Abstract
Lumbar 3-joint complex degeneration is a multifactorial, pathological process. Previous studies included insufficient quantitative analyses to prove the relationship between disc degeneration and facet joint osteoarthritis (OA). We assessed the correlation between intervertebral disc and lumbar facet joint degeneration using computed tomography (CT) and magnetic resonance imaging (MRI) parameters.
A total of 152 participants who underwent conventional MRI and CT in the clinostat position were included in this study. The presence of lumbar disc degeneration was identified using the Pfirrmann grading system, and the presence of lumbar facet joint degeneration was identified using the Weishaupt grading system. Facet tropism was defined as a divergence more than 7° between the facet joint angles of both sides at the same segment. The intervertebral disc heights were also measured.
Most facet joint OA probably appeared at the segment with intervertebral disc degeneration of more than grade III. Facet joint OA was significantly exacerbated with the progression of disc degeneration grade. The intervertebral height significantly decreased with the progression of facet joint degeneration grades, except for grades 0 and 1.
Our current study found that each individual joint degeneration influences the other 2 in the lumbar 3-joint complex. Facet tropism was significantly associated with lumbar disc degeneration. Narrowing of the intervertebral disc height probably aggravates the facet joint degeneration further at the same level.
Keywords: degeneration, facet tropism, intervertebral disc height, intervertebral disc, lumbar complex joints degeneration, lumbar facet joint
Key Points
Highlights: The degeneration of the lumbar 3-joints complex is a disease process.
There is a correlation between intervertebral disc and lumbar facet joints.
MRI and CT scans show increasing degeneration with increasing grade.
1. Introduction
Each lumbar segment consists of the paired posterior synovial joints (facet joints) and the anteriorly situated intervertebral disc, which form the lumbar complex joints and are also known as the lumbar 3-joint complex.[1] Many biomechanical studies have considered that the intervertebral disc and the 2 facet joints carry loads together in the normal lumbar spine.[2,3] The 2 facet joints transmit segmental load between 3% and 25% during normal conditions.[4] Lumbar facet joints are specifically designed to allow for a greater range of flexion motion on the sagittal plane but prevent gross rotatory instability from occurring.[5]
Many studies determined that the intervertebral disc is the initial site of spinal degeneration and that the facet joint degenerates as a result of disc degeneration.[5–9] However, other authors have indicated that disc degeneration does not necessarily precede facet degeneration.[10–13] Videman et al[12] reported that facet joint degeneration appears to precede disc degeneration in 20% of thoracic and lumbar segments. Muehleman and coworkers[14] found that facet joint degeneration is common and occurs as early as age 15 years. Furthermore, Eubanks et al[10] found that facet joint osteoarthritis (OA) often occurs before changes due to disc degeneration in younger individuals.
Many researchers believed that low back pain, as a result of lumbar degeneration, begins in the intervertebral disc, followed by spine malalignment and facet joint degeneration.[6,15] It is quite likely that the intervertebral disc and facet joints contribute to the initial degenerative process.[11,14,16] However, the actual sequence of events is unclear[14] because no study has examined low back pain in a large, community-based sample.[13] In addition, previous studies did not have enough quantitative data to prove the relationship between disc degeneration and facet joint OA.[13]
Our current study aimed to assess the correlation between lumbar intervertebral disc and facet joint degeneration using computed tomography (CT) and magnetic resonance imaging (MRI) parameters and to further analyze the risk factors for lumbar degeneration.
2. Materials and methods
2.1. Ethics statement
This study was approved by the ethical review committee of The First Affiliated Hospital of Nanchang University.
2.2. Patient and inclusion criteria
We retrospectively selected patients aged between 18 and 85 years who underwent both conventional MRI (1.5T, Siemens) and CT (SOMATOM Definition AS) in the clinostat position at our hospital, the Haitai PACS clinical system, between November 2016 and November 2017.
