Abstract
Background
The ultrasonography-guided technique is superior to the traditional palpation technique for artery cannulation. However, considering the complexity of assembling the ultrasonography machine, this technique has not been extensively used. Here, we compared the ultrasonography-guided technique with the traditional palpation technique in adult patients in the pre-anesthesia room.
Material/Methods
A total of 66 patients were enrolled and divided into 2 groups: the ultrasonography group and the palpation group. Anesthesiologists then cannulated the radial artery via either method. The primary outcomes included the first-attempt success and total success rates, as well as the cannulation duration and total procedure duration. The secondary outcome was the rate of complications attributable to cannulation.
Results
Overall, 60 patients were analyzed in the present study. The first-attempt success rate in the ultrasonography group (96.6%) was significantly higher than that in the palpation group (73.3%; P=0.03). There was no significant difference in the cannulation duration and the total procedure duration between the 2 groups. The rate of complications caused by cannulation in 2 groups was similar.
Conclusions
The ultrasonography-guided radial artery cannulation technique is more efficient for arterial cannulation in the pre-anesthesia room compared with the traditional palpation method.
MeSH Keywords: Arteries, Catheterization, Ultrasonography
Background
Blood pressure monitoring is necessary for monitoring patients who are undergoing major surgery or for those in critical condition. The radial artery is commonly used because it has a superficial course, has a low risk of complications, and the hand has a dual blood supply [1–3]. However, in some patients the convergence time needs to be extended for difficult catheterization, and this delays the surgery procedure. In recent years, several studies have suggested that ultrasonography-guided radial artery catheterization can increase the first-attempt success rate for cannula insertion while decreasing the total procedure duration and the incidence of complications attributable to cannulation in adult patients, particularly in extremely challenging patients and neonates [4–12]. However, some authors have raised concerns regarding the benefits of the ultrasonography-guided technique in radial artery cannulation and the potential increase in risk of infection at the puncture site [13]. Moreover, some hospitals have fewer ultrasonography machines than operation rooms; therefore, machine assembly may require additional time. Owing to this concern, numerous operators prefer the traditional palpation technique to the ultrasonography-guided technique. The First Affiliated Hospital of Anhui Medical University has a pre-anesthesia room in which anesthesiologists can perform arterial catheterization before patients are transferred to the operating room. Hence, the purpose of this study was to investigate the efficacy of ultrasonography-guided radial artery cannulation in the pre-anesthesia room.
Material and Methods
The present study was approved by the Ethics Committee of the First Affiliated Hospital of Anhui Medical University. This study was registered at the Chinese Clinical Trial Registry with the registration number ChiCTR1800014828. Written informed consent was obtained from all patients who participated in this study.
We enrolled adult patients (ages 18–90 years) undergoing an elective surgical procedure from October 2018 to December 2018 who required continuous invasive arterial blood pressure monitoring as determined by the attending anesthesiologist. We excluded patients in shock, those who had a positive Allen test result, those who were unconscious, and those who had an ASA classification of ≥IV, and patients who had received radial artery cannulation within the previous 30 days. Moreover, patients whose catheter retention time was >6 h were also excluded. All patients were randomized to either the ultrasonography-guided group or the palpation group. A total of 62 patients were enrolled in the present study; 2 were excluded because their catheter retention time was >6 h. Overall, 60 patients were included in the final analysis (Figure 1).
Figure 1.
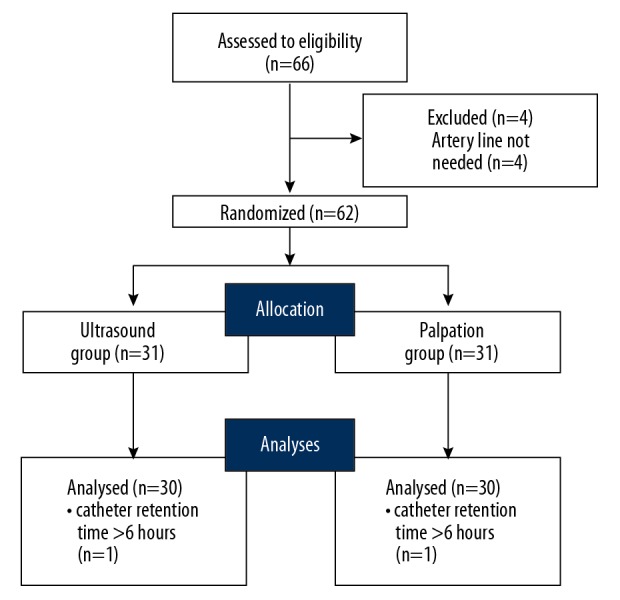
A flow diagram as per the consolidated standards of randomized controlled trial. Ultrasonography group=group for which ultrasonography-guided radial artery cannulation was performed. Palpation group=group for which the traditional palpation technique was used for radial artery cannulation.
