Abstract
Anti-CD19 chimeric antigen receptor T cell (CAR-T) therapy has changed the typical outcomes of relapsed/refractory B-cell leukemia and lymphoma. However, treatment effectiveness for patients with relapsed/refractory B-cell non-Hodgkin lymphoma has been less satisfactory compared with patients with B-cell acute lymphoblastic leukemia. The present study described a case of refractory follicular lymphoma. A high expression of programmed cell death 1 (PD-1) was measured on CD3+ T cells (80.90%) in peripheral blood samples obtained from the patient enrolled in this study, indicating that treatment with autologous CAR-T 19 cell therapy may not be successful. Therefore, a therapy regimen consisting of CAR-T 19 cells in combination with a reduced dose of nivolumab (1.5 mg/kg) for PD-1 blockade was used. A low dose of PD-1 blockade therapy was used to reduce the adverse effects associated with the combination of a PD-1 inhibitor and CAR-T 19 cells. This salvage therapy resulted in remission that lasted for >10 months.
Keywords: chimeric antigen receptor, programmed cell death 1 blockade, programmed cell death 1 inhibitor, immunotherapy, lymphoma
Introduction
Although refined chemotherapy, including rituximab (an anti-CD20 monoclonal antibody), and autologous stem cell transplantation have improved the prognosis for B-cell non-Hodgkin lymphoma (B-NHL), patients with refractory B-NHL still have a poor prognosis (1,2). Approximately 19–26% of patients with follicular lymphoma (FL) receiving first-line immunochemotherapy with rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone (R-CHOP) experienced progression of disease within 24 months (2). Chimeric antigen receptor (CAR) T cells are a remedial treatment for these patients. Anti-CD19 CAR T cell (CAR-T 19) therapies have exhibited potent activity against numerous subtypes of B-NHL, including FL (3). Nivolumab, the human immunoglobulin G4 programmed death-1 (PD-1) immune checkpoint inhibitor antibody with high affinity to PD-1 receptors on T cells, could block their interaction with PD ligands 1 and 2 (PD-L1/PD-L2) and restore T-cell function (4). A significant association between the expression levels of PD-1 on T cells and the immunosuppression of T cells has previously been reported (5). A study that focused on the use of Nivolumab in a cohort of 10 patients with relapsed or refractory FL, reported the overall response rate was four patients (40%), and one achieved complete response (6). Meanwhile, PD-1 inhibitors may lead to an imbalance in immune tolerance and uncontrolled immune response, even fatal myocarditis (7). The present study describes a patient with successfully treated refractory FL, who received anti-CD19 CAR-T cells combined with decreased dose PD-1 inhibitor regimen.
