15.8-100.0) | 33.1 (24.7 - 42.3) |
| Orthopnea | 1.2 (0.0 - 6.7) | 100.0 (91.0 - 100.0) | 100.0 (2.5 - 100.0) | 32.8 (24.4 - 42.0) |
| Prolonged expiratory phase | 1.2 (0.0 - 6.7) | 100.0 (91.0 - 100.0) | 100.0 (2.5 - 100.0) | 32.8 (24.4 - 42.0) |
| Bradypnea | 0.0 (-)* | 100.0 (-)* | - | 32.5 (-)* |
*(-) = it was not possible to calculate because the defining characteristic did not present one of the levels
Table 3 shows the RF of the nursing diagnosis IBP in both groups, with and without the IBP nursing diagnosis. The RF that were associated with IBP were group of diseases, fatigue, obesity and bronchial secretion. Thus, patients with fatigue, obesity and bronchial secretion had higher percentages of IBP compared to those without these conditions. On the other hand, patients diagnosed with cardiocirculatory and respiratory diseases and other groups of diseases presented lower percentages of IBP in comparison to those diagnosed with trauma. The mean age of patients with IBP was higher than those without IBP. The related conditions musculoskeletal damage, chest wall deformity, bone deformity and hypoventilation syndrome were presented in 67.5% of the patients and, not be statistically significant between the groups (p-value>0.05).
Table 3. Related factors according to presence or absence of the Nursing Diagnosis Ineffective Breathing Pattern. Rio Branco, AC, Brazil, 2015-2016.
| Ineffective Breathing Pattern | Total | ODDS RATIO | p-value | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Absent | Present | |||||||
|
| ||||||||
| n | % | n | % | N | % | |||
| Anxiety | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | 0.272* | |
| Absent | 38 | 33.9% | 74 | 66.1% | 112 | 100.0% | 1.00 | |
| Present | 1 | 12.5% | 7 | 87.5% | 8 | 100.0% | 3.59 | |
| Group of diseases | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | 0.008† | |
| Trauma | 6 | 16.7% | 30 | 83.3% | 36 | 100.0% | 1.00 | |
| Cardiocirculatory | 13 | 37.1% | 22 | 62.9% | 35 | 100.0% | 0.34 | |
| Respiratory | 5 | 22.7% | 17 | 77.3% | 22 | 100.0% | 0.68 | |
| Others | 15 | 55.6% | 12 | 44.4% | 27 | 100.0% | 0.16 | |
| Pain | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | 0.058* | |
| Absent | 38 | 35.5% | 69 | 64.5% | 107 | 100.0% | 1.00 | |
| Present | 1 | 7.7% | 12 | 92.3% | 13 | 100.0% | 6.61 | |
| Fatigue | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | <0.001† | |
| Absent | 38 | 48.7% | 40 | 51.3% | 78 | 100.0% | 1.00 | |
| Present | 1 | 2.4% | 41 | 97.6% | 42 | 100.0% | 38.95 | |
| Respiratory muscle fatigue | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | 1.000* | |
| Absent | 39 | 33.1% | 79 | 66.9% | 118 | 100.0% | 1.00 | |
| Present | 0 | 0.0% | 2 | 100.0% | 2 | 100.0% | (1)† | |
| Hyperventilation | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | 0.172* | |
| Absent | 39 | 33.9% | 76 | 66.1% | 115 | 100.0% | 1.00 | |
| Present | 0 | 0.0% | 5 | 100.0% | 5 | 100.0% | (1)† | |
| Obesity | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | 0.019* | |
| Absent | 35 | 38.0% | 57 | 62.0% | 92 | 100.0% | 1.00 | |
| Present | 4 | 14.3% | 24 | 85.7% | 28 | 100.0% | 3.68 | |
| Position of the body that prevents lung expansion | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | 0.550* | |
| Absent | 39 | 33.3% | 78 | 66.7% | 117 | 100.0% | 1.00 | |
| Present | 0 | 0.0% | 3 | 100.0% | 3 | 100.0% | (1)† | |
| Bronchial secretion | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | 0.016* | |
| Absent | 39 | 35.8% | 70 | 64.2% | 109 | 100.0% | 1.00 | |
| Present | 0 | 0.0% | 11 | 100.0% | 11 | 100.0% | (1)† | |
| Smoking | 39 | 32.5% | 81 | 67.5% | 120 | 100.0% | 0.155* | |
| No | 27 | 38.0% | 44 | 62.0% | 71 | 100.0% | 1.00 | |
| Yes | 8 | 32.0% | 17 | 68.0% | 25 | 100.0% | 1.30 | |
| Ex-smoker | 4 | 16.7% | 20 | 83.3% | 24 | 100.0% | 3.07 | |
*p-value = descriptive level of Fisher’s exact test or Chi-Square; †(1) OR not presented = absence of negative Ineffective Breathing Pattern cases in the presence of the related factor
Table 4 shows the related univariate and multivariate logistic regression models. Patients with fatigue were observed to present a chance of having IBP 61.96 times greater than those without fatigue. On the other hand, it was observed that patients with cardiocirculatory diseases and with other types of diseases were, respectively, 93% and 85% less likely to have IBP than those diagnosed with trauma. It was also noted that with the increase of one year of age, the chance of IBP increases by 6%.
