Abstract
Background: Acute visual loss is a common chief complaint in emergency department (ED) patients, but the scarcity of ophthalmologists in most EDs limits its evaluation.
Introduction: Our objective was to evaluate whether nonmydriatic fundus photography (NMFP) in the ED helps triage patients with acute visual loss.
Materials and Methods: We included 213 patients with acute visual loss evaluated in the ED with NMFP as part of the Fundus Photography versus Ophthalmoscopy Trial Outcomes in the ED studies. Demographics, referral patterns, results of NMFP, and final diagnoses were recorded.
Results: A final ophthalmological diagnosis was made in 109/213 (51%) patients. NMFP allowed a definite diagnosis in 51/109 (47%) patients: 14 nonglaucomatous optic neuropathies, 10 papilledema, 13 acute retinal ischemia, 2 retinal detachments, 2 choroidal metastases, 4 maculopathies, and 6 glaucoma. In 58/109 (53%) patients, NMFP was not diagnostic even when interpreted remotely by ophthalmologists due to disorders undiagnosable with NMFP. Ophthalmology consultation was requested in 109/213 (51%) patients, 41/54 (76%) patients with abnormal NMFP versus 68/159 (43%) patients with normal NMPF (p < 0.001).
Discussion: Although NMFP allowed rapid diagnosis in 51/213 (24%) patients presenting to the ED with acute visual loss, NMFP alone was not sufficient to detect all ocular diseases; ophthalmology consultation was more often requested when NMFP was abnormal.
Conclusions: Our study emphasizes the limitations of teleophthalmology with NMFP in remotely detecting ocular diseases related to acute visual loss in the ED. NMFP helped triage and referral decisions and can be used to complement ophthalmology consultations in the ED.
Keywords: nonmydriatic fundus photography, acute vision loss, teleophthalmology, emergency department, ocular pathology detection, telehealth
Introduction
Acute visual loss is a common chief complaint in emergency department (ED) patients, and can be related to sight-threatening or even life-threatening conditions.1 However, evaluation of patients with visual loss is made difficult by the lack of ophthalmologists readily available in most EDs, leading to possible disparities in eye care.2 In one U.S.-based study,1 ED visits for ocular disorders increased by 30% between 2001 and 2014, with one-fourth of patients presenting with nonurgent ocular conditions, potentially generating delays in the care of patients visiting the ED for urgent reasons.
Teleophthalmology is an effective tool for remote detection of retinal diseases, especially retinopathy of prematurity and diabetic retinopathy.3–5 In a pilot study of patients presenting to an eye clinic for routine eye examination, excellent agreement was found between tele-eye and face-to-face screening examinations for cataract and age-related macular degeneration, allowing appropriate referral to the ophthalmologist 86.5% of the time.6 Subset analyses of the Fundus Photography versus Ophthalmoscopy Trial Outcomes in the Emergency Department (FOTO-ED) studies7–9 showed that nonmydriatic fundus photography (NMFP) can help triage patients with acute neurological conditions, and those presenting with severely elevated blood pressure or headaches in the ED.
In this study, we evaluated the subset of patients presenting with acute visual loss enrolled in the three phases of the FOTO-ED studies.7–9 Our goal was to assess the value of NMFP in the diagnosis and triage of patients presenting with visual loss in the ED.
Materials and Methods
Standard Protocol Approvals, Patient Informed Consents
The study was approved by our Institutional Review Board. A modified written informed consent was obtained from all study participants enrolled in the FOTO-ED I and II studies. Phase III was a quality improvement project reviewed as exempt from IRB review at the time of execution, and we obtained approval for a retrospective review of cases included during phase III for this study.
