Abstract
Background: Although the American Heart Association promotes telehealth models to improve care access, there is limited literature on its use in underserved populations. This study is the first to compare utilization and quality of life (QoL) for underserved black and Hispanic heart failure (HF) patients assigned to telehealth self-monitoring (TSM) or comprehensive outpatient management (COM) over 90 days.
Methods: This randomized controlled trial enrolled 104 patients. Outcomes included emergency department (ED) visits, hospitalizations, QoL, depression, and anxiety. Binary outcomes for utilization were analyzed using chi-square or Fisher's exact test. Poisson or negative binomial regression, repeated-measures analysis of variance, or generalized estimating equations were also used as appropriate.
Results: Of 104 patients, 31% were Hispanic, 69% black, 41% women, and 72% reported incomes of <$10,000/year. Groups did not differ regarding binary ED visits (relative risk [RR] = 1.37, confidence interval [CI] = 0.83–2.27), hospitalization (RR = 0.92, CI = 0.57–1.48), or length of stay in days (TSM = 0.54 vs. COM = 0.91). Number of all-cause hospitalizations was significantly lower for COM (TSM = 0.78 vs. COM = 0.55; p = 0.03). COM patients reported greater anxiety reduction from baseline to 90 days (TSM = 50–28%; COM = 57–13%; p = 0.05).
Conclusions: These findings suggest that TSM is not effective in reducing utilization or improving QoL for underserved patients with HF. Future studies are needed to determine whether TSM can be effective for populations facing health care access issues.
Keywords: cardiology/cardiovascular disease, home health monitoring, telehealth, telemedicine
Introduction
According to the American Heart Association (AHA), one in nine deaths in the United States is attributable to heart failure (HF).1 Blacks and Hispanics experience a disproportionately high prevalence of HF compared with whites and are diagnosed earlier.2–4 Likewise, Hispanics with HF are diagnosed younger and die earlier than non-Hispanic whites.5 Reasons for this greater disease burden are complex, resulting from the interaction of factors such as hypertension, diabetes, obesity, reduced health care access, and socioeconomic and cultural factors.2,6–9
HF is characterized by recurrent periods of clinical exacerbation resulting in high rates of emergency department (ED) and inpatient hospital utilization, leading to poor health outcomes, decreased quality of life (QoL), and exorbitant health care costs, largely attributable to a 30-day all-cause readmission rate of ∼25%.10 The use of telehealth is a promising approach to optimizing outcomes in the treatment of HF.11 Despite AHA recommendations, telehealth is underused for disparity populations.12,13
Recent systematic reviews found that remote monitoring of HF patients significantly reduced the odds of HF-related death and hospitalization and improved QoL, HF knowledge, and self-care behaviors compared with usual care.14–20 Conversely, large randomized clinical trials have not found rehospitalization or mortality benefits of home telemonitoring.21,22
Although many randomized controlled trials (RCTs) of telehealth monitoring have been published, there is limited literature on the use of telehealth in underserved populations.23,24 Given the great prevalence of HF in underserved populations and disparities in access to innovative and effective treatment, it is imperative that researchers and clinicians bring effective interventions to these at-risk populations. The purpose of this study was to compare health care utilization and QoL for underserved black and Hispanic HF patients assigned to telehealth self-monitoring (TSM) or comprehensive outpatient management (COM) over 90 days.
Methods
Study Design
This RCT enrolled 104 black and Hispanic patients from underserved communities with a primary diagnosis of HF, a New York Heart Association (NYHA) Classes 1–3 and a Folstein Mini-Mental Status Examination (MMSE) score of at least 21. Patients were randomized to either TSM or COM as detailed hereunder. Both cohorts received a phone call within 72 h of discharge from a bilingual research nurse coordinator (RNC), and a clinic appointment within 7 days of discharge, as per AHA HF clinic guidelines.25–27 A cardiologist on call was available to both groups to address urgent problems when patients contacted the clinic after hours.
The TSM intervention was tailored to the needs of the targeted community using a community-based participatory research (CBPR) approach, the ADAPT-ITT (Assessment Decision Administration Production Topical Experts—Integration Training Testing) model to facilitate usability and feasibility.28,29 Spanish and/or English-speaking patients 18 years and older and recently discharged from the hospital were followed for 90 days. Patients were excluded if they were already receiving telehealth monitoring. Patients were offered enrollment within 1 week of discharge from a large “safety net” hospital in the New York Metropolitan Area from March 31, 2014 to June 30, 2016.
All patients were assessed for the following outcomes at days 1 and 90: (1) inpatient (primary) and ED utilization, based on patient self-report and validated through medical record review; (2) QOL, through the Minnesota Living with Heart Failure Questionnaire (MLHFQ)30; (3) anxiety and depression through the Patient Health Questionnaire-4 (PHQ-4).31,32
TSM comprised two main components: (1) daily vital signs self-monitoring and (2) weekly telehealth visits between the patient and the RNC. All TSM patients also received outpatient management. A Food and Drug Administration-approved computerized monitoring device (American TeleCare LifeView®) connected the patient's residence through a wireless air card, broadband, or a standard telephone line, to the provider station. As per protocol, TSM patients received telemonitoring equipment within 7 days of hospital discharge and/or enrollment.
A bilingual equipment installer visited the patients' residence to install the equipment, provide training, and establish an initial video connection with the telehealth nurse at her office-based telehealth provider station. The installer would stay at home for as long as was needed, and would return if technological problems arose, or if the patient needed further training. Several patients required more than one visit. Patients also received a chart indicating where to hold the stethoscope on specific areas on their chest if alone, or on their back if a caregiver was present.