Case report
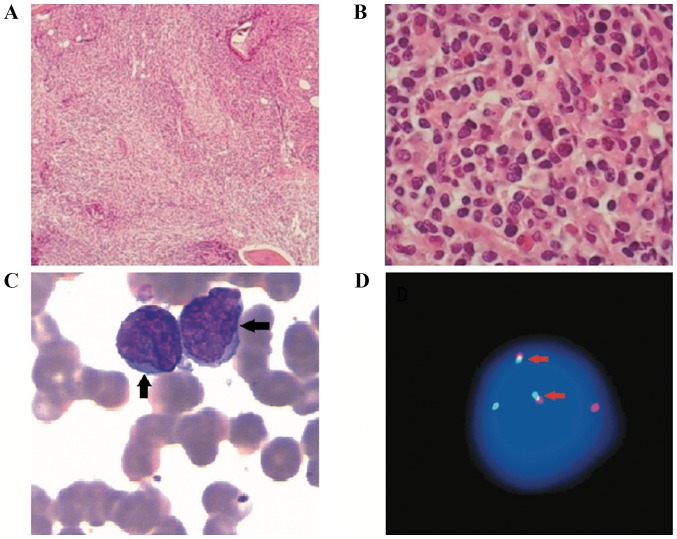
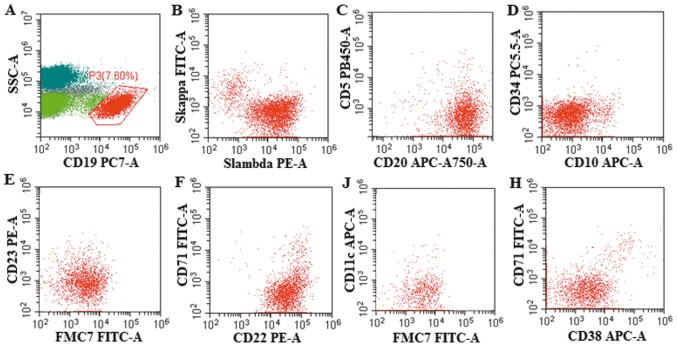
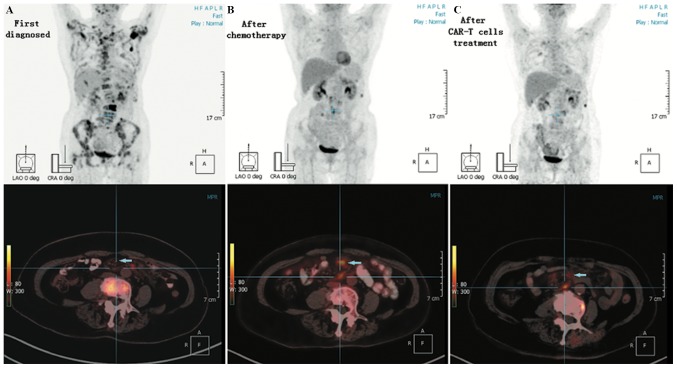
A 70-year-old female patient was admitted to the Tianjin First Central Hospital (Tianjin, China) in July 2017, presenting with fever and lower back pain, which had persisted for 10 days. A number of inpatient laboratory tests were performed. A bone marrow biopsy revealed lymphocyte dysplasia, small cell bodies, slightly irregular nuclei and thicker chromatin. The biopsy was fixed for 16–18 h with 10% formaldehyde, which was composed of 90 ml distilled water and 40% formaldehyde 10 ml and incubated for 18–20 h in Richman decalcification solution at room temperature which composed of 8% hydrochloric acid 40 ml and 10% formaldehyde 60 ml and embedded in paraffin. Subsequently, the 3-µm thin sections were cut and incubated with the following blocking reagents: Peroxide Block (ready to use; cat. no. DS9263; Leica Microsystems, Inc.) or EnVsion FLEX Peroxidase-Blocking Reagent (ready to use; cat. no. DM821; Dako; Agilent Technologies, Inc.), at room temperature for 3–5 min. Immunohistochemical staining was performed using commercially available primary antibodies at room temperature for 20–30 min according to the manufacturer's protocol to the following antigens: CD20 (1:100; cat. no. RTU-CD20-7D1-QH; Beijing Xin'ao Medical Technology Co., Ltd.), CD138 (1:100; cat. no. RTU-CD138-QH; Beijing Xin'ao Medical Technology Co., Ltd.), PAX-5 (1:100; cat. no. PM-0111; Shanghai Ruijing Biotechnology Co., Ltd.), CD10 (1:100; cat. no. CRM-0191; Shanghai Ruijing Biotechnology Co., Ltd.) and Bcl-2 (1:100; cat. no. RTU-BCL-2-486-QH; Beijing Xin'ao Medical Technology Co., Ltd.). All antibodies were observed under an Olympus light microscope at ×100, ×400 and ×1,000 magnification. Abnormal lymphocytes were observed in the bone marrow morphology (Fig. 1A-C). The results of the immunohistochemistry revealed that samples were CD20+, PAX5+, CD138+, CD10 partially positive and BCL2+. Approximately 107 nucleated cells were resuspended per 100 µl of buffer. The nucleated cells were incubated with the human FcR Blocking Reagent (dilution, ready to use; cat. no. 130-059-901, Miltenyi Biotec GmbH) in the dark at 2–8°C for 10 min No fixative was used for the bone marrow fluid samples. Staining was performed using commercially available antibodies at room temperature for 15 min according to the manufacturer's protocol: Anti-Skappa (ready to use; cat. no. 349516; BD Biosciences), anti-Slambda (ready to use; cat. no. 349516; BD Biosciences), CD19 (ready to use; cat. no. 130-113-647; Miltenyi Biotec GmbH), anti-CD34 (ready to use; cat. no. 348053; BD Biosciences), anti-CD10 (ready to use; cat. no. IM3633; Beckman Coulter, Inc.), anti-CD45 (ready to use; cat. no. 347463; BD Biosciences), anti-CD20 (ready to use; cat. no. 130-113-371; Miltenyi Biotec GmbH), anti-CD5 (ready to use; cat. no. 651154; BD Biosciences), anti-FMC7 (ready to use; cat. no. 340919; BD Biosciences), anti-CD23 (ready to use; cat. no. 341007; BD Biosciences), anti-CD71 (ready to use; cat. no. 347513, BD Biosciences), and anti-CD22 (ready to use; cat. no. 347573; BD Biosciences). Flow cytometry was performed using the Beckman Coulter cell telescopic flow cytometer and cells were assessed using CytExpert software (version 2.3.0.84; Beckman Coulter, Inc.). There were 7.6% abnormal monoclonal small B lymphocytes expressing CD19+, CD20+, CD22+, FMC7+, CD23−, CD38−, CD71−, CD5−, CD10−, CD11c− detected by flow cytometry in the bone marrow (Fig. 2). The IgH/BCL2 gene rearrange was 4.8% detected by fluorescence in situ hybridization (FISH), as analyzed by Tianjin Sino-US-Diagnostics Technology Co., Ltd. in bone marrow (Fig. 1D). MYD88-L265P gene examination was negative, detected by direct sequencing as performed by Tianjin Sino-US-Diagnostics Technology Co., Ltd.) (Fig. 1D). Positron emission tomography-computed tomography (PET-CT) examination revealed that bone density was not uniform, with partial bone destruction. Additionally, PET-CT revealed that bone metabolism was increased [L3 vertebral body local maximum standardized uptake value (SUVmax), 28.20; bilateral neck, right supraclavicular fossa enlarged lymph node SUVmax, 8.59] and that the metabolism of a soft tissue mass in the left mesenteric region of lumbar 2–3 disc level was increased (SUVmax, 8.57; Fig. 3A). The patient was diagnosed with advanced-stage IV FL, and treated with a combination regimen of rituximab, cyclophosphamide, doxorubicin, vincristine and prednisolone (R-CHOP). Following six cycles of R-CHOP treatment, the patient presented with generalized weakness, lower back pain and intermittent abdominal pain. No abnormal phenotype B lymphocytes were observed in the bone marrow at this time. A PET-CT examination revealed that the increased metabolism of the bones and the soft tissue mass in the left mesenteric region was decreased; however, the density of mesenteric lymph nodes at the lumbar 1–5 level was increased (SUVmax, 6.70; Fig. 3B). PET-CT examination revealed a maximum probability that the mesenteric lymph nodes were new lymphoma lesions. However, the patient had comorbid hypertension and diabetes, and was therefore unable to undergo a further biopsy to confirm this result. In addition, high expression of PD-1 in CD3+ T cells (80.76%) was detected in the peripheral blood samples from this patient by flow cytometry.
Figure 1.
