Objectives:
Outborn (born outside tertiary centers) infants, especially extremely preterm infants, are at an increased risk of mortality and morbidity in comparison to inborn (born in tertiary centers) infants. Extremely preterm infants require not only skilled neonatal healthcare providers but also highly specialized equipment and environment surroundings. Maternal transport at an appropriate timing must be done to avoid the delivery of extremely preterm infants in a facility without the necessary capabilities. Cases of unexpected deliveries at birth centers or level I maternity hospitals need to be attended emergently. We compared the differences in short- and long-term outcomes between outborn and inborn infants to improve our regional perinatal system.
Design:
Retrospective cohort study.
Setting:
Neonatal Research Network of Japan database.
Patients:
Extremely preterm infants (gestational age between 22 + 0 and 27 + 6 wk) in the Neonatal Research Network of Japan database between 2003 and 2011.
Interventions:
None.
Measurements and Main Results:
A total of 12,164 extremely preterm infants, who were divided into outborn (n = 785, 6.5%) and inborn (n = 11,379, 93.5%) groups, were analyzed. Significant differences were observed in demographic and clinical factors between the two groups. Outborn infants had higher short-term odds of severe intraventricular hemorrhage (adjusted odds ratio, 1.49; 95% CI, 1.11–2.00; p < 0.01), necrotizing enterocolitis (adjusted odds ratio, 1.49; 95% CI, 1.11–2.00; p < 0.01), and focal intestinal perforation (adjusted odds ratio, 1.58; 95% CI, 1.09–2.30; p = 0.02). There were no significant differences in long-term outcomes between the two groups, except in the rate of cognitive impairment (adjusted odds ratio, 1.49; 95% CI, 1.01–2.20; p = 0.04).
Conclusions:
The frequency of severe intraventricular hemorrhage, necrotizing enterocolitis or focal intestinal perforation, and cognitive impairment was significantly higher in outborn infants. Thus, outborn/inborn birth status may play a role in short- and long-term outcomes of extremely preterm infants. However, more data and evaluation of improvement in the current perinatal environment are needed.
Keywords: inborn, outborn, perinatal system, preterm, retrieval system, very-low-birth-weight
Outborn infants, especially extremely preterm (EPT, birth at < 28 wk of gestation) infants, are at increased risk of mortality and morbidity in comparison to inborn infants because of their prominent vulnerability (1–3). There has been no clear progress in terms of the prevention of EPT births until recently, and the frequency of preterm birth is currently not decreasing (4). Short- and long-term outcomes of EPT infants have recently improved (5–8). However, long-term neurodevelopmental impairments (NDIs) remain a major concern, and there are few reports concerning the long-term outcomes of outborn EPT infants (5–8). EPT infants are at the highest risk and have the most specialized needs such as subspecialized neonatologists, highly skilled nursing staff, pediatric surgical specialists, physiologic monitoring equipment, and laboratory facilities. An appropriate timing must be selected for maternal transport to avoid the delivery of EPT infants in a facility without the necessary capabilities, where it is extremely difficult to stabilize the infants at birth and transport them to a neonatal ICU (NICU) of a tertiary center. The American Academy of Pediatrics and the American College of Obstetrics and Gynecologists Guidelines for Perinatal Care recommend that hospital-based services should be organized within geographical regions. Maternity hospitals should be located based on functional capabilities to provide adequate care for pregnant women and neonates at increased risk of EPT births (8, 9). The regionalization of perinatal care has been in place since around 1990 in Japan. However, Japan is unique in that approximately 50% of deliveries are managed at birth centers or level I hospitals for maternal care (10). Transporting women at risk of very preterm births to tertiary centers has significantly decreased the neonatal mortality and morbidity rate (11, 12). Considering the organization of parturient facilities in Japan and the difficulty of predicting EPT deliveries, it is possible that EPT outborn infants may be born at birth centers or level I maternity hospitals. In most cases, there is insufficient transportation time because of the rapid progression of labor. Thus, solving the present perinatal problems (e.g., appropriate resuscitation and transportation of vulnerable EPT infants) at birth centers or level I maternity hospitals remains a crucial issue.
This study aimed to evaluate whether the birth status (outborn or inborn) of EPT infants influenced their short- and long-term outcomes based on information from the Neonatal Research Network of Japan (NRNJ) database.
