Supplemental Digital Content is available in the text
Keywords: epidemiology, health examination, risk factor, stroke
Abstract
Health examination is an important method for early detection of people with different risk of stroke. This study estimates the risk of stroke and identify risk factors for people who underwent health examinations at the Health Examination Center at West China Hospital, Sichuan University from July 2014 to February 2018.
A total of 31,464 people were recruited in this study and divided into 3 groups (low risk, moderate risk, and high risk) according to risk of stroke. We explored possible factors associated with the risk of stroke by using multivariable stepwise logistic regression analysis.
Among the participants, 17,959 were at low risk, 11,825 were at moderate risk, and 1680 were at high risk. Age, smoking, alcohol consumption, body mass index, uric acid, diastolic pressure, systolic pressure, triglycerides, low-density lipoprotein cholesterol, glucose, and brachial-ankle pulse wave velocity (baPWV) were independent significant risk factors for stroke, whereas high-density lipoprotein cholesterol was an independent protective factor for stroke. Interestingly, with increasing age, the percentage of people at moderate or high risk of stroke was increased. The percentages of people at moderate and high risk of stroke were also increased with respect to the stages of baPWV.
This study showed that >40% of the participants were at moderate or high risk of stroke, especially the older participants. Several factors were related to the risk of stroke, especially baPWV. Some preventive action may be adopted early, and more attention can be paid to the health examination population.
1. Introduction
According to the ‘World Health Organization’ criteria, stroke events are defined as “rapidly developing signs of focal (or global) disturbance of cerebral function lasting >24 hours (unless interrupted by surgery or death) with no apparent nonvascular cause.”[1] Stroke is estimated to be the second leading cause of death and a major cause of serious disability for adults worldwide.[2] The proportion of deaths resulting from stroke is approximately 10% to 12% in Western countries, and 12% of these deaths are people <65 years’ old.[3] Stroke can be generally classified into 2 subgroups, ischemic stroke and hemorrhagic stroke, and in China, 43.7% to 78.9% of all stroke cases were ischemic stroke.[4] Furthermore, in China, the annual stroke mortality rate is approximately 115 per 100,000,[5] exceeding heart disease as the leading cause of adult death and disability. The mortality owing to stroke is about 25% higher than ischemic heart disease in China in 2017. Notably, there are >2 million new stroke cases annually.[5] Currently, Asia, East Europe, and Russia are experiencing the highest rates of mortality and disability-adjusted life years lost as a result of stroke.[6] The consequences of stroke-related disability and death are significant for both society and individuals. Stroke accounts for approximately 2% to 4% of total health care costs in the world, and industrialized countries have shown that >4% of direct health care costs are because of stroke. Because of the burgeoning elderly population in Western societies, stroke-related disability in these societies is estimated to be ranked as the fourth most important cause of disability-adjusted life years by 2030.[7] Similarly, with an increase in the aging population, the disease burden will increase greatly during the next 20 years, especially in developing countries. The lifestyle in China has changed significantly, along with dramatic transformations in social, economic, and environmental conditions, during the last 30 years. The effect of stroke has now caused serious public health problems in China.[8] Therefore, all measures capable of downregulating the incidence rate of stroke and disability are extremely important.
Currently, the prevalence of stroke in China is similar to that in developed countries; for example, the total age-adjusted incidence of first-ever stroke in China (115.61–219 per 100,000 per year) is not significantly different from that in developed countries (130–410 per 100,000 per year).[8] Therefore, paying more attention to people with a high risk of stroke and searching for possible factors underlying the risk of stroke is very important. Early detection, diagnosis, and treatment are essential for the prevention and control of stroke. Thus, regular health examination is an important method for the early detection of people at risk for stroke. In the present study, we performed a health risk assessment of stroke for people who underwent health examinations at West China Hospital, Chengdu, to reveal the distribution characteristics of risk of stroke among the health examination population. We also discussed the factors that are related to the risk of stroke.
2. Methods
2.1. Study population
This study is a retrospective study. From July 2014 to February 2018, a total of 31,464 cases >18 years’ old (17,396 males, 14,068 females) were voluntary, and went to the Health Examination Center at West China Hospital, Sichuan University, for health examination. In the Health Examination Center, the participants did health examination. The following methods were carried out in accordance with the approved guidelines. The corresponding protocol was approved by the Ethics of Research Committee of the West China Hospital of Sichuan University. Written informed consent was obtained from all participants.
