Abstract
Context: Spinal cord injury (SCI) presents numerous physiological, psychosocial, and environmental complexities resulting in significant healthcare system resource demands.
Objective: To describe the current health system surveillance mechanisms in Ontario, Canada and highlight gaps in health surveillance among adults with SCI across their lifespan.
Methods: A review of administrative data sources capturing SCI-specific information took place via internet searching and networking among SCI rehabilitation and health services experts with emphasis on functionality, health service utilization, and quality of life data.
Results: The review identified a distinct paucity of data elements specific to the health surveillance needs of individuals with SCI living in the community. The gaps identified are: (1) a lack of data usability; (2) inadequate linkage between available datasets; (3) inadequate/infrequent reporting of outcomes; (4) a lack of relevant content/patient-reported outcomes; and, (5) failure to incorporate additional data sources (e.g. Insurance datasets).
Conclusion: Currently, SCI-specific health data is disproportionately weighted towards the first 3–6 months post injury with detailed data regarding pre-hospital care, acute management and rehabilitation, but little existing infrastructure supporting community-based health surveillance. Given this reality, the bolstering of meaningful community health surveillance of this population across the lifespan is needed. Addressing the identified gaps in health surveillance must inform the creation of a comprehensive community health dataset incorporating patient-reported outcome measures and enabling linkage with existing administrative and/or clinical databases. A future harmonized data surveillance strategy would, in turn, positively impact function, health services, resource utilization and health-related quality of life surveillance.
Keywords: Spinal cord injury, Health care utilization, Community health, Service delivery gaps, Health data
Introduction
In Canada, there are over 86,000 individuals living with spinal cord injury (SCI) with an estimated 3,675 new cases per year of either traumatic or non-traumatic etiology.1 Ontario makes up approximately 38% of the Canadian general population. Thus, it is estimated that there are 32,500 individuals in Ontario with SCI and 1,400 new cases per year in the province.2 These relatively low incidence and prevalence rates translate into a disproportionately high and sizeable health system economic impact with an estimated lifetime economic burden of $1.5–$3.0 million per person, depending on the neurologic level and severity of the individual’s injury.3 Further, individuals with SCI elicit approximately eight times the direct health care expenditures when compared to their non-SCI, age-matched peers.4
SCI typically results in a heterogeneous constellation of motor, sensory and autonomic impairments which impact an individual’s ability to: move about their home and community, bathe and dress independently, regulate their body temperature, heart rate, blood pressure, and breathing; and, impair their voluntary control of bladder and bowel evacuation. The clinical expression of these physiological impairments varies based on the neurological level of injury and severity of injury. Variable expression of secondary health conditions presents a significant challenge when describing the SCI population and their population-specific health care needs across the lifespan particularly given the frequency of multimorbidity.
Although SCI is relatively rare,1 it is nevertheless a complex condition that contributes to significant morbidity5,6 and health system economic3 impact due to the myriad of frequently occurring secondary health conditions which are defined as “physical or psychological health conditions that are influenced directly or indirectly by the presence of a disability or underlying physical impairment”.7 The concept of “multimorbidity” has been defined as “any combination of chronic diseases with at least one other disease (acute or chronic) or biopsychosocial factor, including the social network, the burden of diseases, health care consumption, and individual coping style” impacting the health of patients with SCI.8,9 This manuscript describes the current state of community health data collection and highlights current gaps in health surveillance among adults with SCI across their lifespan.
After the onset of traumatic SCI, individuals are typically immobilized prior to transfer to a local Emergency Department or regional trauma center via emergency medical services, and then admitted to a Level I trauma center for definitive imaging and surgical management of the cord injury and other trauma-related impairments.10 Once medically stable, individuals are transferred to a tertiary SCI rehabilitation hospital for rehabilitation.11,12 In order to achieve improved neurological outcomes, this surgical management should take place within 24 h of SCI onset.13 The processes for detection of non-traumtic SCI and transfer to a tertiary spine center are not well delineated within the health system prior to neurosurgical intervention and relevant data among this population is scarce. There have been several recent efforts to address ICD coding for patients with non-traumatic SCI and facilitate case finding and health surveillance for this population nationally and internationally.14–16 This acute post-operative phase of injury management is associated with a Canadian median rehabilitation onset of 26–30 days for those with traumatic injury prior to rehabilitation admission to a tertiary rehabilitation facility.17,18 Recently published examinations from multiple sites across Canada involving >1000 individuals with traumatic SCI, revealed that median rehabilitation length of stay, is 78–79 days (Interquartile Range 64–68 days).17,18
During the inpatient phases of injury management and rehabilitation, patients receive a variety of health services which are captured by existing provincial and national administrative databases, and/or related clinical or research databases. In Ontario, these databases include the Rick Hansen Spinal Cord Injury Registry (RHSCIR) (http://rickhanseninstitute.org/work/our-projects-initiatives/rhscir), the Discharge Abstract Database (DAD) (https://www.cihi.ca/en/discharge-abstract-database-metadata), the National Rehabilitation Reporting System (NRS) (https://www.cihi.ca/en/national-rehabilitation-reporting-system-metadata), the National Ambulatory Care Reporting System (NACRS) (https://www.cihi.ca/en/national-ambulatory-care-reporting-system-metadata), the Electronic Medical Record Administrative data Linked Database (EMRALD), and the Ontario Health Insurance Plan (OHIP) (https://www.ices.on.ca/Data-and-Privacy/ICES-data) databases. These datasets provide extensive and extremely valuable information to understand the health system trajectories and inform health policy. They enable us to understand the resource requirements for patients with SCI within the health system across prehospital, inpatient acute, post-acute and rehabilitation settings. These systems provide limited to no information regarding the outcome of patients following discharge from the inpatient tertiary SCI rehabilitation center without linkage to the aforementioned databases.
Upon discharge from tertiary rehabilitation, a majority of patients with SCI transition into the community and then rely on management of their conditions through their primary care physician and related electronic medical record (EMR).10 Where available and accessible, they use outpatient rehabilitation services and specialist care from providers with subspecialty expertise in spinal cord injury care (i.e. neurosurgery, physiatry, neuro-urology, sexologist, neurology, neuro-psychiatry, physical and occupational therapy, etc.). While there are mechanisms in place to follow individuals as they transition into the community through community-based organizations such as Spinal Cord Injury Ontario (SCIO) and the RHSCIR database, these data elements are limited to those who consent to enrollment and, in the case of RHSCIR, primarily serve those with traumatic SCI. In the case of SCIO data, it reflects only those who were referred and have registered as SCIO clients and are utilizing their peer support or attendant care services. Within the RHSCIR community follow-up data set, dropout rates are high after the transition to the community due to relocation and loss of valid contact information, and interim morbidity.19 The post-inpatient phase of SCI rehabilitation service, therapys and management will, in all likelihood, represent the greatest portion of an individual’s remaining lifetime requiring a significant amount of specialized care to maintain the individual’s health, functional independence, overall well-being, and quality of life while living dwelling in the community.
