Supplemental Digital Content is available in the text
Keywords: LASIK, patient-reported outcomes, SMILE
Purpose:
Laser in situ keratomileusis (LASIK) and small-incision lenticule extraction (SMILE) are popular refractive surgeries. The objective refractive outcomes of LASIK and SMILE have been studied extensively; both procedures have comparable safety, efficacy, and predictability. However, owing to various psychosocial factors, refractive patients may report dissatisfaction despite good postoperative vision. Hence the importance of studies on subjective patient-reported outcomes. This review discusses the role of psychometric-technique-based validated questionnaires when evaluating subjective outcomes. It also summarizes the literature on patient-reported outcomes for LASIK and SMILE.
Design:
A literature search was performed on PubMed database to identify studies that have assessed patient-reported outcomes for LASIK and SMILE.
Results:
Several studies have looked into patient-reported outcome measures for LASIK, but the number of equivalent studies for SMILE is limited. Questionnaires (validated and non-validated) are used to evaluate patient-reported outcomes. Validated questionnaires are designed based on psychometric techniques, such as Classic Test Theory, Item Response Theory, and Rasch analysis. The Quality of Life Impact of Refractive Correction (QIRC) questionnaire, a validated questionnaire administered to both LASIK and SMILE patients, suggests that both groups have comparable vision-related quality of life in the first few months postoperatively; but SMILE might confer a slight advantage in the later postoperative period (postoperative month 6).
Conclusions:
Future LASIK-SMILE comparative studies utilizing standardized validated questionnaires for patient-reported outcome measures with longer follow-up durations would be a welcome contribution to this important aspect of refractive surgery.
Refractive surgeries are one of the most common operations performed globally.1 Refractive surgical options include laser corneal surgeries such as photorefractive keratectomy, laser assisted keratomileusis, laser-assisted subepithelial keratectomy, and refractive lenticule extraction (ReLEx, Carl Zeiss Meditec AG).2
Laser in situ keratomileusis (LASIK) is a popular refractive procedure.3 A flap is first created with a microkeratome or a femtosecond laser, after which an excimer laser is used to ablate the cornea stromal bed.4 Refractive lenticule extraction is a newer refractive procedure. The procedure was first introduced as femtosecond lenticule extraction (FLEx, Carl Zeiss Meditec AG), where a femtosecond laser is used to create a flap and cut out an underlying stromal lenticule. The lenticule is then removed by reflecting the flap.5 Small-incision lenticule extraction (SMILE, Carl Zeiss Meditec AG) was subsequently introduced in 2011, where the stromal lenticule is extracted through a small 2 to 4 mm arcuate corneal incision.5–8 Refractive lenticule extraction surgery confers a few advantages over LASIK, it only requires a single laser machine,9 has lower total laser energy requirements,10,11 and avoids flap-related complications such as dry eyes, cornea neurotrophy, and postoperative discomfort.12 SMILE is also a potentially reversible procedure as the stored lenticule might be reimplanted.13
The refractive outcomes of LASIK and SMILE are relatively comparable. Meta-analyses and literature reviews8,14,15 have concurred that the safety, efficacy, and predictability of both procedures are relatively similar.
Refractive surgery is usually performed on healthy eyes with good aided visual acuity. Hence refractive patients have high expectations. Nichols et al1 observed that myopic individuals keen on refractive surgery tended to have higher expectations for postoperative vision improvement as compared with other myopic individuals not interested in LASIK. Anecdotally, it is also not uncommon for patients to report dissatisfaction with their refractive surgery despite of 20/20 vision. This might be accounted for by higher order aberrations, glare, contrast sensitivity, night vision symptoms, and dry eye symptoms.16 However, these objective psychophysical measures may not always be indicative of patient satisfaction.1,17–20 This discordance between objective outcomes and subjective perceptions highlights the importance of evaluating patient-reported outcome measures on top of the objective outcomes. Patient-reported outcomes provide better insights into the effect that refractive surgery has on a patient's subjective visual function and performance in the real world setting. It can be considered as a more comprehensive assessment of the success of a refractive procedure.19,21
This review article serves as a primer to help refractive surgeons better understand the various questionnaires used to evaluate patient-reported outcomes and aims to summarize the available literature on qualitative outcomes of LASIK and SMILE based on a literature search on PubMed.
QUESTIONNAIRES FOR PATIENT-REPORTED OUTCOME MEASURES
Patient-reported outcomes are often assessed through survey questionnaires. Some questionnaires are merely a list of questions, created by investigators, that enquire about various symptoms and concerns before and after surgery.17,20,22–29 These questionnaires are nonstandardized and not widely adopted. Their findings are of limited value, as it is difficult to make comparisons across studies that use different questionnaires.
In contrast to nonvalidated questionnaires, validated questionnaires are more scientifically robust and better at understanding patient-reported outcomes.30
First, question-items in validated questionnaires tend to be better targeted at the population of interest. Validated questionnaires are usually created after extensive literature review and focus group discussions with patients and industry experts to guide the selection of relevant questions.31,32 With first-hand information of the entire range of functional, emotional, psychological, and social concerns, these questionnaires pose poignant questions that address key concerns amongst refractive patients.
Second, the design of validated questionnaires is guided by psychometric analysis techniques. In contrast, nonvalidated surveys comprising of random questions might result in inaccurate conclusions because of poor data collection methodology. The main types of psychometric analysis techniques include classical test theory (CTT) and item response theory (IRT) such as Rasch analysis.33 Several previous questionnaires on qualitative outcomes in ophthalmology have been developed based on CTT methods, whereas newer questionnaires have been designed based on IRT and Rasch analysis methods.34 Some examples of CTT based on commonly used refractive questionnaires include the National Eye Institute Refractive Error Quality of Life Instrument, Refractive Status Vision Profile survey, Prospective Evaluation of Radial Keratotomy study questionnaire, Canadian Refractive Surgery Research Group Quality of Vision questionnaire, Myopia-specific quality of life questionnaire, and Subjective Vision questionnaire.2 Meanwhile, questionnaires based on IRT analysis include Quality of Life Impact of Refractive Correction (QIRC), Quality of Vision (QoV), Visual Function and Quality of Life, and Near Activity Visual Questionnaire.35
When questionnaires based on older psychometric techniques like CCT were compared with newer psychometric analysis techniques (IRT and Rasch analysis), some were found to have invalid measures.2,33,36–38 Despite of certain flaws, several of these CTT-based questionnaires are still being used in various studies.
