Abstract
We aimed to investigate whether combined reverse total shoulder arthroplasty (RTSA) and subscapularis repair leads to improved clinical and functional outcome in comparison with RTSA alone. Two reviewers independently conducted a systematic search according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) using the MEDLINE/PubMed database and the Cochrane Database of Systematic Reviews. These databases were queried with the terms “reverse” AND “shoulder” AND “arthroplasty” AND “with” AND “subscapularis” AND “repair”. From the 72 initial studies, we finally chose five studies which were eligible to our inclusion-exclusion criteria. The total mean modified Coleman methodology test was 55/100 (range: 47/100 to 60/100). The eligible studies included 1087 patients, in total. Regarding the subjective functional scores as well as range of motion (ROM), the differences amongst groups were insignificant in almost all studies. The mean complications’ rate of the repair group was 10.4%, whereas the respective rate of the nonrepair group was 10.2%. All studies concluded that the repair of subscapularis did not affect the complications’ rate of patients who were treated with RTSA. The mean dislocations’ rates of the repair and the nonrepair group were 1.5% and 2.3%, respectively. Although subscapularis repair was proven safe and effective for the augmentation of RTSA, it did not offer any additional clinical or functional benefit in the outcome of patients treated with lateralized RTSA. Therefore, it is not supported its routine use for patients who have a preoperatively sufficient subscapularis tendon.
Key words: reverse total shoulder arthroplasty, systematic review of comparative trials, subscapularis repair, rotator cuff arthropathy
Introduction
In 1987, Grammont et al. introduced the reverse total shoulder arthroplasty (RTSA) to treat rotator cuff tear arthropathy.1 Since then, the indications for performing RTSA has been increasing.2 RTSA is a valuable surgical option for the treatment of cuff tear arthropathy and shoulder pseudoparalysis resulting from a massive cuff tear, severe fractures, prosthetic revision, and tumor surgery.3 RTSA increases the efficiency of the deltoid as a forward elevator and abductor by increasing its tension and lever arm with a distalized and medialized center of rotation coupled with a semi-constrained articulation.4 Furthermore, the humerus is lowered relative to the acromion, restoring and even increasing deltoid tension.5
Repair of subscapularis tendon is of vital importance in total shoulder arthroplasty; however, its utilization in RTSA has recently been questioned.6 Leaving the subscapularis tendon intact after RTSA has garnered much attention as a potential risk factor for complications, particularly dislocation, especially with the deltopectoral approach.7 Some authors advocate subscapularis tenotomy and reattachment,8,9 where others could not find any correlation between reattachment and range of motion (RoM), pain scores and stability.10-12
A biomechanical study conducted by Hansen et al. supported that not repairing the subscapularis requires significantly less force to be generated by the deltoid and the posterior rotator cuff throughout arm abduction.13 Giles et al. confirmed these findings in another cadaver study, while they hypothesized that rotator cuff repair, especially in conjunction with glenosphere lateralization, produced an antagonistic effect that increased deltoid and joint loading, which is the force placed across the RTSA articulation.14 On the contrary, Chalmers et al reported increased risk of dislocation in males with subscapularis deficiency after RTSA,15 while Edwards et al. found that all postoperative dislocations were seen in the patients with irreparable subscapularis at the time of RTSA surgery.8
Recently, a number of clinical studies compared the outcome of combined RTSA and subscapularis repair with that of RTSA alone,16-18 while no relative review of the literature has been conducted yet.
Our aim was to investigate whether a combined RTSA and subscapularis repair will lead to improved clinical and functional outcomes in comparison with RTSA without subscapularis repair. We hypothesized that subscapularis repair will not provide with any additional clinical or functional benefit patients who are treated with RTSA.
Materials and Methods
Two reviewers (MM, DG) independently conducted a systematic search according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) using the MEDLINE/PubMed database and the Cochrane Database of Systematic Reviews.19 These databases were queried with the terms “reverse” AND “shoulder” AND “arthroplasty” AND “with” AND “subscapularis” AND “repair”. To maximize the search, backward chaining of reference lists from retrieved papers was also undertaken. A preliminary assessment of only the titles and abstracts of the search results was initially performed. The second stage involved a careful review of the fulltext publications.
Inclusion criteria were clinical studies investigating the clinical and functional outcomes of subscapularis repair for patients treated with RTSA. The clinical trials included should have contained at least a 6- month follow-up evaluation, with at least one clinical and/or functional subjective score reported, while all of the studiesincluded must have been written in English as full-text manuscript. Furthermore, they should have been published until March 25, 2018 (end of our search).