2.2. Data collection
All participants completed the questionnaire, physical examination, and laboratory test, and peripheral blood was collected from each subject. Demographic characteristics, including age, sex, marital status, and lifestyle habits (smoking and alcohol consumption) were assessed by trained investigators. Weight was evaluated with a calibrated electronic digital scale, accurate to 100 g, with subjects wearing only light underwear. Height was measured without shoes to the nearest 0.1 cm using a secure portable stadiometer. Body mass index (BMI) was calculated by weight (kilogram)/height2 (square meter) for each participant. Blood pressure (BP) was recorded twice on the right arm with an electronic sphygmomanometer with participants in the sitting position after a 10-minute rest. Serum levels of fasting blood glucose, uric acid (UA), total cholesterol (TC), triglycerides (TGs), low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C) for each individual were detected by an automatic biochemical analyzer (Mindary, BS-820, Shenzhen, China). Brachial-ankle pulse wave velocity (baPWV) was measured by a volume-plethysmographic apparatus (Vasera VS-1000, Fukuda Denshi, Japan). In brief, participants were examined in the supine position after a sufficient sedentary period. A microphone for detecting heart sounds was placed on the left edge of the sternum at the fourth intercostal space. Occlusion and monitoring cuffs were wrapped on both brachial and ankles, and pressure waveforms of the brachial and tibial arteries were collected.[9] Criteria for classification of baPWV were as followings: soft (<1100 cm/s), normal (1100–1400 cm/s), medium hard (1400–1680 cm/s), hard (>1680 cm/s). With respect to ankle-brachial index (ABI), BP was measured in both arms and legs using a manual sphygmomanometer (Welch Allyn Tycos 7670–01, Welch Allyn, Skaneateles Falls, NY) and a portable vascular Doppler (Nicolet n800, Natus Medical Inc., San Carlos, CA) with an 8 MHz probe, following a counterclockwise sequence: right arm, right posterior tibialis, right dorsalis pedis, left posterior tibialis, left dorsalis pedis, and left arm. The ABI was computed by dividing the higher of the posterior tibialis or dorsalis pedis BP in each leg by the higher arm systolic BP (right or left).[10] Classification of ABI was defined as: normal (0.9–1.3), hard (0.8–0.9), mild clogging (0.5–0.8), clogging (<0.5).
The risk of stroke for each participant was determined according to the manufacturer's protocol (Hehe Science And Technology Group Co., Ltd., Hangzhou, China), and there were 3 risk subgroups, including cases with high risk, moderate risk, and low risk. In brief, the calculation of the risk of stroke for each individual included 4 parts: family history, history of present illness, physiological index, and lifestyle. Based on the results of the 4 parts, indices in each part were given with weight/scores. After collecting the total score of all the indices, we divided the risk of stroke for each participant into 3 groups: high risk of stroke (total score >20), moderate risk of stroke (total score between 5 and 20), and low risk of stroke (total score <5). For instance, with respect to family history, there are 8 indices, namely, father with stroke, mother with stroke, (paternal) grandfather with stroke, (paternal) grandmother with stroke, (maternal) grandfather with stroke, (maternal) grandmother with stroke, father with hypertension, and mother with hypertension. If the father of the participant had a stroke, the score was 2.5. Similarly, if the mother of the participant had a stroke, the score was 2.5. Otherwise, the score is 0. In addition, if the grandfathers or grandmothers of the participant had a stroke, the score was 0.5, otherwise, the score was 0. Moreover, if the mother or father of the participant had hypertension, the score was 0.1. In contrast, if the mother or father of the participant was not diagnosed with hypertension, the score was 0. Other indices in each part and how to assign the scores are listed in supplementary Table 1.
2.3. Statistical analysis
All statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC). With respect to the results expressed as the mean ± standard deviation, the statistical significance of the data was determined by analysis of variance analysis. When data were expressed as percentages for categorical variables, the χ2 test and the Cochran-mantel-haenszel test were used to compare categorical variables. Multivariable logistic regression analysis was used to identify the factors related to risk of stroke (risk of stroke as a dependent variable and sex, age, smoking status, alcohol consumption status, BMI, systolic pressure, diastolic pressure, glucose, UA, TC, TGs, HDL-C, LDL-C, baPWV, and ABI as independent variables). The odds ratio (OR) and its 95% confidence interval (CI) were presented to show the risks. Significance was indicated by a P value <.05.
