Abstract
ATP has been identified as an excitatory neurotransmitter in both the CNS and peripheral nervous system; however, little is known about the functional properties of ATP-gated channels in central neurons. Here we used a culture preparation of the postnatal rat retina to test the responsiveness of identified retinal ganglion cells (RGCs) and putative amacrines to exogenous ATP and other purinoceptor agonists. Rapidly activating ATP-induced currents (IATP) were exclusively generated in a subpopulation (∼65%) of RGCs. The latter were identified by Thy1.1 immunostaining, repetitive firing patterns, and activation of glutamatergic autaptic currents. None of the putative amacrine cells was ATP-sensitive. IATP could be induced with ATP, ADP, and α,β-mATP but not with adenosine. It was antagonized by suramin. The current–voltage relationship ofIATP showed marked inward rectification. Dose–response analysis yielded an EC50 of 14.5 μm, with a Hill coefficient of 0.9. Noise analysis ofIATP suggested a mean single channel conductance of 2.3 pS. Retinal P2X purinoceptor channels exhibited a high permeability for Ca2+. PCa/PCs obtained from reversal potentials of IATP under bi-ionic conditions amounted to 2.2 ± 0.7. In the majority of cells, the decay ofIATP was biphasic. The degree of current inactivation during the first 2 sec of agonist application was highly variable. Heterogeneity was also found with respect to the sensitivity to ADP and α,β-mATP and the blocking action of suramin, suggesting expression of multiple P2X receptor subtypes. Our results indicate that activation of P2X receptor channels represents an important pathway for Ca2+ influx in postnatal RGCs.
Keywords: adenosine triphosphate, purinoceptors, P2X, rat, retina, retinal ganglion cells, patch clamp, Ca2+permeability, fura-2
ATP has been regarded as a fast neurotransmitter or co-transmitter with noradrenaline or acetylcholine (Westfall et al., 1990; von Kügelgen and Starke, 1991; Edwards, 1994). In sensory structures of the spinal cord and brain, the action of ATP was excitatory, and voltage-clamp experiments demonstrated that exogenous ATP or its analogs induced cation conductances (Jahr and Jessell, 1983; Ueno et al., 1992; Shen and North, 1993). Purinergic excitatory synaptic currents have been demonstrated in rat medial habenular neurons (Edwards et al., 1992) and cultured neurons from rodent celiac ganglion (Evans et al., 1992).
Extracellular ATP is rapidly degraded by ecto-nucleotidases (Zimmermann, 1996). The targets of ATP and its degradation product adenosine are P2 and P1 receptors, respectively. P2 receptors have been classified according to their transduction mechanisms into ionotropic (P2X) and G-protein-coupled metabotropic (P2Y) receptors. Molecular cloning studies have identified seven different P2X subunits that assemble to cation channels with distinct functional properties (North and Barnard, 1997; Soto et al., 1997). In the vertebrate CNS, P2X purinoceptors are abundant but display great variability in their regional expression patterns (Collo et al., 1996; Séguéla et al., 1996; Vulchanova et al., 1996).
In contrast to the wealth of data concerning nucleotide signaling in the somatosensory and peripheral auditory system (Brake and Julius, 1996; Housley, 1998), very little is known about the role of extracellular nucleotides in the visual system. A functional role for ATP and its metabolites in visual signal processing has been suggested by Blazynski and Perez (1991), who showed that nucleotides were released from the rabbit retina via Ca2+-dependent and Ca2+-independent mechanisms. Using an eye-cup preparation from rabbit, it was shown that P2 antagonists increased and exogenous ATP decreased the light-induced release of acetylcholine (Neal and Cunningham, 1994). These authors envisaged the possibility that co-released ATP modulates light-evoked acetylcholine release from amacrine cells via an inhibitory feedback loop. Stores of endogenous adenosine were discovered in the inner retina of the rabbit (Blazynski and Perez, 1991). In the rat retina, receptors for ATP were found in photoreceptors and neurons of the inner nuclear and ganglion cell layer (Greenwood et al., 1997). However, the cellular distribution of retinal P2X receptors and their functional properties have remained unexplored.
We used a previously established culture model of the postnatal rat retina (Taschenberger and Grantyn, 1995) to characterize the current responses to exogenous ATP in defined neuronal populations. The first aim of our study was to clarify which neurons in the inner retina express P2X receptors. Furthermore, we addressed the possible heterogeneity of retinal purinoceptor channels by comparing kinetic properties and pharmacological profiles of ATP-activated currents because it is known that the rodent retina contains several P2X subunits (Brändle et al., 1998). Finally, we asked whether P2X receptor channels can serve as a pathway for Ca2+influx. Our data show that exogenous ATP induces depolarizing currents with slow inactivation and high fractional Ca2+influx selectively in ganglion cells.
A preliminary report of this work has appeared previously in abstract form (Taschenberger and Grantyn, 1998b).
MATERIALS AND METHODS
Cell culture. Experiments were performed on cultured retinal neurons between 6 hr after plating up to 17 d in vitro (DIV). Dissociated cell cultures were obtained from the postnatal rat retina (postnatal day 3–7) and prepared as described previously (Taschenberger and Grantyn, 1995), with one important modification. The culture medium consisted of DMEM (Sigma, St. Louis, MO) and was supplemented with a mixture of co-factors, vitamins, and antioxidants essentially as described by Brewer and Cotman (1989). Additionally, 20 ng/ml recombinant BDNF and 5 μmforskolin were added (Meyer Franke et al., 1995). Neuritogenesis and survival of retinal ganglion cells (RGCs) were greatly enhanced under these culture conditions. Retinal cultures were maintained at 35.5°C in a 10% CO2, 90% moist air atmosphere. During the first 3 DIV, the culture medium was supplemented with 2% horse serum and 2% fetal calf serum. When non-neuronal cells reached 50–70% confluence (usually at DIV 3), the culture medium was completely exchanged, and cells were kept in serum-free medium for the rest of the culture period.
Discrimination between retinal ganglion cells and putative amacrine cells. A combination of morphological and functional criteria allowed us to discriminate between GABAergic putative amacrine cells and glutamatergic RGCs at different stages of their in vitro development. In the rat retina, ganglion cells constitute the neuron population with the largest soma diameter (Huxlin and Goodchild, 1997). Among short-term (DIV 0–3) cultured neurons of the postnatal rat retina, all neurons with soma diameter >13 μm can be retrogradely labeled (Grantyn and Korenbaum, 1992) and are Thy1.1-positive (Guenther et al., 1994). Neurons that satisfied this size criterion were therefore regarded as RGCs (see Fig.3A,B). In long-term cultures (≥4 DIV), both cell types were unambiguously distinguished by anti-Thy1.1 immunostaining (see Fig.3C,D). Vital immunostaining of retinal cultures was performed as described previously (Taschenberger and Grantyn, 1995). Briefly, cultures were incubated with the monoclonal mouse anti-Thy1.1 antibody MRC OX-7 (1:40) (Serotec, Indianapolis, IN). Subsequently, RGCs were identified by visualization of the Thy1.1 epitope under fluorescent illumination after incubation with phycoerythrin-conjugated goat anti-mouse antibody (1:100) (Jackson ImmunoResearch, West Grove, PA). After staining, cultures were used for electrophysiological experiments (see Fig. 3C,D). A small population of GABAergic putative amacrine cells express Thy1.1 on a low level (Perry et al., 1984; Taschenberger and Grantyn, 1995). These very weakly stained cells were clearly discernible from Thy1.1-positive RGCs and, for the sake of simplicity, will also be referred to as Thy1.1-negative.
Fig. 3.

ATP-activated P2X receptor channels are exclusively expressed in RGCs. A–C, Phase-contrast images illustrating three different ATP-sensitive RGCs after anin vitro period of 6 hr (A, B) and 10 DIV (C), respectively. D, Corresponding fluorescence image of the cell shown in C. In young cultures (DIV 0–3) RGCs were identified by a size criterion (soma diameter >13 μm) (A, B), whereas in long-term cultures (≥DIV 4) vital anti-Thy1.1 immunostaining was applied.E, Amplitudes of INa(V)determined in a total of 97 multipolar cells that included 65 ATP-sensitive and 32 ATP-insensitive cells (≥7 DIV). Peak amplitudes ranged from −0.39 nA to −24.83 nA with a mean value of −7.90 ± 0.54 nA. INa(V) was significantly larger in ATP-sensitive compared with ATP-insensitive neurons (p < 0.0001; Mann–Whitney test, two-tailed). The number of tested cells is indicated. F, If no preselection criterion was applied, the fraction of ATP-sensitive cells was 4%. If recordings were restricted to RGCs identified after anti-Thy1.1 immunostaining (second column) or by size (third column), the fraction of ATP-sensitive was 65 and 67%, respectively. Above each column, the number of ATP-sensitive cells and total number of tested neurons are inparentheses.
In addition, cultured RGCs and putative amacrines differ in amplitudes of voltage-activated Na+ currents and can be separated according to the intrinsic pattern of the action potentials that they generate on sustained current injection under current-clamp conditions (Taschenberger and Grantyn, 1995). Glutamatergic RGCs are regular spiking neurons with slow-frequency adaptation, whereas GABAergic amacrines generate only few spikes that tend to inactivate quickly (see Fig. 2A–C). Synaptic glutamate release from RGCs was demonstrated by recording autaptic responses to short depolarizing voltage steps (400 μsec, −5 mV).
Fig. 2.