MATERIALS AND METHODS
The protocol of this study was approved by the central internal review board at Tokyo Women’s Medical University, where all data were collected and stored. Written informed consent was obtained from the parents or guardians of all infants in the NRNJ. This was a retrospective analysis of 12,164 EPT infants, defined as those with a gestational age between 22 + 0 and 27 + 6 weeks, among very-low-birth-weight (VLBW) singleton and twin infants. Clinical data between 2003 and 2011 were obtained from the NRNJ database, which was created with a grant from the Ministry of Health, Labor, and Welfare of Japan. There was a systematic registration of VLBW infants so that almost all cases that were handled in the study period would be present in the medical records. This database collected data on greater than 50% of EPT infants born in Japan during the study period, and 186 facilities (including 84 tertiary centers) were registered for the NRNJ in 2011. This database contains information on morbidity, mortality, and follow-up data of EPT infants in participating facilities. Exclusion criteria were as follows: multiple births (more than triplets), any major congenital malformations, admission after greater than 1 day after birth, transported to other hospitals at birth, and those without records of mortality status and information on the mode of delivery. Data for 81 infants who were born alive but died in the delivery room were also excluded (Fig. 1). Gestational age was calculated based on ultrasound examination during the first trimester and the data of the last menstrual period. The presence of pathologic chorioamnionitis was examined based on Blanc’s criteria. Premature rupture of membranes (PROM) was defined as the rupture of membranes before the onset of labor. Antenatal corticosteroid (ACS) administration was defined as at least one dose of ACS to the mother at any time before delivery to accelerate fetal lung maturity. Small for gestational age (SGA) was defined as a birth weight below the 10th percentile of the standard birth weight for gestational age published by the Japan Pediatric Society (13). Respiratory distress syndrome (RDS) was diagnosed on the basis of clinical presentation and characteristic radiographic appearance. Chronic lung disease (CLD) was defined as a persistent requirement for supplemental oxygen 28 days after birth or at 36 weeks postmenstrual age. Patent ductus arteriosus (PDA) was diagnosed based on both echocardiographic and clinical findings. Severe intraventricular hemorrhage (IVH) was defined as grade III to IV, according to the Papile criteria. Cystic periventricular leukomalacia (PVL) was defined as any cyst formation observed at any time in the periventricular white matter on cranial ultrasound or head MRI. The presence of sepsis was determined by positive blood culture results. Necrotizing enterocolitis (NEC) was defined according to Bell’s classification stage II or greater. Retinopathy of prematurity (ROP) was considered to be severe if the worst stage of ROP was III (intermediate) or greater according to the criteria proposed by the task force of the Ministry of Health, Labor and Welfare of Japan, which was equivalent to stage III or greater in the International Classification of ROP, and if treatment was required with laser coagulation, cryocoagulation therapy, or both. Neonatal mortality was defined as death of an infant before hospital discharge. The follow-up protocol consisted of routine physical and neurologic evaluations and developmental assessments at three years (36–42 mo) of chronological age for surviving EPT infants at each participating center (14). Neurologic evaluation at 3 years old included signs and symptoms of cerebral palsy (CP) and sensory abnormality. CP was defined as a nonprogressive CNS disorder characterized by abnormal muscle tone in at least one extremity and abnormal control of movement and posture. Visual impairment was defined as unilateral or bilateral blindness diagnosed by ophthalmologists. Severe hearing impairment was defined as when amplification was required. The assessment of cognitive function was performed using the Kyoto Scale of Psychologic Development (KSPD) test (15). This test was administered by experienced testers who were certified psychologists blinded to the perinatal details at each participating center. All information about the infants was collected anonymously, and the stored data were unlinked from individual data. When the development quotient (DQ) was less than 70, the infant was judged as having a cognitive impairment according to the protocol of the Society for Follow-up Study of High-risk Infants. If the KSPD assessment was not available, the pediatrician estimated the child’s developmental level as delayed or not delayed. In cases judged as delayed, the developmental level was assumed as equivalent to a DQ score less than 50. Infants with CP, visual impairment, severe hearing impairment, and cognitive impairment were designated as having NDI. We analyzed the effect of place of birth (outborn vs inborn) on short- and long-term outcomes. Short-term outcomes were RDS, CLD, surgery for PDA, severe IVH, cystic PVL, sepsis, NEC or intestinal perforation, severe ROP, and neonatal mortality. The chosen long-term outcomes were death after hospital discharge up to 3 years, CP, visual impairment, severe hearing impairment, cognitive impairment, and NDI.
