Abstract
BACKGROUND:
Persons with moderate to severe TBI are at increased risk for unintentional injury or harm in the home and community; however, there is currently no standard measure of safety risk they face now and in the future.
OBJECTIVE:
To develop comprehensive and content valid scales and item pools for assessing safety and risk for persons with moderate to severe traumatic brain injuries.
METHOD:
Qualitative psychometric methods for developing scales and items were used including literature review, item development and revision, focus groups with interdisciplinary rehabilitation staff (n = 26) for rating content validity, and cognitive interviewing of TBI family members (n = 9) for assuring item clarity.
RESULTS:
The Safety Assessment Measure is comprised of 6 primary scales – Cognitive Capacity, Visuomotor Capacity, Wheelchair Use, Risk Perception, Self-Regulation, and Compliance Failures with Safety Recommendations – in which family caregivers or clinicians rate the risk for unintentional injury or harm in adults who have sustained moderate or severe TBI. The scale item pools encompass a broad spectrum of everyday activities that pose risk in the home and community and were rated as having excellent levels of content validity.
CONCLUSIONS:
The Safety Assessment Measure scales and items cover a broad range of instrumental activities of daily living that can increase the risk of unintentional injuries or harm. Empirical evidence suggests that the Safety Assessment Measure items have excellent content validity. Future research should use modern psychometric methods to examine each scale unidimensionality, model fit, and precision.
Keywords: Unintentional injuries, brain injuries, cognition, diagnosis, rehabilitation
1. Introduction
Persons with moderate to severe TBI are at increased risk for unintentional injury or harm (UIH) when transitioning from medical inpatient and outpatient rehabilitation to home and community settings (Seel, et al., 2007). Four TBI registry studies show that unintentional injury is a leading cause of death (18–20%) in the year following discharge, and the standardized mortality rate from UIH is 3 to 36 times greater for people with TBI compared to the general population (Harrison-Felix, et al., 2006; McMillan & Teasdale, 2007; Selassie, et al., 2005; Ventura, et al., 2010). Unintentional injuries also cause high rates of emergency room (ER) visits and hospitalizations. Carlson et al. (2012) found that 32% of TBI participants (n = 504) had unintentional injuries that resulted in 228 ER visits or hospitalizations from 3-months to several years following discharge for a TBI. These unintentional injuries were similar to those found in the general population, such as falls; motor vehicle crashes; pedestrian, bicycle or motorcycle crashes; improper use of electrical equipment; fire and burns; being struck by or against an object; poisoning; and firearm-related incidents (Carlson, et al., 2012). Additional risk of harm may occur due to victimization, loss of money or valuables, property damage, medication errors, and inappropriately responding to emergency situations or managing medical conditions (J. S. Kreutzer, et al., 2009; Reichard, et al., 2007; Tyson, Pham, Brown, & Mayer, 2012). Caregivers and payers often manage these risks by providing part-or full-time supervision, which have high economic and social costs.
Self-managing activities that increase UIH risk is challenging for persons who have sustained TBI. Impaired attention, memory, visuomotor skills, awareness and self-regulation affect individuals’ abilities to perform everyday activities, recognize risk, take preventive actions, learn safety strategies, and apply compensatory skills (Riley, Brennan, & Powell, 2004; Tyson, et al., 2012). Persons with TBI who report difficulties performing activities often experience anxiety, frustration, loss of confidence, and depression that result in activity avoidance and diminished life quality (Riley et al., 2004; Seel, Macciocchi, & Kreutzer, 2010; Selassie et al., 2008). Conversely, persons with TBI who highly value their independence may dismiss family and provider concerns about safety, which can lead to confrontation, conflict, power struggles, and strained relations (Durgin, 2000).
For family members, balancing supervisory needs, independent return to activities, and safety is complicated. Families often rely on rehabilitation providers’ determinations of supervision needs (Cooney, Kennedy, Hawkins, & Hurme, 2004; Galski, Ehle, McDonald, & Mackevich, 2000; Macciocchi & Stringer, 2001; Tyson et al., 2012) but short rehabilitation stays often do not allow providers to assess patient safety on instrumental activities of daily living (IADLs) in the home and community. Further, little time is available to train families how to manage high risk situations. Providers often recommend high levels of supervision and activity restrictions, which may unnecessarily limit clients’ autonomy (Banja, 1994; Macciocchi, 2009; Macciocchi & Stringer, 2001; Ruchinskas, Macchiocchi, Howe, & Newton, 2001). While many persons with TBI-related impairments show improvement in physical and cognitive functioning over time, some families continue to follow providers’ initial supervision recommendations or may not know how or when to help survivors transition to independent and safe engagement in IADLs. Other families may have limited support or may need to return to work, which may force them to leave TBI survivors on their own and in environments that present hazards and increased risk (Pai, Zadov, & Hickman, 2012). Consequently, many people with TBI who are at high risk for UIH are under-supervised while others who have low risk are overly restricted (Durgin, 2000).
Currently, there is no established measure to guide family members, rehabilitation providers, and payers in assessing safety risk in the home and community for persons who have sustained TBI. An empirically validated safety assessment measure would improve rehabilitation practice by providing observable, quantified evidence that can improve caregiver knowledge of activities and factors associated with unsafe events in the home and community following TBI. Such a measure would provide an evidence basis to guide the level of family involvement required to keep persons that have TBI-related impairments safe within the least restrictive environment. A safety assessment measure may also provide an evidence basis to justify additional healthcare service provision including outpatient rehabilitation, home health/community supports, or life skills coaching to facilitate selfmanagement of safety-related activities in high risk TBI survivors.
Using a contemporary, state-of-the-science, mixed qualitative-quantitative methods approach within the framework of modern measurement theory would facilitate the development of a safety assessment measure that could enhance clinical practice and research. Qualitative methods that incorporate stakeholder input and feedback to develop an ecologic and content valid item pool have become a standard initial phase in the outcome measurement development process (Administration, 2009; Cella et al., 2007; Lasch et al., 2010; Magasi et al., 2012; Velozo, et al., 2012). A safety assessment measure based on item response theory (IRT) methods would possess a hierarchical, progressive set of items that could serve as a behavioral diagnostic for treatment planning, modifying home environments, and implementing technological supports. An empirically valid, interval level, safety assessment measure would also provide clinicians and researchers with a reliable instrument that could evaluate longitudinal changes in safety risk, including outcomes for clinical trials that evaluate interventions to improve safety.
This study is the first phase of a three phase scale development project to develop and evaluate the Safety Assessment Measure (SAM) for persons who have sustained moderate or severe TBI. The SAM is a set of scales that captures a wide range of safety issues that persons with TBI face in their everyday living situations in the home and the community. The SAM is intended for use following inpatient rehabilitation discharge with the primary raters of safety and risk being family and non-family caregivers, as well as clinicians and paraprofessionals in outpatient rehabilitation, day program, brain injury clubhouse, home health, and neurobehavioral treatment settings. The primary objectives of this study are to define the conceptual framework and constructs that ground the SAM scales and items, describe the item pool for each proposed scale, and evaluate each scale’s content validity.
2. Method
2.1. Qualitative approach to develop the safety assessment measure
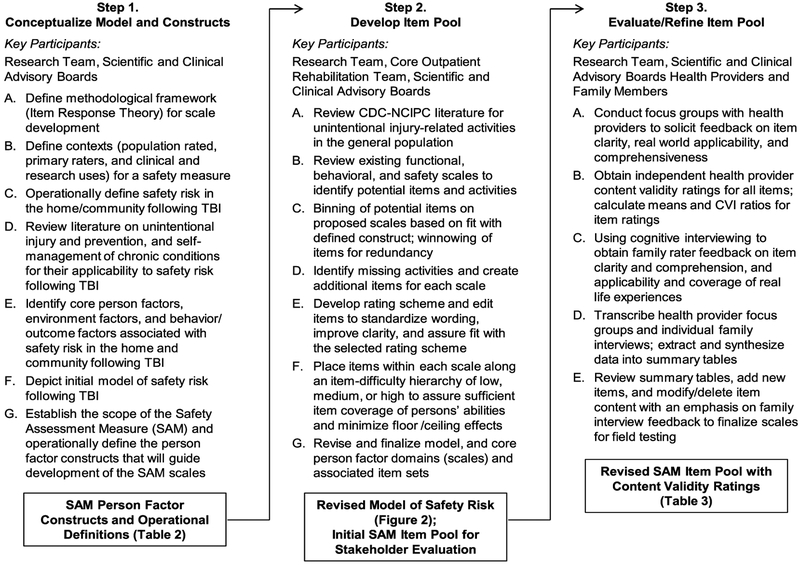
Based on state-of-the-science recommendations on developing health outcome measures, we undertook three qualitative steps (see Fig. 1) to develop the SAM item pool: step 1-conceptualize a theoretical model and scale constructs; step-2 develop an item pool; and step 3-evaluate and revise the item pool (Cella et al., 2007; Velozo et al., 2012). Participants included the research team, the scientific and clinical advisory boards, five clinicians from our TBI day rehabilitation program, additional TBI rehabilitation health providers who participated in focus groups, and family members of persons with TBI who provided feedback in cognitive interviews. Key methods within each step are denoted using capital letters. The resulting primary products (denoted within framed text boxes at the bottom of each step) were then used to inform proceeding steps (indicated by arrows).
