Abstract
Although all-ceramic crowns have excellent biocompatibility and esthetic appearance, chipping may occur. The mechanical properties of monolithic zirconia restorative material are superior to those of all-ceramic restorative materials, and chipping caused by chewing hard foods could be avoided. This study aimed to evaluate the clinical efficacy of monolithic zirconia crowns for posterior teeth restorations.
A total of 46 patients requiring posterior teeth restorations involving 49 teeth were treated with monolithic zirconia crown procedure. The treatment results were evaluated according to the modified California Dental Association criteria immediately after the procedure, and at 2, 24, 48, and 96 weeks after the procedure. The plaque index, gingival index, probing depth, crown marginal integrity, and attrition of the abutment teeth, antagonist teeth, corresponding contralateral teeth, and antagonist of the corresponding contralateral teeth were assessed. The patients were followed for up to 96 weeks.
The marginal adaptation results of all 46 patients were evaluated as excellent, resulting in an excellent rate of 100%. Regarding the crown color match, only 3 cases (6.1%) were evaluated as acceptable. Marginal adaptation, anatomic form, crown margin integrity, color match, and gross fracture did not show significant differences compared with the different time points (P = .999). Surface texture at different time did not change significantly (P = .807). During the 96-week follow-up, 1 crack in the antagonist teeth was found in 1 patient. There were no significant differences in wear of the antagonist teeth at different time points (P = .972). The rate of “excellent” evaluation for crown restorations was 93.9% to 100%.
The monolithic zirconia crown had no detectable adverse effects on the periodontal tissues, and the antagonist teeth attrition was small. Therefore, it has good potential in the clinical application of posterior teeth restorations in the short term.
Keywords: attrition, clinical efficacy, monolithic zirconia crowns, posterior teeth, restorations
1. Introduction
The all-ceramic crown is a common restoration method for a broken or cracked tooth.[1] Compared with the metal crown and the metal-ceramic crown, it has excellent biocompatibility and esthetic appearance, compatibility with magnetic resonance imaging, and superior refractive index and transparency.[1,2] At present, the materials used in all-ceramic crowns mainly include glass-infiltrated alumina-based ceramics, glass ceramics by injection molding, and yttria-stabilized tetragonal zirconia polycrystals (Y-TZP).[1] Among these, Y-TZP has a flexural strength of 900 to 1200 MPa and a fracture toughness of 7 to 9 MPa m1/2,[3–5] which are 2 to 3 times those of the alumina-based all-ceramic materials.[6] Its advantageous mechanical properties make it the most popular all-ceramic restoration material.
Although Y-TZP ceramics exhibit low-temperature degradation when exposed to low temperature or hydrothermal environment for a long time, resulting in increased surface roughness and a decreased failure load, its flexural strength is still enough to withstand chewing forces applied to the posterior region.[7] The addition of a stabilizer with Y2O3 as the main component in the zirconia preparation can significantly improve its antiaging properties and enhance its biological and mechanical properties.[8]
Clinically, the veneering porcelain has been found to chip or even delaminate after long-term wear of the crown, resulting in restoration failures.[9] This problem was resolved by gradually introducing the monolithic zirconia crown into clinical practice. The monolithic zirconia crown restoration is fabricated with computer-aided design and computer-aided manufacturing (CAD/CAM) technique with the removal of veneering porcelain. It is made from a single piece of monolithic zirconium oxide ceramic ingot by computer numerical controlled cutting and sintering. The fabricated crowns have high flexural strength and high fracture toughness, both of which are remarkably better than those of the alumina-based ceramic crowns.[10] The mechanical properties of monolithic zirconia restorative material are notably superior to those of other all-ceramic restorative materials, as the risk of chipping of porcelain veneers caused by chewing hard foods can be avoided.[11] Besides, the monolithic zirconia crown restoration requires a less amount of tooth structure trimming compared with the all-ceramic crown,[11] retaining a more natural tooth structure.
