Abstract
Background
With climate change, heat waves are expected to become more frequent in the near future. Already, on average more than 25 000 “heat deaths” are estimated to occur in Europe every year. However, heat stress and heat illnesses arise not just when ambient temperatures are high. Physical exertion increases heat production within the organism many times over; if not enough heat is lost, there is a risk of exertional heat stress. This review article discusses contributing factors, at-risk groups, and the diagnosis and treatment of heat illnesses.
Methods
A selective literature search was carried out on PubMed. Current guidelines and expert recommendations were also included.
Results
Apart from muscular heat production (>70% of converted energy), there are other factors that singly or in combination can give rise to heat stress: clothing, climate/acclimatization, and individual factors. Through its insulating properties, clothing reduces the evaporation of sweat (the most effective physiological cooling mechanism). A sudden heat wave, or changing the climate zone (as with air travel), increases the risk of a heat-related health event. Overweight, low fitness level, acute infections, illness, dehydration, and other factors also reduce heat tolerance. In addition to children, older people are particularly at risk because of their reduced physiological adaptability, (multi-)morbidity, and intake of prescription drugs. A heat illness can progress suddenly to life-threatening heat stroke. Successful treatment depends on rapid diagnosis and cooling the body down as quickly as possible. The aim is to reduce core body temperature to <40 °C within 30 minutes.
Conclusion
Immediately effective cooling interventions are the only causal treatment for heat stroke. Time once lost cannot be made up. Prevention (acclimatization, reduced exposure, etc.) and terminating the heat stress in good time (e.g., stopping work) are better than any cure.
Time and again, heatwaves claim lives. In Europe, on average, over 25 000 heat-related deaths are believed to occur every year (e1– e4). With climate change, these sudden episodes of extreme weather are expected to be more frequent (e5, e6), impacting a population that is largely insufficiently acclimatized.
However, heat stress and health risks do not only arise when environmental temperatures are high; they can be triggered by physical exertion—even at apparently low-risk temperatures (1– 3). Intense and rapid heat production takes place in the working muscles, such that at a high intensity of activity core body temperatures of over 39 °C can be reached within 20 minutes (4– 6). Whether at work, in leisure pursuits, or during sporting activity, physical exertion can lead to overheating of the organism (heat stress) and to heat illness; higher environmental temperatures further increase the risk (7– 13).
This review article focuses on:
The main factors (physical exertion, clothing, environmental conditions, and individual characteristics) that singly or in combination can trigger heat stress in an organism (1– 3, 14, 15);
Population groups at increased risk of a heat-related health event; and
The diagnosis and treatment of heat illness.
Methods
A selective literature search was carried out on PubMed for heat illness associated with the following topic clusters: climate, risk factors, prevention, treatment, and diagnosis. Guidelines and expert recommendations (16) were also included. Search terms and the search procedure were as shown in the eBox and the eTable.
eBOX. Method.
The selective literature search was carried out on PubMed without restriction (no filters). The eTable shows the various search terms used during the primary search. Guidelines and expert recommendations were also included.
Search terms within the various topic clusters (“hyperthermia,” “climate,” “risk factors,” and “prevention/treatment/diagnosis”) were first combined into clusters using the OR operator. A total of four independent search strategies were followed by then combining each topic cluster separately with the superordinated main topic “heat illness” using the AND operator.
eTable. Search strategy for the heat illness topic cluster.
|
Heat illness Heat illness/heat injury/heat stroke/heat strain/exertional heatstroke/exertional heat illness | |||
| Hyperthermia | Climate | Risk factors | Prevention/treatment/diagnosis |
| Exercise-heat stress Exertional heat illness Exertional heatstroke (EHS) Heat casualties Heat cramps Heat collapse Heat exhaustion Heat illness Heat injury Heat load Heat-related illness Heat stress Heat stress disorder Heat stress syndrome Heat syncope Heat strain Heat stroke Thermal strain Thermal stress Uncompensable heat stress (UCHS) |
Air motion Ambient temperature Climate Climate change Climatic change Climate indices Environmental heat stress index Heat radiation Heat waves Humidity Temperature Thermal regulatory model Universal thermal climate index (UTCI) Wet bulb globe temperature (WBGT) Wet bulb globe temperature index Wind speed |
Body heat exchange Clothing Dehydration Exercise Heat production Metabolic heat production Metabolic rate Military Motivation Obesity Occupation Occupational exposure Overweight Physical activity Protective clothing Risk factor Sports Thermal insulation Work load |
Acclimatisation Acclimatization (Body) core temperature Body temperature regulation Compensable heat stress (CHS) Clothing Cooling Dehydration Electrolyte replacement Environmental exposure Fitness Fluid replacement Heat adaptation behavior Heat exposure Heat (stress) management Heat shock proteins Heat tolerance Hydration Hyponatremia Physical fitness Prevention Rehydration Rectal temperature Rest cycles SIRS Sweat evaporation Sweat rate Sweating rate Therapy Thermoregulation Work cycles |
Muscles as heat engines
The combination of heat with physical work puts enormous stress on the human organism and can lead to sudden loss of performance and threats to health (1, 3, 17– 19). However, the organism can also become overheated in ambient temperatures below 0° C: for example, during ski patrols in an ambient temperature of –8 °C, core body temperatures of over 38 °C have been measured (1, 20). In a few cross-country skiers, core temperatures of over 40 °C have been recorded (1, 4).
Muscle work can lead to a rate of heat production that is more than ten times that in the resting state. As with a heat engine, by far the greatest part of the energy converted within the muscle is released in the form of heat (>70%) (1, 21– 24). During running, the mechanically usable part of the energy is 25% at most. In domestic work or occupational activities, such as carrying loads or moving about in protective clothing, the efficiency is much lower (1, 19, 25, 26). Because humans have a low tolerance (37 °C to around 40 °C) for increases in core body temperature, under conditions of heat even moderate physical work can result in heat illness, which may be as extreme as heat stroke, without warning (2, 18).
Insulating effect of clothing
Insulation provided by clothing should be variably adapted to ambient environmental conditions (e.g., in heat waves) in order to avoid additional thermal stress. Where there is a particularly high need for protection, however, such stress can be unavoidable even in temperate conditions (1, 27), e.g., in sport (football, fencing) or in certain occupations (e.g., police, firefighters, the military, the chemical industry). Furthermore, the weight and movement restrictions imposed by protective clothing and equipment can lead to increased muscle work and metabolic heat production (28).
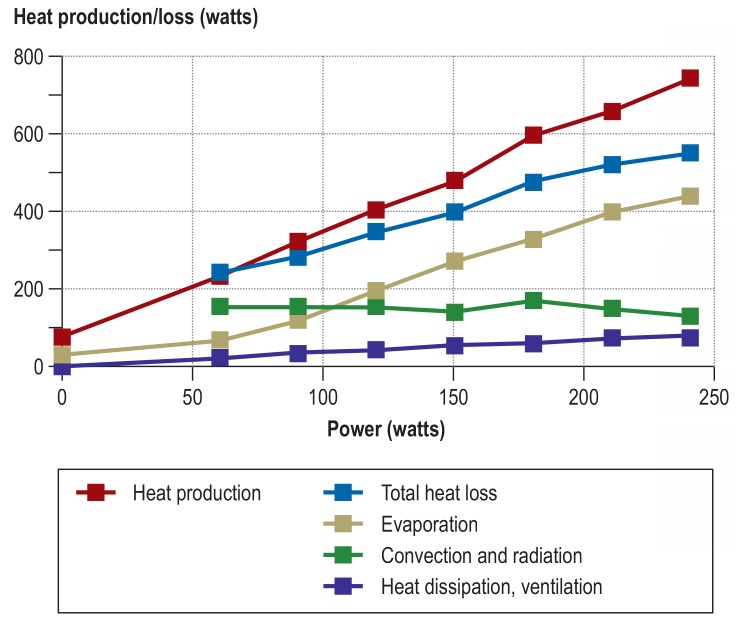
Figure 1 shows heat production and dissipation at rest and during physical work. When protective clothing is worn, the most important and most efficient (70% to 80%) physiological cooling mechanism during physical work—heat loss through the evaporation of sweat—is very greatly restricted (1, 27). As a result of this, high rates of metabolic heat production can result in fatal heat stroke (29, 30). No representative data exist as to the incidence of fatal heat stroke in persons carrying out physical work in protective clothing.