Daily Vital Signs Monitoring
Patients were trained to use equipment peripherals to measure vital signs. During daily transmissions, patients were prompted by the patient station screens, in the patient's language of choice, to use the peripheral devices to transmit vital signs that were stored on the server database. Vital signs collected included the following: blood pressure, oxygen saturation rate, weight, and pulse/heart rate. The RNC reviewed vital signs within 24 h of transmission on weekdays and within 72 h on weekends. If vital signs were outside the normal range (“normal range” was specifically determined for each patient by their cardiologist), the RNC would either contact the patient's health care practitioner to discuss/revise the treatment plan, including medication adjustment (i.e., diuretic) or, for urgent matters, instruct the patient to call 911.
Weekly Video Visit
Once a week, TSM patients were instructed to attend a scheduled televisit with the RNC, during which time the patient and RNC discussed vital signs values and symptoms of HF and behaviors that may have contributed to symptoms. If necessary, the RNC used the stethoscope to listen to the patient's heart and lung sounds.
COM, delivered in the outpatient setting, was based upon AHA 2013 Guidelines for Management of HF.29 Adherence to standards included monitoring medications, blood pressure, weight, diet, lipid profiles, and patient education. Patients typically have routine or “well” visits every 3 months. In addition, COM patients received one clinic visit within a week of discharge and weekly “check-in” phone calls with the RNC during the first month of enrollment, addressing AHA guideline standards. Patients with symptoms indicative of worsening HF or with major weight alterations were either scheduled for an HF clinic visit or were managed by phone based on clinician assessment. Patients who did not have a scale at home were provided with a weight scale. After the first month of enrollment, COM patients were followed by their cardiologist or HF clinic at the discretion of the clinician and queried for the remainder of the study period about ED and hospital utilization to maintain a comparable frequency of contact.
Patients were randomized to either TSM or COM using permuted block randomization, with stratification by heart class, to ensure equal representation of heart class across the two groups. Concealed allocation was achieved by maintaining randomization allocation in the biostatistics office.
Analytical and Statistical Approaches
The primary analysis of this randomized clinical trial was based on the intention-to-treat (ITT) principle that included all subjects randomized. Primary outcomes included ED visits, inpatient utilization, and length of stay (LOS). ED utilization was defined as whether an individual patient had at least one ED visit over the 90-day period. Binary outcomes for ED visits and hospitalizations were analyzed using the standard chi-square or Fisher's exact test. Associated 95% confidence intervals (CIs) for these proportions and their differences were computed using exact methods. Cumulative LOS (inpatient days) was analyzed using negative binomial regression.
QoL (MLHFQ)30 and anxiety and depression (PHQ-4)31 were analyzed using repeated-measures analysis of variance (mixed-models approach) to compare changes at enrollment and at 90 days between groups. The subscales of anxiety and depression, as measured by the PHQ-431 were dichotomized (presence or absence); generalized estimating equations were used to analyze these binary data.
Finally, post hoc analyses were conducted, including a comparison of racial/ethnic subgroups, a comparison of NYHA class (2 vs. 3) and TSM patient adherence to daily uploads and weekly televisits. Adherence was calculated only for the TSM group. Patients in the TSM group were asked to upload vital signs daily (90 uploads/90 days). The minimally acceptable level of adherence was arbitrarily defined as <10 uploads over the 90-day period (low adherence), whereas high adherence was defined as 10 or more uploads over 90 days, corresponding to the frequency of real-time virtual nursing visits. For this study, adherence is defined as patient transmission of any vital sign to the provider.
A result was considered statistically significant at the p < 0.05 level of significance. All analyses were performed using SAS 9.4 (SAS Institute, Inc., Cary, NC). The Institutional Review Board (No. 13-518A) approved the study protocol. Clinical trial registration: ClinicalTrials.gov identifier: NCT02196922.
Results
Participant Characteristics
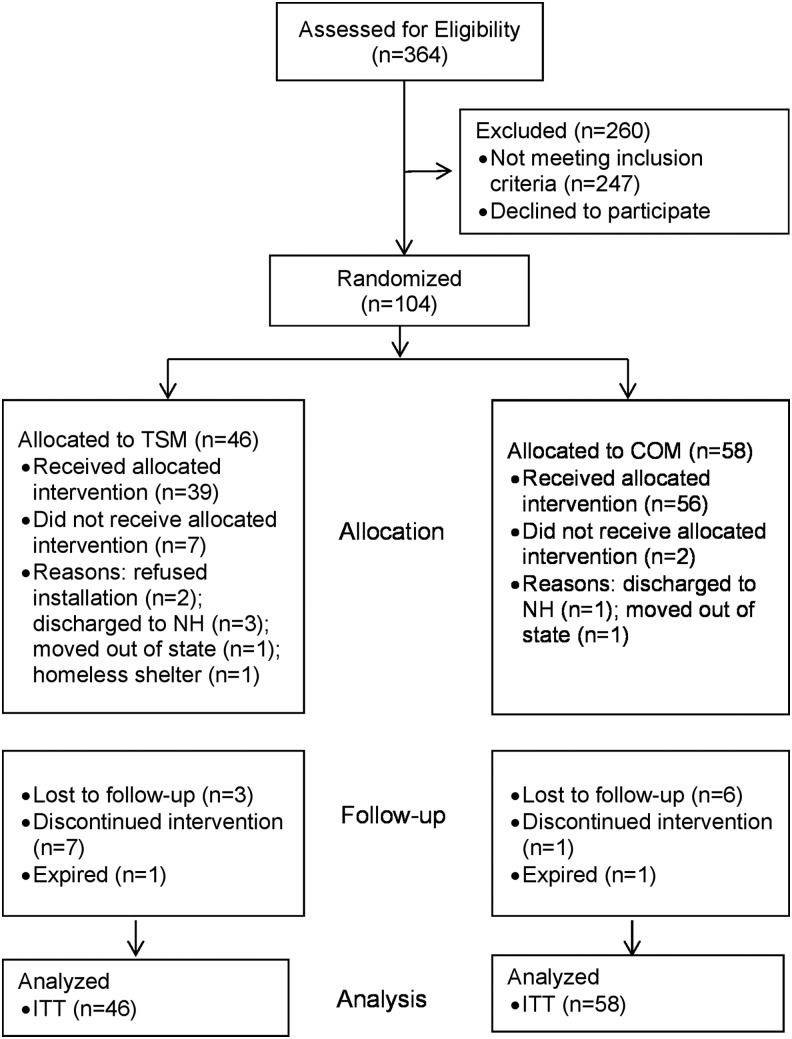
Of the 364 patients screened for eligibility, 247 did not meet inclusion criteria, 13 declined participation, and 104 were randomized; 46 were allocated to TSM and 58 to COM (Fig. 1). None of the patients screened declined participation owing to technology, but two did not permit installation after randomization to TSM. Eighty-one percent of all subjects had complete outcome data for the 90-day study period. Some subjects dropped out before 90 days for the following reasons: transferred to hospice or skilled nursing facility, expired, moved away, or requested termination of their study participation.
