Abstract
Background:
Osteochondral autograft transplantation (OAT) is usually performed for a defect that is <400 mm2 because of the limitations of autografts.
Purpose:
To present the surgical technique and clinical outcomes of OAT using the eyeglass technique for large osteonecrotic lesions of the femoral condyle (LOFs) (>400 mm2) with residual normal cartilage.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Cases (group 1) included 15 patients (18 knees) who underwent OAT using the eyeglass technique for LOFs with residual normal cartilage, while controls (group 2) included 11 patients (11 knees) who underwent OAT using the standard technique for small osteonecrotic lesions of the femoral condyle (≤400 mm2). Clinical outcomes were evaluated preoperatively and at the final follow-up (group 1, 56 months; group 2, 48 months) according to the International Knee Documentation Committee (IKDC) objective grade, the IKDC subjective score, and the Japanese Orthopaedic Association (JOA) score.
Results:
The mean lesion size was 685 mm2 in group 1 and 230 mm2 in group 2. Patients in group 1 had postoperative scores equivalent to those in group 2. The postoperative IKDC subjective scores in group 1 (mean, 86.9) and group 2 (mean, 87.0) showed no significant difference at the final follow-up (P = .653). For postoperative IKDC objective grades, 83.3% of group 1 and 81.8% of group 2 were graded as “nearly normal” or better, and no significant intergroup difference was found for the IKDC objective grade (P = .989). Also, no significant intergroup difference was found for the postoperative JOA score (group 1, 93.9; group 2, 81.4; P = .480). Nine second-look arthroscopic procedures were performed in group 1 compared with 4 in group 2, and all patients had plugs that were graded as “nearly normal” or better by the International Cartilage Repair Society classification system.
Conclusion:
The postoperative results of patients who underwent OAT using the eyeglass technique for large osteonecrotic lesions (>400 mm2) were equivalent to the results of patients who underwent OAT using the standard technique for small osteonecrotic lesions (≤400 mm2).
Keywords: osteochondral autograft transplantation, osteochondral autograft transfer, OAT, eyeglass technique, large osteonecrotic lesions
First described by Ahlbäck et al2 in 1968, osteonecrosis of the knee can be a devastating disease that leads to end-stage arthritis of the knee. Spontaneous osteonecrosis of the knee (SONK) is considered to be the most common form of osteonecrosis of the knee, and recent studies have reported incidences of 3.4% and 9.4% in patients older than 50 and 65 years, respectively.36 On the other hand, steroid-induced osteonecrosis of the femoral condyle is a relatively uncommon condition.22,38 The decision to treat is based largely on the size of the osteonecrotic area. Large lesions (>500 mm2) usually lead to condyle collapse.1,29
Various surgical techniques have been performed, such as high tibial osteotomy, unicompartmental knee arthroplasty (UKA), and total knee arthroplasty (TKA).11 However, patients who have progressed to subchondral collapse may benefit more from osteochondral autograft transplantation (OAT) because it allows for restoration of the cartilage surface. Some authors have reported good outcomes in patients who have undergone OAT for the treatment of SONK.8,40 OAT enables the restoration of articular cartilage, and cartilage regeneration is expected. However, as has been repeatedly reported in the literature,4,6,12,16,17,24,39 the prime indication for OAT is chondral or osteochondral lesions in the size range of 100 to 400 mm2. In these defects, OAT continues to provide good to excellent results in approximately 90% of cases. OAT requires multiple cylindrical autogenous osteochondral plugs that are usually taken from the less weightbearing joint area as a mosaic to fill the lesions for a resurfaced area. Therefore, it is usually performed for a defect that is <400 mm2 in size because of the limitations of autografts, and there may be some complications such as patellofemoral pain, hemarthrosis, and osteoarthritis at the graft donor site years later because of cylindrical cutting devices.15,23
The size of osteonecrotic lesions that require surgery is often >400 mm2. In such cases, and if normal articular cartilage in the recipient site can be used, we utilize the eyeglass technique26 to repair large lesions and to reduce the number of autogenous osteochondral plugs. The purpose of this retrospective study was to present the eyeglass technique and the clinical outcomes of OAT for large osteonecrotic lesions of the femoral condyle (LOFs) with residual normal cartilage. The clinical outcome of the eyeglass technique was compared with that of a control group that underwent OAT using the standard technique for small osteonecrotic lesions of the femoral condyle (≤400 mm2). We hypothesized that OAT using the eyeglass technique in patients with LOFs with residual normal cartilage would provide satisfactory clinical results at short-term to midterm follow-up.
Methods
This study was reviewed and approved by the research ethics committee of our hospital. A retrospective review was conducted of all surgical procedures performed at our 2 related institutions by 2 surgeons between September 1997 and April 2014. During that time, 18 knees (7 right, 11 left) of 15 patients (2 men, 13 women) underwent OAT using the eyeglass technique for LOFs with residual normal cartilage (group 1). Eleven controls (group 2) were selected from patients who underwent OAT using the standard technique for small osteonecrotic lesions of the femoral condyle (≤400 mm2) in the same period. Patient characteristics between the 2 groups are shown in Table 1.