Exclusion criteria were MRI or CT deficiency, lumbar spondylolisthesis, lumbar scoliosis (Cobb angle >10°), history of lumbar surgery, lumbar fracture or infection, and lumbar tumor. The total number of patients was 185.
Thirty-three patients were excluded from this study: 10 patients who had lumbar spondylolisthesis; 7 patients who had scoliosis (Cobb angle >10°); 8 patients who had old lumbar fractures; 4 patients who had a lumbar infection; and 4 patients who had lumbar tumors. Finally, 152 patients were included. The subjects were between 19 and 83 years old (average age, 56.3 ± 12.4 years). There were 78 females and 74 males included in the study. None of the patients had undergone surgery or chemonucleolysis before the study.
2.3. Radiographic measurements
MRI was used to determine disc degeneration. CT scans were used to measure facet joint angles and to determine tropism. Two independent observers (2 clinical senior attending physicians) performed the radiographic analysis. Each observer reviewed each radiograph independently. When the 3-joint complex was scored by 2 observers who were in disagreement, a consensus was reached as determined by the chief physician. The lower 3 lumbar levels (L3–4, L4–5, and L5–S1) were examined. Lumbar facet joints were graded on the left and right sides. Facet joint OA was divided into 4 grades according to the CT scan (FOV = 16 cm; thickness=5 mm; matrix = 512 × 512) using Weishaup grading[17] (Figs. 1 and 2). Disc degeneration was classified into 5 grades according to T2-weighted midsagittal images (SAG T2 FSE; TR = 3200 ms; TE = 100 ms; FOV = 16 cm; thickness = 5 mm; matrix = 320 × 224) and according to the grading system proposed by Pfirrmann et al[18] (Fig. 3). According to the measurement method introduced by Noren et al,[19] axial angles of L3/4, L4/5, and L5/S1 were measured on MRI T2 images. The angle of the lumbar facet joint is between the anterior and posterior ends of the articular surface of the superior articular process and the median sagittal line of the same vertebral body. According to the previously reported classification of facet joint asymmetry,[20] facet joint asymmetry is defined as the absolute value of the subtraction of left and right facet joint angles ≥7°. The disc height was defined as the average distance of the anterior, intermediate, and posterior disc space heights.[21]
Figure 1.

(A) The facet joint with grade 0 degeneration. (B) The facet joint with grade 1 degeneration.
Figure 2.

(A) The facet joint with grade 2 degeneration. (B) The facet joint with grade 3 degeneration.
Figure 3.

(A) The disc with grade I degeneration. (B) The disc with grade II degeneration. (C) The disc with grade III degeneration. (D) The disc with grade IV degeneration. (E) The disc with grade V degeneration.
2.4. Statistical analysis
All data were analyzed with SPSS 22.0 statistical software (SPSS Inc., Chicago, IL). The chi-square test was used to compare the radiographic parameters. The correlation between disc degeneration and facet joint OA was examined using Spearman correlation. Correlations exceeding 0.5 have been suggested as the minimum to provide evidence of construct validity (convergent validity).[22] Least significant difference t tests were used to compare the intervertebral disc height among the study groups. We analyzed the interobserver reliability and intraobserver reliability (agreement) for the variance of radiographic parameter grading using Cohen k agreement analysis. A P-value of <.05 was considered statistically significant.
3. Results
A total of 456 lumbar motion segments were evaluated with both CT and MRI. The differences in the mean ages of the female and male patients (female, 56.0 years; male, 56.7 years) were not statistically significant.