Fig. 1.
Qualitative methodology implemented for theoretical model and item pool development.
2.2. Conceptualize model and constructs
2.2.1. Methodological framework for measurement
Item response theory (IRT) and use of Rasch methods are the state-of-the-science framework for developing and evaluating outcome measures (Administration, 2009; Cella et al., 2007; Reeve & Fayers, 2005; Velozo et al., 2012). A core principle of IRT is that the probability of rating an item with a response that indicates a higher level of functioning is dependent on “person ability,” “item difficulty,” and the item’s success in discriminating person ability on an outcome of interest (Velozo et al., 2012). Thus, a difficult item on a measurement scale should have a higher probability of being successfully performed by persons with high ability than persons with medium or low ability. Another core principle of IRT is that scale items must be unidimensional (i.e., measure a single latent construct), and be capable of detecting differences in person ability related to the construct (Reeve & Fayers, 2005; Velozo et al., 2012). Differentiation within a scale requires that items are developed in an a priori hierarchical difficulty order within each of the scales (Stone, 1997; Velozo et al., 2012).
2.2.2. Definition of safety risk and contexts for scale use
We defined safety as “the ability to participate in home activities and community living free from harm.” Safety risk is a state of uncertainty in which unintentional harm may arise from a future event, activity, or behavior. Temporally, the threat of a safety risk is likely or imminent. Safety risk is observable and can lead directly to unintentional harm including death, physical injury, financial loss, property damage, or incarceration. The scope of safety risk is not limited to the person with TBI-safety risk may affect other persons, animals, and property. Exposure to violent and aggressive acts is also a safety risk. Conversely, pre-meditated, intentional harmful acts to one’s self (e.g., self-mutilation, suicide), another person, or property secondary to sociopathic and psychiatric disorders are outside the scope of our assessment.
The target of evaluation is persons aged 16 and older who sustained moderate or severe TBI, required acute hospitalization for their injury, and are now returning to everyday activities of daily living in the home and community. Self-assessment by persons with attention, memory, judgment, and self-control deficits are affected by impaired awareness and metacognition (Cavallo, Kay, & Ezrachi, 1992; Hart, Sherer, Whyte, Polansky, & Novack, 2004; Malec, 2004; Seel, Kreutzer, & Sander, 1997). Therefore, we focused on collecting safety ratings from family members and health providers in this initial phase of measure development.
The primary use for the safety measure is clinical with an emphasis on using the measure to: (a) make empirically-based prognoses on risk of unsafe events;(b) assess current safe functioning level and identify primary person factors that drive risk; (c) inform individualized treatment planning related to prevention, supervision needs, and specific functional areas and activities to be targeted; and (d) assess change in safety risk over time, including evaluating individual treatment as well as program effectiveness. A second important use is research and includes longitudinal, prognosis and treatment efficacy and effectiveness studies. Long-term, payers and policy-makers may find epidemiological and treatment effectiveness data useful for reimbursing home health care/supervision and/or prevention education and treatment.
2.2.3. Model and construct development
The research team used a simple concept mapping approach to develop models and scale constructs. First, we reviewed the literature and evaluated models related to unintentional injury and prevention, and self-management of chronic medical conditions, to identify potential person-centered behavioral determinants (Sleet & Gielen, 2007; Sleet, et al., 2006). Next, we considered how TBI-related impairments–cognitive, physical, and behavioral-might play a role in safety risk. Social Cognitive Theory models provided input on person-environment-behavior factors and interactions (Bandura, 1986; Simons-Morton, 2006; Sleet et al., 2006). Then, we constructed a model based on an individual level behavior change framework with four person factor constructs and operational definitions that would serve as the basis for creating scales. Two conference calls each were conducted with the clinical and scientific advisory boards to review the proposed constructs, obtain agreement on their importance, and evaluate the operational definitions of constructs for completeness and unidimensionality.
2.3. Develop item pool
2.3.1. Item identification, binning and winnowing
Item pool content was developed with consideration given to the primary scales and their operational definitions, safety concerns in the general population, safety concerns specific to the TBI population, and feedback from TBI therapists and our clinical advisory board. We reviewed the research literature to identify measures and items that were relevant to the core scale constructs that would comprise the Safety Assessment Measure (SAM) (DeWalt, et al., 2007). We reviewed 11 self-report or clinician-rated measures of neurobehavioral function, decision-making, risk-taking, awareness of impairment, and safety judgment and function in rehabilitation or psychiatric populations (Blais & Weber, 2006; Borgaro & Prigatano, 2003; Chiu & Oliver, 2006; Hart, 2000; Hart et al., 2006; J. Kreutzer & Marwitz, 2000;J. S. Kreutzer et al., 2009; J. Kreutzer, Seel, & Marwitz, 1999; Morrongiello & Corbett, 2006; Oliver, Blathwayt, Brackley, & Tamaki, 1993; Patton, Stanford, & Barratt, 1995; Sherer et al., 1995; Velozo & Peterson, 2001; Whyte, Hart, Bode, & Malec, 2003; Yudofsky, et al., 1986). Only 2 measures specifically addressed safety issues in the home and community, both of which were organized predominately by activity type (Chiu & Oliver, 2006; J. Kreutzer & Marwitz, 2000). Conversely, the SAM scale constructs are predominately organized by functional abilities that would identify the underlying causes of safety risk across everyday activities and participation. From these 11 measures, we binned and winnowed items that were potentially associated with our 6 primary scale constructs (DeWalt et al., 2007) Forty-six of these extracted items were modified and included in the field test version of the SAM scale item pools.
2.3.2. Item revision and development
To assure full coverage of real life experiences within each scale construct, the research and clinical team developed additional items. In addition to personal experience with the TBI population, we used the Centers for Disease Control and Prevention-National Center for Injury Prevention and Control (Centers for Disease Control and Prevention, (n.d.)) injury reporting structure for the general population to assist in identifying activities in which injuries may be likely to occur (see Table 1) (Centers for Disease Control and Prevention, (n.d.)). We supplemented the CDC list, based on feedback from the clinical team, clinical advisory board and family members, with other activities and aspects of harm that are common in persons who sustain moderate to severe TBI (see Table 1, column 1). We also considered the settings in which UIH occurs including inside and outside of the home; on streets, highways, sidewalks, and parking lots; in sports facilities, recreation centers, lakes, rivers and pools; and in the community such as in public buildings. Because the focus of our scale was adults who were transitioning from basic self-care to instrumental activities of daily living, we did not create items for hospital-based, school, or workplace settings.
Table 1.
