Abstract
The use of complementary and alternative medicines (CAMs) for treatment of acute and chronic diseases is on the rise world over, especially in Asian countries, and mostly in China and India. Drug-induced liver injury (DILI) due to CAM is increasingly reported in the literature from multiple centers all around the world and with large-number patient series published from the West, mostly based on nation-wide DILI networks and multicenter collaboration. Comprehensive DILI networks are lacking among major Asian countries with high incidence of CAM practices. Chinese medical societies dealing with drug toxicity, CAM practice and hepatobiliary disease have adopted an integrated approach to establishing identification, diagnosis and treatment of CAM-related DILI, representing a systematic approach that could be iterated by other countries for improving patient outcomes. In this exhaustive review, we provide published data on CAM-related DILI in Asia, with detail on incidences along with analysis of patient population and their clinical outcomes. Concise and clear discussion on commonly implicated CAM agents in major Asian countries and associated chemical and toxicology analyses as well as descriptions of liver biopsy findings are discussed with future directions.
Keywords: CAM, Herbals, Ayurveda, Chinese, DILI, Hepatitis, Cirrhosis, ACLF, Liver biopsy
Introduction
Complementary and alternative medicine (CAM) comprise various health care practices and products that do not form part of conventional (modern) evidence-based medical care (EBM). Complementary medicine is that which is utilized along with EBM, while alternative medicine wholly replaces EBM. Traditional medicine (TM), which differs from CAM, is defined by the World Health Organization as the “sum total of the knowledge, skill, and practices based on the theories, beliefs, and experiences indigenous to different cultures, used in the maintenance of health as well as in the prevention, diagnosis, improvement or treatment of physical and mental illness.”1,2
Most CAM systems incorporate TM practices. In Asia, the major CAM practices include traditional Chinese medicine (TCM) in Mainland China, Ayurveda in India, traditional Korean medicine in Korea, and TCM-based TM in Japan (known as Kampo). A mixture of influences from these major systems along with indigenous practices form part of CAM in other countries in the South-East Asian region. Siddha medicine, a system of traditional medicine originating in ancient Tamil Nadu (a Southern state in India) is followed in South India and Sri Lanka. The Persian-Arabic traditional medicine system known as Unani, which was practiced in Mughal India, is followed in modern-day Central Asia.
In India, six CAM systems have official recognition (Ayurveda, Yoga, Naturopathy, Unani Medicine, Siddha, and Homeopathy, known as AYUSH) with institutionalized education systems, governed by the ministry of AYUSH and under regulation by the Central Council for Indian Medicine, which is independent from the Indian Medical Council, the latter which regulates modern medicine. In China, TCM is fully integrated into the main healthcare system, with TCM institutions governed by the same national legislation on conventional or mainstream medicine.3,4 There is strong general public, political, cultural and social acceptance to CAM in almost all countries in Asia, but the lack of scientific evidence-based knowledge, paucity in adequate basic science as well as clinical trial-based research on CAM and ignorance regarding potential drug toxicity with CAM practices and associated products have led to a drift in general acceptance in utilizing these systems for healthcare among conventional medical practitioners and specialists.
While conventional modern medicine drugs require preclinical and phased clinical trials before approval of marketing and use, CAM drugs do not have to undergo this process. Wide word-of-mouth and social media popularity on assumed but an ‘assured’, ‘safer’ profile associated with CAM has led to a massive surge in use of these practices among the general population and patients with acute as well as chronic diseases. This has led to emergence of varying severities of drug hepatotoxicity, associated with CAM.5 In this review, we provide succinct evaluation of published data on CAM-related drug-induced liver injury (CAM-DILI), excluding dietary supplements, in Asia and discuss commonly implicated CAM therapies associated with DILI, explore clinical outcomes, detail the histopathological features, and appraise future directions in this regard.
Prevalence, incidence, patterns of use and outcomes: Current perspectives
Data regarding the true prevalence of CAM-DILI in Asia is lacking in the literature. However, large series from single centers or the seldom-performed multicenter studies have been able to shed light on the ‘region-specific’ incidence. Harris and colleagues reviewed data of 49 surveys in 15 countries and found that prevalence of CAM use ranged from 9.8% to 76%, depending on the region surveyed. Surveys among Asian countries were insufficient or absent to properly delineate prevalence. However, of the national samples’ surveys, the highest rates of CAM use were reported in East Asian countries such as Japan, South Korea, and Malaysia. This is probably not accurate, though, since Chinese and Indian surveys were nonexistent/not included at the time. Periodic population and health surveys are important tools that help monitor level of CAM use. This could become more robust with participation of government health agencies, using standardized methods for data collection – a system deficient in most of the countries entrenched in the practice of CAM.6
Singapore
In a retrospective followed by prospective analysis on DILI in Singapore by Wai et al.,7,8 CAM (mostly Chinese herbal medicines) accounted for 71% and 52% of cases of hepatotoxicity in 2006 and 2007, respectively. Teo et al.9 reviewed CAM-associated adverse events in an Asian community in Singapore from 2009 to 2014. In their study, CAM included complementary health products (including Chinese proprietary medicines, health supplements, and other traditional medicines), which were associated with hepatotoxicity in overall 9% of patients. Females comprised 51%, the majority being above 40 years of age. Around 70% of the patients had needed hospitalization for management of CAM-DILI, of whom, 58% did not show clinical and biochemical recovery on last follow up and 9% died. Sixty-one percent of the cases involved TCM; this was followed by health supplements (28%), and 11% of cases involved Indian Ayurvedic products and Malay Jamu traditional medicines. Reasons for CAM use in this study included promotion of wellbeing, weight loss and treatment of upper respiratory tract and gastrointestinal symptoms and febrile illnesses. Acute hepatocellular pattern of liver injury was noted in 60% of cases, while only 5% had cholestatic hepatitis. However, the concurrent use of western medicines was also reported in 53% of the cases. Among the Indian Ayurvedic drugs retrieved, none of the ingredients or their components could be identified accurately, showing lack of proper labelling and product description (Fig. 1) associated with this type of CAM. This issue with Ayurvedic medicines has been highlighted multiple times in the literature.9,10,11
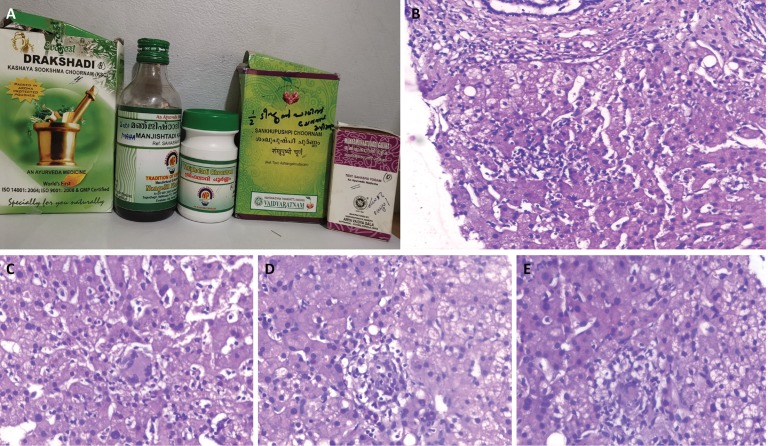
Fig. 1. Retrieved Ayurvedic drugs from two patients.
The absence of labeling, regarding ingredient and component detail, is evident in both. The first patient took the decoction and dried herbs for management of diabetes mellitus (A) while the second patient ingested the drugs for cure from hepatitis B virus infection. Both patients developed severe drug-induced liver injury, leading to death in the latter due to acute on chronic liver failure.
