This cohort study examines whether positive adolescent family relationships are associated with reduced depressive symptoms among females and males as they enter midlife.
Key Points
Question
How are adolescent family relationships associated with trajectories of depressive symptoms from adolescence into midlife for women and men?
Findings
In this cohort study of 18 185 individuals (9233 females and 8952 males), those who experienced positive adolescent family relationships had significantly lower levels of depressive symptoms from early adolescence to midlife (late 30s to early 40s) than did those who experienced less-positive family relationships.
Meaning
The findings suggest an association of early intervention in family relationships during adolescence with better mental health into adulthood and midlife.
Abstract
Importance
National longitudinal studies that examine the linkages between early family experiences and sex-specific development of depression across the life course are lacking despite the urgent need for interventions in family settings to prevent adult depression.
Objective
To examine whether positive adolescent family relationships are associated with reduced depressive symptoms among women and men as they enter midlife.
Design, Setting, and Participants
This study analyzed data from the National Longitudinal Study of Adolescent to Adult Health, which used a multistage, stratified school-based design to select a prospective cohort of 20 745 adolescents in grades 7 to 12 from January 3, 1994, to December 26, 1995 (wave 1). Respondents were followed up during 4 additional waves from April 14 to September 9, 1996 (wave 2); April 2, 2001, to May 9, 2002 (wave 3); April 3, 2007, to February 1, 2009 (wave 4); and March 3, 2016, to May 8, 2017 (sample 1, wave 5), when the cohort was aged 32 to 42 years. The study sample of 8952 male adolescents and 9233 female adolescents that were analyzed was a US national representation of all population subgroups by sex, race/ethnicity, socioeconomic status, and geography.
Exposures
Adolescent family cohesion and low parent-child conflict.
Main Outcomes and Measures
Levels of depressive symptoms (Center for Epidemiologic Studies–Depression Scale [CES-D]) from ages 12 to 42 years were used to estimate propensity score–weighted growth curve models to assess sex differences in trajectories of depression by levels of positive adolescent family relationships.
Results
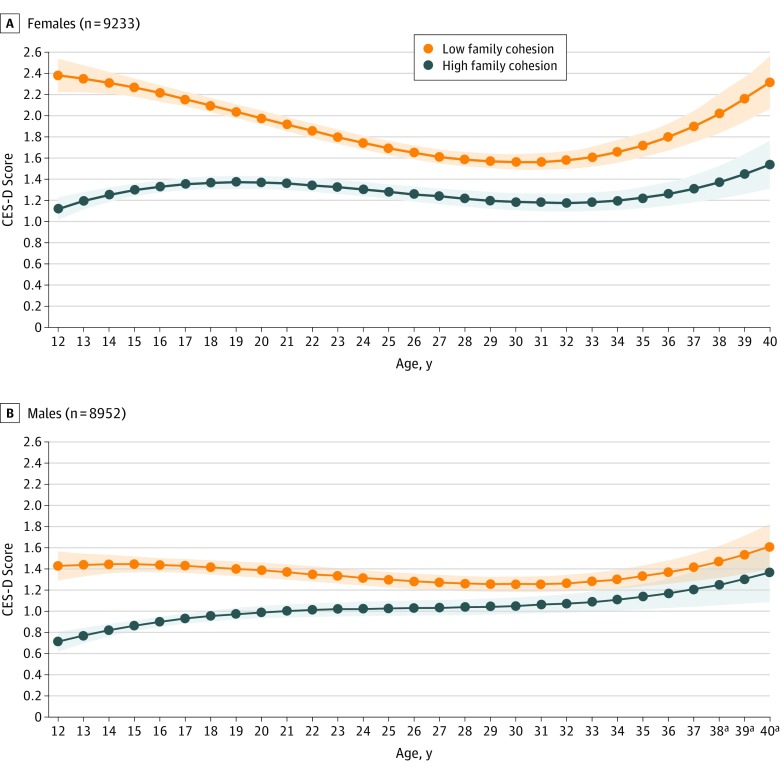
A total of 18 185 individuals (mean [SD] age at wave 1, 15.42 [0.12] years; 9233 [50.8%] female) participated in the study. Females and males who experienced positive adolescent family relationships had significantly lower levels of depressive symptoms from early adolescence to midlife than did those who experienced less positive adolescent family relationships. For example, depressive symptoms were lower among those with high levels of family cohesion compared with those with low cohesion between 12 (1.26 lower CES-D score; 95% CI, 1.10-1.42) and 40 (0.78 lower CES-D score; 95% CI, 0.50-1.06) years of age among females and between 12 (0.72 lower CES-D score; 95% CI, 0.57-0.86) and 37 (0.21 lower CES-D score; 95% CI, 0.00-0.41) years of age among males. The reduction in depressive symptoms associated with positive adolescent family relationships was greater for females than males during the adolescent and early adulthood years (ie, early 20s) (eg, low-high cohesion difference in mean CES-D score, −1.26 [95% CI, −1.42 to −1.10] for females and −0.72 [95% CI, −0.86 to −0.57] for males at 12 years of age; low-high cohesion difference in mean CES-D score, −0.61 [95% CI, −0.69 to −0.53] for females and −0.40 [95% CI, −0.48 to −0.31] for males at 20 years of age), after which females and males benefited equally from positive adolescent relationships throughout young adulthood to midlife.
