Abstract
Objective: To describe the development of structure, process and outcome indicators that will advance the quality of walking rehabilitation for Canadians with spinal cord injury or disease (SCI/D) by 2020.
Method: A framework for the evaluation of the quality of walking rehabilitation was developed by experts in walking after SCI/D. A systematic literature review identified factors influencing walking outcomes and potential walking indicators. A Driver diagram analysis summarized the factors affecting walking outcomes and subsequently informed the selection of structure and process indicators. Psychometric properties and clinical utility of potential walking indicators were considered during the selection of outcome indicators.
Results: The structure indicator is the number of physical therapists using evidence-based walking interventions per number of ambulatory individuals with SCI/D. The process indicator is the number of received hours of walking interventions during inpatient rehabilitation per number of ambulatory individuals with SCI/D. The intermediary outcome indicator, which is collected at discharge from inpatient rehabilitation, is either the modified Timed Up and Go or the 10-Meter Walk Test, the choice of measure is dictated by the stage of walking recovery, as defined by the Standing and Walking Assessment Tool. The final outcome indicator, collected at 18 months post-discharge, is the Spinal Cord Independence Measure III-Mobility subscale.
Conclusion: The selected indicators align with current clinical practice in Canada. The indicators will direct the timing and enhance the volume of walking therapy delivered, to ultimately increase the proportion of patients who achieve their walking potential by 18 months post-rehabilitation.
Keywords: Walking, Healthcare Quality indicators, Rehabilitation, Gait, Spinal cord injuries
Introduction
Regaining the ability to walk is a prime concern for individuals living with spinal cord injury or disease (SCI/D), especially among those with incomplete injuries.1,2 Walking is reported to be a higher priority among individuals early after SCI (i.e. <2 years post-injury) than among those with more chronic injuries (i.e. ≥5 years post-injury).2 The likelihood of return to walking after SCI is largely dependent upon injury severity (neurological level of injury (NLI) and American Spinal Injury Association Impairment Scale (AIS) grade).3–5 Return to walking is a realistic goal for those with motor incomplete SCI (AIS grades C and D and lower extremity motor score (LEMS) more than 20),6 as up to 75% of these individuals will regain some walking ability in the first year after injury.3 Conversely, the proportion who regain walking is much smaller among those with motor complete injury (i.e. AIS A and B); 20–50% of individuals diagnosed with AIS B injuries in acute care walk to some extent at one-year post-injury, while those with AIS A injuries rarely do.3 Early intervention to promote the recovery of walking is desirable to leverage the heightened potential for neuroplasticity7,8 and augment the natural recovery that occurs during the first year post-injury.9
With respect to walking, recovery is greatest during the first 9–12 months after injury onset and plateaus at around 12–18 months.3 Given that the mean duration of inpatient rehabilitation is 78 days (IQR 64 days) in Canada,10 this is the optimal time for individuals with SCI to participate in individually customized walking training regimens. Presently, walking rehabilitation after SCI/D is focused on those with the greatest potential to walk. A large multi-site study in the United States reported that 36% of inpatients with SCI participated in interventions targeting walking.11 A majority (96%) of whom had AIS D impairment received, on average, 7.5 ± 6.1 h of walking training during their inpatient stay.11 The mean time spent on walking was 60 min per week; this training time exceeded the mean time spent on other activities, such as bed mobility, stretching, strengthening and transfers.11
In Canada, interventions targeting walking have similarly focused on inpatients with SCI/D who are ambulatory (i.e. AIS D) or have the potential to become ambulatory. These individuals were observed to engage in high-intensity activities during inpatient physical therapy, such as walking and leg cycling.12 In a single physical therapy session, participants took a median of 51 steps (interquartile range: 0–176 steps) at admission to inpatient rehabilitation, and this volume of training increased to a median of 115 steps (interquartile range: 21–313 steps) by discharge.13 Metrics such as the duration of walking training (minutes) and the number of steps per training session facilitate evaluation of therapy intensity or volume. Despite the potential clinical utility of these metrics, the number of steps or the duration of walking training are not currently collected using systematic, standardized methods in Canadian SCI/D rehabilitation clinical settings; although they are routinely used in research settings in Alberta, British Colombia, Ontario, and Quebec.
In addition to the aforementioned therapy metrics, psychometrically sound measures of walking are important for accurate monitoring and intervention selection during inpatient SCI/D rehabilitation, and monitoring individuals with SCI/D as they transition to outpatient and/or community rehabilitation services. Incorporation of these measures supports the notion that service delivery models should be data-driven, and not dictated by inpatient rehabilitation length of stay.14
Walking assessment in SCI rehabilitation and related research settings has focused on timed measures of walking, such as the 6-minute walk test (6MWT) and 10-meter walk test (10MWT).15,16 The 6MWT measures the distance walked overground in six minutes, while the 10MWT measures the time taken to walk 10 m overground. In Canada, the 6MWT and 10MWT are two walking measures included in the Standing and Walking Assessment Tool (SWAT).17 The SWAT has been implemented at a national level through the Rick Hansen SCI Registry (RHSCIR)18,19 as current best practice for walking assessment during inpatient SCI rehabilitation. The SWAT was developed to address the need for a standardized approach to the assessment of walking during inpatient SCI rehabilitation.20 The SWAT is a staging tool routinely completed at rehabilitation admission and discharge, or when a patient changes stage on the SWAT; whereby, a patient’s stage of walking recovery is used to inform the selection of walking measures to describe and evaluate walking ability during inpatient rehabilitation.17 The SWAT data elements are included in RHSCIR 2.0 and 3.0, enabling site-specific and national-level evaluation of walking outcomes after SCI.21 Implementation of SWAT in clinical practice, however, has been incomplete,21 and further attention is required to support the implementation of walking assessment during inpatient SCI/D rehabilitation.
