Abstract
Background
Humanitarian emergencies are a major global health challenge with the potential to have a profound impact on people’s mental and psychological health. Effective interventions in humanitarian settings are needed to support the mental health and psychosocial needs of affected populations. To fill this gap, this systematic review synthesises evidence on the effectiveness of a wide range of mental health and psychosocial support (MHPSS) programmes delivered to adults affected by humanitarian emergencies in low and middle-income countries (LMICs).
Methods
A comprehensive search of 12 electronic databases, key websites and citation checking was undertaken in 2015 and updated in May 2018. We included controlled trials published in English from 1980. We extracted data and assessed risk of bias prior to performing a meta-analysis using random effects models. When meta-analysis was not used, we narratively described individual trial effect sizes using forest plots.
Results
Thirty-five studies were included. Overall, MHPSS programmes show benefits in improved functioning and reducing post-traumatic stress disorder. There are also indications from a limited pool of evidence that cognitive–behavioural therapy and narrative exposure therapy may improve mental health conditions. Other psychotherapy modalities also showed a positive trend in favour of MHPSS programmes for improving several mental health outcomes.
Conclusion
In addition to MHPSS programme for improving mental health outcomes in adults affected by humanitarian emergencies in LMICs, there is also a need to generate robust evidence to identify potential impact on broader social dimensions. Doing so could aid the future development of MHPSS programmes and ensure their effective implementation across different humanitarian contexts in LMICs. Future research on MHPSS programmes which focus on basic services and security, community and family programmes, their cost-effectiveness and mechanisms of impact could also strengthen the MHPSS evidence base to better inform policy and practice decision-making in humanitarian settings.
Protocol registration number
CRD42016033578.
Keywords: systematic review: global health, humanitarian crisis, evaluation, mental health, psychosocial intervention
Key questions.
What is already known?
Humanitarian emergencies can have a long-lasting impact on people’s mental health and psychosocial well-being.
Numerous primary studies evaluating mental health and psychosocial support (MHPSS) programmes designed for adults affected by humanitarian emergencies have been evaluated, contributing to our knowledge of what works and why.
What are the new findings?
The evidence consistently shows that MHPSS programmes are effective in improving functioning and post-traumatic stress disorder. However, the effects of some MHPSS programmes on other mental health conditions and psychological well-being are inconclusive.
Future research should aim to investigate the impact of basic services and security, community and family support, and consider outcomes beyond mental health to include social dimensions alongside assessment of cost-effectiveness.
What do the new findings imply?
The findings highlight the importance of considering social, cultural, methodological and ethical issues when designing and implementing MHPSS programmes for different populations and contextual settings. This would allow exploration of the impact and the resources needed to develop resilience, mitigating adverse consequences in humanitarian emergencies.
Introduction
There is growing concern about how to appropriately respond to the needs of populations affected by the humanitarian crisis. By the end of 2017, we have witnessed an unprecedented number of 68.5 million people, who have been forcibly displaced by conflict and violence and more than 95 million people affected by natural disasters.1 2 In addition, the number of people living in low and middle-income countries (LMICs) disproportionally affected by humanitarian emergencies is expected to rise due to recent and protracted conflicts, and the increased likelihood of extreme weather hazards and climate change.3–5 This makes identification of how best to respond to humanitarian emergencies a research priority in addressing the international policy concerns.
Although many retain good mental health, by drawing on individual and social resources to support resilience and protect against the adverse effects of humanitarian emergencies, exposure to short-term and protracted crises can have a long-lasting impact on people’s physical and psychological well-being.6 7 Emergencies can limit an individual’s ability to function and cope with everyday life6 and erode protective services and infrastructure that normally are available to serve their local communities.7 At the same time, it can increase the risk of creating new mental health and psychological problems and intensify any pre-existing individual, family, community or societal difficulties. Addressing these potential impacts is reflected in the scope and aims of mental health and psychosocial support (MHPSS) programmes, which can range from individualised clinical-based approaches to programmes focusing on economic livelihoods and social development.8 MHPSS programmes may vary regarding the extent to which they are developed to serve local populations or may require additional contextual adaptation in order to deliver programmes that meet local needs. For this review, we used the term MHPSS programmes to refer to a broad range of interventions that seek to ‘protect or promote psychosocial well-being and/or prevent or treat mental disorders’6 (p 11).
A considerable amount of evidence synthesis in the field of MHPSS programmes has emerged in the past 5 years, reflecting an increase in primary research and the importance in the field of mental health.9–17 However, only a few have explored the extent to which MHPSS programmes are effective or cause unintended consequences, in humanitarian emergencies, by rigorously evaluating the impact of MHPSS programmes delivered to adults affected by all possible humanitarian emergencies (eg, natural disasters, mass violence and armed conflicts). For example, while one review included 18 trials assessing the impact of psychotherapy (PST) interventions in adult survivors of mass violence they omitted studies conducted in natural disaster settings18; while other reviews limit their scope to narrow outcome domains14 or focus on different populations.15 19 This systematic review contributes to the recent evidence base by systematically reviewing the breadth of MHPSS programmes delivered to adults, affected by any type of humanitarian emergency in LMICs, on a wide range of outcomes.
Methods
Search strategy and selection criteria
We conducted a systematic review following the international standard described in the Cochrane Handbook for Systematic Review of Interventions and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.20 21 The methods were designed a priori with the consultation with an advisory group. We carried out a scoping exercise as part of a broader systematic review to assess the impact of MHPSS programmes on populations affected by humanitarian emergencies. The findings from the scoping exercise informed the focus of this systematic review and the search strategy development.22
We searched 12 bibliographic databases across disciplines: Medline, ERIC, PsycINFO, EconLit, Cochrane Library, IDEAS, IBSS, CINHAL, Scopus, ASSIA, Web of Science and Sociological Abstracts. Specialist databases and websites of relevant organisations were also searched for both published and unpublished literature. Citations of the references in the relevant systematic reviews, and of studies subsequently included in the reviews were inspected for possible inclusion. Search terms were developed iteratively based on the findings from the scoping exercise. Search strings were tailored and adapted for each database using a combination of three key aspects of the systematic review: ‘humanitarian emergencies’, ‘mental health and psychosocial’ and ‘study design’. The database searches were finalised in November 2015 and websites in June 2016. We updated the search in May 2018. (See online supplementary file A for Medline search strategy.)
bmjgh-2019-001484supp001.pdf (81.3KB, pdf)
We included controlled trials, which evaluated the impact of MHPSS programmes on adult populations affected by any type of humanitarian emergencies in LMICs. For this review, the term ‘humanitarian emergencies’ refers to natural (eg, earthquakes, landslides, storms or extreme weathers) and/or man-made (eg, political violence and armed conflicts) disasters. There was no restriction on the outcomes of interest. However, we only considered studies if they were published in English in or after 1980 as this was when the humanitarian community started to design and deliver MHPSS services to populations affected by conflicts.23 24 The studies that evaluated MHPSS programmes designed for military personnel or people working in the context of humanitarian emergencies were excluded.
The inclusion and exclusion criteria were piloted by two review team members (KD and MB). The guidance notes were used to assist reviewers to make decisions consistently and any disagreement was resolved through discussion between the review team members. We initially screened each study on the basis of titles and abstracts. When there was insufficient information to make a judgement, full reports were retrieved and then rescreened by the same reviewers.