Fig. 1.
Consort diagram (patient flow). COM, comprehensive outpatient management; ITT, intention-to-treat analysis; NH, nursing home; TSM, telehealth self-monitoring.
Of the 104 patients randomized, 31% self-identified as Hispanic and 69% black, and 41% were women (Table 1). The majority (72%) reported an income of <$10,000 a year. In terms of insurance, 23% were uninsured and 33% were receiving Medicaid at enrollment. In terms of education, 31% did not complete high school. In terms of clinical characteristics, 70% of patients were classified as NYHA Class 3 and 30% were NYHA Class 2; 61% had reduced ejection fraction (EF), 10% had borderline EF, and 29% had preserved EF. Average age was 59.9 years (range: 19–93 years).
Table 1.
Baseline Characteristics
| VARIABLES | TOTAL | COM GROUP | TSM GROUP |
|---|---|---|---|
| Participants (n) | 104 | 58 | 46 |
| Age: mean (SD, range) | 59.9 (15.1, 19–93) | 61.1 (15.0, 26–90) | 58.4 (15.2, 19–93) |
| Gender: female, n (%) | 43 (41) | 23 (40) | 20 (43) |
| Hispanic, n (%) | 32 (31) | 17 (29) | 15 (33) |
| Black, n (%) | 72 (69) | 41 (71) | 31 (67) |
| Female, n (%) | 43 (41) | 23 (40) | 20 (44) |
| Reduced EF (≤40%), n (%) | 62 (61) | 36 (63) | 26 (58) |
| Borderline EF (41–49%), n (%) | 10 (10) | 6 (11) | 4 (9) |
| Preserved EF (≥50%), n (%) | 30 (29) | 15 (26) | 15 (33) |
| Index hospitalization LOS (days), n (SD) | 5.97 (4.6) | 5.88 (4.3) | 6.09 (5.3) |
| NYHA Class 3, n (%) | 73 (70) | 40 (69) | 33 (72) |
| NYHA Class 2, n (%) | 31 (30) | 18 (31) | 13 (28) |
| Uninsured, n (%) | 23 (23) | 11 (20) | 12 (27) |
| Medicaid, n (%) | 33 (33) | 21 (38) | 12 (27) |
| Medicare, n (%) | 21 (21) | 8 (15) | 13 (29) |
| Dual eligible, n (%) | 6 (6) | 5 (10) | 1 (2) |
| Private insurance, n (%) | 9 (9) | 4 (7) | 5 (11) |
| Other insurance, n (%) | 8 (8) | 6 (11) | 2 (4) |
| Income: <$10,000/year, n (%) | 74 (72) | 39 (68) | 35 (76) |
| Education: graduated from high school, n (%) | 53 (54) | 28 (53) | 25 (55) |
No significant between group differences were found.
COM, comprehensive outpatient management; LOS, length of stay; NYHA, New York Heart Association; TSM, telehealth self-monitoring; SD, standard deviation.
Clinical Outcomes: ITT Analysis
ED visits
For ED utilization by group (Table 2), 32.6% of TSM patients were seen at least once in the ED over the 90-day period compared with 44.8% of COM patients; this difference was not statistically significant (relative risk [RR] = 1.37, 95% CI = 0.83–2.27, p = 0.21). A 30-day ED utilization was 4/46 (8.7%) for TSM and 14/58 (24.1%) for COM (p = 0.07). No significant differences between groups were observed for the number of patients with at least one HF-related or cardiovascular disease (CVD)-related ED utilization visit over 90 days.
Table 2.