Figure 1.
Heat metabolism: heat production and heat dissipation at rest and during increasing physical exertion (60 minutes on a cycle ergometer) in an unclothed human being at an ambient temperature of 22° C (adapted from [e7, e8])
Climate and acclimatization
When protective clothing is worn, even small amounts of thermal environmental stress increase the risk of heat illness (1, 9, 17– 19, 29, 31, 32). In addition to air temperature, humidity, wind speed, and heat radiation are all significant climatic factors. Thermal environmental indices have been created to reduce various combinations of these effect sizes into a single value. For outdoor heat exposure, the WBGT (wet bulb globe temperature) index is widely used (16, 33). It is used to estimate risk in order to reduce heat-related health events at work (16) or during sport (34).
Through acclimatization (classic signs of adaptation: increased sweat rate, lower heart rate and core body temperature), heat tolerance can be improved and heat stress more easily compensated (35– 38). However, it takes about 7 to 10 days for acclimatization to occur (18, 37, 39, 40). Sudden heat waves (on land) or changing climate zones (air travel) increase the risk of a heat-related event due to lack of or insufficient acclimatization (e1, e9, e10).
Risk factors in the individual and at-risk groups
Heat tolerance can vary greatly within a single person: acute infections and disease, dehydration, disturbances in electrolyte levels, overmotivation, insufficient acclimatization, or intake of prescription drugs all make heat illness more likely (1, 15, 26, 29, 32, e11, e12). Everyday observation, too, reveals variations in the ability to tolerate heat stress. For example, there are wide variations between individuals as to how much they sweat. Children are much more vulnerable than adults to high heat stress (1, e13– e15), because they have lower sweat rates, both absolute and relative (i.e., relative to their body surface area) (e14, e16). Despite sex-related differences (women have more subcutaneous fat tissue, later onset of sweat secretion, menstruation-related changes in core body temperature, etc.), men and women appear to have similar abilities to withstand heat stress (1, 19, e17–e19; on the ability of children and women to withstand heat stress, see review articles e13, e20, e21).
Older people
Older people in particular (from the age of 75) are at risk on hot days and during heat waves (e22– e25). Most heat-related deaths in Germany (2001–2015) are estimated to have occurred in 2003 (n = 7600), 2006 (n = 6200), and 2015 (n = 6100), and most were in this age group (e22). The main causes are the higher prevalence of chronic disease and the reduced physiological adaptability of this population group (e26). For example, skin blood flow is lower in old age and the redistribution of blood volume from retroperitoneal venous networks to the skin capillary bed is decreased (e27, e28). Older people also sweat later and less than younger ones (e29, e30). As a result of these changes, less heat can be dissipated through the skin in old age (e31). Disease can further restrict thermoregulation. For example, in patients with cardiac insufficiency, the thermophysiological increase in skin blood flow may be reduced, because it requires cardiac output to be increased while at the same time maintaining adequate blood pressure.
Heat waves at the beginning of the summer generally result in higher death rates than those at the end of the summer (e32). Important risk factors for higher mortality include advanced age; low social status; addictive disorders; restricted mobility; the presence of pulmonary, cardiovascular, or psychogeriatric disease; and chronic renal disease (e33). People who live high up in a building or live alone also have a statistically increased risk (e34). It is now widely accepted that heat stress is particularly dangerous to old, frail, and often (multi-) morbid people and this is a generalized problem in geriatrics (e26).
One thing that is not universally known is that prescription drugs can also damage heat resilience (e35). Medical drugs can interfere with at least five important defense mechanisms. The perception of thirst, for example, can be impaired by ACE inhibitors (e36). Opioids, serotonin reuptake inhibitors, carbamazepine, anticholinergics, and tricyclic antidepressants can impair central thermoregulation (e34, e37). Hypohidrosis can be triggered by antimuscarinic agents such as anticholinergics, tricyclic antidepressants, or antipsychotics (e38). Sympathomimetics, by causing cutaneous vasoconstriction, can affect the regulation of skin blood flow (e39). In patients being treated with sedatives (e.g., benzodiazepines, opioids), early recognition of warning symptoms is harder because they already have altered attention and alertness (e26).
It should also be noted that heat affects pharmacokinetics by means of various mechanisms, and thus influences the effective level (concentration) of an active substance in patients (e35). Local heat, for example, can quadruple cutaneous blood flow, increasing the systemic availability of transcutaneously administered drugs (e.g., opioid patches) (e40). The same is true of subcutaneously administered drugs (such as insulin), which are more rapidly released with increased temperature and have a correspondingly stronger effect. Renal and hepatic blood flow may diminish by around one third (e35). The latter affects the bioavailability of orally administered substances with high hepatic extraction rates (i.e., substances with a high first-pass effect), such as beta-blockers.
Overweight and low physical fitness
Overweight and a low fitness level reduce heat tolerance markedly (1– 3, 14, 15, 19, 29). Impressive results were presented by Bedno et al., who studied the occurrence of heat illness in 9455 male US army recruits during their first 180 days of service. These authors showed that fitness and weight status are independently associated with the occurrence of heat illness. In comparison to trained normal-weight recruits, untrained normal-weight recruits had twice the risk of heat illness. Trained overweight recruits had an almost four-fold increased risk, and untrained overweight recruits an almost eight-fold increased risk of a heat event (2, e41).
Risk of heat stress in sport and at work
Physical exertion leads to a considerable increase in heat production. In athletes during maximal exertion, rectal temperatures of >41 °C have been reported (6, e42– e45). Most of these reports come from clinical case reports. In studies, testing usually has to be stopped before a core body temperature of 39.0 °C (16) is reached.
In long-distance events (marathon or half-marathon), considerable fluid/electrolyte loss can occur, even in temperate conditions, as can exertional heat stress (10, 11, 36, e46). Dangerous heat stress can also occur in other popular sports (such as tennis or football), for example if older people or those with health-related risk factors play to the limit of their capacity (e46, e47). In some areas of professional sport (2019 Australian Open tennis tournament in Melbourne; 2014 Football World Championship in Brazil), heat/cooling-down breaks have been introduced (e48– e50). Increased risks exist in other sports in which protective clothing is used (fencing, motor racing, and others). Every year, heat stress–related deaths are seen in American football (e45, e51, e52).
In the world of work, many kinds of industrial jobs are carried out in hot work environments (e.g., steel, glass, and ceramics production). Less well known is heat exposure in work environments where high humidity is added to the ambient thermal stress (kitchens, laundries, sculleries, etc.). The protective clothing worn by firefighters, police, military personnel, and also some medical personnel (barrier nursing, etc.), which insulates and impedes the loss of heat through evaporation, also leads to the risk of overheating, requiring restrictions on the length of time for which they can be worn (e53) or else microclimate body cooling (27). All over the world, people working in civil engineering, or in agricultural or forestry work, are at risk of heat illness (7, 8) and the carcinogenic effects of UV light (e54, e55).