Data extraction and risk of bias assessment
The data were extracted from the included studies using a data extraction tool developed and piloted by two systematic reviewers (MB and KD). The pilot process aimed to consider whether (A) all essential information was captured or (B) additional guidance was required. Information extracted included study and population characteristics (aim, country, type of humanitarian crises, gender, age group, or other sociodemographic information), study design (unit of allocation, actual sample size, allocation procedure, type of control group, data collection and analysis methods, attrition), description of MHPSS programmes (focus of the interventions, programme design and component, implementation and delivery process, programme intensity or duration), outcome measures and findings. The second reviewer also checked the information and findings extracted from the included studies to ensure accuracy and comprehensiveness.
Two review authors (MB and LF) assessed the risk of bias of the included studies following the procedure outlined in the Cochrane Handbook for Systematic Reviews of Interventions.21 We assessed the risk of bias according to the following domains: (A) random sequence generation; (B) allocation concealment; (C) blinding of participants and personnel; (D) blinding of outcome assessment; (E) incomplete outcome data; (F) selective outcome reporting; and (G) other bias. We judged each potential source of bias as high, low or unclear. Any disagreements were resolved by discussion with the third review member (KD).
Data analysis and synthesis
We developed synthetic narrative statements and organised the impact of MHPSS programme by the characteristics of the included studies and the outcomes reported. In this review, we developed a conceptual framework by drawing on definitions of MHPSS used in the included studies and the broader literature. This enabled us to meaningfully ‘match’ and ‘group’ studies against our definitions prior to synthesis. This resulted in classifying studies into five broad MHPSS programme domains, based on their shared programme components and approaches to addressing the mental health and psychosocial needs of adult populations affected by humanitarian emergencies. These domains included: cognitive–behavioural therapy (CBT), narrative exposure therapy (NET), ‘other’ PST modalities, psychosocial programmes and psychoeducation (see table 1).
Table 1.
Types of MHPSS programmes
| MHPSS programmes | Key components |
| Cognitive–behavioural therapy (CBT) |
|
| Narrative exposure therapy (NET) |
|
| Other psychotherapy modalities |
|
| Psychosocial programmes |
|
| Psychoeducation |
|
MHPSS, mental health and psychosocial support.
We calculated and reported the standardised mean difference (SMD) and their SD to combine outcomes that were measured using different scales. We used SMD to calculate the pooled effect size and a random effects model to run the meta-analysis. The results are summarised in forest plots with a 95% CI. As we had no responses from the study authors when trying to obtain missing data, we computed from other reported data including CI, t-statistics, SE or p value, or imputed the missing SD using the SD of reported ‘baseline’ scores available in each study. When there were multiple time point assessments, outcomes from the longest available follow-up were used.
The individual data were used as the unit of analysis in the meta-analysis. The heterogeneity was assessed using the χ2 test. Meta-analysis was performed when studies reported conceptually similar outcomes and programme design. When meta-analysis was deemed to be inappropriate due to heterogeneity, we presented individual trial effect sizes using forest plots and narratively reported the findings.
Summary of evidence
We assessed the extent to which the overall summary of the evidence is trustworthy in addressing the review question by considering three main dimensions of that body of evidence:
(A) Quality: This dimension is to consider the overall quality of the evidence in drawing overall conclusions. We used the risk of bias dimensions to summarise the overall risk of bias as follows:
Low-risk study
Selection bias and attrition bias, both domains must be rated as the low risk of bias, and;
No other high risk of bias in other domains.
Moderate - risk study
Selection bias or attrition bias domain must be rated to be unclear, or;
Selection bias and attrition bias, both domains must be rated as the low risk of bias but one or more other domains were judged to be high risk of bias.
High - risk study
Selection bias or attrition bias domain must be rated as the high risk of bias.
(B) Size: We considered whether there is sufficient evidence for drawing overall conclusions. This is based on a minimum number of low-risk studies considered in a particular outcome.
(C) Consistency: We considered the degree of similarity in the effect sizes across the included studies. We used the heterogeneity test (I2) to indicate whether a body of evidence is not sufficiently consistent (I2>50%) or when there is a low degree of overlap in CIs in each study.
Based on the three dimensions and the previous work in the field of public health, we developed a framework to assess the strength of the evidence summary of each outcome25–28 (see online supplementary file B). All studies identified from the search were imported into the systematic review software EPPI-Reviewer V.4,29 where the screening, data extraction, quality assessment and meta-analysis were performed. Two reviewers (MB and KD) made decisions about the classification of MHPSS programmes, quality assessment and summary of evidence.
bmjgh-2019-001484supp002.pdf (34KB, pdf)
Patient and public involvement
Patients were not involved in this study.
Results
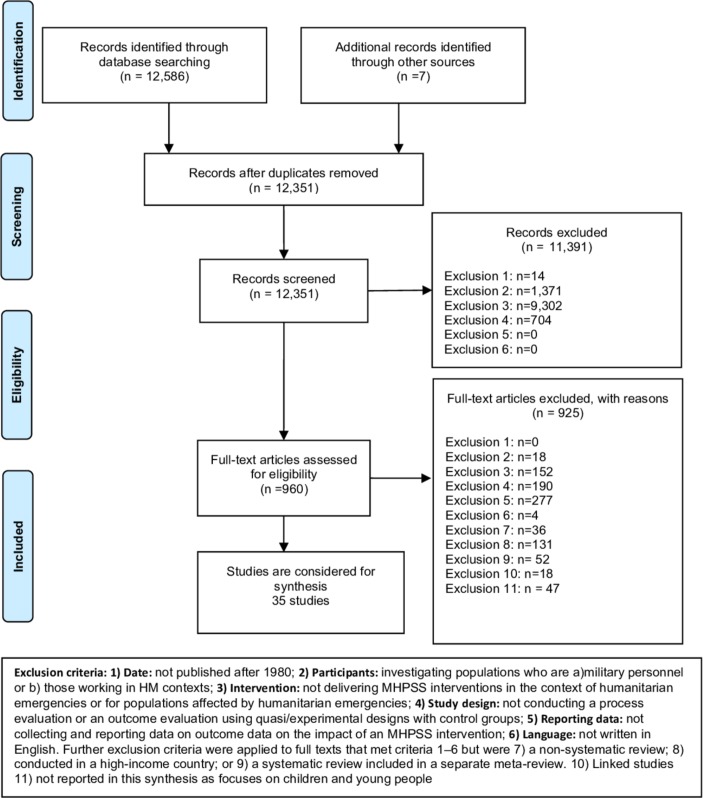
Searches generated a total of 12 593 references, with 242 citations removed as duplicates. References were screened on title and abstract. We obtained and rescreened the full-text reports of all remaining 960 citations, excluding a further 925 citations at the screening stage. This resulted in 35 studies being included in this review (see figure 1).
Figure 1.
Summary of the flow of studies through the review. MHPSS, mental health and psychosocial support; HM, Humanitarian Emergencies
Characteristics of MHPSS programmes
We identified 35 studies assessing the impact of MHPSS programmes on adult populations affected by humanitarian emergencies in 19 countries. The majority of the MHPSS programmes were delivered to participants on a one-to-one basis (n=26); eight studies were delivered in a group format.30–37 One study evaluated the impact of a group yoga intervention with one-to-one exposure therapy on survivors of East Asian Tsunami.38 Ten were delivered in clinics34 39–47; four were based in the community32 35 42 48; three were delivered in refugee camps36 49 50; and three at participants’ homes.51–53 In one MHPSS programme, participants received the intervention at home, clinic or in the community.54 Fourteen studies did not clearly specify the delivery setting. With limited human resources available in LMICs, nearly half of the MHPSS programmes were delivered by paraprofessionals or trained local community workers, or volunteers.31 32 34–38 42 45 46 48 50 52–56
The MHPSS programmes included in the review used a combination of techniques, including sessions for participants to share and discuss traumatic experiences, provide psychoeducation, psychosocial support, and/or to teach relaxation techniques. Two43 44 programmes offered medication as part of their intervention components; and the other two programmes30 36 were developed collaboratively with local community members.