Emergency Department and Hospital Utilization: Intention-to-Treat Analysis
| ED VISITS/90 DAYS | HOSPITALIZATIONS/90 DAYS | |||
|---|---|---|---|---|
| GROUP | TSM | COM | TSM | COM |
| Participants (n) | 46 | 58 | 46 | 58 |
| All-cause visits—binary (≥1 visit), n (%) | 15 (32.6) | 26 (44.8) | 19 (41.3) | 22 (37.9) |
| RR, 95% CI | 1.37, 0.83–2.27 | 0.92, 0.57–1.48 | ||
| p–Value | 0.21 | 0.73 | ||
| All-cause visits, mean (SD) | 0.63 (1.18) | 0.69 (0.99) | 0.78 (1.3) | 0.55 (0.9) |
| p–Value | 0.73 | 0.03 | ||
| All-cause LOS, mean (SD) | N/A | N/A | 5.2 (8.1) | 3.6 (6.9) |
| p–Value | N/A | 0.12 | ||
| HF-related visits—binary (≥1 visit) | 10.8% | 12.1% | 10.9% | 13.8% |
| RR, 95% CI | 1.11, 0.38–3.27 | 1.27, 0.44–3.6 | ||
| p–Value | 0.85 | 0.65 | ||
| HF-related visits, mean (SD) | 0.13 (0.4) | 0.14 (0.4) | 0.15 (0.47) | 0.16 (0.41) |
| p–Value | 0.83 | 0.76 | ||
| HF-related hospital LOS, mean (SD) | N/A | N/A | 0.54 (1.7) | 0.91 (3.0) |
| p–Value | N/A | 0.60 | ||
| CVD-related visits—binary (≥1 visit) | 13.0% | 15.5% | 13.0% | 17.2% |
| RR, 95% CI | 1.19, 0.46–3.1 | 1.32, 0.52–3.4 | ||
| p–Value | 0.72 | 0.56 | ||
| CVD-related visits, mean (SD) | 0.17 (0.49) | 0.17 (0.42) | 0.20 (0.54) | 0.19 (0.44) |
| p–Value | 0.70 | 0.65 | ||
| CVD-related LOS, mean (SD) | N/A | N/A | 1.0 (3.7) | 1.6 (5.2) |
| p-Value | N/A | 0.67 | ||
Bold values indicate significance at the <0.05 level.
CVD, cardiovascular disease; CI, confidence interval; ED, emergency department; HF, heart failure; N/A, not applicable; RR, relative risk.
Inpatient utilization
For inpatient utilization by group (Table 2), 41.3% of patients in the TSM group were hospitalized at least once during the 90-day study period compared with 37.9% of COM patients; this difference was not statistically significant (RR = 0.92, 95% CI: 0.57–1.48, p = 0.73). A 30-day hospitalization was 7/46 (15.2%) for TSM and 9/58 (15.5%) for COM (p = 0.97). No significant differences between groups were observed for the number of patients with at least one HF-related or CVD-related hospitalization over 90 days.
Length of stay
For all-cause LOS data by group (Table 2), the mean total LOS for TSM patients was 5.2 days (standard deviation [SD] = 8.1) versus 3.6 days (SD = 6.9) for COM patients (p = 0.12). For HF- and CVD-related LOS, the LOS was shorter for the TSM group, although differences between groups were not statistically significant.
Quality of life
Overall, QoL (lower scores indicate improved QoL) did not differ between groups over time (Table 3). MLHFQ QoL was 62.7 for TSM at enrollment versus 59.9 for COM and 36.3 for TSM versus 27.8 for COM at 90 days (p = 0.50). Physical and emotional subscale results were also similar for both groups (p = 0.30 and p = 0.82).
Table 3.
Quality of Life, Anxiety and Depression
| ITT ANALYSIS | ||
|---|---|---|
| GROUP | TSM | COM |
| QoL (MLHFQ) range: 0–105, 21 items | Baseline: 62.7 90 days: 36.3 |
Baseline: 59.9 90 days: 27.8 |
| p-Value | 0.50 | |
| Physical subscale (MLHFQ) range: 0–40, 8 items | Baseline: 29.8 90 days: 18.1 |
Baseline: 28.9 90 days: 13.3 |
| p-Value | 0.30 | |
| Emotional subscale (MLHFQ) range: 0–25, 5 items | Baseline: 9.5 90 days: 6.2 |
Baseline: 8.6 90 days: 4.9 |
| p-Value | 0.82 | |
| PHQ-4 (total) range: 0–12 | Baseline: 4.96 90 days: 2.79 |
Baseline: 4.98 90 days: 1.98 |
| p-Value | 0.43 | |
| PHQ-4 (anxiety subscale): % of positive screens | Baseline: 50% 90 days: 28% |
Baseline: 57% 90 days: 13% |
| p-Value | 0.05 | |
| PHQ-4 (depression subscale): % of positive screens | Baseline: 43% 90 days: 21% |
Baseline: 43% 90 days: 17% |
| p-Value | 0.74 | |
Bold values indicate significance at the < 0.05 level.
ITT, intention-to-treat; MLHFQ, Minnesota Living with Heart Failure Questionnaire; PHQ-4, Patient Health Questionnaire-4; QoL, quality of life.
Screening scale for anxiety and depression (PHQ-4)
Scores for overall psychological distress (lower scores represent decreased anxiety and depression) did not significantly differ over time (5.0 for TSM vs. 5.0 for COM at enrollment, and 2.8 for TSM vs. 2.0 for COM at 90 days, p = 0.43) (Table 3). Differences over time for the PHQ-4 anxiety subscale between enrollment and 90 days were statistically significant, indicating that while anxiety symptoms improved for both groups, the improvement was greater for COM patients than TSM patients (50% of TSM vs. 57% of COM screened positive at enrollment, and 28% TSM vs. 13% COM screened positive at 90 days, p = 0.05). No significant differences were found over time between the proportions of patients who screened on the PHQ-4 depression subscale between enrollment and 90 days.