Conclusions and Relevance
The findings suggest that positive adolescent family relationships are associated with better mental health among females and males from early adolescence to midlife. Interventions in early family life to foster healthy mental development throughout the life course appear to be important.
Introduction
Depression is a prevalent mental condition worldwide and a significant contributor to the global burden of disease.1,2 Depression often initially occurs during adolescence,3 may continue or recur in adulthood,4 and tends to become a lifetime chronic mental disorder.5 Poor mental health and depressive symptoms may be associated with the recent increase in midlife premature deaths due to suicide, alcohol, and drugs.6,7,8,9,10
Although treatment methods and intervention efforts continue to advance, a large proportion of depressive conditions remain irreversible.11 The push for prevention and early, affordable, and feasible interventions has been stronger than ever, especially for young people.12 The family context, in particular, has received considerable attention from mental health care professionals and researchers for early intervention efforts.13,14 Prior research has identified risk (eg, neglect, physical and sexual abuse, financial insecurity, residential mobility, and sexual harassment) and protective (eg, family attachment, parental support, parent-child communication, and financial stability) factors for youth depression in the family setting.15,16,17,18,19,20,21,22,23 Most research focuses on risk factors, but prevention efforts may be more effective by focusing on protective factors. For example, warm and cohesive family relationships provide social support and resources that help buffer youths from stresses of adolescent life.15,17,20,24,25,26 In addition, close parent-child relationships facilitate communication about personal problems and coping strategies.15,23
Most of this research, however, comes from small cross-sectional studies15,16,17,18,19,20,23 with clinical or community samples and suggests only a short-term role of positive family factors in lessening depressive symptoms during childhood and adolescence. Whether positive family relationships promote better mental health beyond adolescence and through the early years of adulthood is unknown. There is a dearth of national longitudinal studies that track individuals over time to understand the interconnections between early family life and the development of life-course depression.27 We implemented a longitudinal, developmental, and life-course approach using nationally representative data and estimating propensity score–weighted growth curve models to examine the long-term association of adolescent family relationships with the trajectories of depressive symptoms from early adolescence to midlife.
The literature on sex differences in depression is well established,28,29 especially during adolescence, when rates of depression in females first increase compared with those among males.16,21,22,30 Research also suggests that females benefit more from social support in lowering their risks of depression and anxiety compared with males.17,23 We therefore examined the differences among males and females in the trajectories of depression from early adolescence to midlife and the differential benefits of positive family relationships associated with depressive symptoms over time.
Methods
This cohort study used data from the National Longitudinal Study of Adolescent to Adult Health (Add Health), a nationally representative cohort study of 20 745 adolescents in grades 7 to 12 January 3, 1994, to December 26, 1995 (wave 1; ages 12-21 years), in the United States.31,32 Respondents were followed up during 4 additional waves from April 14 to September 9, 1996 (wave 2); April 2, 2001, to May 9, 2002 (wave 3); April 3, 2007, to February 1, 2009 (wave 4); and March 3, 2016, to May 8, 2017 (sample 1, wave 5), when the cohort was aged 32 to 42 years. Add Health used a multistage, stratified, school-based, cluster sampling design to select a probability sample of more than 20 000 adolescents from school rosters. Written informed consent was obtained from all participants. Survey procedures were approved by the institutional review board at the University of North Carolina. All data were deidentified.