The majority of MHPSS programmes were implemented in man-made disaster settings across 11 countries in sub-Saharan Africa, Asia, Eastern Europe and Middle East (n=19). A quarter of the studies were conducted in three countries, India (n=4), China (n=3) and Turkey (n=3), to evaluate the impact of MHPSS programmes affected by natural disasters. The impact of MHPSS programmes was investigated in refugee camps in four countries (Uganda, Turkey, Thailand and Egypt). We identified four studies31–33 40 evaluating MHPSS programmes that included only women and only one study55 included only male participants in a yoga intervention.
The MHPSS programmes lasted on average between 4 and 13 sessions, each for approximately 1–2 hours, and over 2–12 weeks. We identified four brief MHPSS programmes where they delivered in one or two sessions for 1 hour or less per session.41 53 57 58 One study conducted by Yeomans and colleagues37 evaluated a 3-day reconciliation workshop for Burundian participants. Nearly three-quarters of the studies included in the review evaluated the impact of the MHPSS programmes compared with wait-list controlled groups (n=25), four with treatment as usual, five with other active interventions and seven compared with no intervention groups. Of 35 studies, six had more than one intervention arm.37 38 44 46 49 50 Twenty-five studies were randomised controlled trials (RCT); one study was a clustered RCT, assigning participants into groups by village,31 and nine used a non-randomisation process to allocate participants to groups. The majority of the study measured the impact of MHPSS programmes at immediately or short-term follow-ups at 3 months (n=32). Only one study assessed the impact of MHPSS at more than 1 year.41 (See further details in online supplementary file C.)
bmjgh-2019-001484supp003.pdf (104KB, pdf)
The impact of MHPSS programmes on adults
Cognitive–behavioural therapy
This group of nine studies includes MHPSS programmes that encompass both trauma-focused CBT and those adapting CBT for populations with different needs. Two studies assessed a single-session CBT intervention designed for survivors of the 1999 earthquake in Turkey.41 57 Other studies reported the impact of adapted CBT combined with other different approaches, including: a CBT intervention designed for survivors of terrorist attacks in southern Thailand59; a dialogical exposure programme for women who had lost their husbands during the war in Bosnia and Herzegovina33; a cognitive processing therapy (CPT) designed for female survivors of sexual violence31; a transdiagnostic community-based mental health treatment delivered to refugees in Thailand54; the Problem Management Plus programme delivered by lay health workers in primary care settings in Pakistan45; a transdiagnostic intervention, Common Elements Treatment Approach (CETA) and CPT compared with a wait-list controlled group46; a trauma-focused CBT adults in postconflict Timor-Leste60; and a culturally sensitive CBT-based intervention (EMPOWER) designed for war-affected adults in Uganda.36
The finding from the meta-analysis of CBT studies showed that with limited evidence, CBT might reduce post-traumatic stress disorder (PTSD), depression, anxiety symptoms and grief, and may improve functioning. There is insufficient evidence to support that CBT would have an impact on reducing anger, conduct and emotional problems, and fear and avoidance symptoms (see table 2).
Table 2.
A summary of evidence of CBT
| Outcomes | Number of studies, Number of participants(n) and a summary risk of bias | Findings and heterogeneity | Strength of evidence |
| PTSD | 8 studies; n=1484 Three low risks of bias studies |
Pooled SMD=−0.66; 95% CI (−0.87 to −0.44); Q=22.0935; df=8; p=0.0047; I2=63.8%; tau-squared=0.0627 | Limited |
| Depression | 7 studies; n=1162 Three low risks of bias studies |
Pooled SMD=−0.69; 95% CI (−0.98 to −0.39); Q=31.585; df=7; p=04.85E-5; I2=77.84%; tau-squared=0.1247 | Limited |
| Functional impairment | 6 studies; n=1337 Two low risks of bias studies |
Pooled SMD=−0.57; 95% CI (−0.83 to−0.31); Q=22.322; df=6; p=0.001; I2=73.12%; tau-squared=0.0842 | Limited |
| Anxiety | 4 studies; n=1044 Two low risks of bias studies |
Pooled SMD=−0.71; 95% CI (−0.96 to−0.45); Q=14.51; df=4; p=0.0058, I2=72.44%; tau-squared=0.0582 | Limited |
| Grief | 2 studies; n=147 One low risk of bias study |
Pooled SMD=−0.23; 95% CI (−0.63 to 0.16); Q=0.227; df=1; p=0.634; I2=0%; tau-squared=0 | Limited |
Negative sign of pooled SMD indicates a positive effect of CBT.
CBT, cognitive–behavioural therapy; n, number of participants; PTSD, post-traumatic stress disorder; SMD, standardised mean difference.
Narrative exposure therapy
Eight studies assessed the impact of NET. All but one study51 were delivered to participants individually. Of the eight studies, two were delivered to survivors of the 2008 Sichuan earthquake in China,61 62 and further two evaluated the impact of NET in refugee settlements in Uganda49 50; one study evaluated its impact on former political detainees in Romania56; one on widowed and orphaned survivors of the Rwandan genocide51; one on survivors of civil war53; and one delivered culturally adapted testimony therapy in Cambodia.63
The findings from the meta-analysis suggested that NET may reduce PTSD, depression and anxiety symptoms. One study providing a brief testimony therapy in Cambodia reported a short-term improvement at 3 months on PTSD, depression and anxiety symptoms; however, there was no significant difference between the treatment and control groups when these outcomes were assessed at 6-month follow-up.63 On other outcomes, NET may also reduce common mental health problems and probably has little impact on social support. The impact of NET on emotional problems and coping based on one study is inconclusive (see table 3).
Table 3.
A summary of evidence of NET
| Outcomes | Number of studies, number of participants (n) and a summary risk of bias | Findings and heterogeneity | Strength of evidence |
| PTSD | 7 studies; n=650 Four low risks of bias studies |
Pooled SMD=−0.96; 95% CI (−1.55 to −0.36); Q=40.6; df=7; p = 9.62E-7; I2=82.8%; tau-squared=0.498 | Limited |
| Depression | 4 studies; n=146 Three low risks of bias studies |
Pooled SMD=−0.82; 95% CI (−1.69 to 0.05); Q=19.5046; df=4; p=0.0006; I2=79.49%; tau-squared=0.7517 | Limited |
| Anxiety | 3 studies; n=128 Three low risks of bias studies |
Pooled SMD=−0.90; 95% CI (−1.87 to 0.07); Q=14.0716; df=3; p=0.0028; I2=78.68%; tau-squared=0.7290 | Limited |
| Common mental health symptoms | 4 studies; n=301 Three low risks of bias studies |
Pooled SMD=−1.27; 95% CI (−2.31 to−0.23) Q=25.2; df=4; p=4.53E-5; I2=84.1%; tau-squared=1.12 |
Limited |
| Social support | 2 studies; n=52 Two low risks of bias studies |
Pooled SMD=0.08; 95% CI (−0.49 to 0.64); Q=0.627; df=2; p=0.731; I2=0%; tau-squared=0 | Moderate |
| Coping | 1 studies; n=22 One low risk of bias study |
Effect size=0.31; 95% CI (−0.53 to 1.16) | Limited |
| Emotional problems (a comorbidity of mental health symptoms) | 1 study; n=43 One low risk of bias study |
Effect size=0.48; 95% CI (−0.32 to 1.28) | Limited |
Negative sign of pooled SMD indicates a positive effect of mental health and psychosocial support (MHPSS), except for social support and coping.
n, number of participants; NET, narrative exposure therapy; PTSD, post-traumatic stress disorder; SMD, standardised mean difference.
