Abstract
Background
Adverse experiences, such as low care, overprotection, or abuse in childhood increase the likelihood of depression via their effects on personality traits. Similarly, being victimized in childhood may affect the likelihood of depression via personality traits. In this case-control study, we hypothesized that being victimized in childhood is associated with depression in adulthood via its effect on neuroticism, and verified this hypothesis using path analysis.
Subjects and methods
Eighty-two major depressive disorder (MDD) patients and 350 age-and-sex matched healthy controls completed self-administered questionnaires of demographic data, Patient Health Questionnaire-9, neuroticism, and victimization. The association between victimization, neuroticism, and depressive symptoms or having major depression was investigated by path analysis.
Results
Multiple group path analysis, in which depressive symptoms were considered as dependent variables, showed that the direct effect of victimization in childhood on depressive symptoms was not statistically significant in either healthy controls or MDD patients (standardized path coefficient: 0.079 and 0.084, respectively), but their indirect effects via neuroticism were statistically significant (standardized path coefficient: 0.059 and 0.141, respectively). Path analysis, in which the distinction between healthy controls and MDD patients was a dependent variable, showed that both direct effects and indirect effects of victimization in childhood via neuroticism on the distinction between healthy controls and MDD patients were statistically significant (standardized path coefficient: 0.186 and 0.164, respectively).
Limitations
Recall bias and the relatively small number of MDD patients are limitations of this study. Because it was a case-control survey, this study could not make any conclusions regarding causal associations.
Conclusion
This study suggests the possibility of causal associations between victimization in childhood and depressive symptoms or MDD in adulthood, and the mediation of this association by neuroticism.
Keywords: victimization, neuroticism, depression, major depressive disorder, path analysis
Introduction
Victimization has become a serious social problem, and experiences of being victimized in childhood cause various types of pain in children. As one example, it has been reported that experiences of being victimized in childhood is associated with psychiatric disorders, such as depression in adolescence.1–7 Although such experiences in childhood may affect depressive symptoms in adulthood, to our knowledge, few studies have analyzed the effects of being victimized in childhood on depressive symptoms in adulthood.6,8
When considering the association between childhood events and events in adulthood, it is assumed that there are mediating factors that affect the individual during the long time interval. Previous studies have shown by structural equation modeling that adverse experiences in childhood, such as abuse or overprotection, indirectly affect depressive symptoms and the mental health of adults, with changes in personality characteristics as mediating factors.9–12 However, mediating factors in the association between experiences of being victimized in childhood and depressive symptoms in adulthood has not been studied to date.
Because childhood victimization may affect brain development, and negative life events are associated with lasting changes in neuroticism, we hypothesized that childhood victimization may affect neuroticism via changes in brain development, and then neuroticism may act as a mediating factor between childhood victimization and depression in adulthood.13,14 In this case-control study, we conducted a self-administered questionnaire-based investigation, assessing depressive symptoms, neuroticism, and the degree and frequency of victimization. This study used path analysis to investigate the effects of the experience of being victimized in childhood on depressive symptoms in healthy controls and patients with major depressive disorder (MDD), and the distinction between controls and MDD in adulthood.
Subjects And Methods
Subjects
MDD patients who were treated at Seijin Hospital between March 2017 and August 2018 were recruited, and 82 of the patients provided complete responses to the questionnaires and hence participated in the study. As healthy controls, out of the 597 adults volunteers who were recruited between April 2017 and April 2018, 350 healthy controls who were age and sex-matched with the MDD patients were chosen. Inclusion criteria of the MDD patients were as follows: a) meeting the diagnostic criteria for MDD of DSM-5 (The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition)15 in the past or present, b) age between 20 and 70 years old, c) having no severe physical disorder, and d) being able to consent to participate in the research. Inclusion criteria of healthy controls were as follows: a) having no history of mental illness, b) age between 20 and 70 years old, c) Patient Health Questionnaire-9 (PHQ-9) score of less than 10, and d) having no severe physical disease. All participants provided written informed consent.
Demographics and clinical features of the subjects were analyzed, and a questionnaire survey (see below) was performed. In accordance with the Declaration of Helsinki, this study was conducted with approval from the ethics committees of Tokyo Medical University and Seijin Hospital. When dealing with raw data and consent forms concerning research implementation, protection of the subjects’ confidentiality and strict management of data were considered.