3. Results
3.1. Characteristics of recruited participants
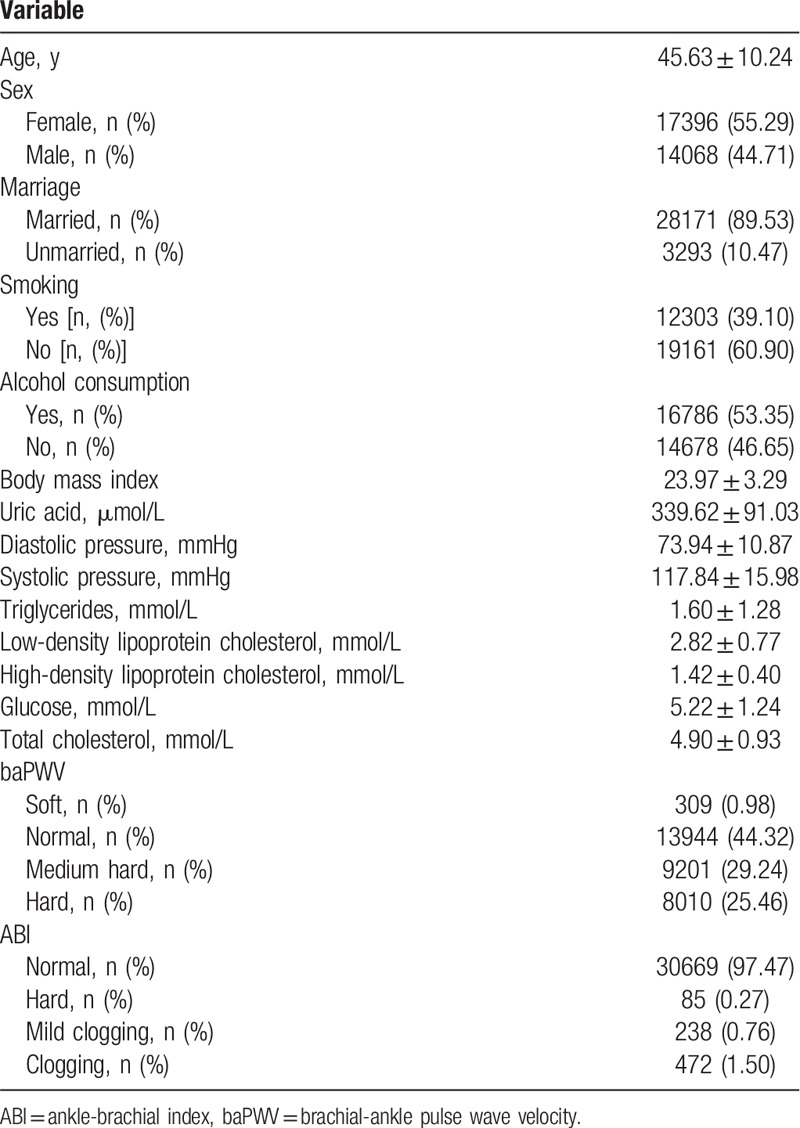
The general characteristics and possible risk factors for stroke in the study population are presented in Table 1. With respect to baPWV stages, 309 cases were soft, 13,944 were normal, 9201 were medium hard, and 8010 were hard; 30,669 cases were normal with respect to ABI stages, 85 were hard, 238 were mild clogging, and 472 were clogging.
Table 1.
Characteristics of recruited participants.
3.2. Comparison of possible risk factors in people at different stages of stroke susceptibility
In the present study, the mean age of people with low risk was 43.18 ± 10.07 years, people with moderate risk was 48.69 ± 9.61 years, and people with high risk was 50.35 ± 8.79 years. The results showed that there was a significant difference in age among the 3 groups (P < .001) (Table 2). To further elucidate the correlation between age and risk of stroke, we divided the participants into 7 groups by age (group 1: 18–20 years, group 2: 21–30 years, group 3: 31–40 years, group 4: 41–50 years, group 5: 51–60 years, group 6: 61–70 years, group 7: 71–80 years). The number (percentage) of people at different stages of stroke susceptibility in different age groups is listed in Table 3 and Figure 1. We found that the percentage of people with moderate or high risk was increased with increasing age. These data suggest that age is related to the risk of stroke and that older age may positively correlate with moderate or high risk. With respect to sex, the percentage of males at low risk was higher than that of females, whereas the percentage of females at moderate or high risk was higher than that of males, suggesting that female sex may positively correlate with moderate and high risk of stroke (Table 2). Similarly, we found that the percentage of people who consumed alcohol at moderate or high risk was higher than that of people who did not consume alcohol (Table 2). The percentage of people who smoked at moderate or high risk was higher than that of people who did not smoke, suggesting that smoking may positively correlate with the risk of stroke. In addition, we discussed other parameters that may correlate with the risk of stroke, including body mass index (BMI), systolic pressure, diastolic pressure, UA, TC, TGs, LDL-C, HDL-C, and glucose. The results showed that people at high risk had higher BMI, systolic pressure, diastolic pressure, UA, TC, TGs, LDL-C, and glucose compared with people at low risk overall (Table 2). People with high risk had lower HDL-C than people with low risk.
Table 2.
Comparison of possible risk factors in different stages of stroke susceptibility.
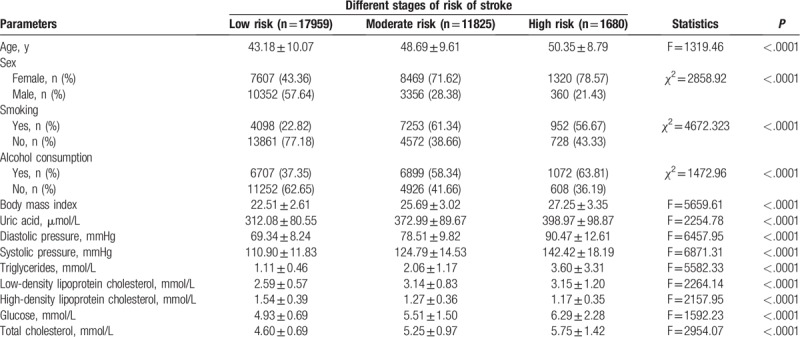
Table 3.