Psychotherapy
We identified 18 PST programmes, each of which took a range of different therapeutic approaches to address broad psychological concerns such as questions of meaning, social connectedness and depression. These programmes sought to work on a verbal and non-verbal level, aiming to address the intrapsychic and interpersonal impact of humanitarian crises and increase overall psychological functioning and coping skills. The majority of the PST were supportive counselling.30 34 40 42 49 50 52 One study in Sierra Leone evaluated the impact of drug treatment with counselling.43 Two studies assessed the impact of interpersonal psychotherapy, one on Sudanese refugees living in Cairo and the other on the survivors of the 2008 Sichuan earthquake in China.48 64 Two studies focused on mind-body therapies such as yoga in natural disaster settings.38 55 One study each evaluated the impact of the eye movement desensitisation and reprocessing (EMDR) programme on Syrians in a refugee camp in Turkey39; the resource-oriented trauma therapy with EMDR in Cambodia47; thought field therapy, a brief intervention designed for Rwandan genocide survivors58; reconciliation workshop in Burundi37; sociotherapy in Rwanda35; and psychosocial care for women survivors of humanitarian disasters in India.32
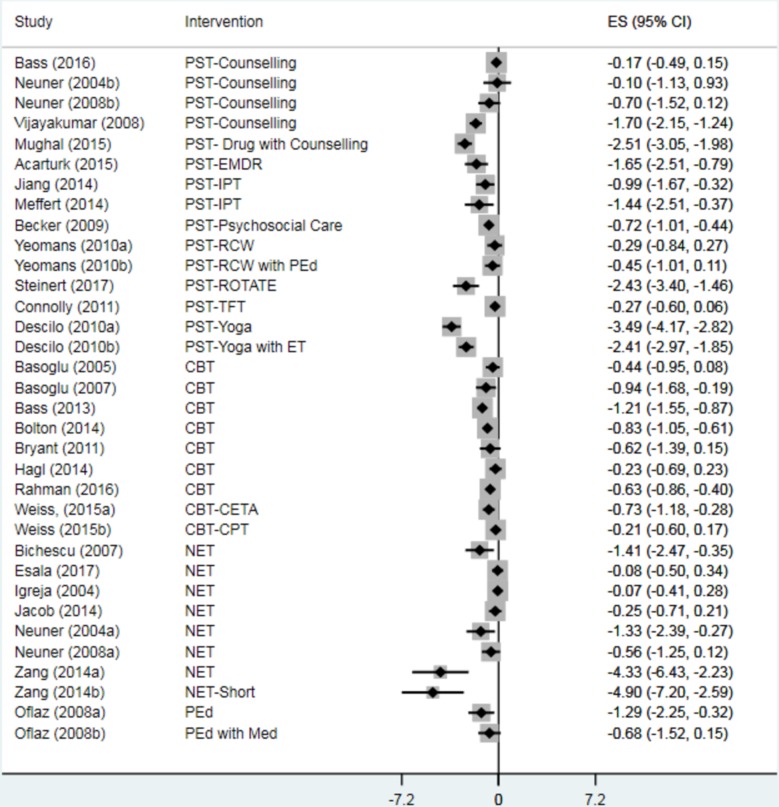
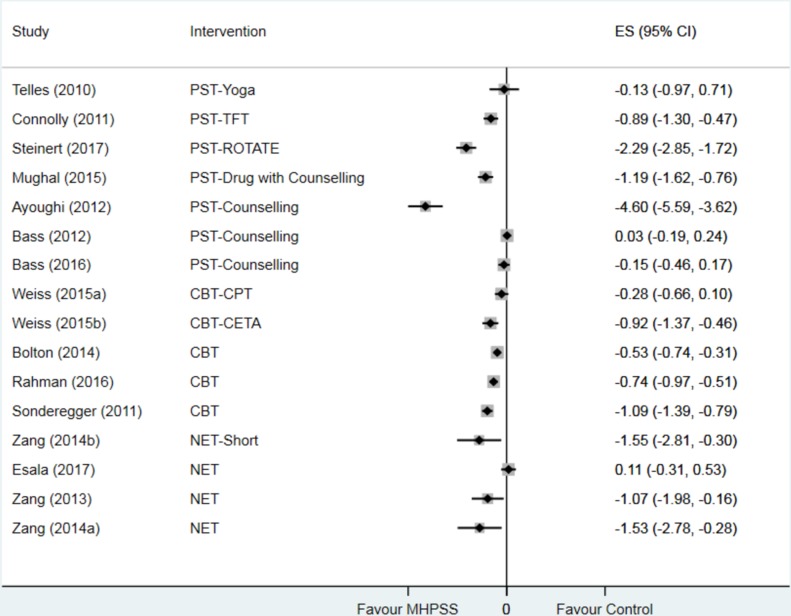
Due to heterogeneity, we presented the individual trial effect sizes using forest plots and narratively reported the effects of PST on relevant outcomes. Thirteen studies evaluating PST reported the positive effects on PTSD symptoms.32 37–39 42 43 47–50 52 58 64 Of these, eight studies reported a significant difference between groups, all in favour of PST (SMD ranging from −3.49, 95% CI −4.17 to −2.82, to SMD −0.10, 95% CI −1.13 to 0.93) (figure 2).
Figure 2.
The impact of mental health and psychosocial support (MHPSS) on post-traumatic stress disorder (PTSD; 27 studies). CBT, cognitive–behavioural therapy; CETA, transdiagnostic intervention, Common Elements Treatment Approach; CPT, cognitive processing therapy; EMDR, eye movement desensitisation and reprocessing; ET, exposure therapy; IPT, interpersonal psychotherapy; Med, medication; NET, narrative exposure therapy; PEd, psychoeducation; PST, psychotherapy; RCW, reconciliation workshop; ROTATE, resource-oriented trauma therapy with EMDR; TFT, thought field therapy.