Activities associated with unintentional injury or harm and their representation in the safety assessment measure item pool
| Activities/Causes of Unintentional Injury or Harm | # Items on SAM | % of Items on SAM |
|---|---|---|
| CDC-NCIPC Related Activities or Causes | ||
| ► Transportation (including motor vehicle, bicycle, motorcycle, pedestrian, train, boat, and airplane). | 30 | 24% |
| ► Falls, e.g., walking, standing, transferring | 18 | 14% |
| ► Aggressive or violent behavior | 12 | 10% |
| ► Identification, avoidance or response to persons or animals who intend harm | 11 | 9% |
| ► Medication (and medical condition) management | 9 | 7% |
| ► Recreation, e.g., sports, water activities | 8 | 6% |
| ► Fires, burns, scalds, e.g., use of fire, hot water, or chemicals | 8 | 6% |
| ► Poisoning (swallowing or breathing harmful substances such as bleach, carbon monoxide, or too many pills or drugs) | 4 | 3% |
| ► Use of electric devices or equipment | 4 | 3% |
| ► Use of firearms | 2 | 2% |
| ► Use of sharp objects or devices | 2 | 2% |
| ► Eating (food poisoning, allergic reaction) | 2 | 2% |
| Additional Risk Activities in Persons with TBI | ||
| ► Wheelchair Use | 6 | 5% |
| ► Money, Valuables Management | 6 | 5% |
| ► Sexual | 4 | 3% |
| ► Emergency Identification and Response | 3 | 2% |
Notes. CDC-NCIPC = Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; Activities based on CDC-NCPIC: A Report to Congress, 1999. Total number of items reflected in column 2 (130) exceeds the total number of items on scale (126) due to a few items covering more than one activity.
Several sets of administration instructions and item rating schemes were considered that emphasized family and clinician raters’ direct observation of person behavior on specific activities, controlled for the confounds of assistance or supervision during activities, and allowed for judgment in determining levels of risk (DeVellis, 2006). The SAM rating instructions read as follows: “The following Items in this questionnaire ask about behaviors that could put a person with a brain injury at increased risk for harm. Based on your best judgment of the person’s current ability and behavior, please rate the likelihood of each behavior occurring if the person with TBI did not have any help or supervision – for example, if no one was there to step in, how likely is it that the person will not be able to exit a room on their own in an emergency?”
The item rating scheme has the following four responses: 4-highly likely to occur; 3-somewhat likely to occur; 2-somewhat unlikely to occur; and 1-highly unlikely to occur. A not applicable response is offered for a subset of items with a specific reason for each not applicable response noted, e.g., for the item, “Is not responsible with firearms,” “Not applicable, person with TBI does not use firearms”.
The research team edited and standardized item wording to: (a) fit the selected rating scheme; (b) be unidirectional, e.g., not reverse scored; (c) be easy to understand with examples provided if deemed helpful; and (d) maintain no higher than a 9th grade reading level. To meet the key assumptions of IRT, the research and clinical teams re-reviewed items and the proposed scale constructs for unidimensionality (Reeve & Fayers, 2005). Each item was then rated as being of high, medium, or low difficulty to assess coverage and identify “gaps” in the scale’s hierarchical difficulty continuum including floor and ceiling effects (Stone, 1997; Velozo et al., 2012). The clinical and scientific advisory boards provided feedback on the rating scheme, item selection and editing, and the final model and scales.
2.4. Evaluate and refine the item pool
2.4.1. Health provider focus groups and rating of content validity
Health providers participated in 6 focus groups to discuss item content, clarity, and comprehensiveness. Participants were recruited from Shepherd Pathways Day Rehabilitation Program, Marcus Community Bridge Program, Side-by-Side Brain Injury Clubhouse, and Restore Neurobehavioral Center in Atlanta, Georgia. The 5 clinicians involved in item development did not participate in the focus groups. Focus group sizes ranged from 2–6 participants and lasted 60–70 minutes. The research coordinator led semi-structured group interviews. Following group discussion, simple concept mapping was used in which healthcare providers independently quantified the extent that each scale item represented the safety experiences of persons with TBI using a 4-point rating scale (4-critically important, 3-very important, 2-somewhat important, and 1-not important). All focus group proceedings were audio taped and transcribed with identifiers removed.
Following the completion of all focus groups, the research coordinator reviewed the transcripts, created a spreadsheet summarizing respondent comments, and entered health provider item ratings into an SPSS data file. The mean importance score for each item was calculated. An Item Level-Content Validity Indicator (I-CVI) ratio was determined by computing the percentage of critically important plus very important ratings for each item (Polit & Beck, 2006). Excellent item validity is indicated by an I-CVI ratio of ≥78% (Polit & Beck, 2006). The research team reviewed the focus group summaries and content validity ratings, and modified, expanded, deleted, or added items accordingly.
2.4.2. Cognitive interviewing of family members and final item revisions
The lead research coordinator conducted cognitive interviews with family members of persons with TBI using a semi-structured script to obtain feedback on item comprehension, meaningfulness, and comprehensiveness (DeWalt et al., 2007; Willis, 2005). Interviews were audio-taped and transcribed. Five family members were interviewed and items revised based on their feedback. Following these revisions, four more family members were interviewed. With minor changes following their feedback, the research team was satisfied that the item pool was comprehensive and understandable.
3. Results
3.1. Social cognitive theory framework of unsafe events following TBI
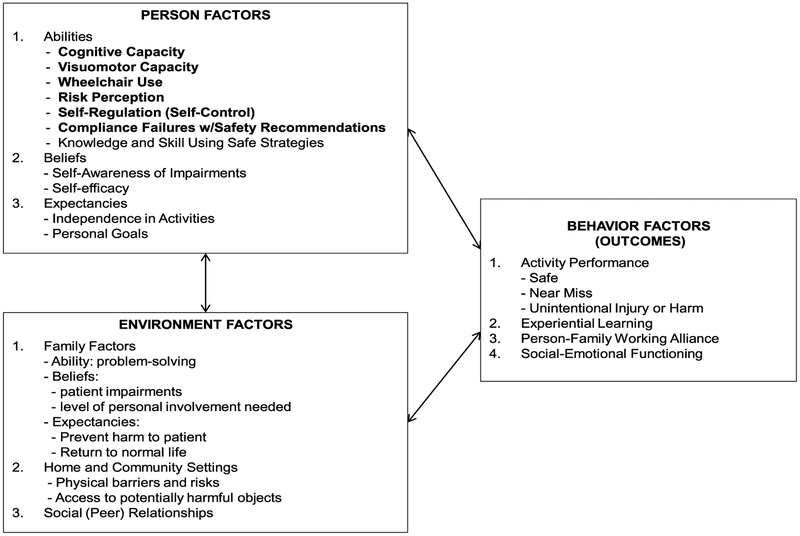
Social cognitive theory was selected as the most suitable framework for understanding person, environment, and behavior factors that represent safety risk in the home and community. We conceptualized unsafe behavior and events as the result of interactions between the person with TBI, his or her everyday environment, and behavior (see Fig. 2). Personal factors including the abilities, beliefs and expectancies of a person who has sustained moderate to severe TBI are considered the primary determinants of safety risk and behaviors that result in UIH. The 6 primary SAM scales measure person abilities (indicated by bold lettering) and are hypothesized to be the most critical factors associated with UIH. Environmental factors such as family members’ abilities, beliefs, and expectancies; the home and community settings; social relationships; and community supports play mediating roles to varying degrees in shaping personal factors and behavior. In particular, the amount and proximity of family involvement (e.g., supervision, care coordination) is a primary environmental factor that interacts with person factors to influence UIH. The behavior factors of persons with TBI include their activity levels, performance of activities, experiential learning, social interactions, emotional responses, and working alliance with family members. These behavior factors provide an observable gauge of safe and unsafe functioning and feedback that shapes person and environmental responses to behavior.
Fig. 2.
Social Cognitive Theory model of safety risk in the home and community following TBI.
3.2. Scale constructs (Personal Ability Factors) and definitions
The proposed constructs, a summary of stakeholder and expert feedback on the constructs, and the final construct/scale names and their operational definitions are presented in Table 2. Primary decisions reflected in Table 2 include: (a) removing primarily upper extremity based activities from the Physical Capacity Scale and focusing on walking mobility as a primary construct, (b) adding Wheelchair Use as a primary construct/scale; and (c) separating activities and behaviors related to complying with medical recommendations from perceiving risk and creating separate scales. The six scales are: Cognitive Capacity, Visuomotor Capacity, Wheelchair Use, Risk Perception, Compliance Failures with Safety Recommendations, and Self-Regulation.
Table 2.
