Abstract
Objective: To establish structure, process and outcome indicators to evaluate tissue integrity in Canadians with spinal cord injury or disease (SCI/D) in the first 18 months following inpatient rehabilitation admission.
Method: A Working Group comprised of Canadian subject matter experts in the Domain of Tissue Integrity was formed to define the construct of tissue integrity. A literature review was conducted and a Driver diagram produced to identify factors that influence tissue integrity in individuals with SCI/D. Facilitated meetings were conducted to identify and achieve consensus on structure, process and outcome indicators. Rapid cycle testing was used to pilot test proposed indicators for face validity and feasibility within a quality improvement context.
Results: The structure indicators are the proportion of patients with SCI/D who have access to a mirror for skin checks and the proportion of patients who have access to patient education on tissue integrity; the process indicator is the proportion of patients who completed daily head-to-toe skin checks; the intermediary outcome indicator is pressure injury (PI) incidence during inpatient rehabilitation; and the final outcome indicator is the proportion of individuals with intact skin at 18 months following rehabilitation admission.
Conclusion: The set of indicators established for the Domain of Tissue Integrity are specifically focused on aspects of care that can impact the maintenance of tissue integrity and the prevention of PI and align with current practice guidelines. The implementation and evaluation of these indicators nationally have the potential to improve care for Canadians with SCI/D.
Keywords: Pressure injury, Indicators, Outcomes, Healthcare quality indicators
Introduction
Spinal cord injury or disease (SCI/D) is a life-altering condition that impacts multiple body systems leading to several secondary health conditions. Pressure injury (PI) is a common yet serious health complication following SCI/D, with lifetime prevalence of 85–95%.1,2 The National Pressure Ulcer Advisory Panel (NPUAP)3 defines PI as “localized damage to the skin and underlying soft tissue usually over a bony prominence or related to a medical or other device. The injury can present as intact skin or an open ulcer and may be painful. The injury occurs as a result of intense and/or prolonged pressure or pressure in combination with shear. The tolerance of soft tissue for pressure and shear may also be affected by microclimate, nutrition, perfusion, co-morbidities and condition of the soft tissue.”4 Up to 66% of individuals with SCI will experience a PI in their lifetime.5 It has been reported that 50% of wheelchair users experience tissue breakdown due to prolonged sitting.6 Thirty-one percent of PI in individuals with SCI occur over the ischium, followed by trochanters (26%), sacrum (18%), heel (5%), malleolus (4%) and feet (2%).7
PIs can occur at any time following a SCI, 20-33% of individuals with SCI will develop a PI before admission to inpatient rehabilitation.8–10 During inpatient SCI rehabilitation, PI incidence ranges from 10% to 48%.8,11,12 Individuals who develop a PI during SCI rehabilitation have poorer rehabilitation participation, outcomes9,11, and longer lengths of stay.9,13 A non-healing PI can have life-altering consequences resulting in reduced quality of life,14,15 increased morbidity, and mortality. Premature death attributed to PIs occurs in 7-8% of those with SCI who develop a PI.16
PIs have a significant economic impact on the healthcare system. A recent review of cost analyses estimated that mean one-year hospital costs of PI and leg ulcers for the general adult population without SCI was $15,400 CAD for PI and $11,000 CAD for leg ulcers.17 The additional PI hospital episode cost was $1,151 from a health-care public payer perspective and $31,344 from a hospital perspective.17 The Rick Hansen Spinal Cord Injury Registry (RHSCIR) reported that participants with traumatic SCI experiencing one or more PIs resulted in an increase of approximately $7,451 CAD to the cost of each acute RHSCIR site hospital admission.18
In order to address the significant impact of PI, maintenance of tissue integrity and PI prevention has become an important patient safety priority in healthcare settings in Canada and globally and is reflected in many accreditation programs.19–22 Priority areas include: prevention and effective management of PIs through best practice guidelines,23 care pathways, and patient and caregiver resources.4,24,25
PI risk factors after SCI/D include: increasing age, male, increasing time post-injury, motor complete injury, severity of muscle atrophy, presence of urinary or fecal incontinence, renal impairment, anemia, underweight, increased tissue temperature,24 difficulties with level transfers26 or deep tissue injury on ultrasound.27,28 With greater focus on patient safety in healthcare settings, organizations like the Agency for Healthcare Research and Quality and the Institute for Healthcare Improvement have identified the need for quality indicators related to PI to measure the effectiveness of quality improvement interventions.21,29 Despite this, further active implementation initiatives30 are needed to integrate existing learnings in the area of tissue integrity. Calls to action urging improved coordination of care to reduce the incidence and impact of PI on individuals with SCI are also needed.31,32
Indicators of quality rehabilitation care, which include the prevention and management of PI, can be categorized as structure, process and outcome. Structure indicators are defined by the properties of the setting in which healthcare services occur33 while process indicators describe the specific activities in providing and receiving of care.34 Outcome indicators reflect the patient’s mortality, morbidity, health status, health-related quality of life and patient/family/provider satisfaction as a result of the care.34 Together, these indicators can create an evaluation framework for implementation across settings to inform the development of benchmarks of exemplary care.