The ultrasonography machine (Fujifilm, Sonosite, Inc., Bothell. WA) was prepared, and the depth was set at 1.8–2.2 cm by a technician before the patient was sent to the pre-anesthesia room. Electrocardiography, pulse oximetry, and non-invasive blood pressure measurements were performed. The left hand was chosen unless the surgeon or attending anesthesiologist requested use of the right hand.
The 2 operators were resident anesthesiologists (had finished 3 years of Chinese standard training for residents) who were trained in arterial cannulation using ultrasonography or palpation and had performed the procedure at least 30 or 200 times, respectively. The technique used in certain patients was chosen via a sealed envelope. All the cannulation procedures were performed using a 20-G catheter (Braun Company, Melsungen, Germany). Sterile techniques were used, including the use of sterile gloves, operating towels, and ultrasound probe covers; the wrist was prepped with ChloraPrep 2%. The patient’s arm was placed slightly extended with a small roll placed under the wrist before sterilization. Local anesthesia was administered with lidocaine 2% (Zhaohui Company, Shanghai, China) at the puncture site.
When the trolley that transferred the patient reached the pre-anesthesia room, a timer was started, and when the patient was prepared to be transferred to the operating room, the timer was stopped; this duration was marked as the total procedure duration (T1). Another timer was started when the ultrasonography scanning and palpation of the patient’s prepped wrist was started in the ultrasonography and palpation groups, respectively. The timer was stopped when the blood could be pumped smoothly back with a syringe connected to the catheter. This duration was recorded as the cannulation duration (T2). If T1 was >15 min or T2 was >5 min, the operator was allowed to use any technique to cannulate. In such circumstances, the T1 and T2 were recorded as 900 s or 300 s, respectively. First-attempt success was defined as the successful insertion of the tube into the artery after 1 pass through the skin with the needle. Patients were followed up 1 day after the operation to observe whether the cannulation site was infected or showed the presence of hematomas. Infection was defined as inflammation at the cannulation site 48 h after removing the catheter. We collected the following data for analyses: sex, age, weight, and blood pressure (obtained noninvasively).
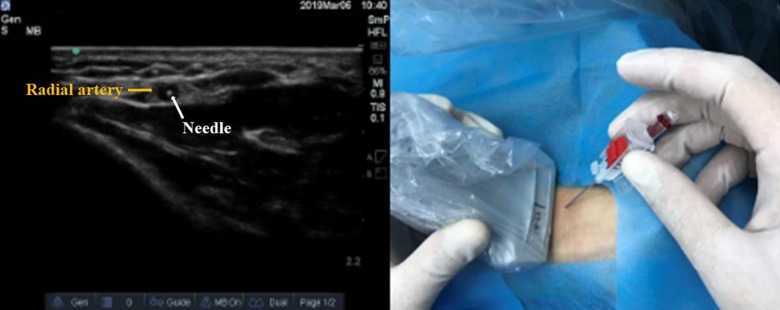
In the ultrasonography group, the operator performed the cannulation using the technique introduced by Kiberenge et al. – the dynamic needle tip positioning (DNTP) technique [2]. A short axis out-of-plane view of the radial artery was obtained using the ultrasonography machine with a high-frequency probe (5–13 MHz). The probe was moved to obtain the image of the radial artery in the center of the ultrasonography screen; thereafter, the middle of the probe was chosen as the puncture site (Figure 2). The needle and the catheter were moved forward until the hyperechoic dot was observed on the ultrasonography image. The probe was then moved to the radial artery in the proximal direction until the hyperechoic dot disappeared. Maintaining a stable position for the probe, the needle and the catheter were advanced a few millimeters until the hyperechoic dot was observed again. These steps were repeated until the hyperechoic dot could be observed in the lumen of the radial artery (Figure 3). The tilting of the probe can optimize the image in cases in which the artery or the needle cannot be clearly observed on the screen.