Japan
In a study from Japan on 1676 cases of DILI between 1997 and 2006, 10% and 7% of DILI were caused by proprietary herbal dietary supplements and Chinese herbal medicines respectively (higher compared to the survey findings between 1989 and 1998). DILI caused by CAMs was predominant among females, and the time to onset was longer compared to prescription drugs. Hepatocellular type of liver injury was common and symptoms such as general malaise, nausea, and anorexia were more frequent in the CAM group. Eosinophilia was less frequent and the death rate was lower in cases in which Chinese herbal medicines were implicated.12
In a study by Liem et al.13 on use of TCM among patients with chronic hepatitis B virus infection, it was found that 74% of the patients were Asian, 60% were males and only 46% used antivirals. Seventy-one percent of these patients were using CAM that contained potential hepatotoxic agents, such as green tea extracts and St. John’s wort. Family history of chronic hepatitis B virus infection, lower levels of viral load, and higher socioeconomic status were independently associated with CAM use in this cohort of patients. The authors shed light on important factors associated with CAM use among patients with chronic disease.
Korea
Suk et al.14 performed a prospective nationwide study of DILI in Korea, in which the most common causative agent implicated was TCM (27.5%). Dietary supplements, medicinal plants, folk remedies, and poly-herbal preparations were found to cause DILI in 13.7%, 9.4%, 8.6%, and 3.2%, respectively. The frequency of DILI due to herbs was significantly higher among female patients, and liver enzyme elevation was higher in patients who consumed CAM. The acute hepatocellular type of DILI was the most common pattern of liver injury. Three out of five patients who died in this series had DILI due to CAMs and one who underwent liver transplantation also had herbal medicine-related DILI. Recently, Cho and colleagues15 evaluated the risk of herbal medicine-related DILI in a nationwide prospective study in Korea. Out of 1001 in-patients, 6 were found to have CAM-DILI with Roussel Uclaf Causality Assessment Scoring Method scores ranging from 4 to 7. All were women with the hepatocellular type of DILI. One patient fulfilled Hy’s law, and all recovered after drug withdrawal.
China
Chinese herbal medicine, medicines for tuberculosis, and antibiotics were described as leading causes for DILI in China, a different pattern compared to the West. A meta-analysis that followed demonstrated that from 2006 to 2012, the most common cause was due to TCM (in 30.8%). In two systematic analyses consisting of 9,335 and 24,112 patients with DILI respectively, TCM was found responsible for DILI in 18.6% and 21.2% cases.16 Woo et al.17 showed that, among a total of 1169 in-patients, only 0.43% cases were attributed to TCM alone. In a study on 300 patients with DILI, Hou et al.18 found that Chinese herbal medicines were the leading cause of liver injury (in 40.3%), and almost 50% of these patients used herbal medications for treatment of dermatological and orthopedic diseases.
In a most recent study, the largest ever, on DILI from Mainland China, Shen et al.19 demonstrated that TCM and herbal and dietary supplements were the leading causes for liver injury, in almost 27% (n = 25,927), and most commonly among women, showing a rising and alarming trend in hepatotoxicity associated with CAM in China. In 16% of the implicated TCMs, formulation components were unknown. Zhang et al.20, in 2016, systematically reviewed data on TCM-induced liver injury, with particular focus on clinical characteristics and causative herbs. Among 58 cases, the majority being male, with DILI latency the median period was 30 days. Nine of eleven cases with well-defined information of actual and recommended dosage had excessive consumption of TCM, assuming safety associated with natural products. Liver enzyme elevation was higher with CAM compared to prescription drugs, and the hepatocellular type of liver injury was common; ninety-six point three percent of patients recovered.
Lai and coworkers21 reported on the clinical characteristics and liver histological changes in 138 patients with DILI from a single center in China. They found that Chinese herbal and proprietary medicines and health products accounted for almost 60% of DILI in their series. Wang and colleagues22 summarized the current literature with regards to clinical presentation, disease course, and prognosis of TCM-related DILI. The proportion of TCM-related DILI out of all DILI ranged from 22%–34% in most of the regions in China. Women and elderly were the most common users, and gynecologic and orthopedic diseases were the most common indications for CAM use. Male gender, higher levels of direct bilirubin, aspartate aminotransferase, and hypoalbuminemia were the predictors of mortality. Higher risk of death or liver transplantation was notable in patients with cholestatic-type TCM-related DILI, and the mortality rate associated with TCM-DILI was 4.67%.
Ou et al.23 reported that the crude annual incidence rate of DILI was 92.95 cases per 100,000 patients, with Chinese herbal medicines identified as the primary cause of DILI in 36% of the patients and an overall mortality of approximately 9% (out of which, 70% died of progressive liver failure). The model for end-stage liver disease score and hypoalbuminemia at baseline were found to be independent predictors of death.
India
Udayakumar et al.24 showed that the use of traditional indigenous herbal medicine (South-Indian Tamil native healers) in patients with acute liver failure (ALF) increased risk of death. In the first detailed single center study on DILI (n = 313) from India, Devarbhavi and colleagues25 found that DILI associated with CAM (Indian Ayurvedic medicines) was seen only in 1.3% patients, of whom 50% died due to progressive liver failure. Philips and colleagues26 were the first to study clinical outcomes and analyze component toxicology of patients developing acute liver injury due to use of Ayurvedic herbal medications (AHMs). Out of 1440 liver disease patients, 94 were found to have a severe liver injury and associated AHM intake, of whom, 33 patients had AHM-DILI by the Roussel Uclaf Causality Assessment Scoring Method. One-third of the patients consumed AHM from unregistered traditional Ayurvedic healers. Males predominated (70.4%) and median duration of drug intake to symptom development was 28 days. The most common reason for use of CAMs was for gastrointestinal symptoms. Overall mortality was approximately 19%. Independent predictors of mortality included hepatic encephalopathy and hypoalbuminemia at presentation. Another unique feature of the patient population was the identification of autoantibodies in patients, revealing the possibility of a drug-induced autoimmune-like hepatitis associated with CAM-DILI.
The same study group also described characteristics and clinical outcomes in cirrhosis patients ingesting CAMs. The authors found that out of 1,666 patients with cirrhosis, 68% had used CAM and 35.7% patients presented with CAM-related DILI leading to acute on chronic liver failure (ACLF). In patients with CAM-DILI-related ACLF, 63% self-medicated based on social media sharing, 83% were male patients and overall 53% of patients died, with a median survival 194 days. Baseline overt hepatic encephalopathy and CLIF-C-organ failure score, total bilirubin, hyponatremia and leukocytosis, and grade of ACLF predicted 1-, 3-, 6- and 12-month mortality, respectively.27
CAM-related chronic liver disease and ACLF
Recently, a large multicenter study demonstrated that ACLF in Asia-Pacific countries was predominantly due to CAMs (in approximately 72% of patients; n = 3132) and that the most common cause for chronic liver disease was alcohol. The authors found that encephalopathy, bilirubin, blood urea, lactate, and international normalized ratio predicted mortality in drug-induced ACLF.28 Zhu and coworkers29 studied predictors of poor outcomes in 488 patients with herb-induced liver injury, at a single tertiary center in China. The hepatocellular type of liver injury was most common, with median age 45 years. Eighty-two percent of patients had complete normalization of clinical and biochemical abnormalities, while fourteen percent developed chronic liver disease, and cirrhosis developed in 7.6%. Approximately 4% of patients in this series died without provision for liver transplantation. Arguably, it is possible that CAM-DILI is higher in the Chinese patient population (probably due to better surveillance and integrated reporting) but outcomes are worse in those developing CAM-DILI in the Indian subcontinent. Furthermore, the presence of chronic liver disease or cirrhosis significantly increases the risk of death in patients who develop ACLF.
