Abstract
Periprostatic abscess is a rare complication of hydrogel spacers in radiotherapy for prostate cancer. We present the case of a 61-year-old man who developed this condition. Abdominopelvis CT scan revealed a 54×35×75 mm collection in the location of the SpaceOAR, for which ultrasound-guided transperineal percutaneous drainage of the periprostatic abscess was performed. The patient remains well with serial CT scans showing near resolution of the collection.
Keywords: prostate, urinary tract infections, interventional radiology
Background
The use of hydrogel spacers in radiotherapy for prostate cancer has gained noticeable interest in recent years, allowing administration of higher radiation doses to the prostate while minimising rectal toxicity. Its safety and efficacy has been evaluated in several studies, with very rare spacer-related complications having been reported in literature.1 We present the case of a patient who developed a spacer-related periprostatic abscess.
Case presentation
A 61-year-old man presented to our hospital with purulent urethral discharge, anal pain, fever and a 5 kg weight loss. He had completed a course of external beam radiotherapy (EBRT) for an early organ-confined prostate cancer a few weeks earlier. He had three gold fudicials and a hydrogel spacer (SpaceOAR) inserted transperineally prior to the radiation treatment with conventional antibiotic prophylaxis using cephazolin. His other significant medical history included ulcerative colitis, which was well-controlled and asymptomatic with sulfasalazine 100 mg three times daily.
On examination, he was febrile at 38.1°C with a heart rate of 105 beats/min and blood pressure 135/85 mm Hg. His abdomen was soft but acutely tender in the suprapubic region. He had a tender prostate gland with no evidence of pus or blood in the rectum.
Investigations
Investigation revealed an elevated white cell count of 13×109/L and a C-reactive protein of 149 mg/L. An abdominopelvis CT scan revealed a 54×35×75 mm collection in the location of the SpaceOAR. Subsequent CT cystogram (figure 1) did not reveal any fistulous connection between the collection and the bladder.
Figure 1.
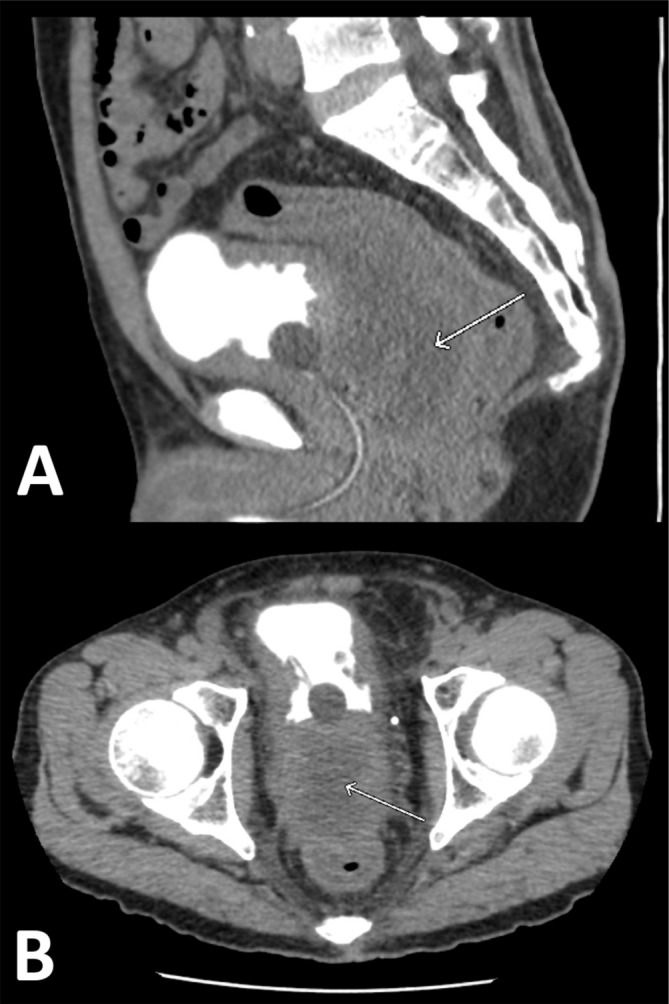
CT cystogram showing the SpaceOAR abscess formation (indicated by the arrow) in the (A) sagittal plane and (B) axial plane.
Differential diagnosis
The patient was assessed as most likely having a periprostatic abscess in the setting of spaceOAR insertion. Differential diagnosis included a rectal fistula given the patient’s history of ulcerative colitis and recent EBRT treatment.
Treatment
The patient underwent ultrasound-guided transperineal percutaneous drainage and drain tube insertion into the periprostatic abscess. Forty cubic centimetres of purulent fluid was aspirated and sent for microscopy and culture. A pigtail drain was inserted for continual drainage (figure 2). Abscess fluid cultured sensitive for Streptococcus anginosus and anaerobes. He also underwent a sigmoidoscopy to exclude a fistulous communication into the rectum. He was treated with a prolonged 5-week course of antibiotics.
Figure 2.

Fluoroscopic image demonstrating the abscess cavity taken at the time of insertion of the transperineal drain tube.
Outcome and follow-up
The pigtail drain was removed at day 14 once the drain output had ceased. Subsequent serial CT scans demonstrated a reduction in size of the collection over the intervening 2 months to 26×27×15 mm. He remained well off antibiotics with no further fevers, pain or urinary symptoms on follow-up.