Post hoc Analyses
Post hoc analysis 1: ED and hospitalization by HF class
ED visits
As given in Table 4, 7.7% of Class 2 patients in the TSM group had at least one ED visit compared with 44.4% of COM patients, whereas 42.4% of TSM Class 3 patients had at least one ED visit versus 45.0% for the COM group (p = 0.08). No significant differences between groups by heart class were found for HF-related ED visits, or CVD-related ED visits.
Table 4.
Utilization by New York Heart Association Class, Race/Ethnicity and Adherence
| NYHA CLASS 2 TSM N = 13 | NYHA CLASS 2 COM N = 18 | NYHA CLASS 3 TSM N = 33 | NYHA CLASS 3 COM N = 40 | BLACK TSM SUBJECTS N = 31 | BLACK COM SUBJECTS N = 41 | HISPANIC TSM SUBJECTS N = 15 | HISPANIC COM SUBJECTS N = 17 | LOW ADHERENCE TSM SUBJECTS N = 23 | HIGH ADHERENCE TSM SUBJECTS N = 23 | |
|---|---|---|---|---|---|---|---|---|---|---|
| ED visits (binary ≥1 visit) | 7.7% | 44.4% | 42.4% | 45.0% | 32.3% | 48.8% | 33.3% | 35.3% | 34.8% | 30.4% |
| p-Value | 0.08* | 0.16 | 0.91 | a0.75 | ||||||
| Hospitalization (binary ≥1 visit) | 15.4% | 27.8% | 51.5% | 42.5% | 38.7% | 43.9% | 46.7% | 23.5% | 52.2% | 30.4% |
| p-Value | 0.29* | 0.66 | 0.17 | 0.13 | ||||||
| LOS (days) | 1.00 (2.83) | 1.06 (2.31) | 6.82 (8.88) | 4.68 (7.90) | 5.23 (8.48) | 4.0 (7.25) | 5.07 (7.45) | 2.47 (5.91) | 7.74 (9.74) | 2.61 (4.97) |
| p-Value | 0.03** | 0.93** | 0.17** | 0.01 | ||||||
Bold values indicate significance at the < 0.05 level.
Group × NYHA class interaction.
Kruskal–Wallis test.
Inpatient utilization
As given in Table 4, 15.4% of TSM Class 2 patients were admitted at least once compared with 27.8% of COM patients, whereas 51.5% of TSM Class 3 patients had at least one hospitalization versus 42.5% for the COM group. Differences between groups were not statistically significant (p = 0.29). Similarly, no significant differences were observed between groups for HF-related hospitalizations or CVD-related hospitalizations.
Post hoc analysis 2: utilization by subpopulations (black/Hispanic)
Given the low number of events (and relatively small subgroup sample size) when analyzing outcomes by race/ethnicity, we only present all-cause utilization outcomes (Table 4). For the black cohort, 32.3% of TSM patients had at least one ED visit over 90 days versus 48.8% of COM patients (p = 0.16). Similarly, 38.7% of black TSM patients were hospitalized at least once versus 43.9% of black COM patients (p = 0.66). For the Hispanic cohort, 33.3% of TSM patients had at least one ED visit over 90 days versus 35.3% of COM patients (p = 0.91). Whereas 46.7% of Hispanic TSM patients were hospitalized at least once, fewer (23.5%) Hispanic COM patients were hospitalized (p = 0.17), although not significantly.
Post hoc analysis 3: adherence and utilization (TSM group only)
Table 4 presents utilization data by adherence level for patients in the TSM group only. For this study, adherence was defined as patient transmission of any vital sign to the provider. Usually, uploads included at least three vital signs. Although patients were asked to upload daily vital signs and attend a weekly televisit with the RNC, 23 (50%) TSM patients had provided <10 uploads over the 90-day period. No significant differences were found between patients in the high adherence group versus the low adherence group for one or more ED visits (30.4% vs. 34.8%, p = 0.75) or for one or more hospitalizations (30.4% and 52.2%, p = 0.13). Patients with higher adherence had a significantly lower mean all-cause LOS (2.6 days, SD = 5.0) versus low adherence patients (7.7 days, SD = 9.7, p = 0.01).
Discussion
This RCT was the first, to our knowledge, to use a telehealth self-management intervention to monitor daily vital signs and symptoms exclusively in Hispanic and black patients recently discharged from the hospital for HF-related symptoms. For both main binary outcomes (all-cause ED and hospital utilization) and cumulative LOS, TSM did not result in a significant improvement over COM. Furthermore, the average number of all-cause hospitalizations was significantly lower for the COM group over 90 days. In addition, COM patients reported a significantly greater reduction of anxiety symptoms at 90 days than the TSM group. It is important to note that TSM adherence was extremely low: 50% provided <10 uploads over the 90-day period.
As for QoL, patients in both arms reported improved QoL over the 90-day study period based on the MLHFQ. Similar to findings from Konstam et al.,33 we did not find an effect of TSM on HF-related QoL.
COM patients reported a significantly greater reduction of anxiety symptoms at 90 days than the TSM group. This is consistent with findings of Huygens et al.34 that demonstrated increased anxiety for cardiovascular patients monitoring vital signs. With regard to this study, reasons for this greater reduction of anxiety in the COM group cannot be determined from our data. This higher anxiety for patients in the TSM group may arise from taking the measurements themselves, discomfort with out of range data, and/or unease with frequent reminders of their chronic condition. More research is warranted to explore the reasons for this variation in anxiety over time.