Figure 2.
Radial artery observed under ultrasonographic guidance. The radial artery is visible on the ultrasonography screen, and the radial artery was punctured 1 cm away from the middle position of the probe. The yellow arrow indicates the radial artery.
Figure 3.
Radial artery cannulation under ultrasonographic guidance. The blood flooded back from the needle, and the needle is visible in the middle of the vessel lumen. The yellow arrow indicates the radial artery and the white arrow indicates the tip of the needle.
In the palpation group, the operator chose the puncture site by palpating the radial artery. The needle and catheter were advanced toward the radial artery until a flash-back of blood was observed. The catheter was inserted using the Seldinger technique.
Statistical analyses
The sample size was calculated based on data from a previous study [4]; a study population of at least 28 patients for each group was needed to produce statistical power ≥90%, with α=0.05 (two-tailed), based on 48% incidence of shivering in the palpation group and 83% in the ultrasonography-guided group. In this study, 66 patients were enrolled to increase the power.
Statistical analyses were conducted using SPSS (version 25.0; IBM Corp.). Parametric data (cannulation duration and total procedure duration) were analyzed using the Kolmogorov-Smirnov test and the t test, whereas non-parametric data (first-attempt success rate, total success rate, and rate of complications) were analyzed using the Pearson χ2 test. The effect sizes of the standardized differences in the patients’ baseline characteristics of sex, age, and pre-cannulation blood pressure were analyzed. P<0.05 was considered significant.
Results
Overall, 62 patients were enrolled in the study, with 31 patients in each group. The basic characteristics are shown in Table 1. Two patients were excluded because their catheter retention time was >6 h. Therefore, 60 patients were analyzed. There were no significant differences between groups in baseline characteristics (Table 1).
Table 1.
Patient characteristics and details.
| Ultrasound group (n=30) | Palpation group (n=30) | P value | |
|---|---|---|---|
| Age (years) | 58.83±14.65 | 54.57±13.44 | .245 |
| Weight (kg) | 75.60±32.82 | 63.90±9.20 | .053 |
| Height (cm) | 154.07±31.10 | 165.43±5.04 | .065 |
| Systolic blood pressure (mmHg) | 133.70±14.20 | 133.53±12.53 | .962 |
| Diastolic blood pressure (mmHg) | 75.43±6.61 | 75.07±6.11 | .824 |
| Sex (Male/Female) | 17/13 | 16/14 | .795 |
| The length of catheter retention time (seconds) | 182.20±37.4 | 167.37±28.05 | .09 |
Date are expressed as mean ± standard deviation or n(%) values. No significant differences are observed between the 2 groups in any baseline characteristic.
Primary outcomes
The first-attempt success rate in the ultrasonography group (96.6%) was significantly higher than that in the palpation group (73.3%, P=0.03). There was no significant difference in the total success rate between the ultrasonography group (100%) and the palpation group (93.3%). No significant differences were observed in the total procedure duration and cannulation duration in the 2 groups (Table 2).
Table 2.
Arterial cannulation characteristics.
| Ultrasound group (n=30) | Palpation group (n=30) | P | |
|---|---|---|---|
| First Attempt success rate | 29 (96.6) | 22 (73.3) | .03* |
| Total success rate | 30 (100.0) | 28 (93.3) | .47 |
| Cannulation time (seconds) | 44.2±28.2 | 71.2±83.3 | .10 |
| Total time (seconds) | 542.5±26.8 | 580.0±122.7 | .11 |
| Hematoma | 0 | 2 (.07) | .472 |
| Infection | 0 | 0 | – |
Date are expressed as mean ± standard deviation or n(%) values.
P<0.05.
The first-attempt success rate in the ultrasonography group was significantly higher than that in the palpation group. No significant differences between the 2 groups were observed in the total success rate, total procedure duration, cannulation duration, or rate of complications caused by cannulation.
Secondary outcomes
Local hematoma occurred in 2 patients in the palpation group and in none of the patients the ultrasonography group (P=0.472; Table 2). No case of infection was observed in either group.
Discussion
The present study demonstrates that the use of the DNTP-ultrasonographic technique can provide a higher first-attempt success rate for radial artery cannulation without extending the cannulation duration and total procedure duration. Our result is similar to those of previous reports [4].