Exogenous ATP exclusively excites a subpopulation of Thy1.1-positive glutamatergic RGCs, whereas Thy1.1-negative putative amacrine cells are ATP insensitive. Recordings from four different cells were submitted to vital anti-Thy1.1 immunostaining before patch-clamp recording. A, B, Recordings from two RGCs with strong immunofluorescence, large amplitudes ofINa(V) (top row), and repetitive discharge during depolarization under current-clamp (middle row). Note that some RGCs generatedIATP (A, bottom row), whereas others did not (B, bottom row). C, Thy1.1-negative cells with small INa(V)(top row) and spike inactivation during prolonged depolarization (middle row) were always ATP insensitive (C, bottom row). During agonist application, bursts of glutamatergic EPSCs were frequently observed in both ATP-sensitive and -insensitive cells (also see Fig. 7E). D, ATP-sensitive cells were glutamatergic. IATP(D1) and autaptic currents (D2) were recorded from an RGC at DIV 17. Three consecutive traces are shown in each panel inD2. Autaptic currents were identified as glutamatergic because of complete and reversible block by 20 μm DNQX. Capacitive artifacts were blanked, andINa(V) was truncated for clarity. Bath solution contained 3 mm Ca2+, 1 mm Mg2+ in all experiments. Addition of 50 μm bicuculline methiodide suppressed spontaneous GABAergic synaptic currents.
Experimental solutions. During experiments cells were bathed in control saline containing (in mm): NaCl 136, KCl 5.36, CaCl2 3, MgCl2 1, glucose 25, HEPES 15. To investigate the Ca2+ permeability of retinal ATP-activated channels, the recording chamber contained Na+-free solution consisting of (in mm): 140 N-methyl-d-glucamine (NMDG), 20 CaCl2, 25 glucose, and 15 HEPES, pH 7.3. In the majority of experiments, patch pipettes were filled with a solution of the following composition (in mm): CsCl 145, CaCl2 0.5, MgCl2 1, EGTA 5, HEPES 25, glucose 10, pH 7.3. In some experiments, pipettes contained 115 mmCs-gluconate, 30 mm CsCl or 115 mm K-gluconate, 30 mm KCl instead of 145 mm CsCl.
At the beginning of patch-clamp experiments, current output was set to zero with the pipette being immersed in the bath. The time-dependent drift of the offset potential was measured after the membrane patch was destroyed. It was always ≤3 mV and therefore disregarded. Junction potentials between pipette and bath solutions were measured as described in Neher (1992). For Na+-rich external solution, reported reversal potentials were corrected by −4.5, −11, and −10 mV for CsCl-, Cs-gluconate-, and K-gluconate-filled patch pipettes, respectively. For NMDG+-containing bath solution, Erev was corrected by −7.5 mV (CsCl-filled electrodes). All experiments were performed at room temperature (22–24°C).
Drug application. Drugs were applied via a gravity-driven superfusion system with an outflow pipette of ∼50 μm opening diameter. An additional suction pipette (∼70 μm opening diameter) ensured the complete removal of test solutions from the bath. To switch between superfusion channels we used manually operated valves. In the vicinity of the cell under investigation, the total exchange of test solutions was accomplished in <1 sec. In some experiments rapid drug application was performed by means of computer-operated electromagnetic valves (Taschenberger and Grantyn, 1998a). 6,7-Dinitroquinoxaline-2,3-dione (DNQX) was purchased from Tocris Neuramin. Suramin and α,β-methylene ATP (α,β-mATP) were obtained from RBI (Natick, MA). All other chemicals were from Sigma.
Whole-cell patch-clamp recording. Whole-cell voltage-clamp recordings were performed using an EPC-7 patch-clamp amplifier (List, Darmstadt, Germany). Currents were measured through a 500 MΩ feedback resistor and low-pass-filtered at 3 kHz (three-pole Bessel filter). Capacitive transients were reduced by analog circuitry. Patch pipettes were pulled from thick-walled borosilicate tubing (WPI, Sarasota, FL) on a Sutter P-87 micropipette puller (Sutter Instruments, Novato, CA). The pipette to bath resistance of patch electrodes ranged from 4 to 7 MΩ. Series resistance compensation was applied as much as possible (50–90%). Holding potential (Vh) was set to −70 mV if not otherwise stated. Autaptic currents were evoked by short (400 μsec) depolarizing voltage steps fromVh −70 to −5 mV. To measure the current–voltage (I–V) relations of ligand-activated currents, voltage ramps (from Vh −100 to +50 mV, 200 msec duration) were applied before, during, and after agonist application. The net I–V relations for ligand-activated currents were obtained by digital subtraction of the ramp current in the absence of agonist from that during agonist application. For these experiments, voltage-activated currents were blocked by addition of 1 μm TTX, 200 μm 4-AP, 50 μmNiCl2, and 50 μm CdCl2 to the bath solution.
Fura-2 fluorescence measurements. To examine intracellular Ca2+ concentration ([Ca2+]i), cells were loaded with 5 μm fura-2 AM (Molecular Probes, Eugene, OR; stock solution dissolved in DMSO) for 30 min in culture medium at 35.5°C. After washing, cells were kept in normal bath solution for an additional 15–20 min to ensure de-esterfication. Cultures were then placed on the stage of an inverted microscope (Zeiss Axiovert) and viewed with a 40× phase-contrast objective (Zeiss). A fluorescence ratio-imaging system (Till Photonics, Martinsried, Germany) was used for excitation and monitoring of fluorescence signals. Excitation wavelength was switched between 340 nm (F340) and 380 nm (F380) by means of a monochromator (12 nm bandwidth). Using a 12-bit CCD camera, fluorescence signals were recorded after passing a dichroic beamsplitter (DCLP405) and a 510 WB40 emission filter (Omega Optical, Brattleboro, VT). Acquisition, storage, and analysis were performed with Till Vision (vers. 3.02, Till Photonics). Background fluorescence was measured from a region in the immediate vicinity of the cell under investigation and subtracted. Fluorescence ratio R(F340/F380) was used to describe relative changes in [Ca2+]i without conversion to absolute values of [Ca2+]i concentrations.
Data analysis. Whole-cell currents were digitized on-line using a 12-bit labmaster DMA interfaced with a 586-base computer and pClamp software (vers. 5.5; Axon Instruments, Foster City, CA) at a sampling frequency of 8–25 kHz. Voltage-activated currents were leak-corrected using the P/n protocol implemented in the pClamp software. Off-line analysis was performed using the AutesP software written by H. Zucker (NPI, Tamm, Germany) and Origin (vers. 4.1; Microcal, Northampton, MA). Estimation of the zero current potential (Erev) of ATP-activated currents (IATP) was complicated because of the strong inward rectification of IATP. Therefore, fourth-order polynomial functions that accurately described the inwardly rectifying I–V relationship ofIATP were fitted to individual I–Vcurves. Erev was obtained by solving the roots of the polynomials. To quantify the degree of rectification present in the I–V curves of kainic acid-activated currents (IKA), a rectification index (RI) was calculated as the ratio of the slope conductances at +40 and −60 mV (Taschenberger and Grantyn, 1998a). The slope conductance was estimated by a linear fit to the I–V curves ofIKA in the range of ±10 mV at the respective membrane potential.
The permeability ratio PCa/PCs was calculated from the experimentally determinedErev in Na+-free solution according to the constant field equation for bi-ionic conditions (Iino et al., 1990): PCa/PCs = 0.25 × [Cs+]i/[Ca2+]o× exp(Erev/Ψ) × (1 + exp(Erev/Ψ) with Ψ =R × T/F = 25.42 mV (at room temperature), where F, R, and T have their usual thermodynamic meanings, [Cs+]i is the Cs+concentration in the patch pipette, [Ca2+]o is the Ca2+concentration in the external solution, and Erevis the measured reversal potential in Na+-free solution. PCa and PCs are the permeability coefficients for Ca2+ and Cs+, respectively.
The mean activity coefficient of CsCl and CaCl2 at 25°C were estimated by interpolation of tabulated values and amounted to 0.724 and 0.664 for 145 mm CsCl and 20 mmCaCl2, respectively. The calculated single ion activities were 101.8 and 8.8 mm for Cs+and Ca2+, respectively. Results are presented as mean ± SEM. Statistical comparisons were made using nonparametric tests (SPSS for Windows vers. 6.1; SPSS, Chicago, IL).
RESULTS
Exogenous ATP activates P2X receptor-mediated currents only in a subpopulation of RGCs
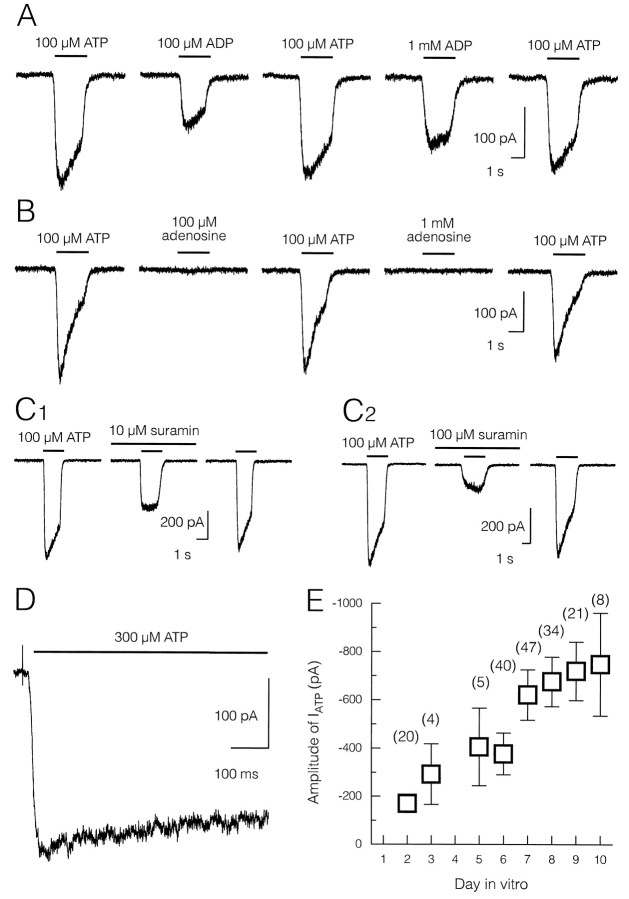
Fast-flow application of micromolar concentrations of the P2 receptor agonist ATP elicited rapid conductance changes in a small fraction of multipolar retinal neurons (Fig.1). Cells were regarded as ATP-sensitive if they generated IATP with peak amplitudes ≥15 pA in response to a saturating concentration of exogenous ATP (300 μm). Although much less effective, application of ADP induced inward currents as well. However, even at a concentration of 1 mm, peak amplitudes of ADP-induced currents were always smaller than IATP elicited by 100 μm ATP (Fig. 1A).