Questionnaires
Patient Health Questionnaire-9 (PHQ-9)
The Japanese version of PHQ-9 is a self-report questionnaire to evaluate the severity of depressive symptoms.16 It includes 9 questions that are evaluated using a 4-point Likert scale (0 points to 3 points), and the total score (0 points minimum to 27 points maximum) was considered as the PHQ-9 score. The higher the score, the more severe the depressive symptoms.
Neuroticism
To evaluate neuroticism, the 12-item neuroticism scale of the short version of the Eysenck Personality Questionnaire-revised (EPQ-R) was used. A high score indicates subjects who readily have feelings of anxiety, worry, and irritation.17
Assessment Scale Of Victimization In Childhood
This study used a revised version of a victimization scale of the National Institute for Educational Policy Research in Japan, because there are no Japanese versions of internationally validated measurement scales of victimization.18 This questionnaire subjectively evaluates the frequency and extent of being victimized in school and the community during childhood. It consists of 5 questions, which were evaluated using a 5-point Likert scale (0 points to 4 points). The total score (0 points minimum to 20 points maximum) was used as the victimization score. The higher the score, the greater the degree of being victimized (Appendix A and B).
Data Analysis
The unpaired t-test and χ2-test were performed using SPSS Statistics 22.0J software (SPSS Chicago, IL, USA) for comparing demographic and questionnaire data between 2 groups. Furthermore, multiple regression analysis and multivariate logistic regression analysis were performed, in which data of demographic characteristics and questionnaires were independent variables and the summary score of the PHQ-9 (depressive symptoms), EPQ-R (neuroticism) score, and the distinction of MDD (healthy controls = 1, MDD patients = 2) were dependent variables.
Multiple group path analysis including victimization, age, EPQ-R, and PHQ-9 were conducted for the combined samples of the healthy controls and MDD patients, and the group effects of healthy controls and MDD patients were compared for direct and indirect path coefficients using Mplus ver. 8.0 (Muthén & Muthén, Los Angeles, CA, USA). In addition, path analysis including victimization, age, EPQ-R, and the distinction between healthy controls and MDD patients (healthy controls = 1, MDD patients = 2) were conducted for the combined samples of healthy controls and MDD patients. Age was included as a possible factor affecting neuroticism and depressive symptoms, and the distinction of MDD.
A p-value of less than 0.05 was considered to indicate a statistically significant difference between 2 groups.
Results
Demographics, Clinical Features, And PHQ-9, EPQ-R, And Victimization Scores
Demographic and clinical features, and PHQ-9, EPQ-R, and victimization scores of 350 healthy controls and 82 MDD patients are shown in Table 1. A significantly larger proportion of healthy controls were employed, educated longer and married, and they tended to have a larger number of offspring. The proportion of subjects living alone and having a comorbid psychiatric disease were significantly higher in MDD patients, and PHQ-9, neuroticism on EPQ-R, and victimization scores were significantly higher in MDD patients than healthy controls.
Table 1.
Comparison Of The Characteristics, PHQ-9, EPQ, And Victimization Data Of MDD Patients And Healthy Controls
| Characteristic Or Measure | Healthy Controls | MDD Patients | t-test or χ2 test (MDD Patients vs Healthy Controls) |
|---|---|---|---|
| Age (years; mean ± S.D.) | 44.6 ± 11.2 | 46.0 ± 10.2 | n.s. |
| Sex (men : women) | 206 : 144 | 46 : 36 | n.s. |
| Years of education | 14.5 ± 1.8 | 13.7 ± 2.4 | p < 0.01 |
| Employment status (employed : nonemployed) | 346: 4 | 48: 34 | p < 0.001 |
| Marital status (single : married) | 90 : 257 | 36 : 46 | p = 0.001 |
| Living alone (yes : no) | 59: 291 | 27 : 55 | p = 0.001 |
| Offspring (yes : no) | 247: 103 | 45 : 37 | p = 0.006 |
| Number of offspring (mean ± S.D.) | 1.5 ± 1.2 | 1.0 ± 1.0 | p < 0.001 |
| Comorbid physical disease (yes : no) | 111: 239 | 33 : 49 | n.s. |
| Comorbid psychiatric disorder (yes : no) | 0: 350 | 13: 69 | p < 0.001 |
| First-degree relative with mood disorder (yes : no) | 26: 324 | 9: 73 | n.s. |
| First-degree relative with MDD (yes : no) | 21: 329 | 7: 75 | n.s. |
| PHQ-9 score | 2.8 ± 2.6 | 15.5 ± 7.1 | p < 0.001 |
| Neuroticism score (from EPQ-R) | 3.5 ± 3.1 | 7.8 ± 3.0 | p < 0.001 |
| Victimization score | 2.0 ± 3.2 | 4.4 ± 3.8 | p < 0.001 |
Notes: Values represent number or mean ± standard deviation (SD).