Figure 1.
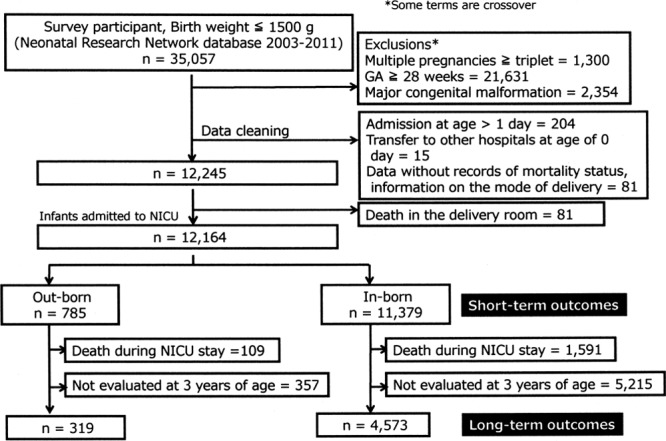
Flow chart of study population. Analyzed data (n = 12,164) were obtained from the Neonatal Research Network of Japan database (2003–2011). GA = gestational age, NICU = neonatal ICU.
Statistical analyses were performed using SPSS Version 24.0 (SPSS, Chicago, IL). The significance level was set at 0.05. Continuous data are presented as means ± sd. Absolute standardized differences (ASDs) were calculated to evaluate the statistical difference at baseline between those who dropped out in the evaluation of long-term prognosis and those who completed follow-up, with an ASD above 10% representing a meaningful imbalance. Differences in perinatal baseline characteristics between the outborn and inborn infants were tested using a chi-square test and t test, as appropriate, to find confounders in the relationship analysis between being outborn and outcomes (short- and long-term outcome). The relationship between being outborn and outcomes was examined by logistic regression analysis. With each outcome (short-term and long-term outcome) as a dependent variable, the odds ratio (OR) and 95% CI of being outborn (vs inborn) were calculated.
RESULTS
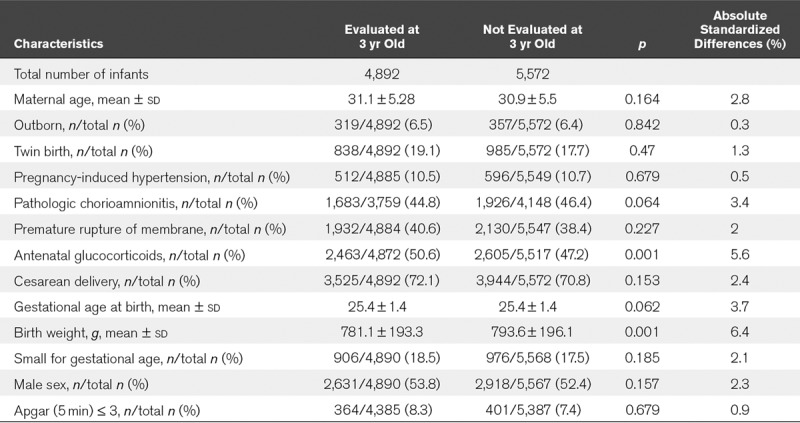
The study group is illustrated in Figure 1. A total of 35,057 VLBW infants were registered in the database between 2003 and 2011. In total, 2,354 infants were excluded because of major congenital malformation, 1,300 infants were excluded because of multiple births (more than triplets), and 21,631 infants were excluded because they were born at gestational ages greater than or equal to 28 + 0 weeks or less than 22 + 0 weeks. After exclusion of inappropriate cases (infants without records of mortality status), data of 12,245 singleton and twin infants born at gestational ages between 22 + 0 and 27 + 6 weeks were available. Of these, 81 infants died in the delivery room and were excluded. A final number of 12,164 EPT infants were enrolled as the study population. Of the 12,164 subjects, 785 (6.5%) were outborn EPT infants. Of the 785 outborn and 11,379 inborn infants, 109 (13.8%) and 1,591 (14.0%), respectively, died before