TABLE 1.
Patient Characteristicsa
| Group 1 (n = 18) | Group 2 (n = 11) | P | |
|---|---|---|---|
| Age at surgery, y | 45.9 (21-73) | 65.8 (46-74) | .021b |
| Sex, male/female, n (%) | 2/16 (11/89) | 3/8 (27/73) | .620c |
| Side affected, right/left, n (%) | 7/11 (39/61) | 7/4 (64/36) | .109c |
| Follow-up period, mo | 56 (24-145) | 48 (25-128) | .081b |
| Osteonecrosis, n | 18 | 11 | |
| Recipient site, n | .005d | ||
| Medial femoral condyle | 9 | 11 | |
| Lateral femoral condyle | 9 | 0 | |
| Concomitant surgical procedure, n | |||
| High tibial osteotomy | 3 | 0 | |
| Meniscectomy | 0 | 0 | |
| Ligament reconstruction | 0 | 0 | |
| Lesion size, mm2 | 685 (420-1125) | 230 (110-360) | <.01b |
aData are shown as mean (range) unless otherwise indicated.
bP value by Mann-Whitney U test.
cP value by Fisher exact test.
dP value by chi-square test.
The study inclusion criteria were the following: (1) LOFs (>400 mm2) with residual normal cartilage in group 1 and small osteonecrotic lesions of the femoral condyle (≤400 mm2) without residual normal cartilage in group 2, (2) recipient site within the medial or lateral compartment of the knee joint, and (3) cases that had been treated with conservative measures (such as analgesia, weight loss, modification of activity, and knee exercise program) for more than 3 months before surgery. The exclusion criterion in both groups was a kissing tibial osteochondral lesion classified as grade 4 according to the International Cartilage Repair Society (ICRS) classification system5 and with a of size >400 mm2.
For LOFs, if articular cartilage in the recipient site was damaged, removing the damaged articular cartilage and curettage of necrotic bone in the recipient site were performed, and we filled plugs at intervals of a few millimeters to cover the lesions.
Second-look arthroscopic surgery was offered to all patients, and only 13 patients consented. Then, it was performed in 9 group 1 knees and 4 group 2 knees. The mean interval between procedures was 12.4 ± 1.0 months. We assessed the condition of the cartilage by visual inspection and probing, along with the ICRS classification system. All patients had more than 2 years of follow-up and were examined. The follow-up rate in this study was 100%.
Preoperative knee radiographs were evaluated, and the extent of the osteochondral lesion was assessed on magnetic resonance imaging (MRI). Long-leg weightbearing alignment radiographs were taken to evaluate abnormal alignment.
Surgery
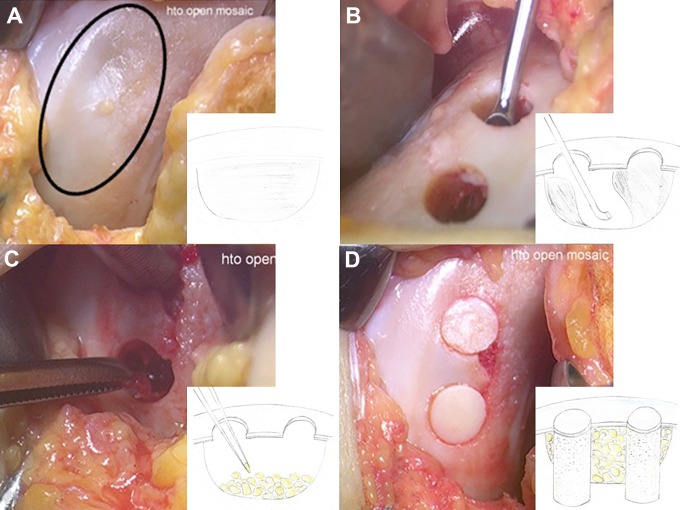
All operative procedures were performed using the Osteochondral Autograft Transfer System (OATS; Arthrex). Under general anesthesia, knee arthroscopic surgery was performed initially. Then, the eyeglass technique was performed in group 1 by the open approach. The medial parapatellar approach was used when the recipient site was the medial femoral condyle, and if the recipient site was the lateral femoral condyle, a lateral parapatellar approach was used. The size of the osteochondral lesion and that of residual normal cartilage were measured (Figure 1A). One or 2 osteochondral holes were excavated from the recipient site where the articular cartilage survived, and necrotic bone around the holes was curetted using the holes (Figure 1B). Iliac bone chips were implanted into the recipient area using the holes (Figure 1C), and autologous osteochondral plugs harvested from less weightbearing areas (∼10 mm from the lateral or medial edges of the trochlea) were then implanted into the holes (Figure 1D). For patients in group 2, OAT was performed with the standard open technique. Removing the damaged articular cartilage and curettage of necrotic bone in the recipient site were performed, and osteochondral grafts were transplanted from the donor site to the recipient site.
Figure 1.