The Spinal Cord Injury Rehabilitation Care High Performance Indicators (SCI-High) Project provided an opportunity to address a priority domain of rehabilitation care related to walking during and following inpatient SCI/D rehabilitation. The overarching aim of the SCI-High Project is to advance SCI/D rehabilitation care, both inpatient and outpatient, for Canadians in the first 18 months after inpatient rehabilitation admission by the year 2020 through the development and implementation of indicators prioritized by clinicians, researchers and individuals living with chronic SCI/D. Quality of care indicators are widely used to identify trends, inform priority setting and policy formulation, and monitor rehabilitation programs and care processes at macro (health system), meso (organization) and micro (patient) levels. Indicators can measure the structure, process or outcome of health care services and their evaluation can facilitate the sustainability of a high-quality health care delivery system that is based on evidence-informed programs and services.22 Structure indicators are defined by the properties of the setting in which the health care services occur23 while a process indicator describes the specific activities in providing and receiving of care.24 Finally, an outcome indicator evaluates health improvements (or deterioration) attributable to the health care or therapy provided, such as mortality, morbidity, health status, health-related quality of life and patient/family/provider satisfaction as a result of the care.24 Indicator data can inform comparisons across different health care settings and systems to ensure continuous quality improvement and the establishment of benchmarks for superior organizations.25,26 This paper describes the context and approach to the development of the Walking indicators for application during the first 18 months after SCI/D rehabilitation admission. The Working Group’s objective was to establish a comprehensive framework of structure, process and outcome indicators specific to the domain construct of Walking for implementation in the Canadian rehabilitation health system environment.
Methods
The SCI-High Project aims to select, implement and evaluate indicators of quality care for 11 domains of SCI rehabilitation in Canada by 2020. A detailed description of the overall SCI-High Project methods and process for identifying Walking as a priority domain for SCI/D rehabilitation care are described in related manuscripts in this issue.27,28 In addition to the Project Team (www.sci-high.ca), an External Advisory Committee, National Data Strategy Committee, and a local quality committee consisting of spinal cord rehabilitation leadership supported the global project goals and provided oversight regarding the context for pilot implementation of planned indicators.
In brief, the approach to developing the Walking Domain structure, process and outcome indicators followed a modified, but substantially similar, approach to that described by Mainz et al.,25 which included the following planning and development phases: (a) formation and organization of the national and local Working Groups; (b) defining and refining the key domain and specific target construct; (c) providing an overview or summary of existing evidence and practice; (d) developing and interpreting a Driver diagram; (e) selecting indicators; and (f) pilot testing and refinement of the domain-specific structure, process and outcome indicators. Throughout these processes, a facilitated discussion occurred amongst the domain-specific Working Group and the SCI-High Project Team to utilize relevant expertise on the topic, while ensuring the broader goals of the SCI-High Project were aligned across the other 10 domain Working Groups (as appropriate).
Experts in walking and relevant stakeholders were invited to participate in the SCI-High Project as members of the domain-specific Working Group based on their practical or empirical knowledge of SCI/D rehabilitation, walking, and patient care. The group was composed of physiotherapists, physiatrists, rehabilitation scientists and postdoctoral fellows. Four meetings of the Walking Working Group were held between February 2016 and June 2017 via conference call, totaling four hours of discussion when developing the indicators, and for an additional two hours thereafter, to refine the indicators and discuss manuscript preparation. The efforts of this Working Group were bootstrapped by the existing SWAT Working Group and their clinical and research activities.29 In addition, individual members of the Working Group completed their own independent review of the prepared materials, shared resources and/or practice standards, with one another, or conducted independent evaluations of the proposed indicators via email or teleconference outside of the formal scheduled meetings.
The Working Groups were asked to develop/select at least one structure, process and outcome indicator related to the Walking Domain. The Project Team stipulated that the indicators must be relevant, concise (10 min or less to implement), feasible, and aligned across the structure, process and outcome indicator in achieving a single substantive advance in SCI/D rehabilitation care. The indicators could be measured using established or new measurement tools (i.e. questionnaires, data collection sheets, laboratory exams, medical record data), depending on the requirements and feasibility of a given indicator.
Domain-specific Working Group meetings
A national Working Group of subject matter experts was assembled to identify quality indicators for walking rehabilitation after SCI/D. The meetings were organized to frame the context for clinical decision making using an, “eliminate and concentrate” decision-making approach to review the key constructs related to Walking, review available outcome indicators and develop an evidence-informed Driver diagram to establish three indicators of the quality of walking rehabilitation for implementation from the time of rehabilitation admission to 18 months post-injury. Initially, the Working Group used a systematic method that combined scientific evidence and expert consensus for developing a construct definition for walking after SCI/D. In addition, a small number of fundamental and strategically important indicators for the construct of Walking, which were deemed feasible to collect at a clinical level, were selected via consensus. The selection of structure, process and outcome indicators involved a literature search followed by consideration of the factors affecting walking rehabilitation using an Ishikawa (fishbone) or Driver diagram.30
Literature search
A comprehensive literature search using MEDLINE, CINAHL and EMBASE applying the MeSH terms “walking” and “spinal cord injury” was conducted by two members of the Project Team independently (MA, MO). The search aimed to identify potential outcome indicators for Walking, as well as the factors that influence walking outcomes in SCI/D rehabilitation. Non-English manuscripts and inappropriate study designs were excluded.