Exclusion criteria were studies not specifically focusing on the therapeutic value of subscapularis repair in patients treated with RTSA, non-comparative trials, studies dealing with preoperative subscapularis insufficiency, preclinical, cadaveric or animal studies, abstracts, literature reviews, case reports, technical notes, editorial comments, expert opinions, studies with less than 6 months follow-up, studies without any clinical outcomes, and articles not written in English.
Differences between reviewers were discussed until agreement was achieved. In case of disagreement, the senior author of this review (EA) was responsible for the final decision. They independently extracted data from each study and assessed variable reporting of outcome data. Descriptive statistics were calculated for each study and parameters analyzed. The methodological quality of each study and the different types of detected bias were assessed independently by each reviewer with the use of modified Coleman methodology score. Selective reporting bias like publication bias were not included in the assessment. The primary outcome measure was the postoperative statistically significant improvement of the clinical, functional and radiographic scores in comparison with the preoperative scores per study. Secondary outcome was the complications’ and reoperation’s rate per study.
Results
From the 72 initial studies we finally chose and assessed five clinical studies which were eligible to our inclusion-exclusion criteria.6,7,16-18 A summary flowchart of our literature search according to PRISMA guidelines can be found in Figure 1.
All eligible studies (100%) were retrospective case-control studies level III.6,7,16-18 As a result, none from these studies (0%) was randomized or blinded. These articles were published between 2012 and 2018 (Table 1).
Demographics
The follow-up evaluation ranged between six and 91 months, while the overall mean follow-up was 29.2 months. Three studies (60%) had a minimum follow-up of 24 months,6,17,18 whereas one study (20%) had a 12-month follow-up and another one (20%) six months (Table 2).7,16 The eligible studies included 1087 patients in total. Demographic data were available in all five (100%) studies regarding age6,7,16-18 and in four studies (80%) as for sex.6,7,16-18 The majority of the patients included in this review were relatively old, with a mean age of 71.4 years. There was not any statistically significant difference in age between the subscapularis repair and non-repair groups at any of the studies. Females outweighed males in four out of the five studies (80%) in which data were available (532 females: 353 males) (Table 2).7,16-18
Figure 1.
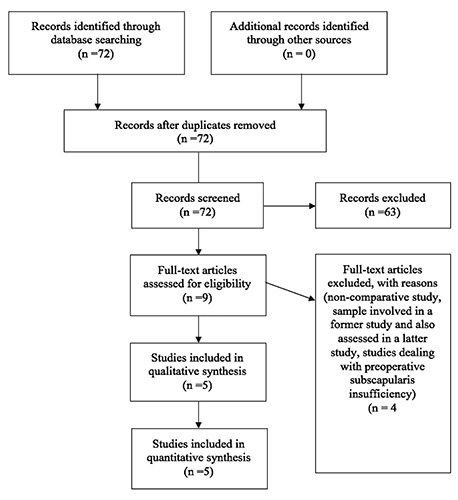
PRISMA flow chart.
Table 1.
Year of publication, type of study and level of evidence.
| Authors [ref] | Year | Type of study | Level |
|---|---|---|---|
| De Boer et al. 16 | 2016 | Retrospective case control | III |
| Clark et al.7 | 2012 | Retrospective case control | III |
| Werner et al.17 | 2018 | Retrospective case control | III |
| Vourazeris et al.6 | 2016 | Retrospective case control | III |
| Friedman et al.18 | 2016 | Retrospective case control | III |
Indication for surgery
The main indication for RTSA varied widely amongst studies, while the most common reasons for surgery were rotator cuff arthropathy, osteoarthritis with irreparable rotator cuff tear, and inflammatory arthritis. Four studies (80%) noted that patients who underwent RTSA due to humeral head fracture were excluded from their statistical analysis.6,16-18
The decision to repair the subscapularis tendon or not was intra-operatively taken in all five studies (100%) of this review.6,7,16-18 It was based on the surgeon’s preference and subscapularis tendon’s macroscopic condition.