Person factor constructs (scales) and operational definitions for the safety assessment measure
| Proposed Construct | Stakeholder / Expert Feedback and Research Team Decisions | Field Testing Scale Name | Operational Definition of Scale Construct |
|---|---|---|---|
| Cognitive Capacity |
|
Cognitive Capacity |
|
| Physical Capacity |
|
Visuomotor Capacity |
|
|
Wheelchair Use |
|
|
| Perceived Susceptibility to Harm |
|
Risk Perception |
|
| Compliance Failures with Safety Recommendations |
|
||
| Self-Regulation |
|
Self-Regulation |
|
Note. Following field testing, patients and families in focus groups to develop a translational report recommended renaming the scales; the final scale names reflect their feedback and research team decisions.
Risk due to substance use was developed as a stand-alone SAM scale and 19 items were generated. Following clinical and research advisory board review, there was consensus that alcohol and other drug use is not a unidimensional construct and that items would not conform to a hierarchical continuum. We decided to use existing measures to assess the presence and severity of alcohol and other drug use, and evaluate their association with safety risk. Motor vehicle operation and childcare items were initially developed and distributed across the 6 primary SAM scales. Given these activity sets are applicable to only a relatively small subset to persons with moderate or severe TBI, the clinical and research advisory boards and research team agreed that these activities would best be assessed on supplemental scales named Motor Vehicle Operation and Child Caretaking.
3.3. Safety Assessment Measure item pool and content validity ratings
Focus groups evaluated the Safety Assessment Measure item pool (n = 145 items) for the 6 primary and 2 supplemental scales. Participants were 26 TBI healthcare professionals with backgrounds in case management, nursing, occupational therapy, physical therapy, speech language pathology, therapeutic recreation, and psychology. On average, healthcare professionals were aged 40.7 (SD = 12.2), predominately female (85%), predominately white (69%) or black (19%), and were well-educated (42% with master’s and 35% with bachelor’s degrees). Health providers had a mean of 9.2 (SD = 7.9) years of TBI rehabilitationexperienceandreportedonaverage36.6 (SD = 9.5) hours weekly treating clients with TBI.
Based on focus group feedback and core research team re-examination of items, 32 items were removed from the pool primarily due to confounds (e.g., multiple activities or behaviors assessed within item content), similarity with retained items, or the activity lacked an imminent safety threat. The retained items (n = 115 items) and their content validity ratings, as well as 11 new items recommended in either the focus groups or the family member cognitive interviews are presented in Table 3, columns 1–3. Overall, the SAM item pool was rated as having high levels of content validity. Of the 115 retained SAM scale items, 106 items (92%) had Item-Content Validity Index ratios ≥78%, indicating excellent content validity. Sixty-nine (60%) of the retained items had I-CVI ratios ≥90%.
Table 3.
Safety assessment measure: Scales, items, and content validity
| Scale and Associated Item Pool (n = 126 total items) | I-CVI | Mean | Activity/Cause | Primary Harm to: |
|---|---|---|---|---|
| Cognitive Capacity (n = 21 items) | ||||
| Crosses street inappropriately (e.g., does not look, misinterprets walk signs, misjudges traffic) | 100% | 3.96 | Transportation | Self |
| Mistakenly takes wrong dose of medication (e.g. too little, takes twice) | 100% | 3.96 | Medical Management | Self |
| Forgets to take prescribed medication (e.g. seizure, diabetes, high blood pressure) | 100% | 3.92 | Medical Management | Self |
| Uses other people’s prescribed medications (e.g. pain, sleep) | 100% | 3.92 | Medical Management | Self |
| Does not know when an injury or illness requires medical care (e.g. deep cut, chest pain) | 100% | 3.77 | Medical Management | Self |
| Leaves cooking food unattended | 100% | 3.67 | Fire/Burns | Self. Property |
| Forgets to use mitt or towel when picking up hot items | 100% | 3.63 | Fire/Burns | Self |
| Leaves flammable items too close to fire (e.g. paper bag near burner) | 96% | 3.74 | Fire/Burns | Self, Property |
| Forgets to turn off appliances (e.g. stove, iron, space heater) | 96% | 3.74 | Fire/Burns | Self, Property |
| Does not respond to emergency alarms (e.g. smoke, carbon monoxide, weather) | 93% | 3.81 | Emergency Response | Self |
| Sets stove burner too high | 93% | 3.30 | Fire/Burns | Self, Property |
| Does not follow emergency procedures | 89% | 3.76 | Emergency Response | Self |
| Forgets to avoid foods that cause allergic reaction | 85% | 3.30 | Eating | Self |
| Unable to find way if lost in the community | 82% | 3.44 | Avoid Harmful Others | Self |
| Forgets to lock doors and windows when leaving home | 74% | 2.85 | Money, Possessions | Property |
| Misuses microwave (e.g. puts metal objects inside, burns food) | 74% | 2.81 | Electric, Equipment | Property |
| Loses wallet or purse | 67% | 2.81 | Money, Possessions | Property |
| Forgets to put medications away | 62% | 2.76 | Poisoning | Others |
| Forgets to put sharp objects away (e.g., scissors, knives) | 62% | 2.71 | Sharp Objects | Others |
| * Does not react appropriately to warning signs (e.g. wet floor, construction, etc.) | NR | NR | Avoid Harmful Others | Self |
| * Does not check surroundings before walking through a parking lot | NR | NR | Transportation | Self |
| Visuomotor Capacity (n = 14 items) | ||||
| Loses balance when walking up or down stairs | 100% | 3.85 | Falls | Self |
| Does not move to an exit in an emergency | 100% | 3.81 | Emergency Response | Self |
| Loses balance getting in or out of tub | 100% | 3.74 | Falls | Self |
| Loses balance getting in and out of car | 96% | 3.67 | Falls | Self |
| Loses balance while getting on or off toilet | 96% | 3.63 | Falls | Self |
| Loses balance when attempting to stand from a sitting position | 96% | 3.56 | Falls | Self |
| Loses balance when reaching forward | 96% | 3.41 | Falls | Self |
| Trips on things (e.g., curbs, objects, uneven surfaces) | 93% | 3.38 | Falls | Self |
| Loses balance when walking on fiat surfaces | 93% | 3.59 | Falls | Self |
| Loses balance when carrying objects | 93% | 3.52 | Falls | Self |
| Trips when walking in low lit areas | 93% | 3.41 | Falls | Self |
| Loses balance when dressing | 89% | 3.44 | Falls | Self |
| * Bumps into walls, objects, or people | NR | NR | Transportation | Self, Property |
| * Trips when walking in well lit areas | NR | NR | Falls | Self |
| Wheelchair Use (n = 6 items) | ||||
| Uses wheelchair in potentially dangerous environments (e.g. street, rough terrain) | 93% | 3.78 | Wheelchair Use | Self |
| Does not follow wheelchair precautions (e.g. locking brakes, wearing seatbelt, keeping fingers away from spokes, etc.) | 89% | 3.59 | Wheelchair Use | Self |
| Uses wheelchair without required assistance | 85% | 3.58 | Wheelchair Use | Self |
| Moves too fast in wheelchair | 81% | 3.27 | Wheelchair Use | Self, Others |
| Loses control of wheelchair (e.g. tips wheelchair) | 81% | 3.12 | Wheelchair Use | Self |
| * Backs up without checking for people or objects | NR | NR | Wheelchair Use | Self, Others |
| Risk Perception (n = 17 items) | ||||
| Stands on unstable objects (e.g. chair with wheels, top step of ladder, cardboard box) | 100% | 3.85 | Falls | Self |
| Rides in a motor vehicle driven by someone who has been drinking or doing drugs | 100% | 3.77 | Transportation | Self |
| Inappropriately reveals personal information (e.g. bank acct number, social security number) | 100% | 3.73 | Money, Possessions | Property |
| Easily influenced to do risky behaviors | 96% | 3.63 | Avoid Harmful Others | Self, Property |
| Falls asleep while smoking | 93% | 3.85 | Fire, Burns | Self, Property |
| Invites strangers into home | 93% | 3.67 | Avoid Harmful Others | Self, Property |
| Operates equipment while drowsy (e.g., power tools, lawnmower) | 93% | 3.63 | Electric, Equipment | Self |
| Meets in person with strangers found on the internet | 93% | 3.58 | Avoid Harmful Others | Self, Property |
| Goes alone in dangerous areas (e.g. high crime, poorly lit areas) | 89% | 3.65 | Avoid Harmful Others | Self, Property |
| Jumps or dives into a body of water without knowing depth | 85% | 3.62 | Recreation | Self |
| Goes with stranger (e.g., gets in car, goes to home) | 85% | 3.60 | Avoid Harmful Others | Self, Property |
| Swings objects without looking for others in path (e.g., clubs, yard equipment) | 85% | 3.31 | Recreation and Equip. | Others, Property |
| Goes on slippery surfaces | 82% | 3.37 | Falls | Self |