With the rapid development of material science and manufacturing techniques, high-translucent Y-TZP ceramics with high purity and nearly zero porosity can be prepared nowadays, overcoming the shortcomings of poor translucency and single-layer appearance of earlier zirconia ceramics.[12] The Zenostar zirconia system from Wieland Dental has outstanding optical and mechanical properties, as well as high translucency and profound resistance to hydrothermal aging; it also provides a broad range of vital shades for esthetic restorations.[13]
Only a few clinical studies have reported on the periodontal conditions and the therapeutic effects of the restorations on the abutment and the antagonist teeth after the monolithic zirconia crowns were placed in patients.[14–16] The aim of this study was to examine the aforementioned indicators at various time points after restorations using full zirconia crowns with respect to the antagonist teeth and the corresponding contralateral teeth. The results should provide a theoretical basis for the clinical application of the monolithic zirconia crown.
2. Materials and methods
2.1. General information
A total of 46 patients (23 males and 23 females) were admitted to the Second Affiliated Hospital of Guilin Medical University and Guilin Stomatological Hospital from January 2016 to May 2016 and needed full-crown restorations for the first and/or second molars. The age of the patients was 20 to 63 years, with an average age of 41.3 years. A total of 49 teeth, including 16 maxillary first molars, 8 maxillary second molars, 17 mandibular first molars, and 8 mandibular second molars, needed monolithic zirconia crown restorations.
The inclusion criteria were: no history of temporomandibular joint disorder or sleep bruxism; the antagonist teeth were natural teeth with normal occlusion and no large filling; the corresponding contralateral teeth were natural teeth without large fillings or crown restorations; patients with acute and chronic pulpitis or periapical periodontitis had completed root canal treatments before crown restoration; X-ray demonstrated no apparent continuous alveolar bone absorption at the apex and no fistula; and patients had no percussion pain. Patients with acute or chronic periodontitis were excluded. The included patients had good periodontal conditions, the target teeth were not loose, and the patients maintained good oral hygiene.
Informed consent was obtained from all subjects, and the study was approved by the Second Affiliated Hospital of Guilin Medical University and Guilin Stomatological Hospital ethics committee.
2.2. Materials and equipment
The zirconia Zenostar Zr Translucent, the milling machine, and the zirconium oxide sintering furnace were all from Wieland Dental, Germany (Lot No.: U17078). The D700 3D Scanner and the Dental System for CAD/CAM design and manufacturing were from 3Shape, Denmark. The RelyX U100 resin cement in the Clicker Dispenser (Lot No.: K182093) was from 3 M Company, Minnesota. The dental diamond burs were from MANI Inc., Japan. The RA322 Polishing Set was from EVE Ernst Vetter GmbH, Germany. The Silagum Putty Soft and Silagum Light silicone impression materials were from DMG, Germany (Lot No.: C367656863).
According to the principles of full-crown preparation,[14] the occlusal surface of the target tooth was trimmed 1.5 to 2.0 mm in thickness and the other axial surfaces were trimmed 1.0 to 1.5 mm, with axial wall taper degrees of 6 to 8 degrees. The 360 degree gingival shoulder was shallow concave-shaped with a slope. After preparing the tooth, the routine gingival retraction, impression, and cast were conducted. The crown shade was selected according to the patient's choice and the color of the surrounding teeth. The teeth model was sent to the technician center for dental crown fabrication, which involved scanning, cutting, grinding to desired contours, and then coloring, sintering, and polishing. In the second visit, the crown was placed over the abutment. The anatomical shape, marginal adaptation, color match, contact with the surrounding teeth, and occlusion with the antagonist teeth were all carefully examined. If adjustments were made, then the crown was polished again strictly following the polishing procedure, which involved a thorough polishing from coarse to fine to reduce surface roughness. Resin cement was used to fix the crown in place after satisfactory trial wear. The patients were instructed to avoid chewing hard objects, maintain good oral hygiene, and revisit the clinic for follow-up as scheduled.
2.3. Efficacy evaluation
According to the modified California Dental Association (CDA) criteria,[17,18] the patients were reviewed immediately after restoration and at 2, 24, 48, and 96 weeks after the procedure. During each review, the restoration results were examined, evaluated, and assigned 1 of the 3 grades, A, B, and C representing excellent, acceptable, and unacceptable, respectively, which was considered a treatment failure. The periodontal parameters of the abutment teeth, antagonist teeth, corresponding contralateral teeth, and antagonist teeth of the corresponding contralateral teeth were described by the plaque index (PLI), gingival index (GI),[19] and probing depth (PD). The wear of the full-contour zirconia crown and the antagonist teeth were measured by attrition grade.[20] The anatomic form, surface texture, and gross fracture were also evaluated.