Fig. 1.
ATP-induced ion currents in retinal neurons have a P2 purinergic pharmacology. A–C, Whole-cell current responses to fast-flow agonist application obtained from four different neurons (Vh = −70 mV). In each experiment, agonist application was followed by a washout period of at least 2 min.Bars indicate application intervals. Agonist concentrations are given above each bar. A, Sequential application of the P2 receptor agonists ATP and ADP elicited rapid conductance changes in retinal neurons. Note that despite higher agonist concentration, ADP-induced currents were smaller thanIATP. B, Current responses to ATP but not adenosine in another neuron. Agonist pulses of a fixed concentration of ATP (100 μm) and two different concentrations of adenosine (100 μm and 1 mm) were sequentially applied at an interval of 120 sec.IATP gradually declined on repeated application of ATP. C, IATPwas partially antagonized by co-application of the P2 receptor antagonist suramin (C1, 10 μm;C2, 100 μm). The blocking action of suramin was reversible at both concentrations as indicated by the nearly complete recovery of IATP. Recordings were obtained from acutely isolated RGCs. D, High-speed agonist application (300 μm ATP) revealed rapid activation time course of IATP followed by slow inactivation. A rapidly inactivating current component was not observed. E, Mean amplitudes ofIATP induced by application of saturating concentrations (300 μm) plotted against DIV. Number of tested ATP-sensitive cells at the given DIV is given inparentheses. IATP increased approximately fourfold from DIV 2 to 10.
ATP is known to be rapidly degraded by ecto-ATPases to ADP and eventually to adenosine (Zimmermann, 1996). Figure 1Billustrates an experiment aimed at clarifying whetherIATP was activated by ATP or by its breakdown product adenosine. In the depicted neuron, the peak amplitude ofIATP was 255.0 ± 16.8 pA, whereas adenosine at both concentrations failed to evoke a sizable current. Similar results were obtained in four other cells. The nonsubtype-selective P2 receptor antagonist suramin that has been used to distinguish P2X receptors from other ligand-gated ion channels (Nakazawa et al., 1991) reversibly antagonizedIATP in a dose-dependent manner. The sensitivity of IATP to suramin was investigated in 13 retinal neurons at DIV 0–3 (Fig. 1C). Application of 10 μm suramin reversibly reduced peak amplitudes ofIATP by 44.1 ± 1.8% (n = 5) (Fig. 1C1). Even 100 μm suramin did not completely block IATP (68.8 ± 1.4% reduction, n = 8) (Fig.1C2).
IATP activated rapidly and decayed quickly on agonist removal. However, the activation and inactivation time course of ligand-gated whole-cell currents is strongly influenced by the speed of agonist application. We therefore measuredIATP in response to fast application of a saturating ATP concentration (300 μm, n = 5). IATP fully activated within tens of milliseconds, suggesting direct coupling between purinergic receptor and ion channel (Fig. 1D). A rapidly inactivating current component as described for IATP in a subpopulation of sensory neurons (Cook et al., 1997) was not revealed. Taken together, these results are consistent with a P2X receptor-mediated action of exogenous ATP in a small population of retinal neurons.
When tested between DIV 2 and 10, peak amplitudes ofIATP varied over a >100-fold range. Current responses elicited by 300 μm ATP ranged from −27 to −3755 pA, with an average of −555 ± 46 pA (n = 171). As illustrated in Figure 1E,IATP increased more than fourfold during the culture period from −170 ± 31 pA to −748 ± 213 pA at DIV 2 to DIV 10, respectively.
Figure 2A–C presents recordings from a culture that had been submitted to Thy1.1 immunostaining before whole-cell recording. IATPwas found only in a subpopulation of retinal ganglion cells (Fig.2A, 3A–D), whereas other RGCs (Fig. 2B) and all Thy1.1-negative amacrine cells were ATP insensitive (Fig. 2C). In five Thy1.1-positive neurons the transmitter phenotype of ATP-sensitive cells was tested by recording autaptic responses to short depolarizations. With no exception, ATP-sensitive cells were identified as glutamatergic (Fig. 2D).
Furthermore, the peak amplitudes of INa(V) were significantly higher in ATP-sensitive (−10.41 ± 0.56 nA,n = 65) compared with ATP-insensitive (−2.82 ± 0.44 nA, n = 32) cells (p < 0.0001). This is in line with our previous observation that cultured RGCs and amacrine cells differ largely in amplitudes ofINa(V) (Taschenberger and Grantyn, 1995) (Fig.3E).
The conclusion that ATP excites RGCs but not amacrine cells was finally also supported by comparing the fraction of ATP-sensitive neurons within the entire population of multipolar neurons and within the RGCs population and the population of Thy1.1-negative GABAergic amacrine cells. As summarized in Figure 3F, only 4% of all multipolar neurons (8 of 199) generated IATP. In contrast, about two-thirds of the tested RGCs were ATP sensitive. The fraction of ATP-sensitive RGCs remained unchanged during the culture period despite the gradual decline in the total number of RGCs. All Thy1.1-negative cells were ATP insensitive (n = 25). Taken together, these results show that IATP is an exclusive property of a subpopulation of RGCs.
Properties of ATP-activated ion currents in RGCs
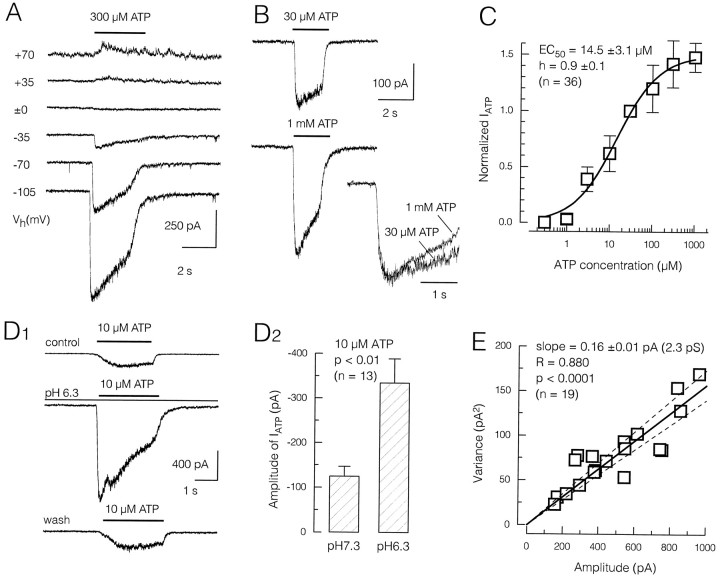
Figure 4Aillustrates a family of ATP-induced currents at differentVh values. IATP reversed near 0 mV and showed a strong inward rectification. In fact, very little outward current was measured even at Vh = 70 mV. Figure 4B presents recordings underlying the dose–response relationship for IATP. When the concentration of ATP was raised from 30 μm to 1 mm, current inactivation of IATP was only slightly accelerated, although its peak amplitude nearly doubled (Fig. 4B).
Fig. 4.
Voltage-dependence, dose–response relationship and noise analysis of IATP in RGCs.A, Family of ATP-induced current responses at differentVh to illustrate strong inward rectification of IATP. B,IATP in response to half-effective concentration (30 μm) and saturating concentration (1 mm) of ATP. Although the peak amplitude ofIATP nearly doubled, the time course of inactivation was similar at both agonist concentrations.C, Dose–response characteristics ofIATP. Pooled data from 36 cells. Current responses were normalized to the peak amplitude evoked by 30 μm ATP. Fitting a Hill function (solid line) to the data yielded an EC50 of ∼14 μm with a Hill coefficient of ∼1.D1, Sensitivity ofIATP to changes of extracellular pH. At low agonist concentrations, the amplitude ofIATP was strongly augmented by acidification. This effect was fully reversible. Recordings from an acutely isolated RGC. D2, In 13 tested RGCs, lowering the extracellular pH by one log unit resulted in an increase of IATP to 341 ± 62%.E, Relation between mean current and variance of current noise. Background noise was subtracted from test variance before plotting. Data points were collected from 19 ATP-sensitive neurons. Agonist concentration was ≤10 μm,Vh = −70 mV. Straight lineand broken lines indicate least-square fit and 95% confidence limits, respectively. Slope of the regression line was 0.16 pA, corresponding to a conductance of 2.3 pS. Electrodes contained CsCl-based internal solution in A–D.
It was difficult to obtain complete dose–response curves in individual RGCs because in many cells IATP recovered incompletely, particularly at higher ATP concentrations. Therefore, only three to four different agonist concentrations were tested in most cells. In each RGC, currents elicited by the various concentrations of ATP were normalized to the corresponding peak amplitudes ofIATP activated by 30 μm ATP. In this way, a pooled concentration–response relationship was obtained from a total of 36 RGCs (Fig. 4C). The data points were fitted by a Hill function yielding an EC50 of 14.5 ± 3.1 μm with a Hill coefficient of h = 0.9 ± 0.1 (n = 36), which is consistent with a 1:1 binding of agonist to the receptor (Krishtal et al., 1983).
Recombinant P2X receptors show different sensitivity to changes in the extracellular pH (Stoop et al., 1997). In RGCs,IATP was strongly and reversibly augmented when tested in acidic bath solution (Fig.4D1). On average, current responses to 10 μm ATP amounted to −126 ± 21 pA at a pH of 7.3 and to −335 ± 54 pA at a pH of 6.3 (n = 13) (Fig.4D2), which corresponds to an increase ofIATP to 341 ± 62%.