(A) A large osteonecrotic lesion with residual normal cartilage (circle) on the medial condyle of the left knee. (B) Two osteochondral holes are excavated from the recipient site where the articular cartilage survived, and the necrotic subchondral bone is curetted using the holes. (C) Iliac bone chips are implanted into the recipient area using the holes. (D) Autologous osteochondral plugs harvested from the medial and lateral trochleae are then implanted into the holes.
In both groups, the location and depth of the osteonecrotic area were measured preoperatively using MRI, and the length of the implanted osteochondral plug was 5 mm more than the depth of osteonecrosis. To obtain a smooth surface, osteochondral plugs were transplanted perpendicular to the articular surface of the femoral condyle, and care was taken to not protrude plugs >1 mm in height. The plug elevation height was measured with a ruler. Finally, normal cancellous bone collected from around the recipient site was transplanted to the bottom of donor defects.
There were no patients in the present series with meniscal injuries or ligament instability. Although a kissing tibial osteochondral lesion of ICRS grade 4 was observed in 7 knees in group 1 (100-225 mm2), OAT was not performed for the tibial lesions. High tibial osteotomy was combined with OAT for a varus knee in 3 knees in group 1 because the femorotibial angle was >180° (6°-9° or more of varus).
The same postoperative protocol was performed in both groups. Continuous passive motion of the knee was started from the third postoperative day after removal of the drain tube. Partial one-third weightbearing was allowed in the fourth week, weightbearing was then gradually increased step by step, and full weightbearing was allowed in the seventh week after surgery.
Clinical Evaluations
Clinical outcomes were evaluated preoperatively and postoperatively according to the International Knee Documentation Committee (IKDC) objective grade, the IKDC subjective score, and the Japanese Orthopaedic Association (JOA) score.32 The JOA score evaluates 4 items: ability to walk (30 points), ability to climb up and down stairs (25 points), range of motion (35 points), and joint swelling (10 points). Each knee joint can achieve a maximum of 100 points. A validation study for the JOA score was conducted by Okuda et al,35 who found that it was significantly correlated with validated patient-rated outcome measures (Japanese Knee Osteoarthritis Measure, Short Form Health Survey–36), indicating concurrent validity of the JOA score. For the morphological evaluation, the Kellgren and Lawrence (KL) classification system21 and the modified magnetic resonance observation of cartilage repair tissue (MOCART) score25 were used. The ICRS score was recorded when second-look arthroscopic surgery was performed. The assessment of donor site morbidity was based on the patellar compression test and complaints of anterior knee pain.
Statistical Analysis
The Mann-Whitney U test was used to compare the numerical data (ie, age, recipient area, IKDC subjective score, and JOA score) between the 2 groups. The Fisher exact test was used to compare the contingency table between the 2 groups (ie, sex and side). The chi-square test was used to evaluate the distribution of more than 3 categories (ie, IKDC objective grade, number of transplanted plugs, ICRS grade). P values <.05 were considered significant.
Results
The preoperative IKDC subjective score, IKDC objective grade, and JOA score were not significantly different between the 2 groups (Table 2). Patients in group 1 had postoperative scores equivalent to those in group 2 (Table 3). The postoperative IKDC subjective scores of group 1 (mean, 86.9) and group 2 (mean, 87.0) showed no significant difference at the final follow-up (P = .653). For postoperative IKDC objective grades, 83.3% of group 1 and 81.8% of group 2 were graded as “nearly normal” or better, and no significant intergroup difference was found in the IKDC objective grade (P = .989). Also, no significant intergroup difference was found in the postoperative JOA score (group 1, 93.9; group 2, 81.4; P = .480). Three patients in group 1 underwent a bilateral procedure, and there was no difference in clinical outcomes compared with patients who underwent a unilateral procedure.
TABLE 2.
Preoperative Outcome Scoresa
| Group 1 (n = 18) | Group 2 (n = 11) | P | |
|---|---|---|---|
| IKDC subjective score | 33.6 (16.9-51.2) | 42.4 (36.8-51.0) | .183b |
| IKDC objective grade, n | .113c | ||
| Normal | 0 | 0 | |
| Nearly normal | 0 | 0 | |
| Abnormal | 10 | 10 | |
| Severely abnormal | 8 | 1 | |
| JOA score | 61.7 (45.0-80.0) | 55.0 (50.0-90.0) | .261b |
aData are shown as mean (range) unless otherwise indicated. IKDC, International Knee Documentation Committee; JOA, Japanese Orthopaedic Association.
bP value by Mann-Whitney U test.
cP value by chi-square test.
TABLE 3.
Postoperative Outcome Scoresa
| Group 1 (n = 18) | Group 2 (n = 11) | P | |
|---|---|---|---|
| IKDC subjective score | 86.9 (51.9-93.5) | 87.0 (74.6-95.4) | .653b |
| IKDC objective grade, n | .989c | ||
| Normal | 8 | 5 | |
| Nearly normal | 7 | 4 | |
| Abnormal | 3 | 2 | |
| Severely abnormal | 0 | 0 | |
| JOA score | 93.9 (85.0-100.0) | 81.4 (65.0-100.0) | .480b |
| Donor site morbidity, n | 0 | 0 |
aData are shown as mean (range) unless otherwise indicated. IKDC, International Knee Documentation Committee; JOA, Japanese Orthopaedic Association.
bP value by Mann-Whitney U test.
cP value by chi-square test.