| Easily tricked into giving strangers money | 81% | 3.19 | Avoid Harmful Others | Property |
| Readily gives money to family or friends without considering consequences | 78% | 3.04 | Money, Possessions | Property |
| Approaches unknown animals | 74% | 3.00 | Avoid Harmful Others | Self |
| Does not prepare for weather (e.g. dress warm on a cold day, wear sunscreen on sunny day) | 67% | 2.73 | Recreation | Self |
| Compliance Failures with Safety Recommendations (n = 20 items) | ||||
| Refuses to take prescribed medications (e.g., seizure, diabetes, high blood pressure) | 100% | 3.96 | Medical Management | Self |
| Drives motor vehicle against recommendations | 100% | 3.89 | Transportation | Self, Others |
| Does not wear a helmet when recommended (e.g. bicycle, scooter, motorcycle) | 100% | 3.77 | Transportation | Self |
| Does not follow precautions when using electrical equipment (e.g. power tools, kitchen appliances) | 100% | 3.73 | Electric, Equipment | Self, Property |
| Does not follow precautions when using fire | 100% | 3.69 | Fire, Burns | Self, Property |
| Does not follow precautions when using sharp devices | 100% | 3.48 | Sharp Objects | Self |
| Uses firearms against recommendations | 96% | 3.78 | Firearms | Self, Others |
| Operates recreational vehicle (e.g. golf cart, boat, jet ski) against recommendations | 96% | 3.63 | Recreation | Self, Others |
| Climbs against recommendations (e.g., stool, ladder, stairs) | 93% | 3.62 | Falls | Self |
| Ignores advice to seek medical care | 93% | 3.48 | Medical Management | Self |
| Participates in sports or recreational activities against recommendations | 93% | 3.46 | Recreation | Self |
| Does not follow precautions on warning labels | 93% | 3.33 | Medical/Fire, Burns | Self |
| Is not responsible with firearms | 91% | 3.61 | Firearms | Self, Others |
| Does not wear a seatbelt | 85% | 3.44 | Transportation | Self |
| Does not follow exercise precautions (e.g. runs in severe heat, lifts too much weight) | 85% | 3.37 | Recreation | Self |
| Goes on amusement park rides (e.g. roller coaster) against recommendations | 85% | 3.22 | Recreation | Self |
| Ignores important diet restrictions for medical condition (e.g. diabetes, swallowing disorder) | 82% | 3.42 | Medical/Eating | Self |
| Goes in water without recommended supervision (e.g., bath, pool, natural body of water) | 82% | 3.35 | Medical/Recreation | Self |
| Does not follow precautions when using chemical solutions (e.g. mixing cleaning products, insecticide in closed space) | 78% | 3.40 | Poisoning | Self |
| Does not use recommended safety equipment (e.g., walker, safety rails, shower chair) | 74% | 3.20 | Falls | Self |
| Self Regulation (n = 20 items) | ||||
| Physically attacks strangers | 100% | 3.89 | Aggressive, Violent | Self, Others |
| Easily provoked into physical fight | 100% | 3.78 | Aggressive, Violent | Self, Others |
| Makes unwelcome physical contact with others | 100% | 3.73 | Sexual | Self, Others |
| Keeps doing activities after being told to stop | 100% | 3.62 | Falls/Transportation | Self |
| Physically abuses family members or caregivers | 96% | 3.81 | Aggressive, Violent | Self, Others |
| Exchanges in sex for goods (e.g., money, drugs, cigarettes; pays for sex) | 96% | 3.69 | Sexual | Self, Others |
| Engages in unsafe sex (e.g., unprotected sex, one night stands, multiple partners) | 96% | 3.69 | Sexual | Self, Others |
| Shoves or pushes others | 93% | 3.48 | Aggressive, Violent | Self, Others |
| Physically abuses animals | 92% | 3.58 | Aggressive, Violent | Self, Animals |
| Wanders | 89% | 3.48 | Avoid Harmful Others | Self |
| Makes unwelcome sexual remarks | 89% | 3.33 | Sexual | Others |
| Throws, hits, or kicks objects in anger | 89% | 3.26 | Aggressive, Violent | Self, Others |
| Gambles excessively | 88% | 3.20 | Money, Possessions | Self, Property |
| Verbally abuses others | 85% | 3.52 | Aggressive, Violent | Others |
| Sends abusive or obscene messages (e.g. email, text, voicemail) | 85% | 3.31 | Aggressive, Violent | Self, Others |
| Tries to eat non-food items | 85% | 3.11 | Poisoning | Self |
| Cannot stop spending money | 84% | 3.12 | Money, Possessions | Self, Property |
| Verbally abuses family and friends | 81% | 3.36 | Aggressive, Violent | Self, Others |
| Takes other people’s things | 81% | 3.28 | Aggressive, Violent | Self, Others |
| Provokes animals | 74% | 2.93 | Avoid Harmful Others | Self, Animals |
| Motor Vehicle Operation (n = 19 items) | ||||
| Does not stop at red lights or stop signs | 100% | 3.89 | Transportation | Self, Others |
| Texts messages while driving | 100% | 3.89 | Transportation | Self, Others |
| Does not yield when required (e.g. for pedestrians, before merging onto road) | 100% | 3.85 | Transportation | Self, Others |
| Does not look out for pedestrians or bicyclists | 100% | 3.85 | Transportation | Self, Others |
| Changes lanes without looking | 100% | 3.78 | Transportation | Self, Others |
| Operates motor vehicle when on sedating medications | 100% | 3.78 | Transportation | Self, Others |
| Backs up without looking | 93% | 3.78 | Transportation | Self, Others |
| Easily distracted when driving | 93% | 3.77 | Transportation | Self, Others |
| Talks on cell phone while driving | 93% | 3.70 | Transportation | Self, Others |
| Operates motor vehicle when drowsy | 93% | 3.63 | Transportation | Self, Others |
| Misjudges turns (e.g. hits curbs, goes too wide) | 89% | 3.58 | Transportation | Self, Others |
| Reacts slowly to changing traffic (e.g., missing traffic signs, not braking soon enough) | 89% | 3.54 | Transportation | Self, Others |
| Drives too closely behind other vehicles | 89% | 3.52 | Transportation | Self, Others |
| Makes illegal turns | 87% | 3.63 | Transportation | Self, Others |
| Drives too fast (15 + MPH over limit) | 83% | 3.33 | Transportation | Self, Others |
| Gets lost when driving | 81% | 3.33 | Transportation | Self |
| * Drifts out of lane | NR | NR | Transportation | Self, Others |
| * Impulsively exits or makes turns (e.g. crosses multiple lanes, swerves at last minute) | NR | NR | Transportation | Self, Others |
| * Forgets where he or she is going | NR | NR | Transportation | Self |
| Child Caretaking (n = 9 items) | ||||
| Leaves children unattended (e.g., left alone in home, in bath, in park) | 100% | 4.00 | Multiple | Self, Others |
| Drives with child in the car after using alcohol or drugs | 100% | 3.96 | Transportation | Self, Others |
| Physically harmful to children | 100% | 3.93 | Aggressive, Violent | Self, Others |
| Does not buckle child in seatbelt, car seat, or booster seat | 100% | 3.85 | Transportation | Self, Others |
| Allows small child to ride in the front passenger seat | 96% | 3.65 | Transportation | Self, Others |
| Verbally harmful to children | 93% | 3.74 | Aggressive, Violent | Self, Others |
| * Leaves child in car while running errands | NR | NR | Poisoning | Self, Others |
| * Does not seek medical help when child is injured or ill | NR | NR | Medical Management | Self, Others |
| * Carries child despite physical limitations | NR | NR | Falls | Self, Others |
Each SAM item was rated for its relevance to preventing unintentional injury or harm as follows: 1 = not at all important; 2 = somewhat important; 3 = very important; 4 = critically important. I-CVI = Item Level-Content Validity Index (the percentage of stakeholders who rated an item as very or critically important; Mean = Average of Item Level Content Validity Ratings; ‘*’ = items added as a result of feedback from the health provider focus groups or family interviews. NR = not rated because they were newly generated from feedback during the focus group and consumer rating sessions
Overall, the SAM item pool covered the full range of activities, behaviors, and causes of injury in the general population and specific to persons with TBI (see Table 1, column 2.). Items related to transportation activities (24%), falls (14%), aggressive or violent behaviors (12%), and identifying, avoiding, or responding to potentially harmful others (9%) comprised 57% of the item pool content. For each of the 6 primary scales and 2 supplemental scales, item content reflected a wide range of activities, behaviors, and causes of injury (see Table 3, columns 4) as well as the people and property that could be potentially affected by harmful activities(see Table 3, columns5). The Cognitive Capacity and Compliance Failures with Safety Recommendations scales covered the largest number of activities/behaviors within their scale content with 10 each. The Risk Perception and Self-Regulation scales had 7 and 6 different activities or behaviors, respectively, covered in their item content. The Visuomotor Capacity, Wheelchair Use, and Motor Vehicle Operation scales had more focused content.