Diagnosis and treatment of heat illness
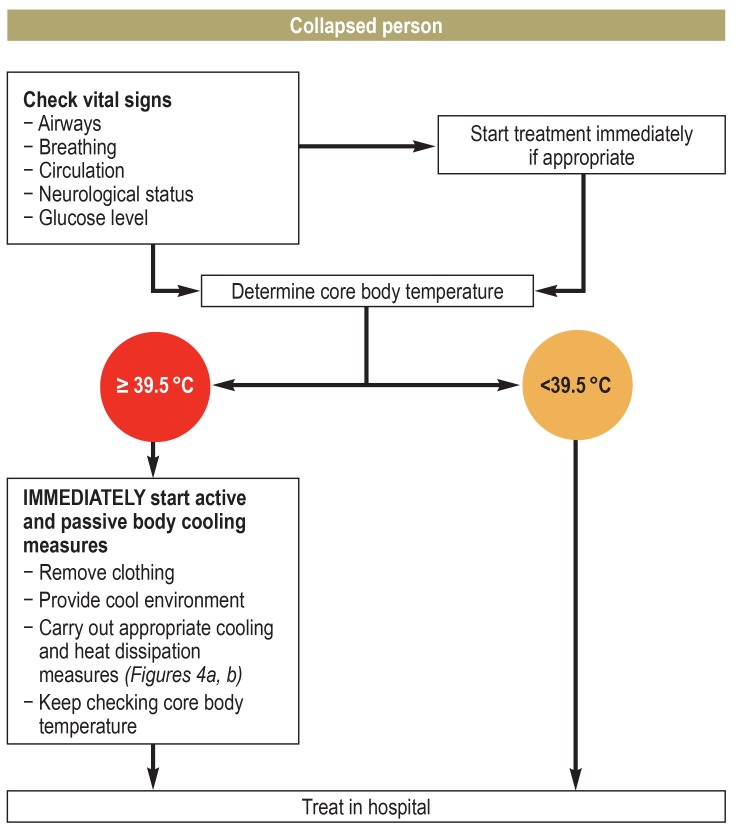
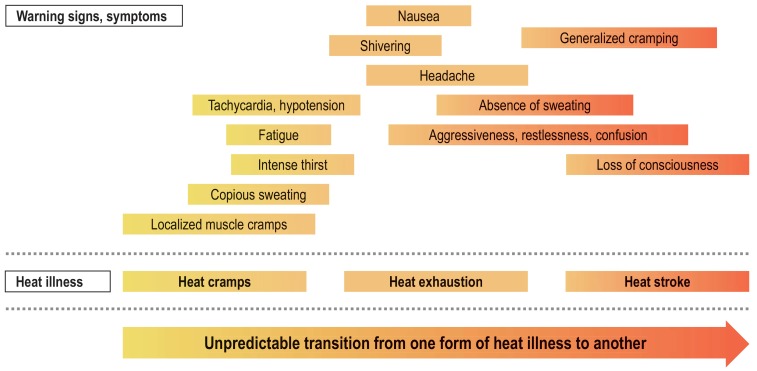
Heat stroke, the most dangerous form of heat illness, can be successfully treated if the condition is diagnosed as quickly as possible and cooling measures are started before the patient is transferred to hospital (figure 2). When heat stroke is suspected, it is extremely important to monitor core body temperature, preferably rectally (e56). There is no single agreed method of clinically determining mean skin temperature, but this should still be considered, in addition to skin color and the presence or absence of sweating, to assess thermoregulatory status (body core versus body shell). Typical symptoms of heat illness are shown in Figure 3; the different forms of heat illness can arise independently, and sudden deterioration can occur (17, e57). For example, there may be a sudden transition from red skin color (skin blood flow present) to pallor (circulation centralized to the core). In suspected cases, nothing, not even rectal temperature measurement, should be allowed to delay the immediate start of cooling treatment (36, e57– e59).
Figure 2.
Flowchart for use in a case of suspected exertional heat stroke (36, e57– e59)
Figure 3.
Symptoms of heat illnesses. Not all the symptoms may appear, and they may not appear in any given order. The various forms of heat illness may develop independently and apparently without warning; i.e., this is not a regular sequence of recognizable stages of illness (adapted from [e78, e81]).
Sunstroke
Direct sun on the uncovered head for a long period can lead to heat stress of the brain, resulting in inflammation of the meninges or even to brain edema (e60). Sunstroke should be seen as primarily a localized condition and is not directly caused by a significant rise in body temperature (e57, e61). Depending on severity, symptoms range from overheating of the head with headache, dizziness, restlessness, nausea, and meningism to altered consciousness and cerebral seizures (e60, e62, e63).
Heat cramps
Heat cramps usually affect the local working muscles, and like heat edema, heat rash, and heat collapse/syncope they are regarded as a mild form of heat illness (e64). Heat cramps are painful muscle contractions and cramps during physical exertion; typically there is no systemic build-up of heat and core body temperature is often normal (e65). In sports that involve much running (e.g., football, marathons), calf cramps are common, whereas in tennis it may be the muscles of the forearm and/or hand that are affected (37, e66). The key element is the combination of intense sweating, electrolyte loss, and a negative fluid balance (e67, e68). Insufficient acclimatization with an elevated electrolyte concentration in the sweat increases the risk of heat cramps (e69). The symptoms of heat cramp, including weakness, headache, and nausea, can occur simultaneously with heat exhaustion (40).
Heat collapse/syncope
Heat collapse/syncope is a risk especially in people who stand for a long time in a hot environment (e64). The heat leads first to dehydration and to redistribution of blood into peripheral sections of the circulation, especially with a strong increase in skin blood flow. This can cause a drop in blood pressure and cerebral blood flow, triggering syncope (e70). Laying the patient flat (with or without elevation of the legs), loosening the clothing, moving the patient into a cool environment, and if necessary giving infusions, will quickly bring this relatively minor health event under control.
Heat exhaustion and heat stroke
Excessive sweating and dehydration during physical exertion in a warm environment are typical of heat exhaustion (e71). Usually only low-grade cerebral symptoms are present (e.g., dizziness). Immediate interventions include heat dissipation (removing clothing, cooling measures), intravenous fluid administration, and monitoring of vital signs (34). Monitoring core body temperature and the cerebral status is extremely important, as heat exhaustion can occasionally progress to heat stroke.
At core body temperatures >40.0 °C, endothelial cells become increasingly damaged, resulting in capillary leak (e72, e73). In heat stroke, this is the trigger for pathophysiological processes with systemic effects that can culminate in multiorgan failure (e72– e74). The generalized endothelial cell damage has effects on various organ systems, and can lead to multiple organ failure via the systemic inflammatory response (SIRS) (e72, e73, e75, e76). Predisposing factors and symptoms of exertional heat stroke are shown in the Box and in Figure 3 (further information is provided in [15, e77–e80]).
BOX. Predisposing factors (with examples) of exertional heat stroke (adapted from [15, e79, e80]).
-
Environmental factors
High environmental temperature
High humidity
No air movement
No shade
-
Constitutional factors
Age
Overweight
Low fitness level
No heat acclimatization
Dehydration
Lack of sleep
-
Medical drugs and other substances
Alcohol
Antihistamines
Benzodiazepines
Beta-blockers, and many more
-
Health status
Viral infection
Diabetes mellitus
Feverish illness
Cardiovascular disease
-
Mental factors
Strong desire to succeed/overmotivation accompanied by (as yet) insufficient performance capacity, e.g., in athletes and military personnel
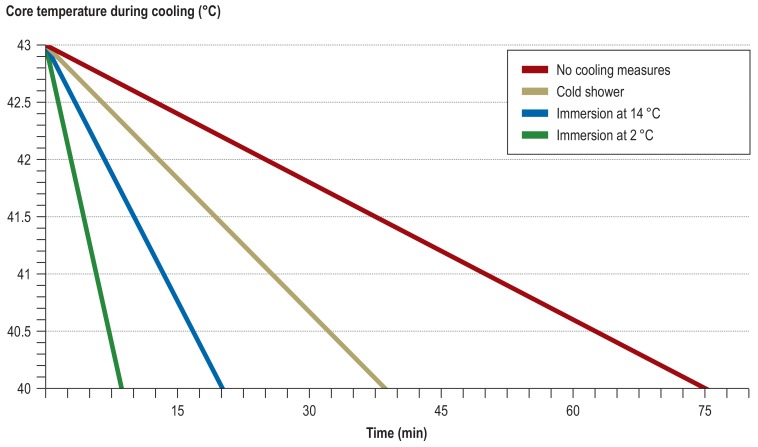
Immediate initiation of cooling is the only causal treatment (Figure 4a, 4b). The longer core body temperature remains above >40 °C, the poorer the expected outcome (36, e76, e82, e83). The aim of treatment is to bring down the core body temperature below 40 °C within 30 minutes (the “golden half hour”) (e84). Whole-body immersion in iced water is the recommended intervention with the most rapid cooling effect (Figure 4a, b). Because the start of treatment is time-critical, it should be carried out as fast as possible: clothing can be removed once the patient is immersed (e85). Other, less effective ways of cooling include immersion in tepid water, immersion of the torso, cold packs on the torso, and so on (e23, e79, e86– e89). The success of treatment depends on the greatest possible temperature gradient between the body core and the cooling intervention (e90). Patients with exertional heat stroke are typically young and without pre-existing cardiovascular disease. No cardiac events due to cooling interventions have been described. Once core body temperature has reached 38–39 °C, the cooling interventions should be halted so as to avoid a further temperature drop due to blood returning from the periphery to the core (afterdrop) (e91). When cooling measures in the form of ice water immersion are implemented without delay, further treatment purely on an outpatient basis has been described (e92– e97).