The mean number of harvested plugs in group 1 and group 2 was 3.3 ± 0.9 and 2.4 ± 0.5, respectively. The mean diameter of harvested plugs was 8.4 ± 0.7 mm in both group 1 and group 2. When the total number of transplanted plugs was considered, more plugs were transplanted in group 1 than in group 2 (P = .048) because more osteochondral holes were needed to curette the widespread necrotic bone (Table 4). There was no donor site morbidity in either group.
TABLE 4.
Lesion Size and Number of Plugs
| Group 1 | Group 2 | ||||
|---|---|---|---|---|---|
| Knee | Lesion Size, mm2 | No. of Plugs | Knee | Lesion Size, mm2 | No. of Plugs |
| 1 | 1025 | 4 | 1 | 136 | 2 |
| 2 | 1125 | 4 | 2 | 300 | 3 |
| 3 | 700 | 4 | 3 | 300 | 3 |
| 4 | 456 | 2 | 4 | 300 | 3 |
| 5 | 900 | 4 | 5 | 150 | 2 |
| 6 | 750 | 4 | 6 | 150 | 2 |
| 7 | 600 | 4 | 7 | 360 | 3 |
| 8 | 420 | 2 | 8 | 216 | 2 |
| 9 | 425 | 2 | 9 | 264 | 2 |
| 10 | 800 | 4 | 10 | 240 | 2 |
| 11 | 1050 | 4 | 11 | 110 | 2 |
| 12 | 825 | 4 | |||
| 13 | 450 | 2 | |||
| 14 | 630 | 4 | |||
| 15 | 500 | 3 | |||
| 16 | 450 | 2 | |||
| 17 | 800 | 4 | |||
| 18 | 420 | 2 | |||
Second-look arthroscopic surgery was performed in 9 group 1 knees and 4 group 2 knees. The condition of the transplanted plugs was acceptable in both groups (Table 5). All plugs showed good survival with a grade of “nearly normal” or better according to the ICRS classification system. No significant intergroup differences were found in the ICRS grade at the midterm follow-up (P = .488). The kissing tibial lesions in the 7 knees in group 1 were unchanged at second-look arthroscopic surgery.
TABLE 5.
ICRS Classification During Second-Look Arthroscopic Surgerya
| Group 1 (n = 9) | Group 2 (n = 4) | P | |
|---|---|---|---|
| Timing of second-look surgery, mean (range), mo | 12.2 (8-14) | 12.8 (12-13) | .936b |
| ICRS grade, n | .488c | ||
| Grade 1, normal | 1 | 0 | |
| Grade 2, nearly normal | 8 | 4 | |
| Grade 3, abnormal | 0 | 0 | |
| Grade 4, severely abnormal | 0 | 0 |
aICRS, International Cartilage Repair Society.
bP value by Mann-Whitney U test.
cP value by chi-square test.
Donor sites were filled with fibrous cartilage-like tissue, and kissing lesions of the patella were not observed. With the numbers used in this study, there was no significant difference in clinical results between the knees with an ICRS grade 4 kissing tibial lesion and the knees with a kissing tibial lesion of grade ≤3 (IKDC subjective score: P = .653; IKDC objective grade: P = .761; JOA score: P = .628).
In group 1, the KL classification was unchanged in 17 knees (7 normal, 10 grade 2) and improved in 1 knee (from grade 3 to 2). The mean modified MOCART score was 57.5 (range, 40-65) at 12-month follow-up. At the latest physical examination (mean, 56 months [range, 24-145 months]), the mean postoperative range of motion of the knee was 143.6° (flexion range, 135°-150°) and 0° (extension range, 0° in all knees), and the rate of the ability to sit straight in the Japanese style, with legs folded under, was increased from 38.9% (7/18) preoperatively to 61.1% (11/18) postoperatively.
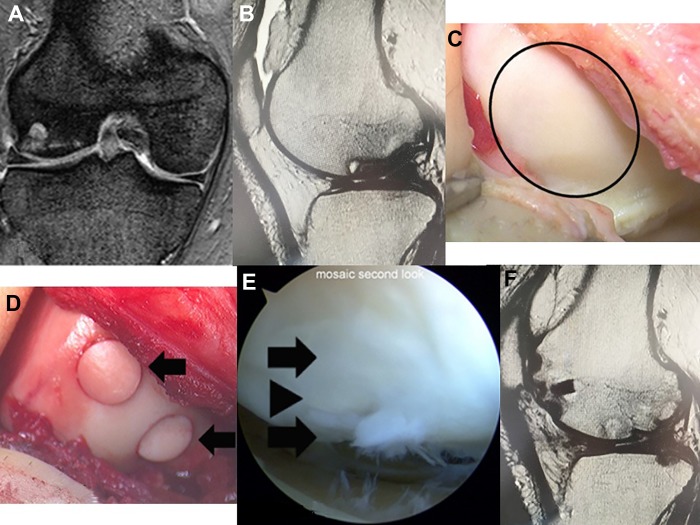
One case in group 1 is presented. The patient was a 54-year-old man in whom the lateral femoral condyle of the right knee had spontaneous osteonecrosis. Preoperative T2-weighted MRI showed an LOF (Figure 2, A and B). His preoperative IKDC objective grade, IKDC subjective score, and JOA score were severely abnormal, 41.3, and 60, respectively. The size of the osteochondral lesion was 800 mm2, and the overlying cartilage appeared normal (Figure 2C). The eyeglass technique was performed. Three osteochondral plugs, 10 mm in diameter, were implanted in the recipient site (Figure 2D). At 42 months after surgery, his postoperative IKDC objective grade, IKDC subjective score, and JOA score were improved to nearly normal, 77.3, and 90, respectively. Second-look arthroscopic surgery was performed 14 months after surgery. Normal cartilage was preserved between the transplanted osteochondral plugs in the recipient site (Figure 2E). His ICRS score was 9. Postoperative T2-weighted MRI at 1 year showed a smooth articular cartilage surface and no recurrence of osteonecrosis (Figure 2F).