Study Conduct
We retrospectively reviewed the subset of 213 patients who presented to the ED with a chief complaint of acute visual loss in one or both eyes, and for whom NMFPs were taken during one of the three phases of the FOTO-ED studies.10–13 Detailed information about study design, protocol, and setting have been previously reported.11,12 In summary, the FOTO-ED study was a sequential trial designed to compare the clinical use of direct ophthalmoscopy performed by emergency providers (EPs) to the clinical use of NMFP interpreted by both EPs and ophthalmologists, for patients who presented to the ED with a chief complaint of headache, acute focal neurological deficit, diastolic blood pressure >120 mmHg, or acute visual changes. Fundus photographs of the posterior pole were taken without pharmacologic dilation by trained ED nurse practitioners, using the Kowa nonmyd-α-D 5 megapixel fundus camera (Kowa α-D, Torrence, CA).11–13
Fundus photographs obtained in the 213 patients with acute visual loss were specifically reviewed and interpreted by ophthalmologists to look for abnormal ocular findings involving the posterior pole. Quality of fundus photographs was rated with a previously validated five-point rating scale (1 = inadequate for any diagnostic purpose, 2 = unable to exclude all emergent findings, 3 = only able to exclude emergent findings, 4 = not ideal but still able to exclude subtle findings, 5 = ideal quality).11 Rating ≥3 was deemed adequate for clinical purposes in an urgent setting. Data regarding demographics (age, gender, race, and body mass index [BMI]), and referral patterns in the ED and after discharge, were collected for all patients. Final diagnoses reported in the patients' medical records following ophthalmologists' examinations in the ED and/or during follow-up visits were recorded.
Data Analysis
Statistical analysis was performed using R: A language and environment for statistical computing (R Foundation for Statistical Computing; www.R-project.org). Two-tailed p-values of 0.05 or less were considered statistically significant. Medians and interquartile ranges (IQRs) were reported for continuous data and percentages were reported for categorical data. Appropriate parametric and nonparametric tests were used to compare groups (medians: Mann–Whitney U test; proportions: chi-square or Fisher exact tests). Binary logistic regression was performed with the presence of an abnormal fundus photograph as the outcome and with age, gender, race, and BMI as multiple predictors of interest. Model selection was performed using the method of Kleinbaum and Klein.14
Results
Demographics
Of 213 patients enrolled, 135 (63%) were women; 93/213 (44%) were black, median age was 46 years (IQR: 33–61), and median BMI was 27 (IQR: 24–32). Based on a logistic regression model, black race increased the odds of an ocular fundus abnormality by 2.6 times (95% confidence interval [CI] 1.2–5.8, p = 0.02) and BMI increased it by 1.4 times per 5 kg/m2 (95% CI 1.1–1.8, p = 0.004).
Quality of Fundus Photographs
The vast majority of patients (195/213: 92%) had fundus photographs of adequate quality (rating quality scale ≥3); 15/213 (7%) patients had fundus photographs that were only able to demonstrate an optic nerve disorder (grade 2), and in 3/213 (1%) patients, fundus photographs were inadequate for any diagnostic purpose (grade 1). Among those three patients whose fundus photographs were rated grade 1, two were not seen by an ophthalmologist; the emergency providers reported a normal ophthalmic examination for each and diagnosed the first patient with headaches in the setting of a known arteriovenous malformation and the second with a periorbital contusion. The third patient was seen by an ophthalmologist in the ED and was diagnosed with a dense vitreous hemorrhage from proliferative diabetic retinopathy.
Ophthalmic Disorder Diagnoses
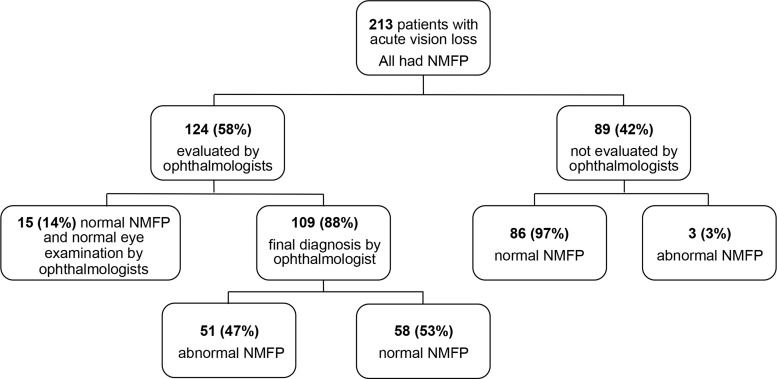
One hundred and twenty four (n = 124) patients (58%) were evaluated by an ophthalmologist during a face-to-face examination before, during, or after their ED visit (Fig. 1). Among these 124 patients, 109 (88%) had a final diagnosis made, and 15 (14%) had a normal ophthalmic examination. Among the remaining 89 patients who did not have an ophthalmic examination by an ophthalmologist, 86 had a normal fundus photograph and 3 had abnormal findings detected remotely by ophthalmologists (1 isolated retinal hemorrhage for whom the final ED diagnosis was “anxiety,” 1 subtle papilledema related to idiopathic intracranial hypertension, and 1 hypertensive retinopathy in whom a stroke was diagnosed). The allocation of results of NMFP and ophthalmic examinations is shown in Figure 1. The main diagnoses obtained in the ED for the 86 patients who were not examined by an ophthalmologist and had normal fundus photography are listed in Table 1. Most patients were diagnosed with migraine or chronic headaches (37/86, 43%), followed by ocular surface disorders (7/86, 8%), psychiatric diseases, and transient ischemic attack (6/86 for each, 7%).