Comparison of different age groups at different stages of stroke susceptibility.
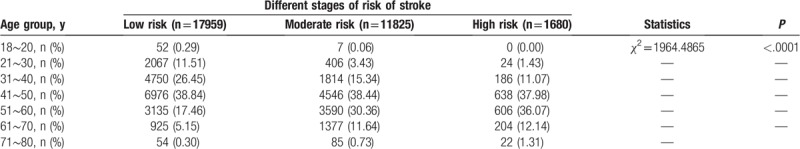
Figure 1.
Percentage of people in different stages of stroke in different age groups. Group 1: 18-20 years, group 2: 21–30 years, group 3: 31–40 years, group 4: 41–50 years, group 5: 51–60 years, group 6: 61–70 years, group 7: 71–80 years.
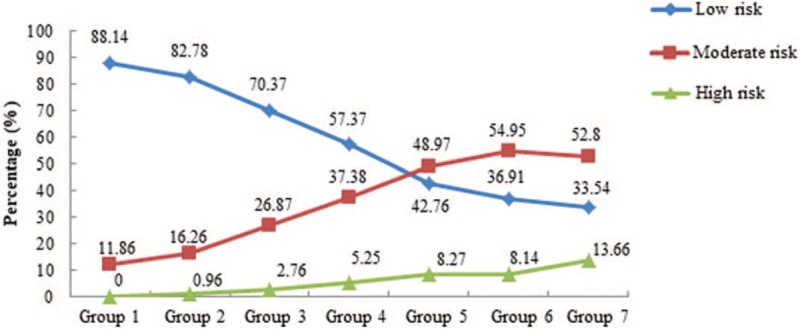
baPWV and ABI have been used as valuable indices of arterial stiffness and as surrogate markers for atherosclerosis. In this study, we discussed the relationship between baPWV and ABI and the risk of stroke. We found that people with a low or moderate risk of stroke showed a higher percentage of soft, normal baPWV compared with that of people with a high risk of stroke (Table 4, Fig. 2). Interestingly, people with a low risk of stroke showed a decreasing percentage of baPWV from soft to hard, whereas people with a moderate risk of stroke showed an increasing percentage of baPWV from soft to hard. With respect to ABI, people with a low risk of stroke showed an increasing percentage of ABI from normal to clogging, whereas people with a moderate risk of stroke showed a decreasing percentage of ABI from normal to clogging overall (Table 5, Fig. 3). These data indicated that people with a higher risk of stroke had a poorer vascular state, including the indices baPWV and ABI.
Table 4.
Comparison of different baPWV statuses at different stages of stroke susceptibility.
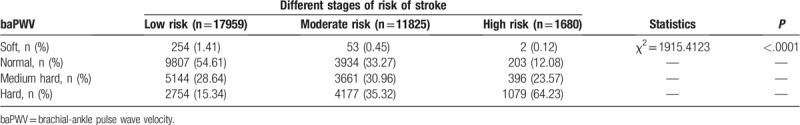
Figure 2.
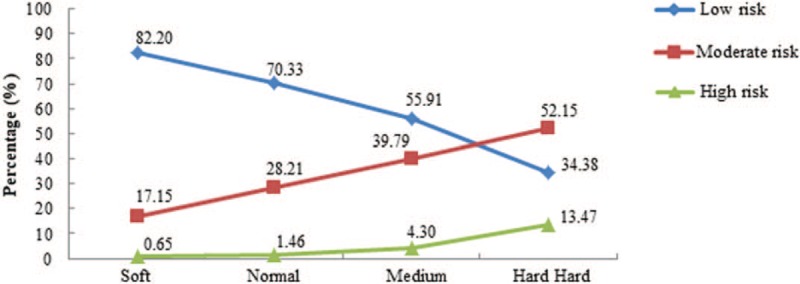
Percentage of people in different stages of stroke with different brachial-ankle pulse wave velocity statuses.
Table 5.
Comparison of different ABI statuses at different stages of stroke susceptibility.
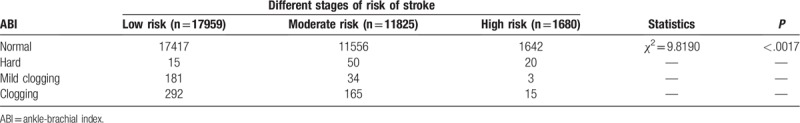
Figure 3.
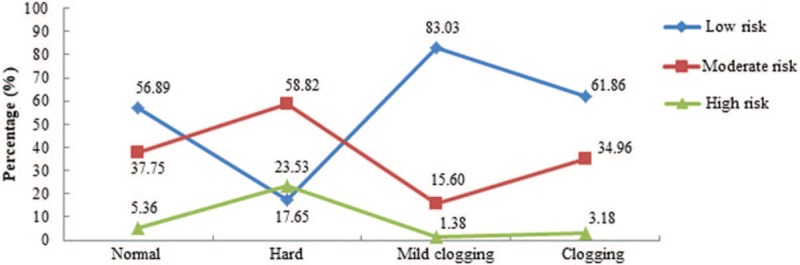
Percentage of people in different stages of stroke with different ankle-brachial index statuses.
