Abstract
Background:
Increased immunoglobulin E (IgE) is associated with lower respiratory tract infections. The study aimed to evaluate the association between IgE and the rate of bronchopneumonia-related readmission within 12 months in children.
Methods:
A total of 1099 children aged over 1 year with bronchopneumonia, from 1 January 2015 to 31 December 2016, were enrolled. Unplanned readmissions within 12 months after discharge were observed. Multivariate regression analysis was used to identify independent risk factors for rehospitalization.
Results:
The rate of rehospitalization was 11.4% (125/1099). Compared to the nonreadmission children, IgE levels, the proportion of children with asthma and hospitalization duration were significantly higher in the readmission children (p < 0.05). Compared to the children with normal IgE (≤ 165 IU/ml) levels, the risk of rehospitalization was significantly higher in children with abnormal IgE [odds ratio (OR) 1.781, 95% confidence interval (CI) 1.209–2.624, p = 0.004]. Children with IgE level more than three times the upper limit had even higher risks of readmission (OR 2.037, 95%CI 1.172–3.540, p = 0.012). Meanwhile, the risk of readmission in children with abnormal IgE combined with or without bronchial asthma was significantly higher (OR 2.548 and 1.918, 95% CI 1.490–4.358 and 1.218–3.020, p = 0.001 and 0.005, respectively).
Conclusions:
Children aged over 1 year with bronchopneumonia who had higher IgE levels are at increased risk for rehospitalization within the first 12 months of the index hospitalization and IgE level may be used as a predictor of rehospitalization in children with bronchopneumonia.
Keywords: bronchial asthma, bronchopneumonia, immunoglobulin E, repeated hospitalization
Background
Bronchopneumonia, also known as lobular pneumonia, is the most common cause of hospitalizations in childhood. For children aged under 5 years in China, the incidence of bronchopneumonia ranged from 0.06 to 0.27 episodes per person-year, and the mortality rate was about 184–1223/100,000.1 Repeated hospitalizations with infectious disease increase the risk of hospital-acquired infection and increase the socioeconomic burden.2,3 Immunoglobulin E (IgE) is produced by plasma cells in the lamina propria of the nasopharynx, tonsils, bronchus, and gastrointestinal mucosa and mediates type I allergy,4 such as bronchial asthma4,5 and rhinitis,6,7 and is associated with the prevalence of lower airway infections.8 Children with asthma and chronic sinusitis have a significantly increased risk of bronchopneumonia and pneumonia,9,10 suggesting that IgE levels may be associated with the occurrence of bronchopneumonia.
There were several case reports showing that children with recurrent bronchopneumonia had high IgE levels,11,12 and that changes in IgE levels may correlate with the severity of bronchopneumonia in children.13 Meanwhile, children with bronchopneumonia, especially those with severe pneumonia, were often accompanied by immune dysfunction.14,15 The occurrence and development of lower respiratory tract diseases can be affected by dysfunction of immune system,16 which may lead to the recurrence of bronchopneumonia in children.
We speculated that the levels of IgE might be associated with repeated hospitalizations of bronchopneumonia in children. In the current study, the readmission rate of children with bronchopneumonia in 12 months following the index hospitalization was calculated; we further measured the plasma levels of IgE in children with bronchopneumonia and investigated the relationship between IgE levels and rehospitalization in children with bronchopneumonia.