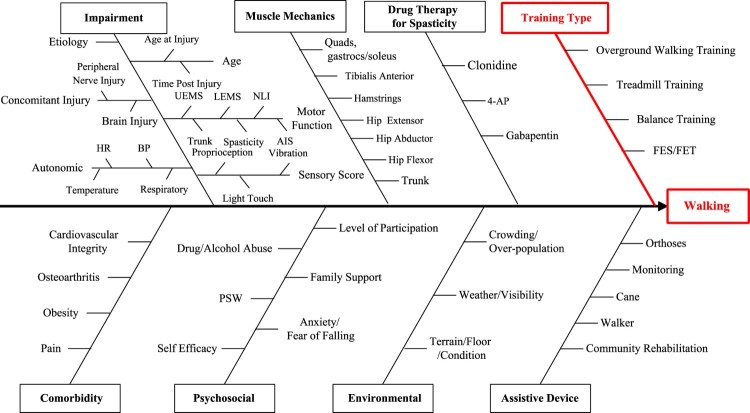
Driver diagram
Following the literature search, the challenge of selecting quality indicators was facilitated by creation of a Driver diagram, which has been reported to enable a root cause analysis of a given problem or situation.30 As part of the analysis, a graphic illustration was constructed to convey the relationships between SCI/D rehabilitation care related to walking, and factors that influence walking outcomes. Following review of the literature search results, the Walking Working Group engaged in a mind-mapping exercise to identify the factors that affect walking. Subsequently, the identified factors were grouped into categories (Fig. 1). Guided by the Driver diagram using RAND/UCLA31 methodology, the Walking Working Group proposed structure, process and outcome (intermediary and final) indicators for the quality of walking rehabilitation to be pilot tested for feasibility at the Lyndhurst Centre, Toronto Rehabilitation Institute-University Health Network, Toronto Canada.
Figure 1.
Walking Domain Driver diagram. UEMS: Upper-Extremity Motor Score; LEMS: Lower-Extremity Motor Score; NLI: Neurological Level of Injury; AIS: ASIA Impairment Scale; HR: Heart Rate; BP: Blood Pressure; 4-AP: 4-Aminopyridine; FES: Functional Electrical Stimulation; FET: Functional Electrical Training; PSW: Personal Support Worker.
Results
Construct definition
The following construct definition was developed by the Walking Working Group to guide the selection of quality indicators:
Walking is the ability to move forward over ground using voluntary lower limb movement while controlling one's balance in an upright posture. Safe and efficient walking allows individuals to move purposefully from place to place to explore and participate in their external environments, with or without the assistance of others and/or assistive technologies – in other words, to be independent moving about their home and community, and in their life activities.
The Walking Working Group further delineated ambulatory individuals with SCI/D as those individuals who were staged at 2A on the SWAT stages: maximum assist for therapeutic walking indoors17 (Table 1).
Table 1. Canadian SCI Standing and Walking Assessment Toolkit (SWAT) Stages of Walking Recovery ©RHSCIR Canadian SCI Standing and Walking Module Group on behalf of Rick Hansen Institute, 2014.
| Stage | Classification | Definition |
|---|---|---|
| 0.0 | No independent sitting capacity | Patient is unable to sit independently of a seating system on a firm surface with hips and knees at 90 degrees and feet on the floor for 60 s without using arms to stabilize. |
| 0.5 | Independent sitting capacity | Patient is able to sit independently of a seating system on a solid surface with hips and knees at 90 degrees and feet on the floor for 60 s without using arms to stabilize. |
| 1 | No walking capacity | Patient cannot ambulate but may be able to stand with total assistance |
| 1A | No lower extremity movement | Unable to stand without total assistance of gait aid and/or orthoses and/or therapist(s). No voluntary LE functional movement (L/E MMTs Gr 1 or less in: Tib. Ant and soleus, Quads, and Gluteus.) |
| 1B | Voluntary non-functional lower extremity movement | Unable to stand independently/Needs partial assistance of gait aid and/or orthoses (except bilateral KAFOs) and/or therapist(s) to stand. The use of Bilateral KAFOs is not allowed. Voluntary L/E Movement (L/E MMTs of Gr 1+/2- to Gr3- in anti-gravity muscles*). |
| 1C | Voluntary functional lower extremity movement | Able to stand independently with minimal assistance of gait aid for limited amount of time (less than 30 secs). Orthoses are allowed except for Bilateral KAFOs. Voluntary L/E Movement. (L/E MMTs of Gr 3 or higher in most anti-gravity muscles* except Gr 1 Tib. Ant with an orthoses would fit this group.) |
| 2 | Therapeutic walking capacity (Indoors) | Patient is starting to ambulate with Therapist Assistance and Gait Aids/Orthoses and progresses toward Minimal Assistance. |
| 2A | Maximum assistant | Ability to stand and initiate reciprocal steps through voluntary L/E movement but requires maximal physical assistance (>50% of total effort) of at least one person and may include use of assistive devices and/or orthoses with the exception of bilateral KAFOs. |
| 2B | Moderate assistant | Ability to stand and initiate reciprocal steps through voluntary L/E movement but requires moderate physical assistance (25–50% of total effort) of one person and may include use of assistive devices and/or orthoses with the exception of the bilateral KAFOs |
| 2C | Minimum assistant | Ability to stand and initiate reciprocal steps through voluntary L/E movement but requires minimal physical assistance (<25% of total effort) of one person and may include use of assistive devices and/or orthoses with the exception of the bilateral KAFOs. |
| 3 | Functional walking capacity (outdoors) | Patient is starting to ambulate without Therapist Assistance but still requires Gait Aids/Orthoses. Patient progresses to ambulating in the Community. |
| 3A | Supervised household ambulator | Ability to ambulate daily using reciprocal steps over ground for short distances (10–100 m) with supervision. Person may use assistive devices and /or orthoses with the exception of bilateral KAFOs. |
| 3B | Independent household ambulator | Ability to ambulate daily using reciprocal steps over ground for short distances (10–100 m) independently. Person may use assistive devices and/or orthoses with the exception of the bilateral KAFOs. |
| 3C | Community ambulator | Ability to ambulate daily using reciprocal steps over ground for long distances (>100 m) independently. Person may use assistive devices and/or orthoses with the exception of the bilateral KAFOs. |
| 4 | Full walking capacity | Patient ambulates independently without Therapist Assistance or Gait Aids/Orthoses. Independent Ambulator – ability to ambulate full time daily at home and in the community without assistive devices, orthoses, or physical assistance. |
Driver diagram
Using the comprehensive search strategy, potential outcome indicators were identified (Table 2), as well as factors that influence walking (Fig. 1). Overall, numerous factors influence walking outcomes during SCI/D rehabilitation, with impairment-related factors being the most frequent. The Walking Working Group arranged the factors that influence the outcome of walking into eight categories: Impairment, Muscle Mechanics, Drug Therapy for Spasticity, Training Type, Comorbidity, Psychosocial, Environmental, and Assistive Device. Figure 1 shows the Driver diagram for walking among individuals with SCI/D within these categories.