Abbreviations: S.D., standard deviation; MDD, major depressive disorder; EPQ-R, Eysenck Personality Questionnaire-revised; PHQ-9, Patient Health Questionnaire-9; n.s., not significant.
Path Analysis
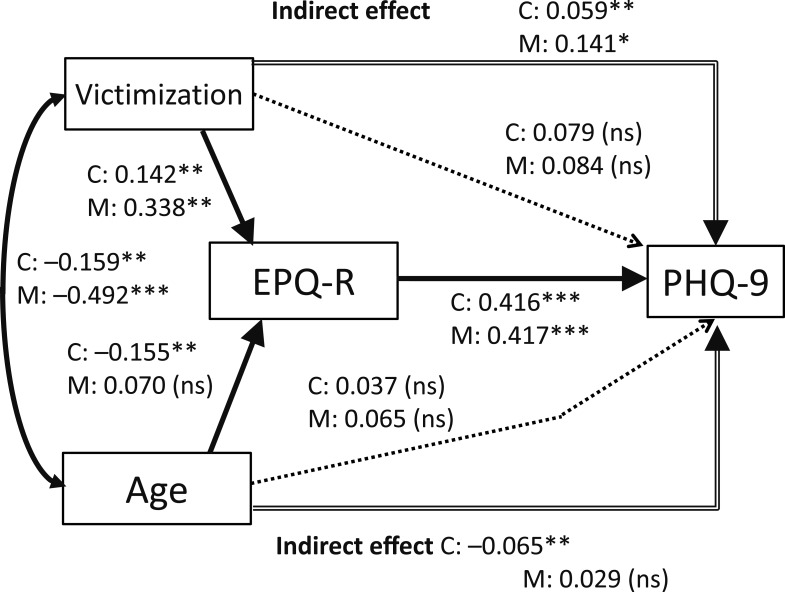
Figure 1 shows the results of multiple group path analysis for healthy controls and MDD patients, in which the severity of depressive symptoms (PHQ-9 score) was the dependent variable, and the effects of victimization, age, and neuroticism on depressive symptoms were analyzed. The paths from the experience of victimization in childhood to neuroticism (EPQ-R score) and the paths from neuroticism to the severity of depressive symptoms were statistically significant for both groups (standardized path coefficient: 0.142 [p = 0.006] and 0.416 [p < 0.001], respectively, for healthy controls; 0.338 [p = 0.003] and 0.417 [p < 0.001], respectively, for MDD patients). The direct paths from the experience of victimization in childhood to the severity of depressive symptoms were not statistically significant for both groups. The indirect paths from the experience of victimization in childhood to depressive symptoms via neuroticism were statistically significant for both groups (standardized path coefficient: 0.059 [p = 0.009] for healthy controls; 0.141 [p = 0.017] for MDD patients). Comparing the nonstandardized coefficients of both groups, only the path coefficient from neuroticism to the severity of depressive symptoms for MDD patients was higher than for healthy controls (p = 0.011), and the differences between both groups in other direct or indirect path coefficients were not statistically significant.
Figure 1.