4. Discussion
4.1. Summary of study findings
Family, provider, and payer understanding of the specific activities in the home and community that pose threats and the cognitive, physical, and behavioral impairments that underlie risk is essential to managing the safety of persons who have sustained TBI. Our study presents a conceptual framework for understanding safety risk in the home and community following moderate to severe TBI. Person factors were identified as the key determinants of unsafe behavior and six primary constructs-Cognitive Capacity, Visuomotor Capacity, Wheelchair Use, Risk Perception, Compliance Failures with Safety Recommendations, and Self-Regulation-represented the most critical person factors that underlie safety risk. This conceptual framework and the operational definitions for the primary person constructs served as the basis for developing the SAM scales and item pool.
The SAM assesses risk on a large number of IADLs as well as the underlying abilities/impairments that underlie safe and unsafe performance of these activities. Our findings provide evidence that the SAM scales and item pool (n = 126 items) cover a wide range of real life experiences and everyday activities that place persons with TBI at risk for UIH. The SAM items cover 16 broad sets of activities, behaviors, and causes of UIH, most of which map to how the CDC monitors unintentional injury causes and activities in the general population. The SAM items also reflect the primary settings such as the home, roads, recreational centers, and the wider community in which harm occurs and the casualties of harm including persons with TBI, other people, animals, and property. The SAM items were generally viewed as being comprehensive, rated as having excellent content validity, and seen as being easily understandable based on feedback from rehabilitation providers participating in focus groups and family members who engaged in cognitive interviews.
4.2. Safety assessment measure methodological considerations and limitations
The structured qualitative methods that we used to develop the SAM scales and item pools are consistent with recommendations to develop “patient-centered” outcome measures that encompass patients’ needs, values and everyday experiences when assessing their health, function, and participation (Administration, 2009; Frank & Polkinghorne, 2010; Lasch et al., 2010; Ohman, 2005; Onwuegbuzie, Bustamante, & Nelson, 2010). Fifteen months was invested in developing a conceptual framework and item pool that reflects a wide range of activities that pose potential harm to the general population as well as persons who have sustained TBI. This time investment including feedback from clinical and family stakeholders was critical to achieving an item pool with high levels of content validity.
Our emphasis on using health provider feedback in developing SAM content reflected our decision to leverage a highly experienced group of clinicians who could reflect on and report their observations of thousands of persons who have sustained TBI in inpatient facilities, outpatient clinics, and in the home and community. We sought family member feedback when evaluating item clarity and understandability so that the SAM would be most usable to a wide range of family members making observations in the home and community. Based on our experience with developing item pools for individuals with disabilities, we used an interview format for the family caregivers, which allowed the instruction that family caregivers need to understand the review process and the individualized attention and time needed to provide comprehensive feedback. Field testing of the SAM with a large group of family raters, including 30-day follow-up interviews on unsafe events, will provide further opportunities to obtain detailed feedback on item content comprehensiveness and clarity.
Our decision to develop items that rate unsuccessful behaviors in the home and community reflects the nature of assessing risk behavior. We also received feedback from families that they found it easier to rate unsuccessful behavior when assessing levels of safety risk. A number of healthcare providers recommended increasing the specificity of causal assessment data as part of the SAM items, e.g., differentiating visual and physical components of losing balance in the Walking Mobility scale item content. Given the importance of obtaining reliable, family rated observations of behavior in the home and community, we decided that these distinctions would be difficult for family raters to make. While pre-injury abilities can play significant roles in safety risk (Pietrapiana et al., 2005), the SAM measures current ability and does not distinguish between pre-injury and injury-related abilities.
The SAM item pool addresses instrumental activities of daily living that may lead to unintentional injuries or harm in the home and community. The SAM does not assess unsafe activities in inpatient medical, school or work settings. The SAM item pool does not describe pre-meditated, intentional harmful acts to one’s self (e.g. self-mutilation, suicide), another person, or property, which are best assessed by existing psychiatric measures. The SAM also does not address the risk of persons with severe TBI being victims of violence by a parent, spouse, child, or other family caregiver in their home. This issue is not well-suited for family and caregiver self-report assessment. The SAM may not be applicable to persons who are dependent in most basic self-care activities and thus would not attempt more complex instrumental activities of daily living.
The SAM was developed for persons at least aged 16 and older who are likely to have been independent in many everyday activities prior to sustaining TBI. Young children, adolescents, or adults with significant pre-injury developmental disability would likely have different presentations, interests, and developmental expectations. A pediatric measure of safety would need to address the expectations and environments in which children participate (e.g., school), as well as consider developmental changes that reflect recovery, ongoing physical and cognitive development, and the acquisition of new versus previously learned functional skills.
4.3. Contributions of this study to the literature and future research
Our development of the SAM item pool is among the first efforts to use state-of-the-science methods to identify a broad range of specific activities and behaviors that are linked to risk of UIH and categorized by common TBI-related impairments. The SAM is unique compared to the few existing safety instruments in that it’s scales and item content are: (a) more highly connected to a theoretical framework for understanding safety risk following TBI; (b), more comprehensive and categorized by person functional ability rather than a limited number of activities; and (c) linked to how the U.S. CDC monitors activities and causes of unintentional injury. The comprehensiveness of the activities covered by the SAM scale items and their categorization by person functional ability will help clinicians and family members identify individual activities and their underlying causes that drive safety risk and prioritize those areas for treatment planning, intervention, progress monitoring, and prognosis.
The SAM is also unique compared to existing safety instruments in that our construct and scale development procedure included formally evaluating the item pool by using semi-structured focus groups with rehabilitation providers and cognitive interviewing of family members. This formal evaluation process with multiple stakeholders produced empirical, quantitative evidence that the content validity of the SAM item pool is generally perceived to be excellent, and increases the likelihood that the SAM scales and items can ultimately standardize observations and improve communication between families, clinicians and payers. Lastly, the SAM is unique in that it was developed using an item response theory framework that emphasized developing items within scales that were unidimensional and covered a range of low, medium and high activity difficulty. This will allow each SAM scale to be further evaluated using Rasch analysis.
4.4. Future research
The SAM scales and items will be field tested on a TBI development sample rated by family members and rehabilitation clinicians. Scale validation using IRT methods and Rasch analysis would evaluate the evidence of scale unidimensionality, person and item fit, and precision. Longitudinal tracking of persons with TBI unsafe behavior and events following a baseline SAM assessment would provide important data to evaluate the diagnostic and prognostic validity of the SAM scale scores. Evidence of diagnostic and prognostic validity would improve interpretation of SAM scale scores so that they could inform optimal levels of family involvement in person with TBI activities and the least restrictive environment in which persons who have sustained TBI can safely participate in activities. Health payers may find value in using SAM scale scores to identify high risk individuals who would benefit from community supports or home healthcare. The relationship between SAM scale scores and formal tests of cognitive and executive function in persons with TBI would also be of interest.