Ultrasonography-guided arterial cannulation is performed using either the long axis/in-plane method or the short axis/out-plane method; most operators prefer the out-plane method [14–16]. The out-plane method was used in this study. Clemmesen et al. [17] reported the first attempt of using DNTP–ultrasonographic technique for peripheral vascular access in 2012; they reported a success rate of 97%. Kiberenge et al. reported a first-attempt success rate of 83% in their study [4]. The main reason for cannulation failure in traditional palpation technique is not puncturing the needle into the artery but rather cannulating the catheter into the artery vessel. The reason for the higher first-attempt success rate (73%) observed in our study compared with that in previous studies is that the operators chose the through-and-through technique in the palpation group. Using ultrasonography, the pinpoint of the needle tip can be detected at any moment during the procedure; therefore, the catheter can directly cannulate into the vessel. The cannulation duration varied in previous studies. Use of the ultrasonography-guided radial artery cannulation technique in neonates can decrease the cannulation duration, as reported by Liu et al. [18]. The cannulation duration was similar in both groups in our study. We included adult patients ages 18–90 years, and patients who were in shock were excluded. Cannulation is relatively easier to perform in these patients than in neonates or in patients in shock, even using the palpation technique. Despite the advantages of the ultrasonography-guided radial artery cannulation technique mentioned in previous studies, several operators preferred the traditional palpation cannulation over the ultrasonography-guided technique in the clinical setting owing to concerns regarding the complexity of assembling the ultrasonography machine. In our study, we compared the total procedure duration, defined as the duration between the patient’s entry into the pre-anesthesia room to the time when the procedure is completed. The total procedure duration was not significantly different between the 2 groups. Cannulation in the operating room requires the assembly of the ultrasonography machine at each instance before the operation, thereby extending the total procedure duration. However, the machine can be assembled once before the patient has entered the room. Although there was no significant difference between the 2 groups in the total procedure duration and total success rate, for 2 patients in the palpation group, the cannulation could not be completed within 20 min. Therefore, the operating room was waiting for the patient and the convergence time for the surgery was extended. Cannulation was achieved in these 2 patients using the ultrasonography-guided technique.
In our study, no case of infection caused by cannulation was observed in the 2 groups. However, some authors have mentioned that the risk of infection is higher with the ultrasonography-guided technique. Strict sterile conditions and a short (≤6 h) catheter retention time may be responsible for the differences between the 2 studies. Two patients experienced hematoma in the palpation group, in whom cannulation was attempted more than twice, whereas no case of such complications occurred in the ultrasonography-guided group. The first-attempt success rate was lower in the palpation group; therefore, more attempts were required to puncture the artery, and this may have caused the hematoma.
One limitation of our study is that the sample size was calculated based on the first attempt; therefore, although cannulation failure and hematoma were observed in 2 cases each in the palpation group, there was no significant difference in the statistical analyses between the 2 groups. Studies with larger sample sizes are needed to confirm these results.
Conclusions
The ultrasonography-guided radial artery cannulation technique is more efficient for arterial cannulation in the pre-anesthesia room compared with the traditional palpation technique. This ultrasonography-guided technique warrants wider use in clinical practice.
Footnotes
Source of support: This work is partially supported by National Natural Science Foundation of China (No.81770295) and Key Project of Excellent Youth in Higher Education Institution of Anhui Province (gxyqZD2018028)
References
- 1.Shiloh AL, Savel RH, Paulin LM, Eisen LA. Ultrasound-guided catheterization of the radial artery: A systematic review and meta-analysis of randomized controlled trials. Chest. 2011;139(3):524–29. doi: 10.1378/chest.10-0919. [DOI] [PubMed] [Google Scholar]