The SCI Rehabilitation Care High Performance Indicators (or “SCI-High”) Project endeavors to advance SCI/D rehabilitation care by 2020 through consensus derived development/selection, implementation, and evaluation of indicators of quality care for 11 Domains of rehabilitation care prioritized by clinicians, researchers and individuals living with chronic SCI/D. (www.sci-high.ca). This paper describes the processes involved to select and develop a framework of structure, process and outcome indicators related to the Domain of Tissue Integrity from the time of rehabilitation admission and up to 18 months thereafter among individuals with SCI/D.
Methods
A detailed description of the overall SCI-High Project, the approach to prioritization of SCI rehabilitation care Domains, and the methods and process for identifying Tissue Integrity as a priority Domain for SCI rehabilitation care are explained in related manuscripts in this issue.35,36 In addition to the Project Team, an External Advisory Committee and Data Strategy Committee supported global project goals and provided oversight and context for implementation.
The approach to developing the structure, process and outcome indicators for Tissue Integrity followed a modified, but similar, approach to that described by Mainz.37 This included the following planning and development phases: (a) formation and organization of the national and local Working Group (e.g. Tissue Integrity Working Group);36 (b) defining and refining the key Domain and specific target construct; (c) providing an overview/summary of existing evidence and practice; (d) developing and interpreting a Driver diagram; (e) selecting indicators; and (f) pilot testing and refinement of the Domain-specific structure, process and outcome indicators. Throughout the process of developing structure, process and outcome indicators for the Tissue Integrity Domain, a facilitated discussion occurred amongst the Working Group and SCI-High Project Team to utilize relevant expertise in the area of tissue integrity, while ensuring the broader goals of the SCI-High Project were aligned across the other Domain Working Groups (as appropriate).
Tissue Integrity Working Group
Experts in tissue integrity and stakeholders from across Canada were invited to participate in the SCI-High Project as members of the Domain-specific Working Group based on their knowledge of SCI/D rehabilitation, tissue integrity, and health service provision. The group was composed of clinicians, scientists and postdoctoral fellows. The Working Group met three times via conference call over two months, totaling three hours of discussions when developing the indicators, and an additional two hours, to refine the indicators and discuss manuscript preparation. The Working Group’s efforts were bootstrapped to prior collaborative efforts among: (1) The Knowledge Mobilization Network, a pan-Canadian collaborative focused on best practice implementation, initially focused on PI prevention at six rehabilitation sites in Alberta, Ontario and Quebec;23 (2) the electrical stimulation for wound healing clinical collaborative38 which led to the release of best practice guidelines for PIs in persons with SCI/D,24 and, (3) RHSCIR 2.0 data sets which included incidence and prevalence of PIs.39 In addition, Working Group members completed independent reviews of prepared materials, shared resources and practice standards via email or teleconference, or conducted independent pilot implementations and evaluations of proposed indicators outside of scheduled meetings.
Construct definition and Driver diagram
Prior to the development of indicators, the Working Group established consensus on the construct definition for tissue integrity and ensured the definition was aligned with newest concepts and terminology.40 The group adapted the construct definition established in the Rehabilitation Environmental Scan Atlas41 to the following: Maintaining tissue integrity after SCI/D involves the prevention and management of pressure injury in areas of the body where sensation is diminished or absent. The overall aim for the Tissue Integrity Working Group was to reduce the overall incidence and severity of pressure injuries among individuals with SCI/D throughout their lifetime.
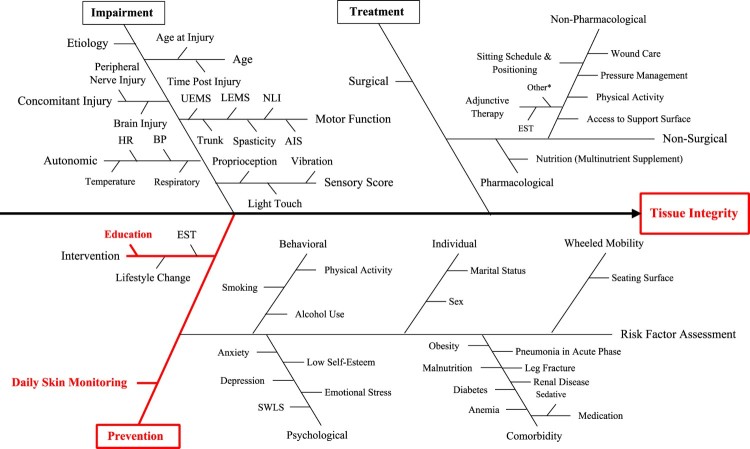
The selection of Tissue Integrity as a Domain of interest for developing indicators emerged from a consensus-building activity to select the broader set of Domains being pursued in the larger initiative. This process involved a systematic search to collect information about SCI/D rehabilitation care related to tissue integrity and factors that influence outcomes and a scoping synthesis of the data acquired. Medline and CINAHL databases were searched using combinations of the following terms: “pressure ulcers”, “wounds and injuries”, and “spinal cord injury”. Non-English manuscripts and inappropriate study designs were excluded. This information was used to create a Driver diagram to illustrate known drivers or factors that impact tissue integrity among individuals with SCI/D (Figure 1). A Driver diagram is a visual display of a high-level quality improvement goal, and a set of underpinning factors/goals. The tool helped to organize change concepts as the Working Group discerned “what changes can we make, that will result in goal attainment”. As the Domain of Tissue Integrity includes prevention and treatment of PIs, both concept areas were incorporated into the Driver diagram (red branches). The impairment branch of the Driver diagram is common to all 11 Domains. The branches shown in red (Figure 1) represent the main foci for development of Tissue Integrity indicators based on expert consensus.