Figure 4a.
Rate of cooling of the human body using various cooling methods. The comparison is for general guidance only, since no standardized comparison is possible for the studies involved (e42, e93– e95, e97) in terms of initial body temperature and patient population characteristics (age, sex, body mass, body surface area to volume ratio, etc.). For the saline infusions, 2 × 1 L 0.9% saline solution was used.
Figure 4b.
Model of reduction over time in core body temperature (adapted from [e96], assuming constant mean cooling rates [e93, e97]), the same initial temperature (43 °C), and the same time of treatment initiation. The chosen endpoint was the lower temperature threshold for cell damage in human beings (40 °C).
If there is a delay in starting treatment, or symptoms are initially misinterpreted, morbidity and mortality rise sharply (e83, e98). Lost time cannot be made up. In patients admitted to emergency departments, cooling measures should be continued with monitoring of core body temperature at close intervals until it has reached 38–39 °C (e23, e87, e99, e100). The clinical (inpatient) course—especially in cases when the start of treatment has been delayed—often requires all the options offered by intensive medicine, up to and including organ transplantation, because of the multiorgan failure (e101, e102). In cases where inpatient treatment is required, life expectancy appears to be shorter even when the patient makes a good initial recovery (e103). No pharmacological alternative to immediate cooling interventions exists. Dantrolene is not an option (e104). Antipyretics do not help either, since the problem is not a fever, but overheating caused by muscle work (e105).
Summary
Heat-related health events can develop quickly, especially during physical exertion (even at apparently innocuous ambient temperatures), and can lead to life-threatening heat stroke. Successful clinical treatment of heat stroke requires the core body temperature to be reduced below 40 °C within the first 30 minutes, and this requires aggressive cooling interventions. Prevention is better than cure with heat illness, and this means effective preventive measures (drinking, acclimatization, reduced exposure, etc.) (16), and terminating the heat stress (e.g., sport or work activity) in good time.
Key messages.
Even in moderate ambient temperatures, physical exertion can lead to exertional heat stress, dramatic loss of performance, and risks to health.
The risk of heat-related health events is higher in sports and work activities involving intense metabolic heat production and/or in which heat dissipation is restricted.
The combination of overweight with low physical fitness increases the risk of a heat-related health event by a factor of eight. Children and older people are also at increased risk.
Heat tolerance can vary greatly within a single person: acute infections and disease, dehydration, insufficient acclimatization, intake of prescription drugs, and other factors can all cause problems with heat.
The only causal treatment for heat stroke is to reduce core body temperature (<40 °C within 30 minutes); there is no pharmacological treatment (such as with dantrolene for malignant hyperthermia). In suspected cases, cooling measures should be started immediately.
Acknowledgments
Translated from the original German by Kersti Wagstaff, MA.
Acknowledgments
The authors are grateful to Frank Uwe Heinze and Matthias Krapick (Bundeswehr Institute for Preventive Medicine) for their professional collaboration in the development of this article.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.Leyk D. Körperliche Arbeit bei Hitzestress: Eine oft unterschätzte Belastung und Gefahr. Wehrmed Mschr. 2018;62:354–356. [Google Scholar]
- 2.Bedno SA, Li Y, Han W, et al. Exertional heat illness among overweight US. Army recruits in basic training. Aviat Space Environ Med. 2010;81:107–111. doi: 10.3357/asem.2623.2010. [DOI] [PubMed] [Google Scholar]
- 3.Epstein Y, Moran DS, Shapiro Y. Pandolf KB, Burr RE, editors. Exertional heatstroke in the Israeli defence forces Textbooks of military medicine. Volume 1: Medical aspects of harsh environments. Falls Church: Office of the Surgeon General. 2001:281–292. [Google Scholar]
- 4.Israel S. Lehrbuch der Sportmedizin. 4th edition. Heidelberg Barth: 1999. Thermoregulation und Wasserhaushalt In: Badtke G, Bittmann F (eds.): pp. 268–276. [Google Scholar]
- 5.Galloway SD, Maughan RJ. Effects of ambient temperature on the capacity to perform prolonged cycle exercise in man. Med Sci Sports Exerc. 1997;29:1240–1249. doi: 10.1097/00005768-199709000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Racinais S, Moussay S, Nichols D, et al. Core temperature up to 415º C during the UCI Road Cycling World Championships in the heat. Br J Sports Med. 2019;53:426–429. doi: 10.1136/bjsports-2018-099881. [DOI] [PubMed] [Google Scholar]
- 7.Lucas RAI, Epstein Y, Kjellstrom T. Excessive occupational heat exposure: a significant ergonomic challenge and health risk for current and future workers. Extrem Physiol Med. 2014;3:1–8. doi: 10.1186/2046-7648-3-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xiang J, Bi P, Pisaniello D, Hansen A. Health impacts of workplace heat exposure. An epidemiological review. Ind Health. 2014;52:91–101. doi: 10.2486/indhealth.2012-0145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Epstein Y, Druyan A, Heled Y. Heat injury prevention—a military perspective. J Strength Condit Res. 2012;26:82–86. doi: 10.1519/JSC.0b013e31825cec4a. [DOI] [PubMed] [Google Scholar]
- 10.Cheuvront SN, Haymes EM. Thermoregulation and marathon running: biological and environmental influences. Sports Med. 2001;31:743–762. doi: 10.2165/00007256-200131100-00004. [DOI] [PubMed] [Google Scholar]
- 11.Veltmeijer MTW, Eijsvogels TMH, Thijssen DHJ, Hopman MTE. Incidence and predictors of exertional hyperthermia after a 15-km road race in cool environmental conditions. J Sci Med Sport. 2015;18:333–337. doi: 10.1016/j.jsams.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 12.Schickele E. Environment and fatal heat stroke War II. An analysis of 157 cases occurring in the army in the U.S. during World War II. Military Surgeon. 1947;100:235–256. [PubMed] [Google Scholar]
- 13.Cassuto Y, Israeli R, Gertner A. Accumulated effects of work under heat stress final report Beersheba. Beer Sheva Ben Gurion University of the Negev. 1980 [Google Scholar]