Bone marrow morphology and IgH/BCL2 gene rearrange in situ hybridization (FISH). (A) Bone marrow biopsy. H&E and Periodic acid-Schiff staining indicated 90% nucleated cells in bone marrow hyperplasia (magnification, ×100). (B) Bone marrow biopsy. Abnormal lymphocyte hyperplasia was distributed focally. The lymphocytes had a small volume, reduced cytoplasm, round or irregular nuclei, and coarse chromatin (magnification, ×400). (C) Abnormal lymphocytes in Wright- and Giemsa-stained bone marrow. Abnormal lymphocytes were observed at high magnification, which were small blue cells with hyperchromatic nuclei little cytoplasm (magnification, ×1,000). (D) FISH (IgH/BCL2) gene rearrange. Count 500 interphase cells. Cytocell two-color labeling IgH/BCL2 probes were adopted. IgH(14q32) gene was marked in green. The BCL2(19q21) gene was marked in red. IgH/BCL2 fusion gene showed yellow or red-green superimposed signal. Normal signal characteristic is 2R2G, positive signal characteristic is 1R1G2F (G is green signal; R is the red signal; F is the fusion signal). IgH/BCL2 gene rearrange was 4.8% above the upper limit of normal value 2.67%.
Figure 2.
Flow cytometry examination. (A) There were 7.6% abnormal monoclonal small B lymphocytes expressing CD19+ detected by flow cytometry in the bone marrow, represented in red. The granulocytes are represented in dark green. Lymphocytes are represented in light green. (B-H), (C) CD20+ was represented in C. CD22+ was represented in F. FMC7+ was represented in E and J. CD38− was represented in H. CD5− was represented in C. CD10− was represented in D and CD11c− was represented in J. FITC, fluorescein isothiocyanate; FS, forward scatter; SSC, side scatter; PE, phycoerythrin; FMC, Flinders Medical Centre.
Figure 3.
PET-CT examination. (A) In the early diagnosis of the disease, the density of bones was not uniform and partial bone destruction was detected. Metabolism of the bones was increased. The SUVmax was 28.20 in the L3 vertebra. (B) PET-CT was reviewed after six cycles of rituximab, cyclophosphamide, doxorubicin, vincristine and prednisolone treatment. A new lymphoma lesion with SUVmax 8.67 was identified at the lumbar 1–5 level. (C) SUVmax of the lumbar 1–5 level was 6.36 following combination treatment with chimeric antigen receptor-T 19 cells and a reduced dose of a programmed cell death 1 blocker. PET-CT, positron emission tomography-computed tomography; SUVmax, maximum standardized uptake value.
The patient was diagnosed as having refractory lymphoma. The Eastern Cooperative Oncology Group Performance Status condition of the patient was 2 points with hypertension and diabetes (8). Following the initial R-CHOP, the patient was subsequently enrolled in a clinical trial at the Department of Hematology, Tianjin First Center Hospital with autologous anti-CD19 CAR-T cell expressing murine anti-CD19 single chain fragment variable and 4-1BB-CD3ζ costimulatory-activation domains (ChiCTR-ONN-16009862) in Jan 2018. The patient received lymphodepleting chemotherapy with fludarabine (30 mg/m2) and cyclophosphamide (400 mg/m2) daily from day −4 to day −2. Autologous anti-CD19 CAR-T cells were infused (1.3×107 cells/kg) on day 0. Because of the high expression of PD-1 in her peripheral blood, a combination of PD-1 blockade therapy and anti-CD19 CAR-T cell treatment was used to improve the efficacy of CAR-T cell therapy and to avoid anti-CD19 CAR-T cell treatment failure for the high expression of PD-1. As PD-1 blockade therapy may result in adverse effects especially for a 70-year-old patient, following the infusion of CAR-T 19 cells, a reduced dose of the PD-1 inhibitor Opdivo® (Nivolumab; 1.5 mg/kg) was administered on day 1. Other than fever and chills, a slight headache, mild low blood pressure and low blood oxygen, the combination therapy was well tolerated (Table I). These adverse effects abated after 14 days. No severe adverse effects of the PD-1 inhibitor were observed during the treatment period. The levels of PD-1 expression on T cells were monitored in peripheral blood samples from the patient and PD-1 expression was maintained at <5% over the following 60 days. The patient did not receive Nivolumab infusion in order to avoid adverse effects in the following therapy. The expression levels of PD-1 remained low for 6 months after the salvage treatment and the patient received no further treatment with a PD-1 inhibitor in the next round of therapy.