Despite the CBPR process utilized to adapt the TSM intervention for use with our target population,35 TSM did not result in significantly improved outcomes. This may be the result of low adherence: only half TSM patients actively participated in the intervention (transmitted their vital signs 10 times or more over 90 days). Reasons for low adherence may be lack of familiarity with technology in general, reported inconsistent connectivity in some areas, and the younger age of our study cohort (at an average age of 60 years, many were employed and may not have had the opportunity to attend weekly video visits during the 9–5 workdays of the RNC). These findings are similar to the tele-HF and to the Better Effectiveness After Transition—Heart Failure studies, wherein telemonitoring did not reduce readmissions and approximately half of the patients were not adherent.21,22 However, even in the Telemedical Interventional Monitoring in Heart Failure study, which reported high adherence (>70% of daily transmissions), telemonitoring did not reduce readmission.36
It is quite conceivable that low adherence to the TSM intervention may have affected our results. Future research is needed to identify methods (e.g., incentives) to improve adherence for this population. Perhaps simpler, smaller, and transportable technology would be more conducive to the needs of this population. Dang et al.37,38 recently implemented a mobile phone-assisted case management program to monitor daily weights and HF-related symptoms in an underserved county hospital population. Although the study demonstrated that the mobile intervention improved self-efficacy and QoL, hospital utilization was not assessed. Future studies are clearly needed to clarify the relationship between telemonitoring adherence and hospital utilization.
When evaluating all-cause hospitalization, it is clear that patients in this study utilized the hospital for many reasons other than HF-related symptoms (i.e., toothache, bronchitis, back pain, cold, and flu symptoms). This hospital utilization (ER and inpatient) for nonacute symptom management is likely to be much more prevalent in underserved populations.39 To this end, some of our post hoc analyses suggest that there may be an effect of telemonitoring on HF-related utilization in our population, despite nonsignificance (HF-related LOS for TSM was about half that of COM). Future studies should be powered to detect group differences in HF-related utilization.
It is worth noting that the observed rate of hospitalization was half of what we had projected based on a previous study by this team in which the average age at enrollment was 81 years.40 This lower observed hospitalization rate may be a function of the much younger age group enrolled in this study (mean age = 60); most telehealth studies have enrolled patients with mean ages older than 70 years.41 It is also notable that our 30-day readmission rate was 15.5% compared with the 25% national rate for Medicare patients (mean age = 81.8), also likely a function of the younger patient cohort enrolled in this study.42
As for QoL, we observed that patients in both arms reported improvements over the 90-day observation period. Anxiety and depression symptoms also decreased over time. Interestingly, the TSM group reported a smaller reduction in anxiety symptoms compared with the COM group. Our results are consistent with previous findings34 that suggested increased anxiety for cardiovascular patients involved in vital signs monitoring. This greater degree of anxiety over time in the TSM group may be attributable to (1) constant reminders of their chronic condition over the 90-day study period; and (2) removal of the telemonitoring intervention (patients' fear of being “on their own”).34 This is supported by previous research suggesting that patients feel “secure” about their health with a monitoring system in place.37 However, the reasons for this smaller decrease in anxiety symptoms cannot be determined from our data. Furthermore, it may well be that some level of anxiety is not necessarily negative, as attendance to vital signs and symptoms does require careful vigilance.
This study had several limitations. First, because this is a single-center study at a “safety net” hospital with an HF clinic, the results may not be generalizable to other underserved populations living in different settings. It should be noted that our COM patients received a relatively high level of care, including weekly phone contact for 30 days after discharge. Second, advances in technology clearly outpace the ability of research studies to evaluate telehealth efficacy. At the start of our study, most platforms—including the one used in this study—required equipment installation in the patient's home. At present, many telehealth providers are offering portable and wireless products that can be used outside the home—in the workplace, for example. This smaller, smarter technology may offer a more viable option—especially in this underserved population, who are more likely to experience shared living arrangements with limited space to house the TSM technology (e.g., living with relatives and shelters), and/or are actively working. Although this technology is bound to become less expensive and simpler to use for both patients and providers, effective integration of TSM into real-world practice will likely require large-scale pragmatic studies. Finally, the number of statistical tests performed for this study was quite large, increasing the probability of finding significance.
In conclusion, our findings suggest that TSM over a 90-day period is not effective in reducing all-cause ED and hospital utilization or improving QoL for patients with HF from underserved black and Hispanic populations. Future studies are needed to determine whether TSM is effective in reducing HF-related utilization and examine the role of adherence in relation to improved outcomes in HF, especially for populations facing health care access issues.
Acknowledgments
The authors thank the PCORI HF Community Advisory Board for their enormous contributions to this study, and the patients who participated in the focus groups and RCT. The authors also acknowledge the assistance of Jill Cotroneo, Stephanie Morahan, and Myia Williams, for administrative, nursing, and research compliance support, respectively. Finally, they thank Tito Orona, Patient Orientation Specialist, who was responsible for delivering, installation, and training of patients in the TSM arm. This work was supported through a PCORI award (No. 6294), Washington, DC. All statements in this report, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the PCORI, its Board of Governors or Methodology Committee.
Disclosure Statement
No competing financial interests exist.