CAMs associated with liver injury
Knowledge on DILI associated with CAMs has mostly come through three sources: case reports, case series and descriptions as part of large retrospective or prospective studies on DILI. In patients with CAM-DILI, the type of liver injury can be classified into hepatocellular, mixed or cholestatic types, based on the R value (https://www.mdcalc.com/r-factor-liver-injury; in which a value >5 is considered hepatocellular, <2 as cholestatic, and 2–5 as mixed type of liver injury). In the majority of published data on CAM-DILI, the hepatocellular pattern of injury is most common. Repositories of DILI are useful sources for identifying causative agents. These also provide important information on DILI associated with medical treatments, showing regional differences, such as for CAMs. Most of the published data on CAM-DILI comprise case reports and small case series, with high-quality, large cohort studies available for certain CAMs only, the latter discussed succinctly below.
Zhao and colleagues30 performed a retrospective analysis of patients diagnosed with ALF in seven hospitals in different areas of China, from January 2007 to December 2012. Out of 177 patients, 63.28% died. The common causes for liver failure were drug toxicity (43.50%), indeterminate etiology (29.38%), and acute viral hepatitis (11.30%). Among those who developed DILI-ALF, TCM was the cause in 39%. The authors found that age, baseline evidence of overt hepatic encephalopathy, coagulation failure, and blood ammonia were independently associated with death due to DILI-ALF. The same group31 later published separately on the 30 cases of ALF due to TCM, describing the patient characteristics and clinical outcomes in detail. The common reasons for TCM consumption were chronic skin diseases, followed by diseases of the respiratory tract. Women predominated, with the average age being 39.7 years. The mortality of patients with TCM-related ALF was 60%, in whom, one-third died of severe coagulation failure-related symptoms and 78% with overt hepatic encephalopathy grade >2 having died. The majority of patients in this series consumed Tripterygium wilfordii (known as Lei Gong Teng in TCM, or Thunder-God Vine). Histopathological patterns were not studied in this series of patients.
In the study by Teo and coworkers,9 the most common CAM components/agents associated with DILI included Fu Ling (Sclerotium poriae cocos), Huang Qin (Radix scutellaria baicalensis), Gan Cao (Radix glycyrrhizae), Ze Xie (Alisma orientalis), and Chuan Xiong (Rhizoma ligustici). Most of the patients used at least 10 different ingredients, and the duration of use ranged from a few months to 3 years.
Lei et al.32 performed a systematic review of case reports and series (450 cases) on liver damage associated with Polygonum multiflorum (PM; known as He Shou Wu). In TCM, raw PM is used for detoxification, to treat skin infections, to prevent malaria, and to improve gut motility, while the processed form (known as P. multiflorum praeparata or PMP) is utilized for improving liver and kidney health, as a hematinic, for blackening hair, and as a hypolipidemic agent. Even though some pharmacological studies have shown the antiinflammatory and hypolipidemic nature of PM, no standard, high-quality, controlled and rigorously-designed human trials exist. Symptomatic liver injury occurred approximately 30-days after intake of PM with prominence of jaundice. Two patients underwent liver transplantation and another seven patients died due to liver failure.
Chinese authors, in general, have considered PMP relatively safe, with raw form PM extracts showing higher potential for liver injury. It was suggested that the ethanol extract produced hepatic lesions more easily than that of water formulation, and the decreasing order of toxic potential was described as PM ethanol extract > PM water extract > PMP ethanol extract > PMP water extract. However, other authors33 have mentioned the toxicity potential differently (PM water extract > PM acetone extract > PMP acetone extract), which has added to the confusion in identification of complex toxicity profiles associated with whole herb preparations.
Recently Jing et al.34 performed a case-control study on the association between the concurrence of pre-existing chronic liver disease and prognosis in patients with PM-induced liver injury. Among these, 22.8% had pre-existing chronic liver disease, with the majority having (52%) alcoholic liver cirrhosis. On comparing PM-DILI with and without chronic liver disease, the latter group showed higher mortality (0.9% vs. 9.1%) and more prolonged course of liver injury (12.5% vs. 30.3%). Four patients (2.8%) in the entire cohort developed ACLF. The concurrent presence of underlying chronic liver disease was found to be an independent risk factor for both of chronicity and mortality in those with PM-DILI. In the Woo et al.17 study from Korea, herbal medicines-related DILI were seen in only <1% of cases reviewed; however, the common causative herbal agents associated with hepatotoxicity were Ephedrae Herba and Scutellariae Radix (skullcap). In the study by Ou and colleagues, among 36% of patients with CAM-DILI, polyherbal mixtures, Radix polygoni multiflora, Panax pseudo-ginseng, Tripterygium wilfordii, saffron and shenbao mixture were found to be common causes for liver injury, in descending order of incidence.23
Thyagarajan and coworkers35 described more than 300 preparations for the treatment of jaundice and chronic liver diseases in Indian systems of medicine, using more than 87 Indian medicinal plants. However, among them, only four terrestrial plants had undergone good quality studies adhering to the internationally acceptable scientific protocols, which remains so, even now, almost 16 years later. Reports on Indian Ayurvedic medicine-related hepatotoxicity are sparse in the literature. Centella asiatica (Asiatic pennywort) or Gotu Kola in Ayurvedic medicine has been reported to produce ALF, granulomatous hepatitis and severe necro-inflammatory liver injury (Fig. 2).36,37 Teschke and Bahre38 presented the case of a 64-year-old female patient on Ayurvedic medications for treatment of vitiligo. The implicated drugs included Bakuchi tablets containing extracts from Psoralea corylifolia leaves, Khadin tablets containing extracts from Acacia catechu leaves, Brahmi tablets containing Eclipta alba, and Usheer tea prepared from Vetivexia zizaniodis.
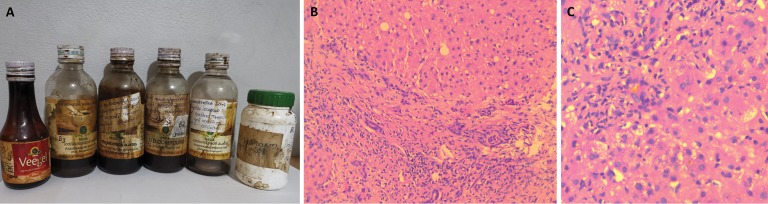
Fig. 2. Ayurvedic medication prescribed by a registered practitioner for a patient with vague digestive complaints.
Multiple medicines (A) were taken over a period of 1 month, leading to severe bilateral leg edema and ascites; transjugular liver biopsy revealed features of extensive lymphocytic and eosinophilic infiltration of sinusoids associated with sinusoidal dilatation (B, hematoxylin and eosin stain, 40×); giant cell transformation of hepatocytes (C, H&E stain, 400×); multiple scattered granulomas in the lobular and portal areas (D and E, H&E stain, 400×) suggestive of granulomatous hepatitis with sinusoidal obstruction. Taken together, the Ayurvedic medications had close to 50 different types of herbal and nonherbal components.
Abbreviation: H&E, hematoxylin and eosin.
Fleig et al.39 performed a randomized controlled trial on the Ayurvedic medicine Liv 52 in a large cohort of patients with alcoholic liver disease. They found that Liv 52 did not improve liver-related events or survival in treated patients, and that its use in patients with Child C cirrhosis led to increased mortality. This study led to nationwide ban of Liv 52 in the USA; however, it remains heavily utilized among patients in Asian countries currently.
