Abstract
Objective:
To examine the relationship between psychiatrists’ religious/spiritual beliefs and their attitudes regarding religion and spirituality in clinical practice.
Methods:
A cross-sectional survey of religion/spirituality (R/S) in clinical practice was conducted with 121 psychiatrists from the largest academic hospital complex in Brazil.
Results:
When asked about their R/S beliefs, participants were more likely to consider themselves as spiritual rather than religious. A total of 64.2% considered their religious beliefs to influence their clinical practice and 50% reported that they frequently enquired about their patients’ R/S. The most common barriers to approaching patients’ religiosity were: lack of time (27.4%), fear of exceeding the role of the doctor (25%), and lack of training (19.1%). Those who were less religious or spiritual were also less likely to find difficulties in addressing a patient’s R/S.
Conclusion:
Differences in psychiatrists’ religious and spiritual beliefs are associated with different attitudes concerning their approach to R/S. The results suggest that medical practice may lead to a religious conflict among devout psychiatrists, making them question their faith. Training might be of importance for handling R/S in clinical practice and for raising awareness about potential evaluative biases in the assessment of patients’ religiosity.
Keywords: Religion; ethics; education, psychiatric; psychotherapy
Introduction
Although a relationship between medicine, religiosity, and spirituality has been observed since antiquity, only in the last few decades has a significant increase in scientific publications addressing such topics been observed. A bibliometric study using the Boolean expression “spiritual* OR religion*” and covering a period of 15 years found that the number of PubMed publications increased steadily between 1999 and 2013, resulting in a total of 30,532 references.1 The evidence obtained so far indicates a positive relationship between religious involvement/spirituality (R/S) and physical health on one side and mental health and R/S on the other, including an increase in coping capacity.2
Overall, research in the mental health area indicates that R/S is associated with improved well-being, feelings of meaning and peace,3 and reductions in suicide rates, depression, anxiety, and substance abuse.4,5 Such benefits are not restricted to mild and moderate conditions, but also include patients with severe mental illness.6
Based on these studies, many professional organizations, such as the World Psychiatric Association (WPA),7 the Royal College of Psychiatrists (RCP),8 the American Psychiatric Association (APA),9 the Joint Commission on Accreditation of Healthcare Organizations (JCAHO),10 and the Brazilian Psychiatry Association (ABP)11 have noted the importance of taking spirituality into consideration and have raised awareness of its implications for clinical practice and medical training.
There is a growing body of research investigating how the patient’s R/S is approached in clinical practice.12 The evidence shows that a large majority of physicians consider it important to integrate R/S into their practice, but most of them face difficulties in addressing such topics with their patients, due to a lack of time and a lack of appropriate training.13,14
Psychiatry is no different from other areas of medicine in this regard. Even though psychiatrists reported having fewer difficulties and more experience in handling their patients’ R/S, these attitudes and perceptions have not always been reflected in their practice, and they face the same barriers as other medical specialists when approaching patients’ R/S.15 In a recent survey of 484 Brazilian psychiatrists, all members of the ABP, Menegatti-Chequini et al. found that more than half of the participants (55.5%) did not enquire frequently about their patients’ R/S. The most common reasons for not doing so included being afraid of exceeding the role of the doctor (30.2%) and lack of training (22.3%).16
The evidence suggests that the religious characteristics and beliefs of physicians (including psychiatrists) are directly related to their attitudes and behaviors regarding R/S in clinical practice.13,17-20 When psychiatrists consider themselves to be more religious or spiritual, they are also more likely to ask their patients about their R/S and to see the integration of R/S into clinical practice as important.16 However, more research is needed to clarify the relationship between psychiatrists’ attitudes toward R/S, as well as their approach to these issues in clinical practice, including the role of specific religious or spiritual beliefs and religious coping.
The aim of the present study was to investigate the religious and spiritual beliefs of Brazilian psychiatrists working at the Instituto de Psiquiatria, Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo (IPq-HC-FMUSP) to verify whether these beliefs affected their approach to their patients’ R/S. The IPq-HC-FMUSP is the largest academic psychiatric hospital in Brazil and a national reference in psychiatry.21 In this respect, although not representative of Brazilian psychiatrists, the obtained results reflect the beliefs, attitudes, and behaviors of influential professionals in this area regarding R/S.
The study also aimed to investigate in more detail some aspects of psychiatrists’ attitudes toward religion and spirituality that have not been assessed previously,16 including: 1) religious and spiritual beliefs, such as God, life after death, and reincarnation; 2) the specific ways in which their perspective on R/S influence clinical practice; 3) the ways in which medical practice affects their own R/S; and 4) the potential impact of religious coping strategies in their practice as physicians.