3.1. Degeneration of the disc and facet joint
Tables 1 and 2 show each grade of disc degeneration and facet joint OA for all 456 selected lumbar 3-joint complexes according to Weishaup grading and Pfirrmann grading methods. There were 10 intervertebral discs with grade 1 degeneration: 9 left facet joints had grade 0 degeneration and 1 left facet joint had grade 1 degeneration. Ten right facet joints had grade 0 degeneration. There were 47 intervertebral discs with grade 2 degeneration: 4 left facet joints had grade 0 degeneration and 43 had a grade 1 degeneration. Six right facet joints had grade 0 degeneration, 39 had grade 1 degeneration, and 2 had grade 2 degeneration. There were 139 intervertebral discs with a grade 3 degeneration. There were 110 left facet joints with grade 1 degeneration: 28 had grade 2 degeneration, 105 had grade 1 degeneration, and 1 had grade 3 degeneration. Thirty-two had grade 2 degeneration and 2 had grade 3 degeneration. There were 197 intervertebral discs with degeneration grade 4: 1 left facet joint had grade 1 degeneration, 140 had grade 2 degeneration, and 56 had grade 3 degeneration. One right facet joint had grade 1 degeneration, 138 had grade 2 degeneration, and 58 had grade 3 degeneration. There were 63 intervertebral discs with grade 5 degeneration. Twenty-five left facet joints had grade 2 degeneration and 38 had grade 3 degeneration. Twenty-four right facet joints had grade 2 degeneration and 39 had grade 3 degeneration.
Table 1.
Comparison of the degeneration data of the disc and the left facet joint.

Table 2.
Comparison of the degeneration data of the disc and the right facet joint.

Left facet joint OA and right facet joint OA significantly increased with the progression of the disc degeneration grade (both P < .001; Spearman = 0.824 and 0.806, respectively) (Tables 1 and 2). There were no significant differences based on sex regarding the grading of disc and facet joint degeneration for each lumbar 3-joint complex.
3.2. Disc degeneration and facet joint tropism
Table 3 presents the relationship between facet tropism and disc degeneration for each 3-joint complex. A total of 227 motion segments had tropism in this study. One hundred (61%) motion segments had tropism with disc degeneration grade IV. Forty (63%) motion segments had tropism with disc degeneration grade V. Facet tropism was significantly different (P < .001) with disc degeneration.
Table 3.
Comparison of the degeneration data of the disc and facet tropism.

3.3. Disc degeneration and intervertebral height
The intervertebral disc height was measured at each segment with different disc degeneration grades. The mean disc height was 12.65 ± 0.69 mm when the disc degeneration was grade I, 12.05 ± 1.08 mm when the disc degeneration was grade II, 11.51 ± 1.23 mm when the disc degeneration was grade III, 9.97 ± 1.17 mm when the disc degeneration was grade IV, and 7.34 ± 1.31 mm when the disc degeneration was grade V.
The intervertebral height significantly decreased with the progression of disc degeneration grade, but there was no significant difference between grade I and grade II (I vs III and II vs III: P < .05), (I vs IV, I vs V, II vs IV, II vs V, III vs IV, III vs V, and IV vs V: P < .001). Figure 4 shows the associations between disc degeneration and intervertebral height. The intervertebral disc height significantly decreased with disc degeneration (Pearson r = −0.728).
Figure 4.

The trend of intervertebral height decreased with the progression of the disc degeneration grade.
3.4. Facet joint degeneration and intervertebral height
The intervertebral disc height was also measured at each segment with different facet joint degeneration grades. The mean intervertebral height was 12.44 ± 0.56 mm when the facet joint degeneration was grade 0, 11.63 ± 1.24 mm when the facet joint degeneration was grade 1, 9.88 ± 1.65 mm when the facet joint degeneration was grade 2, and 8.92 ± 1.80 mm when the facet joint degeneration was grade 3.
When the facet joint degeneration grade increased, the intervertebral disc height significantly decreased, except between grade 0 and grade 1 (0 vs 2, 0 vs 3, 1 vs 2, 1 vs 3, and 2 vs 3: P < .001). Figure 5 shows the association between facet joint degeneration and intervertebral height. The intervertebral disc height significantly decreased with facet joint degeneration (Pearson r = −0.573).
Figure 5.