In the study by Philips et al.,26 almost 40% of CAMs retrieved from patients with CAM-DILI were proprietary Indian Ayurvedic herbal medicines in the form of bottled branded decoctions, pills, tablets, and powders. One-third of the CAMs were unlabeled polyherbal mixtures, prescribed by traditional Ayurvedic healers. On chemical and toxicology analysis, lead was detected in 73% (maximum detected: 7318.1 mg/kg), mercury in 64% (751.5 mg/kg), and arsenic in 58% (111 mg/kg). Apart from heavy metals, multiple volatile organic compounds and industry grade chemicals were also detected in the more than 70% of the samples analyzed. However, in the study on CAM-DILI-related ACLF, the most common CAM utilized by the cirrhosis patient population was that of Ayurveda (77%), of which, the majority were traditional indigenous herbal medicines prescribed by local healers for diabetes mellitus management. These included aloe vera, passionflower and guava leaf extracts, Phyllanthus niruri, Polygonum aviculare (wire weed), Malabar nut tree leaf extracts, Datura stramonium (devil’s weed) and Chlorophytum borivilianum (safed musli).26,27
Zhu et al.40 analyzed the causes, clinical, laboratory and pathological features, and outcomes of DILI in 69 children (up to 14 years of age) and compared the differences between TCM and Western medicine-related liver injury. Autoantibodies were detected in 32 children with DILI, in their series. Western medicine-related DILI was noted in 56%, TCM use in 22%, and combinations in 22%. The major implicated herbs were Ephedra sinica and PM, followed by Andrographis paniculate, Xanthium sibiricum, Mentha haplocalyx, Smilax glabra, and Tripterygium wilfordii. Chronicity was noted more in the Western medicine group, while development of ALF and death rates were higher in children with DILI due to CAM.
In the recent study by Zhu and colleagues29 on outcomes in 488 patients with herb-induced liver injury, the major implicated agent was polyherbal TCMs which contained in common, Fructus psoraleae, Gynura segetum and PM, apart from a multitude of other components. However, these three herbs as single agents were also responsible for ALF leading to death or liver transplantation in three patients. Similarly, those herbs, as single agents, associated with chronic herb-induced liver injury in the study patients, included Radix polygoni multiflora, Tripterygium wilfordii, Semen cassiae, and Smilax scobinicaulis.
Lee et al.41 found that Chinese herbal medicines such as Xiao-Chai-Hu-Tang, Long-Dan-Xie-Gan-Tang, or others, containing more than 19 gram of radix bupleuri (made from dried root of Bupleurum falcatum L. or B. falcatum L. var. scorzonerifolium) prescribed for management of chronic hepatitis (mainly hepatitis B virus-related) could lead to severe liver injury. The relative risk of developing liver injury by subsequent addition of 19 g of radix bupleuri was 2.19. Jakkula et al.42 found that a regimen of Chinese herbal medicines did not improve quality of life, liver chemistry results, or viral load in a cohort of patients with hepatitis C virus, in a randomized trial.
Yuen et al.43 found that in approximately 16% of patients with chronic hepatitis B virus-related liver disease, acute liver injury was attributable to traditional Chinese medicine, with all patients showing clinical presentation of acute exacerbation of chronic hepatitis B. There were two deaths and one patient underwent liver transplantation. The identified hepatotoxic components included Polygonum multiflorum Thunb, Cassia obtusifolia L, Melia toosendan Sieb., Rheum palmatum L., Scolopendra subspinipes mutilans L, Alisma orientale Juzepe, Glycyrrhiza uralensis Fisch., and Mentha haplocalyx Briq, while one TCM medicine was adulterated with a highly hepatotoxic agent, N-nitrosofenfluramine. The authors concluded that TCM–CAM-related DILI resulted in high mortality in chronic hepatitis B patients and that prospective randomized-controlled trials with the same stringent criteria as Western medicine clinical trials are required for CAMs for appropriate documentation of efficacies and safety before marketing. In similar lines, Philips and coworkers demonstrated that use of AHMs could lead to reactivation of chronic hepatitis B akin to that seen with chemotherapy, corticosteroid or biological use in predisposed patients, due to presence of unknown and unresearched immunomodulating components in whole herbs (Fig. 3).44
Fig. 3. Ayurvedic medicines prescribed by a registered practitioner for a patient with chronic hepatitis B-related cirrhosis with low viral load.
Multiple medications (A), most of which unlabeled and with directions for use, written over the bottles themselves, were handed over to the patient. After consuming the medicines for almost 1 month, the patient developed cholestatic jaundice, ascites and hepatic encephalopathy within 2 weeks, suggestive of acute on chronic liver failure. Transjugular liver biopsy revealed severe mixed portal inflammation with ductular reaction (B, H&E, 40×) associated with extensive periportal necrosis and cholestasis with cholangitis (C, H&E, 400×). He subsequently died on the liver transplant wait-list.
Abbreviation: H&E, hematoxylin and eosin.
A compilation of important CAMs of Asian origin implicated in DILI and utilized in Asian countries is shown in Table 1.5,45–48
Table 1. Complementary and alternative medicines used in Asian countries implicated in drug-induced liver injury.
| No | Region | Name of complementary and alternative drug | Salient features |
| 1 | Pan-Asian | Aloe perfoliata var. vera (aloe vera) |
|
| 2 | China | Podophyllum pleianthum (Ba Jiao Lian or Chinese may apple) |
|
| 3 | China/Taiwan | Breynia vitis-idaea (Chi R Yun or Large calyx breynia) |
|
| 4 | China | Jin Bu Huan Polyherbal formulation containing Lycopodium serratum (club moss), Panax pseudo ginseng (ginseng) and Polygala chinensis (milkwort) |
|
| 5 | China | Ephedra sinica (Ma Huang or yellow hemp) |
|
| 6 | China/Japan | Sho-saiko-to or Xiao Chai Hu Tang (polyherbal) Bupleurum chinense (thorowax), Scutellaria baicalensis (Chinese skullcap), Pinellia ternate (crow-dipper), Zingiber officinale (ginger), Glycyrrhiza glabra (licorice), Codonopsis pilosula (Poor man’s ginseng), Ziziphus jujube (Chinese date) |
|
| 7 | China | Polygonum multiflorum Thunb. (Shou Wu Pian or Chinese climbing knotweed) |
|
| 8 | India | Garcinia cambogia (Malabar tamarind) |
|
| 9 | China/Korea | Panax ginseng (ginseng) |
|
| 10 | Pan-Asian | Camellia sinensis (green tea) |
|
| 11 | China/India | Piper methysticum (kava, intoxicating pepper) |
|
| 12 | South-East Asia | Mitragyna speciose (kratom) |
|
| 13 | China/Japan/India | Viscum album and Loranthus ferrugineus (mistletoe) |
|
| 14 | India/China | Morinda citrifolia (Indian mulberry/noni/Ba Ji Tian) |
|
| 15 | India | Cassia angustifolio (senna) |
|
| 16 | India | Cassia occidentalis (coffee senna) |
|
| 17 | China/India |
Scutellaria lateriflora (skullcap) Known as ‘huang qin’ in China Component of anti-inflammatory proprietary drug marketed as Univestin (Unigen®) Macvestin (Macleods®)/Cardivestin or Ostivestin (Zydus Cadilla®) |
|
| 18 | India/China/Korea | Arthrospira platensis (spirulina, blue-green algae; cyanobacteria) |
|
| 19 | India | Curcuma longa (curcumin/turmeric) |
|
| 20 | India/South-East Asia (Malaysia) | Azadirachta indica (margosa oil or Indian neem oil) |
|
| 21 | India | Centella asiatica (Asiatic pennywort or Gotu Kola) |
|