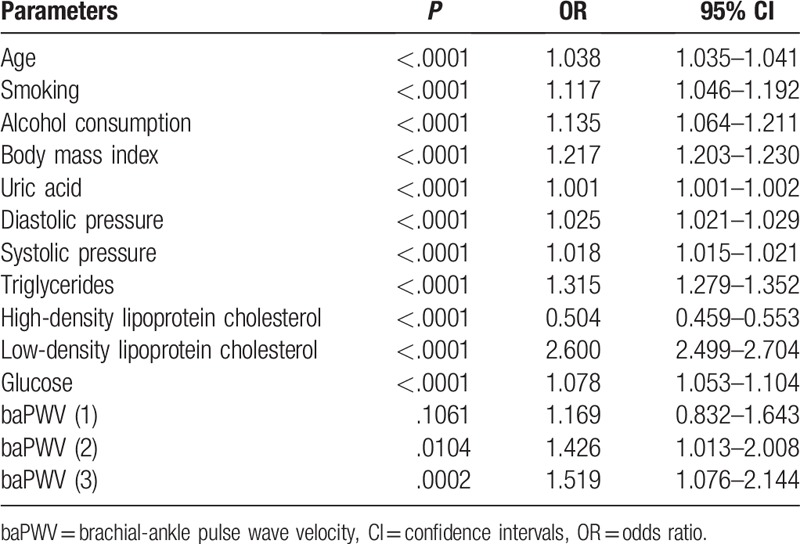
3.3. Independent risk factors for stroke susceptibility by logistic analysis
To clearly elucidate the association between possible risk factors and stroke risk, multivariable stepwise logistic regression analysis was used to identify the factors related to risk of stroke. Methods to define dumb variables (stages of risk of stroke) and how to assign variables are listed in supplementary Table 2. The results showed that age, smoking, alcohol consumption, systolic pressure, diastolic pressure, glucose, BMI, UA, TGs, LDL-C, and baPWV were independent risk factors for stroke, whereas HDL-C was an independent protective factor for stroke risk (Table 6).
Table 6.
Multivariate stepwise logistic regression analysis for risk factors related to stroke.
4. Discussion
Hypertension is recognized as a risk factor for stroke. In a national hypertension survey in China, a 10% increase in the prevalence of hypertension correlated with a 2.80-fold higher incidence of and 2.68-fold higher mortality from stroke.[11] In a study from the United Kingdom, an increase of 10 mmHg in systolic pressure showed a relative hazard ratio (HR) of 1.22 for stroke.[12] Similarly, a study focused on Asian populations reported an increase of 10 mmHg in systolic pressure related to an HR of 3.4 for stroke.[13] In our study, both diastolic pressure and systolic pressure were significantly correlated with the risk of stroke. People with a higher risk of stroke showed higher diastolic pressure and systolic pressure, suggesting that people who show relatively high blood pressure during a health examination should be aware of stroke. Notably, 2 national hypertension surveys in China revealed that the treatment rates for hypertensive patients were 28.2%,[14] and 20.3%.[15] More than 28.8% of treated hypertensive patients had uncontrolled blood pressure.[16] Moreover, the ratio of controlled to treated individuals was 1:4.2.[15] Therefore, numerous hypertensive patients in China are either uncontrolled or untreated and are likely to suffer a stroke.
A previous study showed that diabetes mellitus, BMI, hyperlipidemia, smoking, and alcohol consumption are risk factors for stroke because the economy and society have significantly improved in China in recent years.[17] First, with transportation and exchanges becoming increasingly convenient, there has been a reduced intake of marine fish food but an increased intake of poultry food. Second, a high-salt diet and low intake of fruits and vegetables are common in China.[18–20] Third, the number of people engaged in manual labor was reduced, although the same labor intensity has been maintained because of changes in industrial structure.[20] In addition, unplanned urbanization and air pollution caused by industrialization play an important environmental role.[20,21] These risk factors were partly confirmed by other investigators and our findings.[22] For instance, aberrant glucose regulation, including diabetes and impaired fasting glucose, is recognized as an important risk factor for the occurrence and recurrence of ischemic stroke in Europe and America.[23,24] In the present study, we found that people with a higher risk of stroke revealed a higher percentage of smoking, alcohol consumption, increased BMI, TC, TGs, LDL-C, and glucose, and reduced HDL-C levels compared with people with a relatively low risk of stroke. After stepwise logistic analysis, smoking, alcohol consumption, BMI, TGs, LDL-C, and glucose were confirmed to be independent risk factors for stroke, whereas HDL-C was an independent protective factor for stroke risk.