References
- 1. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jimenez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER, 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB. Heart disease and stroke statistics-2016 update: A report from the American Heart Association. Circulation 2016;133:e38–e60 [DOI] [PubMed] [Google Scholar]
- 2. Choi D, Nemi E, Fernando C, Gupta M, Moe GW. Differences in the clinical characteristics of ethnic minority groups with heart failure managed in specialized heart failure clinics. JACC Heart Fail 2014;2:392–399 [DOI] [PubMed] [Google Scholar]
- 3. Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. Contribution of major diseases to disparities in mortality. N Engl J Med 2002;347:1585–1592 [DOI] [PubMed] [Google Scholar]
- 4. Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation 2005;111:1233–1241 [DOI] [PubMed] [Google Scholar]
- 5. Vivo RP, Krim SR, Cevik C, Witteles RM. Heart failure in Hispanics. J Am Coll Cardiol 2009;53:1167–1175 [DOI] [PubMed] [Google Scholar]
- 6. Bibbins-Domingo K, Pletcher MJ, Lin F, Vittinghoff E, Gardin JM, Arynchyn A, Lewis CE, Williams OD, Hulley SB. Racial differences in incident heart failure among young adults. N Engl J Med 2009;360:1179–1190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Daviglus ML, Talavera GA, Aviles-Santa ML, Allison M, Cai J, Criqui MH, Gellman M, Giachello AL, Gouskova N, Kaplan RC, LaVange L, Penedo F, Perreira K, Pirzada A, Schneiderman N, Wassertheil-Smoller S, Sorlie PD, Stamler J. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the united states. JAMA 2012;308:1775–1784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yancy CW. Heart failure in African Americans. Am J Cardiol 2005;96:3i–12i [DOI] [PubMed] [Google Scholar]
- 9. Yancy CW, Strong M. The natural history, epidemiology, and prognosis of heart failure in African Americans. Congest Heart Fail 2004;10:15–18 [DOI] [PubMed] [Google Scholar]
- 10. Albert NM, Barnason S, Deswal A, Hernandez A, Kociol R, Lee E, Paul S, Ryan CJ, White-Williams C. Transitions of care in heart failure: A scientific statement from the American Heart Association. Circ Heart Fail 2015;8:384–409 [DOI] [PubMed] [Google Scholar]
- 11. Bashi N, Karunanithi M, Fatehi F, Ding H, Walters D. Remote monitoring of patients with heart failure: An overview of systematic reviews. J Med Internet Res 2017;19:e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Adler-Milstein J, Kvedar J, Bates DW. Telehealth among us hospitals: Several factors, including state reimbursement and licensure policies, influence adoption. Health Aff (Millwood) 2014;33:207–215 [DOI] [PubMed] [Google Scholar]
- 13. Kobb R, Hoffman N, Lodge R, Kline S. Enhancing elder chronic care through technology and care coordination: Report from a pilot. Telemed J E Health 2003;9:189–195 [DOI] [PubMed] [Google Scholar]
- 14. Kotb A, Cameron C, Hsieh S, Wells G. Comparative effectiveness of different forms of telemedicine for individuals with heart failure (HF): A systematic review and network meta-analysis. PLoS One 2015;10:e0118681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Clark RA, Inglis SC, McAlister FA, Cleland JG, Stewart S. Telemonitoring or structured telephone support programmes for patients with chronic heart failure: Systematic review and meta-analysis. BMJ 2007;334:942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schofield RS, Kline SE, Schmalfuss CM, Carver HM, Aranda JM, Jr., Pauly DF, Hill JA, Neugaard BI, Chumbler NR. Early outcomes of a care coordination-enhanced telehome care program for elderly veterans with chronic heart failure. Telemed J E Health 2005;11:20–27 [DOI] [PubMed] [Google Scholar]
- 17. Finkelstein SM, Speedie SM, Potthoff S. Home telehealth improves clinical outcomes at lower cost for home healthcare. Telemed J E Health 2006;12:128–136 [DOI] [PubMed] [Google Scholar]
- 18. Hebert MA, Korabek B, Scott RE. Moving research into practice: A decision framework for integrating home telehealth into chronic illness care. Int J Med Inform 2006;75:786–794 [DOI] [PubMed] [Google Scholar]
- 19. Cooper R, Cutler J, Desvigne-Nickens P, Fortmann SP, Friedman L, Havlik R, Hogelin G, Marler J, McGovern P, Morosco G, Mosca L, Pearson T, Stamler J, Stryer D, Thom T. Trends and disparities in coronary heart disease, stroke, and other cardiovascular diseases in the united states: Findings of the national conference on cardiovascular disease prevention. Circulation 2000;102:3137–3147 [DOI] [PubMed] [Google Scholar]
- 20. Inglis SC, Clark RA, Dierckx R, Prieto-Merino D, Cleland JG. Structured telephone support or non-invasive telemonitoring for patients with heart failure. Cochrane Database Syst Rev 2015;10:CD007228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ong MK, Romano PS, Edgington S, Aronow HU, Auerbach AD, Black JT, De Marco T, Escarce JJ, Evangelista LS, Hanna B, Ganiats TG, Greenberg BH, Greenfield S, Kaplan SH, Kimchi A, Liu H, Lombardo D, Mangione CM, Sadeghi B, Sarrafzadeh M, Tong K, Fonarow GC. Effectiveness of remote patient monitoring after discharge of hospitalized patients with heart failure: The Better Effectiveness After Transition—Heart Failure (BEAT-HF) randomized clinical trial. JAMA Intern Med 2016;176:310–318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chaudhry SI, Mattera JA, Curtis JP, Spertus JA, Herrin J, Lin Z, Phillips CO, Hodshon BV, Cooper LS, Krumholz HM. Telemonitoring in patients with heart failure. N Engl J Med 2010;363:2301–2309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Trief PM, Izquierdo R, Eimicke JP, Teresi JA, Goland R, Palmas W, Shea S, Weinstock RS. Adherence to diabetes self care for white, African-American and Hispanic American telemedicine participants: 5 Year results from the IDEATel project. Ethn Health 2013;18:83–96 [DOI] [PubMed] [Google Scholar]