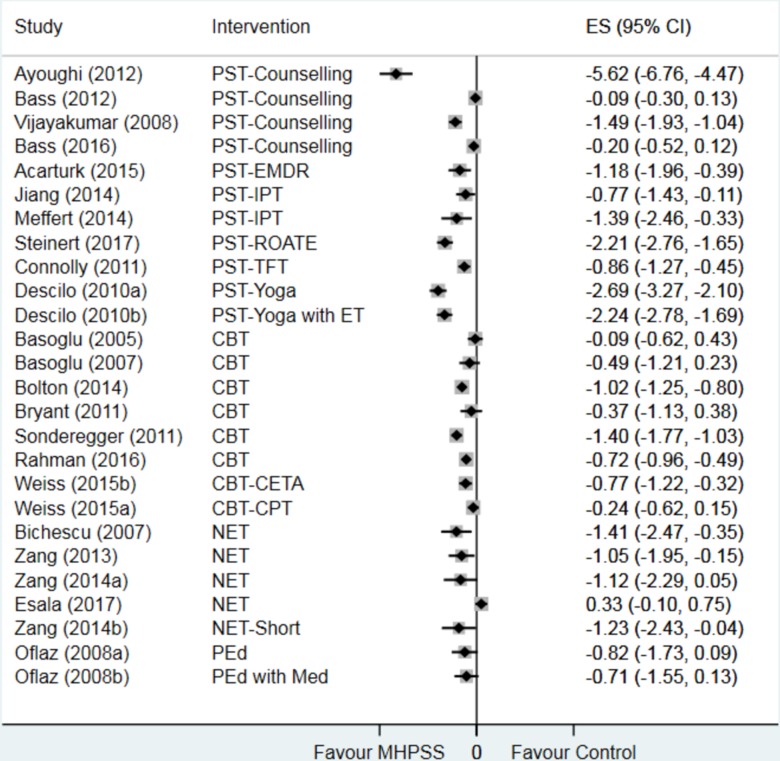
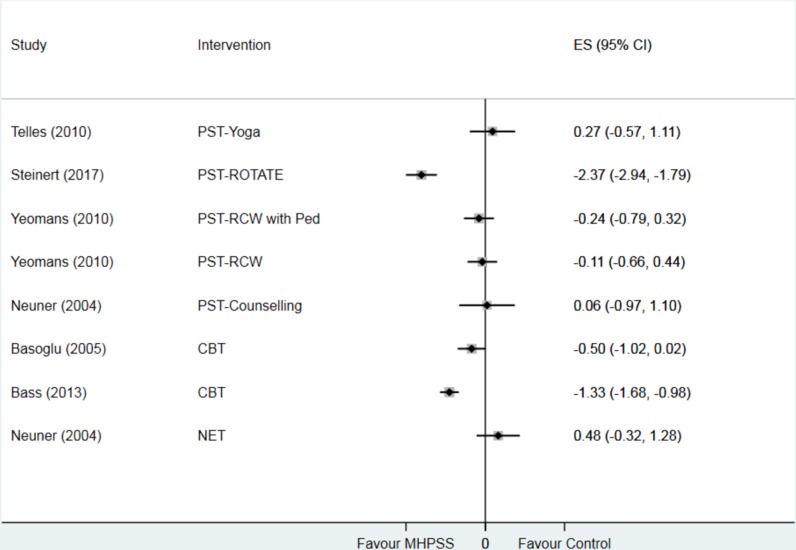
We also observed a positive trend in improving depression in 10 studies.30 38–40 42 47 48 58 64 Of these, eight studies reported a significant reduction in depression symptoms in the intervention groups compared with the control groups (SMD ranging from −5.62, 95% CI −6.76 to −4.47, to SMD −0.77, 95% CI −1.43 to −0.11)(figure 3).
Figure 3.
The impact of MHPSS on depression (21 studies). CBT, cognitive–behavioural therapy; CETA, transdiagnostic intervention, Common Elements Treatment Approach; CPT, cognitive processing therapy; EMDR, eye movement desensitisation and reprocessing; ET, exposure therapy; IPT, interpersonal psychotherapy; Med, medication; MHPSS, mental health and psychosocial support; NET, narrative exposure therapy; PEd, psychoeducation; PST, psychotherapy; ROTATE, resource-oriented trauma therapy with EMDR; TFT, thought field therapy.
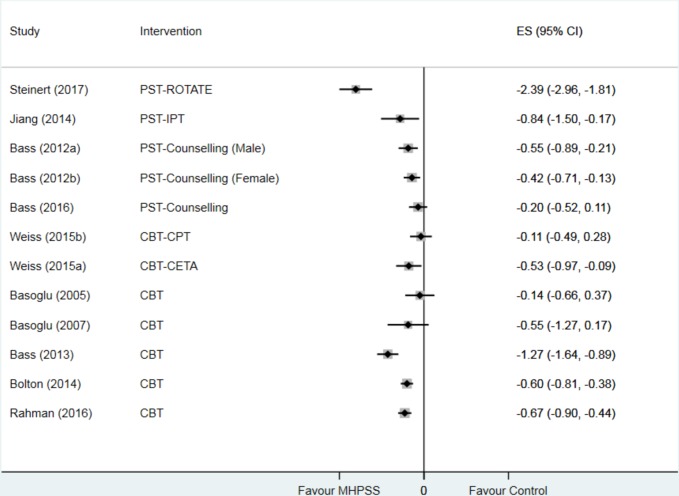
Three of four studies30 47 64 that reported the impact of PST on functioning showed a significant improvement at end-point measurement in the intervention groups compared with the control group (SMD ranging from −2.39, 95% CI −2.96 to −1.81, to SMD −0.42, 95% CI −0.71 to −0.13) (figure 4). Other studies also suggested there were benefits from participating in PST on other outcomes including anger,48 58 64 somatic symptoms,30 partner violence,48 64 fear and avoidance55 58, grief42 and coping.30 40
Figure 4.
Impact of MHPSS on functioning (10 studies). CBT, cognitive–behavioural therapy; CETA, transdiagnostic intervention, Common Elements Treatment Approach; CPT, cognitive processing therapy; IPT, interpersonal psychotherapy; MHPSS, mental health and psychosocial support; PST, psychotherapy; ROTATE, resource-oriented trauma therapy with EMDR.
However, evidence on the impact of PST on anxiety and emotional problems is mixed. Four studies40 43 47 58 showed a significant reduction in anxiety symptoms (SMD ranging from −4.60, 95% CI −5.59 to −3.62, to SMD −0.89, 95% CI −1.30 to −0.47). Two studies found no significant reduction in anxiety symptoms in treatment groups when compared with the control groups.42 55 Bass et al 30 investigated the impact of problem-solving counselling in 589 adults in postconflict settings in Indonesia and found a small, non-significant increase in anxiety symptoms in the adults receiving the intervention (figure 5). For emotional problems, only one study reported a significant improvement.47 Two of the three studies showed a non-significant unintended impact of yoga55 and counselling interventions on emotional problems when compared with the control groups49 (figure 6).
Figure 5.
Impact of MHPSS on anxiety (14 studies). CBT, cognitive–behavioural therapy; CETA, transdiagnostic intervention, Common Elements Treatment Approach; CPT, cognitive processing therapy; MHPSS, mental health and psychosocial support; NET, narrative exposure therapy; PST, psychotherapy; ROTATE, resource-oriented trauma therapy with EMDR; TFT, thought field therapy.
Figure 6.
Impact of MHPSS on emotional problems (seven studies). CBT, cognitive–behavioural therapy; MHPSS, mental health and psychosocial support; NET, narrative exposure therapy; PEd, psychoeducation; PST, psychotherapy; RCW, reconciliation workshop; ROTATE, resource-oriented trauma therapy with EMDR.
Psychoeducation
We found one study that evaluated the impact of psychoeducation intervention only and psychoeducation with medication compared with medication only group.44 The intervention was delivered in six sessions (60–90 min), focusing on problem solving to improve PTSD and coping. The findings suggested that psychoeducation only programme could reduce PTSD symptoms (SMD=−1.29; 95% CI −2.25 to −0.32)(figure 2). In addition, the results were shown that psychoeducation only programme or psychoeducation with medication may reduce depression, fear and avoidance symptoms compared with the medication only control group, although the effects were not statistically significant.