For PLI, the Silness and Löe criteria were adopted, and the thickness and amount of plaque were recorded and rated on a scale of 0 to 3, with 0 indicating no plaque on the free gingival margin, 1 indicating a small amount of plaque that can be seen using probe, 2 indicating moderate plaque on the gingival margin and/or adjacent tooth surface, and 3 indicating a large amount of plaque on the gingival margin and/or pocket.
For GI, a periodontal probe was inserted 1 mm below the gingival margin and gently slid along the margin to observe the gingival bleeding. The result was scored on a scale of 3, with 0 indicating healthy gingiva; 1 indicating mild inflammation of gingiva and no bleeding on probing; 2 indicating moderate inflammation of gingiva with redness, edema, and glazing, with bleeding on probing; and 3 indicating severe inflammation of gingiva, marked redness, hypertrophy, and/or ulceration, with a tendency to spontaneous bleeding.
For PD, the depths of the gingival margin of the abutment teeth to the base of the pocket at 6 gingival sites (mesiobuccal, mid-buccal, distobuccal, mesiolingual, mid-lingual, and distolingual) were measured. The average value was the result scored on a scale of 3, with 0 indicating healthy gingiva, with a PD of <3 mm; 1 indicating mild gingivitis, with a PD of ≤3 mm; 2 indicating early periodontal disease, with a PD of 4–5 mm; and 3 indicating moderate and advanced periodontal disease, with a pocket depth of >6 mm.
The attrition grades were defined as follows: Grade 0, no enamel wear and no damage to the occlusal surface; Grade 1, only enamel wear and changes in occlusal surface morphology; Grade 2, mild dentin wear, exposure of occlusal dentine with an area of ≤2 mm2, and decreased crown height due to morphological change in the occlusal surface; Grade 3, severe dentine wear, exposure of occlusal dentine with an area of >2 mm2, partial or total loss of occlusal surface morphology, and loss of crown height; Grade 4: secondary dentine wear (pulp exposure).
The PLI, GI, and PD of the abutment teeth, antagonist teeth, and corresponding contralateral teeth were graded and recorded, and the results were analyzed. The crown margin integrity was evaluated at each follow-up by clinical examinations, photographing of the occlusal surface, and careful examination of the plasters; crown fracture, crack, or tooth defect, if any, were recorded. All clinical examinations and evaluations were performed by the same 4 independent attending dentists with >10 years of clinical work experience.
2.4. Statistical analysis
The data were analyzed using SPSS 22.0 (IBM, Armonk, NY). The clinical indexes and attrition at various follow-up time points were comparatively analyzed by the composition ratio and Wilcoxon rank-sum test.
3. Results
The 46 patients included in the study were all successfully followed for 96 weeks (Figs. 1–6). The results of examination and evaluations are shown in Tables 1–3. The marginal adaptation results of all 46 patients were evaluated as excellent, resulting in an excellent rate of 100%. Regarding the crown color match, only 3 cases (6.1%) were evaluated as acceptable and all the others were excellent during follow-up. No marginal discoloration, secondary caries, or gross fracture was found; therefore, all cases (100%) were evaluated as excellent for this parameter.
Figure 1.

The degree of attrition of antagonist teeth #16 was level 1 at 24 weeks.
Figure 6.

The degree of gingival index of monolithic zirconia crown #26 was level 1 at 48 weeks, with bleeding on probing.
Table 1.
Evaluation of clinical effects of restorations (based on the modified CDA criteria).