As an individual’s duration of injury increases, they are likely to experience comorbid secondary health conditions which increase in number and severity. These include but are not limited to cardiovascular disease, type 2 diabetes, dyslipidemia, sexual dysfunction, reduced tissue integrity, urinary tract infections, and increased risk of pneumonia, urinary tract infections, social isolation, and depression, and an overall reduction in health-related quality of life.5,20–22
Individuals with SCI have a 2.6 times higher risk of rehospitalization compared to an age and gender-matched non-SCI cohort. Approximately 36% of individuals with SCI require hospital readmission within the first 12 months post discharge from inpatient rehabilitation.23–25 Further, individuals with SCI spend an average of 3.3 more days in a hospital, and require approximately 30 times more hours of home care, when compared to non-SCI age-matched controls.23 The provision of these community health services often comes from a variety of different practitioners; within the first 12 months of injury, individuals with SCI typically require approximately 30 physician visits and 17 specialist visits within the first year post-discharge from inpatient rehabilitation.26,27 It is important to note, however, that these trends have not been investigated or reported for individuals living with SCI in the community beyond the first 12 months post-discharge.
Despite the lack of long term surveillance at the community level, evidence suggests that there is a significant ongoing need for care beyond the first 12 months given that a majority of individuals report a mean of seven secondary health conditions are reported at 5–8 years post injury28 and low mean health utility index scores (mean HUI-Mark III was 0.24 (range, –0.28 to 1.00)) are reported among individuals with chronic SCI living in Ontario.6 Further, increases in attendant care services and health condition severity have been reported to increase in the last 10 years prior to death among aging Ontarians with SCI.29 The multi-faceted health care demands, difficulties in physically accessing some diagnostic and clinical services, and the current uncoordinated approach to care creates a lack of “crosstalk” between primary care, specialist practitioners and interprofessional rehabilitation teams.30 This likely creates opportunity for the provision of redundant and/or counterproductive services which may result in unmet patient needs, reduced safety, increased patient burden, and excessive health resource utilization.31,32 Given the complexity and diversity of care and resource requirements among individuals with SCI following discharge from inpatient rehabilitation, a greater emphasis should be placed on understanding this complex, yet critically important, phase of care for individuals with SCI.
SCI can occur in individuals living in rural (all territory outside an urban area33) or urban (areas with a population of at least 1000 and a population density of 400 persons per square kilometer33) locations, although some people living with SCI in a rural location move to an urban center within 1 year after injury to access health care and attendant care services, most remain in their rural area.34 While the needs of many individuals with SCI may be similar, the aforementioned variability in impairment, community setting and access to services may create additional circumstances and inequity that impacts the quality, form and utilization of health services in either a positive or negative way.8,25,35,36 Strategies to alleviate additional undue hardship for individuals living in more isolated locations with limited or insufficient primary care access, should be a significant priority among SCI service organizations.37 That said, the success of any such data strategy necessitates a high quality, current and accurate set of community-based health data to portray the location, current health and health services, and quality of life among individuals with SCI living in communities across the province of Ontario. Data of this nature could be used to identify service gaps and/or cost-effective opportunities to enhance health care services and systems while decreasing morbidity and mortality.
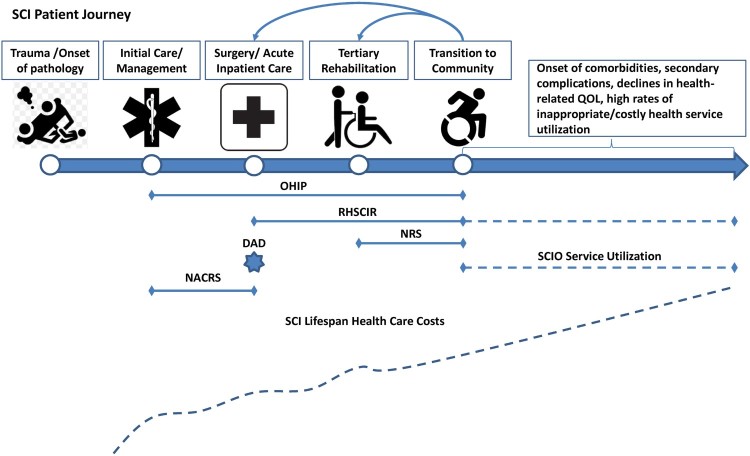
Figure 1 depicts the common experience of someone with SCI and highlights the currently available administrative health databases with this journey. After reviewing Fig. 1, it will be readily apparent that there is a disproportionate weighting of administrative resources allocated to the early stages of this journey before community re-entry, which is problematic given the health service and resource demands and health care costs associated with tertiary-rehabilitation and post-rehabilitation care among this population.25–27,38 While some data may be captured post-discharge from tertiary rehabilitation, it may only reflect the utilization of services by a small catchment of individuals living in the community proximal to the tertiary rehabilitation setting. The overarching motivation for this paper is to describe the current state and highlight the opportunities to enhance the nature, volume, and quality of community health data that is collected to ultimately enhance the quality of care provided to individuals with SCI living in the community through enhanced health system surveillance.
Figure 1.
The SCI patient journey from injury onset to transition back into the community. OHIP, Ontario Health Insurance Plan; RHSCIR, Rick Hansen Spinal Cord Injury Registry; NRS, National Rehabilitation Reporting System; DAD, Discharge Abstract Database; NACRS, National Ambulatory Care Reporting System; SCIO, Spinal Cord Injury Ontario; QOL, quality of life.
Summary of current community health surveillance data
To fully understand the current state of community health data surveillance, a non-systematic, yet thorough review in search of existing databases that capture information among individuals with SCI took place. Given that reports on community health data sources can appear in the gray literature (i.e. government reports, SCI epidemiological reports), this review took place via internet searching using various combinations of the terms; Canada, Ontario, spinal cord injury, health services, health surveillance, health databases, health datasets, community health, health care utilization, health-related quality of life, function. Word-of-mouth networking among experts in the field of SCI rehabilitation and health services also took place and relied upon the authors’ wealth of accumulated experience performing clinical research in the area of spinal cord injury. A review of all data holdings of the Canadian Institute for Health Information (CIHI) and the Institute for Clinical Evaluative Sciences (IC/ES), the known primary entities capturing administrative health data in Ontario (and the rest of Canada), was conducted to identify the community health care administrative data sources available for interactions between the Ontario population and the publicly funded health care system. The Institute for Clinical Evaluative Sciences has a data repository that collects all publicly funded health care administrative data in Ontario. Variables that may be important for health services research, as determined by the authors were identified in each data source and reported. These include; the source of patient data, the perspective of the data source (i.e. health system vs practitioner vs patient), method for capturing health care utilization, the detection of comorbidities, and the collection of data related to impairment, function and health-related quality of life. The information collected from this review is summarized in Table 1.