Results of path analysis of 350 healthy adults and 82 major depressive disorder (MDD) patients with age, victimization, neuroticism (EPQ-R), and depressive symptoms (PHQ-9). The solid arrows represent statistically significant direct paths, and the dotted arrows represent nonsignificant direct paths. The arrows with double lines represent indirect paths from victimization or age to PHQ-9 via neuroticism. The numbers beside the arrows show the standardized path coefficients (minimum: −1; maximum: 1). C, healthy controls; M, MDD patients. *p<0.05, **p < 0.01, ***p < 0.001; ns, not significant.
Among the direct and indirect paths from age, only the direct path to neuroticism for healthy controls and indirect path to the severity of depressive symptoms via neuroticism for healthy controls were statistically significant (standardized path coefficient: –0.155 [p = 0.003] and –0.065 [p = 0.005], respectively).
Therefore, for both healthy controls and MDD patients, the experience of victimization in childhood did not exacerbate their depressive symptoms directly but did so indirectly via its effect on neuroticism, even after considering the effect of age. This model explained 18.5% of the variability of depressive symptoms in healthy controls and 19.6% in MDD patients.
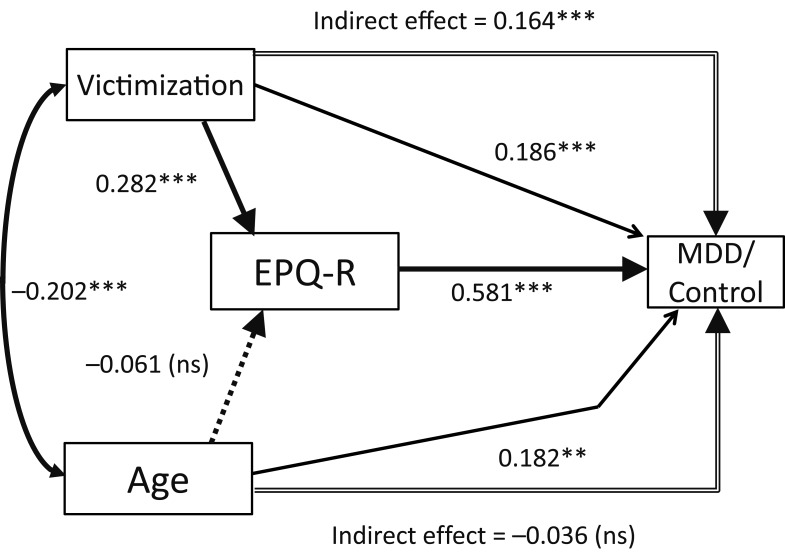
Figure 2 shows the results of path analysis using the distinction between healthy controls and MDD patients (healthy controls = 1, MDD patients = 2) as the dependent variable, and the effects of victimization, age, and neuroticism (EPQ-R score) on the distinction of MDD were analyzed in a group comprising both healthy controls and MDD patients. The path from victimization in childhood to neuroticism and the path from neuroticism to the distinction of MDD were statistically significant (standardized path coefficient: 0.282 [p < 0.001] and 0.581 [p < 0.001], respectively). The direct path from victimization in childhood to the distinction of MDD was statistically significant (standardized path coefficient: 0.186 [p < 0.001]). The indirect path from victimization in childhood to the distinction of MDD via neuroticism was significant (standardized path coefficient: 0.164 [p < 0.001]).
Figure 2.
Results of path analysis of 350 healthy adults and 82 major depressive disorder patients with age, victimization, neuroticism (EPQ-R), and the distinction of MDD (control = 1, MDD = 2). The solid arrows represent statistically significant direct paths, and the dotted arrow represents the nonsignificant direct path. The arrows with double lines represent the indirect paths from victimization or age to the distinction of MDD via neuroticism. The numbers beside the arrows show the standardized path coefficients (minimum: −1; maximum: 1). **p < 0.01, ***p < 0.001; ns, not significant.
Among the direct and indirect paths from age, only the direct path to the distinction of MDD was statistically significant (standardized path coefficient: 0.182 [p = 0.002]). This model explained 43.0% of the distinction between healthy controls and MDD patients.
Multiple Regression Analysis And Logistic Regression Analysis
We conducted multiple regression analyses for the paths of both healthy controls and MDD patients, in which age, sex, marital status, years of education, and employment status were controlled (Figure 1). In these models, the standardized partial regression coefficients of victimization on neuroticism and those of victimization and neuroticism on depressive symptoms were very similar to those of the standardized path coefficients in the path analyses, and the statistical significances were not different (data not shown). This means that the effects of victimization and neuroticism in the path analysis of Figure 1 were not confounded by the above 5 factors.