Figure 2.
A 54-year-old male patient in group 1. (A, B) Preoperative T2-weighted magnetic resonance imaging (MRI) shows a large osteonecrotic lesion on the lateral femoral condyle of the right knee. (C) The size of the osteonecrotic lesion is 800 mm2 (circle) and the overlying cartilage appears normal. (D) Three osteochondral plugs (arrows) are implanted on the border of the lesion. (E) Arthroscopic view of the recipient site 14 months after surgery. Normal cartilage (arrowhead) is preserved between the transplanted osteochondral plugs (arrows). (F) Postoperative T2-weighted MRI at 1 year shows a smooth articular cartilage surface and no recurrence of osteonecrosis.
Discussion
In past reports on the size of osteonecrotic lesions,1,28 small lesions (<350 mm2) usually regress with nonsurgical management, medium lesions (350-500 mm2) may or may not regress, and large lesions (>500 mm2) usually lead to condyle collapse. Juréus et al20 evaluated long-term outcomes in relation to the need for major knee surgery in a cohort of 40 patients with osteonecrosis of the knee. After 27-month follow-up, 15 of the 40 patients required arthroplasty, and 2 required osteotomy. The majority of patients (6/7) who had a lesion of >40% of the affected femoral condyle required a knee prosthesis, whereas none of the 10 patients with <20% of the femoral condyle affected required surgery.20 Therefore, we performed OAT in patients who presented with LOFs. Within the limits of this study, the postoperative results of patients who underwent OAT using the eyeglass technique for large osteonecrotic lesions (>400 mm2) were equivalent to the results of patients who underwent OAT using the standard technique for small osteonecrotic lesions (≤400 mm2).
The main advantages of OAT are the reconstruction of the mechanically durable articular bone plate and articular cartilage and the removal of collapsed tissue. Tanaka et al40 reported on 6 patients with SONK who underwent OAT; all patients reported favorable pain relief after a mean follow-up of 28 months. Similarly, Duany et al8 reported excellent outcomes with a mean Knee Society Score of 85 points in 9 patients who underwent OAT for the treatment of SONK. With respect to OAT for steroid-induced osteonecrosis, Nakagawa et al31 reported 1 case and Fujita et al10 reported 3 cases, and their outcomes were good. Although OAT is typically used for defects of >400 mm2, Hangody et al15 reported that usually both of the patellofemoral peripheries allow graft harvest for a defect of 300 to 400 mm2. OAT can therefore be used for lesions as large as 800 to 900 mm2 as a salvage procedure, but such an extension of the indication can result in a higher rate of donor site morbidity. For large lesions, Gudas et al12 have performed several additional investigations, including a 10-year follow-up study, which also supported the notion that a size >200 mm2 is associated with a higher risk of failure.
The size of osteonecrotic lesions requiring surgery is often <400 mm2. If articular cartilage in the recipient site cannot be used, we fill plugs at intervals of a few millimeters to cover LOFs. In this way, Nakagawa et al31 reported a case of steroid-induced osteonecrosis of the femoral condyle measuring 1000 mm2 treated by OAT with a satisfactory result. The use of allografts may also be effective. Yet, we cannot use allogenic osteochondral transplantation in our country.
When articular cartilage in the recipient site can be used, we utilize the eyeglass technique to repair LOFs and to reduce the number of autogenous osteochondral plugs. However, there is only 1 report regarding the eyeglass technique for LOFs with residual normal cartilage,26 and its long-term results are unknown. Therefore, this report presented 18 knees of 15 patients who had LOFs with residual normal cartilage treated successfully with the eyeglass technique. Although the mean lesion size was >400 mm2, all patients achieved satisfactory results during the mean 56-month follow-up period; moreover, the postoperative results of patients who underwent OAT using the eyeglass technique for LOFs were equivalent to the results of patients who underwent OAT using the standard technique for small osteonecrotic lesions. In previous studies, OAT for small lesions has been reported to have good to excellent results in approximately 90% of cases. Therefore, we believe that the eyeglass technique for LOFs is also effective.