- 14.Gardner JW, Kark JA, Karnei K, et al. Risk factors predicting exertional heat illness in male marine corps recruits. Med Sci Sports Exerc. 1996;28:939–944. doi: 10.1097/00005768-199608000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Moore AC, Stacey MJ, Bailey KGH, et al. Risk factors for heat illness among British soldiers in the hot collective training environment. J R Army Med Corps. 2016;162:434–439. doi: 10.1136/jramc-2015-000427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Glitz KJ, Gorges W, Leyk D, Piekarski C. Arbeit unter klimatischer Belastung: Hitze LEITLINIE. In: Deutsche Gesellschaft für Arbeitsmedizin und Umweltmedizin e. V. (DGAUM) (ed.) Leitlinien der Deutschen Gesellschaft für Arbeitsmedizin und Umweltmedizin e. V. AWMF online - Das Portal der wissenschaftlichen Medizin. 2012 [Google Scholar]
- 17.Gaffin SL, Hubbard RW. Pandolf KB, Burr RE, editors. Pathophysiology of heatstroke Textbooks of military medicine. Volume 1: medical aspects of harsh environments. Falls Church: Office of the Surgeon General. 2001:161–208. [Google Scholar]
- 18.Glitz KJ, Leyk D. Der Schlag der Hitze Präventionsmaßnahmen eines Hitzemanagements. Wehrmed Wehrpharm. 2016;16:95–97. [Google Scholar]
- 19.Sawka MN, Pandolf KB. Pandolf KB, Burr RE, editors. Physical exercise in hot climates: physiology, performance, and biomedical issues Textbooks of military medicine. Volume 1: medical aspects of harsh environments. Falls Church: Office of the Surgeon General. 2001:87–133. [Google Scholar]
- 20.Rintamäki H, Rissanen S. Heat strain in cold. Ind Health. 2006;44:427–432. doi: 10.2486/indhealth.44.427. [DOI] [PubMed] [Google Scholar]
- 21.Di Prampero PE. Energetics of muscular exercise. Rev Physiol Biochem Pharmacol. 1981;89:143–222. doi: 10.1007/BFb0035266. [DOI] [PubMed] [Google Scholar]
- 22.Margaria R, Cerretelli P, Aghemo P, Sassi G. Energy cost of running. J Appl Physiol. 1963;18:367–370. doi: 10.1152/jappl.1963.18.2.367. [DOI] [PubMed] [Google Scholar]
- 23.Noakes TD. A modern classification of the exercise-related heat illnesses. J Sci Med Sport. 2008;11:33–39. doi: 10.1016/j.jsams.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 24.Smith J, Wallis L. Cooling methods used in the treatment of exertional heat illness. Br J Sports Med. 2005;39:503–507. doi: 10.1136/bjsm.2004.013466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spitzer H, Hettinger T, Kaminsky G. Beuth Verlag. Berlin, Köln: 1982. Tafeln für den Energieumsatz bei körperlicher Arbeit 6th edition. [Google Scholar]
- 26.Stegemann J. Leistungsphysiologie: Physiologische Grundlagen der Arbeit und des Sports. Stuttgart: Thieme. 1977 [Google Scholar]
- 27.Glitz KJ, Seibel U, Gorges W, Witzki A, Piekarski C, Leyk D. Reducing heat stress under thermal insulation in protective clothing: microclimate cooling by a ‘physiological’ method. Ergonomics. 2015;58:1461–1469. doi: 10.1080/00140139.2015.1013574. [DOI] [PubMed] [Google Scholar]
- 28.Dorman LE, Havenith G. The effects of protective clothing on energy consumption during different activities. Eur J Appl Physiol. 2009;105:463–470. doi: 10.1007/s00421-008-0924-2. [DOI] [PubMed] [Google Scholar]
- 29.Glitz KJ, Seibel U, Gorges W, Piekarski C, Leyk D. Gesundheit und Leistung im Klima 1. Mitteilung: Hitze. Wehrmed Mschr. 2011;55:290–294. [Google Scholar]
- 30.Lee JH, Kim YK, Kim KS, Kim S. Estimating clothing thermal insulation using an infrared camera. Sensors. 2016;16 doi: 10.3390/s16030341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yaglou CP, Minard D. Control of heat casualties at military training centers. AMA Arch Ind Health. 1957;16:302–316. [PubMed] [Google Scholar]
- 32.Stacey M, Woods D, Ross D, Wilson D. Heat illness in military populations: asking the right questions for research. J R Army Med Corps. 2014;160:121–124. doi: 10.1136/jramc-2013-000204. [DOI] [PubMed] [Google Scholar]
- 33.DIN (Deutsches Institut für Normung e. V) Beuth Verlag GmbH. Berlin: 2017. DIN EN ISO 7243: Ergonomie der thermischen Umgebung - Ermittlung der Wärmebelastung durch den WBGT-Index (wet bulb globe temperature); 13.100(7243) [Google Scholar]
- 34.Armstrong LE, Casa JD, Millard-Stafford M, Moran DS, Pyne WS, Roberts OW. Exertional heat illness during training and competition. Med Sci Sports Exerc. 2007;39:556–572. doi: 10.1249/MSS.0b013e31802fa199. [DOI] [PubMed] [Google Scholar]
- 35.Wenzel HG, Piekarski C. Bayerisches Staatsministerium für Arbeit und Sozialordnung. München: 1982. Klima und Arbeit. [Google Scholar]
- 36.Casa DJ, DeMartini JK, Bergeron MF, et al. National athletic trainers‘ association position statement: exertional heat illnesses. JAT. 2015;50:986–1000. doi: 10.4085/1062-6050-50.9.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Périard JD, Racinais S, Sawka MN. Adaptations and mechanisms of human heat acclimation: applications for competitive athletes and sports. Scand J Med Sci Sports. 2015;25:20–38. doi: 10.1111/sms.12408. [DOI] [PubMed] [Google Scholar]
- 38.Sawka MN, Castellani JW, Pandolf KB, Young AJ. Human adaptations to heat and cold stress. In: North Atlantic Treaty Organization (NATO), editor. RTO HFM Symposium on „Blowing Hot and Cold: Protecting Against Climatic Extremes“. Dresden: 2002. KN4-1-15. [Google Scholar]
- 39.Racinais S, Alonso JM, Coutts AJ, et al. Consensus recommendations on training and competing in the heat. Scand J Med Sci Sports. 2015;25:6–19. doi: 10.1111/sms.12467. [DOI] [PubMed] [Google Scholar]
- 40.Huonker M. Hitzeerkrankungen beim Sport - Prophylaxe und Therapie. Dtsch Z Sportmed. 2003;54:122–123. [Google Scholar]
- E1.Robine JM, Cheung SLK, Le Roy S, et al. Death toll exceeded 70,000 in Europe during the summer of 2003. C R Biol. 2008;331:171–178. doi: 10.1016/j.crvi.2007.12.001. [DOI] [PubMed] [Google Scholar]
- E2.Barriopedro D, Fischer EM, Luterbacher J, Trigo RM, García-Herrera R. The hot summer of 2010 Redrawing the temperature record map of Europe. Science. 2011;332:220–224. doi: 10.1126/science.1201224. [DOI] [PubMed] [Google Scholar]
- E3.Bund/Länder Ad-hoc Arbeitsgruppe, Gesundheitliche Anpassung an die Folgen des Klimawandels (GAK) Handlungsempfehlungen für die Erstellung von Hitzeaktionsplänen zum Schutz der menschlichen Gesundheit. Bundesgesundheitsblatt. 2017;60:662–672. doi: 10.1007/s00103-017-2554-5. [DOI] [PubMed] [Google Scholar]
- E4.Merte S. Estimating heat wave-related mortality in Europe using singular spectrum analysis. Climatic Change. 2017;142:321–330. [Google Scholar]
- E5.Deutscher Wetterdienst. Hitzewellen. www.dwd.de/DE/service/lexikon/Functions/glossar.html?lv2=101094&lv3=624852 (last accessed on 4 July 2019) [Google Scholar]
- E6.Sévellec F, Drijfhout SS. A novel probabilistic forecast system predicting anomalously warm 2018-2022 reinforcing the long-term global warming trend. Nat Commun. 2018;9 doi: 10.1038/s41467-018-05442-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E7.Åstrand PO, Rodahl K, editors. New York McGraw-Hill: 1986. Textbook of work physiology: physiological bases of exercise. [Google Scholar]