Methods
Study design and sampling
The study comprised a cross-sectional investigation of 121 psychiatrists working at IPq-HC-FMUSP. Participants were personally approached by one of the authors (MCMC) and invited to collaborate with the study by answering a brief and confidential questionnaire. Data collection occurred between December 2013 and May 2014.
Survey content
A questionnaire was developed based on the instrument Religion and Spirituality in Medicine: Physicians’ Perspectives, by Curlin et al.22 to investigate attitudes and behaviors of physicians from different specialties concerning R/S in clinical practice.
The questionnaire was translated into Portuguese and tested in a pilot study with two groups: initially with 30 health professionals (from different specialties) and with 20 psychiatrists in training (residents) at IPq-HC-FMUSP. The questions were considered clear and no additional adaptation was necessary during the testing phase.
The questionnaire consisted of a self-report measure assessing the three principal areas described below.
Sociodemographic and professional characteristics
This section included data related to age, gender, marital status, psychiatric specialty, degree level, and the number of years of professional experience.
Participants’ religious and spiritual characteristics
The R/S dimension was measured based on two questions, one evaluating the reported level of religiousness (“To what extent do you consider yourself a religious person?”) and the other evaluating spirituality (“To what extent do you consider yourself a spiritual person?”). Each question contained four alternatives: 1 = not at all, 2 = slightly, 3 = moderately, and 4 = very. It was decided not to define the terms religiousness or spirituality. Thus, participants were given the opportunity to rely on their own interpretations of these concepts.
Psychiatrists were also questioned about their beliefs in God, life after death, and reincarnation. Their answers to these questions were given based on three alternatives: 2 = yes, 1 = undecided, and 0 = no. These beliefs were chosen because of the marked syncretism of Brazilian religiosity and the widespread influence of Christian and spiritualist ideas in this cultural context.23
Religious affiliation was determined based on the following choices: Catholic, Protestant or Evangelical, Spiritist, other religion (including Judaism, Islam, Hinduism, Buddhism, and Mormonism), and none (including agnostic and atheist). Religious affiliations were presented according to the Brazilian context, where Catholics, Evangelicals, and Spiritists constitute the majority of the religious followers.24
Coping styles were measured based on two questions extracted from the Spiritual/Religious Coping Scale (RCOPE)25: one evaluating religious coping (“I look to God for strength, support, and guidance.”) and the other evaluating individual or non-religious coping (“I try to make sense of the situation and decide what to do without relying on God.”). Each question contained four alternatives: 1 = never, 2 = rarely, 3 = occasionally, and 4 = often.
Opinions and behaviors related to religiousness/spirituality
Participants were questioned on the extent to which they agreed with the following statements: “My experience as a physician has made me question my religious and spiritual beliefs”; “I find it challenging to remain faithful to my religion in my work as a physician,” and “My religious/spiritual beliefs influence my clinical practice.” Four possible alternatives were given to participants: 1 = not at all, 2 = slightly, 3 = moderately, and 4 = strongly.
Regarding the approach to R/S in clinical practice, participants were questioned on the frequency with which they usually enquire about a patient’s R/S. The four alternatives included 1 = never, 2 = rarely, 3 = occasionally, and 4 = frequently. Additionally, they were asked whether enquiring about the patient’s R/S is something the psychiatrist can (or should) do. Their answers to these questions were selected from three alternatives: 2 = yes, 3 = undecided, and 1 = no.
To identify the barriers and difficulties most frequently found by psychiatrists in addressing patients’ R/S, participants were asked to answer a multiple-choice question including the following alternatives: 1) None, 2) Fear of exceeding the role of the doctor, 3) Lack of training, 4) Lack of time, 5) Not being comfortable with the issue, 6) Irrelevance of the subject for the patient, 7) Fear of offending the patient, 8) Fear of disapproval from peers, 9) It is not the doctor’s job, and 10) Do not know why.
Statistical analysis
SPSS version 17 was used for the data analyses. Chi-square tests were generated to estimate associations between categorical variables. The t-test and ANOVA were employed to evaluate differences between groups. Pearson product-moment coefficients were obtained to investigate correlations between variables. Finally, a stepwise multiple regression analysis was undertaken to identify which of the difficulties faced by the psychiatrists in addressing R/S in clinical practice were most important in the decision to enquire (or not) about their patients’ R/S.
Ethics
The study was approved by the local research ethics committee. Participants were informed of their rights to deny participation, to withdraw from the study at any time, and to have their anonymity preserved. They were also informed about the study’s objectives and the voluntary nature of their participation.
Results
Of the 121 psychiatrists employed by IPq-HC-FMUSP, 86 answered the questionnaire (71%). Two response forms were eliminated due to incompleteness. The remaining 84 were analyzed.