RoM and functional outcome
Clinical and functional subjective scores were utilized in all studies of this review (100%).6,7,16-18 The Constant-Murlay Shoulder Score,6,16,18 and the American Shoulder and Elbow Score (ASES)6,17,18 were the most commonly used subjective outcome variables. They were both used in three (60%) studies. The Shoulder Pain and Disability Index (SPADI), University of California at Los Angeles (UCLA) Score and the Simple Shoulder Test (SST) were reported in the same two (40%) articles.6,18 Finally, the Visual Analogue Scale (VAS)7 and the Oxford Shoulder Score (OSS)16 were deployed in one (20%) study. The Range of Motion (RoM) was measured in four out of the five studies (80%) of this review,6,7,16-18 whereas muscle strength was documented in two trials (40%) (Table 3).6,16
Significant postoperative improvement in comparison with the preoperative values
Two studies of this review (40%) compared the mean preoperative and postoperative scores.7,18 Regardless of the use of subscapularis repair or not, both studies depicted that there was a significant improvement of all clinical and functional outcome variables at the last follow-up (Table 3).7,18
Comparison between the subscapularis repair group and the non-repair group
Regarding the subjective clinical/functional scores as well as RoM of four out of the five studies of this review (80%), the differences between the two groups were found insignificant.6,7,16,17 On the other hand, one study (20%) reported that the subscapularis repair group illustrated significantly higher improvement of Constant score, SST and active internal and external rotation, when compared with the nonrepair group.18 The subscapularis non-repair group had significantly higher active abduction and passive external rotation in comparison with the repair group (Tables 3 and 4).18
Table 2.
Number of patients, sex, mean age and mean follow-up per study.
| Authors [ref] | No. patients | Sex | Mean age | Mean follow up (months) |
|---|---|---|---|---|
| De Boer et al.16 | Total: 65 Repair-Group: 25 No Repair-Group: 40 | Repair-Group: 6M,19 F No Repair-Group: 10M,30F | Total: 73,8 Repair-Group: 73 No Repair-Group: 74,4 | Total: 36 Repair-Group: 30,5 No Repair-Group: 40 |
| Clark et al.7 | Total: 120 Repair-Group: 65 No Repair-Group: 55 | Repair-Group: 19M,46F No Repair-Group: 12M,43F | Repair-Group: 68,6 No Repair-Group: 68,3 | Repair-Group: 13,2 No Repair-Group: 9,9 |
| Werner et al.17 | Total: 109 Repair-Group: 71 No Repair-Group: 38 | Repair-Group: 28M,43F No Repair-Group: 15M,23F | Repair-Group: 71,1 No Repair-Group:70,7 | 24 minimum |
| Vourazeris et al.6 | Total: 202 Repair-Group: 86 No Repair-Group: 116 | N/A | Repair-Group: 71,6 No Repair-Group: 71,1 | 24 minimum Repair-Group: 40 No Repair-Group: 37 |
| Friedman et al.18 | Total: 591 Repair-Group: 340 No Repair-Group: 251 | Repair-Group: 119M,221F No Repair-Group: 105M,146F | Total: 72,5 (50-93) Repair-Group: 72,7 No Repair-Group: 71,7 | Total: 36,6 (24 minimum) Repair-Group: 37,3 No Repair-Group: 35,7 |
Table 3.
Scales measuring the clinical outcome, significant differences between the two groups and significant improvement from preto postoperative scores.
| Authors [ref] | Clinical Outcome Scale | Significant difference between repair and no repair | Significant difference from pre- to post-operative |
|---|---|---|---|
| De Boer et al.16 | Constant, Oxford, RoM, Strength | No (for all scores) | N/A |
| Clark et al.7 | VAS, ROM | No | YES in both groups (all score) |
| Werner et al.17 | ASES | No Less improvement in ASES when repair and lateralization combined | N/A |
| Vourazeris et al.6 | SPADI, ASES, UCLA, Constant, SST, RoM, Strength | No | N/A |
| Friedman et al.18 | ASES, Constant, UCLA, SST, SPADI, RoM | The non-repair group had more active abduction and passive external rotation. The repair group had higher internal rotation and greater improvement in SST, Constant and active external rotation | YES in both Groups (all Scores) |
Mean values of RoM and functional outcome variables
Overall, the mean values of the postoperative Constant score of the repair group and the non-repair group were 72.7 and 70.5, respectively, while the mean postoperative ASES was 79.3 and 78.7, respectively, the mean SST was 9.8 and 9.4, respectively, and the mean UCLA was 29.2 and 29.3, respectively.
Table 4.
Preoperative and postoperative clinical and functional mean scores per study and other variables.