- E8.Nielsen M. Die Regulation der Körpertemperatur bei Muskelarbeit. Skand Arch Physiol. 1938;79:193–230. [Google Scholar]
- E9.Bittner MI. Auswirkungen von Hitzewellen auf die Mortalität in Deutschland [Effects of heat waves on mortality in Germany] Gesundheitswesen. 2014;76:508–512. doi: 10.1055/s-0033-1355404. [DOI] [PubMed] [Google Scholar]
- E10.Holst F. Konditionstraining unter Hitzeakklimatisation Kursbuch Reisemedizin. In: Jelinek T, editor. Georg Thieme Verlag. Stuttgart: 2012. pp. 276–277. [Google Scholar]
- E11.Armstrong LE, Maresh CM. The induction and decay of heat acclimatisation in trained athletes. Sports Med. 1991;12:302–312. doi: 10.2165/00007256-199112050-00003. [DOI] [PubMed] [Google Scholar]
- E12.Taylor NAS. Human heat adaptation. Compr Physiol. 2014;4:325–365. doi: 10.1002/cphy.c130022. [DOI] [PubMed] [Google Scholar]
- E13.Bytomski JR, Squire DL. Heat illness in children. Curr Sports Med Rep. 2003;2:320–324. doi: 10.1249/00149619-200312000-00007. [DOI] [PubMed] [Google Scholar]
- E14.Bar-Or O. Boileau RA, editor. Children and physical performance in warm and cold environments Advances in pediatric sport sciences. Vol 1: Biological issues. Champaign: Human Kinetics Publishers. 1984:117–130. [Google Scholar]
- E15.Müller S, Thöns M. Memorix Kindernotfälle. Stuttgart: Georg Thieme Verlag. 2019 [Google Scholar]
- E16.Falk B, Dotan R. Children’s thermoregulation during exercise in the heat—a revisit. Appl Physiol Nutr Metab. 2008,;33:420–427. doi: 10.1139/H07-185. [DOI] [PubMed] [Google Scholar]
- E17.Frye AJ, Kamon E. Sweating efficiency in acclimated men and women exercising in humid and dry heat. J Appl Physiol Respir Environ Exerc Physiol. 1983;54:972–977. doi: 10.1152/jappl.1983.54.4.972. [DOI] [PubMed] [Google Scholar]
- E18.Plowman SA, Smith DL. Lippincott Williams & Wilkins Health. Philadelphia: 1997. Exercise physiology for health, fitness, and performance 4th edition. [Google Scholar]
- E19.Shapiro Y, Pandolf KB, Avellini BA, Pimental NA, Goldman RF. Heat balance and transfer in men and women exercising in hot—dry and hot—wet conditions. Ergonomics. 1981;24:375–386. doi: 10.1080/00140138108924859. [DOI] [PubMed] [Google Scholar]
- E20.Sidman RD, Gallagher EJ. Exertional heat stroke in a young woman Gender differences in response to thermal stress. Acad Emerg Med. 1995;2:315–319. doi: 10.1111/j.1553-2712.1995.tb03229.x. [DOI] [PubMed] [Google Scholar]
- E21.Marsh SA, Jenkins DG. Physiological responses to the menstrual cycle: implications for the development of heat illness in female athletes. Sports Med. 2002;32:601–614. doi: 10.2165/00007256-200232100-00001. [DOI] [PubMed] [Google Scholar]
- E22.Heiden M, Muthers S, Niemann H, Buchholz U, Grabenhenrich L, Matzarakis A. Schätzung hitzebedingter Todesfälle in Deutschland zwischen 2001 und 2015 [Estimation of heat-related deaths in Germany between 2001 and 2015] Bundesgesundheitsblatt. 2019;62:571–579. doi: 10.1007/s00103-019-02932-y. [DOI] [PubMed] [Google Scholar]
- E23.Bouchama A, Dehbi M, Chaves-Carballo E. Cooling and hemodynamic management in heatstroke. Practical recommendations. Crit Care. 2007;11 doi: 10.1186/cc5910. R54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E24.Bunker A, Wildenhain J, Vandenbergh A, et al. Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly. A systematic review and meta-analysis of epidemiological evidence. EBioMedicine. 2016;6:258–268. doi: 10.1016/j.ebiom.2016.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E25.Siebert H, Uphoff H, Grewe HA. Monitoring hitzebedingter Sterblichkeit in Hessen [Monitoring heat-related mortality in Hesse] Bundesgesundheitsblatt. 2019;62:580–588. doi: 10.1007/s00103-019-02941-x. [DOI] [PubMed] [Google Scholar]
- E26.Herrmann A, Haefeli WE, Lindemann U, Rapp K, Roik P, Becker C. Hitzebedingte Gesundheitsschäden älterer Menschen - Epidemiologie und Prävention. Z Geront Geriat. 2019 doi: 10.1007/s00391-019-01594-4. Accepted for Publication. [DOI] [PubMed] [Google Scholar]
- E27.Fenske NA, Lober CW. Structural and functional changes of normal aging skin. J Am Acad Dermatol. 1986;15:571–585. doi: 10.1016/s0190-9622(86)70208-9. [DOI] [PubMed] [Google Scholar]
- E28.Tsuchida Y. Age-related changes in skin blood flow at four anatomic sites of the body in males studied by xenon-133. Plast Reconstr Surg. 1990;85:556–561. doi: 10.1097/00006534-199004000-00010. [DOI] [PubMed] [Google Scholar]
- E29.Bar-Or O. Effects of age and gender on sweating pattern during exercise. Int J Sports Med. 1998;19(Suppl 2):S106–S107. doi: 10.1055/s-2007-971970. [DOI] [PubMed] [Google Scholar]
- E30.Anderson RK, Kenney WL. Effect of age on heat-activated sweat gland density and flow during exercise in dry heat. J Appl Physiol. 1987;63:1089–1094. doi: 10.1152/jappl.1987.63.3.1089. [DOI] [PubMed] [Google Scholar]
- E31.Ho CW, Beard JL, Farrell PA, Minson CT, Kenney WL. Age, fitness, and regional blood flow during exercise in the heat. J Appl Physiol. 1997;82:1126–1135. doi: 10.1152/jappl.1997.82.4.1126. [DOI] [PubMed] [Google Scholar]
- E32.Braga AL, Zanobetti A, Schwartz J. The time course of weather-related deaths. Epidemiology. 2001;12:662–667. doi: 10.1097/00001648-200111000-00014. [DOI] [PubMed] [Google Scholar]
- E33.Flynn A, McGreevy C, Mulkerrin EC. Why do older patients die in a heatwave? QJM. 2005;98:227–229. doi: 10.1093/qjmed/hci025. [DOI] [PubMed] [Google Scholar]
- E34.Becker C, Haefeli WE, Herrmann A, Rapp K, Lindemann U. Prävention hitzebedingter Risiken bei älteren Menschen: Vermeidung von hitzebedingter Übersterblichkeit. ÄBW. 2018;47:362–363. [Google Scholar]
- E35.Vanakoski J, Seppälä T. Heat exposure and drugs A review of the effects of hyperthermia on pharmacokinetics. Clinical Pharmacokinetics. 1998;34:311–322. doi: 10.2165/00003088-199834040-00004. [DOI] [PubMed] [Google Scholar]
- E36.Westaway K, Frank O, Husband A, et al. Medicines can affect thermoregulation and accentuate the risk of dehydration and heat-related illness during hot weather. J Clin Pharm Ther. 2015;40:363–367. doi: 10.1111/jcpt.12294. [DOI] [PubMed] [Google Scholar]
- E37.Kraft U. Gesundheitsrisiken in Hitzeperioden. Fulda. 2015 [Google Scholar]
- E38.Lõhmus M. Possible biological mechanisms linking mental health and heat—a contemplative review. Int J Environ Res Public Health. 2018;15 doi: 10.3390/ijerph15071515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E39.Cheshire WP, Fealey RD. Drug-induced hyperhidrosis and hypohidrosis: incidence, prevention and management. Drug Saf. 2008;31:109–126. doi: 10.2165/00002018-200831020-00002. [DOI] [PubMed] [Google Scholar]