Sociodemographic characteristics
Almost two-thirds of the participants were male. Most were married or in a stable relationship. The majority were post-graduates and treated adult patients. None of these demographic variables showed statistically significant associations with our measures of R/S (p > 0.05). Those dedicated to child psychiatry presented higher levels of spirituality (Table 1).
Table 1. Sociodemographic and professional characteristics and their relations to religiosity and spirituality.
| Religiosity | Spirituality | ||||||
|---|---|---|---|---|---|---|---|
| Mean (SD) | r | p-value | Mean (SD) | r | p-value | ||
| Age in years, mean (SD) | 45.6 (9.8) | - | 0.03 | 0.744 | - | 0.07 | 0.455 |
| Gender, n (%) | 0.373 | 0.962 | |||||
| Female | 32 (38.1) | 1.84 (0.95) | 2.43 (0.94) | ||||
| Male | 52 (61.9) | 2.03 (0.94) | 2.42 (0.91) | ||||
| Marital status, n (%) | 0.459 | 0.323 | |||||
| Without a partner | 24 (28.6) | 2.08 (0.88) | 2.58 (0.88) | ||||
| With a partner | 60 (71.4) | 1.91 (0.97) | 2.36 (0.93) | ||||
| Subspecialty, n (%) | 0.247 | 0.508 | |||||
| Adult | 70 (83.3) | 1.88 (0.90) | 2.37 (0.93) | ||||
| Child | 18 (21.4) | 2.33 (0.97) | 2.77 (0.73) | ||||
| Old age | 13 (15.5) | 1.92 (1.18) | 2.30 (1.10) | ||||
| Forensic | 11 (13.1) | 2.45 (1.28) | 2.54 (0.68) | ||||
| Other | 8 (9.5) | 2.12 (0.99) | 2.37 (0.91) | ||||
| Years as a psychiatrist, mean (SD) | 19.8 (10.1) | - | -0.02 | 0.828 | - | -0.09 | 0.326 |
| Level of instruction, n (%) | 0.446 | 0.433 | |||||
| Residency | 12 (14.3) | 1.75 (1.05) | 2.16 (1.11) | ||||
| Specialization | 15 (17.9) | 1.66 (0.89) | 2.20 (0.86) | ||||
| Masters | 13 (15.5) | 2.23 (0.72) | 2.76 (0.82) | ||||
| Doctorate | 32 (38.1) | 2.00 (0.98) | 2.50 (0.91) | ||||
| Post-doctorate | 12 (14.3) | 2.16 (1.02) | 2.41 (0.90) | ||||
r = Pearson’s correlation coefficient; SD = standard deviation.
Religious and spiritual beliefs
With respect to the psychiatrists’ levels of R/S, the participants in this sample were slightly more spiritual (mean [M] = 2.43; standard deviation [SD] ± 0.92) than religious (M = 1.96; SD ± 0.95). Only 31% of the respondents considered themselves to be very or moderately religious, whereas 53.5% considered themselves to be very or moderately spiritual.
More than half of the psychiatrists (57.7%) said they had a religion, of which the majority was Catholic (Table 2). Almost two-thirds of the sample (59.5%) stated that they believe in God. Approximately half of the participants (47.6%) answered no when questioned about their belief in the existence of life after death. In addition, more than two-thirds (69%) answered that they do not believe in reincarnation.
Table 2. Psychiatrists’ religious/spiritual characteristics.
| n (%) | |
|---|---|
| Religious affiliation | |
| Catholic | 28 (33.7) |
| Protestant or Evangelical | 8 (9.6) |
| Spiritist | 5 (6.0) |
| Other religion | 7 (8.4) |
| None | 35 (42.8) |
| Missing value | 1 |
| Do you believe in God or a higher power? | |
| Yes | 50 (59.5) |
| No | 20 (23.8) |
| Undecided | 14 (16.7) |
| Do you believe there is life after death? | |
| Yes | 24 (28.6) |
| No | 40 (47.6) |
| Undecided | 20 (23.8) |
| Do you believe in reincarnation? | |
| Yes | 16 (19.0) |
| No | 58 (69.0) |
| Undecided | 10 (11.9) |
| I try to make sense of the situation and decide what to do without relying on God | |
| Often | 39 (48.1) |
| Occasionally | 22 (27.2) |
| Rarely | 9 (11.1) |
| Never | 11 (13.6) |
| Missing values | 3 |
| I look for God as a source of strength, support, and guidance. | |
| Often | 18 (21.9) |
| Occasionally | 15 (18.3) |
| Rarely | 16 (19.5) |
| Never | 33 (40.2) |
| Missing values | 2 |
Regarding religious coping, 58.3% of the respondents look for God as a source of strength, support and guidance, while 83.3% decide what to do without relying on God. As one might expect, the latter option was chosen significantly more often by non-religious (M = 3.34; SD ± 1.16) than by religious participants (M = 2.89; SD ± 0.96); t (78) = 1.92; p = 0.049. In terms of mean values, the psychiatrists in this sample refer to individual or non-religious coping strategies slightly more often than they look for God’s support (Table 2).