Discussion
We included 35 trials evaluating the impact of MHPSS programmes on adults affected by humanitarian emergencies on a wide range of outcomes. It is clear from the available data that there is a positive trend in favour of MHPSS programmes in reducing PTSD symptoms and improving functioning. When examining the effect of MHPSS by programme type, there are indications that CBT and NET programmes may reduce PTSD, depression and anxiety symptoms, consistent with previous research in similar populations and settings.65–67 For other outcomes, the findings, based on a small number of studies, suggest that CBT may improve functioning and slightly reduce grief. NET probably has no impact on perceived social support. The impact of NET on emotional problems and coping is inconclusive.
We address an important research gap in the field by systematically assessing recent evidence from trials on the impact of MHPSS programmes delivered to adults affected by humanitarian emergencies in LMICs. We extensively searched and included unpublished and published literature that investigated the impact of MHPSS programmes in natural and man-made contexts. In taking this approach we also encountered some common review limitations when undertaking a broad synthesis of the evidence. For example, based on our comprehensive search, we were able to identify a substantial literature, highlighting the extensive range of MHPSS evaluated and delivered across different humanitarian contexts in LMICs, reflecting the growing body of evidence, in the field in recent years. However, this can be a challenge when attempting to synthesise research findings from a wide range of programme designs and implementation approaches, and from studies assessing common outcomes using different measures.
Furthermore, we included many studies that evaluated MHPSS programmes with multiple components to address complex presentations and issues in the field. In some cases, the studies provided only a name of the intervention with limited descriptions of the MHPSS programmes and their components. This posed a challenge when allocating studies to programme domains. To address this issue, first the review authors read the author descriptions as outlined in the study, and matched those descriptions against initial review-specific programme grouping definitions devised by a review author (KD). We then discussed and refined these definitions iteratively as a team to reach final agreements. Subsequently, the review authors read and re-read the descriptions of the studies and reapplied the definitions to studies, until all study groupings were agreed between authors.68
Some notable gaps and recommendations arise from our systematic review. First, we identified only a few studies evaluating the impact of MHPSS programmes focusing on basic services and security, community and family support provision, echoing previous research.11 19 Second, there is a variation of measurement tools to assess common outcomes. This highlights a potentially critical limitation in study designs, and a need for more culturally adapted and validated tools for use across different linguistic and sociocultural contexts. Third, less frequently reported in the studies was psychosocial well-being, such as resilience, hopefulness, social support or coping strategies. It is important that these outcomes are considered when assessing the impact of MHPSS programmes along with other self-reported outcomes. This would allow exploration of the impact of the interventions that extend beyond mental health problems to focus on mental health well-being and the resources individuals need to mitigate the impact of humanitarian emergencies at individual, social and structural levels.69 70 Fourth, we did not identify any research meeting our inclusion criteria that reported cost-effectiveness of MHPSS programmes in adult populations. Finally, there is the need to actively consider the context in which programmes are delivered, for example, by articulating, reporting and critically assessing MHPSS programme pathways to impact.71 Humanitarian crises often occur in the low-resource settings where the implementation of many effective approaches designed for Western contexts may limit their effectiveness.72 Recent methodological development efforts have been made to address the challenges in designing contextually sensitive humanitarian responses and evaluating complex interventions in development.16 73 Adopting these approaches offers an opportunity to enhance understanding of the factors affecting intervention effectiveness to inform the design and implementation of programmes, supporting the mental health needs of adults in different contexts and minimising unintended consequences.
Acknowledgments
We thank Dr Anna Chiumento who offered guidance on mental health research for the review and provided feedback on the first draft of the review.
Footnotes
Handling editor: Seye Abimbola
Contributors: MB and KD designed the study, and developed and wrote the initial draft of the protocol. LF led on writing the method section of the meta-analysis. All authors contributed to writing the final version of the review. MB managed the overall project. MB and KD developed the search strategy, retrieved the full texts and screened all the studies. MB and LF performed data extraction and quality assessment of the included studies. MB and KD planned the analysis. MB and LF performed the meta-analysis. MB wrote the initial draft of the manuscript with all the other authors who contributed subsequent versions.
Funding: This study received financial support from the Humanitarian Evidence Programme, a partnership between Oxfam GB and Feinstein International Centre at Friedman School of Nutrition Science and Policy, Tufts University, funded by the UK Department for International Development.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: There are no data in this work.
References
- 1. UNHCR Global trends: forced displacement in 2017. Geneva: United Nations High Commissioner for Refugees, 2018. [Google Scholar]
- 2. OCHA World humanitarian: data and trends 2017. United Nations Office for the Coordination of Humanitarian Affairs, 2018. [Google Scholar]
- 3. Who Building back better: sustainable mental health care after emergencies. World Health Organization, 2013. [Google Scholar]
- 4. Eapsg Prioritization of themes and research questions for health outcomes in natural disasters, humanitarian crises or other major healthcare emergencies. PLOS Currents Disasters, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Walker P, Glasser J, Kambli S. Climate change as a driver of humanitarian crises and response. Fienstien International Centre, 2012. [Google Scholar]
- 6. Iasc Guidelines on mental health and psychosocial support in emergency setting. Geneva: IASC, 2007: 0042–9686. [Google Scholar]
- 7. Colliard C, Bizouerne C C. The psychosocial impact of humanitarian crise: a better understanding for better interventions. ACF-International. [Google Scholar]
- 8. van Ommeren M, Saxena S, Saraceno B. Mental and social health during and after acute emergencies: emerging consensus? Bull World Health Organ 2005;83:71–5. discussion 5-6 doi:/S0042-96862005000100017 [PMC free article] [PubMed] [Google Scholar]
- 9. Gouweloos J, Dückers M, te Brake H, et al. Psychosocial care to affected citizens and communities in case of CBRN incidents: a systematic review. Environ Int 2014;72:46–65. 10.1016/j.envint.2014.02.009 [DOI] [PubMed] [Google Scholar]