5. Conclusions
The Safety Assessment Measure scales and associated item pools assess a broad range of instrumental activities of daily living that can lead to unintentional injuries or harm in the home and community for adults who have sustained moderate or severe TBI. The Safety Assessment Measure scales assess risk related to diminished cognitive capacity, visuomotor capacity and/or wheelchair use, risk perception, compliance with safety recommendations, and selfregulation. Interdisciplinary rehabilitation clinicians rated most SAM items as having excellent content validity. Future research should use modern psychometric methods to examine scale unidimensionality, model fit, and precision.
Acknowledgments
We gratefully acknowledge the contributions of the clinical staff and advisory board members from the four centers/programs who participated in this study. In particular, we thank Leanne Dennis, CTRS, CCM, Greg Wright, MS, CRC, CCM, Tracey Wallace, MS, CCC-SLP, and Sary Newman, PT (Shepherd Pathways); Cindi Johnson, MA, CBIST (Side-by-Side Brain Injury Clubhouse); Virginia Martin,M.Ed., CCC-SLP, CCM (Shepherd Transition Care Program); Sara Kirkpatrick, PhD (Restore Neurobehavioral Center); and Matt Breiding at the Centers for Disease Control and Prevention.
Footnotes
Conflict of interest
We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated. We certify that all financial and material support for this research and work are clearly identified in the title page of the manuscript. The contents of this article were developed under a grant from the National Institute on Disability and Rehabilitation Research (grant no. H133G080153). However, these contents do not necessarily represent the official policy of the Department of Education or the Centers for Disease Control and Prevention. No endorsement by the Federal Government is implied.
References
- Administration, U.S. Food and Drug. (2009). Guidance for industry-patient-reported outcome measures: Use in medical product development to support labeling claims. [DOI] [PMC free article] [PubMed]
- Bandura A (1986). Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, N.J.: Prentice-Hall. [Google Scholar]
- Banja J (1994). Risk assessment and patient autonomy. Journal of Head Trauma Rehabilitation, 9(4), 70–72. [Google Scholar]
- Blais A, & Weber E (2006). A Domain-Specific Risk-Taking (DOSPERT) scale for adult populations. Judgment and Decision Making, 1, 33–47. [Google Scholar]
- Borgaro SR, & Prigatano GP (2003). Modification of the Patient Competency Rating Scale for use on an acute neuro rehabilitation unit: The PCRS-NR. Brain Injury, 17(10), 847–853. [DOI] [PubMed] [Google Scholar]
- Carlson KF, Meis LA, Jensen AC, Simon AB, Gravely AA, Taylor BC,… & Griffin JM (2012). Caregiver reports of subsequent injuries among veterans with traumatic brain injury after discharge from inpatient polytrauma rehabilitation programs. Journal of Head Trauma Rehabilitation, 27(1), 14–25. doi: 10.1097/HTR.0b013e318236bd86 [DOI] [PubMed] [Google Scholar]
- Cavallo MM, Kay T, & Ezrachi O (1992). Problems and changes after traumatic brain injury: Differing perceptions within and between families. Brain Injury, 6(4), 327–335. [DOI] [PubMed] [Google Scholar]
- Cella D, Yount S, Rothrock N, Gershon R, Cook K,Reeve B,… & Group, Promis Cooperative. (2007). The Patient-Reported Outcomes Measurement Information System (PROMIS): Progress of an NIH Roadmap cooperative group during its first two years. Medical Care, 45(5 Suppl 1), S3–S11. doi: 10.1097/01.mlr.0000258615.42478.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control, Prevention (1999). National Center for Injury Prevention and Control. ((n.d.)). Traumatic Brain Injury in the United States: A Report to Congress, 1999.
- Chiu T, & Oliver R (2006). Factor analysis and construct validity of the SAFER-HOME. Occupational Therapy Journal of Research: Occupation, Participation, and Health, 26(4), 132–142. [Google Scholar]
- Cooney LM Jr., Kennedy GJ, Hawkins KA, & Hurme SB (2004). Who can stay at home? Assessing the capacity to choose to live in the community. Archives of Internal Medicine, 164(4), 357–360. doi: 10.1001/archinte.164.4.357 [DOI] [PubMed] [Google Scholar]
- DeVellis R (2006). Scale development: Theory and applications(2nd ed.) Thousand Oaks, CA: Sage Publications. [Google Scholar]
- DeWalt DA, Rothrock N, Yount S, & Stone AA, Group, Promis Cooperative. (2007). Evaluation of item candidates: The PROMIS qualitative item review. Medical Care, 45(5 Suppl 1), S12–21. doi: 10.1097/01.mlr.0000254567.79743.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durgin CJ (2000). Increasing community participation after brain injury: Strategies for identifying and reducing the risks. Journal of Head Trauma Rehabilitation, 15(6), 1195–1207. [DOI] [PubMed] [Google Scholar]
- Frank G, & Polkinghorne D (2010). Qualitative research in occupational therapy: From the first to the second generation. Occupation, Participation, and Health, 30(2), 51–57. [Google Scholar]
- Galski T, Ehle HT, McDonald MA, & Mackevich J (2000).Evaluating fitness to drive after cerebral injury: Basic issues and recommendations for medical and legal communities. Journal of Head Trauma Rehabilitation, 15(3), 895–908. [DOI] [PubMed] [Google Scholar]
- Harrison-Felix C, Whiteneck G, Devivo MJ, Hammond FM, & Jha A (2006). Causes of death following 1 year postinjury among individuals with traumatic brain injury. Journal of Head Trauma Rehabilitation, 21(1), 22–33. [DOI] [PubMed] [Google Scholar]
- Hart T (2000). The Patient Competency Rating Scale: The Center for Outcome Measurement in Brain Injury. [Google Scholar]
- Hart T, Sherer M, Whyte J, Polansky M, & Novack TA (2004). Awareness of behavioral, cognitive, and physical deficits in acute traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 85(9), 1450–1456. [DOI] [PubMed] [Google Scholar]
- Hart T, Whyte J, Millis S, Bode R, Malec J, Richardson RN, & Hammond F (2006). Dimensions of Disordered Attention in Traumatic Brain Injury: Further Validation of the Moss Attention Rating Scale. Archives of Physical Medicine and Rehabilitation, 87, 647–655. [DOI] [PubMed] [Google Scholar]
- Kreutzer J, & Marwitz JH (2000). Judgment and Safety Screening Inventory (JASSI). Richmond, VA: VCU MCV PM&R Neuropsychology Service. [Google Scholar]
- Kreutzer JS, Livingston LA, Everley RS, Gary KW,Arango-Lasprilla JC, Powell VD, & Marwitz JH (2009). Caregivers’ concerns about judgment and safety of patients with brain injury: A preliminary investigation. PM & R, 1(8), 723–728. doi: 10.1016/j.pmrj.2009.07.005 [DOI] [PubMed] [Google Scholar]
- Kreutzer J, Seel R, & Marwitz JH (1999). The Neurobehavioral Functioning Inventory (NFI) Manual. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Lasch KE, Marquis P, Vigneux M, Abetz L, Arnould B, Bayliss M,… & Rosa K (2010). PRO development: Rigorous qualitative research as the crucial foundation. Quality of Life Research, 19(8), 1087–1096. doi: 10.1007/s11136-010-9677-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macciocchi SN (2009). Doing good: The pitfalls of beneficence. Journal of Head Trauma Rehabilitation, 24(1), 72–74. doi: 10.1097/HTR.0b013e31819a9088 [DOI] [PubMed] [Google Scholar]
- Macciocchi SN, & Stringer AY (2001). Assessing risk and harm: The convergence of ethical and empirical considerations. Archives of Physical Medicine and Rehabilitation, 82(12 Suppl2), S15–S19. [PubMed] [Google Scholar]
- Magasi S, Ryan G, Revicki D, Lenderking W, Hays RD, Brod M,… & Cella D (2012). Content validity of patient reported outcome measures: Perspectives from a PROMIS meeting. Quality of Life Research, 21(5), 739–746. doi: 10.1007/s11136-011-9990-8. [DOI] [PubMed] [Google Scholar]