Attitudes and behaviors related to the approach to R/S in clinical practice
Questioning of faith
A total of 63.1% of participants stated that their experience as a physician made them question their religious beliefs at least a little, while 39.3% found some degree of challenge in remaining faithful to their religion in their job as a physician (Table 3). Questioning of faith showed moderate correlations with different religious and spiritual characteristics (Table 4), indicating that the more religious or spiritual the psychiatrists were, the more their work as physicians made them question their religious and spiritual beliefs.
Table 3. Psychiatrists’ attitudes regarding religion/spirituality in clinical practice.
| n (%) | |
|---|---|
| My experience as a physician has made me question my religious beliefs. | |
| Strongly | 9 (11.0) |
| Moderately | 22 (26.8) |
| Slightly | 22 (26.8) |
| Not at all | 29 (35.4) |
| Missing values | 2 |
| I find it challenging to remain faithful to my religion in my work as a physician. | |
| Strongly | 4 (4.9) |
| Moderately | 8 (9.7) |
| Slightly | 21 (25.6) |
| Not at all | 49 (59.7) |
| Missing values | 2 |
| My religious beliefs influence my clinical practice. | |
| Strongly | 6 (7.1) |
| Moderately | 31 (36.9) |
| Slightly | 17 (20.2) |
| Not at all | 30 (35.7) |
| How often do you enquire about patients’ religious/spiritual issues? | |
| Frequently | 42 (50.0) |
| Occasionally | 27 (32.1) |
| Rarely | 12 (14.3) |
| Never | 3 (3.6) |
| Enquiring about the religion/spirituality of the patient is something the psychiatrist can (or should) do. | |
| Yes | 74 (88.1) |
| No | 7 (8.3) |
| Undecided | 3 (3.6) |
Table 4. Pearson correlations for the influence of beliefs and religious coping in clinical practice and the influence of medical practice in the questioning of faith.
| Belief in God | Belief in life after death | Belief in reincarnation | Spirituality | Religiosity | Coping: without God | Coping: looking for God | |
|---|---|---|---|---|---|---|---|
| Influence of beliefs in clinical practice | |||||||
| My religious beliefs influence my clinical practice. | 0.533 † | 0.457 † | 0.234* | 0.633 † | 0.665 † | -0.263* | 0.691 † |
| Do you think the psychiatrist can or should ask about the patient’s religion/spirituality? | -0.148 | 0.051 | 0.175 | -0.125 | -0.153 | 0.013 | -0.093 |
| How often do you enquire about patients’ religious/spiritual issues? | -0.077 | 0.059 | 0.232* | -0.097 | -0.092 | -0.101 | -0.052 |
| Questioning of faith | |||||||
| My experiences as a physician have made me question my religious beliefs. | 0.355 † | 0.362 † | 0.274* | 0.236* | 0.242* | -0.139 | 0.337* |
| I find it challenging to remain faithful to my religion in my work as a physician. | 0.271* | 0.142 | 0.170 | 0.171 | 0.093 | 0.037 | 0.188 |
p < 0.05;
p < 0.001.
Influence of beliefs in clinical practice
More than half of the sample (64.2%) considered their religious and spiritual beliefs to influence their clinical practice. This variable showed moderate to strong correlations with religiosity, spirituality, religious coping, and belief in God, life after death, and reincarnation (Table 4). As might be expected, the influence of beliefs in clinical practice differed between religious and non-religious affiliations (F4,78 = 10.42; p < 0.001). The least significant difference post-hoc tests indicate that all religious groups scored significantly higher (p < 0.05) than atheists and non-religious participants in the influence they attribute to religious and spiritual beliefs in clinical practice.
Psychiatrists who worked with children (t [82] = 2.52; p = 0.013) and adults (t [82] = 2.03; p = 0.045) were more likely to think that their beliefs influence clinical practice.
A total of 88.1% of psychiatrists consider enquiring about the patient’s R/S as something the psychiatrist can or should do. Half of the sample (50%) answered that they frequently ask their patients about their religious/spiritual beliefs, while 46.4% enquire occasionally or rarely. None of the sociodemographic or professional characteristics were associated with addressing the patient’s R/S. However, belief in reincarnation correlated positively with the frequency with which psychiatrists ask about patients’ R/S (Table 4).