Questionnaires developed by the Rasch analysis are psychometrically superior to those developed based on CCT.38–42 They have a few key advantages. First, they assign an appropriate weightage to each question by accounting for the context of the visual disability assessed. For example, if a questionnaire poses questions about one's ability to drive at night and one's ability to drive in the day, Rasch analysis provides an appropriate weightage factor to each of the two questions as it accounts for the fact that it is more difficult to drive at night.43 Second, Rasch analysis ensures that summated question scores are unidirectional, whereby only questions assessing a similar outcome measure are summated. For example, if a survey comprises questions that evaluate emotional and functional outcomes, Rash analysis ensures that questions pertaining to each category are summated in 2 separate scores.31 This is important as a multidimensional summary score would be confounded by other latent traits assessed.33,44 Third, Rasch analysis ensures that questions are relevant to the population being studied (item targeting). For example, a questionnaire designed for refractive patients should have a different set of questions as compared with a questionnaire for low-vision patients, as both groups have different vision capabilities. Meanwhile, analytical techniques such as differential item functioning help identify poorly designed questions that might elicit inappropriately skewed responses from certain groups of respondents. Also, item-fit statistics, recorded as mean square standardized residuals (MNSQ) help identify questions which are redundant (low MNSQ) and irrelevant questions that result in noise (high MNSQ).31
Rasch analysis-guided questionnaires are better than CTT-based questionnaires, but they have their own set of shortcomings. For example, the QIRC was criticized to be multidimensional and hence was split into 2 unidimensional scales (functional and emotional outcomes).2,45 Meanwhile, the QoV has been criticized for suboptimal targeting and differential item functioning,46 whereas the NAVQ is limited by suboptimal item-fit statistics and targeting.2
Kandel et al2 published a literature review in 2017 that evaluated the psychometric performance of various qualitative questionnaires for refractive patients. They provided a good overview of some of the more commonly administered questionnaires (available at). The review concluded that the QoV questionnaire was the most appropriate questionnaire for assessing visual symptoms. But the QIRC questionnaire was recommended for assessing quality of life and the NAVQ was recommended for assessing activity limitation resulting from presbyopia.
The validity of results obtained from questionnaires is largely determined by how responses were obtained. Hence, to best understand the patients’ perspective of refractive surgery outcomes, we should be discerning by only looking at studies that have utilized validated questionnaires designed based on sound psychometric techniques.
Patient-Reported Outcome Measures in SMILE and LASIK: Comparative Studies With Validated Questionnaires
To date, there are only 2 studies that employed validated questionnaires to directly compare patient-reported outcomes in LASIK and SMILE.39,47 These 2 comparative studies used the QIRC questionnaire to compare patient-reported outcomes in LASIK and SMILE, they were conducted in Singapore and Russia by Ang et al39 and Klokova et al,47 respectively.
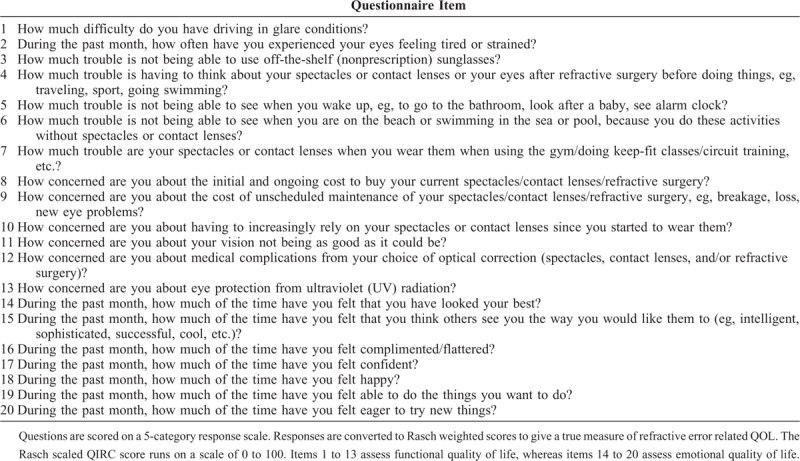
The QIRC was designed to assess the quality of life of patients who require refractive correction such as spectacles, contact lenses, and refractive surgery.31 It has been proven to be a valid and reliable survey for the assessment of refractive correction-related QOL by Rasch analysis and standard psychometric analysis techniques.31,32 The QIRC covers 20 items that look at visual function, symptoms, convenience, cost, health concerns, and emotional well-being (Table 1). Questions are scored on a 5-category response scale, with evenly spaced descriptions ranging from “not at all’ to “extremely.”31 Responses are converted to Rasch weighted scores to give a true measure of refractive error-related QOL. The Rasch-scaled QIRC score runs on a 0 to 100 scale. A higher QIRC score represents a better quality of life. The results from the QIRC questionnaire can be divided into 2 separate scales, functional (item 1–13) and emotional (item 14–20).
TABLE 1.
The 20 Items in the Quality of Life Impact of Refractive Correction Questionnaire QIRC Questionnaire31
Ang et al's39 study administered the QIRC survey on 25 patients undergoing FS-LASIK and another 25 patients undergoing SMILE at postoperative month 1 and 3. This qualitative study was embedded within a large consecutive case series looking at outcomes of FS-LASIK (688 eyes) and SMILE (172 eyes). It was found that the functional and emotional QIRC scores of LASIK and SMILE patients were not significantly different at postoperative month 1 and 3 (P ≥ 0.054). The QIRC scores are presented graphically in Figure 1, alongside QIRC scores from Klokova et al's47 study.
FIGURE 1.