Table 2. List of walking outcome measures.
Selected indicators
Structure indicator: This indicator reflects the delivery of walking rehabilitation. As suggested by the “Training” backbone in the Driver diagram (Fig. 1), walking training after SCI/D consists of task-specific and repetitive practice.36 All walking training methods listed on the “Training” branch of the Driver diagram embody these training principles. The literature on walking training after SCI/D, however, does not support one mode of training over another.36 For this reason, rather than selecting a physical structure or piece of equipment as the structure indicator, the Walking Working Group chose to describe the physical therapy expertise. The selected structure indicator is the number of physical therapists at a given rehabilitation site, whom demonstrate regular use of evidence-based interventions for walking rehabilitation (see “Training” branch, Fig. 1) after SCI/D, per total number of physical therapists participating in walking intervention service provision at each site in a fiscal year. Here ‘regular use’ means that evidence-based walking interventions are used with all patients with SCI/D who are ambulatory. The structure indicator is to be collected and reported annually.
Process indicator: This indicator reflects the appropriateness of the health care received with respect to walking rehabilitation. Given that walking gains are typically dose-dependent (i.e. the greater the amount of walking practice, the greater the gains),7,37 the process indicator is the total number of hours of evidence-based walking training received. Physical therapists will enter the total number of minutes spent on walking training as part of their daily workload documentation. This indicator is to be calculated (sum of training minutes) for each patient with SCI/D who meet the requirements of SWAT [stage 2a or higher (Table 1)] at the time of discharge from inpatient rehabilitation. Integral to the accurate reporting of this quality indicator is a clear guideline of what therapeutic interventions are considered to be walking interventions. The Walking Working Group agreed upon two criteria for therapists to consider when determining whether a therapeutic activity could count as part of the process of walking rehabilitation. First, the therapeutic activity must be undertaken with the goal of walking in mind. Second, the therapeutic activity must involve whole-or part-practice of walking as task-specificity is deemed a training parameter associated with gains in overground walking function.7,36 To facilitate the reporting of the process indicator (i.e. minutes spent engaged in walking training), the Walking Working Group adapted the Physical Therapy Taxonomy created by the SCIRehab Project.38 The time spent on each of the 19 activities listed in the Taxonomy was used as a measure of intensity by the SCIRehab researchers and clinicians.38 For the purposes of the SCI-High process indicator for walking, 12 activities listed in the SCIRehab Taxonomy were removed as they did not involve whole- or part-practice of walking (e.g. bed mobility, wheelchair mobility, range of motion/stretching, airway/respiratory management, education). Other activities were modified to increase the task-specificity for walking. For example, transfers between sitting and standing were deemed important for the task of walking, while other transfer types found in the SCIRehab Taxonomy were excluded. Further, while the SCIRehab Taxonomy included stair-climbing under the activity of Gait, the Walking Working Group chose to list Stairs as an independent activity, as ascending and descending steps or stairs are commonly performed in daily life.39 Lastly, the aquatic environment was not listed as an independent activity as it is in the SCIRehab Taxonomy, but rather it was considered as another medium for walking training. Thus, six therapeutic activities were included in the SCI-High taxonomy of walking interventions to support documentation of the process indicator (Table 3).
Table 3. Taxonomy of walking interventions for process indicator tracking.
| Walking interventions* | |
|---|---|
| Transfers | Between sitting and standing |
| Pre-gait activities | Part-practice of gait events & Standing activities |
| Gait | Whole practice of gait |
| Balance | Challenged during whole-gait |
| Endurance | Challenged during whole-gait |
| Stairs | Part or whole practice of ascending or descending stairs |
*Interventions may include use of orthoses, electrical stimulation, gait aids, body weight support, physical assistance and the aquatic environment.
Intermediary outcome indicators: The literature review revealed multiple walking measures that have been used with the SCI/D population. The list of measures was reduced by identifying those with high clinical utility and strong psychometric properties in individuals with SCI/D. Factors contributing to a measure’s clinical utility include the time, expense and training required to administer the measure.40 Six measures of walking were identified as having high clinical utility and established psychometric properties in individuals with SCI/D (Table 2). From this list of six measures, the 10MWT (completed at a comfortable speed) and the modified Timed Up and Go (mTUG) were selected as the intermediary outcome indicators. These measures will be completed within the five days prior to discharge from inpatient SCI/D rehabilitation. The 10MWT has been recommended previously for use with individuals with SCI/D by numerous groups of expert clinicians and researchers.15,17,41 Further, it is a walking measure that has been reported to change in response to inpatient SCI rehabilitation.42 The disadvantage of the 10MWT, however, is that it is appropriate only for those individuals with SCI who can walk without the assistance of another person (i.e. stage 3B or greater on the SWAT).17 Hence the mTUG,34 which accounts for the level of physical assistance in the scoring, was included as an intermediary outcome indicator for those individuals unable to walk without the physical assistance of another person (i.e. SWAT stages 2A, 2B, 2C and 3A).
Final outcome indicator: The main consideration when selecting the final outcome indicator was the feasibility of completion. Since this quality indicator is evaluated at 18 months post-discharge from inpatient rehabilitation, a measure that can be completed via survey from the patients’ home environments was desired. Therefore, the SCIM III Mobility sub-scale was selected because, as a self-report measure, it can be completed over the phone.43,44 Table 4 summarizes the selected structure, process and outcome indicators for the Walking Domain.