Figure 1.
Tissue Integrity Driver diagram. UEMS: Upper-Extremity Motor Score; LEMS: Lower-Extremity Motor Score; NLI: Neurological Level of Injury; AIS: ASIA Impairment Scale; HR: Heart Rate; BP: Blood Pressure; EST: Electrical Stimulation Therapy; SWLS: Satisfaction with Life Scale. * Electromagnetic energy, ultraviolet-C light, noncontact non-thermal acoustic therapy, topical oxygen, Maggot therapy, topical recombinant growth factors, recombinant human erythropoietin, anabolic steroids, activated factor XIII, tension therapy, and hyperbaric oxygen.
Selection of indicators
The Working Groups were asked to develop/select at least one structure, process and outcome indicator related to the Domain of Tissue Integrity. Leaders stipulated that indicators must be relevant, concise and feasible (10 minutes or less) to implement, and aligned across structure, process and outcome indicator in achieving a single substantive advance in SCI rehabilitation care. The indicators could be measured using established or new measurement tools (i.e. questionnaires, data collection sheets, and medical record data), depending on requirements and feasibility of a given indicator. With this consideration, Tissue Integrity indicators that met the above criteria and could address aspects of PI prevention were identified. Consensus was attained among the Working Group using their clinical and research expertise to decide which indicators would most directly relate to the overall goal of reducing PI incidence.
Indicator piloting
Once consensus was established on a proposed set of indicators, pilot testing for feasibility was conducted at an inpatient rehabilitation setting using rapid Plan-Do-Study-Act (PDSA) cycles.42 These short-term quality improvement testing cycles allowed for quick qualitative evaluations, feedback and refinement of tools or processes.
Results
Selection/development of structure, process and outcome indicators for Tissue Integrity required review and refinement of the Driver diagram shown in Figure 1. To select indicators with maximum impact, the group decided to focus on the prevention branch of the Driver diagram, with the rationale that prevention of PIs was the area that could be monitored for all patients. PI interventions/treatments would only address patients who had a PI, and would not serve all individuals potentially at risk. Table 1 summarizes the type of indicators, denominator, and timing of each measurement for the selected Tissue Integrity indicators chosen by the Working Group.
Table 1. Structure, process and outcome indicators for Tissue Integrity, with a focus on prevention of pressure injury.
| Indicator | Denominator | Type of indicator | Time of measurement |
|---|---|---|---|
| Proportion of patients with access to education/resources related to tissue integrity and pressure injury | Number of non-ambulatory individuals with SCI/D | Structure | Annual |
| Proportion of individuals with SCI/D with access to hand-held or portable mirror for skin check | Number of non-ambulatory individuals with SCI/D | Structure | Discharge |
| Proportion of individuals with SCI/D who completed daily head to toe skin checks | Mean of the daily head to toe skin check per month | Process | Annual |
| Proportion of individuals with SCI/D diagnosed with a pressure injury | Number of non-ambulatory individuals with SCI/D | Outcome – Intermediary | Rehabilitation admission/ Discharge |
| Proportion of individuals with SCI/D diagnosed with intact skin | Number of non-ambulatory individuals with SCI/D | Outcome – Final | 18-month post rehabilitation admission |
Indicator piloting
The described indicators are intended for use with all patients admitted for tertiary SCI/D rehabilitation regardless of impairment etiology (trauma or non-trauma), whether for an initial or subsequent admission, and to follow patients longitudinally from the time of rehabilitation admission through to 18 months after the date of rehabilitation admission.
The feasibility of the structure indicator questionnaire and the process indicator were tested within a tertiary SCI/D inpatient rehabilitation hospital in Toronto using rapid PDSA cycles. Six patients undergoing SCI/D rehabilitation were visited for 10 consecutive days to test the feasibility of the process indicator.
Structure indicator
Both structure indicators were pilot tested using the patient questionnaire (Table 2) during the first visit. The Project Team also reviewed the variety of hand-held mirrors and consulted with the local skin and wound clinic regarding desired mirror features and price. Mirror features including the length of handle, tilt options, weight and ability of persons of varying ability to lift and carry as well as process considerations for use and replacement were also discussed.
Table 2. Patient questionnaire for the Tissue Integrity structure indicator.
| 1. Has someone from your healthcare team (nurses, doctors, therapists) spoken to you about the risk of pressure sores/injuries? □ No □ Yes □Not sure |
| 2. Has someone from your healthcare team (nurses, doctors, therapists) taught you how to check your skin? □ No □ Yes □Not sure |
| 3. Do you have a hand-held mirror? □Yes, I use daily □Yes, I use it often (more than 3 times/week) □Yes, but I hardly use it (less than 3 times/week) □No □Not sure |
| 4. If you do not have a mirror, please select all that apply: □Not needed □Unable to purchase one □Unable to use it □Lost/Broken □Not Sure □Nobody told me □Other: ______________ |
| 5. Do you have any questions or concerns with regards to your skin health? _________________ |
The questionnaire was piloted by five of six inpatients who reported receiving information about tissue integrity management while four indicated that they were taught how to “check their skin”. Although tissue care education was well-established, all six pilot inpatients interviewed reported they did not own a mirror because they didn’t perceive a need for one (low risk or unable to use mirror) and financial constraints, or because they planned that someone else (family/caregiver, healthcare staff) would check their skin post-discharge. No challenges were identified after the first and only PDSA cycle for the structure indicator patient questionnaire, resulting in no major changes except removing the option “Unknown” in all questions, and adding the option “Unable to use it” in question 4.