| 22 | India | Liv 52 and Liv 52 DS (proprietary Ayurvedic drug manufactured by Himalaya Drug Company®) Capparis spinosa, Cichorium intybus, Mandur Bhasma, Solanum nigrum, Terminalia arjuna, Cassia occidentalis, Achillea millefolium, Tamarix gallica Processed in extracts of Eclipta alba, Phyllanthus amarus, Boerhaavia diffusa, Tinospora codifolia, Raphanus sativus, Emblica officinalis, Plumbago zeylanica, Embelia ribes, Terminalia chebula, Fumaria officinalis |
|
Histopathological characteristics of CAMs associated with liver injury
Histopathology of CAM-related DILI is nonspecific and includes acute or chronic hepatitis, cholestatic liver disease (including vanishing bile duct syndrome), vascular liver disease (mostly sinusoidal obstruction syndrome), autoimmune features, granulomatous hepatitis, giant cell hepatitis and the syndrome of ALF with massive hepatic necrosis. Most of the histopathological descriptions on CAM-DILI are based on isolated case reports, and specific findings related to CAM on liver biopsy remain difficult to describe in view of multiple CAM use at a time, each with multiple ingredients in a single patient. Liver histopathological examination has shown that CAM-DILI, especially related to TCM and Ayurvedic herbals, mimics severe nonalcoholic steatohepatitis, alcoholic hepatitis, acute hepatitis with varying severity of necrosis, hepatocellular and canalicular cholestatic features, veno-occlusive disease and cirrhosis, associated pigment changes, and neutrophilic, lymphoplasmacytic, eosinophilic or mixed inflammatory patterns affecting lobular, portal and interface areas.49–53
Large studies on descriptive histopathology associated with CAM-related DILI are infrequent in the published literature. Lai et al.21 in their study on DILI in 138 patients found that the most common cause for liver injury was CAM, mainly those of Chinese herbal medicine. The liver biopsy features included macro- and microvesicular steatosis, cholestasis, hepatocyte apoptosis, epithelioid granulomas, eosinophilic, neutrophilic and lymphoplasmacytic infiltration, and iron deposition. The inflammation, necrosis and Ishak fibrosis score in patients with cholestatic and mixed type of liver injury were higher than those with predominantly hepatocellular type of injury.
Zhu et al.41 described liver biopsy of 55 children in whom the major cause for DILI was TCM. They found that liver cell degeneration, necrosis (bridging, confluent and submassive type), and lobular inflammation were common findings. Approximately 29% had varying degrees of interface hepatitis, while hepatocellular and canalicular cholestasis were observed in 27%. Almost half of the liver biopsies showed eosinophil infiltration, while in a quarter of the children, after complete normalization of liver biochemistries, histological features of moderate portal inflammation, interface hepatitis and fibrosis prevailed, suggesting chronicity.
Another recent study from India on Ayurvedic medicine-related liver injury among the general population, was the first to detail liver histopathological characteristics linked to patient outcomes. Chronic hepatitis was the most common type of inflammation, seen in 81.5%. Portal-based inflammation predominated (89%), and necrosis was noted in almost 56% of patients with AHM-related injury. Fibrosis was seen in 77.8% and cholestasis in 67%. The presence of necrosis and steatosis correlated positively and negatively with mortality respectively. The same study group also identified and described liver histopathology findings among patients with cirrhosis consuming Ayurvedic medications and developing ACLF. Out of 30 patients with Roussel Uclaf Causality Assessment Scoring Method scores suggestive of probable and possible CAM-DILI-related ACLF, 12 consented to transjugular liver biopsy. Pertinent findings included portal-based moderate to severe mixed inflammation, neutrophilic predominance, eosinophilic infiltration of portal tracts, cholangitis, intracanalicular and hepatocellular cholestasis, varying grades of ductular reaction, and extensive siderosis.26,27
In summary (Table 2), liver biopsy is not mandatory for confirmation of diagnosis of CAM-DILI since histological features are nonspecific and can mimic any other acute or chronic liver disease etiology. However, the patterns and severity of injury on liver biopsy helps prognosticate patient outcomes in specific situations and should be performed if adequate expertise in both interventional radiology and liver histopathology is available. This would also help in identification of patients who require liver transplantation at the outset for early listing, so as to prevent certain futility on medical management.
Table 2. Published large patient series on liver histopathology related to CAM-related liver injury.
| AuthorRef | Year | Patient population | Most common CAM | Number | Salient findings |
| Lai et al.21 | 2012 | Adults, general population | Traditional Chinese herbal medicines | 74/138 | Macro and microvesicular steatosis, cholestatic hepatitis, eosinophilic and neutrophilic predominant portal and lobular inflammation and severe grades of hepatic siderosis Higher grades of inflammation, necrosis and Ishak fibrosis score in cholestatic and mixed type of liver injury No separate analysis on CAM-DILI-related histology and outcomes |
| Zhu et al.40 | 2015 | Children, general population | Traditional and proprietary Chinese medicine | 15/69 | Severe grades of apoptosis and necrosis, lobular inflammation, varying degrees of interface hepatitis Lesser incidence of hepatocellular and canalicular cholestasis Evidence for chronic DILI noted in children on liver histology, after normalization of biochemical parameters Separate analysis on CAM-DILI subgroup not provided |
| Philips et al.26 | 2018 | Adults, general population | Proprietary and traditional Ayurveda and herbal medicines | 33 | Presence of necrosis linked to mortality Presence of massive and submassive necrosis worst prognosis Predominant steatotic type of liver histopathology favorable outcome Arsenic and mercury in CAM associated with poor survival First to provide linkage on histopathology related outcomes in CAM-DILI and chemical and toxicology analysis in CAM related to DILI |
| Philips et al.27 | 2019 | Adult patients with cirrhosis | Traditional Ayurveda and herbal medicines | 30 | First to discuss histopathology in CAM-DILI leading to ACLF Portal-based moderate to severe mixed inflammation, neutrophilic/eosinophilic predominance, varying grades of hepatocellular and canalicular cholestasis with cholangitis and extensive siderosis notable |
Abbreviations: ACLF, acute on chronic liver failure; CAM, complementary and alternative medicine; DILI, drug-induced liver injury.
Current perspectives and future directions
Problems associated with CAM use in many countries stem from the fact that these practices and products are 1) mostly classified as foods and dietary supplements and 2) considered safe as per ancient practices forming part of a separate pharmacopeia deep-rooted in religious, cultural and social acceptance, and are thus exempt from rigorous clinical testing and quality control. For example, in India, CAM prepared and marketed as per classical Ayurvedic literature does not require preclinical and phased-clinical trials based on the fact that these ‘drug recipes’ are knowledge passed down through thousands of years of practice and as such, are taken as granted to be safe and efficacious.