discharge from the hospital. Of the surviving 676 outborn and 9,788 inborn infants, follow-up data at 3 years old were collected from 319 (47.2%) and 4,573 (46.7%), respectively. Maternal and delivery characteristics for the outborn and inborn groups are listed in Table 1. There were no differences between the groups in terms of the distribution of infants from 22 to 27 gestational weeks. The outborn group had significantly lower rates of twin birth (p < 0.01), pregnancy-induced hypertension (PIH) (p < 0.01), pathologic chorioamnionitis (p < 0.01), PROM (p < 0.01), administration of ACS (p < 0.01), cesarean delivery (p < 0.01), and SGA (p < 0.01) and higher rate of Apgar (5 min) less than or equal to 3 (p < 0.01). The outborn group also had lower maternal age (p < 0.01) and higher birth weight (p < 0.01). The effects on short-term outcomes are listed in Table 2. The multivariate logistic regression analysis performed after adjusting for confounders (twin birth, PIH, pathologic chorioamnionitis, PROM, ACS administration, cesarean delivery, SGA, Apgar [5 min] ≤ 3, maternal age, and birth weight) showed that outborn infants had higher odds of severe IVH (adjusted OR, 1.49; 95% CI, 1.11–2.00; p < 0.01) and NEC or FIP (adjusted OR, 1.58; 95% CI, 1.09–2.30; p = 0.015) for short-term outcomes. The effects on long-term outcomes are listed in Table 3. There were no significant differences between the outborn and inborn groups, except for the rate of cognitive impairment (adjusted OR, 1.49; 95% CI, 1.01–2.20; p = 0.04) in the multivariate logistic regression analysis. ASD values were calculated to evaluate statistical difference in baseline characteristics between those who dropped out of the evaluation of long-term prognosis and those who completed follow-up. All ASD values were under 10% (Table 4).
TABLE 1.
Demographics and Baseline Characteristics (n = 12,164)
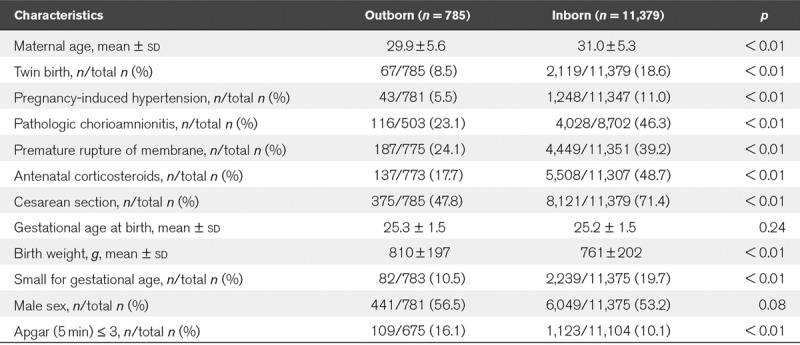
TABLE 2.
The Multivariate Logistic Regression Analysis of Short-Term Outcomes
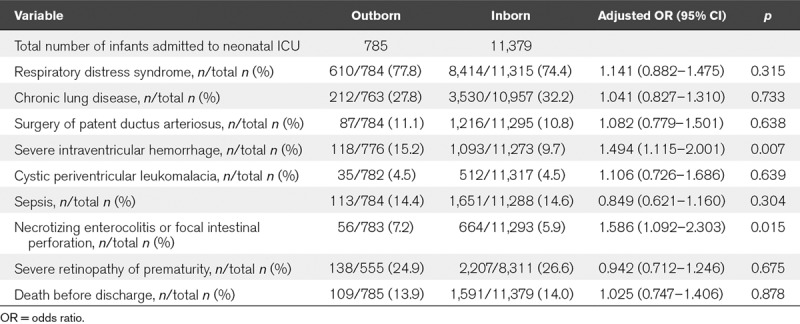
TABLE 3.
The Multivariate Logistic Regression Analysis of Long-Term Outcomes
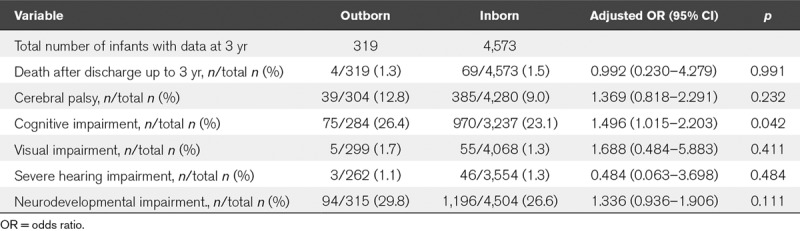
TABLE 4.