In Figure 2, we conducted multivariate logistic regression analysis, in which the distinction between healthy controls and MDD patients was the dependent variable, and age, sex, marital status, years of education, employment status, neuroticism, and victimization were the independent variables. In this model, neuroticism and victimization were statistically significant predictors for the distinction of MDD as well as age, sex, and employment status (data not shown). This means that the effects of victimization and neuroticism on the distinction between healthy controls and MDD patients were not confounded by the above 5 factors.
Discussion
The results of our present study suggest that the experience of being victimized in childhood affects depressive symptoms in adulthood via neuroticism in both MDD patients and healthy controls. Regarding the distinction between MDD patients and healthy controls, the experience of being victimized in childhood had a significant indirect effect through neuroticism, as well as a direct effect on the distinction. Therefore, neuroticism plays a different role in depressive symptoms and MDD; neuroticism shows complete mediation of the effect of victimization on depressive symptoms expressed by PHQ-9, but only partial mediation of the effect of victimization on the distinction of MDD. These results imply that there may be personality traits other than neuroticism that mediate the path from the experience of being victimized in childhood to the distinction between MDD patients and healthy controls. In any case, this study is the first study to our knowledge demonstrating the mediating effect of neuroticism on the influence of the experience of being victimized in childhood on the distinction between healthy controls and MDD patients, as well as the severity of depressive symptoms in adulthood by path analysis.
Previous studies have reported the association between the experience of being victimized in childhood and neuroticism. Individuals being victimized are known to have a high level of neuroticism in childhood.19,20 In a survey of adults, the experience of being victimized was shown to lead to high neuroticism.21 Research on a 3-wave-survey with a long interval in a workplace showed that being victimized is associated with increased neuroticism, and neuroticism decreases in the absence of victimization.22 These reports imply that being victimized increases neuroticism.
There have been a few observational studies to date that have investigated the association between the experience of being victimized in childhood and depressive symptoms or the onset of MDD in adulthood. A prospective study by Bowes et al1 showed that the experience of being victimized in childhood increases the onset of MDD in adolescents, and prospective studies by Copeland et al6 and Takizawa et al8 showed an association between being victimized in childhood and MDD in adulthood.
Several studies have analyzed the association between neuroticism and depressive symptoms on the onset of depression. The prospective study by Kendler et al23 showed that a high neuroticism level was associated with a high hazard ratio of the onset of major depressive episodes when stressful life events occurred. The meta-analysis by Liu et al24 also showed that high neuroticism increases the risk of occurrence of depressive symptoms.
Although few studies have analyzed the molecular mechanisms that cause increased neuroticism as a result of victimization, a previous molecular biological study reported that DNA methylation in the glucocorticoid receptor gene (NR3C1) is associated with adverse experiences in childhood, including victimization and depression.25–27 A molecular biological hypothesis of the causal association assumes that being victimized may cause epigenetic changes, which may be expressed as high neuroticism. Further research is warranted to prove this hypothesis.
The limitations of this research are recall bias and the relatively small number of MDD patients. Moreover, as the path analysis of this study was based on retrospective data, it is not possible to confirm the exact causal association between the factors. In the future, long-term prospective studies are necessary to confirm that neuroticism mediates the effects of childhood victimization on adulthood depressive symptoms or the onset of MDD.
In conclusion, this study showed that being victimized in childhood, like the experience of childhood abuse or maltreatment by parents, affects the distinction between healthy controls and MDD patients, as well as the severity of depressive symptoms through neuroticism as a mediating factor. Taking these results together with those of previous studies, systematic evaluation of personality traits, such as neuroticism, and childhood stress, such as the experience of being victimized, abused, and parenting, may contribute to the elucidation of the detailed pathology and mechanism of depressive symptoms in adulthood.
Acknowledgments
This work was partly supported by a Grant-in-Aid for Scientific Research (No. 16K10194, T. Inoue) from the Japanese Ministry of Education, Culture, Sports, Science and Technology, the Research and Development Grants for Comprehensive Research for Persons with Disabilities from Japan Agency for Medical Research and Development, AMED, and SENSHIN Medical Research Foundation.