Utilization of modern research tools in such instances can help identify toxic components and beneficial compounds for multiple disease conditions. Much of current CAM-based research studies are of poor quality, inclusive of paltry hypotheses, suffering from inadequate methodology, meddled with impecunious statistical analysis, and ultimately lost to predatory or low-grade nonindexed journals, being further showcased as clinical data to an unknowing patient population for better for-profit sale of the product.54,55 A prime example is of the Ayurvedic antimalarial drug AYUSH-64, on which a non-controlled clinical trial was published (in the year 1981; without ethical statements and disclosures; alarmingly showcasing complete confidential patient details in Table 1 of the published study) in a journal (Journal of Research in Ayurveda and Siddha, Vol 2, No 4, pages 309–26), which is currently not traceable to any valid scientific data indexing repositories. Properly conducted clinical trials on the same drug decades later showed absence of blood schizonticide activity on preclinical testing, with efficacy <50% in curing malaria in humans when compared to standard drug chloroquine.56,57
The need for evidence of quality, quality tests, and production standards that are currently without homogeneity and control in CAM has to be addressed by the industry and appropriate government agencies. An important example in this aspect is CAM prescribed by indigenous and traditional health practitioners, the majority being uncertified and not licensed but enjoying public and social acceptance for providing healthcare, and has been associated with severe DILI as well as death due to progressive liver failure (Fig. 4). Practitioners and producers of CAM must be trained and regulated to provide exhaustive information, such as component descriptions, indications, precautions, usage directions, side effects, storage details, and regulatory information regarding the drugs. This information is usually provided on a leaflet inserted into the product package in conventional medicine, which is almost nonexistent or immensely vague in proprietary and nonproprietary CAM.
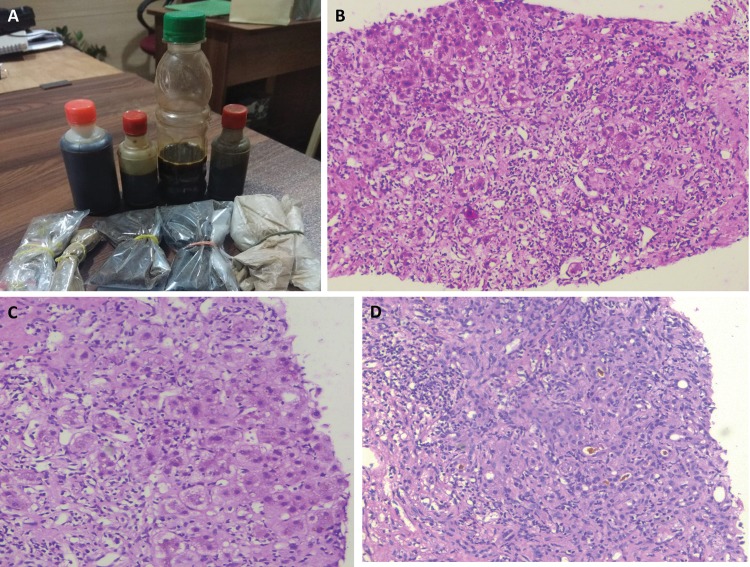
Fig. 4. Herbal medicine and decoctions without any identifiable components (A) prescribed by a TAH, for management of complications of diabetes mellitus in a middle-aged man.
After 3 weeks of medicine use, the patient presented with severe cholestatic liver injury. He went back to the TAH for management of cholestatic jaundice and was advised to continue the same drugs at half dose with dietary restrictions (only rice porridge with boiled vegetables, as required). After 1 week, severe clinical worsening with malnutrition ensued, and the patient was brought to the emergency unit. Transjugular liver biopsy revealed hepatic lobular distortion due to severe mixed inflammation at the portal and lobular regions (B, H&E, 40×), severe ballooning of hepatocytes with apoptosis (C, H&E, 400×), and periportal and perivenular necrosis with severe hepatocellular and canalicular cholestasis (D, H&E stain, 100×). The patient recovered completely with drug withdrawal and aggressive supportive care, including eight sessions of plasma-exchange.
Abbreviations: H&E, hematoxylin and eosin; TAH, traditional Ayurvedic healer.
First and foremost, treating primary physicians and specialists who care for liver disease patients must realize and accept the fact that use of CAM is here to stay and will almost certainly rise among the general and patient population. Secondly, they have to realize that CAM is not without side effects, and liver injury due to CAM is a real concern. The physicians must educate the patient and the family, who will in turn educate the locality and thereby the community regarding CAM and associated adverse events. Industry, government agencies, and practitioners of CAM need to understand the importance of bench-to-bedside work and should be motivated to perform studies that are rich in scientific methodology. This ensures 1) identifying efficacious and toxic components associated with CAM and 2) integration of a refined logic in CAM that can ultimately be used along with conventional medicine.
This aspect is beautifully undertaken in China where an integrated guideline approach to diagnosis and management of CAM-DILI was recently published.58 The guidelines specify evaluation, identification and treatment of CAM-DILI in China according to the strength of evidence through a structured diagnostic workflow. It also recommends either identifying the species of Chinese or herbal medicine or excluding adulterations and toxin contaminants associated with DILI, to improve the level of evidence for a clinical diagnosis. This acceptance, as seen in the Chinese Guidelines, for improving patient outcomes through an integrative medical approach is an unmet need in countries entrenched in promotion and practice of CAM in Asia.
Conclusions
CAM use is widely prevalent in Asia and is associated with, among other adverse effects, hepatotoxicity. Both proprietary as well as nonproprietary or traditional CAMs have been implicated in hepatotoxicity. Acute hepatocellular pattern of liver injury is the most common type of liver injury seen, and the spectrum of liver-related adverse events range from simple elevation of liver enzymes to the very serious ALF and ACLF, which may, at times, require liver transplant.
CAM-related liver injury is one among the major causes for hepatotoxicity, including ALF and ACLF worldwide, with high incidence among Asian countries. Patient outcomes associated with CAM-DILI are generally poor, with very high mortality rates in those with chronic liver disease. Stringent regulations, at par with that of conventional modern medicine, are required, and may help improve safety of patients seeking CAM for their health needs. Regional surveillance including postmarketing analysis from government agencies associated with drug regulation and control in tandem with national as well as regional level hepatology societies are important for understanding the true prevalence of DILI associated with CAM. An integrated approach used by practitioners combining conventional and traditional medicine to identify safety and efficacy of CAMs is an unmet need in most of the Asian countries. Endorsement of scientific methodology with good quality preclinical and clinical trials and abolishment of unhealthy publication practices is an area that needs immediate attention in CAM practice. Such holistic standard science-based approaches could help ameliorate liver disease burden in the general and patient population.
Abbreviations
- ACLF
acute on chronic liver failure
- AHM
Ayurvedic herbal medication
- ALF
acute liver failure
- AYUSH
Ayurveda, Yoga, Naturopathy, Unani Medicine, Siddha, and Homeopathy
- CAM
complementary and alternative medicine
- CAM-DILI
CAM-related drug-induced liver injury
- EBM
evidence-based medical care
- TCM
traditional Chinese medicine
- PM
Polygonum multiflorum
- PMP
P. multiflorum praeparata
- TM
traditional medicine
References
- 1.PDQ Integrative, Alternative, and Complementary Therapies Editorial Board Topics in Integrative, Alternative, and Complementary Therapies (PDQ®): Health Professional Version. PDQ Cancer Information Summaries [Internet]; Bethesda (MD). National Cancer Institute (US); 2002. Available from: https://www.ncbi.nlm.nih.gov/books/NBK126745 . [PubMed] [Google Scholar]
- 2.World Health Organization WHO traditional Medicine strategy 2014–2023. Available from: http://www.searo.who.int/entity/health_situation_trends/who_trm_strategy_2014-2023.pdf?ua=1 .
- 3.World Health Organization WHO global report on traditional and complementary medicine 2019. Available from: https://apps.who.int/iris/bitstream/handle/10665/312342/9789241515436-eng.pdf?ua=1 .