Table 1. Summary of identified health datasets collecting SCI-specific information pertaining to health care utilization and overall health/function.
| Dataset | Source | Perspective | Health care utilization | Comorbidities | Impairment/function/HRQOL | |
|---|---|---|---|---|---|---|
| Impairment/function | HRQOL | |||||
| Canadian Institute for Health Information (CIHI) | ||||||
| NRS | Inpatient rehabilitation | Health System | Yes – Rehabilitation Patient Grouping | Yes – Admit/discharge comorbidities DHC codes | Yes – FIM | |
| NACRS | Ambulatory care, including Emergency Dept. visits | Health System | Yes – Resource intensity weights | Yes – Other problem – ICD-10 codes | No | |
| DAD | Acute inpatient hospital | Health System | Yes – Resource intensity weights | Yes – Diagnosis code – ICD-10 | No | |
| CCRS | Complex continuing care/long term care | Health System | Yes – Resource intensity weights | Yes – tracked comorbidities | Yes – ADLs, signs and symptoms | |
| Homecare database | Home care | Health System | Yes – Services used | No | Yes – Diagnosis code – ICD-10 | |
| OMHRS | Inpatient mental health hospital visits | Health System | Yes – SCIPP grouper (Inpatient psychiatry classification system) | No | Yes – ADLs, Self-rated health, signs and symptoms | |
| Ontario Ministry of Health and Long-Term Care/Institute for Clinical Evaluative Sciences (IC/ES) | ||||||
| OHIP | Physician visits/ laboratory and diagnostic tests | Practitioner | Yes – OHIP fee code | No | Yes – OHIP diagnosis code | |
| ODB | Drugs for those over 65 + those on social assistance programs | Health System | Yes – drug identification number | No | No | |
| Assistive Devices Program | Assistive devices | Health System | No | Yes – functional status – manual wheelchair | ||
| Other | ||||||
| EMRALD | Physician visits | Practitioner | No | No | No | |
| RHSCIR | Acute care + rehabilitation + “follow-up” | Patient | Yes | Yes, secondary comorbidities tracked | Yes – FIM | LiSat-11, SF36 |
| SCICS* (published 2014) | Community survey | Patient | No | Yes, secondary complications tracked | Yes | LiSat-11, social participation, needs/ perceptions of health |
| SCIO Service Utilization Data | SCIO Client services | Patient / Community Service Provider | SCIO Services only | No | Yes – Client disability questionnaire | Social determinants of health questionnaire |
Notes: HRQOL, health-related quality of life; NRS, National Rehabilitation reporting System; FIM, functional independence measure; DHC, diagnostic health condition; NACRS, National Ambulatory Care Reporting System; ICD-10, International Classification of Diseases; DAD, Discharge Abstract Database; CCRS, Continuing Care Reporting System; ADL, activities of daily living; OMHRS, Ontario Mental Health Reporting System; SCIPP, System for Classification of In-Patient Psychiatry; OHIP, Ontario Health Insurance Plan; ODB, Ontario Drug Benefit; EMRALD, Electronic Medical Record Administrative data linked Database; RHSCIR, Rick Hansen Spinal Cord Injury Registry; LiSat 11, Lifestyle Satisfaction questionnaire; SF-36, short form health survey; SCICS, Spinal Cord Injury Community Survey; SCIO, Spinal Cord Injury Ontario.
*The SCICS is an isolated project and not an ongoing database.
Datasets
Several administrative databases collect information on publicly-funded health care services provided to Ontario residents. These databases include health care provided to individuals receiving: ambulatory care, emergency department care, hospital care as an inpatient or resident of a long-term care facility, physician services, drugs and home care services. All data are collected from CIHI or the Ministry of Health and Long-term Care (MOHLTC) and sent to IC/ES for evaluation purposes. The identified databases from CIHI are the NRS, NACRS, DAD, Continuing Care Reporting System (CCRS), Ontario Mental Health Reporting System (OMHRS), and the Homecare Database. From MOHLTC, we identified the Ontario Health Insurance Plan (OHIP) database, the Ontario Drug Benefit (ODB) database, and the Ontario Assistive Devices Program. Another growing dataset is EMRALD which is populated by the electronic medical records (EMRs) from a large number of participating primary care physicians. The Greater Toronto Area (GTA) Rehab Network is made up of both publicly funded hospitals and community-based organizations with a goal of improving the planning and delivery of rehabilitative care. The GTA Rehab Network collects data pertaining to ambulatory outpatient rehabilitative care but it is not specific to those with SCI and was therefore not included in Table 1. Tertiary rehabilitation hospitals throughout the province also report visits to the Ministry of Health. Finally, data is collected by service-based organizations such as SCIO who are mandated to capture information related to individuals currently using their services, hours of care, days waited for service initiation, plus number of face-to-face and non-face-to-face visits. SCIO also captures information related to community-based goals, disability characteristics and social determinants of health among those who consent to register for their services. These centralized data repositories enable information from each of the databases to be linked through individual’s health card numbers. This allows for longitudinal health care utilization evaluation at the patient level.
Various other publicly funded service organizations provide health care services to individuals in the community, but do not formally provide data to CIHI or IC/ES through the MOHLTC. These include organizations that offer attendant care, home and vehicle modification services such as the March of Dimes, the GTA Rehab Network, and the provincial SCI organizations that originated from the Canadian Paraplegic Association, such as SCIO. CIHI and IC/ES also does not have data for special programs within the MOHLTC such as the Direct Funding program (https://www.dfontario.ca/). This program provides publicly-funded attendant care services to individuals with disabilities by allowing the individual the ability to interview and hire their attendant care providers.
In addition to the health care provided through public funds, individuals may receive additional services and equipment through a third-party insurance provider depending on the circumstances surrounding the etiology of injury. If an individual was injured as a result of an automobile collision, they may receive funding for some health care services through their automobile insurance. All health care resulting from workplace-related injuries are compensated by the Workplace Safety and Insurance Board (WSIB). Injuries that are not automobile or workplace related may be covered by employer-sponsored or independently purchased private insurance. The range of services and level of care provided by the different insurance providers differ. Currently, data from third-party insurance providers are not linked with publicly funded services.
Data gaps
After reviewing the characteristics and data elements presented in Table 1 and cross-referencing the depiction of a SCI patient’s journey presented in Fig. 1, it is abundantly clear that there is a disconnect between the data that are currently being captured and the lifespan health system demands of individuals with SCI. There is an apparent need to develop a new health data surveillance strategy for persons with SCI living in the community that includes patient-reported outcome measures to better reflect the needs and perceptions of those with SCI. The majority of current data sets are almost exclusively populated using inpatient data while those with a community follow-up component are limited in number of respondents and in the number of potentially valuable data elements collected. Furthermore, from the review of community health datasets, five critical gaps relating to the surveillance of community health data, utilization patterns, and overall health and wellbeing of individuals with SCI were identified. These key gaps include; the usability health data in existing databases, a lack of linkage between health databases created and maintained by different sources, a lack of consistent reporting of information from existing databases, inadequate content which lacks PROMs, and a failure to take advantage of existing avenues for data collection currently being done by third-party health service organizations, such as insurers.
Gap 1: data usability
The data collected in the reviewed databases are of limited use among researchers and health service providers who focus on working with individuals with SCI living in the community. Using RHSCIR as an example, there are several factors limiting its scalability and ability to work as an effective post-discharge dataset. These barriers include that RHSCIR captures data pertaining to traumatic SCI etiology among consenting individuals, and although there are 31 RHSCIR sites in Canada, an individual living with SCI in the community may not re-connect with these health care facilities if their place of residence is outside of the facility’s established catchment. In turn, this may limit the opportunity to re-engage participants and conduct follow-up data collection. Furthermore, RHSCIR was developed using the International Classification of Functioning, Disability and Health as the foundation and thus currently has a clinical outcome focus, as opposed to a “health systems approach” to data collection, reporting and evaluation.
Conversely, typical administrative data sources, such as NRS, NACRS and DAD, are neither created, nor implemented from a patient perspective and have glaring omissions including but not limited to PROMs. These three aforementioned databases also lack accuracy in identifying cohorts and fail to capture important functional information outside of FIM scores in the inpatient settings. Despite the potential to inform health service utilization during the early stages of the SCI patient journey, these data sources do not adequately provide health data that can be applied to the needs of individuals with SCI after their transition into the community.