- Malec JF (2004). The Mayo-Portland Participation Index: A brief and psychometrically sound measure of brain injury outcome. Archives of Physical Medicine and Rehabilitation, 85(12), 1989–1996. [DOI] [PubMed] [Google Scholar]
- McMillan TM, & Teasdale GM (2007). Death rate is increased for at least 7 years after head injury: A prospective study. Brain, 130(Pt 10), 2520–2527. doi: 10.1093/brain/awm185 [DOI] [PubMed] [Google Scholar]
- Morrongiello BA, & Corbett M (2006). The Parent Supervision Attributes Profile Questionnaire: A measure of supervision relevant to children’s risk of unintentional injury. Injury Prevention, 12(1), 19–23. doi: 10.1136/ip.2005.008862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohman A (2005). Qualitative methodology for rehabilitation research. Journal of Rehabilitation Medicine, 37(5), 273–280. [DOI] [PubMed] [Google Scholar]
- Oliver R, Blathwayt J, Brackley C, & Tamaki T (1993).Development of the Safety Assessment of Function and the Environment for Rehabilitation (SAFER) tool. Canadian Journal of Occupational Therapy. Revue Canadienne d Ergotherapie, 60(2), 78–82. [DOI] [PubMed] [Google Scholar]
- Onwuegbuzie A, Bustamante RM, & Nelson JA (2010). Mixed research as a tool for developing quantitative instruments. Journal of Mixed Methods Research, 4(1), 56–77. [Google Scholar]
- Pai AB, Zadov Y, & Hickman A (2012). Patient safety in rehabilitation medicine: Traumatic brain injury. Physical Medicine and Rehabilitation Clinics of North America, 23(2), 349–370. doi: 10.1016/j.pmr.2012.02.009 [DOI] [PubMed] [Google Scholar]
- Patton JH, Stanford MS, & Barratt ES (1995). Factor structure of the Barratt Impulsiveness Scale. Journal of Clinical Psychology, 51(6), 768–774. [DOI] [PubMed] [Google Scholar]
- Pietrapiana P, Tamietto M, Torrini G, Mezzanato T, Rago R, & Perino C (2005). Role of premorbid factors in predicting safe return to driving after severe TBI. Brain Injury, 19(3), 197–211. [DOI] [PubMed] [Google Scholar]
- Polit DF, & Beck CT (2006). The content validity index: Are you sure you know what’s being reported? Critique and recommendations. Research in Nursing and Health, 29(5), 489–497. doi: 10.1002/nur.20147 [DOI] [PubMed] [Google Scholar]
- Reeve BB, & Fayers P (2005). Applying item response theory modeling for evaluating questionnaire item and scale properties In Fayers P & Hays R (Eds.), Assessing quality of life in clinical trials: Methods and practice (2nd ed., pp. 55–73). Oxford, NY: Oxford University Press. [Google Scholar]
- Reichard AA, Langlois JA, Sample PL, Wald MM, & Pickelsimer EE (2007). Violence, abuse, and neglect among people with traumatic brain injuries. Journal of Head Trauma Rehabilitation, 22(6), 390–402. doi: 10.1097/01.HTR.0000300234.36361.b1 [DOI] [PubMed] [Google Scholar]
- Riley GA, Brennan AJ, & Powell T (2004). Threat appraisal and avoidance after traumatic brain injury: Why and how often are activities avoided? Brain Injury, 18(9), 871–888. doi: 10.1080/02699050410001671829 [DOI] [PubMed] [Google Scholar]
- Ruchinskas R, Macchiocchi S, Howe G, & Newton R (2001).Clinical decision making in the prediction of falls. Rehabilitation Psychology, 46(3), 262–270. [Google Scholar]
- Seel RT, Kreutzer JS, & Sander AM (1997). Concordance of patients’ and family members’ ratings of neurobehavioral functioning after traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 78(11), 1254–1259. [DOI] [PubMed] [Google Scholar]
- Seel RT, Macciocchi S, & Kreutzer JS (2010). Clinical considerations for the diagnosis of major depression after moderate to severe TBI. Journal of Head Trauma Rehabilitation, 25(2), 99–112. doi: 10.1097/HTR.0b013e3181ce3966 [DOI] [PubMed] [Google Scholar]
- Seel RT, Wright G, Wallace T, Newman S, & Dennis L (2007). The utility of the FIM+FAM for assessing traumatic brain injury day program outcomes. Journal of Head Trauma Rehabilitation, 22(5), 267–277. doi: 10.1097/01.HTR.0000290971.56130.c8 [DOI] [PubMed] [Google Scholar]
- Selassie AW, McCarthy ML, Ferguson PL, Tian J, & Langlois JA (2005). Risk of posthospitalization mortality among persons with traumatic brain injury, South Carolina 1999–2001. Journal of Head Trauma Rehabilitation, 20(3), 257–269. [DOI] [PubMed] [Google Scholar]
- Selassie AW, Zaloshnja E, Langlois JA, Miller T, Jones P, & Steiner C (2008). Incidence of long-term disability following traumatic brain injury hospitalization, United States, 2003. Journal of Head Trauma Rehabilitation, 23(2), 123–131. doi: 10.1097/01.HTR.0000314531.30401.39 [DOI] [PubMed] [Google Scholar]
- Sherer M, Boake C, Silver B, Levin E, Ringholz G, Wilder M, & Oden K (1995). Assessing awarness of deficits following acquired brain injury: The Awareness Questionnaire. Journal of the International Neuropsychological Society, 1, 163. [Google Scholar]
- Simons-Morton B, & Nansel T (2006). The application of social cognitive theory to injury prevention In Gielen AC. Sleet DA, DiClemente R (Ed.), Injury and Violence Prevention: Behavior Change Theories, Methods and Applications. San Francisco, CA: Jossey-Bass. [Google Scholar]
- Sleet D, & Gielen A (2007). Developing injury interventions: The role of behavioral science In Doll L, Bonzo S, Mercy J, & Sleet D (Eds.) Handbook of Injury and Violence Prevention. New York: Springer. [Google Scholar]
- Sleet D, & Trifiletti LB, Simons-Morton B, Gielen AC (2006). Individual-level models for behavior change in injury prevention In Gielen AC. Sleet D & DiClemente R (Eds.), Injury and Violence Prevention: Behavior Change Theories, Methods and Applications. San Francisco, CA: Jossey-Bass. [Google Scholar]
- Stone MH (1997). Steps in item construction. Rasch measurement transactions, 11, 559. [Google Scholar]
- Tyson BT, Pham MT, Brown NT, & Mayer TR (2012). Patient safety considerations in the rehabilitation of the individual with cognitive impairment. Physical Medicine and Rehabilitation Clinics of North America, 23(2), 315–334. doi: 10.1016/j.pmr.2012.02.007 [DOI] [PubMed] [Google Scholar]
- Velozo CA, & Peterson EW (2001). Developing meaningful fear of falling measures for community dwelling elderly. American Journal of Physical Medicine and Rehabilitation, 80(9), 662–673. [DOI] [PubMed] [Google Scholar]
- Velozo CA, Seel RT, Magasi S, Heinemann AW, & Romero S (2012). Improving measurement methods in rehabilitation: Core concepts and recommendations for scale development. Archives of Physical Medicine and Rehabilitation, 93(8 Suppl), S154–163. doi: 10.1016/j.apmr.2012.06.001 [DOI] [PubMed] [Google Scholar]
- Ventura T, Harrison-Felix C, Carlson N, Diguiseppi C, Gabella B, Brown A,… & Whiteneck G (2010). Mortality after discharge from acute care hospitalization with traumatic brain injury: A population-based study. Archives of Physical Medicine and Rehabilitation, 91(1), 20–29. doi: 10.1016/j.apmr.2009.08.151, [DOI] [PubMed] [Google Scholar]
- Whyte J, Hart T, Bode RK, & Malec JF (2003). The Moss Attention Rating Scale for traumatic brain injury: Initial psychometric assessment. Archives of Physical Medicine and Rehabilitation, 84(2), 268–276. doi: 10.1053/apmr.2003.50108 [DOI] [PubMed] [Google Scholar]
- Willis GB (2005). Cognitive interviewing: A tool for improving questionnaire design. Thousand Oaks, California: Sage Publications. [Google Scholar]
- Yudofsky SC, Silver JM, Jackson W, Endicott J, & Williams D (1986). The Overt Aggression Scale for the objective rating of verbal and physical aggression. American Journal of Psychiatry, 143(1), 35–39. [DOI] [PubMed] [Google Scholar]