Process indicator
Two PDSA cycles were completed for the process indicator. During the first, we quickly identified that some patients did not answer the question regarding daily skin checks, but answered once the administrator came to switch the cards. Thus, we added fields to track if completing the card was patient-initiated or triggered by the administrator checking the card.
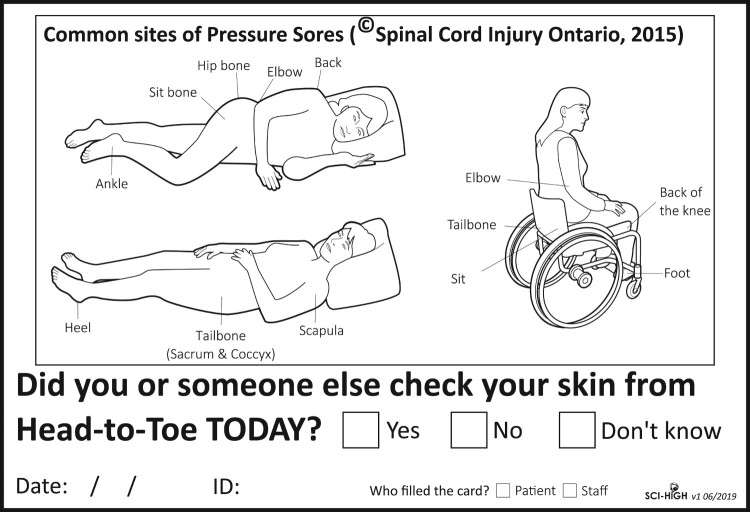
During the second PDSA, all six patients received a SCI-High Daily Skin Check Card (Figure 2) daily, for 10 days. Patients were instructed to complete the daily skin check cards for 10 consecutive days. The cards asked a yes/no question: “Did you or someone else check your skin from head-to-toe today?”. The completed card was collected during lunch (12-pm) daily and a new card was provided, resulting in 60 total cards distributed. A YES response was coded if the entire head-to-toe skin check was completed. Otherwise, if a region on the card was missed (e.g. ankles), the response was coded as NO. Assistance was provided by the administrator, healthcare provider or family in physically completing the paper questionnaire if individuals were unable to complete independently. Barriers to implementation of the structure indicator questionnaire and the daily skin check cards were also noted.
Figure 2.
SCI-High daily skin check cards for the process indicator. Illustration used with permission from Spinal Cord Injury Ontario and adapted from Preventing and Treating Pressure Sores: A guide for people with spinal cord injuries (2015). https://sciontario.org/support-services/resources/living-with-an-sci/skin-health-pressure-injuries/.
When considering all responses, independent of who completed the card (i.e. patient or administrator), 4 out of 6 patients checked their own skin daily or had their skin checked daily by a healthcare team member for 10 days. The remaining two patients reported only two times where their skin was not checked, and one time where they did not know if it had been checked.
We also recorded if completing the card had to be triggered by the administrator or the patient, in response to the results of the first PDSA cycle. One person filled their own card eight times in 10 days; one person filled their own card seven times in 10 days; the remaining four patients filled their own card less than three times in 10 days. Although the patient’s proactivity in filling out cards was low (e.g. completed by administrator or healthcare member; n = 37), patients reported that cards were a helpful visual reminder for daily skin checks. Eleven out of 60 cards were not filled out, and the patient was not available for clarification of reason during the scheduled card exchange.
Skin check feasibility questionnaire
During the last day of data collection, patients were asked about the feasibility of the skin check cards (Table 3). Data were collected from five of six participants; one participant was discharged from hospital on the last day of piloting and therefore did not complete the feasibility questionnaire. Two patients rated the usefulness of skin check cards as reminders to check their skin for PIs as a 4, on a 5-point scale, with 1 being not useful and 5 being very useful. Two patients gave a rating of 2. All but one patient agreed that cards were easy to use, requiring an average of 12 seconds (standard deviation: 10.4) to complete. We also inquired about patient’s interest in converting from a paper to software version of skin check cards (i.e. mobile technologies). Two of three patients indicated they would not use a cell phone application to record completion of daily skin check after discharge from inpatient rehabilitation. This was contrary to our assumption that an application linked to an individual’s cell phone might be a good daily prompt for skin check completion and a means of tracking daily skin check completion.