Serum UA (SUA) is a final enzymatic product of purine metabolism. The criterion for a diagnosis of hyperuricemia is generally defined as SUA concentration >6.8 mg/dL.[25] A meta-analysis with a large sample size showed that hyperuricemia was positively associated with risk of stroke incidence and mortality.[26] This result was in agreement with our findings showing that people with a higher risk of stroke had higher levels of SUA compared with people with a low risk of stroke. Several studies indicated that hyperuricemia correlated with endothelial dysfunction, increased oxidative stress, and thrombus formation and that increased circulating levels of systemic inflammatory mediators may lead to an increased risk of stroke.[26,27]
Available epidemiological studies from China revealed that the rate of stroke incidence increases with age. The highest rate in different age groups was observed in people older than 75 years and was 30 times higher than that reported in the 350- to 44-year age group.[28] Interestingly, the prevalence of stroke will be markedly increased all over the world in the years ahead as the global population older than 65 years increases by approximately 9 million people every year.[29] In the present study, people with a higher risk of stroke were older, and the percentage of people with a high risk increased as age increased. Women are suggested to have an increased risk of dying of stroke compared with men.[30] This finding may be related to several reasons. The life expectancy in females is higher than in males, and females were more likely to live alone.[31,32] Older women were more likely to neglect stroke warning signs and delay emergent management.[33] In addition, risk factors for stroke, such as diabetes and dyslipidemia, were likely to adversely affect women,[34–36] and women suffered more frequently from atrial fibrillation and hypertension.[31,32] Furthermore, a lack of protective effects from estrogen may be a probable explanation for stroke death in postmenopausal women.[37] In this study, we found that females showed a higher percentage of moderate and high risk of stroke than males, suggesting that the government should pay increased attention to women, especially older women with a high risk of stroke.
Pulse wave velocity is an index of arterial stiffness and has been used for noninvasive evaluation of subclinical atherosclerotic changes.[38] baPWV, a type of pulse wave velocity, is a promising test method for evaluating the stiffness of both aortic and peripheral arteries.[39] It not only reflects early atherosclerotic changes[40–42] but also serves as a valuable predictor of mortality due to cardiocerebrovascular events.[43] In a study discussing the potential association between baPWV and metabolic syndrome (MetS) in a Chinese community population,[44] 1271 subjects had MetS out of 5181 study participants; MetS was significantly associated with baPWV (OR: 2.74; 95% CI: 2.28–3.30), and this association strengthened with increasing numbers of MetS components. Similarly, Wang et al discussed the association between baPWV and long-term blood pressure variability (BPV), showing that increased baPWV was accompanied by increased BPV and that baPWV was positively correlated with long-term BPV.[45] In our study, we found that the percentage of people with low risk of stroke was decreased from soft to hard with respect to baPWV, whereas the percentages of people with moderate and high risk were increasing, suggesting that the higher the risk of stroke, the higher the percentage of poor baPWV results. ABI, a simple noninvasive marker of atherosclerosis, is a stroke predictor in addition to the established risk factors that are part of the Framingham risk score.[9] Gronewold et al revealed that 4299 subjects without previous stroke, coronary heart disease, or myocardial infarction were followed up for ischemic and hemorrhagic stroke events during 109.0 ± 23.3 months and found that 104 incident strokes occurred. Subjects suffering stroke had significantly lower ABI values at baseline than the remaining subjects, and ABI predicted stroke in the general population, especially in subjects with classical risk factors, where ABI identified subjects at particularly high stroke risk.[46] This result was similar to our findings, where we found a decreasing percentage of people with moderate or high risk of stroke with respect to ABI from normal to clogging, suggesting that increased risk of stroke was negatively related to ABI.
There were some limitations in this study. First, some data that may correlate with stroke risk were not collected, such as educational level. Second, this study evaluated participants at different stages of stroke risk but did not follow-up the participants, especially participants with a high risk of stroke. Therefore, it is necessary to follow-up the participants in the future and possibly take some preventive actions. Although this study had some deficiencies, it had a large sample size, and the results were credible. In addition, the results indicate that participants of different ages and sex may have different stages of stroke risk and that the participants can understand their susceptibility to stroke.
In conclusion, the present study showed that several factors were related to the risk of stroke, especially baPWV. Therefore, surveillance of these factors may be used in health examination populations, especially older people with a high risk of stroke.
Author contributions
Conceptualization: Huairong Tang.
Formal analysis: Wang-Dong Xu.
Funding acquisition: Huairong Tang.
Investigation: Ya-Li Lei, Wen-Xia Huang.
Methodology: Ya-Li Lei.
Software: Ting Bao.
Validation: Han-Wei Yang.
Writing – original draft: Rui-Cen Li, Huairong Tang.
Writing – review & editing: Rui-Cen Li, Huairong Tang.