- 2.Scheer B, Perel A, Pfeiffer UJ. Clinical review: Complications and risk factors of peripheral arterial catheters used for haemodynamic monitoring in anaesthesia and intensive care medicine. Crit Care. 2002;6(3):199–204. doi: 10.1186/cc1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nuttal G, Burckhardt J, Hadley A, et al. Surgical and patient risk factors for severe arterial line complications in adults. Anesthesiology. 2016;124(3):590–97. doi: 10.1097/ALN.0000000000000967. [DOI] [PubMed] [Google Scholar]
- 4.Kiberenge RK, Ueda K, Rosauer B. Ultrasound-guided dynamic needle tip positioning technique versus palpation technique for radial arterial cannulation in adult surgical patients: A randomized controlled Trial. Anesth Analg. 2018;126(1):120–26. doi: 10.1213/ANE.0000000000002261. [DOI] [PubMed] [Google Scholar]
- 5.Ueda K, Bayman EO, Johnson C, et al. A randomized controlled trail of radial artery cannulation guided by Doppler vs. palpation vs. ultrasound. Anaesthesia. 2015;70(9):1039–44. doi: 10.1111/anae.13062. [DOI] [PubMed] [Google Scholar]
- 6.Hansen MA, Juhl-Olsen P, Thorn S, et al. Ultrasonography-guided radial artery catheterization is superior compared with the traditional palpation technique: A prospective, randomized, blinded, crossover study. Acta Anaesthesiol Scand. 2014;58(4):446–52. doi: 10.1111/aas.12299. [DOI] [PubMed] [Google Scholar]
- 7.Shiver S, Blaivas M, Lyon M. A prospective comparison of ultrasound guided and blindly placed radial artery catheters. Acad Emerg Med. 2006;13(12):1275–79. doi: 10.1197/j.aem.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 8.Levin PD, Sheinin O, Gozal Y. Use of ultrasound guidance in the insertion of radial artery catheters. Crit Care Med. 2003;31(2):481–84. doi: 10.1097/01.CCM.0000050452.17304.2F. [DOI] [PubMed] [Google Scholar]
- 9.Bhattacharjee S, Maitra S, Baidya DK. Comparison between ultrasound guided technique and digital palpation technique for radial artery cannulation in adult patients: An updated meta-analysis of randomized controlled trials. J Clin Anesth. 2018;47:54–59. doi: 10.1016/j.jclinane.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 10.Fujii S, Jones PM. A technique for optimizing ultrasonography-guided radial arterial catheter insertion. Can J Anaesth. 2017;64(6):683–84. doi: 10.1007/s12630-017-0850-z. [DOI] [PubMed] [Google Scholar]
- 11.Shao E, Vaghadia H, Ramsay N, et al. Evaluation of two novel techniques for increasing radial artery size: A pilot study utilizing volunteers. Can J Anaesth. 2017;64(7):786–87. doi: 10.1007/s12630-017-0861-9. [DOI] [PubMed] [Google Scholar]
- 12.Maheshwari P, Kelsheimer B, Maheshwari P. Novel techniques for increasing the size of the radial artery during ultrasound-guided cannulation. Can J Anaesth. 2016;63(4):499–500. doi: 10.1007/s12630-015-0545-2. [DOI] [PubMed] [Google Scholar]
- 13.Grocott HP, Hilary P. Interpreting meta-analysis of ultrasound-guided vs. palpation methods for radial artery cannulation may not fully capture differences in technique optimization. J Clin Anesth. 2018;51:57. doi: 10.1016/j.jclinane.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 14.Mahler SA, Wang H, Lester C, et al. Short- vs. long-axis approach to ultrasound-guided peripheral intravenous access: A prospective randomized study. Am J Emerg Med. 2011;29(9):1194–97. doi: 10.1016/j.ajem.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 15.Berk D, Gurkan Y, Kus A, et al. Ultrasound-guided radial arterial cannulation: Long axis/inplane versus short axis/out-of-plane approaches? J Clin Monit Comput. 2013;27(3):319–24. doi: 10.1007/s10877-013-9437-6. [DOI] [PubMed] [Google Scholar]
- 16.Song IK, Choi JY, Lee JH, et al. Short-axis/out-of-plane or long-axis/in-plane ultrasound-guided arterial cannulation in children: A randomised controlled trial. Eur J Anaesthesiol. 2016;33(7):522–27. doi: 10.1097/EJA.0000000000000453. [DOI] [PubMed] [Google Scholar]
- 17.Clemmesen L, Knudsen L, Sloth E, Bendtsen T. Dynamic needle tip positioning – ultrasound guidance for peripheral vascular access. A randomized, controlled and blinded study in phantoms performed by ultrasound novices. Ultraschall Med. 2012;33(7):E321–25. doi: 10.1055/s-0032-1312824. [DOI] [PubMed] [Google Scholar]
- 18.Liu L, Tan Y, Li S, Tian J. “Modified dynamic needle tip positing” short-axis, out-of-plane, ultrasound-guided radial artery cannulation in neonates: A randomized controlled trial. Anesth Analg. :2018. doi: 10.1213/ANE.0000000000003445. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]