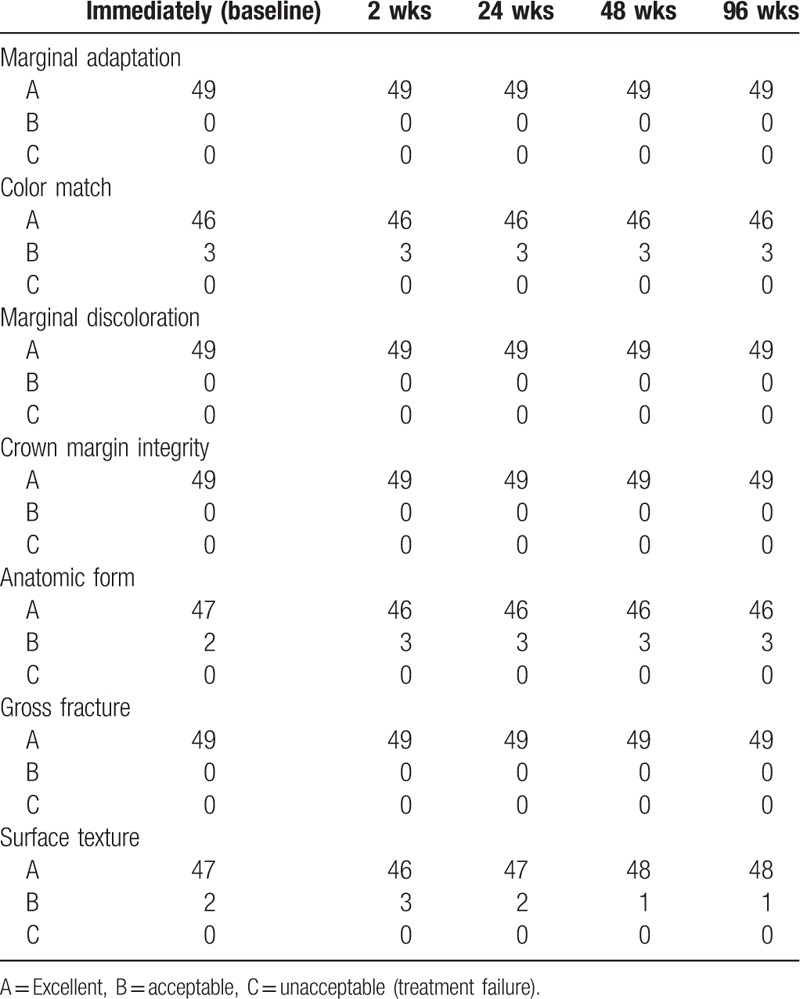
Table 3.
Clinical evaluation of crown surface wear.
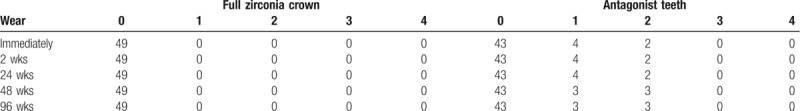
Figure 2.
The degree of attrition of antagonist teeth #16 was level 2 at 48 weeks. The dentin was exposed (arrow).
Figure 3.

The degree of plaque index of monolithic zirconia crown #26 was level 1 at 24 weeks. The plaque indicator shows a lighter color.
Figure 4.

The degree of plaque index of monolithic zirconia crown #26 was level 2 at 48 weeks. The plaque indicator shows a darker color.
Figure 5.

The degree of gingival index of monolithic zirconia crown #26 was level 1 at 24 weeks, and no bleeding on probing.
Regarding the anatomic form, only 2 cases (4.1%) were evaluated as acceptable immediately. Then, starting from the 2 weeks, the acceptable rating changed to 6.1%, and remained the same at the 96-week examination.
Regarding surface texture, the acceptable rating changed from 4.1% to 6.1% at the 2-week examination, and 2 cases (4.1%) were evaluated as acceptable at 24 weeks. From the 48-week to the 96-week examination, the acceptable rate reduced to 2.0%, with only 1 case evaluated as acceptable.
The survival parameters such as marginal adaptation, anatomic form, crown margin integrity, color match, and gross fracture did not show significant differences compared with the different time points (P = .999). Surface texture at different time did not change significantly (P = .807).