Unitary conductances of recombinant P2X receptor channels differ greatly (Evans, 1996). Unfortunately, we failed in our attempts to record single-channel activity in membrane patches excised from somata of ATP-sensitive RGCs (n = 6). Nevertheless, a rough estimate of the unitary conductance of retinal P2X receptor channels was obtained from analysis of whole-cell noise induced by application of low (≤10 μm) ATP concentrations (Fig.4E). In the low concentration range and with the assumption that the current noise is generated by activation of a single-channel population with uniform conductance, the relation between mean current (mI) and variance (var(I)) can be described by the equation var(I)= i × mI, wherei represents the single-channel current (Anderson and Stevens, 1973). The relation between mean IATPand its variance was examined in 19 RGCs. As illustrated in Figure4E, the current variance was almost linearly related to the mean current with a slope of 0.16 ± 0.01 pA (r = 0.88, p < 0.0001). Under the assumption of Erev = 0 mV, the apparent single-channel conductance was estimated to be 2.3 pS.
As first reported by Krishtal et al. (1983), ATP-induced currents desensitize quickly and recover slowly from inactivation. To determine the time course of recovery from inactivation ofIATP in RGCs, we applied test pulses of 300 μm ATP at variable intervals (ranging from 5 to 120 sec) after control applications (Fig. 5) (n = 8). For each RGC, the sequence of intervals between control and test applications was randomized. Between successive agonist applications, cells were allowed a recovery period of ≥150 sec. Figure 5B summarizes pooled data from eight different RGCs. The averaged time course of recovery from inactivation could be approximated with a mono-exponential function yielding a time constant τ = 62.7 sec.
Fig. 5.
IATP recovers slowly from desensitization. Control application of ATP (300 μm, 2 sec duration) was followed by test application after variable intervals ranging from 10 to 120 sec. Each trial was followed by a washout period of 2 min. A, Specimen recordings. Application interval is indicated above each trace.B, Pooled data from eight different cells. For each application interval, IATP was normalized to the respective control amplitude. Solid line indicates a mono-exponential fit to the data yielding a time constant of resensitization of ∼60 sec.
Heterogeneity in the inactivation kinetics and pharmacological properties of IATP in different RGCs
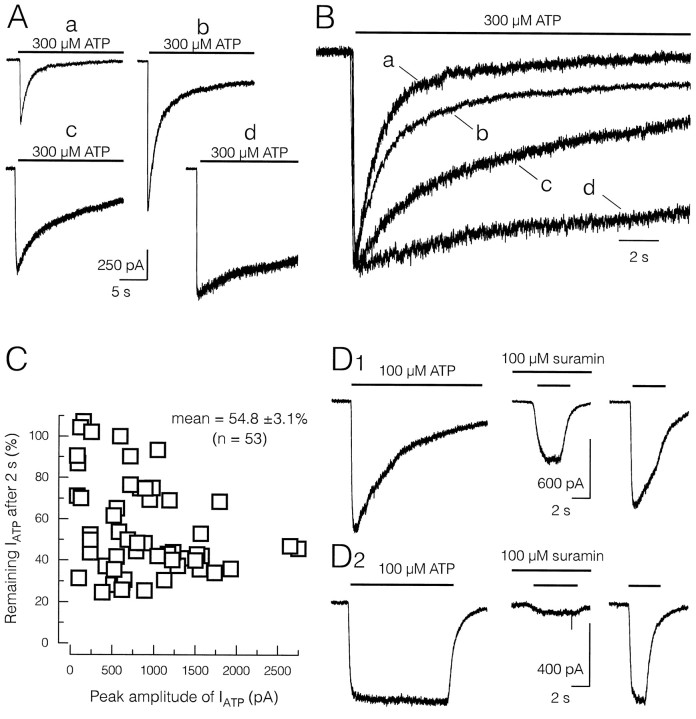
During sustained agonist application, IATPpartially inactivated. There was a considerable variability in the inactivation kinetics of IATP, particularly in older RGCs cultured for >7 DIV. To study the inactivation of IATP during prolonged agonist pulses, 300 μm ATP was applied for 20 sec in a total of 27 RGCs. Figure 6Acompares current responses recorded from four different RGCs. For comparison, scaled currents are shown superimposed in Figure6B. In the majority of cells (n = 19) the decay of IATP was biphasic. In these cells, the decay of IATP was fitted with a double-exponential function yielding a fast and a slow time constant of τfast = 1083 ± 52 msec and τslow = 5498 ± 226 msec, respectively. The relative contribution of these kinetically distinct components to IATP, however, was highly variable (Fig. 6A,B, compare traces a, b, and c). In some RGCs the fast inactivating component dominated (for example, Fig.6A, trace a). In the remaining RGCs (n = 8) only the slow component (τ = 4492 ± 538 msec) was present (Fig. 6A, trace d). In rare cases IATP did not inactivate at all (for example, Fig. 6D2).
Fig. 6.
Heterogeneous inactivation kinetics ofIATP in different ATP-sensitive RGCs.A, Specimen recordings ofIATP from four different RGCs are depicted to illustrate large differences in the decay kinetics ofIATP. Agonist concentration and application interval are indicated by the bars. Calibration bar applies to all four cells. In the majority of cells, the decay ofIATP exhibited a fast and a slow component (traces a, b, c). However, in some cells the fast component dominated the decay (trace a), whereas only the slow component was present in other RGCs (trace d).B, Superposition of the current responses illustrated inA normalized to the same peak amplitude to facilitate comparison. C, Fraction ofIATP remaining after 2 sec of agonist application plotted against the peak amplitude ofIATP. Agonist concentration was 300 μm. In a majority of RGCs,IATP inactivated within 2 sec to 25–60% of its peak amplitude. However, in some RGCs with relatively smallIATP, the fraction of remaining current was >70%. D, RGCs with slowly or noninactivating current responses showed strong attenuation ofIATP by the P2 receptor antagonist suramin (100 μm). Faster inactivation kinetics ofIATP correlated with weaker sensitivity to suramin. In both cases, IATP recovered almost completely after washout.
The heterogeneous inactivation of ATP-induced currents in different RGCs suggests a variable contribution of kinetically distinct P2X receptor channels to IATP. For recombinant P2X receptor channels, the inactivation time course has been described in terms of the fraction of current remaining after prolonged ATP application (Buell et al., 1996a; Collo et al., 1996). Figure6C illustrates the relationship between inactivation ofIATP and peak amplitudes in a total of 53 RGCs. The degree of current inactivation was quantified as the fraction ofIATP remaining after 2 sec of agonist application (300 μm ATP). No significant correlation between both parameters was found. In most RGCs, 40–80% ofIATP inactivated during the initial 2 sec of agonist application; however, in some RGCs current inactivation was <30%.
A high degree of variability was also observed in the efficacy of the antagonist suramin to block IATP. Although fast decaying current responses showed relatively little suramin sensitivity (Fig. 6D1), slowly or noninactivating currents were strongly attenuated by simultaneous application of suramin (Fig.6D2). In nine RGCs with fast inactivating currents, 100 μm suramin reducedIATP to 35.2 ± 4.1% of the control amplitude (n = 9). In contrast, in four other RGCs with slowly inactivating currents suramin almost completely antagonized ATP-induced currents (3.3 ± 3.3% of control).
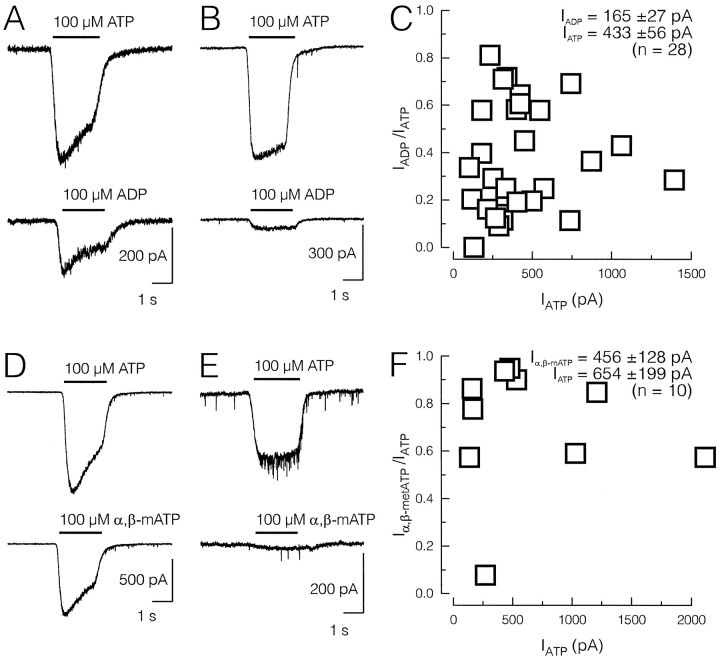
To investigate the potency of the purinoceptor agonists ADP and α,β-mATP, IATP elicited with 100 μm ATP was compared with the current amplitude induced by 100 μm ADP or 100 μm α,β-mATP, respectively (Fig. 7). Both agonists were less potent than ATP. On average 38 and 70% of the ATP-induced current response was elicited by application of ADP and α,β-mATP, respectively (Fig. 7C,F). RGCs with fast decayingIATP showed a higher sensitivity to the ATP analogs (Fig. 7A,D) than cells with slowly inactivating currents (Fig. 7B,E). These differential actions of suramin and ATP analogs suggest expression of multiple P2X receptor subtypes in RGCs.
Fig. 7.
Differential action of the ATP analogs ADP and α,β-mATP suggests expression of multiple subtypes of P2X receptors in RGCs with fast inactivating and slowly or noninactivatingIATP. A, B, D, E, Specimen recordings from four different RGCs with fast (A, D) and slow (B, E) decay kinetics ofIATP, respectively (Vh = −70 mV; CsCl-based pipette solution).IATP (top panels) and current responses to the respective analogs (bottom panels) elicited at the same agonist concentration (100 μm) are illustrated for comparison. C, F, Pooled data plotted as the ratio ofIADP/IATPandIα,β-mATP/IATPagainst peak amplitudes of IATP for 28 and 10 different RGCs, respectively. Note the large scattering of the data points.