Methods
Study populations
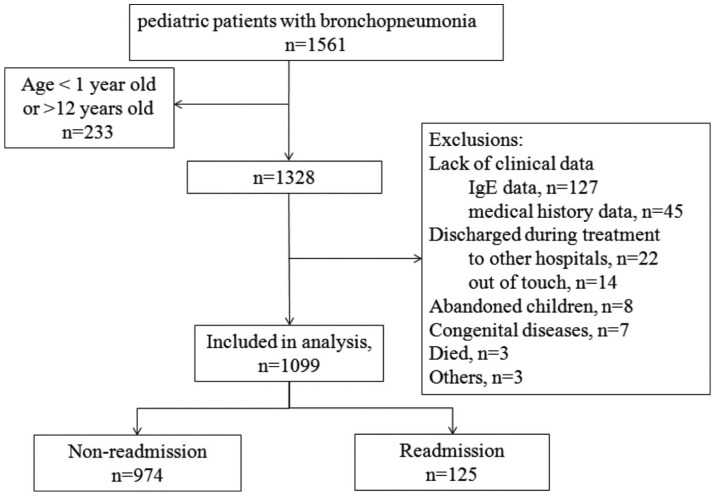
This study enrolled pediatric bronchopneumonia patients who were hospitalized between 1 January 2015 and 31 December 2016 at Minhang Branch, Zhongshan Hospital, Fudan University, Shanghai, China. The diagnosis of bronchopneumonia was usually based on the clinical features and supported by the chest radiography:17 (a) if cough persists for more than 1 week, tends to recur, or is accompanied by fever, or listening to the chest reveals abnormal breath sounds, such as crackles that suggest fluid in the lungs; (b) infection of the lower respiratory tract typically presents radiologically as multifocal bronchopneumonia or lobular pneumonia. Asthma was diagnosed according to the 2016 guideline for the diagnosis and optimal management of asthma in children.17 Inclusion criteria were: (a) the patients were between the ages of 1 and 12; (b) the first discharge diagnoses was registered as ‘bronchopneumonia’ or ‘lobular pneumonia’ in the hospital’s electronic medical records; (c) children who survived the index hospitalization. Exclusion criteria were: (a) children whose parents or guardians refused regular treatment for the children or had the children discharged from the hospital in advance; (b) children with incomplete medical records. The study flowchart is shown in Figure 1.
Figure 1.
Study flowchart.
IgE, immunoglobulin E.
The study was approved by the Ethics Committee of Minhang Branch, Zhongshan Hospital, Fudan University, Shanghai, and waived the need for formal patient consent because the retrospective study only used encrypted clinical data and presented no risk to participants.
Data collection
We initially collected demographic data; the number of hospitalizations within the first 12 months of the index hospitalization; dates and results of inpatient laboratory blood tests from the hospital’s electronic records. Readmission for bronchopneumonia within the first 12 months of the index hospitalization was identified in the hospital database or telephone follow up. Additional data were manually extracted including family history of allergy, comorbidities, and time from discharge to readmission. Comorbidities, including bronchial asthma, agranulocytosis, anemia, and acute otitis media (AOM), were diagnosed during the index hospitalization or previously.
The primary outcome of the study was bronchopneumonia-related readmission within 12 months. The rate of rehospitalization = (number of readmission patients within 12 months/number of discharged patients in the year) × 100%.
Laboratory studies
The blood biochemical test and infection marking in peripheral venous blood were detected within 24 h of admission using the Sysmex xs-800i automatic hematology analyzer (SYSMEX Corp., Kobe, Japan) and total bilirubin and alanine aminotransferase (ALT) were examined using a Vitros350 automatic biochemical analyzer (Johnson & Johnson, New Jersey, USA). High-sensitivity C-reactive protein (hs-CRP) was determined using avidin–biotin–horseradish peroxidase complex enzyme-linked immunosorbent assay (ABC-ELISA). IgE levels were measured using an IMMAGE800 specific protein analyzer (Beckman Coulter, Inc., California, USA). The normal range of IgE in our hospital was set up at ⩽165 IU/ml.
Statistical analyses
Data were analyzed using SPSS 19.0 (IBM, Chicago, IL, USA). Normally distributed data were expressed in mean ± standard deviation and we used the Student’s t test to compare the continuous data between two groups, include white blood cell count, hemoglobin, platelets, and length of stay. Non-normally distributed data were expressed in median (interquartile range, IQR) and compared using the nonparametric Mann–Whitney test, including hs-CRP, total bilirubin, ALT and IgE. Differences in trend of change were examined using the Jonckheere–Terpstra test.
For binary outcomes, associations between first inpatient available IgE during the index hospitalization and outcomes were estimated using univariate analysis. Age and sex, and all other variables with p < 0.15 in univariate analysis were entered into multivariate regression analysis. The association with IgE was estimated using multivariate logistic regression models and Kaplan–Meier survival curves. Sensitivity analyses were performed to estimate the associations between the IgE levels and the comorbidities, laboratory findings and hospitalization time, adjusting for sex and age, with a higher IgE level cut-off (>165 IU/ml, the upper limit of normal range). IgE levels were distributed according to quartile. The first quartile, the median and the third quartile were <32.3 IU/ml, 32.3–95 IU/ml, 95–251 IU/ml and ⩾251 IU/ml respectively; IgE levels were distributed into four categories with thresholds corresponding to equal or below the upper normal limit (UNL ⩽ 165 IU/ml), equal or below two times the UNL (165–330 IU/ml), equal or below three times the UNL (330–495 IU/ml) and higher than three times the UNL (>495 IU/ml), or by combining IgE and bronchial asthma: IgE ⩽ 165 IU/ml and without bronchial asthma, IgE ⩽ 165 IU/ml and with bronchial asthma, IgE > 165 IU/ml and without bronchial asthma and IgE > 165 IU/ml and with bronchial asthma. p < 0.05 was considered statistically significant.