Barriers to addressing religiosity and spirituality in clinical practice
Almost half of the sample stated that they have no difficulty in addressing the religiosity and spirituality of their patients, and they were more likely to be male than female (Fisher’s exact test, p = 0.041; adjusted residual = 2.2), as well as less spiritual (M = 2.19; SD ± 0.97; t [82] = 2.16; p = 0.034) and less religious (M = 1.68; SD ± 0.81; t [82] = 2.55; p = 0.013).
The most commonly reported barriers to approaching patient R/S in clinical practice were lack of time, fear of exceeding the role of the doctor, and lack of training (see Figure 1 for the other responses).
Figure 1. Challenges/barriers to approaching patients’ religiosity/spirituality.
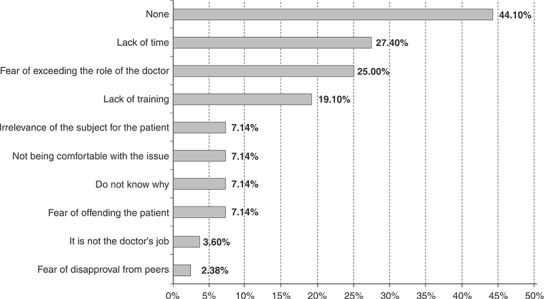
More male than female psychiatrists considered lack of time to be a relevant barrier (Fisher’s exact test, p = 0.023; adjusted residual = 2.4). Those who considered fear of exceeding the role of the doctor as a challenge scored significantly higher in religiosity (M = 2.52; SD ± 1.03; t [82] = -3.30; p = 0.013) and spirituality (M = 2.29; SD ± 0.96; t [50.43] = -3.06; p = 0.004).
A stepwise multiple regression analysis was undertaken to identify which of the barriers or difficulties in addressing a patient’s R/S would best predict the frequency with which they enquire about the patient’s R/S (adjusted R2 = 0.25; F3,80 = 10.15; p < 0.001). The most significant predictors in the final model were: it is not the doctor’s job (β = -0.42; t = -4.34; p < 0.001), do not know why (β = -0.30; t = -3.12; p = 0.002), and lack of time (β = -0.25; t = -2.56; p = 0.012). In terms of whether the psychiatrist should ask about the patient’s R/S (adjusted R2 = 0.16; F2,81 = 9.04; p < 0.001), the best predictors were: it is not the doctor’s job (β = -0.40; t = -3.88; p < 0.001) and not being comfortable with the issue (β = 0.25; t = 2.46; p = 0.016).
Discussion
Differences in psychiatrists’ religious and spiritual characteristics are associated with different attitudes concerning the approach to R/S in clinical practice. For example, the results showed that religious participants attribute more influence to religious and spiritual beliefs in their clinical practice than those not considered religious. In this regard, those who believe in reincarnation were more likely to ask their patients about R/S issues than those who do not. The study also found that experience as a physician might produce a religious conflict among religious psychiatrists, leading them to question their beliefs, which could affect their approach to their patients’ R/S. In this sense, those who reported a fear of exceeding the role of the doctor scored significantly higher in religiosity and spirituality. Accordingly, those who were less religious and less spiritual were less likely to find difficulties in addressing the patient’s R/S.
Training might be of importance in handling R/S in clinical practice (whether the psychiatrist is religious or not) and could also raise awareness about potential evaluative biases in the assessment of patients’ R/S. Training might also help reduce the discomfort reported by some psychiatrists when they need to approach R/S issues. However, certain challenges may be harder to overcome, such as a lack of time, which will depend on circumstances that are not entirely under the psychiatrist’s control.
Although spiritual care may not be considered an exclusive prerogative of healthcare chaplains, making them part of the multi-disciplinary team could also help prevent psychiatrists’ fear of exceeding the role of the doctor when addressing patients’ R/S. This strategy could be important when providing integral care for the patient.
Psychiatrists’ approaches to religious issues appeared to be influenced by gender differences, with males reporting fewer difficulties than females. Although there were no R/S differences between genders, women appeared to give particular relevance to such topics, in a way that is different from male psychiatrists, which should be further investigated.
It was also observed that child psychiatrists scored higher in spirituality and were more likely to think their religious beliefs influenced their clinical practice. Interestingly, Curlin et al.26 reported that family physicians and pediatricians are more religious than physicians from other specialties. There is a current scarcity of reports regarding the potential impact of psychiatry subspecialties on the R/S of psychiatrists.