Author Contributions
S.T. and T.I. designed the study, wrote the protocol, and collected and analyzed the data. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Mayu Naruse has received grants from Mitsubishi Tanabe Pharma Corporation, Public Health Research Foundation, Novartis Pharma K.K., Tokyo Medical University and Japan Society for the Promotion of Science. Jiro Masuya has received personal compensation from Otsuka Pharmaceutical, Eli Lilly, Astellas, and Meiji Yasuda Mental Health Foundation and grants from Pfizer. Masahiko Ichiki has received personal compensation from Otsuka Pharmaceutical, Pfizer, Eli Lilly, Mitsubishi Tanabe Pharma, Mochida Pharmaceutical, Meiji Seika Pharma, Janssen Pharmaceutical, Takeda Pharmaceutical, MSD, Dainippon Sumitomo Pharma, and Eisai; grants from Otsuka Pharmaceutical, Eli Lilly, Eisai, Shionogi, Takeda Pharmaceutical, MSD, and Pfizer; and is a member of the advisory board of Meiji Seika Pharma. Takeshi Inoue has received personal fees from GlaxoSmithKline, Mochida Pharmaceutical, Asahi Kasei Pharma, and Shionogi; grants from Astellas; and grants and personal fees from Otsuka Pharmaceutical, Dainippon Sumitomo Pharma, Eli Lilly, Eisai, Mitsubishi Tanabe Pharma, Pfizer, AbbVie GK, MSD, Yoshitomiyakuhin, Takeda Pharmaceutical, and Meiji Seika Pharma; and is a member of the advisory boards of GlaxoSmithKline, Pfizer, Eli Lilly, Mochida Pharmaceutical and Mitsubishi Tanabe Pharma. The authors report no other conflicts of interest in this work.
References
- 1.Bowes L, Joinson C, Wolke D, Lewis G. Peer victimisation during adolescence and its impact on depression in early adulthood: prospective cohort study in the United Kingdom. Bmj. 2015;350:h2469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lereya ST, Copeland WE, Costello EJ, Wolke D. Adult mental health consequences of peer bullying and maltreatment in childhood: two cohorts in two countries. Lancet Psychiat. 2015;2(6):524–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schaefer JD, Moffitt TE, Arseneault L, et al. Adolescent victimization and early-adult psychopathology: approaching causal inference using a longitudinal twin study to rule out noncausal explanations. Clin Psychol Sci. 2018;6(3):352–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arseneault L. Annual research review: the persistent and pervasive impact of being bullied in childhood and adolescence: implications for policy and practice. J Child Psychol Psychiatry. 2018;59(4):405–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klomek AB, Sourander A, Elonheimo H. Bullying by peers in childhood and effects on psychopathology, suicidality, and criminality in adulthood. Lancet Psychiat. 2015;2(10):930–941. [DOI] [PubMed] [Google Scholar]
- 6.Copeland WE, Wolke D, Angold A, Costello EJ. Adult psychiatric outcomes of bullying and being bullied by peers in childhood and adolescence. JAMA Psychiatry. 2013;70(4):419–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Geoffroy MC, Boivin M, Arseneault L, et al. Childhood trajectories of peer victimization and prediction of mental health outcomes in midadolescence: a longitudinal population-based study. CMAJ. 2018;190(2):E37–E43. doi: 10.1503/cmaj.170219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Takizawa R, Maughan B, Arseneault L. Adult health outcomes of childhood bullying victimization: evidence from a five-decade longitudinal British birth cohort. Am J Psychiatry. 2014;171(7):777–784. [DOI] [PubMed] [Google Scholar]
- 9.Kanai Y, Takaesu Y, Nakai Y, et al. The influence of childhood abuse, adult life events, and affective temperaments on the well-being of the general, nonclinical adult population. Neuropsychiatr Dis Treat. 2016;12:823–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nakai Y, Inoue T, Toda H, et al. The influence of childhood abuse, adult stressful life events and temperaments on depressive symptoms in the nonclinical general adult population. J Affect Disord. 2014;158:101–107. [DOI] [PubMed] [Google Scholar]