Table 4. Selected structure, process and outcome indicators for the Walking Domain, and the related denominator for calculating the indicator and the time of collection.
| Indicator | Denominator | Indicator type | Time of measurement |
|---|---|---|---|
| Number of therapists who demonstrate regular use* of evidence-based walking interventions | Total number of therapists participating in walking intervention service provision at each site per FY | Structure | Annual |
| Total hours of received interventional therapies contributing to walking | Number of ambulatory individuals with SCI/D (SWAT Levels 2A or higher) | Process | Rehabilitation discharge |
| Proportion of ambulatory individuals with SCI/D* that completed a mTUG or 10MWT | Number of ambulatory individuals with SCI/D (SWAT Levels 2A or higher) | Outcome – Intermediary | Within 5 days prior to rehabilitation discharge |
| SCIM III Self-Report, Mobility subscale | Number of ambulatory patients with SCI/D (SWAT Levels 2A or higher) | Outcome – Final | 18 months post rehabilitation admission |
*Regular use implies use of evidence-based walking interventions with all patients with SCI/D who are ambulatory.
FY = Fiscal Year; SWAT = Standing and Walking Assessment Tool; mTUG = modified Timed Up and Go Test; 10MWT = 10 Meter Walk Test; SCIM III = Spinal Cord Independence Measure, Version III.
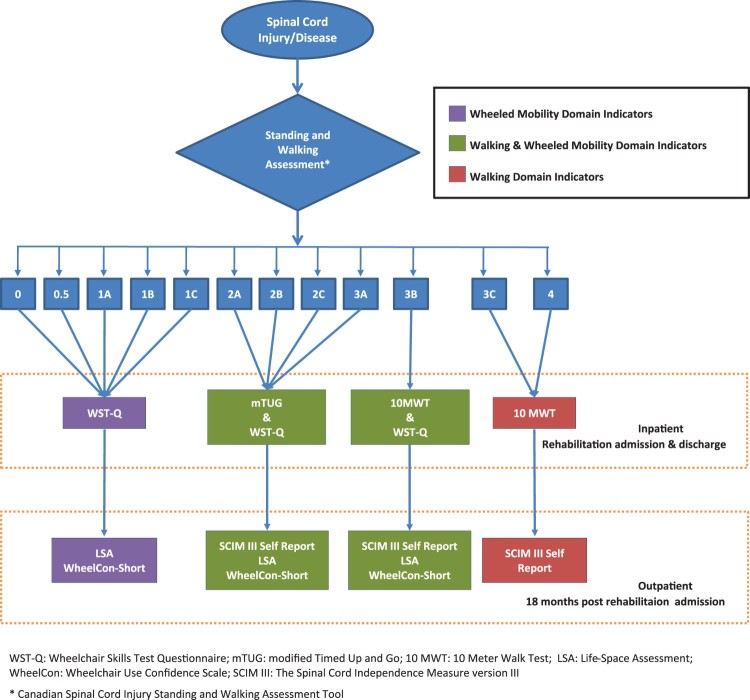
The identified outcome indicators are appropriate for use with individuals who are ambulatory (i.e. SWAT stage 2A or higher). For non-ambulatory individuals (i.e. SWAT stages 1A, 1B and 1C), the wheelchair mobility indicators will be used.45 As some individuals with SCI/D will be wheeling and walking, the Walking Working Group consulted with clinicians to define when: (a) wheelchair mobility indicators should be collected, (b) patients had progressed sufficiently to collect indicators for both wheeling and walking, and (c) walking indicators alone are appropriate to collect. The thresholds for which domain indicators should be collected (i.e. walking or wheeling) are based on the SWAT stages (Fig. 2).
Figure 2.
SCI-High Walking and Wheeled Mobility Domain indicator decision tree. Appropriate indicator data collection in based on the patient's stage of standing and walking recovery ascertained using the Canadian SCI Standing and Walking Assessment Tool.17 The Figure is intended to help clinicians decide when it is appropriate or not to collect Walking or Wheeled Mobility indicators, or both, based on the individual's stage of standing and walking recovery.
Discussion
A comprehensive framework of structure, process and outcome indicators for the quality of walking rehabilitation, as measured during inpatient rehabilitation and post-discharge in the community, was developed (Table 4). The structure, process and outcome indicators were selected in part due to their likelihood of implementation and sustainability. This emphasis on clinical feasibility was a strength of the approach used by the Walking Working Group and the SCI-High Project Team. The intermediary and final outcome indicators (i.e. 10MWT, mTUG and SCIM III Mobility subscale) are commonly used measures in physical therapy practice in Canada. Workload documentation, albeit not specific to walking interventions, is also familiar to physical therapists working in publicly-funded rehabilitation hospitals and clinics. Implementation of the Walking Domain indicators in clinical practice will be facilitated through standardized timing for collection of the process and outcome indicators using established documentation tools. Implementation may be further facilitated by accessing pre-existing SCI/D networks or communities of practice, such as the Canadian SCI Walking and Standing Module Group, to assist with the dissemination of knowledge concerning the SCI-High Walking Domain indicators.
Implementation of the structure, process and outcome indicators for walking will impact Canadian SCI/D rehabilitation practices. Through collection and analysis of the Walking indicator data, rehabilitation administrators will have site-specific metrics concerning the quality of walking rehabilitation that can be compared to national-level benchmarks. This information may be used to modify site-specific practices, as well as inform provincial-level funding policy decisions and advances in care nationally. For example, the Walking indicators will provide objective data concerning the amount of evidence-based walking interventions received by individuals with SCI/D. Short lengths of hospital stay are known to impact the type and intensity of walking interventions delivered in the USA.2 During these short hospital stays, instead of focusing on walking, the frequent priority in rehabilitation was wheeled mobility, a skill which enables sufficient independence for discharge.2 The reader is encouraged to review the related manuscript describing the indicators associated with wheeled mobility.45 Likewise, collection and analysis of intermediary and final outcome indicators will provide an objective description of the trajectory of walking recovery after inpatient rehabilitation among ambulatory individuals with SCI/D, providing insight into whether the current duration of inpatient rehabilitation in Canada10 is optimal or sub-optimal to address walking deficits in this population. Health system barriers, such as length of stay, are difficult to overcome; however, the Walking indicators may provide valuable data that contributes to future policy discussions.