Furthermore, these datasets are not freely available and require a lengthy and onerous process that demands considerable expertise to access or link the data. This process presents a significant barrier limiting the usability of existing datasets in Ontario.
Other datasets, such as the WSIB claims database, typically are not designed with clinical or health outcomes research in mind and may not be suitable stand-alone sources of relevant information to dictate policy change at the community level,39 although they may inform the role of case management services in directing resources.
Gap 2: linkage
Despite the fact that there are several different datasets collecting health information early on in a SCI patient’s journey, linkage between the measured variables and comprehensive datasets reflecting these data from individuals post-discharge from their tertiary rehabilitation stay is notably missing from the current health surveillance infrastructure.
In Ontario, the primary health care administrative datasets are all located and maintained by the Institute for Clinical Evaluative Sciences (IC/ES). This centralized location provides the ability to link different databases through an individual’s health card number. This linkage helps to optimize reporting of administrative health data and mutually enhances each database’s ability to portray health system outcomes. There are no such processes in place, however, that reflects the utilization and health service needs of individuals with SCI living in the community.
It is important to note, however, that other data sources, such as RHSCIR, are created and maintained throughout the province in various locations by different information custodians. There are currently no established long term agreements in place for these datasets to link with those housed at IC/ES. There is an opportunity to develop a long term strategy linking RHSCIR to other administrative provincial datasets that includes passive data collection, or facilitated sharing at structured time intervals. The current lack of routine data linkage is likely undermining the ability for health researchers and policy makers to fully understand the complete scope of the health system needs of individuals with SCI living in the community in terms of utilization patterns, cost, presence of comorbidities, functional outcomes, and overall quality of life. Given that analyses by the various data custodians/owners tend to occur in isolation and without broad collaboration, a comprehensive understanding of health and health care use by individuals with SCI in the community remains elusive.
Gap 3: reporting of outcomes
The primary impetus for this manuscript is to describe the general lack of published literature on the health care utilization of individuals with SCI living in the community in Ontario, and the expert opinions of the authors related to a paucity of community health databases that collect health utilization, functionality, comorbidity, wellness and quality of life information on an ongoing basis. Take, for example, the Spinal Cord Injury Community Survey (SCICS) which collected data from 2011 to 2012.40 The SCICS provides a great deal of insight into the demographics, injury and functionality characteristics, as well as perceived and tangible needs among individuals with SCI in Canada40 but there has been no follow-up administration of this survey.
Even among the databases which are more thoroughly populated on an ongoing basis, such as the DAD and NRS, there is a lack of consistent reporting on health care utilization and the quality of health for individuals requiring health care services. This is because the primary purpose of this information is for hospital funding and monitoring of health system performance.
Gap 4: content/relevant outcomes
Review of the content from Table 1 has also revealed a glaring lack of PROMs which can inform policy decisions relevant to the needs of individuals with SCI living in the community and should be included in the evolution towards a learning health system.41 Additionally, there is a striking need to harmonize the data collected and prioritize key aspects of health data so that redundancies can be avoided and to ensure a complete picture of health service utilization, cost, presence of comorbidities, care needs, functionality, and quality of life among individuals living with SCI in the community.
Gap 5: untapped resources
Beyond the databases described in Table 1, there are a number of other potentially valuable sources of data, which may, if deployed properly, provide additional relevant information related to the health service utilization and patient needs of individuals with SCI living in the community. Despite the potential limitations of health insurance data,39 it should be noted that health insurance providers may possess a wealth of data regarding utilization of health services, and their associated costs, among individuals with SCI living in the community.
Discussion
The highlighted gaps in data to describe SCI care represent the findings from a non-systematic, yet insightful review of the current health data surveillance mechanisms in place in Ontario. These gaps should be interpreted as opportunities to address critical infrastructure and to develop strategies that will improve our ability to capture and evaluate relevant health outcomes, service utilization patterns, and economic impact of individuals with SCI living in the community.
Data usability and content
In order to facilitate improvements in health care for individuals with SCI living in the community, there must be significant changes made to the usability of the current health information that is collected. Usability should be at the forefront of health database design so that captured information can be analyzed and applied for multiple purposes. The usability of health data is closely intertwined with the outcome measures collected. The lack of relevant content (i.e. FIM not SCIM) and patient-reported outcome measures persist throughout the current datasets, capturing information among individuals with SCI living in the community. This identified gap aligns with a recent report from the Rick Hansen Institute highlighting the current state of Access to Care and Timing for individuals with SCI.42 While RHSCIR provides a solid framework and does attempt to capture relevant data across the care continuum, collection of data post-discharge from inpatient RHSCIR sites remains a challenge due to consent constraints, relocation following rehabilitation discharge and morbidity. In other Canadian provinces, RHSCIR data infrastructure is utilized to collect data reflecting the use of community care and services while Ontario currently does not adequately capture this information.42 At the community level, there are several barriers to primary care that exist, contributing to the high rates of inappropriate health care utilization. These barriers include a lack of physicians, inaccessibility of physician offices and a lack of physician specialization related to the complex condition of SCI.43,44 In Ontario, the Mobility Clinic, part of the Centre for Family Medicine (http://family-medicine.ca/clinics-services-programs-and-events/clinics-3/mobility-clinic/) is exploring and implementing methodologies to eliminate some of these barriers through various telemedicine approaches. The gathering of relevant patient-related outcome measures would offer a great deal of insight into the current challenges faced by individuals with SCI living in the community and may inform innovative strategies to circumvent the abovementioned barriers.
Linkage and untapped resources
Despite the fact that there is robust infrastructure in place that collects information from time of injury until time of discharge from tertiary rehabilitation, the current health system has not taken the necessary steps to continue this surveillance of health information and service utilization to fully encompass the entire patient journey. In order to describe the usage of health services, the prevalence of secondary complications, functional outcomes and quality of life among individuals with SCI living in the community, this existing infrastructure must be extended beyond its current boundaries and be receptive to a harmonized approach that will link various data sources collecting information reflecting the health, needs, functionality, and perceptions of the SCI community.
Through the input from existing data sources that are currently not linked to the databases described in Table 1, such as those created and populated by insurers, there is an opportunity to dramatically increase our ability to inform public policy and health service delivery in the community if appropriately adapted for research purposes or linked to other complementary datasets.
Reporting of outcomes
Ongoing reporting of relevant health information and utilization patterns among individuals with SCI living in the community would provide a tremendous amount of value to health practitioners, researchers, and policy-makers. Given the ongoing evolution of the health care landscape in Ontario, it is imperative that current data is used when making critical decisions pertaining to the many facets of SCI care such as, self-management recommendations and clinical best practices.
The lack of re-administration of the SCICS is indeed disappointing given the potential for a recurring cycle of administration. That would allow the creation of a longitudinal dataset with the ability to inform health policy and practice to enhance the health and quality of life among individuals with SCI nationally.
For instance, the National Spinal Cord Injury Statistical Center (NSCISC) in the US publishes annual reports on demographic statistics for individuals treated for SCI at any of the US SCI model system hospitals (https://www.nscisc.uab.edu/) in a manner similar to that utilized by RHSCIR (https://rickhanseninstitute.org/work/our-projects-initiatives/rhscir). Long-term follow-up of all individuals allows the NSCISC to also report on long-term impacts on marital status, occupational status, costs and life expectancy. Although annual updates would represent an ideal scenario, it is neither likely, nor feasible to assume that this could take place given the logistical barriers and costs to implementing recurring cycles of survey administration. That said, reports every 4–5 years would provide an immense boost to the current state of community health data.