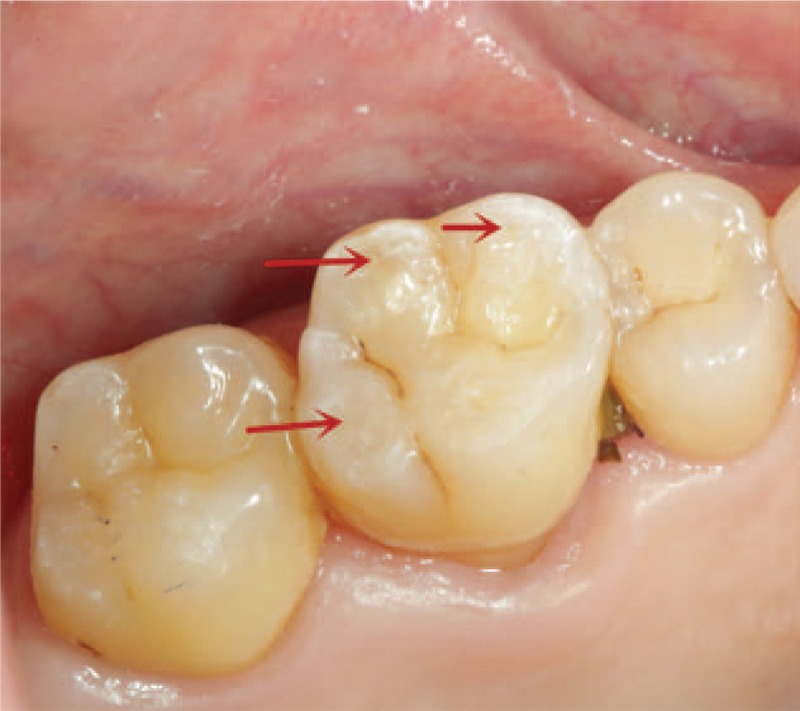
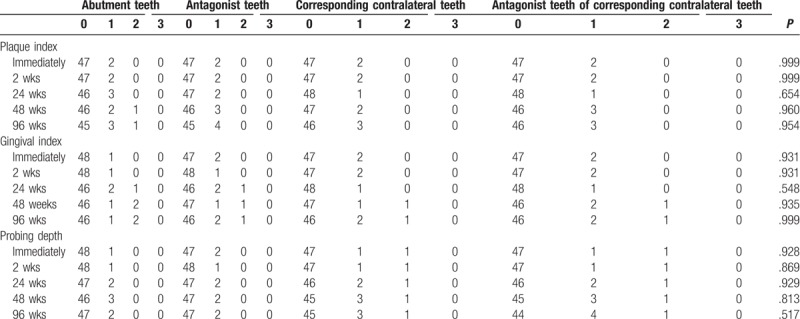
During the 96-week follow-up, 1 crack in the antagonist teeth was found in 1 patient (Fig. 7). When comparing the groups at the same time point, there were no significant differences in the clinical parameters (all P > .05) (Table 2). Similarly, statistical analysis showed that there were no significant differences in the clinical parameters at different follow-up time points (all P > .05). There were no significant differences in wear of the antagonist teeth at different time points (P = .972) (Table 3).
Figure 7.

One tooth crack was found in the antagonist tooth #26 at week 48. The arrow indicates the crack.
Table 2.
Clinical parameters at various follow-up time points.
4. Discussion
In this study, 49 monolithic zirconia crowns in 46 patients were followed for 96 weeks. Compared with the antagonist and corresponding contralateral teeth, the rates of “excellent” evaluation for the full zirconia crown restorations were 93.9% to 100% for the same patient. Only 3 patients were evaluated as “acceptable” for color match. This was because although the highly transparent zirconia was used to make the monolithic zirconia crown, its transparency and brightness were inferior to those of the all-ceramic crown coated with multilayer porcelain. Besides, surface treatments such as occlusal adjustment and polishing affect the final shade of the monolithic zirconia crown after cementation.[21] In addition, the patient's subjective assessment of color match and the physician's and technician's operations all contribute to the color match result of the crown. Nevertheless, the monolithic zirconia crown is primarily used for posterior restoration and it has no serious effect on esthetics because of slight color and brightness mismatch similar to the anterior restorations. Therefore, the subjective assessments made by the 3 patients were acceptable and not downgraded to C. The surface texture of the restorations rated with acceptable increased by 2.0% at the 2-week examination. There are several factors that can affect surface textures such as abrasion, brushing, and wearing.[22,23]
During the 96-week follow-up, all the clinical parameters of the crowns were compared with those of the antagonist teeth and the corresponding contralateral teeth and the antagonist teeth of the corresponding contralateral teeth. The results showed no significant difference in the parameters at various time points. It was probably because of the repeated oral hygiene education provided to patients by dentists during multiple visits, correcting their oral hygiene habits and improving their oral health awareness. In addition, the full zirconia crown itself has excellent biocompatibility, and the CAD/CAM technique help design and fabricate the anatomic full-contour zirconia crown with excellent marginal adaptation. The monolithic zirconia crown has a highly polished surface, making cleaning easy for the patient and disfavoring plaque deposits, without adversely affecting the periodontal tissue.