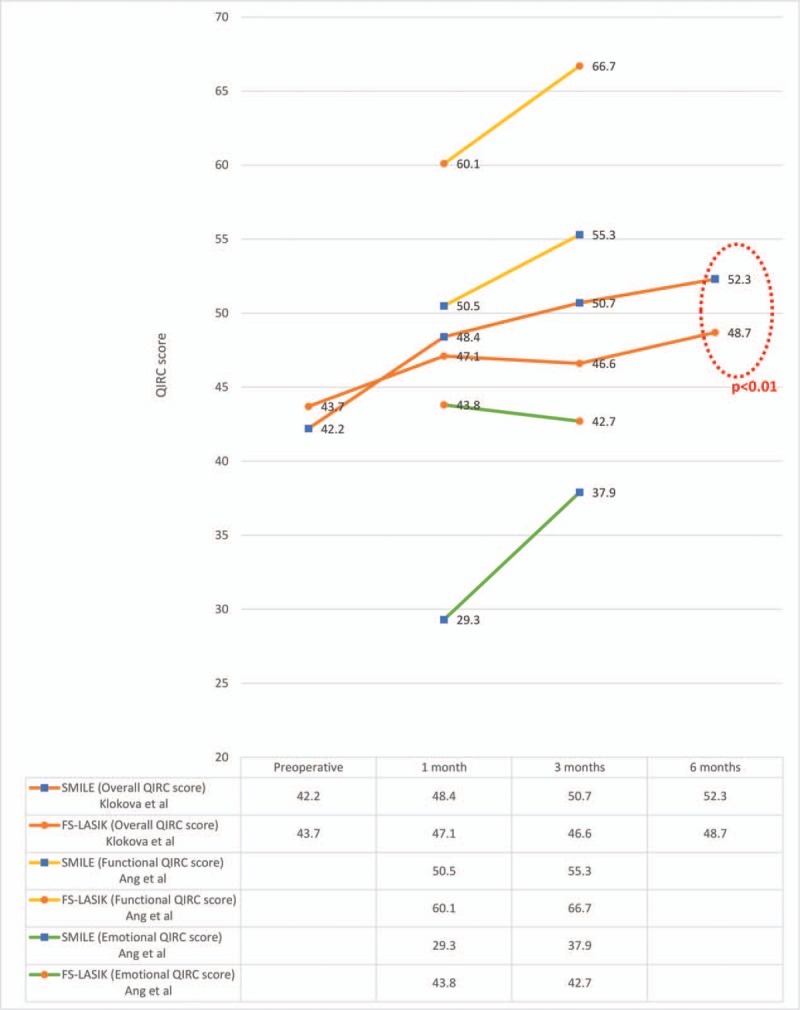
Scores from the QIRC surveys administered by 2 comparative studies looking at patient-reported outcomes in FS-LASIK and SMILE.39,47 Klokova et al showed that at postoperative month 6, patients who underwent SMILE had significantly higher QIRC scores than patients who underwent FS-LASIK. FS-LASIK indicates femtosecond laser-assisted keratomileusis; QIRC, Quality of Life Impact of Refractive Correction; SMILE, small-incision lenticule extraction.
The findings from Ang et al's39 study suggest that vision-related quality of life outcomes are comparable between LASIK and SMILE. However, the study had a few limitations. First, it had a small sample size (25 patients in each arm) and hence might not be adequately powered. Second, it had a limited follow-up period ending at three-month postsurgery. The refractive outcomes of SMILE tend to improve over time22; hence, Ang et al's study might not be representative of the eventual level of satisfaction that patients achieve with SMILE. In fact, Klokova et al's case series47 on SMILE (56 patients) and LASIK (62 patients) showed that at postoperative month 6, patients who underwent SMILE were more satisfied with their visual quality than FS-LASIK patients (overall QIRC score of 48.71 ± 4.77 for FS-LASIK and 52.31 ± 4.45 for SMILE, P < 0.01 Fig. 1). Klokova et al's47 study strength lies in its relatively large sample size and longer follow-up extending to postoperative month 6. However, they reported an overall QIRC score. This is not ideal as it inappropriately combined the functional and emotional aspects of patient reported outcomes, resulting in multidirectionality.
Another case series by Ang et al57 reported that QIRC scores did not differ between low and moderate-high myopes who had undergone SIMLE. This case series, however, did not report on changes in QIRC scores pre- and postoperatively. The current literature on patient-reported outcomes of SMILE and LASIK measured through a validated questionnaire is limited to the above 2 comparative studies.39,47 Several other studies have administered validated questionnaires regarding refractive surgery outcomes on LASIK patients alone, utilizing questionnaires such as the QIRC,48,49 QoV,50 Refractive Status Vision Profile survey,51–53 National Eye Institute Refractive Error Quality of Life Instrument,1,34,38,54,55, NEI VFQ,56 the patient-reported outcomes with LASIK (PROWL) questionnaire,19 Myopia-specific QOL survey,17,52 and others.27 The number of equivalent studies for SMILE is limited as SMILE is a relatively newer procedure.
PATIENT-REPORTED OUTCOME MEASURES IN SMILE AND LASIK: COMPARATIVE STUDIES WITH NONVALIDATED QUESTIONNAIRES
Damgaard et al58 and Ganesh et al59 have attempted to study subjective outcomes in LASIK and SMILE through nonvalidated questionnaires.
Damgaard et al58 conducted a prospective, randomized, paired-eye, single-masked clinical trial comparing outcomes of LASIK and SMILE. 70 patients underwent LASIK in 1 eye and SMILE in the contralateral eye. Questionnaires on the intraoperative experience and postoperative visual symptoms were administered. They observed that patients experienced more blurring after SMILE than LASIK at postoperative month 1 (P = 0.025), but the differences between LASIK and SMILE were no longer significant at postoperative month 3. The various other visual symptoms surveyed (like eye sensitivity, eye discomfort, dryness, tearing, gritty sensation, glare, halos, and fluctuating vision) were scored on a scale of 1 to 6 (1 for not at all to 6 for very severe); these scores were not significantly different between LASIK and SMILE at postoperative month 1 and 3 (P ≥ 0.399).