| Authors [ref] | Preoperative Mean Scores | Postoperatives Mean Scores | Other Variables |
|---|---|---|---|
| De Boer et al16 | N/A | N/A | On U/S post-operative exam (mean 30 months) 10(40%) of the repaired tendons were still sufficient |
| Clark et al.7 | VAS Repair-Group: 7,5 | VAS Repair-Group: 1,4 | N/A |
| VAS No Repair-Group: 8,2 | VAS No Repair-Group: 2,5 | ||
| Active FF in No Repair-Group 20 | FF Repair-Group: 112 | ||
| degrees less than Repair-Group | FF No Repair-Group: 94 | ||
| Werner et al.17 | ASES Repair-Group: 37,9 | ASES Improvement Repair-Group: 35,8 | Subscapularis repair and lateralized glenosphere in isolation had no effect on ASES, but in combination ASES was significantly less improved |
| ASES No Repair-Group: 36,6 | ASES Improvement No Repair-Group: 38 | ||
| Vourazeris et al.6 | N/A | SPADI Repair-Group: 23,4 | N/A |
| SPADI No Repair-Group: 23,2 | |||
| ASES Repair-Group: 77,7 | |||
| ASES No Repair-Group: 79,3 | |||
| UCLA Repair-Group: 28,3 | |||
| UCLA No Repair-Group: 28,8 | |||
| SST Repair-Group: 9,2 | |||
| SST No Repair-Group: 9,1 | |||
| Constant Repair-Group:72,6 | |||
| Constant No Repair-Group: 72,9 | |||
| FF Repair-Group: 120 | |||
| FF No Repair-Group: 122 | |||
| External Rotation Repair-Group: 24 | |||
| External Rotation No Repair-Group: 26 | |||
| ABD Repair-Group: 109 | |||
| ABD No Repair-Group:112 | |||
| ER Strength Repair-Group: 9,9lb | |||
| ER Strength No Repair-Group: 9,9 lb | |||
| Friedman et al.18 | SPADI Repair-Group: 80,2 | SPADI Repair-Group: 15,9 | N/A |
| SPADI No Repair-Group: 84,6 | SPADI No Repair-Group: 23,5 | ||
| ASES Repair-Group: 38,8 | ASES Repair-Group: 86,7 | ||
| ASES No Repair-Group: 34,9 | ASES No Repair-Group: 82,1 | ||
| UCLA Repair-Group: 13,7 | UCLA Repair-Group: 30,2 | ||
| UCLA No Repair-Group: 12,7 | UCLA No Repair-Group: 29,7 | ||
| SST Repair-Group: 3,4 | SST Repair-Group: 10,5 | ||
| SST No Repair-Group: 3,3 | SST No Repair-Group: 9,6 | ||
| Constant Repair-Group:34,8 | Constant Repair-Group:72,9 | ||
| Constant No Repair-Group:33,8 | Constant No Repair-Group:67,9 | ||
| Active ff Repair-Group: 91 | Active ff Repair-Group: 141 | ||
| Active ff No Repair-Group: 85 | Active ff No Repair-Group: 137 | ||
| Active ABD Repair-Group: 67 | Active ABD Repair-Group: 107 | ||
| Active ABD No Repair-Group: 75 | Active ABD No Repair-Group: 119 | ||
| IR Score Repair-Group: 3,3 | IR Score Repair-Group: 5,1 | ||
| IR Score No Repair-Group: 3.2 | IR Score No Repair-Group: 4,4 | ||
| Active ER Repair-Group: 13 | Active ER Repair-Group: 34 | ||
| Active ER No Repair-Group: 20 | Active ER No Repair-Group: 35 | ||
| Passive ER Repair-Group: 23 | Passive ER Repair-Group: 45 | ||
| Passive ER No Repair-Group: 31 | Passive ER No Repair-Group: 50 | ||
| Strength Repair-Group:0,6kg | Strength Repair-Group: 3,9kg | ||
| Strength No Repair-Group:0,5 kg | Strength No Repair-Group: 2,9 kg |
N/A: not applicable, VAS: Visual Analogue Scale, SPADI: Shoulder Pain and Disability Index, ASES, American Shoulder and Elbow Score, UCLA Score: University of California at Los Angeles Score, SST: Simple Shoulder Test, ABD: abduction, ADD: adduction, FF: forward flexion, ER: external rotation, IR: internal rotation, U/S: ultrasound.