Table 3. Skin check feasibility questionnaire.
| 1. Do you think the skin check cards were useful as a reminder to check your skin for pressure injuries daily? Not useful □1 □2 □3 □4 □5 Very useful |
| 2. Were the cards easy to use? Complicated □1 □2 □3 □4 □5 Very simple |
| 3. How long did it take to complete the cards? _______ s |
| 4. How would you improve the skin card system? ________________________________ |
| 5. Thinking about going home, if this was an app, would you use it? __________________ |
| 6. Do you have any other comments or feedback? ________________________________ |
Discussion
This initiative resulted in the development and preliminary pilot testing of a set of structure, process and outcome indicators in the Domain of Tissue Integrity for individuals with SCI/D during the first 18 months after inpatient rehabilitation admission. The objective was to promote and establish patient’s self-awareness regarding daily skin checks prior to rehabilitation discharge. Although the structure and process indicators selected only represent one aspect of tissue integrity, specifically daily skin checks, the Working Group felt that implementing and evaluating these indicators would have a meaningful impact on SCI/D rehabilitation relative to the tissue integrity that others would endorse.43 Provision of prevention education has also been shown to reduce PI recurrence.21 Other drivers21,38 of tissue integrity such as PI risk assessment have previously been implemented through other initiatives26 and are often required to be monitored organizationally.20 We acknowledge that daily skin checks are a beneficial and necessary first step, but are not to sufficient to guarantee the absence of PIs, and that several other practices contribute to maintenance of tissue integrity in individuals with SCI/D.24,44
Despite education regarding the importance of daily skin checks, they are not consistently performed by individuals with SCI/D. A Dutch study indicating that less than 50% of individuals with SCI living in the community performed daily skin checks and pressure relief strategies.45 Our pilot test results, as well as qualitative feedback from clinicians, suggests that the process of monitoring completion of daily skin checks could have a meaningful and longitudinal impact on increasing patient and healthcare provider accountability regarding maintenance of tissue integrity. Interestingly, during pilot testing, some patients reliant on staff to complete their skin check due to poor hand dexterity or severe upper extremity or trunk impairment reported that their skin was not checked. Nonetheless, follow-up with nurses indicated that skin was checked but hadn’t been discussed with the patient, nor documented. These observations created opportunity for immediate feedback and practice improvements to enhance mutual accountability of nurses and patients. Opportunities to augment documentation practices and promote charting by exception within care maps were additional ideas identified to increase clarity of documentation and communication. The initial aim is for nurses to model skin check behavior, and during admission, individual patients learn to complete daily skin checks independently (with or without aids). The Working Group acknowledges that early PI recognition is a key step in reducing the PI severity and that access to appropriate inter-professional expertise and local resources to manage a PI (once detected) to prevent progression and restore tissue integrity are crucial next steps.
During the early Tissue Integrity Working Group discussions, the group expressed apprehension about not focusing our efforts in the acute care phase due to a high percentage of patients with SCI acquiring a PI prior to rehabilitation admission.8–10 The group agreed that although management of PIs in acute care is important, it was beyond the current SCI-High Project scope and context for decision making, but would be an ideal area for future indicator development.
The Tissue Integrity Working Group also suggested the need for indicator development in the community after rehabilitation discharge given the high lifetime incidence of PI in individuals with SCI/D. Working Group members agreed that monitoring the proportion of individuals with intact skin at 18 months following SCI rehabilitation admission would be an important benchmark. Furthermore, the Working Group felt that inpatient rehabilitation is a time following SCI/D, where there is a strong focus on patient education, self-management, and transition to community living. Efforts focusing on prevention of PI during this crucial period while acquiring important skills regarding daily skin monitoring can facilitate the establishment of a strong routine to promote lifelong maintenance of tissue integrity. Surprisingly, respondents did not think that having a mobile application reminder on their cell phone would be helpful. However, it was a small sample size and an alternative reminder system to increase daily skin checks should not be dismissed. These issues require further exploration since Vershueren and colleagues46 found that the occurrence of PI during acute rehabilitation was a strong predictor for future PI development. Therefore, efforts to prevent PI development during inpatient rehabilitation should have lasting effects following community reintegration.
Results from our pilot testing indicate that no participants owned a mirror, suggesting a need for further exploration to better understand barriers for mirror deployment from an organizational perspective, which may be inadvertently influencing behavior among individuals with SCI/D. There may also be unconscious bias in how mirrors are distributed and introduced to patients. For example, ready access to affordable mirrors may facilitate uptake if cost was identified as a barrier. Alternatively, establishing a process for staff to understand who needs a mirror, what type of mirror is appropriate based on impairment may be necessary. Moreover, establishing processes for purchasing and dissemination of mirrors and policies for replacing mirrors may also be necessary to improve mirror usage for daily skin checks.
The Tissue Integrity indicators will be deployed provincially at five sites in Ontario in 2019, with plans for national implementation underway. These indicators when combined with the RHSCIR pressure injury data elements18 and Knowledge Mobilization Network efforts30 will serve to provide a better understanding of the epidemiology of tissue injury across the continuum of care in the first two years following injury.
Conclusion
The overall objective of the SCI-High Project is to advance SCI/D rehabilitation care by 2020. We have described the process for the identification of structure, process and outcome indicators for the Tissue Integrity Domain for implementation as part of SCI/D rehabilitation in Canada. Standardized timing for documentation of mirror deployment and use during daily head to toe skin checks will enable national exploration of the associations between PI incidence and performance of daily skin checks for PI prevention among individuals with SCI/D. We anticipate that the national implementation and evaluation of the proposed structure, process and outcome indicators related to the Domain of Tissue Integrity will drive health system, site, clinician and patient reflection and behavior change related to PI prevention practices with the expectation of improved quality of life for individuals with SCI/D and reduction in economic burden to the health system.
Disclaimer statement
Contributors None.