P2X receptors couple to a nonspecific cation channel with high Ca2+ permeability
To characterize the ion selectivity of ATP-gated P2X receptor channels in RGCs, we recorded IATP during voltage-ramp commands in the presence of blockers of voltage-gated channels (Fig. 8). Reversal potentials ofIATP were obtained from the roots of polynomial functions (fourth degree order) fitted to the individualI–V curves. Figure 8 shows theI–V relation of IATPdetermined with three different sets of ionic conditions. To investigate the contribution of Cl− toIATP (Balachandran and Bennett, 1996), we varied the chloride equilibrium potential (ECl) by partially substituting gluconate− for Cl−. Despite a shift of the calculated ECl from near 0 mV to −39 mV, Erevof IATP did not significantly change (−0.1 ± 0.7 mV vs −2.3 ± 1.7 mV) (Figs. 8A,B,10A,B), indicating that P2X receptor channels in RGCs are impermeable for Cl−.
Fig. 8.
P2X receptor channels in RGCs are impermeable to Cl− but show approximately equal permeability to K+ and Cs+. A–C, Ramp currents (Vh = −100–50 mV, 200 msec duration) were recorded and digitally averaged to study the effect of different internal solutions on the I–Vrelationship of IATP. The composition of the pipette solution, the calculated Erevobtained from polynomials (fourth degree) fitted to individualI–V curves, and the number of RGCs are given on top of each diagram. Arrowsindicate the theoretical equilibrium potential for Cl−. A, With CsCl-based internal solution, IATP reversed near 0 mV.B, No significant shift ofErev was observed after lowering [Cl−]i from 145 to 30 mmby substituting gluconate for Cl−, indicating that retinal P2X receptor channels are Cl− impermeable (compare A and B). Replacing internal Cs+ with K+ did not affectErev of IATP(compare B and C) (p = 0.569, Friedmann test). Likewise, the mean amplitudes of IATP were similar with either Cs+ (D, second column) or K+ (D, third column) as the main internal cation (p = 0.48, Mann–Whitney test, two-tailed), suggesting roughly equal permeability for both cations. The degree of rectification was unaffected by the composition of the pipette solution (compare I–Vcurves in A–C).
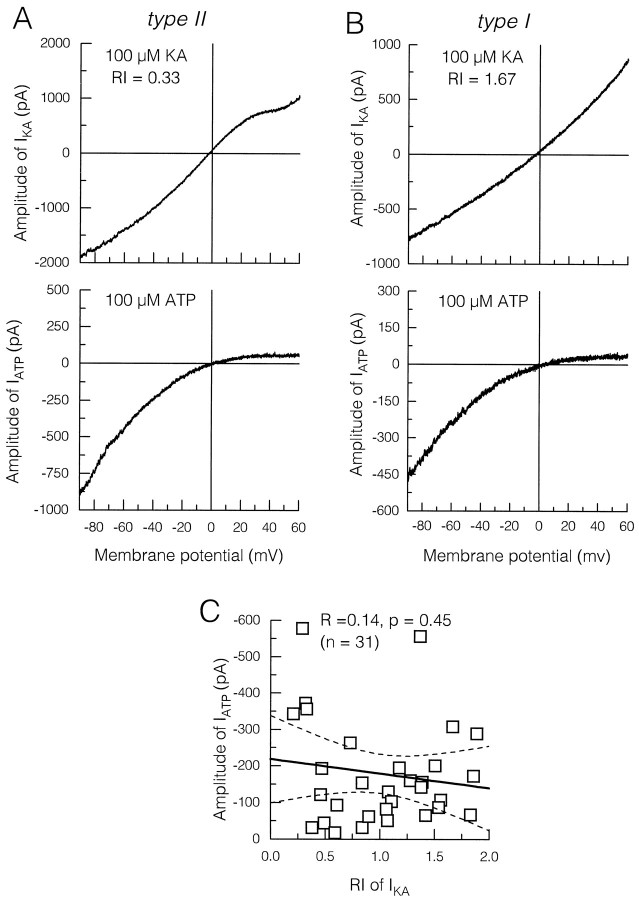
Fig. 10.
In RGCs, P2X receptor channels do not preferentially colocalize with Ca2+-permeable (A, type II RGCs) or Ca2+-impermeable (B, type I RGCs) non-NMDA receptor channels. A, B, Ramp currents during application of kainic acid (100 μm,top panel) and ATP (100 μm,bottom panel) from two different RGCs after 24 hr in culture. RGCs expressing Ca2+-permeable non-NMDA channels and RGCs with Ca2+-impermeable non-NMDA channels were distinguished according to the rectification ofIKA. Note thatIATP was recorded in both type II and type I RGCs. C, Pooled data from a total of 31 RGCs. Peak amplitudes of IATP were plotted against RIs of IKA. Solid andbroken lines indicate linear regression and 95% confidence limits, respectively. No significant correlation was found between RIs of IKA and amplitudes ofIATP.
With K+ as the main internal cation, voltage-activated outward currents were much larger, and consequently estimation of Erev was more difficult. The average value for Erev with potassium-based internal solution was −0.2 ± 2.1 mV (Fig. 8C) and thus was similar to the values obtained with Cs-filled electrodes (Fig.8B). This indicates that ATP activates a nonspecific cation conductance with approximately equal permeability to Na+, K+, and Cs+. This conclusion is supported by the nearly identical mean amplitudes for IATP recorded with Cs+- or K+-filled electrodes. The latter amounted to −547 ± 56 pA (n = 56) and −556 ± 78 pA (n = 78), respectively (Fig.8D). The degree of rectification of theI–V curve was unaffected by the composition of the pipette solution (compare I–V curves in Fig.8A–C; see also Fig. 10A,B).
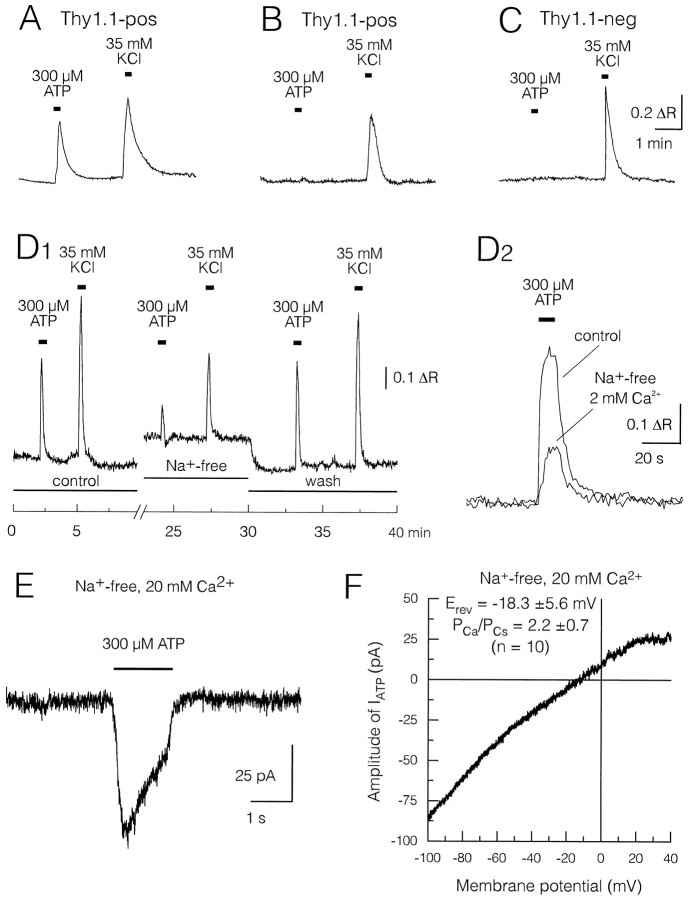
To determine whether activation of P2X receptor channels is associated with changes in the intracellular Ca2+ concentration ([Ca2+]i), we applied ATP (300 μm) to multipolar neurons loaded with fura-2 AM (Fig.9). Again, ATP-induced Ca2+ rises were found only in a subpopulation of Thy1.1-positive cells (Fig. 9A–C), whereas all tested multipolar neurons responded to elevated KCl (35 mm; ΔR = 0.70 ± 0.07, n = 21). We therefore exclude impaired cell viability as an explanation for ATP-response failures. In ATP-sensitive Thy1.1-positive RGCs, the average Ca2+ rise elicited with 300 μmATP amounted to ΔR = 0.60 ± 0.12 (n = 7).
Fig. 9.
P2X receptor channels in RGCs are highly permeable to Ca2+. A, Ca2+imaging experiments from two Thy1.1-positive RGCs (A, B) and one Thy1.1-negative neuron (C) to test for ATP-induced rise of [Ca2+]i. Cells were loaded with the Ca2+ indicator fura-2 and submitted to vital anti-Thy1.1 immunostaining before recording. In imaging experiments, [Ca2+]o was 2 mm, and the external solution contained 1 μmTTX to suppress action-potential generation. A short pulse of 300 μm ATP (15 sec duration) was followed by a washout period of 150 sec. Thereafter, cells were depolarized by application of 35 mm KCl for a period of 15 sec. ATP-induced Ca2+ elevations were found only in a subset of RGCs (A, ΔR = 0.60 ± 0.12,n = 7), whereas all tested neurons responded to elevated KCl. For high KCl responses, ΔR was 0.76 ± 0.19 (n = 6), 0.72 ± 0.13 (n = 7), and 0.64 ± 0.07 (n = 8) in Thy1.1-positive ATP-sensitive, Thy1.1-positive ATP-insensitive, and Thy1.1-negative ATP-insensitive neurons, respectively (p > 0.05, Mann–Whitney test, two-tailed). D1, ATP-induced [Ca2+]i elevations persisted in Na+-free solution. ATP and high KCl were applied in control and Na+-free (Na+substituted by NMDG+) external solution.D2, Superposition of ATP-induced [Ca2+]i rises in normal and Na+-free solution recorded in another RGC. An offset of 0.59 was subtracted from the response in Na+-free solution. On average, ΔR in Na+-free solution was reduced to ∼37% of the ATP-induced [Ca2+]i rises in normal external solution. E, IATPrecorded in Na+-free solution. External Ca2+ was elevated tenfold compared withA–D (Vh = −70 mV).F, Average ramp current obtained from 10 different RGCs to illustrate I–V relationship ofIATP in Na+-free solution. External and pipette solution contained as the only permeant ions 20 mm Ca2+ and 145 mmCs+, respectively. According to the constant field equation, the mean value for Erev measured under bi-ionic conditions (−18.3 ± 5.6 mV) corresponds to a permeability ratioPCa/PCs of 2.2 ± 0.7.