Table I.
Adverse effects following salvage treatment with anti-CD19 CAR-T cell combined with reduced-dose programmed cell death 1 blockade therapy.
| Time point (days) | ||||||
|---|---|---|---|---|---|---|
| Variable | −12 | 0 | 4 | 7 | 14 | 21 |
| Temperature (°C) | 36.7 | 38.0 | 37.6 | 38.8 | 36.4 | 36.5 |
| Chills | No | Yes (twice) | No | No | No | No |
| Blood pressure (mmHg) | 100/60 | 110/74 | 156/89 | 89/52 | 125/76 | 105/70 |
| Blood oxygen (%) | 95 | 93 | 91 | 84 | 89 | 94 |
| Neurological symptoms | – | N | Headache | Headache | N | N |
| White blood cell count (×109/l) | 4.27 | 2.37 | 1.04 | 4.01 | 2.55 | 5.16 |
| Hemoglobin (g/l) | 114 | 106 | 94 | 89 | 105 | 109 |
| Blood platelet count (×109/l) | 155 | 68 | 47 | 104 | 127 | 173 |
Other than fever and chills, a slight headache, mild low blood pressure and low blood oxygen, the combined therapy was well tolerated. The adverse effects were abated 14 days after the combined therapy. -, not applicable; N, normal.
After 30 days of combined therapy, significant clinical improvement was observed. The weakness and lower back pain gradually abated, and the patient resumed normal activities. A PET-CT examination was conducted and reviewed after 60 days of combined therapy. On the PET-CT scan, the density of mesenteric lymph nodes at the lumbar 1–5 level was decreased compared with that of the previous scan (Fig. 3C). The patient achieved complete response (CR) after 60 days of the anti-CD19 CAR-T cells combined with reduced-dose PD-1 blockade treatment. Until now, the patient maintained CR for 16 months following the combination therapy.
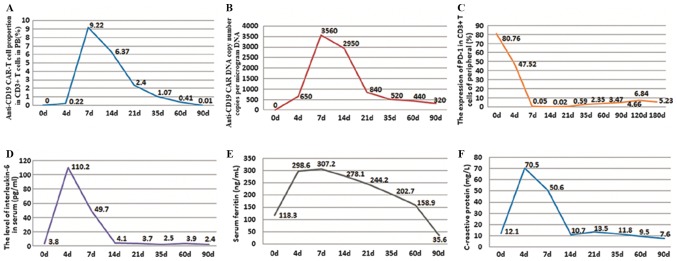
During treatment, the percentage of anti-CD19 CAR-T cells and the expression of PD-1 on CD3+ T cells in peripheral blood samples were detected by flow cytometry. The anti-CD19 CAR DNA was detected by the quantitative PCR in peripheral blood. DNA was obtained from the peripheral blood of the patient. The mRNA level of CD19 CAR was detected via reverse transcription-quantitative PCR (RT-qPCR) analysis. After 24 or 48 h of co-culture, total RNA was extracted from the cells using TRIzol® reagent (Invitrogen; Thermo Fisher Scientific, Inc.) as the template for the reactions. cDNA was synthesized with random primers from 10 µl total RNA with the aid of the Revert AidTM First Strand cDNA Synthesis kit (Fermentas; Thermo Fisher Scientific, Inc.). Following the protocol of the manufacturer, RT-qPCR was performed to characterize the mRNA levels of specific genes using Fast SYBR-Green Master Mix (Applied Biosystems; Thermo Fisher Scientific, Inc.) with a Biosystems StepOne Real-Time PCR machine (Applied Biosystems; Thermo Fisher Scientific, Inc). The primer sequences were restricted by company patents and could not be provided. Each PCR reaction was performed in triplicate as follows: In order to prevent any non-specific PCR, amplification and contamination was performed at 50°C for 2 min. Denaturation was performed at 95°C for 10 min. Annealing and elongation was performed with 35 cycles at 95°C for 15 sec and final extension was performed at 60°C for 1 min. The levels of interleukin-6 (IL-6) in the serum were detected via ELISA, using the one-step sandwich method (Shanghai Renjie Biotechnology Co., Ltd.). Other indicators were measured, including serum ferritin using the chemiluminescence immunoassay method (Beckman Inc.) and C-reactive protein (CRP) using the