Declaration of interest Dr. B. Catharine Craven acknowledges support from the Toronto Rehab Foundation as the Toronto Rehabilitation Institute Chair in Spinal Cord Injury Rehabilitation and receipt of consulting fees from The Rick Hansen Institute. Heather Flett, Dr. Matheus Joner Wiest, Dr. Vivian Mushahwar, Dr. Chester Ho, Dr. Jane Hsieh, Farnoosh Farahani, Dr. S. Mohammad Alavinia, Maryam Omidvar, and Dr. Pamela Houghton report no conflicts of interest.
Conflicts of interest None.
Funding Statement
This work is embedded in the larger SCI-High Project funded by the Rick Hansen Institute (Grant #G2015-33), Ontario Neurotrauma Foundation (ONF; Grant #2018 RHI HIGH 1057), and Toronto Rehab Foundation.
Acknowledgements
The authors would like to acknowledge the time, energy and expertise of Dr. Mark Bayley from Toronto Rehabilitation Institute – University Health Network, and Dr. Sander Hitzig from St. John’s Rehab Research Program–Sunnybrook Research Institute throughout the indicator development process.
ORCID
Heather Flett http://orcid.org/0000-0001-9444-8006
Matheus J. Wiest http://orcid.org/0000-0003-1444-4828
Vivian Mushahwar http://orcid.org/0000-0001-9873-611X
Chester Ho http://orcid.org/0000-0002-4238-5506
Jane Hsieh http://orcid.org/0000-0002-0795-2771
Farnoosh Farahani http://orcid.org/0000-0002-3937-7708
S. Mohammad Alavinia http://orcid.org/0000-0002-5503-9362
Maryam Omidvar http://orcid.org/0000-0003-2415-8921
B. Catharine Craven http://orcid.org/0000-0001-8234-6803
References
- 1.Gunnewicht BR. Pressure sores in patients with acute spinal cord injury. J Wound Care. 1995;4(10):452–4. doi: 10.12968/jowc.1995.4.10.452 [DOI] [PubMed] [Google Scholar]
- 2.Krause JS, Saunders LL.. Health, secondary conditions, and life expectancy after spinal cord injury. Arch Phys Med Rehabil. 2011;92(11):1770–5. doi: 10.1016/j.apmr.2011.05.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Pressure Ulcer Advisory Panel – Pressure injury definition. 2016. Available from: https://www.npuap.org/resources/educational-and-clinical-resources/npuap-pressure-injury-stages/.
- 4.European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel. Pressure ulcer prevention: quick reference guide. Washington, DC: National Pressure Ulcer Advisory Panel; 2009 [cited 2001 November 20]. Available from http://wwwepuaporg/guidelines/Final_Quick_Preventionpdf.
- 5.Schubart JR, Hilgart M, Lyder C.. Pressure ulcer prevention and management in spinal cord-injured adults: analysis of educational needs. Adv Skin Wound Care. 2008;21(7):322–9. doi: 10.1097/01.ASW.0000323521.93058.47 [DOI] [PubMed] [Google Scholar]
- 6.Makhsous M, Rowles DM, Rymer WZ, Bankard J, Nam EK, Chen D, et al. . Periodically relieving ischial sitting load to decrease the risk of pressure ulcers. Arch Phys Med Rehabil. 2007;88(7):862–70. doi: 10.1016/j.apmr.2007.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sezer N, Akkus S, Ugurlu FG.. Chronic complications of spinal cord injury. World J Orthop. 2015;6(1):24–33. doi: 10.5312/wjo.v6.i1.24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ash D. An exploration of the occurrence of pressure ulcers in a British spinal injuries unit. J Clin Nurs. 2002;11(4):470–8. doi: 10.1046/j.1365-2702.2002.00603.x [DOI] [PubMed] [Google Scholar]
- 9.New PW, Rawicki HB, Bailey MJ.. Nontraumatic spinal cord injury rehabilitation: pressure ulcer patterns, prediction, and impact. Arch Phys Med Rehabil. 2004;85(1):87–93. doi: 10.1016/S0003-9993(03)00378-2 [DOI] [PubMed] [Google Scholar]
- 10.Richard-Denis A, Thompson C, Bourassa-Moreau E, Parent S, Mac-Thiong JM.. Does the acute care spinal cord injury setting predict the occurrence of pressure ulcers at arrival to intensive rehabilitation centers? Am J Phys Med Rehabil. 2016;95(4):300–8. doi: 10.1097/PHM.0000000000000381 [DOI] [PubMed] [Google Scholar]
- 11.Wang H, Niewczyk P, Divita M, Camicia M, Appelman J, Mix J, et al. Impact of pressure ulcers on outcomes in inpatient rehabilitation facilities. Am J Phys Med Rehabil. 2014;93(3):207–16. doi: 10.1097/PHM.0b013e3182a92b9c [DOI] [PubMed] [Google Scholar]
- 12.Salzberg C, Byrne D, Kabir R, Van Niewerburgh P, Cayten CG.. Predicting pressure ulcers during initial hospitalization for acute spinal cord injury. Wounds. 1999;11:45–57. [Google Scholar]
- 13.Citterio A, Franceschini M, Spizzichino L, Reggio A, Rossi B, Stampacchia G, et al. . Nontraumatic spinal cord injury: an Italian survey. Arch Phys Med Rehabil. 2004;85(9):1483–7. doi: 10.1016/j.apmr.2003.09.028 [DOI] [PubMed] [Google Scholar]
- 14.Lala D, Dumont FS, Leblond J, Houghton PE, Noreau L.. Impact of pressure ulcers on individuals living with a spinal cord injury. Arch Phys Med Rehabil. 2014;95(12):2312–9. doi: 10.1016/j.apmr.2014.08.003 [DOI] [PubMed] [Google Scholar]