Although in all imaging experiments action potential generation was blocked by TTX, it could not be excluded that ATP-induced depolarizations elicited Ca2+ influx though voltage-activated Ca2+ channels. To eliminate a potential contribution of ICa(V) to the ATP-induced [Ca2+]i rise, 100 μm CdCl2 was included in the external solution. Under these conditions, ATP-induced Ca2+transients were reduced but still observable (50.6 ± 1.9% of the control, n = 3; not illustrated). To record ATP-activated Ca2+ signals in the absence of Na+ entry-mediated depolarization, external Na+ was replaced equimolarly by NMDG+. External Ca2+concentration in Na+-free bath solution was kept at 2 mm. As illustrated in Figure 9D, replacement of extracellular Na+ by NMDG+caused a transient increase of [Ca2+]i, presumably because of inhibition of the Na+/Ca2+exchanger. Although much lower in amplitude, ATP still induced [Ca2+]i rises in Na+-free bath solution (first and third peak in Fig.9D1,D2). In Na+-free solution, ΔR amounted to 0.23 ± 0.04 (n = 5), suggesting that 39% of the ATP-induced [Ca2+]i rise resulted from external Ca2+ entering through P2X receptor channels. This agrees well with the 40% reported by Mateo et al. (1998) for cultured Purkinje neurons.
The lack of specific antagonists complicates the distinction between metabotropic P2Y and ionotropic P2X receptor-mediated responses in Ca2+ imaging experiments. Therefore, we sought to directly measure Ca2+ entry through P2X channels by recording IATP in the absence of external Na+ (Na+ replaced by NMDG+). In Na+- and Ca2+-free solution, no ATP-induced inward currents were recorded at membrane potentials down to −100 mV, indicating that retinal P2X receptor channels are essentially impermeable to NMDG+(PNMDG/PCs < 0.02). To resolve IATP in Na+-free solution, it was necessary to elevate the external Ca2+ concentration ([Ca2+]o) to 20 mm. Although IATP was largely reduced by NMDG+ substitution, it was not eliminated completely (Fig. 9E). An average I–Vrelationship from 10 different RGCs tested in Na+-free solution is illustrated in Figure9F.
The permeability ratioPCa/PCs was estimated from the experimentally determinedErev under bi-ionic conditions with Cs+ and Ca2+ as the only permeant ions at the intracellular and extracellular side, respectively. The mean value of Erev (−18.3 ± 5.6 mV) and the corresponding permeability ratio (PCa/PCs = 2.2 ± 0.7) indicated a more than twofold higher permeability for Ca2+ compared with Cs+ (Fig.9F).
The expression level of Ca2+-permeable P2X receptor channels is unrelated to the Ca2+permeability of non-NMDA receptor channels
Non-NMDA receptor channels with a high permeability for Ca2+ were found in a subset of postnatal rat retinal ganglion cells (Rörig and Grantyn, 1993a; Taschenberger and Grantyn, 1998a). We therefore sought to clarify whether the expression of Ca2+-permeable P2X receptor channels in RGCs is related to the Ca2+ permeability of their non-NMDA receptor channels. Because Ca2+ permeability of non-NMDA receptor channels correlated with inward rectification of kainic acid-activated currents (IKA), we could discriminate between RGCs expressing Ca2+-permeable (RI <1, type II) and Ca2+-impermeable (RI >1, type I) non-NMDA receptor channels by investigating their I–Vcharacteristics (Taschenberger and Grantyn, 1998a).
Recording of IATP and IKawas performed in 31 ATP-sensitive RGCs using agonist concentrations of 100 μm for both ATP and kainic acid. Amplitudes ofIATP at Vh = −70 mV and RIs of IKA were obtained from the correspondingI–V curves. It was found thatIATP was elicited in type II (Fig.10A) as well as in type I RGCs (Fig. 10B). Amplitudes ofIATP and also the shapes ofI–V curves were similar in both types of RGCs. Figure 10C shows the relationship betweenIATP and RIs of IKA. Although we noted a small tendency for type II RGCs to generate largerIATP, a significant correlation was not observed (p = 0.449). Thus, the level of P2X receptor channel expression was unrelated to the Ca2+ permeability of non-NMDA receptor channels.
DISCUSSION
This is the first description of an ATP-activated ion channel in retinal neurons. We show that exogenous ATP excited the majority of cultured retinal ganglion cells but none of the putative amacrine cells. In RGCs, activation of P2X purinoceptors induced inwardly rectifying whole-cell currents and intracellular Ca2+ signals. IATP was also induced by ADP and α,β-mATP but not by adenosine. The purinoceptor antagonist suramin attenuated IATP in a dose-dependent manner. Retinal P2X receptors coupled to nonspecific cation channels with a high permeability for Ca2+. Our results point to an important role of ATP as an extracellular messenger that contributes to Ca2+ signaling in RGCs.
Identification of ATP-sensitive cells
Our conclusion that P2X receptors are selectively expressed in a subpopulation of RGCs crucially relies on an unambiguous cell-type identification in dissociated neuronal cultures. Our experiments were restricted to large multipolar, neurite-bearing cells that generatedINa(V). This excluded the possibility that ATP-induced responses were recorded from photoreceptors, bipolar neurons, or non-neuronal cells. That ATP-sensitive neurons were, in fact, RGCs was concluded on the basis of the following identification criteria. (1) Among short-term cultured neurons, ATP-sensitive cells represented the largest cells, with a soma diameter always >13 μm. (2) ATP-sensitive cells were without exception Thy1.1 positive. (3) In addition, neurons with IATP also generated large voltage-activated Na+ currents and were able to discharge repetitively on depolarization. (4) Finally, and most compelling, ATP-sensitive neurons were glutamatergic, as demonstrated by recording autaptic glutamatergic currents. In contrast, all Thy1.1-negative cells proved to be ATP insensitive. Because the Thy1.1-negative ATP-insensitive neurons had smallerINa(V) and lacked the capacity to generate repetitive spike trains, we concluded that these cells were amacrine cells. Thus, sensitivity to ATP may serve as another criterion to distinguish RGCs from putative amacrine cells in dissociated cell culture.
P2X receptor subtypes in the retina
Previous studies suggested that retinal cells express the purinoceptor subtypes P2X2–5 but not P2X1 or P2X6 (Brändle et al., 1998). Comparison of our results with the properties ofIATP in other preparations gave first indications of which receptor subtypes could mediateIATP in RGCs.
ATP-gated channels of the P2X7 receptor subtype are responsible for ATP-mediated lysis of antigen-presenting cells through the formation of large membrane pores. These pores are readily permeable to organic cations such as NMDG+ and may provide a mechanism of transmitter-induced cell death (Surprenant et al., 1996). This possibility could be considered as a mechanism contributing to the regulated cell death of RGCs during ontogenesis (Beazley et al., 1987). However, recombinant P2X7 receptors are relatively insensitive to the antagonist suramin (Surprenant et al., 1996), and retinal ATP-activated channels are essentially impermeable to NMDG+, which makes a contribution of the P2X7 purinoceptor subtype toIATP in RGCs unlikely.
Recombinant homomeric P2X4 and P2X6 receptors are not activated by α,β-mATP and share the unique pharmacological characteristic of being completely insensitive to suramin (up to 300 μm) (Bo et al., 1995; Buell et al., 1996b; Collo et al., 1996; Soto et al., 1996). In most RGCs, however, α,β-mATP was a potent agonist, and IATP was sensitive to suramin, excluding the possibility that a major fraction ofIATP was mediated by homomeric P2X4 and P2X6 receptors. Heteromeric P2X4+6 receptors are suramin sensitive, but in contrast to IATP in RGCs, acidification of the extracellular solution resulted in a reduction of the ATP-induced currents (Lê et al., 1998).
Homomeric P2X1 purinoceptors channels are activated by ADP, ATP, and α,β-mATP (Valera et al., 1994). However, these channels are characterized by a large unitary conductance (18–19 pS) and completely blocked by low concentrations of suramin (Valera et al., 1994; Evans, 1996). In addition, homomeric P2X1 receptors expressed inXenopus oocytes were activated by submicromolar concentrations of ATP (Valera et al., 1994). The estimated EC50 was more than one order of magnitude lower than in RGCs. Furthermore, complete desensitization of recombinant P2X1 purinoceptors occurs on a millisecond time scale (Lewis et al., 1995). It is thus unlikely that the P2X receptors in RGCs belong to the P2X1 subtype.
In a minority of RGCs, the properties of IATPcorresponded to the characteristics described for homomeric P2X2 or P2X5 receptor channels. These purinoceptor subtypes are antagonized by suramin, are relatively insensitive to α,β-mATP and desensitize only negligibly (Brake et al., 1994; Collo et al., 1996; Garcia-Guzman et al., 1996).
Although the pharmacological properties of IATPwere compatible with an expression of the P2X3 purinoceptor in RGCs, it is conceivable that retinal ATP-gated channels are P2X2+3 heteromers. Homomeric P2X3 receptors desensitize on a millisecond time scale (Chen et al., 1995; Lewis et al., 1995). Heterologous expression of P2X2 and P2X3 receptors gave rise to functional properties not found in the respective homomeric receptors, e.g., slowly desensitizing currents that were activated by α,β-mATP (Lewis et al., 1995). Among native P2X receptor channels, rapidly desensitizing ATP-induced currents were recorded in a subset of nociceptive neurons in the trigeminal ganglia (Cook et al., 1997) but not in nodose (Lewis et al., 1995) or dorsal root ganglion cells (Bean, 1990). The kinetic properties ofIATP in RGCs resembled those of dorsal root ganglion cells (Krishtal et al., 1983; Bean, 1990), e.g., inactivation and recovery from inactivation were in the range of seconds and minutes, respectively. The values for the EC50 and the Hill coefficient in RGCs were also similar to those of rat sensory neurons (Krishtal et al., 1983). Hill slopes larger than unity were reported, however, for bullfrog dorsal root ganglion cells (Bean, 1990). Single-channel events of native P2X receptors in DRGs were brief and flickery (Bean et al., 1990). Such brief openings could account for our inability to resolve single-channel events in outside-out patches from RGCs. Our estimate for the apparent single-channel conductance of P2X receptor channels in RGCs was lower than the values reported previously for dorsal root ganglion cells (Bean et al., 1990). However, in that study a membrane potential of −100 mV was applied, and the slope conductance of IATP in RGCs atVh = −100 mV was almost twice as large compared with Vh = −70 mV.