Ganesh et al's59 prospective randomized study on LASIK (25 patients) and SMILE (25 patients) looked at the objective and subjective postoperative outcomes. Their questionnaire enquired about pain scores on postoperative day 1 (with the Wong-Baker FACES Pain Rating Scale) and the presence of other symptoms such as prickling sensation, watering, redness, and glare (graded on a scale of 0 for glare causing no difficulty to 4 for glare causing severe difficulty) at postoperative day 15. At postoperative day 15, LASIK patients had more complaints of glare than SMILE patients (P < 0.001). Other symptoms surveyed were not significantly different between the 2 groups. Ganesh et al's59 study had a very short follow-up that ended at postoperative day 15; their findings might not be representative of the eventual outcomes of both refractive surgeries. This might explain why glare seemed to be more prominent in their LASIK patients but not in those who participated in Damgaard et al's58 study that surveyed SMILE and LASIK patients at postoperative month 1 and 3. Having said that, it is difficult to draw comparisons between studies that have administered different questionnaires because of nonstandardized scales. For example, the grading scale for glare in Damgaard et al's study ranged from 1 for not at all to 6 for very severe whereas the grading scale for glare in Ganesh et al's study ranged from 0 for glare causing no difficulty to 4 for glare causing severe difficulty. The grading of glare should ideally be scaled against standardized photos, as done in previous questionnaires such as the Patient-Reported Outcomes with LASIK study (PROWL study).19 The use of standardized photos for subjective visual symptoms (eg, glare, halo, starbursts, and diplopia) could be adopted by future questionnaires to evaluate the outcomes of refractive surgeries for more standardized measures.
OTHER PATIENT-REPORTED OUTCOME MEASURES
The refractive outcomes of SMILE tend to improve over time.22 At postoperative month 1, SMILE patients tend to report more concerns about their visual quality as compared with FS-LASIK patients, citing issues with light sensitivity and blurring of vision. However, these concerns resolve as early as postoperative month 3 onwards.39,47,58 This is in keeping with reports that SMILE tends to induce more higher order aberrations in the early postoperative period, but is associated with a reversion back to baseline values after a few months.7,57,59–66 The delay in obtaining the best possible vision after SMILE might be attributed to slower interface healing in SMILE as there is less postoperative inflammation with smaller amounts of laser energy used.67 This theory has been corroborated by animal models.10
Postoperative dry eye is a more prominent problem for LASIK than SMILE. Dry eyes, as measured by objective indicators such as Schirmer test and tear break up time, are worse in patients who had undergone LASIK as compared with those undergone SMILE.8,14,15 Pooled results in meta-analysis also demonstrate that LASIK patients experienced more dry eye symptoms than SMILE patients at postoperative month 6.14 In contradiction, Damgaard et al's58 contralateral eye SMILE and LASIK comparative study reported that the SMILE group tended to experience more visual fluctuations. Having said, it is likely that the visual fluctuations in the SMILE group were from interface irregularities rather than dry eyes. There is yet to be a study comparing subjective dry eye symptoms between LASIK and SMILE patients through a validated questionnaire for dry eye disease such as the Ocular Surface Disease Index.68
There might be demographic variations in patient satisfaction after LASIK and SMILE. Patients with high myopia and astigmatism have been observed to be less satisfied with their outcomes after LASIK as compared with patients with lower preoperative refractive errors.69 However, as mentioned earlier, Ang et al's case series on SMILE patients did not find any significant difference in the quality of life between low- and moderate-high myopes.57 The benefits of SMILE over LASIK for patients with high refractive error have not been conclusively established.64 However, it is possible that the higher laser energy required for LASIK in high myopes results in more inflammation, poorer healing, and hence greater postoperative aberrations. In contrast, the amount of laser energy required in SMILE is comparatively low even when high refractive errors are being corrected.10,11 Nonetheless, with proper preoperative counseling, patient-reported satisfaction after LASIK or SMILE correction for high refractive errors might be independent of the eventual refractive outcome measured objectively. Dissatisfaction often arises from outcomes falling short of expectations; hence, with realistic expectations after preoperative counseling, patients might still be happy with their imperfect visual outcomes. This was clearly demonstrated in McGhee et al's study, which achieved a high level of postLASIK satisfaction among high myopes despite 31.6% of patients failing to achieve an uncorrected vision of 6/12 or better.17
The intraoperative experience is an important component to look at when comparing patient experiences for LASIK and SMILE. This has only been investigated by a couple of studies.28,29,39,58 These studies were all from the same group based in Singapore and employed the same questionnaire enquiring about the intraoperative experience during each stage of the LASIK28,29 and/or SMILE39,58, specifically vision blackout, ability to fixate, pain scores (score of 0–10), and level of fear (score of 0–6).28,29,58 In Damgaard et al's58 paired-eye comparative study of LASIK and SMILE, patients gave the highest fear scores for the excimer laser ablation stage in LASIK (mean score of 3.8 of 6). The docking stage during LASIK received a higher fear score than the equivalent stage in SMILE (P = 0.024), but fear scores were not significantly different between both procedures for the other stages of surgery. The average discomfort score was higher during tissue manipulation in SMILE than flap lifting in LASIK (P = 0.02), meanwhile discomfort scores for the other stages of the surgery (docking, vacuum application, and laser application) were not significantly different between LASIK and SMILE (P ≥ 0.249). The authors postulated that the inadvertent forced eye movements during SMILE lenticule dissection might have induced more discomfort than the simple lifting of the LASIK flap. Hence, surgeons with limited experience with SMILE might want to consider administering more topical anesthesia, prescribing anxiolytics, or sedatives before surgery. In contrast, Ang et al's39 comparative study reported that LASIK patients were more fearful than the SMILE patients in the initial stages of the procedure such as suction (P = 0.015), flap cutting (P = 0.001), and flap lifting (P = 0.035). The authors postulated the mental imagery of a flap creation as opposed to a small-incision made during SMILE might have accounted for more fear experienced amongst LASIK patients. However Ang et al's39 study was not a paired-eye study; hence, inter-patient variation in symptom reporting might be a potential source of bias.