- 15.Lourenco L, Blanes L, Salome GM, Ferreira LM.. Quality of life and self-esteem in patients with paraplegia and pressure ulcers: a controlled cross-sectional study. J Wound Care. 2014;23(6):331–4. 6–7. doi: 10.12968/jowc.2014.23.6.331 [DOI] [PubMed] [Google Scholar]
- 16.Richards S, Waites K, Chen Y, Kogos S, Schmitt MM.. The epidemiology of secondary conditions following spinal cord injury. Top Spinal Cord Inj Rehabil. 2004;10(1):15–29. doi: 10.1310/YXM3-85YW-8VUG-NNUR [DOI] [Google Scholar]
- 17.Chan B, Cadarette S, Wodchis W, Wong J, Mittmann N, Krahn M.. Cost-of-illness studies in chronic ulcers: a systematic review. J Wound Care. 2017;26(sup4):S4–S14. doi: 10.12968/jowc.2017.26.Sup4.S4 [DOI] [PubMed] [Google Scholar]
- 18.Rick Hansen Spinal Cord Injury Registry – a look at traumatic spinal cord injury in Canada in 2017. Vancouver, BC: RHI. 2018. Available from: http://rickhanseninstitute.org/images/stories/Article_PDFs/SCI_Report_dec9_web1.pdf.
- 19.Bolliger M, Blight AR, Field-Fote EC, Musselman K, Rossignol S, Barthelemy D, et al. . Lower extremity outcome measures: considerations for clinical trials in spinal cord injury. Spinal Cord. 2018;56(7):628–42. doi: 10.1038/s41393-018-0097-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Accreditation Agreement Canada Qmentum; standards, spinal cord injury rehabilitation services, for surveys starting after: January 01, 2018; Ver. 12A. https://accreditation.ca/standards/.
- 21.Rintala D, Garber S L, Friedman J, Ann Holmes S.. Preventing recurrent pressure ulcers in veterans with spinal cord injury: impact of a structured education and follow-up intervention. Arch Phys Med Rehabil. 2008;89(8):1429–41. doi: 10.1016/j.apmr.2008.01.015 [DOI] [PubMed] [Google Scholar]
- 22.Evidence to improve care, quality standards, pressure injuries. In: Care MoHaL-T, (ed.) Health Quality Ontario; 2017.
- 23.Scovil C, Flett H, McMillian L, Leber D, Brown J, Burns A, editors. Pressure ulcer risk assessment in an inpatient spinal cord injury (SCI) rehabilitation program: implementation science. Poster session presented at: American Congress of Rehabilitation Medicine. Arch Phys Med Rehabil. 2013;94(10):e22.
- 24.Houghton PE, Campbell KE.. CPG Panel, Canadian best practice guidelines for the prevention and management of pressure ulcers in people with spinal cord injury. A resource handbook for clinicians. 2013. Available from http://onf.org/system/attachments/168/original/Pressure_Ulcers_Best_Practice_Guideline_Final_web4.pdf.
- 25.Consortium for spinal Cord medicine clinical practice guidelines. pressure ulcer prevention and treatment following spinal cord injury: a clinical practice guideline for health-care professionals. 2nd ed. Consortium for Spinal Cord Medicine, Administrative and financial support provided by Paralyzed Veterans of America; 2014. [DOI] [PubMed]
- 26.Scovil CY, Flett HM, McMillan LT, Delparte JJ, Leber DJ, Brown J, et al. . The application of implementation science for pressure ulcer prevention best practices in an inpatient spinal cord injury rehabilitation program. J Spinal Cord Med. 2014;37(5):589–97. doi: 10.1179/2045772314Y.0000000247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gabison S, Mathur S, Nussbaum EL, Popovic MR, Verrier MC.. The Relationship between pressure offloading and ischial tissue health in individuals with spinal cord injury: an exploratory study. J Spinal Cord Med. 2019;42(Suppl 1):S186–S195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Swaine JM, Breidahl W, Bader DL, Oomens CWJ, O'Loughlin E, Santamaria N, et al. . Ultrasonography detects deep tissue injuries in the subcutaneous layers of the buttocks following spinal cord injury. Top Spinal Cord Inj Rehabil. 2018;24(4):371–8. doi: 10.1310/sci17-00031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McPheeters ML, Kripalani S, Peterson NB, Idowu RT, Jerome RN, Potter SA, et al. . Quality improvement interventions to address health disparities. Closing the quality gap: revisiting the state of the science. Evidence Report No. 208. (Prepared by the Vanderbilt University Evidence-based Practice Center under Contract No. 290-2007-10065.) AHRQ Publication No. 12-E009-EF. Rockville, MD: Agency for Healthcare Research and Quality. www.effectivehealthcare.ahrq.gov/reports/final.cfm. August 2012. [PMC free article] [PubMed]
- 30.Scovil CY, Delparte JJ, Walia S, Flett HM, Guy SD, Wallace M, et al. . Implementation of pressure injury prevention best practices across six Canadian rehabilitation sites: results from the spinal cord injury knowledge mobilization network. Arch Phys Med Rehabil. 2019;100(2):327–35. doi: 10.1016/j.apmr.2018.07.444 [DOI] [PubMed] [Google Scholar]
- 31.Craven BC, Balioussis C, Noonan V, Biering-Sørensen F, Campbell K, Gagnon D, et al. . Spinal Cord Injury: A Manifesto for Change: Toronto Rehabilitation Institute-University Health Network; 2014. Available from: http://idapt.com/research/scimanifesto.