Although it was not possible to confirm pathological tissue, second-look arthroscopic surgery showed that normal cartilage was stable between transplanted osteochondral plugs in the recipient sites (mean ICRS score, 11.7), and the residual normal cartilage seemed stable on MRI in all cases. Because the clinical results were also good, we believe that the residual normal cartilage was preserved.
Forming a smooth joint surface is important to achieve satisfactory results. Therefore, osteochondral plugs were transplanted perpendicular to the articular surface. McCoy and Miniaci27 reported that graft prominence of >1 mm is poorly tolerated. Nakagawa et al33 reported that isolated osteochondral plug depression of <1 mm could still promote acceptable cartilage healing, leading to good clinical outcomes. Johnson and LaPrade19 also reported that a proud plug had a negative effect on kissing lesions of the medial tibial plateau. Therefore, we are careful not to protrude plugs >1 mm in height.
With regard to donor site morbidity, Filardo et al9 noted a correlation between the number of plugs and IKDC scores (P = .05), with a mean IKDC score of approximately 85 for patients with 1 plug and a mean score of 50 for patients with 4 plugs. We think that the eyeglass technique is very useful in that the number of plugs can be decreased. In the present study, the mean number of plugs was 3.3, and the mean diameter of the plugs was 8.4 mm. However, there was no donor site morbidity. One of the reasons for this might be that the normal cancellous bone collected from around the recipient site was transplanted to the bottom of donor defects. In this way, it appears that this approach provides favorable conditions for the growth of good fibrocartilage-like tissue at the donor site.
Other surgical treatments for osteonecrosis have been reported, including core decompression, UKA, and TKA. The eyeglass technique seems analogous to extra-articular core decompression with bone grafting, which has also been used to treat SONK. This is because both techniques are used to remove necrotic bone and place new bone within the osteonecrotic lesions. However, patients who have progressed to subchondral collapse may benefit more from an osteochondral autograft because of restoration of the cartilage surface. In UKA for SONK, some authors reported that 96.3% of patients were satisfied at 27-month follow-up,13 10-year survivorship was 89%,7 and 15-year survivorship was 90.6%.18 In TKA for SONK, a study by Mont et al29 involving 30 patients reported a 97% survival rate at a mean follow-up of 108 months. Radke et al37 reported that patients who underwent TKA showed clinically better results than those who underwent UKA at more than 5-year follow-up. However, OAT was superior to TKA and UKA in range of motion of the knee.
We aim for the patient being able to sit straight in the Japanese style after knee surgery because being able to do so is still very important for the Japanese lifestyle. Niki et al34 studied the ability to sit in the Japanese style after TKA and found that 23 patients (29 knees) of a series of 463 total knee replacements in 341 patients were able to sit in the Japanese style. Mukai et al30 showed that in OAT only for osteonecrosis of the knee joints, the rate of the ability to sit in the Japanese style was 0% preoperatively and 65% at follow-up. In the present study, this same rate increased from 38.9% preoperatively to 61.1% postoperatively. Therefore, we select OAT as much as possible instead of UKA or TKA.
Whether OAT has a preventive effect on osteoarthritis progression is under discussion. Hangody et al14 documented the results of OAT as a salvage intervention in 82 athletes with osteoarthritis of the knee. During the 9.6-year follow-up, slight or moderate degenerative changes (Fairbank grade 1 or 2) were seen preoperatively in 27% of the cases and at follow-up in 36% of the cases. Fairbank grade 3 changes were observed in 5 cases, with an average radiographic deterioration of 0.32 on the Fairbank scale (preoperative, 0.34; postoperative, 0.66). In the present study, the postoperative radiographs of the knee joints showed that the KL classification was unchanged in 17 knees and improved in 1 knee. We think that the knee joint space was widened by the thickness of the implanted cartilage.
Limitations
The first limitation of this study was that it was retrospective. Second, the number of patients was small (18 knees in 15 patients). Third, the present series included various stages of osteoarthritis. This is because of the relative rarity of LOFs with residual normal cartilage. Fourth, we could not completely match the patients’ background in the 2 groups because we selected only osteonecrotic lesions of the femoral condyle. Primarily, the control group was older by a mean of 20 years. As for the population normative values for the IKDC score, Anderson et al3 reported that mean scores were determined for women aged 35 to 50 years (mean, 80 ± 23 years) and 51 to 65 years (mean, 71 ± 26 years). Fifth, the ICRS grade was missing for 16 of the 29 knees. Last, follow-up was medium term (mean of 56 months for group 1). A greater number of patients with long-term follow-up is needed.
Conclusion
Although with the condition that the patients in the second group were significantly older, the postoperative results of patients who underwent OAT using the eyeglass technique for large osteonecrotic lesions (>400 mm2) were equivalent to those of patients who underwent OAT using the standard technique for small osteonecrotic lesions (≤400 mm2). Therefore, if the residual normal cartilage in the recipient site has been preserved, the eyeglass technique may be used.
Footnotes
The authors have declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Kyoto Medical Center Ethics Committee.