- E40.Ashburn MA, Ogden LL, Zhang J, Love G, Basta SV. The pharmacokinetics of transdermal fentanyl delivered with and without controlled heat. J Pain. 2003;4:291–297. doi: 10.1016/s1526-5900(03)00618-7. [DOI] [PubMed] [Google Scholar]
- E41.Bedno SA, Urban N, Boivin MR, Cowan DN. Fitness, obesity and risk of heat illness among army trainees. Occup Med. 2014;64:461–467. doi: 10.1093/occmed/kqu062. [DOI] [PubMed] [Google Scholar]
- E42.Armstrong LE, Crago AE, Adams R, Roberts WO, Maresh CM. Whole-body cooling of hyperthermic runners: comparison of two field therapies. Am J Emerg Med. 1996;14:355–358. doi: 10.1016/S0735-6757(96)90048-0. [DOI] [PubMed] [Google Scholar]
- E43.Fink E, Brandom BW, Torp KD. Heatstroke in the super-sized athlete. Pediatr Emerg Care. 2006;22:510–513. doi: 10.1097/01.pec.0000227388.91885.4b. [DOI] [PubMed] [Google Scholar]
- E44.Allen SB, Cross KP. Out of the frying pan, into the fire A case of heat shock and its fatal complications. Pediatr Emerg Care. 2014;30:904–910. doi: 10.1097/PEC.0000000000000296. [DOI] [PubMed] [Google Scholar]
- E45.Schultz J, Kenney WL, Linden AD. Heat-related deaths in American football An interdisciplinary approach. Sport Hist Rev. 2014;45:123–144. [Google Scholar]
- E46.Hawes R, McMorran J, Vallis C. Exertional heat illness in half marathon runners: experiences of the Great North Run. Emerg Med J. 2010;27:866–867. doi: 10.1136/emj.2010.090928. [DOI] [PubMed] [Google Scholar]
- E47.Coris EE, Ramirez AM, van Durme DJ. The dangerous combination of heat, humidity and exercise. Sports Med. 2004;34:9–16. doi: 10.2165/00007256-200434010-00002. [DOI] [PubMed] [Google Scholar]
- E48.Tennis Australia Limited. AO Heat Stress Scale a Grand Slam first. www.ausopen.com/articles/news/ao-heat-stress-scale-grand-slam-first (last accessed on 4 July 2019) [Google Scholar]
- E49.Fifa. Fifa Fussball-Weltmeisterschaft 2014: Abkühlpausen während der WM in Brasilien. https://de.fifa.com/worldcup/news/keeping-the-players-cool-at-brazil-2014-2369525-2369567 (last accessed on 4 July 2019) [Google Scholar]
- E50.Lucena RL, Steinke ET, Pacheco C, Vieira LL, Betancour MO, Steinke VA. The Brazilian World Cup: too hot for soccer? Int J Biometeorol. 2017;61:2195–2203. doi: 10.1007/s00484-017-1425-y. [DOI] [PubMed] [Google Scholar]
- E51.Kerr ZY, Marshall SW, Comstock RD, Casa DJ. Exertional heat stroke management strategies in United States high school football. Am J Sports Med. 2014;42:70–77. doi: 10.1177/0363546513502940. [DOI] [PubMed] [Google Scholar]
- E52.Kucera KL, Klossner D, Colgate B, Cantu RC. Annual survey of football injury research. American Football Coaches Association, Waco, Texas. 2016 [Google Scholar]
- E53.Glitz KJ, Gorges W, Leyk D, Piekarski C. Deutsche Gesellschaft für Arbeitsmedizin und Umweltmedizin e. V. (DGAUM), editor. Arbeit unter klimatischer Belastung: Isolierende Schutzbekleidung als Sonderfall einer Hitzebelastung. Leitlinien der Deutschen Gesellschaft für Arbeitsmedizin und Umweltmedizin e. V. AWMF online - Das Portal der wissenschaftlichen Medizin. 2012:1–16. [Google Scholar]
- E54.Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF (Leitlinienprogramm Onkologie) S3-Leitlinie Prävention von Hautkrebs, Langversion 1. 1, AWMF Registernummer: 032/052OL. 2014 [Google Scholar]
- E55.Drexler H. Schmitz-Spanke S, Nesseler T, Letzel S, Nowak D, editors. UV-Strahlung (Kapitel 43.1). Umweltmedizin. Neue Erkenntnisse aus Wissenschaft und Praxis. Landsberg am Lech: ecomed Medizin. 2017:296–305. [Google Scholar]
- E56.Cheshire WP. Thermoregulatory disorders and illness related to heat and cold stress. Auton Neurosci. 2016;196:91–104. doi: 10.1016/j.autneu.2016.01.001. [DOI] [PubMed] [Google Scholar]
- E57.Müller S. Hitzeschäden Memorix Notfallmedizin. In: Müller S, editor. Thieme Verlag. Stuttgart: 2017. pp. 312–317. [Google Scholar]
- E58.Pryor RR, Bennett BL, O‘Connor FG, Young JMJ, Asplund CA. Medical evaluation for exposure extremes: heat. Wilderness Environ Med. 2015;26:S69–S75. doi: 10.1016/j.wem.2015.09.009. [DOI] [PubMed] [Google Scholar]
- E59.Hahn JM. Hitzenotfälle Kurzlehrbuch Innere Medizin. In: Baenkler HW, Goldschmidt H, Hahn JM, et al., editors. Georg Thieme Verlag. Stuttgart: 2015. pp. 627–639. [Google Scholar]
- E60.Hufschmidt A, Lücking CH, Rauer S, Glocker FX. Georg Thieme Verlag. Stuttgart: 2017. Neurologie compact. [Google Scholar]
- E61.Santelli J, Sullivan JM, Czarnik A, Bedolla J. Heat illness in the emergency department. Keeping your cool. Emerg Med Pract. 2014;16:1–21. [PubMed] [Google Scholar]
- E62.Campell R. Sonnenstich und seine Folgen. Arch Gewerbepath Gewerbehyg. 1955;13:412–418. [Google Scholar]
- E63.Horn P. Über Sonnenstich mit organischen Symptomen. Dtsch Z Nervenheilkd. 1915;54:269–273. [Google Scholar]
- E64.Andreae S, Avelini P, Berg M, et al. Hitzekollaps/Hitzschlag LEXIKON der Krankheiten und Untersuchungen. In: Andreae S, Avelini P, Berg M, et al., editors. Georg Thieme Verlag. Stuttgart: 2008. 431 pp. [Google Scholar]
- E65.Howe AS, Boden BP. Heat-related illness in athletes. Am J Sports Med. 2007;35:1384–1395. doi: 10.1177/0363546507305013. [DOI] [PubMed] [Google Scholar]
- E66.Bergeron MF. Heat cramps during tennis: a case report. Int J Sport Nutr. 1996;6:62–68. doi: 10.1123/ijsn.6.1.62. [DOI] [PubMed] [Google Scholar]
- E67.Eichner ER. Treatment of suspected heat illness. Int J Sports Med. 1998;19:150–153. doi: 10.1055/s-2007-971983. [DOI] [PubMed] [Google Scholar]
- E68.Ganio MS, Casa DJ, Armstrong LE, Maresh CM. Evidence-based approach to lingering hydration questions. Clin Sports Med. 2007;26:1–16. doi: 10.1016/j.csm.2006.11.001. [DOI] [PubMed] [Google Scholar]
- E69.Stofan JR, Zachwieja JJ, Horswill CA, Murray R, Anderson SA, Eichner ER. Sweat and sodium losses in NCAA football players A precursor to heat cramps? Int J Sport Nutr Exerc Metabol. 2005;15:641–652. doi: 10.1123/ijsnem.15.6.641. [DOI] [PubMed] [Google Scholar]
- E70.Carter R, Cheuvront SN, Vernieuw CR, Sawka MN. Hypohydration and prior heat stress exacerbates decreases in cerebral blood flow velocity during standing. J Appl Physiol. 2006;101:1744–1750. doi: 10.1152/japplphysiol.00200.2006. [DOI] [PubMed] [Google Scholar]
- E71.Kenefick RW, Sawka MN. Heat exhaustion and dehydration as causes of marathon collapse. Sports Med. 2007;37:378–381. doi: 10.2165/00007256-200737040-00027. [DOI] [PubMed] [Google Scholar]
- E72.Leon LR, Helwig BG. Heat stroke: role of the systemic inflammatory response. J Appl Physiol. 2010;109:1980–1988. doi: 10.1152/japplphysiol.00301.2010. [DOI] [PubMed] [Google Scholar]