Add Health was designed to study the association of social contexts of adolescent life with the health and behavior of adolescents and their outcomes in adulthood (more design details are given elsewhere31,32). The innovative design provided us with ideal data to achieve our study goals. The analytical sample included 18 185 respondents (8952 males and 9233 females) who had sampling weights and data on family relationships and 1 to 5 measures of depressive symptoms over time. The composition of the analytical sample was similar to that of those excluded because of missing data (eTable 2 in the Supplement).
Measures
Depressive symptoms were measured using a modified version of the Center for Epidemiologic Studies–Depression Scale (CES-D).33,34 The scale included the frequency of experiencing 3 depressive symptoms: (1) could not shake off the blues, even with help from family and friends; (2) felt depressed during the past 7 days; and (3) felt sad (responses include 0, never or rarely; 1, sometimes; 2, a lot of the time; and 3, most or all of the time) during the past 7 days. This composite measure is reliable and valid for assessing depressive symptoms and is invariant across age, race/ethnicity, and immigrant status.34,35 We summed the responses on the 3 CES-D items (range, 0-9, with 0 indicating never having any depressive symptoms and 9 indicating having symptoms most or all of the time) at each wave, with a higher score representing greater depressive symptoms. We explored a different version of the depressive symptoms measure by standardizing the sum of all CES-D items available during each wave, which yielded similar statistical results (eFigures 1-4 in the Supplement). We used the 3-item CES-D for the measure of depressive symptoms because it is invariant across the diverse racial/ethnic Add Health sample and is more easily interpretable than the standardization approach.
We measured family relationships in 2 domains: (1) family cohesion and (2) absence of parent-child conflict (described below). For each domain, we created a binary indicator of positive family relationships (coded as 1) based on face validity by categorizing positive at approximately the top quartile of the sample distribution on each measure.
Family cohesion was measured by mean responses (1, not at all; 2, very little; 3, somewhat; 4, quite a bit; and 5, very much) of adolescent reports on feelings about how much people in their family understood them, they and their family had fun together, and their family paid attention to them (mean [SD] index, 3.7 [0.84]; α = .79).36 The binary version was coded 1 for scores higher than 4 on this composite measure.
No parent-child conflict was measured by the mean response (range, 0-1, with 0 indicating highest level of conflict and 1 indicating no conflict at all between the parent and child) of adolescent reports on whether they had a serious argument about their behavior with their mother and/or their father in the past 4 weeks (separate question for each parent; mean [SD], 0.31 [0.42]). Those who scored a mean of 0 were coded as 1, indicating low conflict between the parent(s) and child.
Statistical Analysis
We estimated sex-specific growth curve models of depressive symptoms (eTables 4-7 in the Supplement). Centered age (in years by subtracting 12) was modeled in linear, quadratic, and cubic forms so that the start (time = 0) of the growth curve represented 12 years of age. Model 1 estimated an unconditional growth curve that included only linear, quadratic, and cubic age variables. Model 2 added exposure variables (family cohesion, low parent-child conflict) and their interaction with age variables to examine whether the initial level and slope of depressive symptoms varied by the 2 levels of family relationships. Model 3 added a number of key risk and protective factors associated with trajectories of depression, including (1) sociodemographic factors (race, ethnicity, and parental educational level), (2) family context (family structure and physical and sexual abuse before 12 years of age), (3) sleep problems as a measure of adolescent health, and (4) life course nonfamily social support (school engagement, friendships, religious involvement, and romantic relationships). Model 3 estimated whether differences in CES-D trajectories by exposure variables remained significant when risk and protective factors were held constant.37 Race/ethnicity was self-reported during the survey. Chow tests were conducted to examine whether a fully interactive model with sex (ie, all variables interacted with sex) resulted in a significantly improved fit to the data than a model without the full set of interactions, requiring stratified models by sex.38,39 The Chow test also enabled us to test whether the exposure variables differed significantly by sex38,39 (eMethods in the Supplement).