Collection of the Walking indicators will be undertaken by physical therapists working within inpatient SCI/D rehabilitation settings, consequently impacting their workload. The burden of the documentation requirements for the Walking indicators has not yet been evaluated; however, based on previous initiatives and literature concerning the use of standardized outcome measures by physical therapists, we may anticipate some barriers to implementation of the Walking indicators. Previous initiatives involving the implementation of outcome measures by physical therapists have identified the following barriers: a perceived lack of confidence in using outcome measures, constraints of the clinical environment (i.e. lack of space, time and measurement tools), and the challenges associated with changing behavior.46,47 Specific to use of the SWAT during inpatient SCI rehabilitation in Canada, the following factors were identified as barriers to implementation: lack of time, unfamiliarity with the tool, lack of workplace policy requiring completion of the SWAT, lack of applicability to patients who are outliers with respect to walking recovery and reluctance to complete in patients with poor gait quality.21 As the indicators of walking rehabilitation quality are implemented at Canadian SCI/D rehabilitation sites, ongoing training sessions and support for inpatient physical therapists will be offered by the SCI-High Project Team to discern when wheeled mobility or Walking indicators should be collected. These sessions will address barriers to implementation through joint problem-solving. Similar targeted knowledge translation activities have resulted in increased use and interpretation of standardized outcome measures by physical therapists in acute care settings.48
Selection of the Walking Domain indicators involved consideration of Canadian SCI/D rehabilitation practice context; hence, the generalizability of the framework of structure, process and outcome indicators for Walking to other clinical settings outside Canada may be limited. For example, physical therapy expertise was selected as the structure indicator; however, in other parts of the world, other health care professionals and/or support workers may be the drivers of walking recovery after SCI/D. In addition, the timing of measurement of Walking indicators that is outlined here (Table 4) also may not align with health care practices outside of Canada, due to varying lengths of hospital stay and access to rehabilitation after SCI/D. Implementation of a similar framework of quality indicators for walking rehabilitation outside of Canada would require modification of the framework to match the local health care practice and health system design.
Conclusion
We have described the process for the identification of the Walking Domain quality indicators for inpatient SCI/D rehabilitation in Canada. Structure, process and outcome indicators that reflect, at a high level, the quantity and quality of therapeutic interventions targeting walking have been selected. Standardized timing for documentation of walking interventions and outcomes will be used to optimize rehabilitative care and promote enhanced walking ability after SCI/D. Facilitation of clinician-, site-, and national-level reflection of current practices, coupled with ongoing review of the collated indicators and related practices will be performed to transform health service delivery for individuals with SCI/D.
Disclaimer statements
Contributors None.
Conflicts of interest Dr. B. Catharine Craven acknowledges support from the Toronto Rehab Foundation as the Toronto Rehabilitation Institute Chair in Spinal Cord Injury Rehabilitation and receipt of consulting fees from the Rick Hansen Institute. Dr. S. Mohammad Alavinia, Farnoosh Farahani, Heather Flett, Dr. Kristin E. Musselman, Dr. Sylvie Nadeau, Maryam Omidvar, Prof. Molly C. Verrier, Dr. Matheus J. Wiest and Dr. Jaynie F. Yang report no conflicts of interest.
Supplementary Material
Funding Statement
This work is embedded in the larger SCI-High Project funded by the Rick Hansen Institute (Grant #G2015-33), Ontario Neurotrauma Foundation (ONF; Grant #2018 RHI-HIGH-1057), and Toronto Rehabilitation Institute Foundation.
ORCID
Kristin E. Musselman http://orcid.org/0000-0001-8336-8211
Heather Flett http://orcid.org/0000-0001-9444-8006
Farnoosh Farahani http://orcid.org/0000-0002-3937-7708
S. Mohammad Alavinia http://orcid.org/0000-0002-5503-9362
Maryam Omidvar http://orcid.org/0000-0003-2415-8921
Matheus J. Wiest http://orcid.org/0000-0003-1444-4828
B. Catharine Craven http://orcid.org/0000-0001-8234-6803
References
- 1.Anderson KD. Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma. 2004;21(10):1371–83. doi: 10.1089/neu.2004.21.1371 [DOI] [PubMed] [Google Scholar]
- 2.Ditunno PL, Patrick M, Stineman M, Ditunno JF.. Who wants to walk? Preferences for recovery after SCI: a longitudinal and cross-sectional study. Spinal Cord. 2008;46(7):500–6. doi: 10.1038/sj.sc.3102172 [DOI] [PubMed] [Google Scholar]
- 3.Burns AS, Marino RJ, Flanders AE, Flett H.. Clinical diagnosis and prognosis following spinal cord injury. Handb Clin Neurol. 2012;109:47–62. doi: 10.1016/B978-0-444-52137-8.00003-6 [DOI] [PubMed] [Google Scholar]
- 4.Marino RJ, Ditunno JF Jr, Donovan WH, Maynard F Jr. Neurologic recovery after traumatic spinal cord injury: data from the Model Spinal Cord Injury Systems. Arch Phys Med Rehabil. 1999;80(11):1391–6. doi: 10.1016/S0003-9993(99)90249-6 [DOI] [PubMed] [Google Scholar]
- 5.Scivoletto G, Tamburella F, Laurenza L, Torre M, Molinari M.. Who is going to walk? A review of the factors influencing walking recovery after spinal cord injury. Front Hum Neurosci. 2014;8(141):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. . International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34(6):535–46. doi: 10.1179/204577211X13207446293695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kleim JA, Jones TA.. Principles of experience-dependent neural plasticity: implications for rehabilitation after brain damage. J Speech Lang Hear Res. 2008;51(1):S225–39. doi: 10.1044/1092-4388(2008/018) [DOI] [PubMed] [Google Scholar]