Several studies have looked at global patient satisfaction through a linear grading scale for LASIK19,26,27,59,67,70–72 and SMILE23,24,59. Solomon et al73 conducted a review on LASIK satisfaction scores reported by peer-reviewed articles published from 1988 to 2008. Their review concluded that collectively, only 4.6% of patients (101/2198 subjects) were dissatisfied with their LASIK surgery.73 Studies included in this review employed arbitrary linear grading scales for patient satisfaction. For example, Ganesh et al's59 randomized comparative study on LASIK and SMILE measured patient satisfaction score on a scale of 1 (excellent) to 4 (poor). The overall satisfaction score was not significantly different between their group of LASIK and SMILE patients (2.56 ± 0.5 and 2.62 ± 0.49 in the LASIK and SMILE groups, respectively). This result, however, does not translate into a meaningful finding due to the nonstandardized arbitrary scoring system used and comparisons cannot be made against other studies. Global satisfaction scores also provide limited information on the reasons for dissatisfaction, be it physical, emotional, psychological, or financial concerns. As such global satisfaction scores are not very useful in illustrating differences in patient-reported outcomes in LASIK and SMILE.
CURRENT LIMITATIONS
Qualitative studies on patient-reported outcomes are an important aspect of refractive surgery research. Newer psychometric analysis techniques, such as Rasch analysis, might facilitate the development of questionnaires that better illicit these subjective outcomes. Well-designed questionnaires for qualitative outcomes are still bound by several limitations. First, subjective outcomes might seem artificially good because of the Hawthorne effect wherein patients feel obliged to give “socially desirable” responses in an effort to maintain good patient–doctor relationship.74 Second, there may be sampling bias as patients who are satisfied are more likely to participate in a survey. Third, innate questionnaire response biases of individuals might not be sufficiently addressed by randomization. Some studies circumvent this issue by implementing paired-eye interventions (eg, 1 eye undergoes LASIK and other eye undergoes SMILE).58 Fourth, even if standardized questionnaires are used, there can be significant heterogeneity in the methodology across studies. This makes direct comparisons among studies difficult. Next, qualitative questionnaires should be contextualized for the local population being studied and results should be interpreted with knowledge that some populations may “catastrophise” mild symptoms due to cultural and ethnic differences.75 Lastly, and most importantly, existing studies have relatively short durations of follow-up. Most have a postoperative follow-up duration of ≤6 months.19,28,39,47,55,58,59 The Wills Eye Institute published a report on dissatisfied post-LASIK patients.76 They noted that majority (66%) of dissatisfied patients presented > 6 months after their LASIK procedure.76 This highlights the importance of longer-term follow-up for a comprehensive evaluation of patient-reported outcomes. This is particularly relevant to SMILE as many of its theoretical benefits such as the avoidance of flap-related complications and better biomechanics might only become apparent years after surgery.
CONCLUSIONS
In conclusion, the available literature suggests that LASIK and SMILE deliver relatively comparable subjective outcomes and patient satisfaction. There is some evidence suggesting that SMILE might even confer a better vision-related quality of life in the late postoperative period. However, the existing studies have methodological limitations. More studies utilizing standardized validated questionnaires for patient-reported outcome measures are required. Future studies should also aim for longer durations of follow-up for a more comprehensive understanding of the patient's experience. A better understanding of these patient-reported outcome measures will in turn benefit future patients seeking refractive surgery.
Supplementary Material
Footnotes
The authors do not have any conflicts of interest to disclose.
REFERENCES
- 1.Nichols JJ, Twa MD, Mitchell GL. Sensitivity of the National Eye Institute Refractive Error Quality of Life instrument to refractive surgery outcomes. J Cataract Refract Surg 2005; 31:2313–2318. [DOI] [PubMed] [Google Scholar]
- 2.Kandel H, Khadka J, Lundstrom M, Goggin M, Pesudovs K. Questionnaires for measuring refractive surgery outcomes. J Refrac Surg 2017; 33:416–424. [DOI] [PubMed] [Google Scholar]
- 3.Sugar A. Ultrafast (femtosecond) laser refractive surgery. Curr Opin Ophthalmol 2002; 13 (4):246–249. [DOI] [PubMed] [Google Scholar]
- 4.Chen S, Feng Y, Stojanovic A, Jankov MR, 2nd, Wang Q. IntraLase femtosecond laser vs mechanical microkeratomes in LASIK for myopia: a systematic review and meta-analysis. J Refract Surg 2012; 28 (1):15–24. [DOI] [PubMed] [Google Scholar]
- 5.Sekundo W, Kunert K, Russmann C, et al. First efficacy and safety study of femtosecond lenticule extraction for the correction of myopia: six-month results. J Cataract Refract Surg 2008; 34:1513–1520. [DOI] [PubMed] [Google Scholar]
- 6.Blum M, Kunert K, Schroder M, Sekundo W. Femtosecond lenticule extraction for the correction of myopia: preliminary 6-month results. Graefes Arch Clin Exp Ophthalmol 2010; 248:1019–1027. [DOI] [PubMed] [Google Scholar]