Table 4. Final related univariate and multivariate logistic regression models. Rio Branco, AC, Brazil, 2015-2016.
| Univariate model | Final multivariate model | |||
|---|---|---|---|---|
|
| ||||
| Gross Odds Ratio (95%) | p-value* | Adjusted Odds Ratio (95%) | p-value* | |
| Anxiety | 3.59 (0.43- 30.29) | 0.239 | - | - |
| Chest wall deformity | (1)† | 0.999 | - | - |
| Bone deformity | (2)‡ | - | - | - |
| Pain | 6.61 (0.83- 52.8) | 0.075 | - | - |
| Fatigue | 38.95 (5.10- 297.4) | <0.001 | 61.96 (6.88- 557.74) | <0.001 |
| Respiratory muscle fatigue | (1)† | 0.999 | - | - |
| Hyperventilation | (1)† | 0.999 | - | - |
| Obesity | 3.68 (1.18- 11.51) | 0.025 | 2.76 (0.64- 11.84) | 0.171 |
| Position of the body that prevents lung expansion | (1)† | 0.999 | - | - |
| Musculoskeletal damage | 3.04 (0.35- 26.17) | 0.311 | - | - |
| Hypoventilation syndrome | (1)† | 1.000 | - | - |
| Bronchial secretion | (1)† | 0.999 | - | - |
| Age (years) | 1.03 (1.01- 1.05) | 0.009 | 1.06 (1.02- 1.09) | 0.001 |
| Smoking (ref. = no) | 0.172 | |||
| Yes | 1.30 (0.5- 3.43) | 0.591 | ||
| Ex-smoker | 3.07 (0.95- 9.94) | 0.062 | ||
| Medical diagnosis (ref. = trauma) | 0.011 | 0.013 | ||
| Cardiocirculatory | 0.34 (0.11- 1.03) | 0.056 | 0.07 (0.01- 0.38) | 0.002 |
| Respiratory | 0.68 (0.18- 2.56) | 0.569 | 0.23 (0.04- 1.30) | 0.096 |
| Others | 0.16 (0.05- 0.51) | 0.002 | 0.15 (0.04- 0.62) | 0.009 |
*Hosmer and Leme show test for goodness of fit of the model (p = 0.649); †(1) = absence of negative Ineffective Breathing Pattern cases in the presence of the related factor; ‡(2) = absence of one of the levels of the related factor
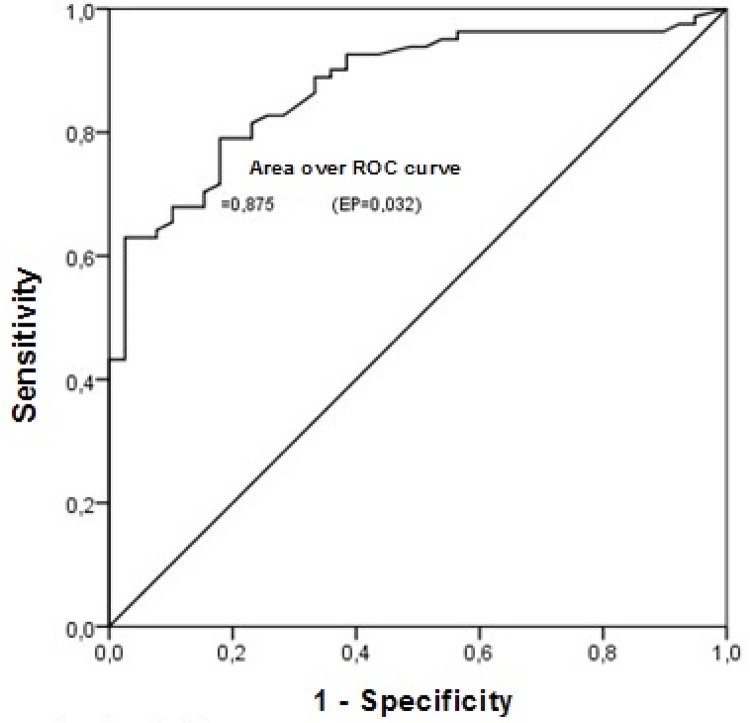
The final model, given the information of the related factors, allows to estimate the probability of a patient to present IBP. Using the ROC curve, a good related capacity of the probabilities of occurrence of IBP estimated by the final model (area under the ROC curve 0.875) with high sensitivity (82.72%) and specificity (74.36%) is observed (Figure 1).