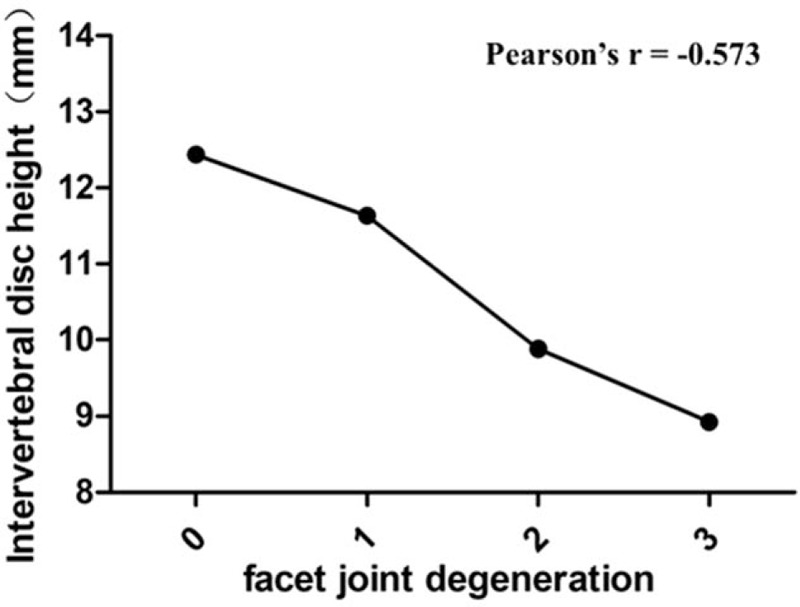
The trend of intervertebral height decreased with the progression of the facet joint degeneration grade.
3.5. Reliability of variance for radiographic evaluation
The weighted kappa coefficient for the interobserver agreement regarding the disc degeneration evaluation was 0.729. The weighted kappa coefficient for the interobserver agreement regarding the facet degeneration evaluation was 0.679.
4. Discussion
This study demonstrates that each individual joint degeneration influences the other 2 in the lumbar 3-joint complex. The results of this study provide evidence of a strong positive correlation between disc degeneration and facet joint degeneration. The study did not reveal a relatively high proportion of degenerated facet joints of moderate to severe grades (grades 2–3) accompanied by milder grades of disc degeneration (grades 1–2), which may not be in complete agreement with results reported in previous studies.[6–9,12] This discrepancy could be solved by designing a prospective long-term follow-up study and creating uniform degeneration grading systems for both intervertebral discs and facet joints.
After analyzing the radiographic parameters of 456 lumbar motion segments, we found a strong positive correlation between the severity of facet OA and disc degeneration. We found 139 lumbar motion segments with grade 3 disc degeneration. A total of 110 (79.1%) lumbar motion segments had grade 1 left facet joint degeneration, while 105 (75.5%) lumbar motion segments had grade 1 right facet joint degeneration. Most facet joints undergo mild degeneration when the lumbar disc is moderately degenerated. Therefore, disc degeneration could potentially occur prior to degeneration of the facet joint. This concept is in agreement with the previous findings of Fujiwara.[9] Vernon-Roberts and Pirie[23] dissected more than 100 lumbar spines and found that disc degeneration was always accompanied by degenerative changes of the facet joint. Based on their observations, there was a negative correlation between the severity of OA and disc structure (the lesser the degeneration, the lesser the degree of OA).