- E73.Epstein Y, Roberts WO. The pathopysiology of heat stroke An integrative view of the final common pathway. Scand J Med Sci Sports. 2011;21:742–748. doi: 10.1111/j.1600-0838.2011.01333.x. [DOI] [PubMed] [Google Scholar]
- E74.Epstein Y, Roberts WO, Golan R, Heled Y, Sorkine P, Halpern P. Sepsis, septic shock, and fatal exertional heat stroke. Curr Sports Med Rep. 2015;14:64–69. doi: 10.1249/JSR.0000000000000112. [DOI] [PubMed] [Google Scholar]
- E75.Casa DJ, Armstrong LE, Kenny GP, O‘Connor FG, Huggins RA. Exertional heat stroke: new concepts regarding cause and care. Curr Sports Med Rep. 2012;11:115–123. doi: 10.1249/JSR.0b013e31825615cc. [DOI] [PubMed] [Google Scholar]
- E76.Bouchama A, Knochel JP. Heat stroke. N Engl J Med. 2002;346:1978–1988. doi: 10.1056/NEJMra011089. [DOI] [PubMed] [Google Scholar]
- E77.Khogali M, Hales JRS, editors. Heat stroke and temperature regulation. Sydney: Academic Press. 1983 [Google Scholar]
- E78.Wilmore JH, Costill DL, Kenney WL. Physiology of sport and exercise 4th ed. Champaign, Ill.: Human Kinetics. 2008 [Google Scholar]
- E79.Pryor RR, Roth RN, Suyama J, Hostler D. Exertional heat illness: emerging concepts and advances in prehospital care. Prehosp Disaster Med. 2015;30:297–305. doi: 10.1017/S1049023X15004628. [DOI] [PubMed] [Google Scholar]
- E80.Krohn AR, Sikka R, Olson DE. Heat illness in football. Current concepts. Curr Sports Med Rep. 2015;14:463–471. doi: 10.1249/JSR.0000000000000212. [DOI] [PubMed] [Google Scholar]
- E81.Porcari J, Bryant C, Comano F. Exercise physiology. Philadelphia: F. A. Davis Company. 2015 [Google Scholar]
- E82.Henderson A, Simon JW, Melia WM, Navein JF, Mackay BG. Heat illness A report of 45 cases from Hong Kong. J R Army Med Corps. 1986;132:76–84. doi: 10.1136/jramc-132-02-03. [DOI] [PubMed] [Google Scholar]
- E83.Shibolet S, Coll R, Gilat T, Sohar E. Heatstroke: Its clinical picture and mechanism in 36 cases. Q J Med. 1967;36:525–548. [PubMed] [Google Scholar]
- E84.Adams WM, Hosokawa Y, Casa DJ. The timing of exertional heat stroke survival starts prior to collapse. Curr Sports Med Rep. 2015;14:273–274. doi: 10.1249/JSR.0000000000000166. [DOI] [PubMed] [Google Scholar]
- E85.Miller KC, Swartz EE, Long BC. Cold-water immersion for hyperthermic humans wearing American football uniforms. JAT. 2015;50:792–799. doi: 10.4085/1062-6050-50.6.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E86.Truxton TT, Miller KC. Can temperate-water immersion effectively reduce rectal temperature in exertional heat stroke? A critically appraised topic. J Sport Rehabil. 2017;26:447–451. doi: 10.1123/jsr.2015-0200. [DOI] [PubMed] [Google Scholar]
- E87.Gaudio FG, Grissom CK. Cooling methods in heat stroke. J Emerg Med. 2016;50:607–616. doi: 10.1016/j.jemermed.2015.09.014. [DOI] [PubMed] [Google Scholar]
- E88.Costrini A. Emergency treatment of exertional heatstroke and comparison of whole body cooling techniques. Med Sci Sports Exerc. 1990;22:15–18. [PubMed] [Google Scholar]
- E89.Miller KC, Truxton T, Long B. Temperate-water immersion as a treatment for hyperthermic humans wearing American football uniforms. JAT. 2017;52:747–752. doi: 10.4085/1062-6050-52.5.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E90.Zhang Y, Davis JK, Casa DJ, Bishop PA. Optimizing cold water immersion for exercise-induced hyperthermia. A meta-analysis. Med Sci Sports Exerc. 2015;47:2464–2472. doi: 10.1249/MSS.0000000000000693. [DOI] [PubMed] [Google Scholar]
- E91.Stewart TE, Whitford AC. Dangers of prehospital cooling: a case report of afterdrop in a patient with exertional heat stroke. J Emerg Med. 2015;49:630–633. doi: 10.1016/j.jemermed.2015.06.009. [DOI] [PubMed] [Google Scholar]
- E92.DeMartini JK, Casa DJ, Stearns R, et al. Effectiveness of cold water immersion in the treatment of exertional heat stroke at the Falmouth Road Race. Med Sci Sports Exerc. 2015;47:240–245. doi: 10.1249/MSS.0000000000000409. [DOI] [PubMed] [Google Scholar]
- E93.Butts CL, McDermott BP, Buening BJ, et al. Physiologic and perceptual responses to cold-shower cooling after exercise-induced hyperthermia. JAT. 2016;51:252–257. doi: 10.4085/1062-6050-51.4.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E94.Morrison KE, Desai N, McGuigan C, Lennon M, Godek SF. Effects of intravenous cold saline on hyperthermic athletes representative of large football players and small endurance runners. Clin J Sport Med. 2018;28:493–499. doi: 10.1097/JSM.0000000000000505. [DOI] [PubMed] [Google Scholar]
- E95.Taylor NAS, Caldwell JN, van den Heuvel AMJ, Patterson MJ. To cool, but not too cool. That is the question-immersion cooling for hyperthermia. Med Sci Sports Exerc. 2008;40 doi: 10.1249/MSS.0b013e31817eee9d. [DOI] [PubMed] [Google Scholar]
- E96.Casa DJ, McDermott BP, Lee EC, Yeargin SW, Armstrong LE, Maresh CM. Cold water immersion: the gold standard for exertional heatstroke treatment. Exerc Sport Sci Rev. 2007;35:141–149. doi: 10.1097/jes.0b013e3180a02bec. [DOI] [PubMed] [Google Scholar]
- E97.Proulx CI, Ducharme MB, Kenny GP. Effect of water temperature on cooling efficiency during hyperthermia in humans. J Appl Physiol. 2003;94:1317–1323. doi: 10.1152/japplphysiol.00541.2002. [DOI] [PubMed] [Google Scholar]
- E98.Amit D, Ran Y, Yuval H. Misdiagnosis of exertional heat stroke and improper medical treatment. Mil Med. 2011;176:1278–1280. doi: 10.7205/milmed-d-11-00104. [DOI] [PubMed] [Google Scholar]
- E99.Roberts WO. Exertional heat stroke and the evolution of field care. A physician‘s perspective. Temperature. 2017;4:101–103. doi: 10.1080/23328940.2017.1316352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E100.Proulx CI, Ducharme MB, Kenny GP. Safe cooling limits from exercise-induced hyperthermia. Eur J Appl Physiol. 2006;96:434–445. doi: 10.1007/s00421-005-0063-y. [DOI] [PubMed] [Google Scholar]
- E101.Holman ND, Schneider AJ. Multi-organ damage in exertional heat stroke. Neth J Med. 1989;35:38–43. [PubMed] [Google Scholar]
- E102.Heneghan HM, Nazirawan F, Dorcaratto D, et al. Extreme heatstroke causing fulminant hepatic failure requiring liver transplantation: a case report. Transplant Proc. 2014;46:2430–2432. doi: 10.1016/j.transproceed.2013.12.055. [DOI] [PubMed] [Google Scholar]
- E103.Wallace RF, Kriebel D, Punnett L, Wegman DH, Amoroso PJ. Prior heat illness hospitalization and risk of early death. Environ Res. 2007;104:290–295. doi: 10.1016/j.envres.2007.01.003. [DOI] [PubMed] [Google Scholar]
- E104.Hausfater P. Dantrolene and heatstroke: a good molecule applied in an unsuitable situation. Crit Care. 2005;9:23–24. doi: 10.1186/cc2939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E105.Leon LR, Bouchama A. Heat stroke. Compr Physiol. 2015;5:611–647. doi: 10.1002/cphy.c140017. [DOI] [PubMed] [Google Scholar]