Figure 1. ROC curve for Ineffective Breathing Pattern. Rio Branco, AC, Brazil, 2015-2016.
Discussion
The related factors of the nursing diagnosis IBP in the studied ICU were fatigue, age, and group of diseases (cardiocirculatory diseases, trauma and other diagnoses). The development of fatigue is an important and common complication in many patients admitted to ICUs and its incidence may range from 30% to 60% in these patients11,24. Fatigue has been investigated in many studies because of its high prevalence and the damage caused to the patients’ quality of life18,25-27. Besides previous co-morbidities, several factors may contribute to fatigue, including systemic inflammation, use of some medications such as corticoids, sedatives and neuromuscular blockers, malnutrition, hyperosmolarity, parenteral nutrition, cardiopathies and prolonged immobility, common conditions in the ICU25-26. Fatigue can be present in patients with diverse pathologies, such as heart, lung, hematological, and oncological diseases, as well as in patients presenting pain, malnutrition and psychological manifestations such as anxiety and depression, which also corroborates the other RF found in this study, that is, group of diseases27.
Other factors that may contribute to the onset of fatigue are age and number of comorbidities17. Regarding the number of morbidities, studies have shown an association between greater number of morbidities and greater perception of fatigue28-29. In the elderly, fatigue occurs due to changes in the body as a whole and in the cardiopulmonary system, in which reduction of oxygen uptake, reduction of respiratory muscle strength, and increase of vascular resistance are observed. In the muscular system, there is a decrease in muscle strength and flexibility, resulting in fatigue, which affects simple activities of daily life of the elderly30.
A recent study, also performed in an ICU in the city of Ribeirão Preto, SP, Brazil, with 626 adult patients, showed that the RF fatigue presented greater sensitivity for the IBP diagnosis23. The authors emphasize that IBP patients present DC related to ventilatory dysfunction and, if not treated adequately, this diagnosis may evolve to the diagnosis of impaired spontaneous ventilation (ISV), characterizing a worse prognosis of the patient23.
Old age was the second predictor of IBP in this study. Ageing is characterized by a chronic decrease in the functions of the organic system, leaving the elderly susceptible to diseases, with risk to trigger the IBP diagnosis2. Ageing leads to physiological changes such as compromised gas exchange efficiency, reduced pulmonary compliance, decreased respiratory muscle strength, and decreased oxygen transport to tissues, resulting in decreased cardiac output, body mass, alveolar volume and ventilation/perfusion ratio, which may lead to the emergence of the Nursing diagnosis IBP20.
In this sense, it is up to nurses to recognize these peculiarities and alterations during the physical examination and to select interventions that improve the respiratory state within the expected for the age. A cross-sectional study conducted in Rio Grande do Sul, Brazil, identified that almost half of the elderly (42.0%) had IBP31. In this study, 86.7% of elderly patients presented IBP. It is also worth mentioning that this group of patients is more vulnerable to influenza due to the higher prevalence of chronic degenerative diseases and immunological deterioration, which may cause breathing changes and the manifestation of IBP31-34.
The third related factor of IBP was group of diseases (trauma, cardiocirculatory diseases, and other diagnoses). External causes, as an important cause of traumas, represented by traffic accidents, represent a serious public health problem in Brazil and are responsible for high morbidity and mortality, disability rates, and sequelae, not to mention considerable economic cost35. A study that analyzed 406 trauma victims in the city of São Paulo, SP, Brazil, identified a prevalence of 82.8% of patients with IBP5.