- 24. Artinian NT, Washington OG, Templin TN. Effects of home telemonitoring and community-based monitoring on blood pressure control in urban African Americans: A pilot study. Heart Lung 2001;30:191–199 [DOI] [PubMed] [Google Scholar]
- 25. Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr., Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL. 2013 ACCF/AHA guideline for the management of heart failure: A report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. Circulation 2013;128:e240–e327 [DOI] [PubMed] [Google Scholar]
- 26. Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr., Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL. 2013 ACCF/AHA guideline for the management of heart failure: Executive summary: A report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. Circulation 2013;128:1810–1852 [DOI] [PubMed] [Google Scholar]
- 27. Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr., Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL. 2013 ACCF/AHA guideline for the management of heart failure: A report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Am Coll Cardiol 2013;62:e147–e239 [DOI] [PubMed] [Google Scholar]
- 28. Wingood GM, DiClemente RJ. The ADAPT-ITT model: A novel method of adapting evidence-based HIV interventions. J Acquir Immune Defic Syndr 2008;47(Suppl 1):S40–S46 [DOI] [PubMed] [Google Scholar]
- 29. Pekmezaris R, Schwartz RM, Taylor TN, DiMarzio P, Nouryan CN, Murray L, McKenzie G, Ahern D, Castillo S, Pecinka K, Bauer L, Orona T, Makaryus AN. A qualitative analysis to optimize a telemonitoring intervention for heart failure patients from disparity communities. BMC Med Inform Decis Mak 2016;16:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rector TS, Cohn JN. Assessment of patient outcome with the Minnesota living with heart failure questionnaire: Reliability and validity during a randomized, double-blind, placebo-controlled trial of pimobendan. Pimobendan Multicenter Research Group. Am Heart J 1992;124:1017–1025 [DOI] [PubMed] [Google Scholar]
- 31. Kroenke K, Spitzer RL, Williams JB, Lowe B. An ultra-brief screening scale for anxiety and depression: The phq-4. Psychosomatics 2009;50:613–621 [DOI] [PubMed] [Google Scholar]
- 32. Rollman BL, Herbeck Belnap B, Mazumdar S, Houck PR, He F, Alvarez RJ, Schulberg HC, Reynolds CF, 3rd, McNamara DM. A positive 2-item patient health questionnaire depression screen among hospitalized heart failure patients is associated with elevated 12-month mortality. J Card Fail 2012;18:238–245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Konstam V, Gregory D, Chen J, Weintraub A, Patel A, Levine D, Venesy D, Perry K, Delano C, Konstam MA. Health-related quality of life in a multicenter randomized controlled comparison of telephonic disease management and automated home monitoring in patients recently hospitalized with heart failure: SPAN-CHF II trial. J Card Fail 2011;17:151–157 [DOI] [PubMed] [Google Scholar]
- 34. Huygens MW, Vermeulen J, Swinkels IC, Friele RD, van Schayck OC, de Witte LP. Expectations and needs of patients with a chronic disease toward self-management and ehealth for self-management purposes. BMC Health Serv Res 2016;16:232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Israel BA, Schulz AJ, Parker EA, Becker AB. Community-campus partnerships for health. Community-based participatory research: Policy recommendations for promoting a partnership approach in health research. Educ Health 2001;14:182–197 [DOI] [PubMed] [Google Scholar]
- 36. Koehler F, Winkler S, Schieber M, Sechtem U, Stangl K, Böhm M, Boll H, Kim SS, Koehler K, Lücke S, Honold M, Heinze P, Schweizer T, Braecklein M, Kirwan BA, Gelbrich G, Anker SD; TIM-HF Investigators. Telemedical Interventional Monitoring in Heart Failure (TIM-HF), a randomized, controlled intervention trial investigating the impact of telemedicine on mortality in ambulatory patients with heart failure: Study design. Eur J Heart Fail 2010;12:1354–1362 [DOI] [PubMed] [Google Scholar]
- 37. Dang S, Karanam C, Gomez-Orozco C, Gomez-Marin O. Mobile phone intervention for heart failure in a minority urban county hospital population: Usability and patient perspectives. Telemed J E Health 2017;23:544–554 [DOI] [PubMed] [Google Scholar]
- 38. Dang S, Karanam C, Gomez-Marin O. Outcomes of a mobile phone intervention for heart failure in a minority county hospital population. Telemed J E Health 2017;23:473–484 [DOI] [PubMed] [Google Scholar]
- 39. Balakrishnan MP, Herndon JB, Zhang J, Payton T, Shuster J, Carden DL. The association of health literacy with preventable emergency department visits: A cross-sectional study. Acad Emerg Med 2017;24:1042–1050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Nouryan CN, Morahan S, Pecinka K, Akerman M, Lesser M, Chaikin D, Castillo S, Zhang M, Pekmezaris R. Home telemonitoring of community-dwelling heart failure patients after home care discharge. Telemed J E Health 2018. [Epub ahead of print]; DOI: 10.1089/tmj.2018.0099 [DOI] [PubMed] [Google Scholar]
- 41. Feltner C, Jones CD, Cene CW, Zheng ZJ, Sueta CA, Coker-Schwimmer EJ, Arvanitis M, Lohr KN, Middleton JC, Jonas DE. Transitional care interventions to prevent readmissions for persons with heart failure: A systematic review and meta-analysis. Ann Intern Med 2014;160:774–784 [DOI] [PubMed] [Google Scholar]
- 42. Kilgore M, Patel HK, Kielhorn A, Maya JF, Sharma P. Economic burden of hospitalizations of medicare beneficiaries with heart failure. Risk Manag Healthc Policy 2017;10:63–70 [DOI] [PMC free article] [PubMed] [Google Scholar]