Fig. 1.
Ophthalmic disorder diagnoses with NMFP. NMFP, nonmydriatic fundus photography.
Table 1.
Diseases Diagnosed by Emergency Providers in the Emergency Department for Patients with Normal Fundus Photographs Who Did Not Have an Ophthalmic Examination by an Ophthalmologist
| DISEASES DIAGNOSED BY EMERGENCY PROVIDERS | NO. OF PATIENTS |
|---|---|
| Migraine/headaches | 37 |
| Psychiatric | 6 each |
| Transient ischemic attack | |
| Hypertension | 5 each |
| Cornea | |
| Contusion | 3 each |
| No diagnosis | |
| Hyperglycemia | 2 each |
| Stye/conjunctivitis | |
| Vertigo | |
| Stroke | 1 each |
| Brain metastasis | |
| Carotid artery dissection | |
| Lymphoma | |
| Myasthenia gravis | |
| Peripheral vascular disease | |
| Preseptal cellulitis | |
| Presyncope | |
| Pulmonary | |
| Pyelonephritis | |
| Scabies | |
| Sinusitis | |
| Vasovagal | |
| Venous sinus thrombosis | |
| Ventriculoperitoneal shunt malfunction | |
| Total | 86 |
Among the 109/213 patients with a diagnosis provided by an ophthalmologist during a face-to-face encounter, NMFPs were abnormal in 51/109 (47%) patients. Ophthalmic disorders diagnosed on NMFP included 13 with acute retinal ischemia (arterial or venous retinal occlusions or related to diabetic or hypertensive retinopathy), 14 with nonglaucomatous optic neuropathy, 10 with papilledema, 8 with vitreoretinal disease, and 6 with glaucoma (Table 2). In the remaining 58/109 (53%) patients, NMFP was nondiagnostic, as those patients were diagnosed with disorders that did not involve the central retina or the optic nerve, including disorders of the anterior segment of the eye (18/58, 31%), orbit/ocular adnexa (2/58, 3.5%), peripheral retina/vitreous (11/58, 19%), and neurological disorders without ocular abnormalities (27/58, 46.5%) (Table 3).
Table 2.
Ophthalmic Disorders Diagnosed with Nonmydriatic Fundus Photography
| Acute retinal ischemia | |
| Central retinal artery occlusion | 5 |
| Central retinal vein occlusion | 2 |
| Diabetic retinopathy | 4 |
| Hypertensive retinopathy | 2 |
| Nonglaucomatous optic neuropathy | |
| Compressive | 7 |
| Inflammatory | 4 |
| Ischemic | 3 |
| Papilledema | |
| Idiopathic intracranial hypertension | 9 |
| Venous sinus thrombosis | 1 |
| Vitreoretinal disease | |
| Maculopathy | 4 |
| Retinal detachment | 2 |
| Choroidal metastasis | 2 |
| Glaucoma | 6 |
| Total | 51 |
Table 3.