- 4.Agarwal V. Complementary and alternative medicine provider knowledge discourse on holistic health. Front Commun. 2018;3:15. doi: 10.3389/fcomm.2018.00015. [DOI] [Google Scholar]
- 5.Amadi CN, Orisakwe OE. Herb-induced liver injuries in developing nations: An update. Toxics. 2018;6:E24. doi: 10.3390/toxics6020024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harris PE, Cooper KL, Relton C, Thomas KJ. Prevalence of complementary and alternative medicine (CAM) use by the general population: a systematic review and update. Int J Clin Pract. 2012;66:924–939. doi: 10.1111/j.1742-1241.2012.02945.x. [DOI] [PubMed] [Google Scholar]
- 7.Wai CT. Presentation of drug-induced liver injury in Singapore. Singapore Med J. 2006;47:116–120. [PubMed] [Google Scholar]
- 8.Wai CT, Tan BH, Chan CL, Sutedja DS, Lee YM, Khor C, et al. Drug-induced liver injury at an Asian center: a prospective study. Liver Int. 2007;27:465–474. doi: 10.1111/j.1478-3231.2007.01461.x. [DOI] [PubMed] [Google Scholar]
- 9.Teo DC, Ng PS, Tan SH, Lim AT, Toh DS, Chan SY, et al. Drug-induced liver injury associated with Complementary and Alternative Medicine: a review of adverse event reports in an Asian community from 2009 to 2014. BMC Complement Altern Med. 2016;16:192. doi: 10.1186/s12906-016-1168-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhalerao S, Munshi R, Tilve P, Kumbhar D. A survey of the labeling information provided for ayurvedic drugs marketed in India. Int J Ayurveda Res. 2010;1:220–222. doi: 10.4103/0974-7788.76785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Devarbhavi H. Ayurvedic and herbal medicine-induced liver injury: It is time to wake up and take notice. Indian J Gastroenterol. 2018;37:5–7. doi: 10.1007/s12664-018-0820-6. [DOI] [PubMed] [Google Scholar]
- 12.Takikawa H, Murata Y, Horiike N, Fukui H, Onji M. Drug-induced liver injury in Japan: An analysis of 1676 cases between 1997 and 2006. Hepatol Res. 2009;39:427–431. doi: 10.1111/j.1872-034X.2008.00486.x. [DOI] [PubMed] [Google Scholar]
- 13.Liem KS, Yim C, Ying TD, Zanjir WR, Fung S, Wong DK, et al. Prevalence and predictors of complementary and alternative medicine modalities in patients with chronic hepatitis B. Liver Int. 2019;39:1418–1427. doi: 10.1111/liv.14105. [DOI] [PubMed] [Google Scholar]
- 14.Suk KT, Kim DJ, Kim CH, Park SH, Yoon JH, Kim YS, et al. A prospective nationwide study of drug-induced liver injury in Korea. Am J Gastroenterol. 2012;107:1380–1387. doi: 10.1038/ajg.2012.138. [DOI] [PubMed] [Google Scholar]
- 15.Cho JH, Oh DS, Hong SH, Ko H, Lee NH, Park SE, et al. A nationwide study of the incidence rate of herb-induced liver injury in Korea. Arch Toxicol. 2017;91:4009–4015. doi: 10.1007/s00204-017-2007-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang GQ, Deng YQ, Hou FQ. Overview of drug-induced liver injury in China. Clin Liver Dis (Hoboken) 2014;4:26–29. doi: 10.1002/cld.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Woo HJ, Kim HY, Choi ES, Cho YH, Kim Y, Lee JH, et al. Drug-induced liver injury: A 2-year retrospective study of 1169 hospitalized patients in a single medical center. Phytomedicine. 2015;22:1201–1205. doi: 10.1016/j.phymed.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 18.Hou FQ, Zeng Z, Wang GQ. Hospital admissions for drug-induced liver injury: clinical features, therapy, and outcomes. Cell Biochem Biophys. 2012;64:77–83. doi: 10.1007/s12013-012-9373-y. [DOI] [PubMed] [Google Scholar]
- 19.Shen T, Liu Y, Shang J, Xie Q, Li J, Yan M, et al. Incidence and Etiology of Drug-Induced Liver Injury in Mainland China. Gastroenterology. 2019;156:2230–2241.e11. doi: 10.1053/j.gastro.2019.02.002. [DOI] [PubMed] [Google Scholar]
- 20.Zhang P, Ye Y, Yang X, Jiao Y. Systematic review on Chinese herbal medicine induced liver injury. Evid Based Complement Alternat Med. 2016;2016:3560812. doi: 10.1155/2016/3560812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lai RT, Wang H, Gui HL, Ye MZ, Dai WJ, Xiang XG, et al. Clinical and pathological features in 138 cases of drug-induced liver injury. Zhonghua Gan Zang Bing Za Zhi. 2012;20:185–189. doi: 10.3760/cma.j.issn.1007-3418.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 22.Wang R, Qi X, Yoshida EM, Méndez-Sánchez N, Teschke R, Sun M, et al. Clinical characteristics and outcomes of traditional Chinese medicine-induced liver injury: a systematic review. Expert Rev Gastroenterol Hepatol. 2018;12:425–434. doi: 10.1080/17474124.2018.1427581. [DOI] [PubMed] [Google Scholar]
- 23.Ou P, Chen Y, Li B, Zhang M, Liu X, Li F, et al. Causes, clinical features and outcomes of drug-induced liver injury in hospitalized patients in a Chinese tertiary care hospital. Springerplus. 2015;4:802. doi: 10.1186/s40064-015-1600-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Udayakumar N, Subramaniam K, Umashankar L, Verghese J, Jayanthi V. Predictors of mortality in hepatic encephalopathy in acute and chronic liver disease: a preliminary observation. J Clin Gastroenterol. 2007;41:922–926. doi: 10.1097/01.mcg.0000225639.45157.ee. [DOI] [PubMed] [Google Scholar]
- 25.Devarbhavi H, Dierkhising R, Kremers WK, Sandeep MS, Karanth D, Adarsh CK. Single-center experience with drug-induced liver injury from India: causes, outcome, prognosis, and predictors of mortality. Am J Gastroenterol. 2010;105:2396–2404. doi: 10.1038/ajg.2010.287. [DOI] [PubMed] [Google Scholar]
- 26.Philips CA, Paramaguru R, Joy AK, Antony KL, Augustine P. Clinical outcomes, histopathological patterns, and chemical analysis of Ayurveda and herbal medicine associated with severe liver injury-A single-center experience from southern India. Indian J Gastroenterol. 2018;37:9–17. doi: 10.1007/s12664-017-0815-8. [DOI] [PubMed] [Google Scholar]
- 27.Philips CA, Paramaguru R, Augustine P, Rajesh S, Ahamed R, George T, et al. A single-center experience on outcomes of complementary and alternative medicine use among patients with cirrhosis. Hepatol Commun. 2019;3:1001–1012. doi: 10.1002/hep4.1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Devarbhavi H, Choudhury AK, Sharma MK, Maiwall R, Al Mahtab M, Rahman S, et al. Drug-induced acute-on-chronic liver failure in Asian patients. Am J Gastroenterol. 2019;114:929–937. doi: 10.14309/ajg.0000000000000201. [DOI] [PubMed] [Google Scholar]
- 29.Zhu Y, Niu M, Wang JB, Wang RL, Li JY, Ma YQ, et al. Predictors of poor outcomes in 488 patients with herb-induced liver injury. Turk J Gastroenterol. 2019;30:47–58. doi: 10.5152/tjg.2018.17847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhao P, Wang C, Liu W, Chen G, Liu X, Wang X, et al. Causes and outcomes of acute liver failure in China. PLoS One. 2013;8:e80991. doi: 10.1371/journal.pone.0080991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhao P, Wang C, Liu W, Wang F. Acute liver failure associated with traditional Chinese medicine: report of 30 cases from seven tertiary hospitals in China. Crit Care Med. 2014;42:e296–e299. doi: 10.1097/CCM.0000000000000136. [DOI] [PubMed] [Google Scholar]