Discussion
Creating a spacing between the prostate and rectum, the injection of a hydrogel rectal spacer into the anterior perirectal space is a novel approach permitting the administration of higher doses of radiation to the prostate while minimising rectal irradiation, and hence rectal toxicity.1 Its safety and efficacy have been evaluated in randomised phase III studies, with low rates of spacer-related complications reported in literature.2 3 One study reports focal rectal mucosal necrosis as a consequence of inadvertent injection of hydrogel into the rectal wall; this however, resolved completely with no further sequelae.4 Another study reports a case of rectal ulcer, following spacer injection, that resolved without intervention.5 The rate of infection associated with spacer injection was reported as 3% (3/100) in one series.6 7 Two cases were due to bacterial peritonitis and one due to bacterial epididymitis.6 7 To our knowledge, we present the first case of a patient who developed a hydrogel spacer-related periprostatic abscess.
Predisposing factors for developing prostatic abscess include an indwelling catheter, instrumentation of the lower urinary tract, bladder outlet obstruction, acute and chronic bacterial prostatitis and immunocompromised states such as sulfasalazine use in this case.8 Prostatic abscess may progress to fistulisation into the bladder, prostatic urethra, rectum or perineum and in severe cases, lead to sepsis and mortality.8 Accurate diagnosis and prompt treatment are therefore required; however, prostatic abscess has proven challenging to diagnose as it shares the signs and symptoms of other diseases of the lower urinary tract. Imaging, such as transrectal ultrasound and CT of the abdomen and pelvis, is thus crucial for diagnosis and treatment.9 A high index of suspicion is warranted in patients presenting with persistent fever and lower urinary tract symptoms that do not respond to antibiotics.
Prostatic abscesses may be conservatively managed with antibiotics alone or combined with surgical drainage. Surgical drainage is generally recommended in patients with multifocal abscesses >1 cm in diameter, septic shock, recurrent abscess or in patients responding poorly to antibiotics for 72 hours or longer.7 Several methods of surgical drainage via transrectal, transurethral and tranperineal approaches have been described, each with varying efficacy and feasibility.6
The use of hydrogel spacers in radiotherapy for prostate cancer to minimise rectal toxicity has gained noticeable interest in recent years. Abscess formation due to hydrogel spacer is rare. A high index of suspicion and investigation with CT is required for prompt diagnosis and subsequent management.
Learning points.
Abscess formation due to hydrogel spacer is rare.
Prostatic abscesses are challenging to diagnose. Imaging, such as transrectal ultrasound and CT of the abdomen and pelvis, is crucial for diagnosis and treatment.
Surgical drainage should be considered in patients with multifocal abscesses >1 cm in diameter, septic shock, recurrent abscess or in patients responding poorly to antibiotics for 72 hours or longer.
Footnotes
Contributors: VH and HH-IY wrote the manuscript of the case report. MG and JGH supervised the writing of the case, contributing to the clinicopathological information that formed the basis of the case, and critically reviewed and edited the manuscript prior to submission.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Chao M, Ho H, Chan Y, et al. Prospective analysis of hydrogel spacer for patients with prostate cancer undergoing radiotherapy. BJU Int 2018;122:427–33. 10.1111/bju.14192 [DOI] [PubMed] [Google Scholar]
- 2. Pinkawa M. Current role of spacers for prostate cancer radiotherapy. World J Clin Oncol 2015;6:189–93. 10.5306/wjco.v6.i6.189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mak RH, Hunt D, Efstathiou JA, et al. Acute and late urinary toxicity following radiation in men with an intact prostate gland or after a radical prostatectomy: a secondary analysis of RTOG 94-08 and 96-01. Urol Oncol 2016;34:430.e1–7. 10.1016/j.urolonc.2016.04.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Uhl M, Herfarth K, Eble MJ, et al. Absorbable hydrogel spacer use in men undergoing prostate cancer radiotherapy: 12 month toxicity and proctoscopy results of a prospective multicenter phase II trial. Radiat Oncol 2014;9 10.1186/1748-717X-9-96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Teh AYM, Ko H-T, Barr G, et al. Rectal ulcer associated with SpaceOAR hydrogel insertion during prostate brachytherapy. BMJ Case Rep 2014;2014:bcr2014206931 10.1136/bcr-2014-206931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Strom TJ, Wilder RB, Fernandez DC, et al. A dosimetric study of polyethylene glycol hydrogel in 200 prostate cancer patients treated with high-dose rate brachytherapy±intensity modulated radiation therapy. Radiother Oncol 2014;111:126–31. 10.1016/j.radonc.2014.02.011 [DOI] [PubMed] [Google Scholar]
- 7. National Institute for Health and Care Excellence Biodegradable spacer insertion to reduce rectal toxicity during radiotherapy for prostate cancer [Internet]. [London]: NICE; 2019 [updated 2017 Aug; cited 2019 Dec 20]. (International procedures guidance [IPG590]). Available: https://www.nice.org.uk/guidance/IPG590
- 8. Abdelmoteleb H, Rashed F, Hawary A. Management of prostate abscess in the absence of guidelines. Int Braz J Urol 2017;43:835–40. 10.1590/s1677-5538.ibju.2016.0472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jang K, Lee DH, Lee SH, et al. Treatment of prostatic abscess: case collection and comparison of treatment methods. Korean J Urol 2012;53:860–4. 10.4111/kju.2012.53.12.860 [DOI] [PMC free article] [PubMed] [Google Scholar]