Another study performed in the urgency and emergency unit of a large public hospital in southern Brazil identified a prevalence of 51.2% of IBP in patients who had been victims of multiple traumas, the main ones being pain, skeletal muscle damage, hyperventilation and neuromuscular dysfunction, and the main DC was tachypnea and bradypnea36. The presence of these clinical indicators occurs due to the changes in pulmonary expansion following the alteration of the chest cavity, besides hypovolemia following hemorrhage and hypoxia caused by traumatic lesions. Thus, the control of cerebral oxygenation and the supply of oxygen to the other organs of the body are fundamental in the care of these patients, besides the control of bleeding. The lack of attention to respiratory care may lead patients to develop IBP36-37.
In relation to the group of diseases related to the cardiocirculatory system, it is known that patients with these comorbidities may present cardiac decompensation with consequent hemodynamic changes, giving rise to the IBP diagnosis. Patients with left heart failure, for example, may present signs and symptoms of pulmonary congestion due to left ventricular failure, evidencing the nursing diagnosis IBP. Moreover, patients with acute coronary syndrome have chest pain as their main symptom. Anginal pain triggers manifestations of the sympathetic system that cause an increase in heart rate and breathing, altering the breathing mechanics regarding depth, number of incursions per minute. Without intervention, this will lead to respiratory muscle fatigue and consequent IBP diagnosis17.
Thus, in the analysis of the final logistic regression model of the related factors of IBP, the curve presented a good related capacity of the probability of occurrence of IBP (ROC curve 0.875), with high sensitivity and specificity to identify this nursing diagnosis.
Other related factors (obesity and bronchial secretion), although not identified as predictors of IBP in our study, have been also associated with this diagnosis. It was also observed that the DC changes in respiratory depth, auscultation with adventitious sounds, dyspnea, reduced vesicular murmurs, tachypnea, cough and use of accessory respiratory muscles were also associated with IBP12-14,19.
In obese individuals, IBP diagnosis is detected by the reduced lung volume and capacity in these patients. Excessive adipose tissue also causes mechanical compression of the diaphragm, resulting in restrictive respiratory insufficiency, decreased pulmonary compliance and increased pulmonary resistance, which consequently increases respiratory work and oxygen, resulting in the IBP diagnosis38-39.
The RF bronchial secretion possibly related to the Nursing diagnosis IBP due to the narrowing of the lumen as consequence of the exacerbated production of secretions and also due to the inability of intensive care patients to expel secretions spontaneously from the respiratory tract, leading to respiratory difficulty and to the IBP diagnosis12.
The DC dyspnea, tachypnea, changes in respiratory depth and use of accessory muscles to breathe are very common alterations among patients with IBP. This is due to respiratory muscle weakness and non-resolution of the underlying problem that led in the first place to respiratory decompensation. Tachypnea is the result of pulmonary hyperventilation, which develops as an adaptive compensation attempt18. The failure of this compensatory mechanism and the imbalance between the demand and the supply of oxygen favor the appearance of the IBP diagnosis40-41. The use of the accessory musculature demonstrates the attempt to re-establish a normal breathing pattern. A study carried out in the city of Fortaleza, CE, Brazil, identified that the use of the accessory musculature brings a seven-fold higher chance of having the IBP diagnosis15.
Cough is a symptom of a wide variety of pulmonary and extra-pulmonary diseases, and is very prevalent in the population, has a negative social impact, non-tolerated at work and family contexts, besides generating a great cost in terms of exams and medications. The major causes of cough are viral infections of the upper airways (common cold), lower airways (acute tracheobronchitis), acute sinusitis, exposure to allergens and irritants, and exacerbations of chronic diseases such as asthma, chronic obstructive pulmonary disease (COPD) and rhinosinusitis42, which can cause changes in pulmonary ventilation, leading the individual to present the IBP diagnosis. A cross-sectional study carried out in Fortaleza, CE, Brazil, showed that the IBP diagnosis was the most prevalent and the most common DC were adventitious respiratory sounds and cough43. Adventitious respiratory sounds are detected in pulmonary auscultation and are common in patients with respiratory changes in ICUs12.
When assessing the specificity, sensitivity and positive and negative related values of DC and RF, it was observed that the DC reduced vesicular murmurs had an association and an excellent measure of accuracy, presenting sensitivity, specificity, positive related value and negative high values for the nursing diagnosis IBP.