- 8.Onifer SM, Smith GM, Fouad K.. Plasticity after spinal cord injury: relevance to recovery and approaches to facilitate it. Neurotherapeutics. 2011;8(2):283–93. doi: 10.1007/s13311-011-0034-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Waters RL, Adkins RH, Yakura JS, Sie I.. Motor and sensory recovery following incomplete paraplegia. Arch Phys Med Rehabil. 1994;75(1):67–72. [PubMed] [Google Scholar]
- 10.Craven BC, Flett H, Hitzig SL, Farahani F, Alavinia SM, Omidvar M, et al. . Moving from prioritization to implementation: the spinal cord injury rehabilitation care high performance indicators (SCI-high) project. J Spinal Cord Med. 2017;40(6). WCA162, 865. [Google Scholar]
- 11.Taylor-Schroeder S, LaBarbera J, McDowell S, Zanca JM, Natale A, Mumma S, et al. . The SCIRehab project: treatment time spent in SCI rehabilitation. Physical therapy treatment time during inpatient spinal cord injury rehabilitation. J Spinal Cord Med. 2011;34(2):149–61. doi: 10.1179/107902611X12971826988057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zbogar D, Eng JJ, Noble JW, Miller WC, Krassioukov AV, Verrier MC.. Cardiovascular Stress during inpatient Spinal Cord injury rehabilitation. Arch Phys Med Rehabil. 2017;98(12):2449–56. doi: 10.1016/j.apmr.2017.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zbogar D, Eng JJ, Miller WC, Krassioukov AV, Verrier MC.. Movement repetitions in physical and occupational therapy during spinal cord injury rehabilitation. Spinal Cord. 2017;55(2):172–9. doi: 10.1038/sc.2016.129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Craven BC, Kurban D, Farahani F, Rivers CS, Ho C, Linassi AG, et al. . Predicting rehabilitation length of stay in Canada: it's not just about impairment. J Spinal Cord Med. 2017;40(6):676–86. doi: 10.1080/10790268.2017.1368962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jackson AB, Carnel CT, Ditunno JF, Read MS, Boninger ML, Schmeler MR, et al. . Outcome measures for gait and ambulation in the spinal cord injury population. J Spinal Cord Med. 2008;31(5):487–99. doi: 10.1080/10790268.2008.11753644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lam T, Noonan VK, Eng JJ, Team SR.. A systematic review of functional ambulation outcome measures in spinal cord injury. Spinal Cord. 2008;46(4):246–54. doi: 10.1038/sj.sc.3102134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Verrier M GD, Musselman K.. and the Canadian SCI Walking and Standing Module Group. Toolkit for SCI Standing and Walking Assessment. Rick Hansen Institute; September 2014 Available from https://scireproject.com/wp-content/uploads/Stand_and_Walk_toolkit.pdf.
- 18.Toolkit For SCI Standing and Walking Assessment [Internet] Rich Hansen Institute. 2017 [cited May 2, 2019]. Available from https://scireproject.com/wp-content/uploads/Stand_and_Walk_toolkit-2.pdf.
- 19.Rick Hansen Spinal Cord Injury Registry – A look at traumatic spinal cord injury in Canada in 2017. Vancouver, BC: RHI; 2018. Available from http://rickhanseninstitute.org/images/stories/Article_PDFs/SCI_Report_dec9_web1.pdf. [Google Scholar]
- 20.Craven BC, Verrier M, Balioussis C, PhD DW, Hsieh J, Noonan V, et al. . Rehabilitation Environmental Scan Atlas: Capturing Capacity in Canadian SCI Rehabilitation, Walking. Rick Hansen Institute; 2012. Available from http://168.144.170.22/research/scimanifesto/C__Walking/.
- 21.Musselman KE, Lemay JF, Walden K, Harris A, Gagnon DH, Verrier MC.. Physical Therapists’ Experiences With the SCI Standing and Walking Assessment Toolkit: An Exploratory Study. American Congress of Rehabilitation Medicine. Chicago: Archives of Physical Medicine & Rehabilitation; 2018.
- 22.Burns AS, Yee J, Flett HM, Guy K, Cournoyea N.. Impact of benchmarking and clinical decision making tools on rehabilitation length of stay following spinal cord injury. Spinal Cord. 2013;51(2):165–9. doi: 10.1038/sc.2012.91 [DOI] [PubMed] [Google Scholar]
- 23.Idvall E, Rooke L, Hamrin E.. Quality indicators in clinical nursing: a review of the literature. J Adv Nurs. 1997;25(1):6–17. doi: 10.1046/j.1365-2648.1997.1997025006.x [DOI] [PubMed] [Google Scholar]
- 24.Selim AJ, Berlowitz DR, Fincke G, Rosen AK, Ren XS, Christiansen CL, et al. . Risk-adjusted mortality rates as a potential outcome indicator for outpatient quality assessments. Med Care. 2002;40(3):237–45. doi: 10.1097/00005650-200203000-00007 [DOI] [PubMed] [Google Scholar]
- 25.Mainz J. Developing evidence-based clinical indicators: a state of the art methods primer. Int J Qual Health Care. 2003;15(Suppl. 1):i5–11. doi: 10.1093/intqhc/mzg084 [DOI] [PubMed] [Google Scholar]
- 26.Rubin HR, Pronovost P, Diette GB.. The advantages and disadvantages of process-based measures of health care quality. Int J Qual Health Care. 2001;13(6):469–74. doi: 10.1093/intqhc/13.6.469 [DOI] [PubMed] [Google Scholar]
- 27.Alavinia SM, Hitzig SL, Farahani F, Flett H, Bayley M, Craven BC.. Prioritization of rehabilitation domains for establishing spinal cord injury high performance indicators using a modification of the Hanlon method: SCI-High Project. J Spinal Cord Med. 2019;42(Suppl 1):S43–S50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Craven BC, Alavinia SM, Wiest MJ, Farahani F, Hitzig SL, Flett H, et al. . Methods for development of structure, process and outcome indicators for prioritized spinal cord injury rehabilitation domains: SCI-High Project. J Spinal Cord Med. 2019;42(Suppl 1):S51–S67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Musselman K, Lemay J, McCullum S, Guy K, Walden K.. Assessment of upright mobility after spinal cord injury: a “how-to” guide to the Canadian spinal cord injury standing and walking assessment tool. J Spinal Cord Med. 2017;40(6):813–69. doi: 10.1080/10790268.2017.1369666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Phillips J SL. Change management tools part 1: using analysis to investigate problems. Nurs Times. 2013;109:18–20. [PubMed] [Google Scholar]
- 31.Fitch K, Bernstein SJ, Aguilar MD, Burnand B, LaCalle JR, Lazaro P, et al. . The RAND/UCLA Appropriateness Method User's Manual. Santa Monica, CA: RAND Corporation; 2001. Available from https://www.rand.org/pubs/monograph_reports/MR1269.html.