Comparing the dental plasters and the occlusal surface images between the crown and the antagonist tooth at various time points and combining the clinical examination evaluations, 1 tooth crack was found in the antagonist tooth of 1 patient at week 48. The crack was located close to the mesiomarginal edge and was shallow, not symptomatic to the patient. The patient claimed that he/she had untreated chronic pulpitis in the contralateral maxillary first molar, and he/she used the crowned side extremely heavily for almost 4 months after restoration. Furthermore, the patient preferred hard foods, making it worse. Therefore, the forces exerted on the antagonist tooth of monolithic zirconia crown were excessively frequent and large, resulting in a crack. The situation was clearly explained to the patient during follow-up. The antagonist tooth crack was repaired with a resin filling, and the contralateral tooth with chronic pulpitis was treated with a conventional resin filling after root canal treatment. The patient was also advised to use both sides of teeth alternatively for chewing and eating. In terms of wear, the antagonist tooth of one patient changed from grade 1 to grade 2 at week 48. The mechanical properties of Y-TZP ceramics determine its higher wear resistance compared with the natural teeth. Despite its high hardness, previous in-vitro studies had shown that monolithic zirconia can safely be used as an antagonist to human teeth,[24–27] but long-term in-vivo observations of a large number of cases are lacking. However, numerous in-vitro experiments demonstrated that the highly polished Y-TZP ceramics causes significantly less wear on the isolated enamel or hydroxyapatite material compared with the unpolished Y-TZP ceramics, the glazed and sintered Y-TZP ceramics, and the metal-ceramic crowns.[28–32] After the surface of Y-TZP ceramics is highly polished, the average surface roughness (Ra) reaches 0.17 ± 0.07 μm, which is lower than that of glazed zirconia (0.69 ± 0.76 μm). Considering the wear mechanism, the surface roughness of a material is an essential factor affecting wear. A clinical study showed that during a 1-year follow-up period, the attrition caused by the monolithic zirconia crown on the occlusal natural tooth was 42.10 ± 4.30 μm for premolars and 127.00 ± 5.03 μm for molars, which was significantly smaller than the attrition caused by metal-ceramics (69.20 ± 4.10 μm for premolars and 179.70 ± 8.09 μm for molars, P < .001).[33] However, the attrition of monolithic zirconia crowns on the natural teeth is greater than that between natural teeth.[25,34,35] Another study demonstrated that at the end of a 2-year follow-up, the vertical height of the antagonist tooth, full-contour zirconia crown, and corresponding contralateral natural teeth, which served as control, decreased by 46 μm, 14 μm, and 19–26 μm on average, respectively.[13] The above research results showed that the attrition caused by a monolithic zirconia crown is greater than the physiological wear of natural teeth during chewing, and a highly polished monolithic zirconia crown caused much less attrition on the enamel compared with other ceramic restorations.
The limitations of this study are that the sample size was small and the observation time was short. Wear behavior may be different if >2 units of crown or large-span fixed dental prostheses are used. Larger clinical trials with more patients are needed, requiring more restorative options and assessments during longer follow-up periods.
5. Conclusions
This clinical study showed that during the 96-week follow-up period, the monolithic zirconia crown has no adverse effect on the periodontal tissues, exhibiting good biocompatibility. The antagonist tooth wear is small, and the success rate of posterior restorations is high. Nevertheless, longer-term effects still need further investigation.
Author contributions
Conceptualization: Zhenyu Tang, Xinyi Zhao.
Data curation: Zhenyu Tang, Hui Wang.
Formal analysis: Hui Wang, Bin Liu.
Methodology: Zhenyu Tang, Bin Liu.
Project administration: Xinyi Zhao.
Resources: Bin Liu.
Software: Hui Wang, Bin Liu.
Validation: Xinyi Zhao.
Visualization: Xinyi Zhao, Hui Wang.
Writing – original draft: Zhenyu Tang.
Writing – review & editing: Zhenyu Tang, Xinyi Zhao, Hui Wang, Bin Liu.
Footnotes
Abbreviations: CAD/CAM = computer-aided manufacturing, CDA = California Dental Association, GI = gingival index, PD = probing depth, PLI = plaque index, Y-TZP = yttria-stabilized tetragonal zirconia polycrystals.
How to cite this article: Tang Z, Zhao X, Wang H, Liu B. Clinical evaluation of monolithic zirconia crowns for posterior teeth restorations. Medicine. 2019;98:40(e17385).