- 32.Craven BC, Verrier M, Balioussis CWD, Hsieh J, Noonan V, et al. . Rehabilitation environmental scan atlas: capturing capacity in Canadian SCI rehabilitation: Rick Hansen Institute; 2012. Available from: http://rickhanseninstitute.org/images/stories/ESCAN/RHESCANATLAS2012WEB_2014.pdf.
- 33.Idvall E, Rooke L, Hamrin E.. Quality indicators in clinical nursing: a review of the literature. J Adv Nurs. 1997;25(1):6–17. doi: 10.1046/j.1365-2648.1997.1997025006.x [DOI] [PubMed] [Google Scholar]
- 34.Selim AJ, Berlowitz DR, Fincke G, Rosen AK, Ren XS, Christiansen CL, et al. . Risk-adjusted mortality rates as a potential outcome indicator for outpatient quality assessments. Med Care. 2002;40(3):237–45. doi: 10.1097/00005650-200203000-00007 [DOI] [PubMed] [Google Scholar]
- 35.Alavinia S, Hitzig S, Farahani F, Flett H, Bayley M, Craven B.. Prioritization of rehabilitation domains for establishing spinal cord injury high performance indicators using a modification of the Hanlon method: SCI-High Project. J Spinal Cord Med. 2019;42(Suppl 1):S43–S50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Craven B, Alavinia S, Wiest M, Farahani F, Hitzig S, Flett H, et al. . Methods for development of structure, process and outcome indicators for prioritized spinal cord injury rehabilitation domains: SCI-High Project. J Spinal Cord Med. 2019;42(Suppl 1):S51–S67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mainz J. Developing evidence-based clinical indicators: a state of the art methods primer. Int J Qual Health Care. 2003;15(Suppl 1):i5–11. doi: 10.1093/intqhc/mzg084 [DOI] [PubMed] [Google Scholar]
- 38.Houghton P. The E-Stim collaboration project: a national pressure ulcer implementation program. Wound Care Canada. 2018;16(1):44–8. Available from: https://www.woundscanada.ca/docman/public/wound-care-canada-magazine/2018-16-no1/1270-wcc-summer-2018-v16n1-final-p-44-49-e-stim/file. [Google Scholar]
- 39.Rick Hansen Spinal Cord Injury Registry V3.0 Pressure Injury Form (Draft CI-Pressure Injuries-MULT): Rich Hansen Institute; 2018.
- 40.National Pressure Ulcer Advisory Panel (NPUAP) announces a change in terminology from pressure ulcer to pressure injury and updates the stages of pressure injury 2016, April 13. Available from: http://www.npuap.org/national-pressure-ulcer-advisory-panel-npuap-announces-a-change-in-terminology-from-pressure-ulcer-to-pressure-injury-and-updates-the-stages-of-pressure-injury/.
- 41.Craven BC, Verrier M, Balioussis C, Dalton W, Hsieh J, Noonan V, et al. . Rehabilitation Environmental scan atlas: capturing capacity in Canadian SCI rehabilitation, skin integrity. Rick Hansen Institute; 2012. Available from: http://168.144.170.22/research/scimanifesto/H__Skin_Integrity/.
- 42.Langley GL, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP.. The improvement guide: a practical approach to enhancing organizational performance. 2nd ed San Francisco: Jossey-Bass Publishers; 2009. [Google Scholar]
- 43.Byrne CA, O'Keeffe DT, Donnelly AE, Lyons GM.. Effect of walking speed changes on tibialis anterior EMG during healthy gait for FES envelope design in drop foot correction. J Electromyogr Kinesiol. 2007;17(5):605–16. doi: 10.1016/j.jelekin.2006.07.008 [DOI] [PubMed] [Google Scholar]
- 44.Hsieh J, McIntyre A, Wolfe DL, Lala D, Titus L, Campbell K, et al. . SCIRE spinal cord injury rehabilitation evidence, pressure ulcers following spinal cord injury. Available from: https://scireproject.com/wp-content/uploads/pressure_ulcers.pdf.
- 45.Bloemen-Vrencken JH, de Witte LP, Post MW, van den Heuvel WJ.. Health behaviour of persons with spinal cord injury. Spinal Cord. 2007;45(3):243–9. doi: 10.1038/sj.sc.3101967 [DOI] [PubMed] [Google Scholar]
- 46.Verschueren JH, Post MW, de Groot S, van der Woude LH, van Asbeck FW, Rol M.. Occurrence and predictors of pressure ulcers during primary in-patient spinal cord injury rehabilitation. Spinal Cord. 2011;49(1):106–12. doi: 10.1038/sc.2010.66 [DOI] [PubMed] [Google Scholar]