- 32.Lei X, Chen J, Ren J, Li Y, Zhai J, Mu W, et al. Liver damage associated with polygonum multiflorum Thunb.: A systematic review of case reports and case series. Evid Based Complement Alternat Med. 2015;2015:459749. doi: 10.1155/2015/459749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu Y, Wang Q, Yang J, Guo X, Liu W, Ma S, et al. Polygonum multiflorum Thunb.: A review on chemical analysis, processing mechanism, quality evaluation, and hepatotoxicity. Front Pharmacol. 2018;9:364. doi: 10.3389/fphar.2018.00364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jing J, Wang RL, Zhao XY, Zhu Y, Niu M, Wang LF, et al. Association between the concurrence of pre-existing chronic liver disease and worse prognosis in patients with an herb- Polygonum multiflorum thunb. induced liver injury: a case-control study from a specialised liver disease center in China. BMJ Open. 2019;9:e023567. doi: 10.1136/bmjopen-2018-023567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Thyagarajan SP, Jayaram S, Gopalakrishnan V, Hari R, Jeyakumar P, Sripathi MS. Herbal medicines for liver diseases in India. J Gastroenterol Hepatol. 2002;17(Suppl 3):S370–S376. doi: 10.1046/j.1440-1746.17.s3.30.x. [DOI] [PubMed] [Google Scholar]
- 36.Jorge OA, Jorge AD. Hepatotoxicity associated with the ingestion of Centella asiatica. Rev Esp Enferm Dig. 2005;97:115–124. doi: 10.4321/S1130-01082005000200006. [DOI] [PubMed] [Google Scholar]
- 37.Dantuluri S, North-Lewis P, Karthik SV. Gotu Kola induced hepatotoxicity in a child - need for caution with alternative remedies. Dig Liver Dis. 2011;43:500. doi: 10.1016/j.dld.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 38.Teschke R, Bahre R. Severe hepatotoxicity by Indian Ayurvedic herbal products: a structured causality assessment. Ann Hepatol. 2009;8:258–266. doi: 10.1016/S1665-2681(19)31777-6. [DOI] [PubMed] [Google Scholar]
- 39.Fleig W, Morgan MY, Hölzer M. The Ayurvedic drug LIV.52 in patients with alcoholic cirrhosis. Results of a prospective, randomized, double-blind, placebo-controlled clinical trial. J Hepatol. 1997;126:127. [Google Scholar]
- 40.Zhu Y, Li YG, Wang JB, Liu SH, Wang LF, Zhao YL, et al. Causes, features, and outcomes of drug-induced liver injury in 69 children from China. Gut Liver. 2015;9:525–533. doi: 10.5009/gnl14184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee CH, Wang JD, Chen PC. Risk of liver injury associated with Chinese herbal products containing radix bupleuri in 639,779 patients with hepatitis B virus infection. PLoS One. 2011;6:e16064. doi: 10.1371/journal.pone.0016064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jakkula M, Boucher TA, Beyendorff U, Conn SM, Johnson JE, Nolan CJ, et al. A randomized trial of Chinese herbal medicines for the treatment of symptomatic hepatitis C. Arch Intern Med. 2004;164:1341–1346. doi: 10.1001/archinte.164.12.1341. [DOI] [PubMed] [Google Scholar]
- 43.Yuen MF, Tam S, Fung J, Wong DK, Wong BC, Lai CL. Traditional Chinese medicine causing hepatotoxicity in patients with chronic hepatitis B infection: a 1-year prospective study. Aliment Pharmacol Ther. 2006;24:1179–1186. doi: 10.1111/j.1365-2036.2006.03111.x. [DOI] [PubMed] [Google Scholar]
- 44.Philips CA, Augustine P, Padsalgi G. Herbal medicines and reactivation of chronic hepatitis B virus infection. Hepat Mon. 2018;18:e81000. doi: 10.5812/hepatmon.81000. [DOI] [Google Scholar]
- 45.Jing J, Teschke R. Traditional Chinese medicine and herb-induced liver injury: Comparison with drug-induced liver injury. J Clin Transl Hepatol. 2018;6:57–68. doi: 10.14218/JCTH.2017.00033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Frenzel C, Teschke R. Herbal hepatotoxicity: Clinical characteristics and listing compilation. Int J Mol Sci. 2016;17:E588. doi: 10.3390/ijms17050588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu C, Fan H, Li Y, Xiao X. Research advances on hepatotoxicity of herbal medicines in China. Biomed Res Int. 2016;2016:7150391. doi: 10.1155/2016/7150391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Teschke R, Eickhoff A. Herbal hepatotoxicity in traditional and modern medicine: actual key issues and new encouraging steps. Front Pharmacol. 2015;6:72. doi: 10.3389/fphar.2015.00072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ma X, Peng JH, Hu YY. Chinese herbal medicine-induced liver injury. J Clin Transl Hepatol. 2014;2:170–175. doi: 10.14218/JCTH.2014.00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Philips CA, Paramaguru R, Augustine P. Severe alcoholic hepatitis in a teetotaler. Am J Gastroenterol. 2018;113:1260–1261. doi: 10.1038/s41395-018-0154-0. [DOI] [PubMed] [Google Scholar]
- 51.Philips CA, Augustine P, Paramaguru R, Ahamed R. Homeopathy-medicine induced severe alcoholic hepatitis. BMJ Case Rep. 2019;12:e229627. doi: 10.1136/bcr-2019-229627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Philips CA, Paramaguru R, Augustine P. Ayurveda metallic-mineral ‘Bhasma’-associated severe liver injury. BMJ Case Rep. 2018;2018:bcr-2018-225590. doi: 10.1136/bcr-2018-225590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Philips CA, Augustine P, Paramaguru R, Ahamed R, Padsalgi G. Ayurveda herbal medicine-induced liver cirrhosis. Cureus. 2019;11:e4122. doi: 10.7759/cureus.4122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kotecha VR. Ayurveda research publications: A serious concern. Ayu. 2015;36:1–2. doi: 10.4103/0974-8520.169004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Samal J, Dehury RK. The need and importance of incorporating academic research results in to the curricula of Ayurveda in India. J Clin Diagn Res. 2017;11:KA01–KA03. doi: 10.7860/JCDR/2017/26742.10112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kazim M, Puri SK, Dutta GP, Narasimham MV. Evaluation of Ayush-64 for blood schizontocidal activity against rodent and simian malaria parasites. Indian J Malariol. 1991;28:255–258. [PubMed] [Google Scholar]
- 57.Valecha N, Devi C, Joshi H, Shahi V, Sharma V, Lal S. Comparative efficacy of Ayush-64 vs chloroquine in vivax malaria. Current Science. 2000;78:1120–1122. [Google Scholar]
- 58.Wang JB, Zhu Y, Bai ZF, Wang FS, Li XH, Xiao XH. Guidelines for the diagnosis and management of herb-induced liver injury. Chin J Integr Med. 2018;24:696–706. doi: 10.1007/s11655-018-3000-8. [DOI] [PubMed] [Google Scholar]