Latex enhanced immunoturbidimetric method, performed by the Nanjing Jiancheng Bioengineering Institute. The highest percentage of anti-CD19 CAR-T cells among CD3+ T cells was 9.22% on day 7 of combination therapy (day 0 was set as the day of CD19 CAR-T cell infusion). Approximately 90 days after combination therapy, the percentage of anti-CD19 CAR-T cells had decreased to ~0.01% (Fig. 4A). The highest anti-CD19 CAR DNA copy number was 3,560 copies/µg of DNA on day 7 after combination therapy. Approximately 90 days after therapy, it had decreased to 320 copies/µg of DNA (Fig. 4B). Notably, the expression of PD-1 in CD3+ T cells was decreased from 80.90% prior to combination therapy, which was 80.76% on day 0 of this therapy, to 0.05% on day 7 following combination therapy. PD-1 expression remained <5% over the following 60 days, and <7% for 180 days following the salvage treatment (Fig. 4C). The highest level of IL-6 in the serum was 110.2 pg/ml on day 4 of combination therapy. The level of IL-6 in serum had decreased to a normal level, whereas symptoms such as fever and headache had abated on day 14 (Fig. 4D). Serum ferritin and CRP levels had similar changes to IL-6 (Fig. 4E and F). Cytokine release syndrome following treatment with CAR-T 19 cells was grade II (5).
Figure 4.
Expression of PD-1 on anti-CD19 CAR T cells and cytokine secretion. (A) The highest percentage of anti-CD19 CAR T cells in CD3+ T cells was 9.22% on day 7 following combination therapy; these cells were almost undetectable on day 90. (B) The highest anti-CD19 CAR DNA copy number was 3,560 copies/µg DNA on day 7 and was decreased to 320 copies on day 90. (C) The expression of PD-1 in CD3+ T cells decreased from 80.76%, detected on the day 0 of the combination therapy, to 0.05% on day 7 and was maintained at a low level. (D) The highest level of IL-6 in the serum was 110.2 pg/ml on day 4 and was decreased to a normal level on day 14. (E) Serum ferritin and (F) C-reactive protein exhibited similar changes to IL-6. PD-1, programmed cell death 1; CAR, chimeric antigen receptor; CAR-T 19, anti-CD19 CAR T cell; CD, cluster of differentiation; IL-6, interleukin-6.
Discussion
B-NHL is the most frequent hematological malignancy. Chemotherapy, anti-CD20 monoclonal antibodies and autologous stem cell transplantation have improved the prognosis of patients with B-NHL in recent decades; however, the prognosis of patients with refractory B-NHL remains poor (9). Anti-CD19 CAR-T cell therapy may improve remission rates and prolong survival time in patients with relapsed/refractory B-lineage hematological malignancies (10,11).
The immunosuppressive PD-1 pathway prevents T cells from entering the tumor area and blocks the effects of T-cell immunotherapy (12,13). Although the effects of the PD-1 inhibitor were significant, it requires regular and repeated administration (14). Anti-CD19 CAR-T cells cultured from PD-1 high expression T cells exhibit decreased anti-tumor immune responses and result in failure of CAR-T cell therapy (15). According to the beneficial effects of PD-1 inhibitors on the clinical treatment of tumors (16), PD-1 inhibitors may be able to partially rescue the deterioration of anti-CD19 CAR-T cell function. Anti-CD19 CAR-T cell in combination with PD-1 blockade may overcome the immunosuppressive effects of high PD-1 expression on T cells, thereby improving the therapeutic efficacy in relapsed/refractory B-NHL.