Results
Patient demographic and baseline characteristics
In total, 1561 children with bronchopneumonia were hospitalized between 1 January 2015 and 31 December 2016. A total of 233 children, aged under 1 year or over 12 years were excluded. And 229 children were also excluded due to other causes, as detailed in the study flowchart (Figure 1). Finally, 1099 children were included in the analysis. In total, 125 (11.4%) children were readmitted for bronchopneumonia within the first 12 months of the index hospitalization. In the 125 readmitted children, the median time to first readmission was 5.1 months (IQR 2.6–7.7); the number of hospitalizations within the first 12 months of the index hospitalization were 2.4 ± 0.8, on average. Patient demographic and baseline characteristics are presented in Table 1. A significantly higher percentage (34.0%) of children in the readmission group had bronchial asthma versus children in the nonreadmission group (19.9%; p = 0.007). Children in the readmission group had significantly higher IgE levels [median (IQR): 144 (46–387)] versus children in the nonreadmission group [median (IQR): 87.6 (30.6–234); p < 0.001]. Children in the readmission group also had a noticeably higher times of hospitalizations, and longer duration compared with the nonreadmission group (p < 0.001). Children in the two groups were comparable in the demographic and other baseline variables (p > 0.05).
Table 1.
Patient demographic and baseline characteristics.
| Variables | All (n = 1099) | Nonreadmission (n = 974) | Readmission (n = 125) | p |
|---|---|---|---|---|
| Male, n (%) | 593 (54.0) | 528 (54.2) | 65 (52.0) | 0.641 |
| Median age, years (IQR) | 4 (3–6) | 4 (2–6) | 4 (3–6) | 0.078 |
| With medical insurance, n (%) | 1008 (91.7) | 896 (92.0) | 112 (89.6) | 0.361 |
| Family history of allergy, n (%) | ||||
| Yes | 85 (7.7) | 73 (7.5) | 12 (9.6) | 0.407 |
| Comorbidities, n (%) | ||||
| Bronchial asthma | 232 (21.1) | 194 (19.9) | 38 (34.0) | 0.007 |
| Allergic rhinitis | 39 (3.5) | 32 (3.3) | 7 (5.6) | 0.196 |
| Agranulocytosis | 28 (2.5) | 25 (2.6) | 3 (2.4) | 1.000 |
| Anemia | 6 (0.5) | 5 (0.5) | 1 (0.8) | 0.516 |
| AOM | 10 (0.9) | 9 (0.9) | 1 (0.8) | 1.000 |
| Laboratory findings | ||||
| WBC (mean ± SD, 109/l) | 7.49 ± 2.95 | 7.5 ± 3.0 | 7.2 ± 2.8 | 0.406 |
| HGB (mean ± SD, g/l) | 124.3 ± 10.0 | 124.6 ± 9.5 | 123.2 ± 11.5 | 0.159 |
| Platelets (mean ± SD, 109/l) | 339.5 ± 102.3 | 343.5 ± 103.7 | 327.1 ± 99.3 | 0.152 |
| Median hs-CRP (IQR), g/l | 4.2 (2.9–5.9) | 4.2 (2.8–5.8) | 5.0 (3.5–7.0) | 0.146 |
| Median total bilirubin (IQR), mmol/l | 5.1 (4.0–6.5) | 5.1 (4.0–6.5) | 5.4 (4.2–6.7) | 0.112 |
| Median ALT (IQR), U/l | 13 (11–16) | 13 (11–16) | 13 (11–15.5) | 0.592 |
| Median IgE (IQR), IU/ml | 95.8 (32.3–250) | 87.6 (30.6–234) | 144 (46–387) | <0.001 |
| Hospitalization time (mean ± SD, days) | 8.1 ± 2.4 | 8.0 ± 2.3 | 8.8 ± 3.1 | <0.001 |
ALT, alanine aminotransferase; AOM, acute otitis media; HGB, hemoglobin; hs-CRP, high-sensitivity C-reactive protein; IgE, immunoglobulin E; IQR, interquartile range; SD, standard deviation; WBC, white blood cell count.