Also, advancing upon the recommendations made by an International Spinal Cord Society (ISCoS) advisory panel to inform the inclusion of SCI-specific data elements in international data sets,45 an internationally collaborative effort has commenced to develop what is being called the International Spinal Cord Injury (InSCI) community survey. The goal of this is to collect internationally comparable data from individuals with SCI living in the community pertaining to their function, health maintenance and subjective well-being.46 While only in its early stages of development and implementation, the InSCI should garner much attention and provide highly relevant information that will inform an Ontario strategy for monitoring community health data among the Canadian SCI population versus other settings globally. The European Multicenter Study about Spinal Cord Injury (EMSCI) does collect some follow-up data related to neurological and functional outcomes but these are collected primarily during inpatient rehabilitation with the final time point being 48 weeks post injury. These other US and ISCoS initiatives signal that the lack of community follow-up data is not unique to Ontario.
In order to fully understand the health care landscape and make informed policy changes, it is critically important, in an increasingly resource constraint health care system, to identify the profile of individuals who require extensive health care services. Previous studies have observed that a small proportion of the population contributes to a substantial percentage of health care expenditures. In Ontario, the top 5% of health care users account for 55% of all health care spending.47 Acute inpatient hospital, inpatient rehabilitation, complex continuing care, day surgery, physician services and prescription drug combine for over 90% of total health care costs.48 Similar patterns of large health care utilization in a small proportion of the population have also been observed in different Canadian provinces, the United States and Australia.49–52 High health care utilization has been associated with increased age, higher co-morbidity burden, poorer self-reported health status and lower income,47 many of which are experienced by individuals with SCI. Ongoing efforts to focus on the characteristics of this small cohort of high-cost users and their care demands will help health care decision-makers develop strategies to improve health service delivery in this population and potentially realize significant health care savings.
Limitations
This review may be limited by its narrow scope and the decision to focus exclusively on the community health data surveillance in the province of Ontario. That said, Ontario is where the majority of Canadians with SCI live. Ontario is accepted amongst many members of the Canadian SCI research community to act as a microcosm for what happens in the rest of Canada, but do the number of patients is often evident in Ontario data prior to other provinces and Ontario has an overall health systems data infrastructure that is more comprehensive than that which exists in the majority of other provinces. After reviewing the existing data surveillance infrastructure across Canada, the majority of provinces are using CIHI data holdings plus varying forms of data collection/management related to health services, physician billing and prescription drug data that are equivalent to or less comprehensive than that which is currently used in Ontario.
Further, there is a well-documented paucity of post-discharge data being a common theme in the SCI field internationally. For example, the annual report from the National Spinal Cord Injury Statistical Center in the United States showed that 17% of participants were lost after one year of follow-up and 64.2% were lost at year 20 post injury.53 In Australia, there is a spinal cord injury registry comparable to RHSCIR but it does not have a post-rehabilitation discharge component and only captures relevant information from the initial and subsequent hospital admissions from designated spinal units.54
Another potential limitation of this review is the non-systematic approach taken to populate the list of datasets included in Table 1. Given that datasets are not a searchable item using conventional systematic approaches, the authors have relied upon their subject-matter expertise and connections to populate this table and believe that it is a thorough and comprehensive depiction of the current landscape of health data surveillance in Ontario.
Moving towards a new strategy
Individuals with SCI, depending on their age at the time of injury onset, may spend decades in this post-rehabilitation phase of living and, during this time, are highly susceptible to the development of secondary health conditions, comorbid chronic diseases, and are vulnerable to adverse psychosocial changes due to small social networks. For these reasons, it has been shown that rates of rehospitalization and inappropriate emergency department visits are quite high among individuals with SCI living in the community.23–25 These expenditures, coupled with the amount of time individuals spend in this phase of their journey translate to a disproportionate weighting of health care costs associated with post-rehabilitation care. It is critically important to address this gap in health data surveillance. We need to establish a robust and comprehensive database that includes PROMs with ongoing follow-up utilizing existing infrastructure to bolster our understanding of the needs and overall health and well-being of individuals with SCI living in the community.
There are several barriers to the success of a harmonized data surveillance strategy. First, there is a question of who will lead this process? A project of this magnitude would require a steering committee consisting of relevant stakeholders and data custodians/owners. However, there still needs to be a primary organization that will be responsible for initiating the project, gathering all stakeholders and providing ground-level oversight. Second, is whether or not there is stable leadership from data custodians/owners that see the value of this strategy? This is important to ensure ongoing data collection from a consistent dataset. Third, is there dedicated and consistent funding to ensure that data linkages and collection will continue uninterrupted over a long period of time? Fourth, how will consensus be obtained among all stakeholders (researchers, practitioners, policy makers, insurance companies, community health service employees, and individuals with SCI) regarding the key data to be collected and shared and assure role clarity throughout the process? The Spinal Cord Injury Research Evidence (SCIRE) platform should be thoroughly referenced throughout the process of decision-making related to relevance and psychometric validation of outcome measures (https://scireproject.com/). Finally, privacy is also a major barrier to the collection of community health data and communication between datasets. In order to have community health datasets “talk” to each other, there must be a rigorous evaluation of privacy standards and meticulous steps taken to ensure that patient/individual health information is appropriately protected.
One avenue to enhance the quality of health service data surveillance for individuals with SCI living in the community would be the establishment of a provincially mandated data collection strategy that expands the scope of data collection beyond that which is captured by the primary administrative datasets while still maintaining connectivity through Health Card numbers or EMR. Such a strategy would capture a great deal of information related to the utilization, quality, and economic impact of health and community services relevant to the care needs of individuals with SCI.
The potential implications of enhanced community health data may also inspire local research and practice initiatives on a smaller scale. Examination into the use of health services, presence of comorbid conditions, and overall health-related quality of live among individuals living with SCI in the community may inform the content and delivery of specialized outpatient services, identify underserviced local subgroups, and help improve timely access to relevant health care. A comprehensive set of linked community health data can also enhance health services research studies by expanding the scope of the research question. For instance, a study examining the health care cost of a community-dwelling SCI cohort with neuropathic pain published in this issue present the total cost of health care reported by the study participants. The inclusion of community health data could be used to confirm participant reports and provide additional context of the health care delivered including the specific services provided, reimbursement amounts billed to the payer and the identity of the health care payer (i.e. public, private insurance).
Furthermore, a harmonized data surveillance system could provide opportunity to enhance the coordination of community-based health care avoiding potential redundancies in service delivery, examine the utilization of community-based infrastructure such as fitness facilities, evaluate the effectiveness of self-management strategies or interventions, and potentially capture different perspectives of the various stakeholders involved with the provision of health services and care to individuals with SCI living in the community.