Baseline Characteristics of Missing Data Not Evaluated at 3 Years Old
DISCUSSION
In this study, we found that the outborn group included more cases at small risk of EPT and had a significantly higher frequency of severe IVH, NEC or FIP, and cognitive impairment. We could not find studies about the long-term outcomes of outborn EPT infants, although there were some reports on short-term outcomes. To the best of our knowledge, this is the first large cohort study to explore short- and long-term outcomes of EPT inborn and outborn infants. Higher rates of mortality and morbidity for outborn infants have been reported (1–3).
Significant differences were observed between the inborn and outborn groups in demographic and clinical factors. The outborn group may include more cases at smaller risk of EPT when compared with the inborn group, since the inborn group had significantly higher rates of twin birth, PIH, pathologic chorioamnionitis, PROM, SGA, and lower birth weight. If only background factors are considered, a good outcome for outborn infants can be expected, with the exceptions of ACS treatment and higher rate of a low Apgar score at 5 minutes. We found no difference in mortality risk between outborn and inborn infants. However, a significant difference in severe IVH and NEC or FIP was found, even after adjusting for perinatal risk factors. Nevertheless, the rates of all these morbidities remain low compared with other studies (7). There were no significant differences in long-term outcomes between the two groups, except for the rate of cognitive impairment. The high rate of cognitive impairment may be due to the high rate of severe IVH and NEC or FIP seen in the short-term outcomes.
Our data did not include stillbirths and deaths in the delivery room at birth hospitals other than the participating tertiary centers. Data about resuscitation of outborn livebirths were only available for those referred to tertiary centers and not for outborn infants who died at the birth hospital without being referred. Thus, it was not possible to obtain information on decision-making or other aspects of care for outborn livebirths that were not referred to tertiary centers. Insufficient time to administer ACS, suboptimal resuscitation at birth, and lack of medical equipment and staff expertise have been identified as risk factors contributing to mortality in EPT infants (16). Previous studies emphasize the value of high-volume level III NICU care in minimizing neonatal mortality and morbidity among VLBW infants (17, 18).
Unfortunately, there is no nationwide standard for the transportation of EPT infants (including use of transport incubators and presence of a neonatologist and neonatal nursing staff) in Japan at present. Improvements in the regional perinatal system, such as optimized transportation to tertiary centers, can improve the outcomes of EPT infants, as several factors at birth or during transport play a role in the health risks of outborn EPT infants (2, 19). The risk of severe IVH and NEC or FIP in outborn infants may reflect the influence of inappropriate circumstances such as insufficient resuscitation at the time of birth and unstable environment such as hypo- or hyperthermia in an ambulance during the transportation period. The association between admission temperature and mortality and morbidity in EPT infants has been reported (19). It seems unlikely that there will be a dramatic improvement in this situation in the future, as small regional birth centers and level I maternity care hospitals handle approximately 50% of deliveries in Japan. In other words, EPT outborn births will continue to occur for a long period in Japan. Part of the solution to improve neonatal retrieval services of the births in birth centers and level I maternity care hospitals could be to increase efforts to transport the pregnancies at risk of EPT in utero. Retrieval services means not only emergency transport services but also for subspecialized neonatologists to be present at births of the EPT infants in nontertiary hospitals to resuscitate and to stabilize the infants whenever possible. The regional maternal and neonatal transport system has been improving gradually, but the neonatal retrieval services for the regional perinatal system have remained largely unimproved in the past 20 years. Improved quality of resuscitation was reported when dedicated neonatal retrieval teams resuscitated outborn infants in the delivery room (16). Retrieval services may make it possible to provide outborn infants with intensive care or interventions such as intubation, surfactant administration, cardiorespiratory monitoring, ventilation support, and accurate drug administration at the birth hospital and during transport, thus increasing the possibility that outborn infants will receive intensive care approximately equal to that of a level III NICU at birth centers or level I maternity care hospitals. It was reported that the mortality before NICU admission for EPT outborn infants was significantly higher when compared with that for inborn infants (20). We may need to equip the regional perinatal system to send the neonatal retrieval team to birth hospitals in case of emergency as much as possible; however, there are several issues to address, such as securing neonatologists, sharing information between the birth hospital and tertiary center, and arranging the ambulance for exclusive use for newborn babies. Naturally, obstetricians at birth hospitals should acquire enough knowledge and skills to resuscitate EPT infants and to stabilize their general condition until the arrival of the retrieval team or transport to a tertiary hospital.