Supplementary Material
Footnotes
Abbreviations: ABI = ankle-brachial index, baPWV = brachial-ankle pulse wave velocity, BMI = body mass index, BP = blood pressure, HDL-C = high-density lipoprotein cholesterol, LDL-C = low-density lipoprotein cholesterol, TC = total cholesterol, TGs = triglycerides, UA = uric acid.
How to cite this article: Li RC, Xu WD, Lei YL, Bao T, Yang HW, Huang WX, Tang HR. The risk of stroke and associated risk factors in a health examination population. Medicine. 2019;98:40(e17218).
Availability of data and supporting materials: The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
This work was partly supported by grants from the National Key Research & Development Program of China (2017YFC0907504), Sichuan Provincial Science and Technology Project (2018SZ0261), and Sichuan Provincial Cadre Health Care Research Project (2017–119).
The authors report no conflicts of interest.
Supplemental Digital Content is available for this article.
References
- [1].Hatano S. Experience from a multicentre stroke register: a preliminary report. Bull World Health Organ 1976;54:541–3. [PMC free article] [PubMed] [Google Scholar]
- [2].Kim AS, Cahill E, Cheng NT. Global stroke belt: geographic variation in stroke burden worldwide. Stroke 2015;46:3564–70. [DOI] [PubMed] [Google Scholar]
- [3].Feigin VL, Forouzanfar MH, Krishnamurthi R, et al. Global and regional burden of stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet 2014;383:245–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Wu L, Shen Y, Liu X, et al. The 1425G/A SNP in PRKCH is associated with ischemic stroke and cerebral hemorrhage in a Chinese population. Stroke 2009;40:2973–6. [DOI] [PubMed] [Google Scholar]
- [5].Wu S, Wu B, Liu M, et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol 2019;18:394–405. [DOI] [PubMed] [Google Scholar]
- [6].Kim AS, Johnston SC. Global variation in the relative burden of stroke and ischemic heart disease. Circulation 2011;124:314–23. [DOI] [PubMed] [Google Scholar]
- [7].Norrving B, Kissela B. The global burden of stroke and need for a continuum of care. Neurology 2013;80:S5–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Wu L, Wang A, Wang X, et al. Factors for short-term outcomes in patients with a minor stroke: results from China National Stroke Registry. BMC Neurol 2015;15:253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Munakata M. Brachial-ankle pulse wave velocity in the measurement of arterial stiffness: recent evidence and clinical applications. Curr Hypertens Rev 2014;10:49–57. [DOI] [PubMed] [Google Scholar]
- [10].Del Brutto OH, Sedler MJ, Mera RM, et al. The association of ankle-brachial index with silent cerebral small vessel disease: results of the Atahualpa Project. Int J Stroke 2015;10:589–93. [DOI] [PubMed] [Google Scholar]
- [11].He J, Klag MJ, Wu Z, et al. Stroke in the People's Republic of China. II. Meta-analysis of hypertension and risk of stroke. Stroke 1995;26:2228–32. [PubMed] [Google Scholar]
- [12].Staessen JA, Gasowski J, Wang JG, et al. Risks of untreated and treated isolated systolic hypertension in the elderly: meta-analysis of outcome trials. Lancet 2000;355:865–72. [DOI] [PubMed] [Google Scholar]
- [13].Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003;42:1206–52. [DOI] [PubMed] [Google Scholar]
- [14].Gu D, Reynolds K, Wu X, et al. Prevalence, awareness, treatment, and control of hypertension in china. Hypertension 2002;40:920–7. [DOI] [PubMed] [Google Scholar]
- [15].Wu Y, Huxley R, Li L, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation 2008;118:2679–86. [DOI] [PubMed] [Google Scholar]
- [16].Yong H, Foody J, Linong J, et al. A systematic literature review of risk factors for stroke in China. Cardiol Rev 2013;21:77–93. [DOI] [PubMed] [Google Scholar]
- [17].Hankey GJ. Stroke. Lancet 2017;389:641–54. [DOI] [PubMed] [Google Scholar]
- [18].Tomonari T, Fukuda M, Miura T, et al. Is salt intake an independent risk factor of stroke mortality? Demographic analysis by regions in Japan. J Am Soc Hypertens 2011;5:456–62. [DOI] [PubMed] [Google Scholar]
- [19].Sharma S, Cruickshank JK, Green DM, et al. Impact of diet on mortality from stroke: results from the U.S. multiethnic cohort study. J Am Coll Nutr 2013;32:151–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Yang G, Wang Y, Zeng Y, et al. Rapid health transition in China, 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet 2013;381:1987–2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Chen R, Zhang Y, Yang C, et al. Acute effect of ambient air pollution on stroke mortality in the China air pollution and health effects study. Stroke 2013;44:954–60. [DOI] [PubMed] [Google Scholar]