Looking forward, through the use of technology, and a coordinated approach to standardize community data sources, the development of a strategy that will provide linkage between existing datasets could provide valuable insight into the health of individuals with SCI and increase our understanding of how they utilize health services. One such way to accomplish this is to implement and routinely evaluate health indicators among persons with SCI. This approach has been advocated by the Access to Care and Timing working group10 and others advocating for health system transformation.55,56
The SCI-HIGH project is a bold initiative that has, with input from subject-matter experts and stakeholders from across Canada and through a systematic approach, identified structure, process and outcome indicators for 11 prioritized domains of rehabilitation.57 The provincial implementation of this project provides a mechanism through which consistent community health data can be collected and evaluated from a variety of sources across the province. Additionally, the VIP4SCI project is a virtual platform that, developed in concert with SCI Ontario and ForaHealthyMe Inc., allows individuals with SCI to connect with their circle of care through video conferencing and/or direct messaging in addition to providing them with vetted health information and goal setting tools. This platform could provide valuable infrastructure to a community health data surveillance strategy and a secure means through with data could be collected remotely via video conferencing between health care practitioners and patients with SCI. Both of the aforementioned projects are still in the early stages of implementation. With time, they will provide valuable information to facilitate health care decision making among both clinicians and individuals with SCI at the aggregate level to inform best-practices and resource allocations made by researchers and policy makers. Until that time, it is important to thoroughly examine the present data available for health care utilization among persons with SCI living in the community.
Broadly speaking, the development of a harmonized data surveillance strategy would promote the creation of a learning health system. According to the Agency for Healthcare Research and Quality, a learning health system takes place when “internal data and experience are systematically integrated with external evidence and that knowledge is put into practice”.58 This should be understood as a cycle, where the changes to practice, that are informed by internal data, perpetuate the accumulation of new data and experiences. Through the incorporation of big-data analytics approaches and machine learning, a tremendous opportunity exists to apply novel analytics approaches can tap into previously unused data sources and apply new tools in an effort to strengthen the foundations of a learning health system.59 A recent McMaster University Health Forum (Hamilton, Ontario) developed an Ontario-specific definition of a rapid-learning health system as one that combines both a health and research system with a scope that ranges from self-management to the clinical interaction to the level of the government.60 This system is patient-centered (patient includes current and potential users of the health care system and their family and caregivers), data is evidence-driven, supported by appropriate decision supports and is surrounded by an environment of continued rapid learning and improvement.60 The continuous collection of important near real-time data with advanced analytics and frequent reporting cycles will provide stakeholders with valuable insight on patterns and trends in health care utilization over time. This will guide decision-makers towards necessary modifications of current health care practices or the introduction of timely innovative strategies to improve health. Over time, with the advancement of sophisticated learning predictive models and guided artificial intelligence tools, improvements to health care delivery can potentially become proactive as opposed to reactive, thus providing individuals the opportunity to access the necessary care before they spiral into costly, high health care system users.
Conclusion
The authors fully acknowledge the challenges associated with collecting accurate and reliable data that incorporates a variety of stakeholder perspectives, from the macro to micro system perspectives from within the health system including patient-reported outcome measures from various community settings or though linkage to electronic health records.41 That said, it must be strongly reinforced that there is a profound opportunity, if executed properly, to create an up-to-date comprehensive community health dataset that allows for linkage with existing administrative databases and addition of value-laden data elements as specified in the aforementioned discussion. Carrying data forward into a single dataset would preclude the current process and resource duplication for re-collecting the same data among individuals with SCI. The established dataset could then be used to inform health practices for providers, characterize utilization and resource requirements for administrators and policy makers, and serve to measure progress toward stakeholder priorities in a transparent manner on behalf of governmental organizations and patient and stakeholder coalitions.
Funding Statement
This work has been supported by the SCI-HIGH project team funded by the Rick Hansen Institute [grant number G2015-33], Ontario Neurotrauma Foundation, and the Toronto Rehab Foundation. Dr Rowan acknowledges fellowship salary support from Spinal Cord Injury Ontario through the Ontario Centres of Excellence (grant number 27020) and the Toronto Rehab Foundation, Dr Chan acknowledges support from an Ontario Neurotrauma Foundation mentor-mentee training award [grant number 2017-RHI-FELLOW-1021].
Acknowledgements
The authors would like to express their appreciation to Sheila Casemore of SCIO and Joanne Zee from University Health Network for their contributions to manuscript preparation. Dr Jaglal acknowledges support from the Toronto Rehab Foundation as the Institute Chair for the University of Toronto. Dr Craven acknowledges support from the Toronto Rehab Foundation as the KITE, Toronto Rehab- University Health Network Chair in Spinal Cord Injury Rehabilitation.
Disclaimer statements
Contributors None.
Conflicts of interest One of the authors acknowledges receipt of consulting fees from the Rick Hansen Institute. The other authors have no conflicts to declare.
ORCID
Chip P. Rowan http://orcid.org/0000-0002-0552-3439
Brian C.F. Chan http://orcid.org/0000-0001-5037-0446
Susan B. Jaglal http://orcid.org/0000-0002-2930-1443
B. Catharine Craven http://orcid.org/0000-0001-8234-6803
References
- 1.Noonan VK, Fingas M, Farry A, Baxter D, Singh A, Fehlings MG, et al. Incidence and prevalence of spinal cord injury in Canada: a national perspective. Neuroepidemiology. 2012;38(4):219–26. doi: 10.1159/000336014 [DOI] [PubMed] [Google Scholar]
- 2.Statistics Canada. Table 17-10-0009-01 population estimates, quarterly. 2018. Available from https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000901.