- 32.van Hedel HJ, Wirz M, Dietz V.. Assessing walking ability in subjects with spinal cord injury: validity and reliability of 3 walking tests. Arch Phys Med Rehabil. 2005;86(2):190–6. doi: 10.1016/j.apmr.2004.02.010 [DOI] [PubMed] [Google Scholar]
- 33.Itzkovich M, Gelernter I, Biering-Sorensen F, Weeks C, Laramee M, Craven BC, et al. . The Spinal Cord Independence measure (SCIM) version III: Reliability and validity in a multi-center international study. Disabil Rehabil. 2007;29(23):1926–33. doi: 10.1080/09638280601046302 [DOI] [PubMed] [Google Scholar]
- 34.Musselman K, Brunton K, Lam T, Yang J.. Spinal cord injury functional ambulation profile: a new measure of walking ability. Neurorehabil Neural Repair. 2011;25(3):285–93. doi: 10.1177/1545968310381250 [DOI] [PubMed] [Google Scholar]
- 35.Dittuno PL, Ditunno JF Jr. Walking index for spinal cord injury (WISCI II): scale revision. Spinal Cord. 2001;39(12):654–6. doi: 10.1038/sj.sc.3101223 [DOI] [PubMed] [Google Scholar]
- 36.Yang JF, Musselman KE.. Training to achieve over ground walking after spinal cord injury: a review of who, what, when, and how. J Spinal Cord Med. 2012;35(5):293–304. doi: 10.1179/2045772312Y.0000000036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yang JF, Musselman KE, Livingstone D, Brunton K, Hendricks G, Hill D, et al. . Repetitive mass practice or focused precise practice for retraining walking after incomplete spinal cord injury? A pilot randomized clinical trial. Neurorehabil Neural Repair. 2014;28(4):314–24. doi: 10.1177/1545968313508473 [DOI] [PubMed] [Google Scholar]
- 38.Natale A, Taylor S, LaBarbera J, Bensimon L, McDowell S, Mumma SL, et al. . SCIRehab Project series: the physical therapy taxonomy. J Spinal Cord Med. 2009;32(3):270–82. doi: 10.1080/10790268.2009.11760781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Musselman KE, Yang JF.. Walking tasks encountered by urban-dwelling adults and persons with incomplete spinal cord injuries. J Rehabil Med. 2007;39(7):567–74. doi: 10.2340/16501977-0090 [DOI] [PubMed] [Google Scholar]
- 40.Tyson S, Connell L.. The psychometric properties and clinical utility of measures of walking and mobility in neurological conditions: a systematic review. Clin Rehabil. 2009;23(11):1018–33. doi: 10.1177/0269215509339004 [DOI] [PubMed] [Google Scholar]
- 41.Bolliger M, Blight AR, Field-Fote EC, Musselman K, Rossignol S, Barthelemy D, et al. . Lower extremity outcome measures: considerations for clinical trials in spinal cord injury. Spinal Cord. 2018;56(7):628–42. doi: 10.1038/s41393-018-0097-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zbogar D, Eng JJ, Miller WC, Krassioukov AV, Verrier MC.. Physical activity outside of structured therapy during inpatient spinal cord injury rehabilitation. J Neuroeng Rehabil. 2016;13(1):99. doi: 10.1186/s12984-016-0208-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Almeida C, Coelho JN, Riberto M.. Applicability, validation and reproducibility of the Spinal Cord Independence measure version III (SCIM III) in patients with non-traumatic spinal cord lesions. Disabil Rehabil. 2016;38(22):2229–34. doi: 10.3109/09638288.2015.1129454 [DOI] [PubMed] [Google Scholar]
- 44.Fekete C, Eriks-Hoogland I, Baumberger M, Catz A, Itzkovich M, Luthi H, et al. . Development and validation of a self-report version of the Spinal Cord Independence measure (SCIM III). Spinal Cord. 2013;51(1):40–47. doi: 10.1038/sc.2012.87 [DOI] [PubMed] [Google Scholar]
- 45.Bayley MT, Kirby RL, Titus L, Smith C, Routhier F, Gagnon D, et al. . Development of wheeled mobility indicators to advance the quality of spinal cord injury rehabilitation: SCI-High Project. J Spinal Cord Med. 2019;42(Suppl 1):S130–S140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Swinkels RA, van Peppen RP, Wittink H, Custers JW, Beurskens AJ.. Current use and barriers and facilitators for implementation of standardised measures in physical therapy in the Netherlands. BMC Musculoskelet Disord. 2011;12:106. doi: 10.1186/1471-2474-12-106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Van Peppen RP, Maissan FJ, Van Genderen FR, Van Dolder R, Van Meeteren NL.. Outcome measures in physiotherapy management of patients with stroke: a survey into self-reported use, and barriers to and facilitators for use. Physiother Res Int. 2008;13(4):255–70. doi: 10.1002/pri.417 [DOI] [PubMed] [Google Scholar]
- 48.McDonnell B, Stillwell S, Hart S, Davis RB.. Breaking Down barriers to the Utilization of standardized Tests and outcome measures in acute care physical Therapist practice: An Observational Longitudinal study. Phys Ther. 2018;98(6):528–38. doi: 10.1093/ptj/pzy032 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.