The mean postoperative forward flexion in our review was 124° as for the repair group and 118° concerning the non-repair group, while the mean postoperative active abduction was 108° and 116°, respectively, and the mean active external rotation was 29° and 31°, respectively. Three out of the four studies where RoM was reported were found without any significant differences amongst groups (Table 4).6,7,16
Postoperative internal rotation with or without subscapularis repair
Three studies (60%) investigated the difference in internal rotation between the two groups.6,16,18 Postoperative internal rotation, as it was documented in the study of Friedman et al., illustrated significantly higher improvement in the repair group.18 On the other hand, Vourazeris et al. found similar postoperative internal rotation amongst groups (L2 level),6 while there were not any significant differences in the study which was conducted by De Boer et al.16
Postoperative external rotation with or without subscapularis repair
Three studies (40%) investigated the difference in external rotation between the two groups.6,16,18 Vourazeris et al. depicted that there were not any significant differences amongst groups as for the both the passive and the active postoperative external rotation.6 In addition, De Boer et al. documented no significant differences amongst groups.16 On the contrary, Friedman et al. reported a significantly superior passive external rotation of the non-repair group in comparison with the repair group.18 However, the same study illustrated that the active postoperative external rotation was similar in both groups.18
The role of lateralized glenosphere in relation to subscapularis repair
Only one study investigated the effect of the lateralized glenosphere in relation to subscapularis repair after RTSA.16 Werner et al. divided the subscapularis repair and non-repair groups into two subgroups depending on the use of a lateralized glenosphere or not.17 According to them, there was not any significant difference in mean postoperative ASES score of the two groups (repair and non-repair group) when a standard glenosphere was used.17 On the contrary, when subscapularis repair was combined with a lateralized glenosphere, the mean postoperative ASES score was significantly lower in comparison with all other three subgroups (subscapularis repair without lateralized sphere, non-repair with lateralized sphere, non-repair without lateralized sphere).17
Postoperative integrity of subscapularis repair
The integrity of subscapularis repair was checked only in one study (20%). De Boer et al examined the integrity of subscapularis repair using ultrasonography (U/S) at a mean follow-up point of 30 months.16 They reported that the repair was still sufficient in 40% of the treated patients.16 No significant difference between the subscapularis repair and nonrepair groups was found in relation to the mean postoperative subjective clinical/functional scores and RoM as well as the subgroup of the patients where the subscapularis repair was intact (40% of their patients) (Tables 4 and 5).16
Table 5.
Complications, potential risk of bias, and modified Coleman methodology score per study.
| Authors [ref] | Complications | Type of Bias | Coleman Score (0-100/100) |
|---|---|---|---|
| De Boer et al.16 | N/A | Selection, Performance, Detection, Attrition | 57 |
| Clark et al. 7 | No significant difference between Groups. | Selection, Performance, Detection, Attrition | 53 |
| Repair-Group: Overall: 13(20%) out of 65; Dislocation: 2; | |||
| Infection: 5; Fracture: 2. | |||
| No Repair-Group: Overall: 11(20%) out of 55; | |||
| Dislocation: 3; Infection: 3; Fracture: 3 | |||
| Werner et al.17 | No significant difference between Groups. | Selection, Performance, Detection, Attrition | 47 |
| Repair-Group: Dislocation: 2(2.8%); | |||
| Scapular Notching: 6 (8.5%) | |||
| No Repair-Group: Dislocation: 0; | |||
| Scapular Notching: 3 (7.9%) | |||
| Vourazeris et al.6 | No significant difference between Groups. | Selection, Performance, Detection, Attrition | 60 |
| Repair-Group: Overall: 4.7%; Dislocation: 0; Infection: 1; | |||
| Base plate failure: 2; Humerus loosening: 1 | |||
| No Repair-Group: Overall: 6%; | |||
| Dislocation: 3 (2.6%); Infection: 1; Fracture: 3 | |||
| Friedman et al.18 | No significant difference between Groups. | Selection, Performance, Detection, Attrition | 58 |
| Repair-Group: Overall: 7.4%; | |||
| Dislocation: 0; Scapular Notching: 10.4%. | |||
| No Repair-Group: Overall: 6,8%; | |||
| Dislocation: 3 (1.2%); Scapular Notching: 10.7% |
ASES: American Shoulder and Elbow Score, ROM: range of motion, RTSA: reverse total shoulder arthroplasty, N/A: not applicable, U/S: ultrasound.
Complications’ rate
Data regarding complications were collected in 80% of the studies included in this review. All these studies concluded that the repair of subscapularis tendon did not affect the complications’ rate of patients treated with RTSA.6,7,16-18 As for the repair group, the mean complications’ rate was found 10.4%, whereas the respective rate of the non-repair group was 10.2% (Table 5).
The mean dislocations’ rate of the repair group and the non-repair group were 1.5% and 2.3%, respectively. Vourazeris et al. and Friedman et al. reported no cases of dislocation when subscapularis was repaired,6,18 while Werner et al.17 documented two dislocations in the repair group and no dislocations in the non-repair group (Table 5).
Quality of studies, possible risk of bias, and relative conflicts of interest
The “quality assessment” of the studies for methodological deficiencies, as a common alternative to “risk of bias” was examined by the modified Coleman methodology Score.20,21 The total mean modified Coleman methodology test was 55/100, whereas the modified Coleman methodology score ranged amongst studies between 47/100 and 60/100 (Table 5).