- 7.Shah R, Shah S, Sengupta S. Results of small incision lenticule extraction: all-in-one femtosecond laser refractive surgery. J Cataract Refract Surg 2011; 37:127–137. [DOI] [PubMed] [Google Scholar]
- 8.Zhang Y, Shen Q, Jia Y, Zhou D, Zhou J. Clinical outcomes of SMILE and FS-LASIK used to treat myopia: a meta-analysis. J Refract Surg 2016; 32:256–265. [DOI] [PubMed] [Google Scholar]
- 9.Shah R, Shah S. Effect of scanning patterns on the results of femtosecond laser lenticule extraction refractive surgery. J Cataract Refract Surg 2011; 37:1636–1647. [DOI] [PubMed] [Google Scholar]
- 10.Riau AK, Angunawela RI, Chaurasia SS, Lee WS, Tan DT, Mehta JS. Early corneal wound healing and inflammatory responses after refractive lenticule extraction (ReLEx). Invest Ophthalmol Visual Sci 2011; 52:6213–6221. [DOI] [PubMed] [Google Scholar]
- 11.Kim TI, Del Barrio JLA, Wilkins M, Cochener B, Ang M. Refractive surgery. Lancet 2019; 393:2085–2098. [DOI] [PubMed] [Google Scholar]
- 12.Vestergaard A, Ivarsen A, Asp S, Hjortdal JO. Femtosecond (FS) laser vision correction procedure for moderate to high myopia: a prospective study of ReLEx((R)) flex and comparison with a retrospective study of FS-laser in situ keratomileusis. Acta Ophthalmol 2013; 91:355–362. [DOI] [PubMed] [Google Scholar]
- 13.Mohamed-Noriega K, Toh KP, Poh R, et al. Cornea lenticule viability and structural integrity after refractive lenticule extraction (ReLEx) and cryopreservation. Mol Vision 2011; 17:3437–3449. [PMC free article] [PubMed] [Google Scholar]
- 14.Shen Z, Shi K, Yu Y, Yu X, Lin Y, Yao K. Small Incision Lenticule Extraction (SMILE) versus Femtosecond Laser-Assisted In Situ Keratomileusis (FS-LASIK) for myopia: a systematic review and meta-analysis. PLoS One 2016; 11:e0158176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee JK, Chuck RS, Park CY. Femtosecond laser refractive surgery: small-incision lenticule extraction vs. femtosecond laser-assisted LASIK. Curr Opin Ophthalmol 2015; 26 (4):260–264. [DOI] [PubMed] [Google Scholar]
- 16.Jabbur NS, Kraff C, Visx Wavefront Study G. Wavefront-guided laser in situ keratomileusis using the WaveScan system for correction of low to moderate myopia with astigmatism: 6-month results in 277 eyes. J Cataract Refract Surg 2005; 31:1493–1501. [DOI] [PubMed] [Google Scholar]
- 17.McGhee CN, Craig JP, Sachdev N, Weed KH, Brown AD. Functional, psychological, and satisfaction outcomes of laser in situ keratomileusis for high myopia. J Cataract Refract Surg 2000; 26:497–509. [DOI] [PubMed] [Google Scholar]
- 18.Hammond SD, Jr, Puri AK, Ambati BK. Quality of vision and patient satisfaction after LASIK. Curr Opin Ophthalmol 2004; 15:328–332. [DOI] [PubMed] [Google Scholar]
- 19.Eydelman M, Hilmantel G, Tarver ME, Hofmeister EM, May J, Hammel K, et al. Symptoms and Satisfaction of Patients in the Patient-Reported Outcomes With Laser In Situ Keratomileusis (PROWL) Studies. JAMA Ophthalmol 2017; 135:13–22. [DOI] [PubMed] [Google Scholar]
- 20.Buhren J, Martin T, Kuhne A, Kohnen T. Correlation of aberrometry, contrast sensitivity, and subjective symptoms with quality of vision after LASIK. J Refract Surg 2009; 25:559–568. [DOI] [PubMed] [Google Scholar]
- 21.McLeod SD. Beyond snellen acuity: the assessment of visual function after refractive surgery. Arch Ophthalmol 2001; 119:1371–1373. [DOI] [PubMed] [Google Scholar]
- 22.Ivarsen A, Asp S, Hjortdal J. Safety and complications of more than 1500 small-incision lenticule extraction procedures. Ophthalmology 2014; 121:822–828. [DOI] [PubMed] [Google Scholar]
- 23.Sekundo W, Kunert KS, Blum M. Small incision corneal refractive surgery using the small incision lenticule extraction (SMILE) procedure for the correction of myopia and myopic astigmatism: results of a 6 month prospective study. Br J Ophthalmol 2011; 95:335–339. [DOI] [PubMed] [Google Scholar]
- 24.Vestergaard A, Ivarsen AR, Asp S, Hjortdal JO. Small-incision lenticule extraction for moderate to high myopia: Predictability, safety, and patient satisfaction. J Cataract Refract Surg 2012; 38:2003–2010. [DOI] [PubMed] [Google Scholar]
- 25.Brown MC, Schallhorn SC, Hettinger KA, Malady SE. Satisfaction of 13,655 patients with laser vision correction at 1 month after surgery. J Refract Surg 2009; 25 (7 suppl):S642–S646. [DOI] [PubMed] [Google Scholar]
- 26.Tuan KM. Visual experience and patient satisfaction with wavefront-guided laser in situ keratomileusis. J Cataract Refract Surg 2006; 32:577–583. [DOI] [PubMed] [Google Scholar]
- 27.Tahzib NG, Bootsma SJ, Eggink FA, Nabar VA, Nuijts RM. Functional outcomes and patient satisfaction after laser in situ keratomileusis for correction of myopia. J Cataract Refract Surg 2005; 31:1943–1951. [DOI] [PubMed] [Google Scholar]
- 28.Hall RC, Rosman M, Chan C, Tan DT, Mehta JS. Patient and surgeon experience during laser in situ keratomileusis using 2 femtosecond laser systems. J Cataract Refract Surg 2014; 40:423–429. [DOI] [PubMed] [Google Scholar]
- 29.Tan CS, Au Eong KG, Lee HM. Visual experiences during different stages of LASIK: Zyoptix XP microkeratome vs Intralase femtosecond laser. Am J Ophthalmol 2007; 143:90–96. [DOI] [PubMed] [Google Scholar]
- 30.Gnanasakthy A, Mordin M, Clark M, DeMuro C, Fehnel S, Copley-Merriman C. A review of patient-reported outcome labels in the United States: 2006 to 2010. Value Health 2012; 15:437–442. [DOI] [PubMed] [Google Scholar]