- 3.Krueger H, Noonan VK, Trenaman LM, Joshi P, Rivers CS.. The economic burden of traumatic spinal cord injury in Canada. Chronic Dis Inj Can. 2013;33(3):113–22. [PubMed] [Google Scholar]
- 4.Chan BC, Cadarette SM, Wodchis WP, Krahn MD, Mittmann N.. The lifetime cost of spinal cord injury in Ontario, Canada: a population-based study from the perspective of the public health care payer. J Spinal Cord Med. 2018;42(2):1–10. doi: 10.1080/10790268.2018.1527078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saunders LL, Clarke A, Tate DG, Forchheimer M, Krause JS.. Lifetime prevalence of chronic health conditions among persons with spinal cord injury. Arch Phys Med Rehabil. 2015;96(4):673–9. doi: 10.1016/j.apmr.2014.11.019 [DOI] [PubMed] [Google Scholar]
- 6.Craven C, Hitzig SL, Mittmann N.. Impact of impairment and secondary health conditions on health preference among Canadians with chronic spinal cord injury. J Spinal Cord Med. 2012;35(5):361–70. doi: 10.1179/2045772312Y.0000000046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jensen MP, Molton IR, Groah SL, Campbell ML, Charlifue S, Chiodo A, et al. Secondary health conditions in individuals aging with SCI: terminology, concepts and analytic approaches. Spinal Cord. 2012;50(5):373–8. doi: 10.1038/sc.2011.150 [DOI] [PubMed] [Google Scholar]
- 8.Craven BC. The tipping point: perspectives on SCI rehabilitation service gaps in Canada. Int J Phys Med Rehabil. 2013;01(08):1–4. doi: 10.4172/2329-9096.1000165 [DOI] [Google Scholar]
- 9.Le Reste JY, Nabbe P, Manceau B, Lygidakis C, Doerr C, Lingner H, et al. The European general practice research network presents a comprehensive definition of multimorbidity in family medicine and long term care, following a systematic review of relevant literature. J Am Med Dir Assoc. 2013;14(5):319–25. doi: 10.1016/j.jamda.2013.01.001 [DOI] [PubMed] [Google Scholar]
- 10.Fehlings MG, Cheng CL, Chan E, Thorogood NP, Noonan VK, Ahn H, et al. Using evidence to inform practice and policy to enhance the quality of care for persons with traumatic spinal cord injury. J Neurotrauma. 2017;34(20):2934–40. doi: 10.1089/neu.2016.4938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Noonan VK, Chan E, Santos A, Soril L, Lewis R, Singh A, et al. Traumatic spinal cord injury care in Canada: a survey of Canadian centres. J Neurotrauma. 2017;34(20):2848–2855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parent S, Barchi S, LeBreton M, Casha S, Fehlings MG.. The impact of specialized centers of care for spinal cord injury on length of stay, complications, and mortality: a systematic review of the literature. J Neurotrauma. 2011;28(8):1363–70. doi: 10.1089/neu.2009.1151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fehlings MG, Vaccaro A, Wilson JR, Singh A DWC, Harrop JS, et al. Early versus delayed decompression for traumatic cervical spinal cord injury: results of the surgical timing in acute spinal cord injury study (STASCIS). PloS one. 2012;7(2):e32037. doi: 10.1371/journal.pone.0032037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jaglal SB, Voth J, Guilcher SJT, Ho C, Noonan VK, McKenzie N, et al. Creation of an algorithm to identify non-traumatic spinal cord dysfunction patients in Canada using administrative health data. Top Spinal Cord Inj Rehabil. 2017;23(4):324–32. doi: 10.1310/sci2304-324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guilcher SJT, Voth J, Ho C, Noonan VK, McKenzie N, Thorogood NP, et al. Characteristics of non-traumatic spinal cord dysfunction in Canada using administrative health data. Top Spinal Cord Inj Rehabil. 2017;23(4):343–52. doi: 10.1310/sci2304-343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.New PW, Guilcher SJT, Jaglal SB, Biering-Sorensen F, Noonan VK, Ho C.. Trends, challenges, and opportunities regarding research in non-traumatic Spinal Cord dysfunction. Top Spinal Cord Inj Rehabil. 2017;23(4):313–23. doi: 10.1310/sci2304-313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Craven BC, Kurban D, Farahani F, Rivers CS, Ho C, Linassi AG, et al. Predicting rehabilitation length of stay in Canada: it's not just about impairment. J Spinal Cord Med. 2017;40(6):676–86. doi: 10.1080/10790268.2017.1368962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheng CL, Plashkes T, Shen T, Fallah N, Humphreys S, O’Connell C, et al. Does specialized inpatient rehabilitation affect whether or not people with traumatic spinal cord injury return home? J Neurotrauma. 2017;34(20):2867–76. doi: 10.1089/neu.2016.4930 [DOI] [PubMed] [Google Scholar]
- 19.Patsakos E, Brisbois L, Farahani F, Kaiser A, Craven BC.. Implementation of longitudinal study participant retention methods &development of a standardized operating procedure to minimize participant attrition: rick hansen spinal cord injury registry (RHSCIR) (abstract). J Spinal Cord Med. 2017;40(6):837. [Google Scholar]
- 20.Ullrich PM, Smith BM, Blow FC, Valenstein M, Weaver FM.. Depression, healthcare utilization, and comorbid psychiatric disorders after spinal cord injury. J Spinal Cord Med. 2014;37(1):40–5. doi: 10.1179/2045772313Y.0000000137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boakye M, Leigh BC, Skelly AC.. Quality of life in persons with spinal cord injury: comparisons with other populations. J Neurosurg Spine. 2012;17(Suppl. 1):29–37. doi: 10.3171/2012.6.AOSPINE1252 [DOI] [PubMed] [Google Scholar]
- 22.McKinley WO, Jackson AB, Cardenas DD, DeVivo MJ.. Long-term medical complications after traumatic spinal cord injury: a regional model systems analysis. Arch Phys Med Rehabil. 1999;80(11):1402–10. doi: 10.1016/S0003-9993(99)90251-4 [DOI] [PubMed] [Google Scholar]
- 23.Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias N, Svenson LW, et al. Utilization of health services following spinal cord injury: a 6-year follow-up study. Spinal Cord. 2004;42(9):513–25. doi: 10.1038/sj.sc.3101629 [DOI] [PubMed] [Google Scholar]
- 24.DeJong G, Tian W, Hsieh CH, Junn C, Karam C, Ballard PH, et al. Rehospitalization in the first year of traumatic spinal cord injury after discharge from medical rehabilitation. Arch Phys Med Rehabil. 2013;94(Suppl. 4):S87–97. doi: 10.1016/j.apmr.2012.10.037 [DOI] [PubMed] [Google Scholar]
- 25.Jaglal SB, Munce SE, Guilcher SJ, Couris CM, Fung K, Craven BC, et al. Health system factors associated with rehospitalizations after traumatic spinal cord injury: a population-based study. Spinal Cord. 2009;47(8):604–9. doi: 10.1038/sc.2009.9 [DOI] [PubMed] [Google Scholar]
- 26.Guilcher SJ, Munce SE, Couris CM, Fung K, Craven BC, Verrier M, et al. Health care utilization in non-traumatic and traumatic spinal cord injury: a population-based study. Spinal Cord. 2010;48(1):45–50. doi: 10.1038/sc.2009.78 [DOI] [PubMed] [Google Scholar]
- 27.Munce SE, Guilcher SJ, Couris CM, Fung K, Craven BC, Verrier M, et al. Physician utilization among adults with traumatic spinal cord injury in Ontario: a population-based study. Spinal Cord. 2009;47(6):470–6. doi: 10.1038/sc.2008.173 [DOI] [PubMed] [Google Scholar]
- 28.Hitzig SL, Campbell KA, McGillivray CF, Boschen KA, Craven BC.. Understanding age effects associated with changes in secondary health conditions in a Canadian spinal cord injury cohort. Spinal Cord. 2010;48(4):330–5. doi: 10.1038/sc.2009.135 [DOI] [PubMed] [Google Scholar]
- 29.Pentland W, McColl MA, Rosenthal C.. The effect of aging and duration of disability on long term health outcomes following spinal cord injury. Paraplegia. 1995;33(7):367–73. [DOI] [PubMed] [Google Scholar]