- 10. Siriwardhana C, Ali SS, Roberts B, et al. A systematic review of resilience and mental health outcomes of conflict-driven adult forced migrants. Confl Health 2014;8:13 eCollection 2014 10.1186/1752-1505-8-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tol WA, Barbui C, Galappatti A, et al. Mental health and psychosocial support in humanitarian settings: linking practice and research. The Lancet 2011;378:1581–91. 10.1016/S0140-6736(11)61094-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Burkey MD, Hosein M, Morton I, et al. Psychosocial interventions for disruptive behaviour problems in children in low- and middle-income countries: a systematic review and meta-analysis. J Child Psychol Psychiatr 2018;59:982–93. 10.1111/jcpp.12894 [DOI] [PubMed] [Google Scholar]
- 13. Purgato M, Gastaldon C, Papola D, et al. Psychological therapies for the treatment of mental disorders in low- and middle-income countries affected by humanitarian crises. Cochrane Database Syst Rev 2018;7 10.1002/14651858.CD011849.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Purgato M, Gross AL, Betancourt T, et al. Focused psychosocial interventions for children in low-resource humanitarian settings: a systematic review and individual participant data meta-analysis. Lancet Glob Health 2018;6:e390–400. 10.1016/S2214-109X(18)30046-9 [DOI] [PubMed] [Google Scholar]
- 15. Strohmeier H, Scholte WF. Trauma-Related mental health problems among national humanitarian staff: a systematic review of the literature. Eur J Psychotraumatol 2015;6:28541 10.3402/ejpt.v6.28541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Greene MC, Jordans MJD, Kohrt BA, et al. Addressing culture and context in humanitarian response: preparing desk reviews to inform mental health and psychosocial support. Confl Health 2017;11:21 10.1186/s13031-017-0123-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Augustinavicius JL, Greene MC, Lakin DP, et al. Monitoring and evaluation of mental health and psychosocial support programs in humanitarian settings: a scoping review of terminology and focus. Confl Health 2018;12:9 10.1186/s13031-018-0146-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Morina N, Malek M, Nickerson A, et al. Meta-Analysis of interventions for posttraumatic stress disorder and depression in adult survivors of mass violence in low- and middle-income countries. Depress Anxiety 2017;34:679–91. 10.1002/da.22618 [DOI] [PubMed] [Google Scholar]
- 19. Jordans MJD, Pigott H, Tol WA. Interventions for children affected by armed conflict: a systematic review of mental health and psychosocial support in low- and middle-income countries. Curr Psychiatry Rep 2016;18:9 10.1007/s11920-015-0648-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions : Higgins JPT, Green S, Wiley Online Library, 2011. [Google Scholar]
- 22. Bangpan M, Felix L, Chiumento A, et al. The impact of mental health and psychosocial support interventions on people affected by humanitarian emergencies: a systematic review protocol. Oxfam: Oxford, GB, 2016. [Google Scholar]
- 23. Rehberg K. Revisting therapeutic governance: the politics of mental health and psychosocial programmes in humanitarian settings. Refugee studies centre, Oxford Department of International Development, 2014. [Google Scholar]
- 24. Stavropoulou M, Samuels F. Mental health and psychosocial service provision for adolescent girls in post-conflict settings. ODI, 2015. [Google Scholar]
- 25. Higgins JaG S. The GRADE approach : Cochrane Handbook for Systematic Reviews of Interventions [Internet]. London: Cochrane Collaboration, 2011. [Google Scholar]
- 26. Berkman ND, Lohr KN, Ansari MT, et al. Grading the strength of a body of evidence when assessing health care interventions: an EPC update. J Clin Epidemiol 2015;68:1312–24. 10.1016/j.jclinepi.2014.11.023 [DOI] [PubMed] [Google Scholar]
- 27. DFID How to note: assessing the strength of evidence. London: department for international development. UK: Department for International Development, 2014. [Google Scholar]
- 28. Sutcliffe K, Thomas J, Stokes G, et al. Ica): a pragmatic approach for identifying the critical features of complex interventions. Syst Rev 2015;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Thomas J, Brunton J, Graziosi S. EPPI-Reviewer 4.0: software for research synthesis, 2010. [Google Scholar]
- 30. Bass J, Poudyal B, Tol W, et al. A controlled trial of problem-solving counseling for war-affected adults in Aceh, Indonesia. Soc Psychiatry Psychiatr Epidemiol 2012;47:279–91. 10.1007/s00127-011-0339-y [DOI] [PubMed] [Google Scholar]
- 31. Bass JK, Annan J, McIvor M, et al. Controlled trial of psychotherapy for Congolese survivors of sexual violence. N Engl J Med 2014;370. [DOI] [PubMed] [Google Scholar]
- 32. Becker SM. Psychosocial care for women survivors of the tsunami disaster in India. Am J Public Health 2009;99:654–8. 10.2105/AJPH.2008.146571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hagl M, Powell S, Rosner R, et al. Dialogical exposure with traumatically bereaved Bosnian women: findings from a controlled trial. Clin Psychol Psychother 2015;22 10.1002/cpp.1921 [DOI] [PubMed] [Google Scholar]
- 34. Nakimuli-Mpungu E, Okello J, Kinyanda E, et al. The impact of group counseling on depression, post-traumatic stress and function outcomes: a prospective comparison study in the peter C. Alderman trauma clinics in northern Uganda. J Affect Disord 2013;151:78–84. 10.1016/j.jad.2013.05.055 [DOI] [PubMed] [Google Scholar]
- 35. Scholte WF, Verduin F, Kamperman AM, et al. The effect on mental health of a large scale psychosocial intervention for survivors of mass violence: a quasi-experimental study in Rwanda. PLoS One 2011;6:e21819 10.1371/journal.pone.0021819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sonderegger R, Rombouts S, Ocen B, et al. Trauma rehabilitation for war-affected persons in northern Uganda: a pilot evaluation of the empower programme. Br J Clin Psychol 2011;50:234–49. 10.1348/014466510X511637 [DOI] [PubMed] [Google Scholar]
- 37. Yeomans PD, Forman EM, Herbert JD, et al. A randomized trial of a reconciliation workshop with and without PTSD psychoeducation in Burundian sample. J Trauma Stress 2010;23:305–12. [DOI] [PubMed] [Google Scholar]
- 38. Descilo T, Vedamurtachar A, Gerbarg PL, et al. Effects of a yoga breath intervention alone and in combination with an exposure therapy for post-traumatic stress disorder and depression in survivors of the 2004 south-east Asia tsunami. Acta Psychiatr Scand 2010;121:289–300. 10.1111/j.1600-0447.2009.01466.x [DOI] [PubMed] [Google Scholar]
- 39. Acarturk C, Konuk E, Cetinkaya M, et al. EMDR for Syrian refugees with posttraumatic stress disorder symptoms: results of a pilot randomized controlled trial. Eur J Psychotraumatol 2015;6:6 10.3402/ejpt.v6.27414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ayoughi S, Missmahl I, Weierstall R, et al. Provision of mental health services in resource-poor settings: a randomised trial comparing counselling with routine medical treatment in North Afghanistan (Mazar-e-Sharif). BMC Psychiatry 2012;12:14 10.1186/1471-244X-12-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Basoglu M, Salcioglu E, Livanou M, et al. Single-session behavioral treatment of earthquake-related posttraumatic stress disorder: a randomized waiting list controlled trial. J Trauma Stress 2005;18:1–11. 10.1002/jts.20011 [DOI] [PubMed] [Google Scholar]
- 42. Bass J, Murray SM, Mohammed TA, et al. A randomized controlled trial of a trauma-informed support, skills, and psychoeducation intervention for survivors of torture and related trauma in Kurdistan, Northern Iraq. Glob Health Sci Pract 2016;4:452–66. 10.9745/GHSP-D-16-00017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Mughal U, Carrasco D, Brown R, et al. Rehabilitating civilian victims of war through psychosocial intervention in Sierra Leone. J Appl Soc Psychol 2015;45:593–601. 10.1111/jasp.12322 [DOI] [Google Scholar]