All studies (100%) which were included in this review were found with a high risk of possible selection, performance, detection and attrition bias (Table 5).6,7,16-18
Discussion
To the best of our knowledge, this was the first systematic review to investigate the necessity (or not) of subscapularis repair for patients treated with RTSA. The most important finding of this review was that subscapularis tenotomy and repair was not proven superior than leaving the subscapularis tendon intact in patients who were treated with RTSA. All studies of this review concluded that the mean postoperative clinical and functional scores as well as the complications’ rates did not illustrate any significant differences between the subscapularis repair and the non-repair groups. While both groups showed significant improvement in all mean final postoperative clinical and functional scores as well as RoM in comparison to the mean preoperative values, it seemed that subscapularis tenotomy and repair did not offer any additional clinical or functional benefit. Therefore, we do not further support its use on routine basis for patients treated with RTSA.
Another interest finding was that the mean dislocations’ rate was not differed between the two groups in any of the studies which were included in this review. This variable is of paramount importance for patients treated with RTSA and subscapularis repair, since it has been suggested that repairing the subscapularis will decrease the rate of postoperative dislocations.8,22 Nevertheless, this theory was not confirmed by our results. Therefore, we support that subscapularis tenotomy and repair of a preoperatively sufficient tendon does not decrease the dislocations’ rate after RTSA.
A relative point of controversy has been the differences in rotational movements. It would be expected that subscapularis repair would result in improved internal rotation and in a possible external rotation deficit.23-25 However, only one study supported that the internal rotation was improved after subscapularis tenotomy and repair.18 This study was also the only one to show that the passive external rotation was superior in the non-repair group.18 Although these differences in external and internal rotation were found significant, Friedman et al concluded that they were so small that they were not of any clinical relevance.18 On the other hand, two other studies depicted that there were no differences in both internal and external rotations amongst groups.6,16 As a result, it was deduced from this review that subscapularis repair did not change internal or external rotation after RTSA in a clinically significant level. However, the limited available data were not enough to lead to definitive conclusions, while further studies are required to investigate the effect of subscapularis tenotomy and repair in relation to the postoperative internal and external rotation of these patients.
Regarding the complications’ rate, no differences were found amongst groups. Particularly, there was not any significant difference in relation to the most commonly reported types of complications after RTSA, like nerve injuries, postoperative hematomas, periprosthetic infections, intraoperative fractures, scapular notching and acromial/scapular spine fractures.26
Although there is no consensus, subscapularis repair has been suggested to improve the stability of RTSA in patients who are being treated with the traditional medialized prosthesis.27-32 However, for those patients who are preoperatively found with extension lag sign and significant external rotation deficit, a lateralized prosthesis -with or without latissimus dorsi transfer- would be more appropriate than a medialized implant.33-40 In regard to our analysis, it was interesting that all studies included dealt with a new generation’s lateralized prosthesis. Therefore, it should be notified that the reported insignificant differences in the outcomes of the two groups were particularly correlated with the lateralized type, so that they cannot be generalized to other types of RTSA, such as those using medial glenosphere-medial humeral implants (Grammont-Style).6
Regarding postoperative integrity of subscapularis repair, the only study which investigated this variable showed that only 40% of the patients had an intact repair.16 Furthermore, there were not any differences between the outcomes of patients (60%) who had an ultrasonographic structural failure of the repair and those who remained with a successful repair.16 Despite the limited available evidence, it seemed that subscapularis repair failed in an unacceptably high percentage of patients to be long-lasting, while it offered no additional clinical benefit in those who had a postoperative intact repair.
The main strength of the study conducted by Vourazeris et al.6 was that it compared the results of a single prosthesis design in patients who were treated with primary RTSA by a single surgeon. On the contrary, the integrity of the subscapularis repair was not evaluated in the study of Vourazeris et al.6 In addition, De Boer et al. reported that almost half (48.8%) of their patients were lost during the follow-up.16 Though, the study of Clark et al. noted that operations were carried out by three different surgeons, whereas there was a lack of shoulder subjective scores and the follow-up was small.7 As for the study of Werner et al., seven different surgeons performed the RTSA, while RoM was not documented as well as any information about the rehabilitation protocol. 17 Finally, the surgical technique and the physician’s experience might varied a lot in the study of Friedman et al., since this was a multi-centre study.18 On the other hand, this was the biggest study amongst all comparative trials that were including in this review.18
Overall, there was an absolute lack of randomized or non-randomized prospective controlled clinical trials in this review. The mean quality of the studies which were included in this review was moderate. The mean value of the modified Coleman methodology score was not high, while a number of possible bias might have deteriorated the results in all studies.
Conclusions
Although subscapularis repair was proven safe and effective for the augmentation of RTSA, it did not offer any additional clinical or functional benefit in the outcome of patients treated with lateralized RTSA. Therefore, it is not supported its routine use for patients who have a preoperatively sufficient subscapularis tendon.