Despite its importance, the DC reduced vesicular murmurs is not part of the NANDA-I classification for this nursing diagnosis. Vesicular murmurs are normal sounds auscultated in the lungs and their decrease is pathological and may indicate the presence of atelectasis and even decreased lung expansion44. Atelectasis is a respiratory complication caused by the obstruction of a bronchus, or lung, by secretion or solid bodies that prevent the flow of air and lead to a decrease in the number of alveoli worked44. When there is complete obstruction in a bronchus that supplies air to a normally ventilated region of the lung parenchyma, the gas in the alveoli distal to the obstruction is absorbed into the pulmonary circulation. Once all the alveolar gas is absorbed into the circulation, the alveoli, now without gas, collapse, generating a decrease in vesicular murmurs and causing changes in the respiratory ventilation and ineffective breathing pattern44.
The results of this study showed that there are related factors for the nursing diagnosis IBP and nursing interventions and early targeting should be performed in the case of patients with fatigue, advanced age, with problems such as trauma, cardiocirculatory diseases and other diseases.
As a positive factor, this research used a large sample of critical patients, an objective measurement, manovacuometry, and contributed with new DC and RF for the Nursing diagnosis IBP, which will provide the improvement of the NANDA International, Inc. classification of nursing diagnoses, making it possible a more accurate nursing education, besides bringing evidence to the clinical practice of diagnosing in nursing.
Conclusion
Related factors of IBP were fatigue, old age, trauma, cardiocirculatory diseases and other diseases. When analyzing the final model through the ROC curve, it was observed that the model had a good related capacity for IBP, associated to high specificity and sensitivity. The DC reduced murmurs presented high sensitivity, specificity and related and negative values for IBP, demonstrating its importance in the identification of this nursing diagnosis.
Acknowledgments
To the employees of the Intensive Care Unit of the Hospital of Emergency and Emergency of Rio Branco for the assistance and availability in its unit to carry out this research.
Footnotes
Paper extracted from doctoral dissertation “Predictive factors of the nursing diagnosis ineffective breathing pattern in an intensive care unit”, presented to Universidade Federal de São Paulo, Escola Paulista de Enfermagem, São Paulo, SP, Brazil.
Referências
- 1.Sarkar M, Madabhavi I, Niranjan N, Dogra M. Auscultation of the respiratory system. Ann Thorac Med. 2015;10(3):158–168. doi: 10.4103/1817-1737.160831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wuytack F, Meskell P, Conway A, McDaid F, Santesso N, Hickey FG, et al. The effectiveness of physiologically based early warning or track and trigger systems after triage in adult patients presenting to emergency departments: a systematic review. 38BMC Emerg Med. 2017;17 doi: 10.1186/s12873-017-0148-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim MJ, Larson JL. Ineffective airway clearance and ineffective breathing patterns: Theorical and research base for nursing diagnosis. [Cited Jul 5, 2018];Nurs Clin North Am. 1987 Mar;22(1):125–134. Internet. https://www.ncbi.nlm.nih.gov/pubmed/3644285. [PubMed] [Google Scholar]
- 4.Herdman TH, Kamitsuru S. Diagnósticos de Enfermagem da NANDA: definições e classificação 2018-2020/ [NANDA Internacional] 10a. Porto Alegre: Artmed; 2018. [Google Scholar]
- 5.Sallum AMC, Santos JLF, Lima FD. Nursing diagnoses in trauma victims with fatal outcomes in the emergency scenario. [cited July 5, 2018];Rev. Latino-Am. Enfermagem. 2012 Feb;20(1):3–10. doi: 10.1590/s0104-11692012000100002. Internet. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0104-11692012000100002&lng=en. [DOI] [PubMed] [Google Scholar]