The primary outcome
Children with abnormal IgE (>165 IU/ml) had a noticeably higher rate of bronchopneumonia-related readmission within 12 months versus those with normal IgE [16.0% versus 8.9%, p < 0.001; Figure 2(a)]. The 12-month readmission rate was 7.2%, 9.5%, 13.1% and 15.6% in the groups with the first quartile, the median, the third quartile, and highest IgE level, respectively [p < 0.001; Figure 2(b)]. The bronchopneumonia-related rate of readmission within 12 months was noticeably higher in children whose IgE levels were higher than three times the UNL (18.6%) versus those whose IgE levels were equal or below the UNL [8.9%, p < 0.001; Figure 2(c)]. Consistently, in children with abnormal IgE levels, those who had bronchial asthma, had a significantly higher rate of readmission than those without bronchial asthma [18.9% versus 14.6%, p < 0.001; Figure 2(d)].
Figure 2.
Bronchopneumonia-related rate of readmission within 12 months.
(a) The bronchopneumonia-related rate of readmission within 12 months is higher with higher IgE level (>165 IU/ml); (b) the trend for the readmission rate rises with increasing IgE level, from the lowest to highest quartile; (c) the readmission rate increased with the raised levels of IgE; (d) in children with abnormal IgE levels, those who had bronchial asthma, had a significantly higher rate of readmission than those without bronchial asthma.
IgE, immunoglobulin E.
Multivariate logistic regression analysis
Multivariate logistic regression analysis showed that abnormal IgE levels were a significant risk for readmission within 12 months versus normal IgE levels (adjusted OR 1.781, 95% CI 1.209–2.624, p = 0.004; Table 2). Compared with children whose IgE levels were in the first quartile, children whose IgE levels were in the third quartile had a significantly higher risk of 12-month readmission (adjusted OR 1.922 and 2.149, 95% CI 1.078–3.424 and 1.214–3.802, p = 0.027 and 0.009, respectively). Compared with those with normal IgE levels, children whose IgE levels were more than three times the UNL had a higher risk of readmission (adjusted OR 2.037, 95% CI 1.172–3.540, p = 0.012). At the same time, the risk of readmission was significantly higher in children with abnormal IgE and with bronchial asthma than in children with normal IgE levels and without bronchial asthma (adjusted OR 2.548 and 1.918, 95% CI 1.490–4.358 and 1.218–3.020, p = 0.001 and 0.005, respectively).
Table 2.
Logistic regression analysis of association between IgE levels and readmission.
| Variables | Crude |
Adjusted* |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| n | OR | 95% CI | p | OR | 95% CI | p | |||
| Lg(IgE) | 2.008 | 1.461 | 2.760 | <0.001 | 1.876 | 1.354 | 2.600 | <0.001 | |
| IgE (IU/ml) | |||||||||
| >165 | 381 | 1.948 | 1.338 | 2.835 | <0.001 | 1.781 | 1.209 | 2.624 | 0.004 |
| ⩽165 | 718 | Ref | Ref | ||||||
| IgE (IU/ml) | |||||||||
| ⩾251 | 275 | 2.372 | 1.356 | 4.151 | 0.002 | 2.149 | 1.214 | 3.802 | 0.009 |
| 95–25 | 274 | 1.936 | 1.090 | 3.439 | 0.024 | 1.922 | 1.078 | 3.424 | 0.027 |
| 32.3–95 | 274 | 1.342 | 0.730 | 2.466 | 0.343 | 1.364 | 0.741 | 2.511 | 0.319 |
| <32.3 | 276 | Ref | Ref | ||||||
| IgE (IU/ml) | |||||||||
| >495 (3 × UNL) | 118 | 2.342 | 1.379 | 3.977 | 0.002 | 2.037 | 1.172 | 3.540 | 0.012 |
| 330–495 (2 × UNL) | 109 | 1.758 | 0.975 | 3.169 | 0.061 | 1.623 | 0.893 | 2.950 | 0.112 |
| 165–330 (1 × UNL) | 154 | 1.794 | 1.075 | 2.994 | 0.025 | 1.712 | 1.022 | 2.869 | 0.041 |
| ⩽165 | 718 | Ref | Ref | ||||||
| IgE (IU/ml) | |||||||||
| >165 and with BA | 127 | 2.624 | 1.544 | 4.458 | <0.001 | 2.548 | 1.490 | 4.358 | 0.001 |
| >165 and without BA | 254 | 1.920 | 1.221 | 3.020 | 0.005 | 1.918 | 1.218 | 3.020 | 0.005 |
| ⩽165 and with BA | 105 | 1.732 | 0.920 | 3.261 | 0.089 | 1.731 | 0.917 | 3.264 | 0.090 |
| ⩽165 and without BA | 613 | Ref | Ref | ||||||
Adjusted: sex, age, or BA.