Ophthalmic Disorders Not Diagnosed on Nonmydriatic Fundus Photography
| Anterior segment | |
| Cornea | 9 |
| Conjunctivitis/subconjunctival hemorrhage | 2 |
| Acute glaucoma | 1 |
| Hyphema | 1 |
| Other | 5 |
| Orbit/ocular adnexa | 2 |
| Posterior segment | |
| Dense vitreous hemorrhage | 1 |
| Posterior vitreous detachment | 8 |
| Peripheral retinal tear | 2 |
| Neurological disorders | |
| Transient visual loss | 10 |
| Migraine headaches | 5 |
| Pituitary adenoma/apoplexy | 5 |
| Optic neuritis | 3 |
| Oculomotor nerve palsy | 2 |
| Internal carotid artery aneurysm | 1 |
| Resolved idiopathic intracranial hypertension | 1 |
| Total | 58 |
Referral Patterns
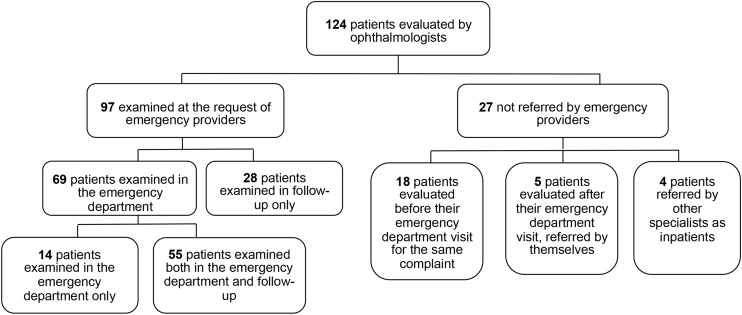
Among the 124 patients evaluated by an ophthalmologist, 97/124 (78%) were examined at the request of the EPs, 69/97 (71%) in the ED, and 28/97 (29%) after discharge (Fig. 2). Of the remaining 27 patients, 18 had been seen by an ophthalmologist before their ED visit for the same complaint and had been most often sent by that outside ophthalmologist to the ED; 5 referred themselves to an ophthalmologist after their ED visit, and 4 had an inpatient consultation with an ophthalmologist after being admitted to the hospital from the ED. Twelve additional patients for whom an ophthalmology consultation was requested by the EPs after the ED visit did not come to the follow-up visit or were sent back to their usual ophthalmologist, so no ophthalmic examination report was available in their medical records.
Fig. 2.
Referral patterns of 124 patients evaluated by an ophthalmologist.
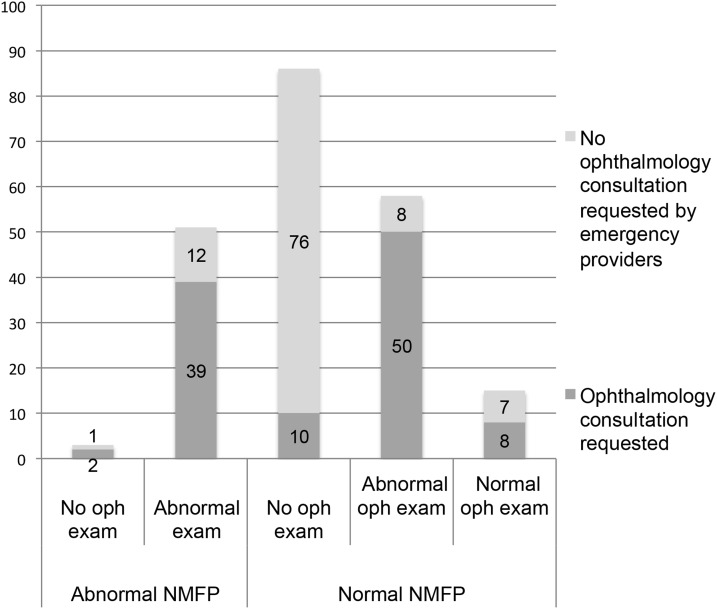
Ophthalmic referrals were requested by the EPs in 41/54 (76%) patients with abnormal NMFP versus in 68 of 159 (43%) patients with normal NMFP (p < 0.001). Among the 58 patients with a normal NMFP for whom a final diagnosis was made during ophthalmic examination by an ophthalmologist, 50 (86%) had an ophthalmology consultation requested by the EPs (Fig. 3).
Fig. 3.
Ophthalmic referrals among patients with abnormal NMFP compared with those with normal NMFP.