Funding Statement
Funding: none.
References
- 1.Grammont P, Trouilloud P, Laffay J, Deries X. Concept study and realization of a new total shoulder prosthesis. Rhumatologie 1987;39:407-18. [Google Scholar]
- 2.Stevens CG, Struk AM, Wright TW. The functional impact of bilateral reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2014;23:1341-8. [DOI] [PubMed] [Google Scholar]
- 3.Alta T, Veeger GEJ, Thomas WJ, et al. Are Shoulders with A Reverse Shoulder Prosthesis Strong Enough? A Pilot Study. Clin Orthop Relat Res 2012;470:2185-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wiater BP, Koueiter DM, Maerz T, et al. Preoperative Deltoid Size and Fatty Infiltration of the Deltoid and Rotator Cuff Correlate to Outcomes After Reverse Total Shoulder Arthroplasty. Clin Orthop Relat Res 2015;473:663-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg 2005;14:S147-61. [DOI] [PubMed] [Google Scholar]
- 6.Vourazeris JD, Wright TW, Struk AM, et al. Primary reverse total shoulder arthroplasty outcomes in patients with subscapularis repair versus tenotomy. J Shoulder Elbow Surg 2017;26:450-7. [DOI] [PubMed] [Google Scholar]
- 7.Clark JC, Ritchie J, Song FS, et al. Complication rates, dislocation, pain, and postoperative range of motion after reverse shoulder arthroplasty in patients with and without repair of the subscapularis. J Shoulder Elbow Surg 2012;21:36-41. [DOI] [PubMed] [Google Scholar]
- 8.Edwards TB, Williams MD, Labriola JE, et al. Subscapularis insufficiency and the risk of shoulder dislocation after reverse shoulder arthroplasty. J Shoulder Elb Surg 2009;18:892-6. [DOI] [PubMed] [Google Scholar]
- 9.Oh JH, Shin SJ, McGarry MH, et al. Biomechanical effects of humeral neckshaft angle and subscapularis integrity in reverse total shoulder arthroplasty. J Shoulder Elb Surg 2014;23:1091-8. [DOI] [PubMed] [Google Scholar]
- 10.Boulahia A, Edwards TB, Walch G, Baratta RV. Early results of a reverse design prosthesis in the treatment of arthritis of the shoulder in elderly patients with a large rotator cuff tear. Orthopedics 2002;25:129-33. [DOI] [PubMed] [Google Scholar]
- 11.Grassi FA, Zorzolo I. Reverse shoulder arthroplasty without subscapularis repair for the treatment of proximal humeral fractures in the elderly. Musculoskelet Surg 2014;98:S5-13. [DOI] [PubMed] [Google Scholar]
- 12.Routman HD. The role of subscapularis repair in reverse total shoulder arthroplasty. Bull Hosp Joint Dis 2013;71:S108-12. [PubMed] [Google Scholar]
- 13.Hansen ML, Nayak A, Narayanan MS, et al. Role of subscapularis repair on muscle force requirements with reverse shoulder arthroplasty. Bull Hosp Jt Dis 2015;73:S21-7. [PubMed] [Google Scholar]
- 14.Giles JW, Langohr GD, Johnson JA, Athwal GS. The rotator cuff muscles are antagonists after reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2016;25:1592-600. [DOI] [PubMed] [Google Scholar]
- 15.Chalmers PN, Rahman Z, Romeo AA, Nicholson GP. Early dislocation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2014;23:737-44. [DOI] [PubMed] [Google Scholar]
- 16.de Boer FA, van Kampen PM, Huijsmans PE. The influence of subscapularis tendon reattachment on range of motion in reversed shoulder arthroplasty: a clinical study. Musculoskelet Surg 2016;100:121-6. [DOI] [PubMed] [Google Scholar]
- 17.Werner BC, Wong AC, Mahony GT, et al. Clinical Outcomes After Reverse Shoulder Arthroplasty With and Without Subscapularis Repair: The Importance of Considering Glenosphere Lateralization. J Am Acad Orthop Surg 2018. doi: 10.5435/JAAOS-D-16-00781. [DOI] [PubMed] [Google Scholar]
- 18.Friedman RJ, Flurin PH, Wright TW, et al. Comparison of reverse total shoulder arthroplasty outcomes with and without subscapularis repair. J Shoulder Elbow Surg 2017;26:662-8. [DOI] [PubMed] [Google Scholar]
- 19.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Viswanathan M, Ansari MT, Berkman ND, et al. Assessing the Risk of Bias of Individual Studies in Systematic Reviews of Health Care Interventions. Methods Guide for Effectiveness and Comparative Effectiveness Reviews [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008-2012. Mar 8. [PubMed] [Google Scholar]