Growth curve models incorporated propensity score weighting,40,41,42 which generated a pseudopopulation in which exposure to positive family relationships was randomized. Adolescents who experience positive family relationships may be different from adolescents who do not on various dimensions that affect their likelihood to have good relationships within their families and experience less depression; thus, propensity score weighting was used to adjust for this potential selection bias and included observed confounders (eg, self-esteem, moodiness, family structure, physical abuse before 12 years of age, parental educational level, and parents’ feelings of happiness)40,41,42,43 (eMethods in the Supplement).
All statistical analyses applied survey weights to account for the unequal probabilities of sample selection to produce population estimates.31,44 Descriptive analyses and inverse probability treatment models also adjusted variance estimates for school clustering and stratification by region.44 Our mixed and multilevel growth curve modeling approach corrected SEs for correlation within respondents on CES-D.45,46,47 We analyzed interactions of each exposure with all age variables but only retained those that were significant at α = .05. All analyses were performed in Stata, version 14.2 (StataCorp). A 2-tailed P < .05 was considered to be statistically significant.
Results
A total of 18 185 individuals (mean [SD] age at wave 1, 15.42 [0.12] years; 9233 [50.8%] female) participated in the study. Table 1 presents the weighted sample statistics for all analytic variables (eTable 1 in the Supplement shows unweighted distributions). Although 8772 adolescents (49.4%) experienced high levels of family cohesion and 11 164 (62.1%) experienced no parent-child conflict, males (4448 [50.5%] for family cohesion and 5770 [65.5%] for no conflict) had slightly more positive relationships than females (4324 [48.0%] for family cohesion and 5394 [58.6%] for no conflict).
Table 1. Sample Demographics and Study Characteristicsa.
| Characteristic | Full Sample (N = 18 185) | Male Sample (n = 8952) | Female Sample (n = 9233) |
|---|---|---|---|
| Family cohesionb | |||
| Lower family cohesion | 9413 (50.6) | 4504 (49.3) | 4909 (51.9) |
| Higher family cohesion | 8772 (49.4) | 4448 (50.7) | 4324 (48.0) |
| Parent-child conflictb | |||
| Conflict | 7021 (37.9) | 3182 (34.5) | 3839 (41.4) |
| No conflict | 11 164 (62.1) | 5770 (65.5) | 5394 (58.6) |
| Age at wave 1, mean (SD), yc | 15.42 (0.12) | NA | NA |
| Sexc | |||
| Male | 8952 (49.2) | NA | NA |
| Female | 9233 (50.8) | NA | NA |
| Immigrant generationc | |||
| First generation | 1496 (5.5) | NA | NA |
| Second generation | 2732 (10.8) | NA | NA |
| Third generation or later | 13 957 (83.8) | NA | NA |
| Race/ethnicityc,d | |||
| Non-Hispanic, white | 9724 (67.7) | 4797 (68.0) | 4927 (67.4) |
| Non-Hispanic, black | 3938 (16.0) | 1857 (15.7) | 2081 (16.4) |
| Non-Hispanic, Asian | 1305 (3.7) | 692 (3.8) | 613 (3.7) |