Discussion
Analysis of the ocular posterior pole with NMFP allowed a rapid remote ocular diagnosis confirmed by a face-to-face examination by an ophthalmologist in 24% of patients presenting to the ED with acute visual loss. Ocular disorders detected by NMFP were serious diseases that needed appropriate and urgent management, such as acute retinal ischemia, optic neuropathy or papilledema, or vitreoretinal diseases, such as retinal detachment. Remote interpretation of NMFP by ophthalmologists allowed a quick and accurate referral to the appropriate specialists. In a previous study, evaluation of fundus photographs taken with an ophthalmoscope adapter for a smartphone changed triage decisions in 20% of patients seen in the ED for urgent ocular diseases.15 In our study, NMFP substantially helped the EPs' triage and referral decisions, as the percentage referred to an ophthalmologist was 76% for abnormal NMFP and 43% for normal NMFP (p < 0.001). A recent survey in California EDs among physicians and nurses concluded that telemedicine may be more valuable for triage than for complete ocular diagnosis.16 Moreover, teleophthalmology in the ED may prevent unnecessary eye clinic appointments. Similar to another study,6 we found that almost half of the patients who presented to the ED with a chief complaint of acute visual loss had a normal NMFP and a normal ophthalmic examination by the EPs.
The quality of pictures obtained with our nonmydriatic table top camera was excellent, as 92% of patients had fundus photographs deemed of adequate quality for interpretation, and only 1% of patients had fundus photographs inadequate for any diagnostic purpose. Our results are better than those described in another study where they used a handheld camera, and found that 15–30% of pictures of the posterior segment were ungradable.17
We found that black race and an elevated BMI increased the risk of having abnormal fundus photographs. This is consistent with the higher risk of cardiovascular and metabolic diseases among individuals of black race and those with obesity, both demographic features predisposing to vascular changes in the retina.18 In addition, more severe papilledema from idiopathic intracranial hypertension has been demonstrated among African American patients.19
In about a quarter of patients, although NMFP was normal, a face-to-face examination by an ophthalmologist allowed for an ocular diagnosis. About a third of these patients had anterior segment disorders (such as corneal ulcers) or orbitopalpebral disorders, and two-thirds had posterior vitreous detachments, vitreous hemorrhage, peripheral retinal tears, or neurological disorders not visible on posterior pole NMFP. Indeed, the vitreous and peripheral retina are difficult to evaluate with fundus photography.20 Additionally, in our study, ophthalmologists interpreted the NMFP remotely only knowing the patients' chief complaints. The limitations of teleophthalmology in remotely detecting ocular diseases in the ED must be emphasized, particularly when only posterior pole fundus photographs are available (such as with most nonmydriatic imaging) and reliable information about patients' ocular histories and symptoms is limited.17
In conclusion, NMFP obtained in the ED by EPs and remotely interpreted by ophthalmologists were not sufficient to detect all ocular diseases associated with acute vision loss in our study. However, they did help the EPs' triage and referral decisions. Teleophthalmology, ideally including anterior segment imaging in addition to NMFP, combined with more extensive clinical information, may be a useful complement to ophthalmology consultations in the ED.
Acknowledgments
This study was supported in part by Research to Prevent Blindness (Department of Ophthalmology), the Philippe Foundation (S.B. and C.V.), and NIH grants P30-EY006360 (Department of Ophthalmology), K23-EY019341 (B.B.B.), and UL1-RR025008 (V.B.).
Disclosure Statement
No competing financial interests exist.