- [22].Wu X, Zhu B, Fu L, et al. Prevalence, incidence, and mortality of stroke in the chinese island populations: a systematic review. PLoS One 2013;8:e78629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Rutten-Jacobs LC, Keurlings PA, Arntz RM, et al. High incidence of diabetes after stroke in young adults and risk of recurrent vascular events: the FUTURE study. PLoS One 2014;9:e87171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Avezum Á, Costa-Filho FF, Pieri A, et al. Stroke in Latin America: burden of disease and opportunities for prevention. Glob Heart 2015;10:323–31. [DOI] [PubMed] [Google Scholar]
- [25].Hu J, Peng C, Li J, et al. Serum Bisphenol A is an independent risk factor of hyperuricemia: A 6-year prospective study. Semin Arthritis Rheum 2019;48:644–8. [DOI] [PubMed] [Google Scholar]
- [26].Li M, Hou W, Zhang X, et al. Hyperuricemia and risk of stroke: a systematic review and meta-analysis of prospective studies. Atherosclerosis 2014;232:265–70. [DOI] [PubMed] [Google Scholar]
- [27].Chao TF, Liu CJ, Chen SJ, et al. Hyperuricemia and the risk of ischemic stroke in patients with atrial fibrillation--could it refine clinical risk stratification in AF? Int J Cardiol 2014;170:344–9. [DOI] [PubMed] [Google Scholar]
- [28].Sun H, Zou X, Liu L. Epidemiological factors of stroke: a survey of the current status in china. J Stroke 2013;15:109–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].World Health Organization. World Health Report 2004: Changing History. Geneva, Switzerland: World Health Organization; 2004. [Google Scholar]
- [30].Zhou G, Nie S, Dai L, et al. Sex differences in stroke case fatality: a meta-analysis. Acta Neurol Scand 2013;128:1–8. [DOI] [PubMed] [Google Scholar]
- [31].Laditka JN, Laditka SB. Stroke and active life expectancy in the United States, 1999–2009. Disabil Health J 2014;7:472–7. [DOI] [PubMed] [Google Scholar]
- [32].Keteepe-Arachi T, Sharma S. Preventing stroke and assessing risk in women. Practitioner 2017;261:13–37. [PubMed] [Google Scholar]
- [33].Lindley RI. Stroke prevention in the very elderly. Stroke 2018;49:796–802. [DOI] [PubMed] [Google Scholar]
- [34].Wagstaff AJ, Overvad TF, Lip GY, et al. Is female sex a risk factor for stroke and thromboembolism in patients with atrial fibrillation? A systematic review and meta-analysis. QJM 2014;107:955–67. [DOI] [PubMed] [Google Scholar]
- [35].Niwa Y, Ishikawa S, Gotoh T, et al. Association between stroke and metabolic syndrome in a Japanese population: Jichi Medical School (JMS) Cohort Study. J Epidemiol 2010;20:62–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Bushnell CD, Jamison M, James AH. Migraines during pregnancy linked to stroke and vascular diseases: US population based case-control study. BMJ 2009;338:b664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Alonso de Leciñana M, Egido JA, Fernández C, et al. Risk of ischemic stroke and lifetime estrogen exposure. Neurology 2007;68:33–8. [DOI] [PubMed] [Google Scholar]
- [38].Katsuda S, Takazawa K, Miyake M, et al. Local pulse wave velocity directly reflects increased arterial stiffness in a restricted aortic region with progression of atherosclerotic lesions. Hypertens Res 2014;37:892–900. [DOI] [PubMed] [Google Scholar]
- [39].Yang Y, Fan F, Kou M, et al. Brachial-ankle pulse wave velocity is associated with the risk of new carotid plaque formation: data from a Chinese community-based Cohort. Sci Rep 2018;8:7037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Weng C, Yuan H, Tang X, et al. Age- and gender dependent association between components of metabolic syndrome and subclinical arterial stiffness in a Chinese population. Int J Med Sci 2012;9:730–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Scuteri A, Cunha PG, Rosei EA, et al. Arterial stiffness and influences of the metabolic syndrome: a cross-countries study. Atherosclerosis 2014;233:654–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Weng C, Yuan H, Yang K, et al. Gender-specific association between the metabolic syndrome and arterial stiffness in 8,300 subjects. Am J Med Sci 2013;346:289–94. [DOI] [PubMed] [Google Scholar]
- [43].Lu YC, Lyu P, Zhu HY, et al. Brachial-ankle pulse wave velocity compared with mean arterial pressure and pulse pressure in risk stratification in a Chinese population. J Hypertens 2018;36:528–36. [DOI] [PubMed] [Google Scholar]
- [44].Wang A, Su Z, Liu X, et al. Brachial-ankle pulse wave velocity and metabolic syndrome in general population: the APAC study. BMC Cardiovasc Disord 2016;16:228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Wang Y, Yang Y, Wang A, et al. Association of long-term blood pressure variability and brachial-ankle pulse wave velocity: a retrospective study from the APAC cohort. Sci Rep 2016;6:21303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Gronewold J, Hermann DM, Lehmann N, et al. Ankle-brachial index predicts stroke in the general population in addition to classical risk factors. Atherosclerosis 2014;233:545–50. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