Funding: This study was supported by the Scientific Research and Technology Development Plan of Guangxi Province (grant No. 14124004-1-10) and the Scientific Research Plan Project of Guailin City (grant No. 20140120-8-1, 2016012709). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors report no conflicts of interest.
References
- [1].Porcelain-Fused-to-Metal Crowns versus All-Ceramic Crowns: A Review of the Clinical and Cost-Effectiveness. Ottawa: Canadian Agency for Drugs and Technologies in Health; 2016. [PubMed] [Google Scholar]
- [2].Barao VA, Gennari-Filho H, Goiato MC, et al. Factors to achieve aesthetics in all-ceramic restorations. J Craniofac Surg 2010;21:2007–12. [DOI] [PubMed] [Google Scholar]
- [3].Kumagai N, Hirayama H, Finkelman MD, et al. The effect of translucency of Y-TZP based all-ceramic crowns fabricated with difference substructure designs. J Dent 2013;41suppl 3:e87–92. [DOI] [PubMed] [Google Scholar]
- [4].Harada K, Shinya A, Gomi H, et al. Effect of accelerated aging on the fracture toughness of zirconias. J Prosthet Dent 2016;115:215–23. [DOI] [PubMed] [Google Scholar]
- [5].Harada K, Shinya A, Yokoyama D, et al. Effect of loading conditions on the fracture toughness of zirconia. J Prosthodont Res 2013;57:82–7. [DOI] [PubMed] [Google Scholar]
- [6].de Kok P, Kleverlaan CJ, de Jager N, et al. Mechanical performance of implant-supported posterior crowns. J Prosthet Dent 2015;114:59–66. [DOI] [PubMed] [Google Scholar]
- [7].Pereira GKR, Guilardi LF, Dapieve KS, et al. Mechanical reliability, fatigue strength and survival analysis of new polycrystalline translucent zirconia ceramics for monolithic restorations. J Mech Behav Biomed Mater 2018;85:57–65. [DOI] [PubMed] [Google Scholar]
- [8].Hao Z, Ma Y, Liu W, et al. Influence of low-temperature degradation on the wear characteristics of zirconia against polymer-infiltrated ceramic-network material. J Prosthet Dent 2018;120:596–602. [DOI] [PubMed] [Google Scholar]
- [9].Rekow ED, Silva NR, Coelho PG, et al. Performance of dental ceramics: challenges for improvements. J Dent Res 2011;90:937–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Candido LM, Miotto LN, Fais L, et al. Mechanical and surface properties of monolithic zirconia. Oper Dent 2018;43:E119–28. [DOI] [PubMed] [Google Scholar]
- [11].Stawarczyk B, Keul C, Eichberger M, et al. Three generations of zirconia: from veneered to monolithic. Part II. Quintessence Int 2017;48:441–50. [DOI] [PubMed] [Google Scholar]
- [12].Krell K, Hutzler T, Klimke J. Transmission physics and consequences for materials selection, manufacturing, and applications. J Euro Cera Soci 2009;29:207–21. [Google Scholar]
- [13].Stober T, Bermejo JL, Schwindling FS, et al. Clinical assessment of enamel wear caused by monolithic zirconia crowns. J Oral Rehabil 2016;43:621–9. [DOI] [PubMed] [Google Scholar]
- [14].Miura S, Kasahara S, Yamauchi S, et al. Clinical evaluation of zirconia-based all-ceramic single crowns: an up to 12-year retrospective cohort study. Clin Oral Investig 2018;22:697–706. [DOI] [PubMed] [Google Scholar]
- [15].Lohbauer U, Reich S. Antagonist wear of monolithic zirconia crowns after 2 years. Clin Oral Investig 2017;21:1165–72. [DOI] [PubMed] [Google Scholar]
- [16].Kitaoka A, Akatsuka R, Kato H, et al. Clinical evaluation of monolithic zirconia crowns: a short-term pilot report. Int J Prosthodont 2018;31:124–6. [DOI] [PubMed] [Google Scholar]
- [17].California Dental Association. Quality Evaluation for Dental Care. Guidelines for the assessment of Clinical Quality and Performance, 3rd edition. Sacramento 1995. [Google Scholar]
- [18].Schmitz JH, Cortellini D, Granata S, et al. Monolithic lithium disilicate complete single crowns with feather-edge preparation design in the posterior region: a multicentric retrospective study up to 12 years. Quintessence Int 2017. 601–8. [DOI] [PubMed] [Google Scholar]