Our study has some limitations. The first was the amount of missing data (53.2%) related to information on NDI at 3 years. We made a comparison for maternal and delivery characteristics between infants evaluated and not evaluated for NDI at 3 years. All ASD values to evaluate statistical difference were under 10%, and the low follow-up rate might not have a clinically important influence on short- and long-term outcomes between EPT infants who had data available for NDI and survivors who were lost to follow-up. The second was that we used the KSPD scale for evaluating developmental outcomes instead of the Bayley Scales of Infant Development III (Bayley III), which is widely used throughout the world. However, one study reported that the KSPD scale correlated well with Bayley III (15). Furthermore, our study design was a case-control comparison using the same developmental scale. Thus, we could not expect any discrepancy in our results. The third was that stillbirths and deaths of neonates who could not be transported to tertiary centers were not included in our data. These data may influence the result of our analysis for the short- and long-term outcomes to some extent. Recently, the unification of the nationwide neonatal and obstetrical data was discussed at the meeting of the Japan Society of Perinatal and Neonatal Medicine. We should acquire the information for outborn livebirths that were not referred to tertiary centers to more accurately determine the current provision of perinatal care.
CONCLUSIONS
Our study pointed out that there was a significantly higher frequency of severe IVH, NEC or FIP, and cognitive impairment in outborn infants compared with the inborn infants. Thus, outborn/inborn birth status may influence short- and long-term outcomes of EPT infants. For the improvement of the current perinatal care standard, we should obtain more precise data of outborn EPT infants, including livebirths that were not referred to tertiary centers. Based on this analysis, more effort is needed to improve our perinatal environment, such as developing a neonatal retrieval system for outborn EPT infants.
ACKNOWLEDGMENTS
We thank all patients for their generous contributions. We also thank the data center at Tokyo Women’s Medical University (Tokyo, Japan) for providing organizational support to the Neonatal Research Network of Japan. List of participating units: Sapporo City Hospital, Asahikawa Kosei Hospital, Kushiro Red Cross Hospital, Obihiro Kosei Hospital, Tenshi Hospital, NTT East Sapporo Hospital, Nikko Kinen Hospital, Sapporo Prefecture Medical University, Asahikawa Medical University, Aomori Prefecture Central Hospital, Iwate Medical University, Iwate Prefecture Ohfunato Hospital, Prefecture Kuji Hospital, Iwate Prefecture Ninohe Hospital, Sendai Red Cross Hospital, Akita Red Cross Hospital, Akita University, Tsuruoka City Shonai Hospital, Yamagata, Yamagata Prefecture Central Hospital, Fukusima Prefecture Medical University, Takeda General Hospital, National Fukushima Hospital, Tsukuba University, Tsuchiura Kyodo Hospital, Ibaraki Children’s Hospital, Dokkyo Medical University, Jichi Medical University, Ashikaga Red Cross Hospital, Gunma Prefecture Children’s Hospital, Kiryu Kosei General Hospital, Gunma University, Saitama Prefecture Children’s Hospital, National Nishisaitama Central Hospital, Saitama Medical University Medical Center, Kawaguchi City Medical Center, Jichi Medical University Saitama Medical Center, Asahi Central Hospital, Chiba City Kaihin Hospital, Kameda General Hospital, Tokyo Women’s Medical University Yachiyo Medical Center, Juntendo University Urayasu Hospital, Tokyo Metropolitan Children’s Medical Center, Tokyo Women’s Medical University, Aiiku Hospital, Nihon University, National International Medical Center, Teikyo University, Showa University, Japan Red Cross