- 31.Pesudovs K, Garamendi E, Elliott DB. The Quality of Life Impact of Refractive Correction (QIRC) Questionnaire: development and validation. Optom Vis Sci 2004; 81:769–777. [DOI] [PubMed] [Google Scholar]
- 32.Khadka J, McAlinden C, Pesudovs K. Quality assessment of ophthalmic questionnaires: review and recommendations. Optometry Vis Sci 2013; 90:720–744. [DOI] [PubMed] [Google Scholar]
- 33.Petrillo J, Cano SJ, McLeod LD, Coon CD. Using classical test theory, item response theory, and Rasch measurement theory to evaluate patient-reported outcome measures: a comparison of worked examples. Value Health 2015; 18 (1):25–34. [DOI] [PubMed] [Google Scholar]
- 34.Nehls SM, Ghoghawala SY, Hwang FS, Azari AA. Patient satisfaction and clinical outcomes with laser refractive surgery performed by surgeons in training. J Cataract Refract Surg 2014; 40:1131–1138. [DOI] [PubMed] [Google Scholar]
- 35.Kandel H, Khadka J, Goggin M, Pesudovs K. Patient-reported outcomes for assessment of quality of life in refractive error: a systematic review. Optometry Vis Sci 2017; 94:1102–1119. [DOI] [PubMed] [Google Scholar]
- 36.Ryan A, Hartnett C, Lanigan B, O’Keefe M. Foldable iris-fixated intraocular lens implantation in children. Acta Ophthalmol 2012; 90:e458–e462. [DOI] [PubMed] [Google Scholar]
- 37.Gundersen KG, Potvin R. Comparison of visual outcomes after implantation of diffractive trifocal toric intraocular lens and a diffractive apodized bifocal toric intraocular lens. Clin Ophthalmol 2016; 10:455–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schmidt GW, Yoon M, McGwin G, Lee PP, McLeod SD. Evaluation of the relationship between ablation diameter, pupil size, and visual function with vision-specific quality-of-life measures after laser in situ keratomileusis. Arch Ophthalmol 2007; 125:1037–1042. [DOI] [PubMed] [Google Scholar]
- 39.Ang M, Ho H, Fenwick E, et al. Vision-related quality of life and visual outcomes after small-incision lenticule extraction and laser in situ keratomileusis. J Cataract Refract Surg 2015; 41:2136–2144. [DOI] [PubMed] [Google Scholar]
- 40.Maurino V, Allan BD, Rubin GS, et al. Quality of vision after bilateral multifocal intraocular lens implantation: a randomized trial–AT LISA 809 M versus AcrySof ReSTOR SN6AD1. Ophthalmology 2015; 122:700–710. [DOI] [PubMed] [Google Scholar]
- 41.McAlinden C, Pesudovs K, Moore JE. The development of an instrument to measure quality of vision: the Quality of Vision (QoV) questionnaire. Invest Ophthalmol Vis Sci 2010; 51:5537–5545. [DOI] [PubMed] [Google Scholar]
- 42.Huang JC, Sun CC, Chang CK, Ma DH, Lin YF. Effect of hinge position on corneal sensation and dry eye parameters after femtosecond laser-assisted LASIK. J Refract Surg 2012; 28:625–631. [DOI] [PubMed] [Google Scholar]
- 43.Pesudovs K, Garamendi E, Keeves JP, Elliott DB. The Activities of Daily Vision Scale for cataract surgery outcomes: re-evaluating validity with Rasch analysis. Invest Ophthalmol Vis Scis 2003; 44:2892–2899. [DOI] [PubMed] [Google Scholar]
- 44.Bond TG, Fox CM. Applying the Rasch Model. Fundamental Measurements in the Human Sciences Erlbaum, 2nd ed.Mahwah, NJ:2007. [Google Scholar]
- 45.Tuisku IS, Lindbohm N, Wilson SE, Tervo TM. Dry eye and corneal sensitivity after high myopic LASIK. J Refract Surg 2007; 23:338–342. [DOI] [PubMed] [Google Scholar]
- 46.Shams N, Mobaraki H, Kamali M, Jafarzadehpour E. Comparison of quality of life between myopic patients with spectacles and contact lenses, and patients who have undergone refractive surgery. J Curr Ophthalmol 2015; 27:32–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Klokova OA, Sakhnov SN, Geydenrikh MS, Damashauskas RO. Quality of life after refractive surgery: ReLEx SMILE vs Femto-LASIK. Clin Ophthalmol 2019; 13:561–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pesudovs K, Garamendi E, Elliott DB. A quality of life comparison of people wearing spectacles or contact lenses or having undergone refractive surgery. J Refract Surg 2006; 22:19–27. [DOI] [PubMed] [Google Scholar]
- 49.Garamendi E, Pesudovs K, Elliott DB. Changes in quality of life after laser in situ keratomileusis for myopia. J Cataract Refract Surg 2005; 31:1537–1543. [DOI] [PubMed] [Google Scholar]
- 50.Luger MH, McAlinden C, Buckhurst PJ, Wolffsohn JS, Verma S, Arba Mosquera S. Presbyopic LASIK using hybrid bi-aspheric micro-monovision ablation profile for presbyopic corneal treatments. Am J Ophthalmol 2015; 160:493–505. [DOI] [PubMed] [Google Scholar]
- 51.Schein OD, Vitale S, Cassard SD, Steinberg EP. Patient outcomes of refractive surgery. The refractive status and vision profile. J Cataract Refract Surg 2001; 27:665–673. [DOI] [PubMed] [Google Scholar]
- 52.Lee J, Lee J, Park K, Cho W, Kim JY, Kang HY. Assessing the value of laser in situ keratomileusis by patient-reported outcomes using quality of life assessment. J Refract Surg 2005; 21:59–71. [DOI] [PubMed] [Google Scholar]
- 53.Waring G, Dougherty PJ, Chayet A, et al. Topographically guided LASIK for myopia using the Nidek CXII customized aspheric treatment zone (CATz). Trans Am Ophthalmol Soc 2007; 105:240–246. discussion 7-8. [PMC free article] [PubMed] [Google Scholar]