A number of adverse effects are associated with PD-1 blockade, particularly immune-associated adverse events in the respiratory and circulatory systems (17). The mechanisms underlying these effects remain unclear; however, they may result in mortality. Additionally, the adverse effects of anti-CD19 CAR-T cells, including cytokine release syndrome, must be taken into account (18). The present study hypothesized that CAR-T 19 cell therapy combined with decreased-dose PD-1 blockade may be effective in treating B-NHL. This combination decreased the adverse effects associated with PD-1 inhibitors and anti-CD19 CAR-T cell, and led to improved therapeutic efficacy.
The present case study demonstrated the therapeutic feasibility of decreased-dose PD-1 inhibitor in combination with CAR-T 19 cells to overcome immunosuppression. A decreased dose of PD-1 inhibitor may decrease its adverse effects, whilst still ensuring efficacy. Future studies are required in order to test the combination of decreased-dose PD-1 inhibitor and CAR-T 19 cells in more patients with refractory lymphoma and high expression of PD-1 in peripheral blood samples. In addition, further studies are required to elucidate the molecular mechanisms underlying this combination therapy and to design a clinical trial to test the efficacy of PD-1 inhibitors combined with CAR-T 19 cells in patients with refractory B-NHL.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Hospital Funding Project (grant no. CM201805).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Authors' contributions
QD conceptualized and designed the study. JW, YJ, HZ and YL performed the clinical trial. RZ acquired the data. JM analyzed and interpreted the data. All authors contributed to the writing and revision of the manuscript.
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of Tianjin First Center Hospital and written informed consent was obtained from the patient.
Patient consent for publication
Informed consent for publication was obtained from the patient.
Competing interests
The authors declare that they have no conflicts of interest.
References
- 1.Van Den Neste E, Schmitz N, Mounier N, Gill D, Linch D, Trneny M, Bouadballah R, Radford J, Bargetzi M, Ribrag V, et al. Outcomes of diffuse large B-cell lymphoma patients relapsing after autologous stem cell transplantation: An analysis of patients included in the CORAL study. Bone Marrow Transplant. 2017;52:216–221. doi: 10.1038/bmt.2016.213. [DOI] [PubMed] [Google Scholar]
- 2.Jurinovic V, Kridel R, Staiger AM, Szczepanowski M, Horn H, Dreyling MH, Rosenwald A, Ott G, Klapper W, Zelenetz AD, et al. Clinicogenetic risk models predict early progression of follicular lymphoma after first-line immunochemotherapy. Blood. 2016;128:1112–1120. doi: 10.1182/blood-2016-05-717355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schuster SJ, Svoboda J, Chong EA, Nasta SD, Mato AR, Anak Ö, Brogdon JL, Pruteanu-Malinici I, Bhoj V, Landsburg D, et al. Chimeric antigen receptor T cells in refractory B-cell lymphomas. N Engl J Med. 2017;377:2545–2554. doi: 10.1056/NEJMoa1708566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang C, Thudium KB, Han M, Wang XT, Huang H, Feingersh D, Garcia C, Wu Y, Kuhne M, Srinivasan M, et al. In vitro characterization of the anti-PD-1 antibody nivolumab, BMS-936558, and in vivo toxicology in non-human primates. Cancer Immunol Res. 2014;2:846–856. doi: 10.1158/2326-6066.CIR-14-0040. [DOI] [PubMed] [Google Scholar]