Similar to what was observed in previous investigations,15,17 the psychiatrists in this sample consider themselves more spiritual than religious. This finding may reflect an understanding of spirituality as a broader category than religion or religiosity. Despite the lack of consensus on R/S concepts, most studies refer to religion as an organized, collective system of beliefs and practices in the search of the sacred or transcendent, while spirituality is understood as a personal form of search or connection with the sacred or transcendent. Spirituality was found in many studies to be related to a sense of well-being, a sense of purpose in life and experiences of life satisfaction without necessarily depending on commitment to a religious community.3,27
More than half of the participants reported a religious affiliation, a percentage significantly lower than that of the Brazilian population, of which only 8% said they had no religion.24 The percentage in our sample was also lower than that of Brazilian physicians from other specialties (94.9%)28 and that of medical students from 12 different schools of medicine (66.1%).29
Compared to medical students, our sample also showed lower percentages for belief in God (59.5% vs. 84.2%), belief in life after death (28.6% vs. 66.8%), and belief in reincarnation (19% vs. 36.9%).29 Our data are in accordance with previous reports in which psychiatrists were less likely to believe in God and declare a religious affiliation than the general population16-18,30 or physicians from other specialties.31 This more secular trait of psychiatrists continues to appear in studies addressing the R/S of health professionals in general.20,32 Some authors33,34 attribute this finding to the influence of psychological theories, such as Sigmund Freud's35 psychoanalysis, which is known to have pathologized religious behavior. According to Curlin et al.,31 the historical tensions between psychiatry and religion influenced many psychiatrists in the past century and continue to be influential today.
In Brazil, the tendency to “pathologize” religious expressions such as trance and possession is also historical. In the second half of the 20th century, these experiences were considered by most Brazilian psychiatrists to be symptoms of mental disorders.36 More recently, a culturally sensitive understanding of these experiences has emerged, and specific diagnostic criteria have been developed to help differentiate pathological from culturally accepted and healthy spiritual manifestations.37 Still, mental health professionals do not generally receive adequate training to address the R/S aspects of their patients,38 including experiences of possession, which would be of paramount importance for avoiding erroneous diagnoses and iatrogenic symptoms.37,39
In conclusion, although half of the psychiatrists in this study often address their patients’ R/S, most report difficulties in approaching this topic and almost half report that their beliefs strongly or moderately influence their medical practice. Their religious/spiritual characteristics are associated with their attitudes and behaviors regarding their approach to R/S in clinical practice. Information and training regarding R/S issues might help psychiatrists overcome the barriers to approaching this topic and adequately integrating the R/S aspects of their patients into therapeutic work.
This investigation has some methodological limitations. First, the range of religious and spiritual beliefs covered in the questionnaire is very limited. Second, the sample was restricted to psychiatrists from only one institution and, despite being one of the most respectable academic organizations in Brazil, the results could not be generalized as a representation of what most Brazilian psychiatrists think. Finally, self-report measures and questionnaires are vulnerable to response bias. Future investigations would benefit from the complementary use of qualitative and in-depth interviews. Additional aspects to be evaluated include psychiatrists’ opinions on the relationship between religion and mental health, their knowledge about issues regarding R/S, the most common approaches to patients’ R/S, and patients’ perceptions of psychiatrists’ approach to their religious and spiritual issues.
Disclosure
The authors report no conflicts of interest.
Acknowledgements
The study received financial support from the Associação Mantenedora João Evangelista, São Paulo, Brazil. EOM is funded by the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP; grant 2015/05255-2).
We would like to thank all the psychiatrists who took the time to complete the survey, as well the IPq-HC-FMUSP staff, Dr. Edson Shiguemi Hirata, Ms. Katia Ichi, and the secretaries of the outpatient units for their help in the data collection.
Footnotes
How to cite this article: Menegatti-Chequini MC, Maraldi EO, Peres MFP, Leão FC, Vallada H. How psychiatrists think about religious and spiritual beliefs in clinical practice: findings from a university hospital in São Paulo, Brazil. Braz J Psychiatry. 2019;41:58-65. http://dx.doi.org/10.1590/1516-4446-2017-2447
References
- 1.Lucchetti G, Lucchetti AL. Spirituality, religion, and health: over the last 15 years of field research (1999-2013) Int J Psychiatry Med. 2014;48:199–215. doi: 10.2190/PM.48.3.e. [DOI] [PubMed] [Google Scholar]
- 2.Moreira-Almeida A, Neto FL, Koenig HG. Religiousness and mental health: a review. Rev Bras Psiquatr. 2006;28:242–50. doi: 10.1590/s1516-44462006000300018. [DOI] [PubMed] [Google Scholar]
- 3.Peres MF, Kamei HH, Tobo PR, Lucchetti G. Mechanisms behind religiosity and spirituality's effect on mental health, quality of life and well-being. J Relig Health. 2017 Apr 25 doi: 10.1007/s10943-017-0400-6. doi: 10.1007/s10943-017-0400-6 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Koenig HG, King D, Carson V. Handbook of religion and health. 2nd ed. New York: Oxford University; 2012. [Google Scholar]
- 5.Bonelli RM, Koenig HG. Mental disorders, religion and spirituality 1990 to 2010: a systematic evidence-based review. J Relig Health. 2013;52:657–73. doi: 10.1007/s10943-013-9691-4. [DOI] [PubMed] [Google Scholar]
- 6.Pargament KI, Lomax JW. Understanding and addressing religion among people with mental illness. World Psychiatry. 2013;12:26–32. doi: 10.1002/wps.20005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moreira-Almeida A, Sharma A, van Rensburg BJ, Verhagen PJ, Cook CC. WPA position statement on spirituality and religion in psychiatry. World Psychiatry. 2016;15:87–8. doi: 10.1002/wps.20304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Royal College of Psychiatrists Spirituality and psychiatry special interest group [Internet] 1999. [cited 2017 Oct 26] www.rcpsych.ac.uk/college/specialinterestgroups/spirituality.aspx.