This study also showed a significant correlation between facet tropism and disc degeneration. The role of facet tropism in the pathogenesis of disc degeneration is a controversial.[24] Vanharanta et al[20] reported that the correlation between facet tropism and disc degeneration was not significant. However, Noren et al[19] concluded that facet joint tropism is an important risk factor in the development of disc degeneration. Additionally, Dai[25] performed a study of 106 subjects and reported that a significant correlation existed between the degree of disc degeneration and facet joint tropism for patients with degenerative spondylolisthesis. Kong et al[24] found a higher incidence of highly degenerated discs at L4/5, which was observed within the facet tropism group. Schleich et al[26] indicated that facet tropism and sagittal orientation of the facet joint represent risk factors for the development of early biochemical alterations of lumbar intervertebral discs. Mohanty et al[27] performed a study of 426 subjects and confirmed the existence of a significant association between lumbar intervertebral disc prolapse and facet tropism. However, the previous studies[28,29] found that facet tropism did not exhibit an association with facet joint OA at the L3/4, L4/5, and L5/S1 levels. In this study, a total of 197 (61%) of lumbar motion segments had facet tropism with disc degeneration IV and 63 (63%) of lumbar motion segments had facet tropism with disc degeneration V. The results of this study showed that there is a significant correlation between facet tropism and disc degeneration. These findings are consistent with those of previous reports.
Many biomechanical studies reported that 2 facet joints may carry parallel loading in the lumbar spine.[2,3] Furthermore, facet tropism may alter the biomechanics of the lumbar spine. Cyron and Hutton[30] deduced that the annulus fibrosus on the side with greater coronal orientation may undergo a higher compressive load and increased rotational stress. Therefore, the loading imbalance would accelerate the degeneration of the facet joints and intervertebral discs.[25]
In this study, we found that for increasing grades of disc degeneration (grades 2–5), there was a significant intervertebral height loss at each level. Teichtahl et al[31] performed a study of 72 community-based individuals not previously examined for low back pain and reported that the estimated marginal means of the intervertebral disc height were 13.2 mm, 11.5 mm, 10.3 mm, and 4.2 mm for disc degeneration grades 2, 3, 4, and 5, respectively, at the L4/5 level. They demonstrated narrowing of 0.98 to 1.60 mm in the disc at various levels within the lumbosacral spine. We assessed intervertebral disc height for each grade of disc degeneration. We found that the average disc height associated with grade 2 disc degeneration was 12.05 mm. The average disc height associated with grade 3 disc degeneration was 11.51 mm. For grade 4 disc degeneration, the average disc height was 9.97 mm and for grade 5 disc degeneration, the average disc height was 7.34 mm. In our study, the intervertebral disc height differences between disc degeneration grades 2 and 3 were less than 0.98 mm. The intervertebral disc height showed no significant differences between disc degeneration grades 1 and 2. The difference between disc degeneration grades 1 and 2 was equivalent to the signal intensity according to Pfirrmann scores.
Our findings showed that intervertebral height loss probably leads to deterioration of the facet joint. Using a large sample, we found that the correlation coefficient of the correlation between facet joint degeneration and disc height was −0.573. Only a few studies have reported the correlation between facet joint degeneration and intervertebral disc height. Suri et al[13] found that some individuals experience facet degeneration without any loss of disc height. To our knowledge, the facet joints play an important role in load transfer because they provide posterior load-bearing assistance.[2] The percentage of segmental load transmitted through the posterior elements can increase up to 47% in degenerated facets with greater losses of disc space height.[4]
4.1. Limitations
Some limitations of the present study should be acknowledged. Since the total number of samples was not large enough, this study did not differentiate between different segments when discussing degeneration of the lumbar 3-joint complex. However, our study revealed an overall trend. As this was a retrospective study, we did not consider the relationship between symptoms and radiographic degeneration.
5. Conclusion
This study discussed various aspects of degeneration of the lumbar 3-joint complex. We found that the mechanical consequences of disc degeneration, including decreased disc height, increase facet joint degeneration.
Acknowledgments
The authors thank the assistance of Editage in Shanghai, which provided English language editing.
Author contributions
Conceptualization: Min Dai.
Data curation: Quanwei Song, Xuqiang Liu, Qi Lai.
Funding acquisition: Zongmiao Wan.
Investigation: Quanwei Song, De-jian Chen, Benyu Tang.
Methodology: Bin Zhang.
Project administration: Zongmiao Wan.
Software: Benyu Tang.
Supervision: Bin Zhang, Min Dai.