References
- 1. Aglietti P, Insall JN, Buzzi R, Deschamps G. Idiopathic osteonecrosis of the knee: aetiology, prognosis and treatment. J Bone Joint Surg Br. 1983;65:588–597. [DOI] [PubMed] [Google Scholar]
- 2. Ahlbäck S, Bauer GC, Bohne WH. Spontaneous osteonecrosis of the knee. Arthritis Rheum. 1968;11:705–733. [DOI] [PubMed] [Google Scholar]
- 3. Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ. The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. Am J Sports Med. 2006;34:128–135. [DOI] [PubMed] [Google Scholar]
- 4. Bartha L, Vajda A, Duska Z, Rahmeh H, Hangody L. Autologous osteochondral mosaicplasty grafting. J Orthop Sports Phys Ther. 2006;36:739–750. [DOI] [PubMed] [Google Scholar]
- 5. Brittberg M, Aglietti A, Gambardella R, et al. ICRS clinical cartilage injury evaluation system. Available at: https://cartilage.org/society/publications/icrs-score/icrs_evaluation. Accessed November 28, 2017.
- 6. Browne JE, Branch TP. Surgical alternatives for the treatment of articular cartilage lesions. J Am Acad Orthop Surg. 2000;8:180–189. [DOI] [PubMed] [Google Scholar]
- 7. Bruni DB, Iacono F, Raspugli G, Zaffagnini S, Marcacci M. Is unicompartmental arthroplasty an acceptable option for spontaneous osteonecrosis of the knee? Clin Orthop Relat Res. 2012;470:1442–1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Duany NG, Zywiel MG, McGrath MS, et al. Joint-preserving surgical treatment of spontaneous osteonecrosis of the knee. Arch Orthop Trauma Surg. 2010;130:11–16. [DOI] [PubMed] [Google Scholar]
- 9. Filardo G, Kon E, Perdisa F, Tetta C, Di Martino A, Marcacci M. Arthroscopic mosaicplasty: long-term outcome and joint degeneration progression. Knee. 2015;22:36–40. [DOI] [PubMed] [Google Scholar]
- 10. Fujita N, Matsumoto T, Kubo S, et al. Autogenous osteochondral graft transplantation for steroid-induced osteonecrosis of the femoral condyle: a report of three young patients. SMARTT. 2012;4:13–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gorczynski C, Meislin R. Osteonecrosis of the distal femur. Bull Hosp Jt Dis. 2006;63:145–152. [PubMed] [Google Scholar]
- 12. Gudas R, Stankevicius E, Monastyreckiene E, Pranys D, Kalesinskas RJ. Osteochondral autologous transplantation versus microfracture for the treatment of articular cartilage defects in the knee joint in athletes. Knee Surg Sports Traumatol Arthrosc. 2006;14:834–842. [DOI] [PubMed] [Google Scholar]
- 13. Guo WS, Zhang QD, Liu ZH, et al. Minimally invasive unicompartmental knee arthroplasty for spontaneous osteonecrosis of the knee. Orthop Surg. 2015;7(2):119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hangody L, Dobos J, Baló E, Pánics G, Hangody LR, Berkes I. Clinical experiences with autologous osteochondral mosaicplasty in an athletic population: a 17-year prospective multicenter study. Am J Sports Med. 2010;38:1125–1133. [DOI] [PubMed] [Google Scholar]
- 15. Hangody L, Feczkó P, Bartha L, Bodó G, Kish G. Mosaicplasty for the treatment of articular defects of the knee and ankle. Clin Orthop Relat Res. 2001;391(Suppl):S328–S336. [DOI] [PubMed] [Google Scholar]
- 16. Hangody L, Feczkó P, Kemény D, Bodó G, Kish G. Autologous osteochondral mosaicplasty for the treatment of full thickness cartilage defects of the knee and ankle. Clin Orthop Relat Res. 2001;391:328–337. [DOI] [PubMed] [Google Scholar]
- 17. Hangody L, Füles P. Autologous osteochondral mosaicplasty for the treatment of full thickness defects of weight bearing joints: 10 years experimental and clinical experiences. J Bone Joint Surg Am. 2002;85(Suppl 2):25–32. [DOI] [PubMed] [Google Scholar]
- 18. Heyse TJ, Khefacha A, Fuchs-Winkelmann S, Cartier P. UKA after spontaneous osteonecrosis of the knee: a retrospective analysis. Arch Orthop Trauma Surg. 2011;131:613–617. [DOI] [PubMed] [Google Scholar]
- 19. Johnson MR, LaPrade RF. Tibial plateau “kissing lesion” from a proud osteochondral autograft. Am J Orthop (Belle Mead NJ). 2011;40:359–361. [PubMed] [Google Scholar]
- 20. Juréus J, Lindstrand A, Geijer M, Robertsson O, Tägil M. The natural course of spontaneous osteonecrosis of the knee (SPONK): a 1- to 27-year follow-up of 40 patients. Acta Orthop. 2013;84:410–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 2000;16:494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kelman GJ, Williams GW, Colwell CW, Walker RH. Steroid-related osteonecrosis of the knee: two case reports and a literature review. Clin Orthop Relat Res. 1990;257:171–176. [PubMed] [Google Scholar]