- [19].Cheng Q, Gao WM, Cao B, et al. Effects of Ginkgo biloba extract on periodontal pathogens and its clinical efficacy as adjuvant treatment. Chin J Integr Med 2014;20:729–36. [DOI] [PubMed] [Google Scholar]
- [20].Smith BG, Knight JK. An index for measuring the wear of teeth. Br Dent J 1984;156:435–8. [DOI] [PubMed] [Google Scholar]
- [21].Kim HK, Kim SH, Lee JB, et al. Effect of polishing and glazing on the color and spectral distribution of monolithic zirconia. J Adv Prosthodont 2013;5:296–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Amer R, Kurklu D, Johnston W. Effect of simulated mastication on the surface roughness of three ceramic systems. J Prosthet Dent 2015;114:260–5. [DOI] [PubMed] [Google Scholar]
- [23].Konstantinidis I, Trikka D, Gasparatos S, et al. Clinical outcomes of monolithic zirconia crowns with CAD/CAM technology. a 1-year follow-up prospective clinical study of 65 patients. Int J Environ Res Public Health 2018;15:E2523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Sripetchdanond J, Leevailoj C. Wear of human enamel opposing monolithic zirconia, glass ceramic, and composite resin: an in vitro study. J Prosthet Dent 2014;112:1141–50. [DOI] [PubMed] [Google Scholar]
- [25].Pathan MS, Kheur MG, Patankar AH, et al. Assessment of antagonist enamel wear and clinical performance of full-contour monolithic zirconia crowns: one-year results of a prospective study. J Prosthodont 2019;28:e411–6. [DOI] [PubMed] [Google Scholar]
- [26].Kim MJ, Oh SH, Kim JH, et al. Wear evaluation of the human enamel opposing different Y-TZP dental ceramics and other porcelains. J Dent 2012;40:979–88. [DOI] [PubMed] [Google Scholar]
- [27].Mormann WH, Stawarczyk B, Ender A, et al. Wear characteristics of current aesthetic dental restorative CAD/CAM materials: two-body wear, gloss retention, roughness and Martens hardness. J Mech Behav Biomed Mater 2013;20:113–25. [DOI] [PubMed] [Google Scholar]
- [28].Kwon SJ, Lawson NC, McLaren EE, et al. Comparison of the mechanical properties of translucent zirconia and lithium disilicate. J Prosthet Dent 2018;120:132–7. [DOI] [PubMed] [Google Scholar]
- [29].Buciumeanu M, Queiroz JRC, Martinelli AE. The effect of surface treatment on the friction and wear behavior of dental Y-TZP ceramic against human enamel. Tribol Int 2017;116:192–8. [Google Scholar]
- [30].Mitov G, Heintze SD, Walz S, et al. Wear behavior of dental Y-TZP ceramic against natural enamel after different finishing procedures. Dent Mater 2012;28:909–18. [DOI] [PubMed] [Google Scholar]
- [31].Pozzobon JL, Pereira GKR, Wandscher VF, et al. Mechanical behavior of yttria-stabilized tetragonal zirconia polycrystalline ceramic after different zirconia surface treatments. Mater Sci Eng C Mater Biol Appl 2017;77:828–35. [DOI] [PubMed] [Google Scholar]
- [32].Mohammadi-Bassir M, Babasafari M, Rezvani MB, et al. Effect of coarse grinding, overglazing, and 2 polishing systems on the flexural strength, surface roughness, and phase transformation of yttrium-stabilized tetragonal zirconia. J Prosthet Dent 2017;118:658–65. [DOI] [PubMed] [Google Scholar]
- [33].Mundhe K, Jain V, Pruthi G, et al. Clinical study to evaluate the wear of natural enamel antagonist to zirconia and metal ceramic crowns. J Prosthet Dent 2015;114:358–63. [DOI] [PubMed] [Google Scholar]
- [34].Esquivel-Upshaw JF, Kim MJ, Hsu SM, et al. Randomized clinical study of wear of enamel antagonists against polished monolithic zirconia crowns. J Dent 2018;68:19–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Yang SW, Kim JE, Shin Y, et al. Enamel wear and aging of translucent zirconias: In vitro and clinical studies. J Prosthet Dent 2019;121:417–25. [DOI] [PubMed] [Google Scholar]