Writing – original draft: Quanwei Song.
Writing – review & editing: Zongmiao Wan.
Footnotes
Abbreviations: CT = computed tomography, MRI = magnetic resonance imaging, OA = osteoarthritis.
How to cite this article: Song Q, Liu X, Chen Dj, Lai Q, Tang B, Zhang B, Dai M, Wan Z. Evaluation of MRI and CT parameters to analyze the correlation between disc and facet joint degeneration in the lumbar three-joint complex. Medicine. 2019;98:40(e17336).
Ethics approval and consent to participate: The study was approved by the Ethics Committee of the First Affiliated Hospital of Nanchang University. Because of the retrospective nature of the study, informed consent was waived.
Consent for publication: Not applicable
Availability of data and materials: The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Funding: This work was supported by the Natural Science Foundation of China (grant numbers 81460341, 81760410); and Educational Department of Jiangxi Province of China (grant numbers GJJ160050) and Youth Science Foundation of Jiangxi Province (grant numbers: 20151BAB215001 and 20171ACB21056 [Key Program]).
The authors have no conflicts of interest to disclose.
References
- [1].Louis R. Spinal stability as defined by the three-column spine concept. Anat Clin 1985;7:33–42. [DOI] [PubMed] [Google Scholar]
- [2].Adams MA, Hutton WC. The mechanical function of the lumbar apophyseal joints. Spine 1983;8:327–30. [DOI] [PubMed] [Google Scholar]
- [3].Putz R. The functional morphology of the superior articular processes of the lumbar vertebrae. J Anat 1985;143:181–7. [PMC free article] [PubMed] [Google Scholar]
- [4].Yang KH, King AI. Mechanism of facet load transmission as a hypothesis for low-back pain. Spine (Phila Pa 1976) 1984;9:557–65. [DOI] [PubMed] [Google Scholar]
- [5].Varlotta GP, Lefkowitz TR, Schweitzer M, et al. The lumbar facet joint: a review of current knowledge: part 1: anatomy, biomechanics, and grading. Skeletal Radiol 2011;40:13–23. [DOI] [PubMed] [Google Scholar]
- [6].Butler D, Trafimow JH, Andersson GB, et al. Discs degenerate before facets. Spine (Phila Pa 1976) 1990;15:111–3. [DOI] [PubMed] [Google Scholar]
- [7].Dunlop RB, Adams MA, Hutton WC. Disc space narrowing and the lumbar facet joints. J Bone Joint Surg Br 1984;66:706–10. [DOI] [PubMed] [Google Scholar]
- [8].Jinkins JR. Acquired degenerative changes of the intervertebral segments at and suprajacent to the lumbosacral junction. A radioanatomic analysis of the nondiscal structures of the spinal column and perispinal soft tissues. Eur J Radiol 2004;50:134–58. [DOI] [PubMed] [Google Scholar]
- [9].Fujiwara A, Tamai K, Yamato M, et al. The relationship between facet joint osteoarthritis and disc degeneration of the lumbar spine: an MRI study. Eur Spine J 1999;8:396–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Eubanks JD, Lee MJ, Cassinelli E, et al. Does lumbar facet arthrosis precede disc degeneration? A postmortem study. Clin Orthop Relat Res 2007;464:184–9. [DOI] [PubMed] [Google Scholar]
- [11].Lewin T. Osteoarthritis in lumbar synovial joints. A morphologic study. Acta Orthop Scand Suppl 1964;Suppl 73:1–12. [DOI] [PubMed] [Google Scholar]
- [12].Videman T, Battie MC, Gill K, et al. Magnetic resonance imaging findings and their relationships in the thoracic and lumbar spine. Insights into the etiopathogenesis of spinal degeneration. Spine (Phila Pa 1976) 1995;20:928–35. [DOI] [PubMed] [Google Scholar]