Hospital, National Center for Child Health and Development, Tokyo Metropolitan Otsuka Hospital, Toho University, Tokyo Metropolitan Bokuto Hospital, Tokyo Jikei Medical University, Saint Luku Hospital, Juntendo University, Sanikukai Hospital, Katsushika Red Cross Hospital, Yokohama Rosai Hospital, Yokohama City University Medical Center, Marianna Medical University, Kanagawa Children’s Medical Center, Tokai University, Kitazato University, Odawara City Hospital, Nippon Medical School Musashi Kosugi Hospital, Saiseikai Eastern Yokohama Hospital, Yokohama Medical Center, Yamanashi Prefecture Central Hospital, Nagano Children’s Hospital, Shinshu University, Iida City Hospital, National Shinshu Ueda Medical Center, Saku General Hospital, Niigata University, Niigata Central Hospital, Niigata City Hospital, Nagaoka Red Cross Hospital, Koseiren Takaoka Hospital, Toyama Prefectural Central Hospital, Toyama University, Ishikawa Prefectural Central Hospital, Kanazawa, Medical University, Fukui Prefectural Hospital, Fukui University, Gifu Prefectural Medical Center, Takayama Red Cross Hospital, Seirei Hamamatsu Hospital, Shizuoka Saiseikai Hospital, Shizuoka Children’s Hospital, Hamamatsu Medical University, Yaizu City Hospital, Fujieda City Hospital, Nagoya Red Cross Daini Hospital, Nagoya University, Nagoya Red Cross Daiici Hospital, Anjokosei Hospital, Koritsu Tosei Hospital, Komaki City Hospital, Toyota Memorial Hospital, Okazaki City Hospital, Konankosei Hospital, National Mie Central Medical Center, Ise Red Cross Hospital, Yokkaichi City Hospital, Otsu Red Cross Hospital, Shiga Medical University, Nagahama Red Cross Hospital, Uji Tokushukai Hospital, Japan Baptist Hospital, Kyoto University, Kyoto Red Cross Daiichi Hospital, National Maizuru Medical Center, Fukuchiyama City Hospital, Kyoto Prefecture Medical University, Kyoto City Hospital, Yodogawa Christian Hospital, Osaka Medical Center and Research Institute for Maternal and Child Health, Osaka University, Takatsuki General Hospital, Kansai Medical University, Osaka City General Hospital, Osaka City Sumiyoshi Hospital, Aizenbashi Hospital, Toyonaka City Hospital, National Cerebral and Cardiovascular Center, Kitano Hospital, Saiseikai Suita Hospital, Chifune Hospital, Bell Land General Hospital, Rinku General Hospital, Yao City Hospital, Osaka City University, Kobe Children’s Hospital, Kobe University, Saiseikai Hyogo Hospital, Kobe City Medical Center Central Hospital, Hyogo Medical University, Himeji Red Cross Hospital, Toyooka General Hospital, Hyogo Prefectural Awaji Hospital, Nara Prefecture Medical University, Wakayama Prefecture Medical University, Tottori Prefectural Central Hospital, Tottori University, Shimane Prefectural Central Hospital, Matsue Red Cross Hospital, Kurashiki Central Hospital, Tsuyama Central Hospital, Kawasaki Medical University, National Okayama Medical Center, Okayama Red Cross Hospital, Hiroshima City Central Hospital, Hiroshima Prefectural Hospital, Tsuchiya General Hospital, National Kure Medical Center, Yamaguchi Prefecture Medical Center, Tokushima University, Kagawa University, Shikoku Medical Center for Children and Adults, Matsuyama Red Cross Hospital, Ehime Prefectural Central Hospital, Kochi Health Science Center, Saint Maria Hospital, National Kyushu Medical Center, Kurume University, Kitakyushu City Hospital, University of Occupational and Environmental Health Japan, Fukuoka University, Kyushu University, Iizuka Hospital, National Kokura Medical Center, National Saga Hospital, National Nagasaki Medical Center, Kumamoto City Hospital, Kumamoto University, Oita Prefectural Hospital, Almeida Memorial Hospital, Nakatsu City Hospital, Miyazaki University, Kagoshima City Hospital, Imakyure General Hospital, Okinara Prefectural Central Hospital, Naha City Hospital, and Okinawa Red Cross Hospital.
Footnotes
*See also p. 994.
The authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Marlow N, Bennett C, Draper ES, et al. Perinatal outcomes for extremely preterm babies in relation to place of birth in England: The EPICure 2 study. Arch Dis Child Fetal Neonatal Ed 2014; 99: F181–F188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Serenius F, Sjörs G, Blennow M, et al. ; EXPRESS study group: EXPRESS study shows significant regional differences in 1-year outcome of extremely preterm infants in Sweden. Acta Paediatr 2014; 103:27–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fellman V, Hellström-Westas L, Norman M, et al. ; EXPRESS Group: One-year survival of extremely preterm infants after active perinatal care in Sweden. JAMA 2009; 301:2225–2233 [DOI] [PubMed] [Google Scholar]
- 4.Iams JD, Romero R, Culhane JF, et al. Primary, secondary, and tertiary interventions to reduce the morbidity and mortality of preterm birth. Lancet 2008; 371:164–175 [DOI] [PubMed] [Google Scholar]
- 5.Moore T, Hennessy EM, Myles J, Johnson SJ, et al. Neurological and developmental outcome in extremely preterm children born in England in 1995 and 2006: The EPICure studies. BMJ 2012; 345:e7961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Serenius F, Källén K, Blennow M, et al. ; EXPRESS Group: Neurodevelopmental outcome in extremely preterm infants at 2.5 years after active perinatal care in Sweden. JAMA 2013; 309:1810–1820 [DOI] [PubMed] [Google Scholar]
- 7.Shah PS, Lui K, Sjörs G, et al. ; International Network for Evaluating Outcomes (iNeo) of Neonates: Neonatal outcomes of very low birth weight and very preterm neonates: An International Comparison. J Pediatr 2016; 177:144–152.e6 [DOI] [PubMed] [Google Scholar]
- 8.American Academy of Pediatrics: Committee on fetus and newborn: Level of neonatal care. Pediatrics 2004; 114:1341–134715520119 [Google Scholar]
- 9.American College of Obstetrics and Gynecologists, Society for Maternal Fetal Medicine: Obstetric Care Consensus No. 2: Levels of maternal care. Obstet Gynecol 2015; 125:502–515 [DOI] [PubMed] [Google Scholar]
- 10.Katsuya K. Maternal and Child Health Statistics of Japan. 2016Tokyo, Japan, Mother`s and Children`s Health Organization. [Google Scholar]
- 11.Towers CV, Bonebrake R, Padilla G, et al. The effect of transport on the rate of severe intraventricular hemorrhage in very low birth weight infants. Obstet Gynecol 2000; 95:291–295 [DOI] [PubMed] [Google Scholar]
- 12.Hohlagschwandtner M, Husslein P, Klebermass K, et al. Perinatal mortality and morbidity. Comparison between maternal transport, neonatal transport and inpatient antenatal treatment. Arch Gynecol Obstet 2001; 265:113–118 [DOI] [PubMed] [Google Scholar]
- 13.Itabashi K, Miura F, Uehara R, et al. New Japanese neonatal anthropometric charts for gestational age at birth. Pediatr Int 2014; 56:702–708 [DOI] [PubMed] [Google Scholar]
- 14.Mishita J. Protocols for follow-up of high-risk infants. Perinat Med 2000; 30:1263–1272 (in Japanese) [Google Scholar]
- 15.Kono Y, Yonemoto N, Kusuda S, et al. Developmental assessment of VLBW infants at 18 months of age: A comparison study between KSPD and Bayley III. Brain Dev 2016; 38:377–385 [DOI] [PubMed] [Google Scholar]
- 16.Lui K, Abdel-Latif ME, Allgood CL, et al. ; New South Wales and Australian Capital Territory Neonatal Intensive Care Unit Study Group: Improved outcomes of extremely premature outborn infants: Effects of strategic changes in perinatal and retrieval services. Pediatrics 2006; 118:2076–2083 [DOI] [PubMed] [Google Scholar]
- 17.Binder S, Hill K, Meinzen-Derr J, et al. Increasing VLBW deliveries at subspecialty perinatal centers via perinatal outreach. Pediatrics 2011; 127:487–493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Phibbs CS, Baker LC, Caughey AB, et al. Level and volume of neonatal intensive care and mortality in very-low-birth-weight infants. N Engl J Med 2007; 356:2165–2175 [DOI] [PubMed] [Google Scholar]
- 19.Laptook AR, Bell EF, Shankaran S, et al. ; Generic and Moderate Preterm Subcommittees of the NICHD Neonatal Research Network: Admission temperature and associated mortality and morbidity among moderately and extremely preterm infants. J Pediatr 2018; 192:53–59.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boland RA, Davis PG, Dawson JA, et al. Outcomes of infants born at 22–27 weeks’ gestation in Victoria according to outborn/inborn birth status. Arch Dis Child Fetal Neonatal Ed 2017; 102:F153–F161 [DOI] [PubMed] [Google Scholar]