BA, bronchial asthma; CI, confidence interval; IgE, immunoglobulin E; Lg(IgE), log10IgE; OR, odds ratio; Ref, reference; UNL, upper normal limit.
The Kaplan–Meier analysis showed that patients with abnormal IgE had significantly higher risk of 12-months readmission than those with normal IgE [log-rank test, p < 0.001, Figure 3(a)]. With the IgE level increased, the risk of readmission was increased [log-rank test, p < 0.001, Figure 3(b)]. Consistently, compared with those whose IgE levels were equal or below the UNL, the risk of readmission was noticeably higher in children whose IgE levels were higher than three times the UNL [log-rank test, p < 0.001, Figure 3(c)]. Moreover, those who had bronchial asthma, had a significantly higher risk of readmission than those without bronchial asthma [log-rank test, p < 0.001, Figure 3(d)].
Figure 3.
IgE levels versus rates of readmission.
(a) The cumulative risk of readmission increases in a higher IgE level (>165 IU/ml); (b) The cumulative risk of readmission increases with the increasing of IgE level, from the lowest to highest quartile; (c) The cumulative risk of readmission was increasing with the raised levels of IgE; (d) In children with abnormal IgE levels, those who had bronchial asthma, had a significantly increased cumulative risk of readmission than those without bronchial asthma.
IgE, immunoglobulin E.
Discussion
This study showed that approximately 1 in 10 children was readmitted within the first 12 months of the index hospitalization. Furthermore, we found that higher IgE levels were an independent risk for repeated hospitalization within the first 12 months of the index hospitalization.
Bronchial pneumonia is one of the most common diseases in the pediatric emergency department. Unexpected repeated hospitalization in children has a serious negative impact on children and their families. Our study found that the incidence of repeated hospitalization within the first 12 months of the index hospitalization was as high as 11.4%, suggesting that the inpatient pediatric population with bronchopneumonia have a larger proportion of rehospitalization. Thus, it is necessary to actively identify risk factors that affect rehospitalization of children in order to provide timely intervention, thereby reducing the incidence of repeated hospitalization. Allergic diseases are known to be important contributors to the occurrence of pneumonia and aggravate the condition,18 and the level of IgE is closely related to the occurrence of allergic diseases.4 A study has found that repeated attacks of bronchial pneumonia in children are often accompanied by a significant increase in IgE levels,11,12 and our findings further support this conclusion. We demonstrated that IgE levels were significantly higher in children who were hospitalized repeatedly, so IgE levels in children with bronchopneumonia deserve more clinical attention.
This study found that regardless of how IgE levels were stratified in children, the incidence of repeated hospitalization within the first 12 months of the index hospitalization was significantly higher in those with higher IgE levels, indicating that physicians should pay more attention to IgE levels in children, and providing a new approach as to prevention of repeated hospitalization for this population of children. It also reminds caregivers of children with high IgE levels to take preventive measures in terms of life care, so as to avoid the occurrence of repeated hospitalization. We also found that when the IgE level exceeded three times of the UNL, the risk of repeated hospitalization within the first 12 months of the index hospitalization had a significant increase. Previous research showed that the concentration of pH in exhaled breath condensate was found to be decreased and related to airway inflammation in asthmatic patients.19 Children with bronchial asthma are often accompanied by the presence of bronchial pneumonia, pneumonia, and other diseases.10 The proportion of bronchial asthma in children with repeated hospitalization was significantly elevated. Further analysis revealed that high IgE levels were also an independent risk factor for repeated hospitalization even if the bronchial asthma was cured. If children with abnormal IgE levels have bronchial asthma, the risk of repeated hospitalization within the first 12 months of the index hospitalization is particularly significant, suggesting that for this group of children, while controlling bronchial asthma, attention should be paid to the IgE levels and the risk of recurrent bronchopneumonia.