The kinetic properties of IATP may be influenced by manipulating the external Ca2+ and Na+ concentrations. In bullfrog DRG neurons, the deactivation of IATP was accelerated with higher [Ca2+]o (Bean, 1990). In rat nucleus solitarii neurons, high external Ca2+ accelerated the inactivation of IATP (Ueno et al., 1992). Desensitization through a calcium-dependent calcineurin-mediated mechanism has recently been suggested for recombinant P2X3 receptor channels (King et al., 1997). Because retinal P2X receptor channels are Ca2+ permeable, heterogeneous inactivation kinetics of IATP during sustained agonist application thus may be related to peculiarities in the regulation of [Ca2+]i in individual RGCs rather than to the expression of different P2X subtypes. Our estimate for the relative Ca2+ permeabilityPCa/PCs of retinal P2X receptor channels is similar to previously reported values forPCa/PNa of recombinant heteromeric P2X2+3 channels (Virginio et al., 1998), taking into account aPCs/PNa = 0.72 (Evans et al., 1996).
Possible role of P2X receptor channels in RGC
The physiological role of P2X receptor channels in RGCs is largely unknown. Our results indicate that ATP can act as an excitatory neurotransmitter or neuromodulator on retinal ganglion cells and thereby influence visual information processing in the inner retina. In the developing ferret retina, cholinergic transmission is required for the propagation of spontaneous excitation waves in the ganglion cell layer (Feller et al., 1996). An attractive, yet at present speculative, hypothesis is that ATP is co-released with acetylcholine from starburst amacrine cells and contributes to the generation of Ca2+ waves in the inner retina by activation of P2X receptors in RGCs. It is unlikely, however, that ATP alone serves as a fast excitatory neurotransmitter in an amacrine–ganglion cell synapse, because in retinal whole mounts from the postnatal rat, excitatory synaptic activity in the ganglion cell layer was completely abolished after addition of the glutamate receptor antagonist DNQX (Rörig and Grantyn, 1993b).
Together with previous studies (Aizenman et al., 1988; Rörig and Grantyn, 1993a; Taschenberger and Grantyn, 1998a), our present results demonstrate that postnatal rat RGCs express several types of ligand-gated ion channels with a high permeability for Ca2+. ATP-activated P2X receptor channels may represent a particularly important pathway for external Ca2+ entry in RGCs, not only because of their highPCa/PCs but also because of their inwardly rectifying I–Vrelationship. In contrast to NMDA receptor channels, P2X receptor channels thus mediate the largest Ca2+ influx at resting or hyperpolarized potentials when the driving force for Ca2+ is high.
Footnotes
This work was supported by the Deutsche Forschungsgemeinschaft (SFB 515). We thank A. Draguhn and W. Müller for helpful discussion and critically reading an earlier version of this manuscript. The technical assistance of Mrs. K. Przezdziecki is gratefully acknowledged.
Correspondence should be addressed to Dr. H. Taschenberger: Vollum Institute, Oregon Health Sciences University L-474, 3181 S.W. Sam Jackson Park Road, Portland, OR 97201.
REFERENCES
- 1.Aizenman E, Frosch MP, Lipton SA. Responses mediated by excitatory amino acid receptors in solitary retinal ganglion cells from rat. J Physiol (Lond) 1988;396:75–91. doi: 10.1113/jphysiol.1988.sp016951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson CR, Stevens CF. Voltage clamp analysis of acetylcholine produced end-plate current fluctuations at frog neuromuscular junction. J Physiol (Lond) 1973;235:655–691. doi: 10.1113/jphysiol.1973.sp010410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Balachandran C, Bennett MR. ATP-activated cationic and anionic conductances in cultured rat hippocampal neurons. Neurosci Lett. 1996;204:73–76. doi: 10.1016/0304-3940(96)12320-x. [DOI] [PubMed] [Google Scholar]
- 4.Bean BP. ATP-activated channels in rat and bullfrog sensory neurons: concentration dependence and kinetics. J Neurosci. 1990;10:1–10. doi: 10.1523/JNEUROSCI.10-01-00001.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bean BP, Williams CA, Ceelen PW. ATP-activated channels in rat and bullfrog sensory neurons: current–voltage relation and single-channel behavior. J Neurosci. 1990;10:11–19. doi: 10.1523/JNEUROSCI.10-01-00011.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beazley LD, Perry VH, Baker B, Darby JE. An investigation into the role of ganglion cells in the regulation of division and death of other retinal cells. Brain Res. 1987;430:169–184. doi: 10.1016/0165-3806(87)90151-9. [DOI] [PubMed] [Google Scholar]
- 7.Blazynski C, Perez MT. Adenosine in vertebrate retina: localization, receptor characterization, and function. Cell Mol Neurobiol. 1991;11:463–484. doi: 10.1007/BF00734810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bo X, Zhang Y, Nassar M, Burnstock G, Schoepfer R. A P2X purinoceptor cDNA conferring a novel pharmacological profile. FEBS Lett. 1995;375:129–133. doi: 10.1016/0014-5793(95)01203-q. [DOI] [PubMed] [Google Scholar]
- 9.Brake AJ, Julius D. Signaling by extracellular nucleotides. Annu Rev Cell Dev Biol. 1996;12:519–541. doi: 10.1146/annurev.cellbio.12.1.519. [DOI] [PubMed] [Google Scholar]
- 10.Brake AJ, Wagenbach MJ, Julius D. New structural motif for ligand-gated ion channels defined by an ionotropic ATP receptor. Nature. 1994;371:519–523. doi: 10.1038/371519a0. [DOI] [PubMed] [Google Scholar]
- 11.Brändle U, Guenther E, Irrle C, Wheeler-Schilling TH. Gene expression of the P2X receptors in the rat retina. Mol Brain Res. 1998;59:269–272. doi: 10.1016/s0169-328x(98)00159-4. [DOI] [PubMed] [Google Scholar]
- 12.Brewer GJ, Cotman CW. Survival and growth of hippocampal neurons in defined medium at low density: advantages of a sandwich culture technique or low oxygen. Brain Res. 1989;494:65–74. doi: 10.1016/0006-8993(89)90144-3. [DOI] [PubMed] [Google Scholar]
- 13.Buell G, Collo G, Rassendren F. P2X receptors: an emerging channel family. Eur J Neurosci. 1996a;8:2221–2228. doi: 10.1111/j.1460-9568.1996.tb00745.x. [DOI] [PubMed] [Google Scholar]
- 14.Buell G, Lewis C, Collo G, North RA, Surprenant A. An antagonist-insensitive P2X receptor expressed in epithelia and brain. EMBO J. 1996b;15:55–62. [PMC free article] [PubMed] [Google Scholar]
- 15.Chen CC, Akopian AN, Sivilotti L, Colquhoun D, Burnstock G, Wood JN. A P2X purinoceptor expressed by a subset of sensory neurons. Nature. 1995;377:428–431. doi: 10.1038/377428a0. [DOI] [PubMed] [Google Scholar]
- 16.Collo G, North RA, Kawashima E, Merlo Pich E, Neidhart S, Surprenant A, Buell G. Cloning of P2X5 and P2X6 receptors and the distribution and properties of an extended family of ATP-gated ion channels. J Neurosci. 1996;16:2495–2507. doi: 10.1523/JNEUROSCI.16-08-02495.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cook SP, Vulchanova L, Hargreaves KM, Elde R, McCleskey EW. Distinct ATP receptors on pain-sensing and stretch-sensing neurons. Nature. 1997;387:505–508. doi: 10.1038/387505a0. [DOI] [PubMed] [Google Scholar]
- 18.Edwards FA. ATP receptors. Curr Opin Neurobiol. 1994;4:347–352. doi: 10.1016/0959-4388(94)90095-7. [DOI] [PubMed] [Google Scholar]
- 19.Edwards FA, Gibb AJ, Colquhoun D. ATP receptor-mediated synaptic currents in the central nervous system. Nature. 1992;359:144–147. doi: 10.1038/359144a0. [DOI] [PubMed] [Google Scholar]
- 20.Evans RJ. Single channel properties of ATP-gated cation channels (P2X receptors) heterologously expressed in Chinese hamster ovary cells. Neurosci Lett. 1996;212:212–214. doi: 10.1016/0304-3940(96)12804-4. [DOI] [PubMed] [Google Scholar]
- 21.Evans RJ, Derkach V, Surprenant A. ATP mediates fast synaptic transmission in mammalian neurons. Nature. 1992;357:503–505. doi: 10.1038/357503a0. [DOI] [PubMed] [Google Scholar]
- 22.Evans RJ, Lewis C, Virginio C, Lundstrom K, Buell G, Surprenant A, North RA. Ionic permeability of, and divalent cation effects on, two ATP-gated cation channels (P2X receptors) expressed in mammalian cells. J Physiol (Lond) 1996;497:413–422. doi: 10.1113/jphysiol.1996.sp021777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Feller MB, Wellis DP, Stellwagen D, Werblin FS, Shatz CJ. Requirement for cholinergic synaptic transmission in the propagation of spontaneous retinal waves. Science. 1996;272:1182–1187. doi: 10.1126/science.272.5265.1182. [DOI] [PubMed] [Google Scholar]