- 44. Oflaz F, Hatipoğlu S, Aydin H. Effectiveness of psychoeducation intervention on post-traumatic stress disorder and coping styles of earthquake survivors. J Clin Nurs 2008;17:677–87. 10.1111/j.1365-2702.2007.02047.x [DOI] [PubMed] [Google Scholar]
- 45. Rahman A, Hamdani SU, Awan NR, et al. Effect of a multicomponent behavioral intervention in adults impaired by psychological distress in a Conflict-Affected area of Pakistan: a randomized clinical trial. JAMA 2016;316:2609–17. 10.1001/jama.2016.17165 [DOI] [PubMed] [Google Scholar]
- 46. Weiss WM, Murray LK, Zangana GAS, et al. Community-Based mental health treatments for survivors of torture and Militant attacks in southern Iraq: a randomized control trial. BMC Psychiatry 2015;15 10.1186/s12888-015-0622-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Steinert C, Bumke PJ, Hollekamp RL, et al. Resource activation for treating post-traumatic stress disorder, co-morbid symptoms and impaired functioning: a randomized controlled trial in Cambodia. Psychol Med 2017;47:553–64. 10.1017/S0033291716002592 [DOI] [PubMed] [Google Scholar]
- 48. Meffert SM, Abdo AO, Alla OAA, et al. A pilot randomized controlled trial of interpersonal psychotherapy for Sudanese refugees in Cairo, Egypt. Psychological Trauma: Theory, Research, Practice, and Policy 2014;6:240–9. 10.1037/a0023540 [DOI] [Google Scholar]
- 49. Neuner F, Schauer M, Klaschik C, et al. A comparison of narrative exposure therapy, supportive counseling, and Psychoeducation for treating posttraumatic stress disorder in an African refugee settlement. J Consult Clin Psychol 2004;72:579–87. 10.1037/0022-006X.72.4.579 [DOI] [PubMed] [Google Scholar]
- 50. Neuner F, Onyut PL, Ertl V, et al. Treatment of posttraumatic stress disorder by trained lay counselors in an African refugee settlement: a randomized controlled trial. J Consult Clin Psychol 2008;76:686–94. 10.1037/0022-006X.76.4.686 [DOI] [PubMed] [Google Scholar]
- 51. Jacob N, Neuner F, Maedl A, et al. Dissemination of psychotherapy for trauma spectrum disorders in postconflict settings: a randomized controlled trial in Rwanda. Psychother Psychosom 2014;83:354–63. 10.1159/000365114 [DOI] [PubMed] [Google Scholar]
- 52. Vijayakumar L, Kumar MS. Trained volunteer-delivered mental health support to those bereaved by Asian tsunami--an evaluation. Int J Soc Psychiatry 2008;54:293–302. 10.1177/0020764008090283 [DOI] [PubMed] [Google Scholar]
- 53. Igreja V, Kleijn WC, Schreuder BJN, et al. Testimony method to ameliorate post-traumatic stress symptoms. community-based intervention study with Mozambican civil war survivors. Br J Psychiatry 2004;184:251–7. 10.1192/bjp.184.3.251 [DOI] [PubMed] [Google Scholar]
- 54. Bolton P, Lee C, Haroz EE, et al. A transdiagnostic community-based mental health treatment for comorbid disorders: development and outcomes of a randomized controlled trial among Burmese refugees in Thailand. PLoS Med 2014;11:e1001757 10.1371/journal.pmed.1001757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Telles S, Singh N, Joshi M, et al. Post traumatic stress symptoms and heart rate variability in Bihar flood survivors following yoga: a randomized controlled study. BMC Psychiatry 2010;10:18 10.1186/1471-244X-10-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Bichescu D, Neuner F, Schauer M, et al. Narrative exposure therapy for political imprisonment-related chronic posttraumatic stress disorder and depression. Behav Res Ther 2007;45:2212–20. 10.1016/j.brat.2006.12.006 [DOI] [PubMed] [Google Scholar]
- 57. BAŞOĞLU M, Salcioglu E, Livanou M. A randomized controlled study of single-session behavioural treatment of earthquake-related post-traumatic stress disorder using an earthquake simulator. Psychol Med 2007;37:203–13. 10.1017/S0033291706009123 [DOI] [PubMed] [Google Scholar]
- 58. Connolly S, Sakai C. Brief trauma intervention with Rwandan genocide-survivors using thought field therapy. Int J Emerg Ment Health 2011;13:161–72. [PubMed] [Google Scholar]
- 59. Bryant RA, Ekasawin S, Chakrabhand S, et al. A randomized controlled effectiveness trial of cognitive behavior therapy for post-traumatic stress disorder in terrorist-affected people in Thailand. World Psychiatry 2011;10:205–9. 10.1002/j.2051-5545.2011.tb00058.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Hewage K, Steel Z, Mohsin M, et al. A wait-list controlled study of a trauma-focused cognitive behavioral treatment for intermittent explosive disorder in Timor-Leste. Am J Orthopsychiatry 2018;88:282–94. 10.1037/ort0000280 [DOI] [PubMed] [Google Scholar]
- 61. Zang Y, Hunt N, Cox T. A randomised controlled pilot study: the effectiveness of narrative exposure therapy with adult survivors of the Sichuan earthquake. BMC Psychiatry 2013;13:41 10.1186/1471-244X-13-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Zang Y, Hunt N, Cox T. Adapting narrative exposure therapy for Chinese earthquake survivors: a pilot randomised controlled feasibility study. BMC Psychiatry 2014;14:262 10.1186/s12888-014-0262-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Esala JJ, Taing S. Testimony therapy with ritual: a pilot randomized controlled Trial*. J Trauma Stress 2017;30:94–8. 10.1002/jts.22163 [DOI] [PubMed] [Google Scholar]
- 64. Jiang R, Tong H, Delucchi KL, et al. Interpersonal psychotherapy versus treatment as usual for PTSD and depression among Sichuan earthquake survivors: a randomized clinical trial. Confl Health 2014;8:14 10.1186/1752-1505-8-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. de J, Knipscheer Jeroen W, Ford N, et al. The efficacy of psychosocial interventions for adults in contexts of ongoing man-made Violence—A systematic review. Health 2014;2014. [Google Scholar]
- 66. Dossa NI, Hatem M. Cognitive-Behavioral therapy versus other PTSD psychotherapies as treatment for women victims of war-related violence: a systematic review. ScientificWorldJournal 2012;2012:1–19. 10.1100/2012/181847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Lambert JE, Alhassoon OM. Trauma-focused therapy for refugees: meta-analytic findings. J Couns Psychol 2015;62:28–37. 10.1037/cou0000048 [DOI] [PubMed] [Google Scholar]
- 68. Lorenc T, Felix L, Petticrew M, et al. Meta-Analysis, complexity, and heterogeneity: a qualitative interview study of researchers' methodological values and practices. Syst Rev 2016;5:192 10.1186/s13643-016-0366-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Herrman H, Jané-Llopis E. The status of mental health promotion. Public Health Rev 2012;34:6 10.1007/BF03391674 [DOI] [PubMed] [Google Scholar]
- 70. Ampuero D, Goldswosthy S, Delgado LE, et al. Using mental well-being impact assessment to understand factors influencing well-being after a disaster. Impact Assessment and Project Appraisal 2015;33:184–94. 10.1080/14615517.2015.1023564 [DOI] [Google Scholar]
- 71. Dickson K, Bangpan M. What are the barriers to, and facilitators of, implementing and receiving MHPSS programmes delivered to populations affected by humanitarian emergencies? A qualitative evidence synthesis. Glob Ment Health 2018;5:e21 10.1017/gmh.2018.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Chowdhary N, Jotheeswaran AT, Nadkarni A, et al. The methods and outcomes of cultural adaptations of psychological treatments for depressive disorders: a systematic review. Psychol Med 2014;44:1131–46. 10.1017/S0033291713001785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Kneale D, Thomas J, Bangpan M, et al. Conceptualising causal pathways in systematic reviews of international development interventions through adopting a causal chain analysis approach. J Dev Effect 2018;10:422–37. 10.1080/19439342.2018.1530278 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2019-001484supp001.pdf (81.3KB, pdf)
bmjgh-2019-001484supp002.pdf (34KB, pdf)
bmjgh-2019-001484supp003.pdf (104KB, pdf)