References
- 1. Stagg BC, Shah MM, Talwar N, Padovani-Claudio DA, Woodward MA, Stein JD. Factors affecting visits to the emergency department for urgent and nonurgent ocular conditions. Ophthalmology 2017;124:720–729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wang SY, Hamid MS, Musch DC, Woodward MA. Utilization of ophthalmologist consultation for emergency care at a University hospital. JAMA Ophthalmol 2018;136:428–431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Woodward MA, Ple-Plakon P, Blachley T, Musch DC, Newman-Casey PA, De Lott LB, Lee PP. Eye care providers' attitudes towards tele-ophthalmology. Telemed J E Health 2015;21:271–273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fierson WM, Capone A, Jr; American Academy of Pediatrics Section on Ophthalmology; American Academy of Ophthalmology, American Association of Certified Orthoptists. Telemedicine for evaluation of retinopathy of prematurity. Pediatrics 2015;135:e238–e254 [DOI] [PubMed] [Google Scholar]
- 5. Shi L, Wu H, Dong J, Jiang K, Lu X, Shi J. Telemedicine for detecting diabetic retinopathy: A systematic review and meta-analysis. Br J Ophthalmol 2015;99:823–831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Maa AY, Evans C, DeLaune WR, Patel PS, Lynch MG. A novel tele-eye protocol for ocular disease detection and access to eye care services. Telemed J E Health 2014;20:318–323 [DOI] [PubMed] [Google Scholar]
- 7. Vuong LN, Thulasi P, Biousse V, Garza P, Wright DW, Newman NJ, Bruce BB. Ocular fundus photography of patients with focal neurologic deficits in an emergency department. Neurology 2015;85:256–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Henderson AD, Biousse V, Newman NJ, Lamirel C, Wright DW, Bruce BB. Grade III or Grade IV hypertensive retinopathy with severely elevated blood pressure. West J Emerg Med 2012;13:529–534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Thulasi P, Fraser CL, Biousse V, Wright DW, Newman NJ, Bruce BB. Nonmydriatic ocular fundus photography among headache patients in an emergency department. Neurology 2013;80:432–437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bruce BB, Lamirel C, Wright DW, Ward A, Heilpern KL, et al. Nonmydriatic ocular fundus photography in the emergency department. N Engl J Med 2011;364:387–389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bruce BB, Lamirel C, Biousse V, Ward A, Heilpern KL, et al. Feasibility of nonmydriatic ocular fundus photography in the emergency department: Phase I of the FOTO-ED study. Acad Emerg Med 2011;18:928–933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bruce BB, Thulasi P, Fraser CL, Keadey MT, Ward A, et al. Diagnostic accuracy and use of nonmydriatic ocular fundus photography by emergency physicians: Phase II of the FOTO-ED study. Ann Emerg Med 2013;62:28–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bruce BB, Bidot S, Hage R, Clough LC, Fajoles-Vasseneix C, Melomed M, Keadey MT, Wright DW, Newman NJ, Biousse V. Fundus photography vs. ophthalmoscopy outcomes in the Emergency Department (FOTO-ED) phase III: Web-based, in-service training of emergency providers. Neuroophthalmology 2018;42:269–274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kleinbaum DG, Klein M. Logistic regression: A self-learning text, 2nd ed. New York, NJ: Springer-Verlag, 2002 [Google Scholar]
- 15. Legarreta JE, Conner IP, Loewen NA, Miller KV, Wingard J. The utility of iPhone-based imaging for tele-ophthalmology in a triage capacity for emergency room consultations. IOVS 2014;55:4876 [Google Scholar]
- 16. Wedekind L, Sainani K, Pershing S. Supply and perceived demand for teleophthalmology in triage and consultations in California Emergency Departments. JAMA Ophthalmol 2016;134:537–543 [DOI] [PubMed] [Google Scholar]
- 17. Woodward MA, Bavinger JC, Amin S, Blachley TS, Musch DC, Lee PP, Newman-Casey PA. Telemedicine for ophthalmic consultation services: Use of a portable device and layering information for graders. J Telemed Telecare 2017;23:365–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Carnethon MR, Pu J, Howard G, Albert MA, Anderson CAM, Bertoni AG, Mujahid MS, Palaniappan L, Taylor HA, Jr, Willis M, Yancy CW; American Heart Association Council on Epidemiology and Prevention; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Functional Genomics and Translational Biology; and Stroke Council. Cardiovascular Health in African Americans: A Scientific Statement from the American Heart Association. Circulation 2017;136:e393–e423 [DOI] [PubMed] [Google Scholar]
- 19. Bruce BB, Preechawat P, Newman NJ, et al. Racial differences in idiopathic intracranial hypertension. Neurology 2008;70:861–867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bar-Sela SM, Glovinsky Y. A feasibility study of an Internet-based telemedicine system for consultation in an ophthalmic emergency room. J Telemed Telecare 2007;13:119–124 [DOI] [PubMed] [Google Scholar]