- 5.Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, Powderly JD, Carvajal RD, Sosman JA, Atkins MB, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366:2443–2454. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Annibali O, Crescenzi A, Tomarchio V, Pagano A, Bianchi A, Grifoni A, Avvisati G. PD-1 /PD-L1 checkpoint in hematological malignancies. Leuk Res. 2018;67:45–55. doi: 10.1016/j.leukres.2018.01.014. [DOI] [PubMed] [Google Scholar]
- 7.Naidoo J, Page DB, Li BT, Connell LC, Schindler K, Lacouture ME, Postow MA, Wolchok JD. Toxicities of the anti-PD-1 and anti-PD-L1 immune checkpoint antibodies. Ann Oncol. 2015;26:2375–2391. doi: 10.1093/annonc/mdv383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP. Toxicity and response criteria of the eastern cooperative oncology group. Am J Clin Oncol. 1982;5:649–655. doi: 10.1097/00000421-198212000-00014. [DOI] [PubMed] [Google Scholar]
- 9.Martelli M, Ferreri AJ, Agostinelli C, Di Rocco A, Pfreundschuh M, Pileri SA. Diffuse large B-cell lymphoma. Crit Rev Oncol Hematol. 2013;87:146–171. doi: 10.1016/j.critrevonc.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 10.Kochenderfer JN, Dudley ME, Kassim SH, Somerville RP, Carpenter RO, Stetler-Stevenson M, Yang JC, Phan GQ, Hughes MS, Sherry RM, et al. Chemotherapy-refractory diffuse large B-cell lymphoma and indolent B-cell malignancies can be effectively treated with autologous T cells expressing an anti-CD19 chimeric antigen receptor. J Clin Oncol. 2015;33:540–549. doi: 10.1200/JCO.2014.56.2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Batlevi CL, Matsuki E, Brentjens RJ, Younes A. Novel immunotherapies in lymphoid malignancies. Nat Rev Clin Oncol. 2016;13:25–40. doi: 10.1038/nrclinonc.2015.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davila ML, Riviere I, Wang X, Bartido S, Park J, Curran K, Chung SS, Stefanski J, Borquez-Ojeda O, Olszewska M, et al. Efficacy and toxicity management of 19-28z CAR T cell therapy in B cell acute lymphoblastic leukemia. Sci Transl Med. 2014;6:224–225. doi: 10.1126/scitranslmed.3008226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jaspers JE, Brentjens RJ. Development of CAR T cells designed to improve antitumor efficacy and safety. Pharmacol Ther. 2017;178:83–91. doi: 10.1016/j.pharmthera.2017.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huang AC, Postow MA, Orlowski RJ, Mick R, Bengsch B, Manne S, Xu W, Harmon S, Giles JR, Wenz B, et al. T-cell invigoration to tumour burden ratio associated with anti-PD-1 response. Nature. 2017;545:60–65. doi: 10.1038/nature22079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li S, Siriwon N, Zhang X, Yang S, Jin T, He F, Kim YJ, Mac J, Lu Z, Wang S, et al. Enhanced cancer immunotherapy by chimeric antigen receptor-modified T cells engineered to secrete checkpoint inhibitors. Clin Cancer Res. 2017;23:6982–6992. doi: 10.1158/1078-0432.CCR-17-0867. [DOI] [PubMed] [Google Scholar]
- 16.Zou W, Wolchok JD, Chen L. PD-L1 (B7-H1) and PD-1 pathway blockade for cancer therapy: Mechanisms, response biomarkers, and combinations. Sci Transl Med. 2016;8:328–324. doi: 10.1126/scitranslmed.aad7118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Läubli H, Balmelli C, Bossard M, Pfister O, Glatz K, Zippelius A. Acute heart failure due to autoimmune myocarditis under pembrolizumab treatment for metastatic melanoma. J Immunother Cancer. 2015;3:11. doi: 10.1186/s40425-015-0057-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brudno JN, Kochenderfer JN. Toxicities of chimeric antigen receptor T cells: Recognition and management. Blood. 2016;127:3321–3330. doi: 10.1182/blood-2016-04-703751. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.