- 6.Okuno MFP, Costa N, Lopes MCBT, Campanharo CRV, Batista REA. The most used nursing diagnoses at an emergency service. [cited July 5, 2018];Acta Paul Enferm. 2012 25(2):256–262. Internet. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0103-21002012000200016&lng=en. [Google Scholar]
- 7.Galdeano LE, Rossi LAR, Pezzuto TM. Nursing diagnosis of patients in the preoperatory period of cardiac surgery. [cited July 5, 2018];Rev Esc Enferm USP. 2004 Sep;38(3):307–316. doi: 10.1590/s0080-62342004000300009. Internet. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0080-62342004000300009&lng=en. [DOI] [PubMed] [Google Scholar]
- 8.Gordon M, Hiltunen E. High frequency: treatment priority Nursing diagnoses in critical care. [cited July 8, 2018];Nurs Diagn. 1995 Oct-Dec;6(4):143–154. doi: 10.1111/j.1744-618x.1995.tb00285.x. Internet. https://www.ncbi.nlm.nih.gov/pubmed/8573434. [DOI] [PubMed] [Google Scholar]
- 9.Araújo DS, Freire AF, Mendonça JKS, Bettencourt ARC, Amaral TLM, Prado PR. Construction and validation of a systematization instrument for nursing in intensive care. Rev Rene. 2015 Jul-Ago;16(4):461–469. doi: 10.15253/2175-6783.2015000400002. [DOI] [Google Scholar]
- 10.Black LF, Hyatt RE. Maximal respiratory pressures: normal values and relationship to age and sex. Am Rev Respir Dis. 1969 May;99(5):696–702. doi: 10.1164/arrd.1969.99.5.696. [DOI] [PubMed] [Google Scholar]
- 11.Souza RB. Sociedade Brasileira de Pneumologia e Tisiologia. Diretrizes para teste de função pulmonar. Pressões respiratórias estáticas máximas. [cited July 9, 2018];Jornal Bras Pneumol. 2002 28(3):S155–S165. Internet. http://www.jornaldepneumologia.com.br/PDF/Suple_137_45_88%20Press%C3%B5es%20respirat%C3%B3rias%20est%C3%A1ticas%20m%C3%A1ximas.pdf. [Google Scholar]
- 12.Prado PR, Bettencourt ARC, Lopes JL. Defining characteristics and related factors of nursing diagnosis ineffective breathing pattern: na integrative literature review. Rev Bras Enferm. 2018 doi: 10.1590/0034-7167-2018-0061. No prelo. [DOI] [PubMed] [Google Scholar]
- 13.Avena M, Pedreira MLG, Gutiérrez MGR. Conceptual validation of the defining characteristics of respiratory nursing diagnoses in neonates. [cited July 9, 2018];Acta Paul Enferm. 2014 Feb;27(1):76–85. Internet. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0103-21002014000100015&lng=en http://dx.doi.org/10.1590/1982-0194201400015. [Google Scholar]
- 14.Cavalcante JCBC, Mendes LC, Lopes MVO, Lima LH. Clinical indicators of ineffective breathing pattern in children with asthma. [cited July 9, 2018];Rev RENE. 2010 Jan-Mar;11(1):66–75. Internet. http://www.revistarene.ufc.br/vol11n1_html_site/a07v11n1.htm. [Google Scholar]
- 15.Silva VM, Araujo TL, Lopes MVO. Evolution of nursing diagnoses for children with congenital heart disease. [cited 2018 Aug 24];Rev. Latino-Am. Enfermagem. 2006 Aug;14(4):561–568. doi: 10.1590/s0104-11692006000400014. Internet. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0104-11692006000400014&lng=en http://dx.doi.org/10.1590/S0104-11692006000400014. [DOI] [PubMed] [Google Scholar]
- 16.Bertoncello KCG, Cavalcanti CDK, Ilha P. Real diagnoses and nursing intervention proposals for multiple trauma victims. Rev Eletron Enferm. 2013 Out-Dez;15(4):905–914. doi: 10.5216/ree.v15i4.19497. Internet. [DOI] [Google Scholar]
- 17.Canto DF, Almeida MA. Nursing outcomes for ineffective breathing patterns and impaired spontaneous ventilation in intensive care. [cited 2018 Aug 24];Rev Gaúcha Enferm. 2013 Dec;34(4):137–145. doi: 10.1590/s1983-14472013000400018. Internet. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1983-14472013000400018&lng=en. [DOI] [PubMed] [Google Scholar]
- 18.Santos NA, Cavalcante TF, Lopes MVO, Gomes EB, Oliveira CJ. Profile of nursing diagnoses in patients with respiratory disorders. Invest Educ Enferm. 2015;33(1):112–118. doi: 10.1590/S0120-53072015000100013. [DOI] [PubMed] [Google Scholar]