- 9.American Psychiatric Association (APA), Committee on Religion and Psychiatry Guidelines regarding possible conflict between psychiatrists' religious commitments and psychiatric practice. Am J Psychiatry. 1990;147:542. doi: 10.1176/ajp.147.4.542. [DOI] [PubMed] [Google Scholar]
- 10.Joint Commission on Accreditation of Healthcare Organizations (JCAHO) Medical Record - Spiritual Assessment [Internet] 2017. [cited 2017 Oct 26] www.jointcommission.org/standards_information/jcfaqdetails.aspx?StandardsFaqId=1492&ProgramId=46.
- 11.Cordeiro Q. Creation of the section on spirituality and mental health at the Brazilian psychiatric association. Psyche Spirit. 2014;1:2–3. [Google Scholar]
- 12.Hvidt NC, Korup AK, Curlin FA, Baumann K, Frick E, Sondergaard J, et al. The NERSH international collaboration on values, spirituality and religion in medicine: development of questionnaire, description of data pool, and overview of pool publications. Religions (Basel) 2016;7:107. [Google Scholar]
- 13.Curlin FA, Chin MH, Sellergren SA, Roach CJ, Lantos JD. The association of physicians' religious characteristics with their attitudes and self-reported behaviors regarding religion and spirituality in the clinical encounter. Med Care. 2006;44:446–53. doi: 10.1097/01.mlr.0000207434.12450.ef. [DOI] [PubMed] [Google Scholar]
- 14.Moreira-Almeida A, Koenig HG, Lucchetti G. Clinical implications of spirituality to mental health: review of evidence and practical guidelines. Rev Bras Psiquiatr. 2014;36:176–82. doi: 10.1590/1516-4446-2013-1255. [DOI] [PubMed] [Google Scholar]
- 15.Curlin FA, Lawrence RE, Odell S, Chin MH, Lantos JD, Koenig HG, et al. Religion, spirituality, and medicine: psychiatrists' and other physicians' differing observations, interpretations, and clinical approaches. Am J Psychiatry. 2007;164:1825–31. doi: 10.1176/appi.ajp.2007.06122088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Menegatti-Chequini MC, Gonçalves JP, Leão FC, Peres MF, Vallada H. A preliminary survey on the religious profile of Brazilian psychiatrists and their approach to patients' religiosity in clinical practice. BJPsych Open. 2016;2:346–52. doi: 10.1192/bjpo.bp.116.002816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neeleman J, King MB. Psychiatrists religious attitudes in relation to their clinical-practice - a survey of 231 psychiatrists. Acta Psychiatr Scand. 1993;88:420–4. doi: 10.1111/j.1600-0447.1993.tb03484.x. [DOI] [PubMed] [Google Scholar]
- 18.Baetz M, Griffin R, Bowen R, Marcoux G. Spirituality and psychiatry in Canada: psychiatric practice compared with patient expectations. Can J Psychiatry. 2004;49:265–71. doi: 10.1177/070674370404900407. [DOI] [PubMed] [Google Scholar]
- 19.Shin JH, Yoon JD, Rasinski KA, Koenig HG, Meador KG, Curlin FA. A spiritual problem? Primary care physicians' and psychiatrists' interpretations of medically unexplained symptoms. J Gen Intern Med. 2013;28:392–8. doi: 10.1007/s11606-012-2224-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yoon JD, Shin JH, Nian AL, Curlin FA. Religion, sense of calling, and the practice of medicine: findings from a national survey of primary care physicians and psychiatrists. South Med J. 2015;108:189–95. doi: 10.14423/SMJ.0000000000000250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seixas A, Zilberman M. O Instituto de psiquiatria do Hospital das Clinicas - FMUSP. In: Mota A, Marinho M, editors. História da psiquiatria: ciências, prática e tecnologias de uma especialidade médica. São Paulo: Casa de Soluções e Editora. 2012:177–90. [Google Scholar]
- 22.Curlin FA, Lawrence RE, Chin MH, Lantos JD. Religion, conscience, and controversial clinical practices. N Engl J Med. 2007;356:593–600. doi: 10.1056/NEJMsa065316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moreira-Almeida A, Pinsky I, Zaleski M, Laranjeira R. Envolvimento religioso e fatores sociodemográficos: resultados de um levantamento nacional no Brasil. Rev Psiquiatr Clin. 2010;37:12–5. [Google Scholar]
- 24.Instituto Brasileiro de Geografia e Estatística (IBGE) Censo Demográfico 2010: características gerais da população, religião e pessoas com deficiência [Internet] 2010. [cited 2017 Oct 26] biblioteca.ibge.gov.br/biblioteca-catalogo?view=detalhes&id=794.