- 21.Sambandam SN, Gul A, Priyanka P. Analysis of methodological deficiencies of studies reporting surgical outcome following cemented total-joint arthroplasty of trapezio-metacarpal joint of the thumb. Int Orthop 2007;31:639-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheung EV, Sarkissian EJ, Sox-Harris A, et al. Instability after reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2018;27:1946-52. [DOI] [PubMed] [Google Scholar]
- 23.Tashjian RZ, Burks RT, Zhang Y, Henninger HB. Reverse total shoulder arthroplasty: a biomechanical evaluation of humeral and glenosphere hardware configuration. J Shoulder Elbow Surg 2015;24:e68-77. [DOI] [PubMed] [Google Scholar]
- 24.Oh JH, Shin SJ, McGarry MH, et al. Biomechanical effects of humeral neckshaft angle and subscapularis integrity in reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2014;23:1091-8. [DOI] [PubMed] [Google Scholar]
- 25.Berhouet J, Garaud P, Favard L. Influence of glenoid component design and humeral component retroversion on internal and external rotation in reverse shoulder arthroplasty: a cadaver study. Orthop Traumatol Surg Res 2013;99:887-94. [DOI] [PubMed] [Google Scholar]
- 26.Zhou HS, Chung JS, Yi PH, et al. Management of complications after reverse shoulder arthroplasty. Curr Rev Musculoskelet Med 2015;8:92-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wall B, Nove-Josserand L, O'Connor DP, et al. Reverse total shoulder arthroplasty a review of results according to etiology. J Bone Joint Surg Am 2007;89:1476-85. [DOI] [PubMed] [Google Scholar]
- 28.Gutierrez S, Keller TS, Levy JC, et al. Hierarchy of stability factors in reverse shoulder arthroplasty. Clin Orthop Relat Res 2008;466:670-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer Award 2005: The Grammont reverse shoulder prosthesis: results in cuff tear arthritis. fracture sequlae.and revision arthroplasty. J Shoulder Elbow Surg 2006;15:527-40. [DOI] [PubMed] [Google Scholar]
- 30.Gerber C, Pennington SD, Nyffeler RW. Reverse total shoulder arthroplasty. J Am Acad Orthop Surg 2009;17:284-95. [DOI] [PubMed] [Google Scholar]
- 31.Jarrett CD, Brown BT, Schmidt CC. Reverse shoulder arthroplasty. Orthop Clin North Am 2013;44:389-408. [DOI] [PubMed] [Google Scholar]
- 32.Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverseball- and-socket total shoulder prosthesis. J Bone Joint Surg Am 2005;87:1476-86. [DOI] [PubMed] [Google Scholar]
- 33.Liou W, Yang Y, Petersen-Fitts GR, et al. Effect of lateralized design on muscle and joint reaction forces for reverse shoulder arthroplasty. J Shoulder Elbow Surg 2017;26:564-72. [DOI] [PubMed] [Google Scholar]
- 34.Huri G, Familiari F, Salari N, et al. Prosthetic design of reverse shoulder arthroplasty contributes to scapular notching and instability. World J Orthop 2016;7:738-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lawrence C, Williams GR, Namdari S. Influence of Glenosphere Design on Outcomes and Complications of Reverse Arthroplasty: A Systematic Review. Clin Orthop Surg 2016;8:288-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Valenti P, Sauzières P, Katz D, et al. Do less medialized reverse shoulder prostheses increase motion and reduce notching? Clin Orthop Relat Res 2011;469:2550-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kalouche I, Sevivas N, Wahegaonker A, et al. Reverse shoulder arthroplasty: does reduced medialisation improve radiological and clinical results. Acta Orthop Belg 2009;75:158-66. [PubMed] [Google Scholar]
- 38.Boughebri O, Kilinc A, Valenti P. Reverse shoulder arthroplasty combined with a latissimus dorsi and teres major transfer for a deficit of both active elevation and external rotation. Results of 15 cases with a minimum of 2-year follow-up. Orthop Traumatol Surg Res 2013;99:131-7. [DOI] [PubMed] [Google Scholar]
- 39.Middleton C, Uri O, Phillips S, et al. A reverse shoulder arthroplasty with increased offset for the treatment of cuff-deficient shoulders with glenohumeral arthritis. Bone Joint J 2014;96B:936-42. [DOI] [PubMed] [Google Scholar]
- 40.Frankle M, Levy JC, Pupello D, et al. The reverse shoulder prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. a minimum two-year follow-up study of sixty patients surgical technique. J Bone Joint Surg Am 2006;88:178-90. [DOI] [PubMed] [Google Scholar]