- 30.Milligan J, Lee J.. Enhancing primary care for persons with spinal cord injury: more than improving physical accessibility. J Spinal Cord Med. 2016;39(5):496–9. doi: 10.1179/2045772315Y.0000000041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McColl MA, Shortt S, Godwin M, Smith K, Rowe K, O’Brien P, et al. Models for integrating rehabilitation and primary care: a scoping study. Arch Phys Med Rehabil. 2009;90(9):1523–31. doi: 10.1016/j.apmr.2009.03.017 [DOI] [PubMed] [Google Scholar]
- 32.McColl MA, Aiken A, McColl A, Sakakibara B, Smith K.. Primary care of people with spinal cord injury: scoping review. Can Fam Physician. 2012;58(11):1207-16, e626–e35. [PMC free article] [PubMed] [Google Scholar]
- 33.Statistics Canada Population Centre and Rural Area Classifications 2016. Ottawa, ON, Canada: Statistics Canada; 2017. [Google Scholar]
- 34.Glennie RA, Batke J, Fallah N, Cheng CL, Rivers CS, Noonan VK, et al. Rural and urban living in persons with spinal cord injury and comparing environmental barriers, their health, and quality-of-life outcomes. J Neurotrauma. 2017;34(20):2877–82. doi: 10.1089/neu.2016.4931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bell N, Kidanie T, Cai B, Krause JS.. Geographic variation in outpatient health care service utilization after spinal cord injury. Arch Phys Med Rehabil. 2017;98(2):341–6. doi: 10.1016/j.apmr.2016.09.130 [DOI] [PubMed] [Google Scholar]
- 36.Goodridge D, Rogers M, Klassen L, Jeffery B, Knox K, Rohatinsky N, et al. Access to health and support services: perspectives of people living with a long-term traumatic spinal cord injury in rural and urban areas. Disabil Rehabil. 2015;37(16):1401–10. doi: 10.3109/09638288.2014.972593 [DOI] [PubMed] [Google Scholar]
- 37.Patients First: Action Plan for Health Care. Toronto, ON: Ontario Ministry of Health and Long Term Care; 2015. [Google Scholar]
- 38.Munce SE, Wodchis WP, Guilcher SJ, Couris CM, Verrier M, Fung K, et al. Direct costs of adult traumatic spinal cord injury in Ontario. Spinal Cord. 2013;51(1):64–9. doi: 10.1038/sc.2012.81 [DOI] [PubMed] [Google Scholar]
- 39.Riis V, Jaglal S, Boschen K, Walker J, Verrier M.. Can administrative claim file review be used to gather physical therapy, occupational therapy, and psychology payment data and functional independence measure scores? Implications for rehabilitation providers in the private health sector. Physiother Can. 2011;63(3):324–33. doi: 10.3138/ptc.2010-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Noreau L, Noonan VK, Cobb J, Leblond J, Dumont FS.. Spinal cord injury community survey: a national, comprehensive study to portray the lives of Canadians with spinal cord injury. Top Spinal Cord Inj Rehabil. 2014;20(4):249–64. doi: 10.1310/sci2004-249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ahmed S, Ware P, Gardner W, Witter J, Bingham CO III, Kairy D, et al. Montreal accord on patient-reported outcomes (PROs) use series – paper 8: patient-reported outcomes in electronic health records can inform clinical and policy decisions. J Clin Epidemiol. 2017;89:160–7. doi: 10.1016/j.jclinepi.2017.04.011 [DOI] [PubMed] [Google Scholar]
- 42.Dvorak MF, Cheng CL, Fallah N, Santos A, Atkins D, Humphreys S, et al. Spinal cord injury clinical registries: improving care across the SCI care continuum by identifying knowledge gaps. J Neurotrauma. 2017;34(20):2924–33. doi: 10.1089/neu.2016.4937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McColl MA, Forster D, Shortt SE, Hunter D, Dorland J, Godwin M, et al. Physician experiences providing primary care to people with disabilities. Healthc Policy. 2008;4(1):e129–47. [PMC free article] [PubMed] [Google Scholar]
- 44.McColl MAH, Shortt S, Hunter D, Dorland J, Godwin M, Rosser W, et al. Access and quality of primary care for people with disabilities: a comparison of practice factors. J Disabil Policy Stud. 2010;21(3):131–40. doi: 10.1177/1044207310376739 [DOI] [Google Scholar]
- 45.Biering-Sorensen F, Charlifue S, DeVivo M, Noonan V, Post M, Stripling T, et al. International spinal cord injury data sets. Spinal Cord. 2006;44(9):530–4. doi: 10.1038/sj.sc.3101930 [DOI] [PubMed] [Google Scholar]
- 46.Fekete C, Post MW, Bickenbach J, Middleton J, Prodinger B, Selb M, et al. A structured approach to capture the lived experience of spinal cord injury: data model and questionnaire of the international spinal cord injury community survey. Am J Phys Med Rehabil. 2017;96(2 Suppl. 1):S5–S16. doi: 10.1097/PHM.0000000000000622 [DOI] [PubMed] [Google Scholar]
- 47.Rosella LC, Fitzpatrick T, Wodchis WP, Calzavara A, Manson H, Goel V.. High-cost health care users in Ontario, Canada: demographic, socio-economic, and health status characteristics. BMC Health Serv Res. 2014;14:532. doi: 10.1186/s12913-014-0532-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Homenauth E, Graves E, Ishiguro L, Saskin R, Schull M, Wodchis W, et al. Examination of high-cost patients in Ontario. Int J Popul Data Sci. 2018;3(4):359. [Google Scholar]
- 49.Roos N, Burchill C, Carriere K.. Who are the high hospital users? A Canadian case study. J Health Serv Res Policy. 2003;8(1):5–10. doi: 10.1177/135581960300800104 [DOI] [PubMed] [Google Scholar]
- 50.Reid R, Evans R, Barer M, Sheps S, Kerluke K, McGrail K, et al. Conspicuous consumption: characterizing high users of physician services in one Canadian province. J Health Serv Res Policy. 2003;8(4):215–24. doi: 10.1258/135581903322403281 [DOI] [PubMed] [Google Scholar]
- 51.Calver J, Brameld KJ, Preen DB, Alexia SJ, Boldy DP, McCaul KA.. High-cost users of hospital beds in Western Australia: a population-based record linkage study. Med J Aust. 2006;184(8):393–7. [DOI] [PubMed] [Google Scholar]
- 52.Berk ML, Monheit AC.. The concentration of health care expenditures, revisted. Health Aff. 2001;20(2):9–18. doi: 10.1377/hlthaff.20.2.9 [DOI] [PubMed] [Google Scholar]
- 53.National Spinal Cord Injury Statistical Center 2018 Annual Statistical Report for the Spinal Cord Injury Model Systems. Birmingham, AL: National Spinal Cord Injury Statistical Center; 2018. [Google Scholar]
- 54.Welfare AIoHa Spinal Cord Injury Australia 2014–2015. Canberra, Australia: Australian Institute of Health and Welfare; 2018. [Google Scholar]
- 55.Fooks C, Goldhar J, Wodchis WP, Baker GR, Coutts J, Brown AS, et al. Effective approaches to integrating care: a three-part series. Healthc Q. 2018;21(2):18–22. doi: 10.12927/hcq.2018.25627 [DOI] [PubMed] [Google Scholar]
- 56.Embuldeniya G, Kirst M, Walker K, Wodchis WP.. The generation of integration: the early experience of implementing bundled care in Ontario, Canada. Milbank Q. 2018;96(4):782–813. doi: 10.1111/1468-0009.12357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Craven BC, Alavinia SM, Wiest MJ, Farahani F, Hitzig SL, Flett H, et al. Methods for development of structure, process and outcome indicators for prioritized spinal cord injury rehabilitation domains: SCI-high Project. J Spinal Cord Med. 2019;42(Suppl 1):S51–S67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Agency for Healthcare Research and Quality Learning Health Systems. Rockville, MD, USA: Agency for Healthcare Research and Quality; 2017. Available from https://www.ahrq.gov/professionals/systems/learning-health-systems/index.html. [Google Scholar]
- 59.Krumholz HM. Big data and new knowledge in medicine: the thinking, training, and tools needed for a learning health system. Health Aff (Millwood). 2014;33(7):1163–70. doi: 10.1377/hlthaff.2014.0053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lavis JN, Gauvin F-P, Reid R, Bullock H, Wodchis WP, Hayes A.. A Rapid Synthesis: Creating a Rapid-learning Health System in Ontario. Hamilton, Canada: McMaster University; 2018. [Google Scholar]