- 54.McDonnell PJ, Mangione C, Lee P, et al. Responsiveness of the National Eye Institute Refractive Error Quality of Life instrument to surgical correction of refractive error. Ophthalmology 2003; 110:2302–2309. [DOI] [PubMed] [Google Scholar]
- 55.Sia RK, Ryan DS, Rivers BA, et al. Vision-related quality of life and perception of military readiness and capabilities following refractive surgery among active duty U.S. military service members. J Refract Surg 2018; 34:597–603. [DOI] [PubMed] [Google Scholar]
- 56.Pesudovs K, Gothwal VK, Wright T, Lamoureux EL. Remediating serious flaws in the National Eye Institute Visual Function Questionnaire. J Cataract Refract Surg 2010; 36:718–732. [DOI] [PubMed] [Google Scholar]
- 57.Ang M, Farook M, Htoon HM, Tan D, Mehta JS. Simulated night vision after small-incision lenticule extraction. J Cataract Refract Surg 2016; 42:1173–1180. [DOI] [PubMed] [Google Scholar]
- 58.Damgaard IB, Ang M, Farook M, Htoon HM, Mehta JS. Intraoperative patient experience and postoperative visual quality after SMILE and LASIK in a randomized, paired-eye, controlled study. Journal of refractive surgery 2018; 34:92–99. [DOI] [PubMed] [Google Scholar]
- 59.Ganesh S, Gupta R. Comparison of visual and refractive outcomes following femtosecond laser- assisted lasik with smile in patients with myopia or myopic astigmatism. J Refract Surg 2014; 30:590–596. [DOI] [PubMed] [Google Scholar]
- 60.Chen X, Wang Y, Zhang J, Yang SN, Li X, Zhang L. Comparison of ocular higher-order aberrations after SMILE and Wavefront-guided Femtosecond LASIK for myopia. BMC Ophthalmol 2017; 17:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tan DK, Tay WT, Chan C, Tan DT, Mehta JS. Postoperative ocular higher-order aberrations and contrast sensitivity: femtosecond lenticule extraction versus pseudo small-incision lenticule extraction. J Cataract Refract Surg 2015; 41:623–634. [DOI] [PubMed] [Google Scholar]
- 62.Khalifa MA, Ghoneim A, Shafik Shaheen M, Aly MG, Pinero DP. Comparative analysis of the clinical outcomes of SMILE and wavefront-guided LASIK in low and moderate myopia. J Refract Surg 2017; 33:298–304. [DOI] [PubMed] [Google Scholar]
- 63.Li M, Zhao J, Miao H, et al. Mild decentration measured by a Scheimpflug camera and its impact on visual quality following SMILE in the early learning curve. Invest Ophthalmol Vis Sci 2014; 55:3886–3892. [DOI] [PubMed] [Google Scholar]
- 64.Xia LK, Ma J, Liu HN, Shi C, Huang Q. Three-year results of small incision lenticule extraction and wavefront-guided femtosecond laser-assisted laser in situ keratomileusis for correction of high myopia and myopic astigmatism. Int J Ophthalmol 2018; 11:470–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pinero DP, Teus MA. Clinical outcomes of small-incision lenticule extraction and femtosecond laser-assisted wavefront-guided laser in situ keratomileusis. J Cataract Refract Surg 2016; 42:1078–1093. [DOI] [PubMed] [Google Scholar]
- 66.Liu M, Chen Y, Wang D, et al. Clinical outcomes after SMILE and femtosecond laser-assisted LASIK for myopia and myopic astigmatism: a prospective randomized comparative study. Cornea 2016; 35:210–216. [DOI] [PubMed] [Google Scholar]
- 67.Bailey MD, Mitchell GL, Dhaliwal DK, Boxer Wachler BS, Zadnik K. Patient satisfaction and visual symptoms after laser in situ keratomileusis. Ophthalmology 2003; 110:1371–1378. [DOI] [PubMed] [Google Scholar]
- 68.Schiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL. Reliability and validity of the Ocular Surface Disease Index. Arch Ophthalmol 2000; 118:615–621. [DOI] [PubMed] [Google Scholar]
- 69.Knorz MC, Wiesinger B, Liermann A, Seiberth V, Liesenhoff H. Laser in situ keratomileusis for moderate and high myopia and myopic astigmatism. Ophthalmology 1998; 105:932–940. [DOI] [PubMed] [Google Scholar]
- 70.Price MO, Price DA, Bucci FA, Jr, Durrie DS, Bond WI, Price FW., Jr Three-year longitudinal survey comparing visual satisfaction with LASIK and contact lenses. Ophthalmology 2016; 123:1659–1666. [DOI] [PubMed] [Google Scholar]
- 71.Hashmani S, Hashmani N, Rajani H, et al. Comparison of visual acuity, refractive outcomes, and satisfaction between LASIK performed with a microkeratome and a femto laser. Clin Ophthalmol 2017; 11:1009–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lazon de la Jara P, Erickson D, Erickson P, Stapleton F. Visual and non-visual factors associated with patient satisfaction and quality of life in LASIK. Eye 2011; 25:1194–1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Solomon KD, Fernandez de Castro LE, Sandoval HP, et al. LASIK world literature review: quality of life and patient satisfaction. Ophthalmology 2009; 116:691–701. [DOI] [PubMed] [Google Scholar]
- 74.Salomao MQ, Ambrosio R, Jr, Wilson SE. Dry eye associated with laser in situ keratomileusis: Mechanical microkeratome versus femtosecond laser. J Cataract Refract Surg 2009; 35:1756–1760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Patel S, Felix ER, Levitt RC, Sarantopoulos CD, Galor A. Dysfunctional coping mechanisms contribute to dry eye symptoms. J Clin Med 2019; 8:E901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Levinson BA, Rapuano CJ, Cohen EJ, Hammersmith KM, Ayres BD, Laibson PR. Referrals to the Wills Eye Institute Cornea Service after laser in situ keratomileusis: reasons for patient dissatisfaction. J Cataract Refract Surg 2008; 34:32–39. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