- 19.Mota DDCF, Cruz DALM, Pime CAM. Fatigue: a concept analyses. [cited July 9, 2018];Acta Paul Enferm. 2005 Sep;18(3):285–293. Internet. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0103-21002005000300009&lng=en. [Google Scholar]
- 20.Ferreira EVM. Respiratory muscles: myths and secrets. [cited July 9, 2018];J Bras Pneumol. 2015 Apr;41(2):107–109. doi: 10.1590/S1806-37132015000200002. Internet. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1806-37132015000200107&lng=en http://dx.doi.org/10.1590/S1806-37132015000200002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Silva GA. Medicina. 2. Vol. 39. Ribeirão Preto: 2006. Abr.-Jun. [cited July 9, 2018]. Obesity hypoventilation syndrome; pp. 195–204. Internet. http://sobrafir.com.br/imagens_up/artigos/Obesidade_e_Hipoventilacao_Alveolar.p. [Google Scholar]
- 22.Caruso P, Albuquerque ALP, Santana PV, Cardenas LZ, Ferreira JG, Prina E, et al. Diagnostic methods to assess inspiratory and expiratory muscle strength. 2015 Mar-Apr;41(2):110–123. doi: 10.1590/S1806-37132015000004474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seganfredo DH, Beltrão BA, Silva VM, Lopes MVO, Castro SMJ, Almeida MA. Analysis of ineffective breathing pattern and impaired spontaneous ventilation of adults with oxygen therapy Rev. [cited July 9, 2018];Latino-Am. Enfermagem. 2017 25:e2954. doi: 10.1590/1518-8345.1950.2954. Internet. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0104-11692017000100395&lng=en http://dx.doi.org/10.1590/1518-8345.1950.2954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ali NA, O’Brien JM, Jr, Hoffmann SP, Phillips G, Garland A, Finley JC, et al. Midwest Critical Care Consortium Acquired weakness, handgrip strength, and mortality in critically ill patients. Am J Respir Crit Care Med. 2008 Aug 1;178(3):261–268. doi: 10.1164/rccm.200712-1829OC. [DOI] [PubMed] [Google Scholar]
- 25.Maramattom BV, Wijdicks EF. Acute neuromuscular weakness in the intensive care unit. Critical Care Medicine. Crit Care Med. 2006 Nov;34(11):2835–2841. doi: 10.1097/01.CCM.0000239436.63452.81. [DOI] [PubMed] [Google Scholar]
- 26.Khan J, Harrison TB, Rich MM. Mechanisms of neuromuscular dysfunction in critical illness. Crit Care Clin. 2008;24(1):165. doi: 10.1016/j.ccc.2007.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Truong AD, Fan E, Brower RG, Needham DM. Benchto-beside review: mobilizing patients in the intensive care unit from pathophysiology to clinical trials. 216Crit Care. 2009 Jul;13(4) doi: 10.1186/cc7885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Latronico N, Herridge M, Hopkins RO, Angus D, Hart N, Hermans G, et al. The ICM research agenda on intensive care unit-acquired weakness. Intensive Care medicine. 2017 Sep;43(9):1270–1281. doi: 10.1007/s00134-017-4757-5. [DOI] [PubMed] [Google Scholar]
- 29.Castell MV, Sânchez M, Julián R, Queipo R, Martín S, Otero A. Frailty prevalence and slow walking speed in persons age 65 and older: implications for primary care. 86BMC Fam Pract. 2013 Jun 19;14 doi: 10.1186/1471-2296-14-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Neri AL, Yassuda MA, Araújo LF, Eulálio MC, Cabral BE, Siqueira MEC, et al. Methodology and social, demographic, cognitive, and frailty profiles of community-dwelling elderly from seven Brazilian cities: the FIBRA Study. [cited July 9, 2018];Cad Saúde Pública. 2013 Apr;29(4):778–792. Internet. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0102-311X2013000400015&lng=en http://dx.doi.org/10.1590/S0102-311X2013000400015. [PubMed] [Google Scholar]
- 31.Lira LN, Santos SSC, Vidal DAS, Gautério DP, Tomaschewski-Barlem JG, Piexak DR. Nursing diagnosis and prescriptions for hospitalized elderly. [cited July 9, 2018];Av Enferm. 2015 May;33(2):251–260. Internet. http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0121-45002015000200007&lng=en http://dx.doi.org/10.15446/av.enferm.v33n2.30762. [Google Scholar]