- 25.Pargament KI, Koenig HG, Perez LM. The many methods of relgious coping: development and initial validation of the RCOPE. J Clin Psychol. 2000;56:519–43. doi: 10.1002/(sici)1097-4679(200004)56:4<519::aid-jclp6>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 26.Curlin FA, Lantos JD, Roach CJ, Sellergren SA, Chin MH. Religious characteristics of U.S. physicians: a national survey. J Gen Intern Med. 2005;20:629–34. doi: 10.1111/j.1525-1497.2005.0119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goldim J, Salgueiro J, Raymundo M, Matte U, Bôer A. Bioética e espiritualidade. Porto Alegre: EDIPUCRS. 2007 [Google Scholar]
- 28.Lucchetti G, Ramakrishnan P, Karimah A, Oliveira GR, Dias A, Rane A, et al. Spirituality, religiosity, and health: a comparison of physicians' attitudes in Brazil, India, and Indonesia. Int J Behav Med. 2016;23:63–70. doi: 10.1007/s12529-015-9491-1. [DOI] [PubMed] [Google Scholar]
- 29.Lucchetti G, de Oliveira LR, Koenig HG, Leite JR, Lucchetti AL. SBRAME Collaborators Medical students, spirituality and religiosity-results from the multicenter study SBRAME. BMC Med Educ. 2013;13:162. doi: 10.1186/1472-6920-13-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bergin AE, Jensen JP. Religiosity of psychotherapists: a national survey. Psychotherapy (Chic) 1990;27:3–7. [Google Scholar]
- 31.Curlin FA, Odell SV, Lawrence RE, Chin MH, Lantos JD, Meador KG, et al. The relationship between psychiatry and religion among US physicians. Psychiatr Serv. 2007;58:1193–8. doi: 10.1176/appi.ps.58.9.1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Robinson KA, Cheng MR, Hansen PD, Gray RJ. Religious and spiritual beliefs of physicians. J Relig Health. 2017;56:205–25. doi: 10.1007/s10943-016-0233-8. [DOI] [PubMed] [Google Scholar]
- 33.Neeleman J, Persaud R. Why do psychiatrists neglect religion. Br J Med Psychol. 1995;68:169–78. doi: 10.1111/j.2044-8341.1995.tb01823.x. [DOI] [PubMed] [Google Scholar]
- 34.Koenig HG. Research on religion, spirituality, and mental health: a review. Can J Psychiatry. 2009;54:283–91. doi: 10.1177/070674370905400502. [DOI] [PubMed] [Google Scholar]
- 35.Freud S. The future of an illusion, civilization and its discontents. In: The Standard Edition of the Complete Psychological Works of Sigmund Freud (trans & ed. Strachey) vol. 21 Londres: Hogarth Press; pp. 1953–1974. [Google Scholar]
- 36.Almeida AAS, Oda AMGR, Dalgalarrondo P. O olhar dos psiquiatras brasileiros sobre os fenômenos de transe e possessão. Rev Psiquatr Clin. 2007;34:34–41. [Google Scholar]
- 37.Moreira-Almeida A, Cardena E. Differential diagnosis between non-pathological psychotic and spiritual experiences and mental disorders: a contribution from Latin American studies to the ICD-11. Rev Bras Psiquiatr. 2011;33:S21–36. doi: 10.1590/s1516-44462011000500004. [DOI] [PubMed] [Google Scholar]
- 38.Moreira-Almeida A, Lotufo-Neto F. Methodological guidelines to investigate altered states of consciousness anomalous experiences. Int Rev Psychiatry. 2017;29:283–92. doi: 10.1080/09540261.2017.1285555. [DOI] [PubMed] [Google Scholar]
- 39.Maraldi EO, Krippner S, Barros MC, Cunha A. Dissociation from a cross-cultural perspective: implications of studies in Brazil. J Nerv Ment Dis. 2017;205:558–67. doi: 10.1097/NMD.0000000000000694. [DOI] [PubMed] [Google Scholar]