- 24.Garcia-Guzman M, Soto F, Laube B, Stühmer W. Molecular cloning and functional expression of a novel rat heart P2X purinoceptor. FEBS Lett. 1996;388:123–127. doi: 10.1016/0014-5793(96)00499-1. [DOI] [PubMed] [Google Scholar]
- 25.Grantyn R, Korenbaum E. Easy identification of dissociated rat retinal ganglion cells by a size criterion. In: Kettenmann H, Grantyn R, editors. Practical electrophysiological methods: a guide for in vitro studies in vertebrate neurobiology. Wiley-Liss; New York: 1992. pp. 84–87. [Google Scholar]
- 26.Greenwood D, Yao WP, Housley GD. Expression of the P2X2 receptor subunit of the ATP-gated ion channel in the retina. NeuroReport. 1997;8:1083–1088. doi: 10.1097/00001756-199703240-00004. [DOI] [PubMed] [Google Scholar]
- 27.Guenther E, Schmid S, Grantyn R, Zrenner E. In vitro identification of retinal ganglion cells in culture without the need of dye labeling. J Neurosci Methods. 1994;51:177–181. doi: 10.1016/0165-0270(94)90008-6. [DOI] [PubMed] [Google Scholar]
- 28.Housley GD. Extracellular nucleotide signaling in the inner ear. Mol Neurobiol. 1998;16:21–48. doi: 10.1007/BF02740601. [DOI] [PubMed] [Google Scholar]
- 29.Huxlin KR, Goodchild AK. Retinal ganglion cells in the albino rat: revised morphological classification. J Comp Neurol. 1997;385:309–323. [PubMed] [Google Scholar]
- 30.Iino M, Ozawa S, Tsuzuki K. Permeation of calcium through excitatory amino acid receptor channels in cultured rat hippocampal neurones. J Physiol (Lond) 1990;424:151–165. doi: 10.1113/jphysiol.1990.sp018060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jahr CE, Jessell TM. ATP excites a subpopulation of rat dorsal horn neurones. Nature. 1983;304:730–733. doi: 10.1038/304730a0. [DOI] [PubMed] [Google Scholar]
- 32.King B, Chen CC, Akopian AN, Burnstock G, Wood JN. A role for calcineurin in the desensitization of the P2X3 receptor. NeuroReport. 1997;8:1099–1102. doi: 10.1097/00001756-199703240-00007. [DOI] [PubMed] [Google Scholar]
- 33.Krishtal OA, Marchenko SM, Pidoplichko VI. Receptor for ATP in the membrane of mammalian sensory neurones. Neurosci Lett. 1983;35:41–45. doi: 10.1016/0304-3940(83)90524-4. [DOI] [PubMed] [Google Scholar]
- 34.Lewis C, Neidhart S, Holy C, North RA, Buell G, Surprenant A. Coexpression of P2X2 and P2X3 receptor subunits can account for ATP-gated currents in sensory neurons. Nature. 1995;377:432–435. doi: 10.1038/377432a0. [DOI] [PubMed] [Google Scholar]
- 35.Lê KT, Babinski K, Séguéla P. Central P2X4 and P2X6 channel subunits coassemble into a novel heteromeric ATP receptor. J Neurosci. 1998;18:7152–7159. doi: 10.1523/JNEUROSCI.18-18-07152.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mateo J, Garcia Lecea M, Miras Portugal MT, Castro E. Ca2+ signals mediated by P2X-type purinoceptors in cultured cerebellar Purkinje cells. J Neurosci. 1998;18:1704–1712. doi: 10.1523/JNEUROSCI.18-05-01704.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Meyer Franke A, Kaplan MR, Pfrieger FW, Barres BA. Characterization of the signaling interactions that promote the survival and growth of developing retinal ganglion cells in culture. Neuron. 1995;15:805–819. doi: 10.1016/0896-6273(95)90172-8. [DOI] [PubMed] [Google Scholar]
- 38.Nakazawa K, Inoue K, Fujimori K, Takanaka A. Effects of ATP antagonists on purinoceptor-operated inward currents in rat phaeochromocytoma cells. Pflügers Arch. 1991;418:214–219. doi: 10.1007/BF00370517. [DOI] [PubMed] [Google Scholar]
- 39.Neal M, Cunningham J. Modulation by endogenous ATP of the light-evoked release of ACh from retinal cholinergic neurones. Br J Pharmacol. 1994;113:1085–1087. doi: 10.1111/j.1476-5381.1994.tb17106.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Neher E. Correction for liquid junction potentials in patch clamp experiments. Methods Enzymol. 1992;207:123–131. doi: 10.1016/0076-6879(92)07008-c. [DOI] [PubMed] [Google Scholar]
- 41.North RA, Barnard EA. Nucleotide receptors. Curr Opin Neurobiol. 1997;7:346–357. doi: 10.1016/s0959-4388(97)80062-1. [DOI] [PubMed] [Google Scholar]
- 42.Perry VH, Morris RJ, Raisman G. Is Thy-1 expressed only by ganglion cells and their axons in the retina and optic nerve? J Neurocytol. 1984;13:809–824. doi: 10.1007/BF01148495. [DOI] [PubMed] [Google Scholar]
- 43.Rörig B, Grantyn R. Rat retinal ganglion cells express Ca2+-permeable non-NMDA glutamate receptors during the period of histogenetic cell death. Neurosci Lett. 1993a;153:32–36. doi: 10.1016/0304-3940(93)90070-2. [DOI] [PubMed] [Google Scholar]
- 44.Rörig B, Grantyn R. Glutamatergic and GABAergic synaptic currents in ganglion cells from isolated retinae of pigmented rats during postnatal development. Dev Brain Res. 1993b;74:98–110. doi: 10.1016/0165-3806(93)90088-r. [DOI] [PubMed] [Google Scholar]
- 45.Séguéla P, Haghighi A, Soghomonian JJ, Cooper E. A novel neuronal P2X ATP receptor ion channel with widespread distribution in the brain. J Neurosci. 1996;16:448–455. doi: 10.1523/JNEUROSCI.16-02-00448.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shen KZ, North RA. Excitation of rat locus coeruleus neurons by adenosine 5′-triphosphate: ionic mechanism and receptor characterization. J Neurosci. 1993;13:894–899. doi: 10.1523/JNEUROSCI.13-03-00894.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Soto F, Garcia-Guzman M, Gomez Hernandez JM, Hollmann M, Karschin C, Stühmer W. P2X4: an ATP-activated ionotropic receptor cloned from rat brain. Proc Natl Acad Sci USA. 1996;93:3684–3688. doi: 10.1073/pnas.93.8.3684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Soto F, Garcia-Guzman M, Stühmer W. Cloned ligand-gated channels activated by extracellular ATP (P2X receptors). J Membr Biol. 1997;160:91–100. doi: 10.1007/s002329900298. [DOI] [PubMed] [Google Scholar]
- 49.Stoop R, Surprenant A, North RA. Different sensitivities to pH of ATP-induced currents at four cloned P2X receptors. J Neurophysiol. 1997;78:1837–1840. doi: 10.1152/jn.1997.78.4.1837. [DOI] [PubMed] [Google Scholar]
- 50.Surprenant A, Rassendren F, Kawashima E, North RA, Buell G. The cytolytic P2Z receptor for extracellular ATP identified as a P2X receptor (P2X7). Science. 1996;272:735–738. doi: 10.1126/science.272.5262.735. [DOI] [PubMed] [Google Scholar]
- 51.Taschenberger H, Grantyn R. Several types of Ca2+ channels mediate glutamatergic synaptic responses to activation of single Thy-1-immunolabeled rat retinal ganglion neurons. J Neurosci. 1995;15:2240–2254. doi: 10.1523/JNEUROSCI.15-03-02240.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Taschenberger H, Grantyn R. Interaction of calcium-permeable non-N-methyl-d-aspartate receptor channels with voltage-activated potassium and calcium currents in rat retinal ganglion cells in vitro. Neuroscience. 1998a;84:877–896. doi: 10.1016/s0306-4522(97)00541-1. [DOI] [PubMed] [Google Scholar]
- 53.Taschenberger H, Grantyn R. Expression of ATP-gated ion channels by retinal neurons in vitro. Proc Göttingen Neurobiol Conf. 1998b;26:443. [Google Scholar]
- 54.Ueno S, Harata N, Inoue K, Akaike N. ATP-gated current in dissociated rat nucleus solitarii neurons. J Neurophysiol. 1992;68:778–785. doi: 10.1152/jn.1992.68.3.778. [DOI] [PubMed] [Google Scholar]
- 55.Valera S, Hussy N, Evans RJ, Adami N, North RA, Surprenant A, Buell G. A new class of ligand-gated ion channel defined by P2x receptor for extracellular ATP. Nature. 1994;371:516–519. doi: 10.1038/371516a0. [DOI] [PubMed] [Google Scholar]
- 56.Virginio C, North RA, Surprenant A. Calcium permeability and block at homomeric and heteromeric P2X2 and P2X3 receptors, and P2X receptors in rat nodose neurones. J Physiol (Lond) 1998;510:27–35. doi: 10.1111/j.1469-7793.1998.027bz.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.von Kügelgen I, Starke K. Noradrenaline-ATP co-transmission in the sympathetic nervous system. Trends Pharmacol Sci. 1991;12:319–324. doi: 10.1016/0165-6147(91)90587-i. [DOI] [PubMed] [Google Scholar]
- 58.Vulchanova L, Arvidsson U, Riedl M, Wang J, Buell G, Surprenant A, North RA, Elde R. Differential distribution of two ATP-gated channels (P2X receptors) determined by immunocytochemistry. Proc Natl Acad Sci USA. 1996;93:8063–8067. doi: 10.1073/pnas.93.15.8063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Westfall DP, Sedaa KO, Shinozuka K, Bjur RA, Buxton IL. ATP as a cotransmitter. Ann NY Acad Sci. 1990;603:300–310. doi: 10.1111/j.1749-6632.1990.tb37681.x. [DOI] [PubMed] [Google Scholar]
- 60.Zimmermann H. Biochemistry, localization and functional roles of ecto-nucleotidases in the nervous system. Prog Neurobiol. 1996;49:589–618. doi: 10.1016/0301-0082(96)00026-3. [DOI] [PubMed] [Google Scholar]