- 23. Li Z, Zhu T, Fan W. Osteochondral autograft transplantation or autologous chondrocyte implantation for large cartilage defects of the knee: a meta-analysis. Cell Tissue Bank. 2016;17:59–67. [DOI] [PubMed] [Google Scholar]
- 24. Lynch TS, Patel RM, Benedick A, Amin NH, Jones MH, Miniaci A. Systematic review of autogenous osteochondral transplant outcomes. Arthroscopy. 2015;31:746–754. [DOI] [PubMed] [Google Scholar]
- 25. Marlovits S, Striessnig G, Resinger CT, et al. Definition of pertinent parameters for the evaluation of articular cartilage repair tissue with high-resolution magnetic resonance imaging. Eur J Radiol. 2004;52(3):310–319. [DOI] [PubMed] [Google Scholar]
- 26. Matsusue Y, Kubo M, Nakagawa Y. Autogenous bone-cartilage transplantation. Tech Knee Surg. 2010;9:85–94. [Google Scholar]
- 27. McCoy B, Miniaci A. Osteochondral autograft transplantation/mosaicplasty. J Knee Surg. 2012;25:99–108. [DOI] [PubMed] [Google Scholar]
- 28. Mont MA, Marker DR, Zywiel MG, Carrino JA. Osteonecrosis of the knee and related conditions. J Am Acad Orthop Surg. 2011;19:482–494. [DOI] [PubMed] [Google Scholar]
- 29. Mont MA, Rifai A, Baumgarten KM, Sheldon M, Hungerford DS. Total knee arthroplasty for osteonecrosis. J Bone Joint Surg Am. 2002;84:599–603. [DOI] [PubMed] [Google Scholar]
- 30. Mukai S, Nakagawa Y, Matsuoka M, Tanaka Y, Nakamura T. The clinical outcome of mosaicplasty for spontaneous osteonecrosis of the knee: the factor of the ability of sitting straight in Japanese style (in Japanese). J Jpn Orthop Soc Knee Arthrosc Sports Med. 2014;39:937–942. [Google Scholar]
- 31. Nakagawa Y, Matsusue Y, Nakamura T. Osteochondral graft transplantation for steroid-induced osteonecrosis of the femoral condyle. Lancet. 2003;362:402. [DOI] [PubMed] [Google Scholar]
- 32. Nakagawa Y, Mukai S, Yamada S, et al. Short-term effects of highly-bioavailable curcumin for treating knee osteoarthritis: a randomized, double-blind, placebo-controlled prospective study. J Orthop Sci. 2014;19:933–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nakagawa Y, Suzuki T, Kuroki H, Kobayashi M, Okamoto Y, Nakamura T. The effect of surface incongruity of grafted plugs in osteochondral grafting: a report of five cases. Knee Surg Sports Traumatol Arthrosc. 2007;15:591–596. [DOI] [PubMed] [Google Scholar]
- 34. Niki Y, Takeda Y, Udagawa K, Enomoto H, Toyama Y, Suda Y. Is greater than 145 degrees of deep knee flexion under weight-bearing conditions safe after total knee arthroplasty? A fluoroscopic analysis of Japanese-style deep knee flexion. Bone Joint J. 2013;95:782–787. [DOI] [PubMed] [Google Scholar]
- 35. Okuda M, Omokawa S, Okahashi K, Akahane M, Tanaka Y. Validity and reliability of the Japanese Orthopaedic Association score for osteoarthritic knees. J Orthop Sci. 2012;17:750–756. [DOI] [PubMed] [Google Scholar]
- 36. Pape D, Seil R, Fritsch E, Rupp S, Kohn D. Prevalence of spontaneous osteonecrosis of the medial femoral condyle in elderly patients. Knee Surg Sports Traumatol Arthrosc. 2002;10:233–240. [DOI] [PubMed] [Google Scholar]
- 37. Radke S, Wolmerstedt N, Bischoff A, Eulert J. Knee arthroplasty for spontaneous osteonecrosis of the knee: unicompartmental vs bicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2005;13:158–162. [DOI] [PubMed] [Google Scholar]
- 38. Sasaki T, Yagi T, Monji J, et al. Steroid-induced osteonecrosis of the femoral condyle: a clinical study of eighteen knees in ten patients. Nippon Seikeigeka Gakkai Zasshi. 1986;60:361–372. [PubMed] [Google Scholar]
- 39. Solheim E, Hegna J, Oyen J, Harlem T, Strand T. Results at 10 to 14 years after osteochondral autografting (mosaicplasty) in articular cartilage defects in the knee. Knee. 2013;20:287–290. [DOI] [PubMed] [Google Scholar]
- 40. Tanaka Y, Mima H, Yonetani Y, Shiozaki Y, Nakamura N, Horibe S. Histological evaluation of spontaneous osteonecrosis of the medial femoral condyle and short-term clinical results of osteochondral autografting: a case series. Knee. 2009;16:130–135. [DOI] [PubMed] [Google Scholar]