Conclusion
Our study shows that IgE levels are strongly associated with repeat hospitalization within the first 12 months of the index hospitalization in children aged over 1 year with bronchopneumonia and may serve as a predictor of repeated hospitalization in this group of children. Based on the results of this study, it may provide a new basis for phenotypic classification of children with bronchopneumonia. Therefore, future studies should focus on the pathophysiological mechanisms of children with high IgE levels, and whether the intervention of such children can reduce the incidence of repeated hospitalization.
Limitation
Our study has several limitations. First, it is a retrospective study. The data were collected from the hospital’s electronic records and may have some omissions. Second, the diagnosis of bronchopneumonia is mainly based on the clinical features and is supported by chest radiography. Thus, bronchopneumonia may not be retrieved in full; the diagnosis of bronchopneumonia and asthma lacking a definitive laboratory test or biomarker acceptable to all disciplines; and the symptoms are nonspecific, so it is difficult to make a clear distinction between asthma and other lower respiratory tract infections, including bronchitis, bronchiolitis, and so on. Some studies suggest that the relationship between high IgE levels and the occurrence of pneumonia may be related essentially to the pneumonia caused by bronchial asthma.20 Children with high IgE levels in this study included some cases with underlying bronchial asthma, which may lead to bias. Another limitation of the study is that a healthy control group is lacking; all we see are correlation, we never see the causal relationship and seasonal variation, comorbidities. Lifestyle after the first episode may introduce biases, but this research is mainly to confirm the correlation between IgE levels and readmission, and the hope of attracting the clinical physician’s attention. Family history of allergy was taken from the parents’ retrospective history, which potentially may be incorrect; we do not expect those limitations to have biased our results. Another limitation was that not all children have etiologic diagnoses; when analyzing the subset of patients with etiologic diagnoses, the association between IgE and bronchopneumonia became stronger. Overall, our study shows that IgE may serve as a predictor of repeated hospitalization in children with bronchopneumonia. Our study generates some questions, and further studies are warranted.
Acknowledgments
Co-authors Cun You and Guo Ran contributed equally to this study.
We thank Qin Xu for data management and the study nurses, Jian ning Ma, Man Huang, Li ping Yu, and Jie Chen for data collection
Footnotes
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: this work was supported by the New Key Subjects of Jiading District (2017-ZD-03) and Science and Technology Commission of Minhang District (2019MHZ114), Shanghai Municipality.
Conflict of interest statement: The authors declare that they have no conflict of interest.
ORCID iD: Fei Wang  https://orcid.org/0000-0001-8908-5618
https://orcid.org/0000-0001-8908-5618
Contributor Information
Cun You, Department of Pediatrics, Minhang Branch, Zhongshan Hospital, Fudan University, Shanghai, China.
Guo Ran, Department of Anesthesiology, Eye, Ear, Nose, and Throat Hospital, Fudan University, Shanghai, China.
Xiao Wu, Emergency Department, Jiading District Central Hospital Affiliated Shanghai University of Medicine and Health Sciences, Shanghai, China.
Yu Wang, Jiuting Town Community Healthcare Center of Songjiang District, Shanghai, China.
Hua Tian, Jiuting Town Community Healthcare Center of Songjiang District, Shanghai, China.
Jiabao Fan, Department of Clinical Laboratory, Minhang Branch, Zhongshan Hospital, Fudan University, Shanghai, China.
Zezhong Yao, Department of pediatrics, Minhang Branch, Zhongshan Hospital, Fudan University, No.170, Xinsong Rd, Minhang, Shanghai 201199, China.
Fei Wang, Emergency Department, Jiading District Central Hospital Affiliated Shanghai University of Medicine & Health Sciences, No.1, Chengbei Rd, Jiading, Shanghai 201800, China.