- [13].Suri P, Miyakoshi A, Hunter DJ, et al. Does lumbar spinal degeneration begin with the anterior structures? A study of the observed epidemiology in a community-based population. BMC Musculoskelet Disord 2011;12:202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Li J, Muehleman C, Abe Y, et al. Prevalence of facet joint degeneration in association with intervertebral joint degeneration in a sample of organ donors. J Orthop Res 2011;29:1267–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kong MH, He W, Hymanson H, et al. 71. Lumbar segmental mobility according to the grade of the disc, the facet joint, the muscle, and the ligament pathology. Spine J 2008;8:37S. [DOI] [PubMed] [Google Scholar]
- [16].Miller JA, Schmatz C, Schultz AB. Lumbar disc degeneration: correlation with age, sex, and spine level in 600 autopsy specimens. Spine 1988;13:173–8. [PubMed] [Google Scholar]
- [17].Weishaupt D, Zanetti M, Boos N, et al. MR imaging and CT in osteoarthritis of the lumbar facet joints. Skeletal Radiol 1999;28:215–9. [DOI] [PubMed] [Google Scholar]
- [18].Pfirrmann CW, Metzdorf A, Zanetti M, et al. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 2001;26:1873–8. [DOI] [PubMed] [Google Scholar]
- [19].Noren R, Trafimow J, Andersson GB, et al. The role of facet joint tropism and facet angle in disc degeneration. Spine (Phila Pa 1976) 1991;16:530–2. [DOI] [PubMed] [Google Scholar]
- [20].Vanharanta H, Floyd T, Ohnmeiss DD, et al. The relationship of facet tropism to degenerative disc disease. Spine (Phila Pa 1976) 1993;18:1000–5. [DOI] [PubMed] [Google Scholar]
- [21].Miyakoshi N, Abe E, Shimada Y, et al. Anterior decompression with single segmental spinal interbody fusion for lumbar burst fracture. Spine (Phila Pa 1976) 1999;24:67–73. [DOI] [PubMed] [Google Scholar]
- [22].Terwee CB, Bot SD, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007;60:34–42. [DOI] [PubMed] [Google Scholar]
- [23].Vernon-Roberts B, Pirie CJ. Degenerative changes in the intervertebral discs of the lumbar spine and their sequelae. Rheumatol Rehabil 1977;16:13–21. [DOI] [PubMed] [Google Scholar]
- [24].Kong MH, He W, Tsai Y, et al. Relationship of facet tropism with degeneration and stability of functional spinal unit. Yonsei Med J 2009;50:624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Dai LY. Orientation and tropism of lumbar facet joints in degenerative spondylolisthesis. Int Orthop 2001;25:40–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Schleich C, Muller-Lutz A, Blum K, et al. Facet tropism and facet joint orientation: risk factors for the development of early biochemical alterations of lumbar intervertebral discs. Osteoarthritis Cartilage 2016;24:1761–8. [DOI] [PubMed] [Google Scholar]
- [27].Mohanty SP, Kanhangad MP, Kamath S, et al. Zygapophyseal joint orientation and facet tropism and their association with lumbar disc prolapse. Asian Spine J 2018;12:902–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Kalichman L, Suri P, Guermazi A, et al. Facet orientation and tropism. Spine 2009;34:E579–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Liu HX, Shen Y, Shang P, et al. Asymmetric facet joint osteoarthritis and its relationships to facet orientation, facet tropism, and ligamentum flavum thickening. Clin Spine Surg 2016;29:394–8. [DOI] [PubMed] [Google Scholar]
- [30].Cyron BM, Hutton WC. Articular tropism and stability of the lumbar spine. Spine 1980;5:168–72. [DOI] [PubMed] [Google Scholar]
- [31].Teichtahl AJ, Urquhart DM, Wang Y, et al. A dose-response relationship between severity of disc degeneration and intervertebral disc height in the lumbosacral spine. Arthritis Res Ther 2015;17:297. [DOI] [PMC free article] [PubMed] [Google Scholar]