- 32.Talbot HK. Influenza in older Adults. Infect Dis Clin North Am. 2017 Dec;31(4):757–766. doi: 10.1016/j.idc.2017.07.005. [DOI] [PubMed] [Google Scholar]
- 33.Stockton J, Stephenson I, Fleming D, Zambon M. Human metapneumovirus as a cause of community-acquired respiratory illness. Emerg Infect Dis. 2002 Sep;8(9):897–901. doi: 10.3201/eid0809.020084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Boivin G, Abed Y, Pelletier G, Ruel L, Moisan D, Côté S, et al. Virological features and clinical manifestations associated with human metapneumovirus: a new paramyxovirus responsible for acute respiratory-tract infections in all age groups. J Infect Dis. 2002 Nov 1;186(9):1330–1334. doi: 10.1086/344319. [DOI] [PubMed] [Google Scholar]
- 35.Santos ZM, Oliveira ML. Assessment of knowledge, attitudes and practices of the elderly about the vaccine against Influenza in a Public Health Unit, Taguatinga, Federal District, Brazil, 2009. Epidemiol Serv Saúde. 2010 Sep;19(3):205–216. doi: 10.5123/S1679-49742010000300003. [DOI] [Google Scholar]
- 36.Malvestio MAA, Sousa RMC. Survival after motor vehicle crash: impact of clinical and prehospital variables. Rev Saúde Pública. 2008 Aug;42(4):639–647. doi: 10.1590/S0034-89102008000400009. [DOI] [PubMed] [Google Scholar]
- 37.ATLS Subcommittee. American College of Surgeons’ Committee on Trauma. International ATLS working group Adv Trauma Life Support (ATLS®): the ninth edition. [cited July 9, 2018];J Trauma Acute Care Surg. 2013 May;74(5):1363–1366. doi: 10.1097/TA.0b013e31828b82f5. Internet. [DOI] [PubMed] [Google Scholar]
- 38.Dal Sasso GTM, Barra DCC, Paese F, Almeida SRW, Rios GC, Marinho MM, et al. Computerized nursing process: methodology to establish associations between clinical assessment, diagnosis, interventions, and outcomes. [cited July 9, 2018];Rev Esc Enferm USP. 2013 Feb;47(1):242–249. doi: 10.1590/s0080-62342013000100031. Internet. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0080-62342013000100031&lng=en http://dx.doi.org/10.1590/S0080-62342013000100031. [DOI] [PubMed] [Google Scholar]
- 39.Schmidt M, Demoule A, Polito A, Porchet R, Aboab J, Siami S, et al. Dyspnea in mechanically ventilated critically ill patients. Crit Care Med. 2011 Sep;39(9):2059–2065. doi: 10.1097/CCM.0b013e31821e8779. [DOI] [PubMed] [Google Scholar]
- 40.Goodridge D, Duggleby W, Gjevre J, Rennie D. Exploring the quality of dying of patients with chronic obstructive pulmonary disease in the intensive care unit: a mixed methods study. Nurs Crit Care. 2009 Mar-Apr;14(2):51–60. doi: 10.1111/j.1478-5153.2008.00313.x. [DOI] [PubMed] [Google Scholar]
- 41.Sociedade Brasileira de Pneumologia e Tisiologia IV Diretrizes brasileiras no manejo da asma. [cited July 9, 2018];J Bras Pneumol. 2006 Nov;32(Suppl 7):S447–SS74. Internet. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1806-37132006001100002&lng=en http://dx.doi.org/10.1590/S1806-37132006001100002. [Google Scholar]
- 42.Pratter MR, Brightling CE, Boulet LP, Irwin RS. An empiric integrative approach to the management of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006 Jan;129(1) Suppl:222S–231S. doi: 10.1378/chest.129.1_suppl.222S. [DOI] [PubMed] [Google Scholar]
- 43.Silveira UA, Lima LHO, Lopes MVO. Defined characteristics of the nursing diagnoses ineffective airway clearance and ineffective breathing pattern in asthmatic children. Rev RENE. 2008 Out-Dez;9(4):125–133. [Google Scholar]
- 44.Cunha CS, Toledo RV. The Performance of the Physiotherapy in the Reversion of the Atelectasis: A report of a case in the Intensive Therapy Unit. [cited July 9, 2018];Cads Unifoa. 2007 Aug;2(2):81–87. Internet. http://revistas.unifoa.edu.br/index.php/cadernos/article/view/881. [Google Scholar]