References
- 1. Guan X, Silk BJ, Li W, et al. Pneumonia incidence and mortality in mainland China: systematic review of Chinese and English literature, 1985–2008. PLoS One 2010; 5: e11721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sun A, Netzer G, Small DS, et al. Association between index hospitalization and hospital readmission in sepsis survivors. Crit Care Med 2016; 44: 478–487. [DOI] [PubMed] [Google Scholar]
- 3. Dinh A, Le Monnier A, Emery C, et al. Predictors and burden of hospital readmission with recurrent Clostridioides difficile infection: a French nation-wide inception cohort study. Eur J Clin Microbiol Infect Dis 2019; 38: 1297–1305. [DOI] [PubMed] [Google Scholar]
- 4. Yu QN, Tan WP, Fan XL, et al. Increased group 2 innate lymphoid cells are correlated with eosinophilic granulocytes in patients with allergic airway inflammation. Int Arch Allergy Immunol 2018; 176: 124–132. [DOI] [PubMed] [Google Scholar]
- 5. Robledo Aceves M, Barron Balderas A, Jaime Ornelas ML. Most commonly isolated viruses in asthma exacerbation and their correlation with eosinophil and total serum immunoglobulin E levels. Arch Argent Pediatr 2018; 116: 192–197. [DOI] [PubMed] [Google Scholar]
- 6. Arasi S, Corsello G, Villani A, et al. The future outlook on allergen immunotherapy in children: 2018 and beyond. Ital J Pediatr 2018; 44: 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rondon C, Eguiluz-Gracia I, Campo P. Is the evidence of local allergic rhinitis growing? Curr Opin Allergy Clin Immunol 2018; 18: 342–349. [DOI] [PubMed] [Google Scholar]
- 8. De Lusignan S, Correa A, Pebody R, et al. Incidence of lower respiratory tract infections and atopic conditions in boys and young male adults: Royal College of General Practitioners Research and Surveillance Centre annual report 2015–2016. JMIR Public Health Surveill 2018; 4: e49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Palma SM, Palma RT, Catapani WR, et al. Predictive factors of hospitalization in children with acute asthma at a university emergency care unit. Pediatr Emerg Care 2013; 29: 1175–1179. [DOI] [PubMed] [Google Scholar]
- 10. Benevides GN, Salgado GA, Jr, Ferreira CR, et al. Bacterial sinusitis and its frightening complications: subdural empyema and Lemierre syndrome. Autops Case Rep 2015; 5: 19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Van de Vosse E, Van Dissel JT, Palamaro L, et al. The R156H variation in IL-12Rbeta1 is not a mutation. Ital J Pediatr 2013; 39: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Palamaro L, Giardino G, Santamaria F, et al. Interleukin 12 receptor deficiency in a child with recurrent bronchopneumonia and very high IgE levels. Ital J Pediatr 2012; 38: 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wang L, Chen Q, Shi C, et al. Changes of serum TNF-alpha, IL-5 and IgE levels in the patients of mycoplasma pneumonia infection with or without bronchial asthma. Int J Clin Exp Med 2015; 8: 3901–3906. [PMC free article] [PubMed] [Google Scholar]
- 14. Wong MT, Lambeck AJ, Van der Burg M, et al. Immune dysfunction in children with CHARGE syndrome: a cross-sectional study. PLoS One 2015; 10: e0142350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ishikawa H, Fukui T, Ino S, et al. Influenza virus infection causes neutrophil dysfunction through reduced G-CSF production and an increased risk of secondary bacteria infection in the lung. Virology 2016; 499: 23–29. [DOI] [PubMed] [Google Scholar]
- 16. Jesenak M, Banovcin P, Jesenakova B, et al. Pulmonary manifestations of primary immunodeficiency disorders in children. Front Pediatr 2014; 2: 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Subspecialty Group of Respiratory Diseases SoPCMA and Editorial Board CJoP. Guideline for the diagnosis and optimal management of asthma in children (2016). Zhonghua Er Ke Za Zhi 2016; 54: 167–181. [DOI] [PubMed] [Google Scholar]
- 18. Sanyal S, Baiz N, Charpin DA, et al. Variation in the association of Der p 1 and Der f 1 with asthma and rhinitis in 9–11-year-old schoolchildren: the French six cities study. Clin Exp Allergy 2018; 48: 745–748. [DOI] [PubMed] [Google Scholar]
- 19. Caffarelli C, Dascola CP, Peroni D, et al. Airway acidification in childhood asthma exacerbations. Allergy Asthma Proc 2014; 35: 51–56. [DOI] [PubMed] [Google Scholar]
- 20. Skaaby T, Husemoen LL, Thuesen BH, et al. IgE sensitization to inhalant allergens and the risk of airway infection and disease: a population-based study. PLoS One 2017; 12: e0171525. [DOI] [PMC free article] [PubMed] [Google Scholar]