| Non-Hispanic, other race | 84 (0.4) | 41 (0.3) | 43 (0.4) |
| Hispanic | 3134 (12.2) | 1565 (12.2) | 1569 (12.2) |
| Parental educational levelc,d | |||
| Less than high school | 2456 (13.0) | 1140 (12.6) | 1316 (13.5) |
| High school or GED | 5304 (31.6) | 2628 (31.6) | 2676 (31.5) |
| Some college | 3791 (21.3) | 1828 (20.7) | 1963 (21.9) |
| College or higher | 6355 (32.7) | 3205 (33.6) | 3150 (31.8) |
| Missing | 279 (1.5) | 151 (1.6) | 128 (1.3) |
| Family structurec,d | |||
| 2 Biological or 2 adopted parents | 9885 (55.4) | 4929 (56.0) | 4956 (54.9) |
| 1 Biological or 1 nonbiological parent | 2929 (16.5) | 1479 (16.7) | 1450 (16.2) |
| Single parent | 4553 (24.0) | 2161 (23.2) | 2392 (24.8) |
| 2 Stepparents/other | 818 (4.1) | 383 (4.1) | 435 (4.1) |
| Physical abuse before 12 y of agec,d | |||
| No | 13 919 (77.3) | 6558 (74.5) | 7361 (80.1) |
| Yes | 2054 (10.7) | 1110 (11.5) | 944 (9.8) |
| Missing | 2212 (12.1) | 1284 (14.0) | 928 (10.1) |
| Parental self-perceived happinessc | |||
| No | 654 (3.4) | NA | NA |
| Yes | 14 846 (84.0) | NA | NA |
| Missing | 2685 (12.6) | NA | NA |
| Moody index measure, mean (SD)c | 1.72 (0.02) | NA | NA |
| Self-esteem index measure, mean (SD)c | 24.69 (0.06) | NA | NA |
| Sexual abuse before 12 y of aged | |||
| No | NA | 7555 (84.7) | 7860 (85.0) |
| Yes | NA | 167 (1.8) | 471 (5.3) |
| Missing | NA | 1230 (13.5) | 902 (9.7) |
| Sleep problemd | |||
| No | NA | 7019 (77.7) | 6906 (74.6) |
| Yes | NA | 1933 (22.3) | 2327 (25.4) |
| Long-term nonfamilial social support index measure, mean (SD)d | NA | 3.23 (0.07) | 3.88 (0.07) |
Abbreviations: GED, general educational development; NA, not applicable; PSW, propensity score weighting.
Data are presented as number (percentage) unless otherwise indicated. Percentages and means were calculated by applying survey weights and adjusting for school clustering and stratification by region.
Each measure was used as Y variable in their PSW model (eTable 3 in the Supplement) and as X variable in their growth curve model (eTables 4-7 in the Supplement).
Covariates that were used in PSW models.
Covariates that were used in growth curve models.
Estimated levels of depressive symptoms among females and males in unconditional growth curve models are shown in Table 2. Females experienced high levels of depressive symptoms during the adolescent years (ages 13-18 years), after which levels of depression declined until the early 30s, when they began to increase again to levels equal to those in adolescence. The pattern for males, however, was flatter, with stable levels from adolescence into the 30s, increasing to the highest levels in the late 30s.
Table 2. Age-Specific CES-D Scores From Growth Curve Models for Overall Sample and by Levels of Family Cohesion in Add Health (1995-2017).
| No. of Participants/Age, y | Unconditional Curve (95% CI)a | Low Family Cohesion (95% CI)b | High Family Cohesion (95% CI)b | Low-High Cohesion Difference (95% CI)c | P Valued |