- 11.Toda H, Inoue T, Tsunoda T, et al. The structural equation analysis of childhood abuse, adult stressful life events, and temperaments in major depressive disorders and their influence on refractoriness. Neuropsychiatr Dis Treat. 2015;11:2079–2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Toda H, Inoue T, Tsunoda T, et al. Affective temperaments play an important role in the relationship between childhood abuse and depressive symptoms in major depressive disorder. Psychiatry Res. 2018;262:13–19. [DOI] [PubMed] [Google Scholar]
- 13.Jeronimus BF, Ormel J, Aleman A, Penninx BW, Riese H. Negative and positive life events are associated with small but lasting change in neuroticism. Psychol Med. 2013;43(11):2403–2415. [DOI] [PubMed] [Google Scholar]
- 14.Quinlan EB, Barker ED, Luo Q, et al. Peer victimization and its impact on adolescent brain development and psychopathology. Mol Psychiatry. 2018. doi: 10.1038/s41380-018-0297-9 [DOI] [PubMed] [Google Scholar]
- 15.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Washington, D.C.: American Psychiatric Publication Inc.; 2013. [Google Scholar]
- 16.Muramatsu K, Miyaoka H, Kamijima K, et al. The patient health questionnaire, Japanese version: validity according to the mini-international neuropsychiatric interview-plus. Psychol Rep. 2007;101(3 Pt 1):952–960. [DOI] [PubMed] [Google Scholar]
- 17.Eysenck S, Eysenck H, Barrett P. A revised version of the psychoticism scale. Pers Individ Dif. 1985;6:21–29. [Google Scholar]
- 18.National Institute for Educational Policy Research in Japan. Ijime Follow-up Research 2010-2012. Tokyo: National Institute for Educational Policy Research in Japan; 2013. https://www.nier.go.jp/shido/centerhp/2507sien/ijime_research-2010-2012.pdf [Google Scholar]
- 19.Alonso C, Romero E. Aggressors and victims in bullying and cyberbullying: a study of personality profiles using the five-factor model. Span J Psychol. 2017;20:E76. [DOI] [PubMed] [Google Scholar]
- 20.Kodžopeljić J, Smederevac S, Mitrović D, Dinić B, Čolović P. School bullying in adolescence and personality traits: a person-centered approach. J Interpers Violence. 2014;29(4):736–757. [DOI] [PubMed] [Google Scholar]
- 21.Pallesen S, Nielsen MB, Magerøy N, Andreassen CS, Einarsen S. An experimental study on the attribution of personality traits to bullies and targets in a workplace setting. Front Psychol. 2017;8:1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Persson R, Høgh A, Grynderup MB, et al. Relationship between changes in workplace bullying status and the reporting of personality characteristics. J Occup Environ Med. 2016;58(9):902–910. [DOI] [PubMed] [Google Scholar]
- 23.Kendler KS, Kuhn J, Prescott CA. The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. Am J Psychiatry. 2004;161(4):631–636. [DOI] [PubMed] [Google Scholar]
- 24.Liu J, Gill NS, Teodorczuk A, Li ZJ, Sun J. The efficacy of cognitive behavioural therapy in somatoform disorders and medically unexplained physical symptoms: a meta-analysis of randomized controlled trials. J Affect Disord. 2019;245:98–112. [DOI] [PubMed] [Google Scholar]
- 25.Efstathopoulos P, Andersson F, Melas PA. NR3C1 hypermethylation in depressed and bullied adolescents. Transl Psychiatry. 2018;8(1):121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Palma-Gudiel H, Córdova-Palomera A, Leza JC, Fañanás L. Glucocorticoid receptor gene (NR3C1) methylation processes as mediators of early adversity in stress-related disorders causality: a critical review. Neurosci Biobehav Rev. 2015;55:520–535. [DOI] [PubMed] [Google Scholar]
- 27.Turecki G, Meaney MJ. Effects of the social environment and stress on glucocorticoid receptor gene methylation: a systematic review. Biol Psychiatry. 2016;79(2):87–96. [DOI] [PMC free article] [PubMed] [Google Scholar]