|---|---|---|---|---|---|
| Females | |||||
| 276/12 | 1.57 (1.47 to 1.68) | 2.39 (2.23 to 2.54) | 1.12 (1.02 to 1.23) | 1.26 (1.10 to 1.42) | <.001 |
| 1429/13 | 1.62 (1.53 to 1.70) | 2.35 (2.23 to 2.48) | 1.20 (1.11 to 1.28) | 1.16 (1.02 to 1.30) | <.001 |
| 2220/14 | 1.64 (1.58 to 1.71) | 2.32 (2.21 to 2.42) | 1.25 (1.19 to 1.32) | 1.06 (0.94 to 1.18) | <.001 |
| 2792/15 | 1.66 (1.60 to 1.71) | 2.27 (2.18 to 2.36) | 1.30 (1.24 to 1.36) | 0.97 (0.87 to 1.07) | <.001 |
| 3227/16 | 1.66 (1.61 to 1.71) | 2.22 (2.14 to 2.29) | 1.33 (1.28 to 1.39) | 0.89 (0.79 to 0.98) | <.001 |
| 3227/17 | 1.65 (1.60 to 1.70) | 2.16 (2.09 to 2.23) | 1.36 (1.30 to 1.41) | 0.81 (0.72 to 0.89) | <.001 |
| 2288/18 | 1.63 (1.58 to 1.68) | 2.10 (2.04 to 2.17) | 1.37 (1.31 to 1.43) | 0.74 (0.65 to 0.82) | .002 |
| 1234/19 | 1.61 (1.56 to 1.66) | 2.04 (1.97 to 2.11) | 1.37 (1.31 to 1.43) | 0.67 (0.59 to 0.75) | .01 |
| 1093/20 | 1.58 (1.53 to 1.63) | 1.98 (1.91 to 2.05) | 1.37 (1.31 to 1.43) | 0.61 (0.53 to 0.69) | .04 |
| 1236/21 | 1.54 (1.49 to 1.59) | 1.92 (1.85 to 1.99) | 1.36 (1.30 to 1.43) | 0.56 (0.47 to 0.64) | .11 |
| 1357/22 | 1.50 (1.45 to 1.55) | 1.86 (1.79 to 1.93) | 1.35 (1.28 to 1.41) | 0.51 (0.43 to 0.60) | .22 |
| 1397/23 | 1.46 (1.41 to 1.51) | 1.80 (1.73 to 1.87) | 1.33 (1.26 to 1.40) | 0.47 (0.38 to 0.56) | .33 |
| 1120/24 | 1.41 (1.37 to 1.46) | 1.75 (1.68 to 1.82) | 1.31 (1.24 to 1.38) | 0.44 (0.35 to 0.53) | .43 |
| 663/25 | 1.37 (1.32 to 1.42) | 1.70 (1.63 to 1.77) | 1.29 (1.22 to 1.36) | 0.41 (0.32 to 0.51) | .50 |
| 976/26 | 1.33 (1.28 to 1.38) | 1.65 (1.59 to 1.72) | 1.26 (1.19 to 1.33) | 0.39 (0.30 to 0.49) | .53 |
| 1151/27 | 1.30 (1.25 to 1.35) | 1.62 (1.55 to 1.69) | 1.24 (1.17 to 1.31) | 0.38 (0.28 to 0.47) | .52 |
| 1419/28 | 1.27 (1.22 to 1.32) | 1.59 (1.52 to 1.66) | 1.22 (1.14 to 1.30) | 0.37 (0.28 to 0.47) | .48 |
| 1430/29 | 1.25 (1.19 to 1.30) | 1.57 (1.50 to 1.65) | 1.20 (1.12 to 1.28) | 0.37 (0.27 to 0.47) | .42 |
| 1359/30 | 1.23 (1.17 to 1.29) | 1.57 (1.49 to 1.64) | 1.19 (1.11 to 1.27) | 0.38 (0.28 to 0.48) | .34 |
| 788/31 | 1.23 (1.17 to 1.29) | 1.57 (1.49 to 1.65) | 1.18 (1.10 to 1.27) | 0.39 (0.28 to 0.49) | .26 |
| 102/32 | 1.24 (1.17 to 1.30) | 1.59 (1.50 to 1.67) | 1.18 (1.09 to 1.27) | 0.41 (0.29 to 0.52) | .19 |
| 71/33 | 1.25 (1.19 to 1.32) | 1.62 (1.52 to 1.71) | 1.19 (1.10 to 1.28) | 0.43 (0.31 to 0.55) | .15 |
| 249/34 | 1.29 (1.22 to 1.36) | 1.66 (1.56 to 1.77) | 1.20 (1.11 to 1.29) | 0.46 (0.33 to 0.60) | .11 |
| 301/35 | 1.34 (1.26 to 1.42) | 1.73 (1.61 to 1.84) | 1.23 (1.13 to 1.33) | 0.50 (0.35 to 0.65) | .09 |
| 369/36 | 1.41 (1.31 to 1.50) | 1.81 (1.67 to 1.94) | 1.26 (1.15 to 1.38) | 0.54 (0.37 to 0.71) | .08 |
| 405/37 | 1.49 (1.38 to 1.60) | 1.90 (1.75 to 2.06) | 1.31 (1.18 to 1.44) | 0.59 (0.40 to 0.79) | .07 |
| 360/38 | 1.60 (1.46 to 1.73) | 2.02 (1.84 to 2.21) | 1.37 (1.22 to 1.53) | 0.65 (0.43 to 0.87) | .06 |
| 289/39 | 1.72 (1.56 to 1.89) | 2.16 (1.95 to 2.38) | 1.45 (1.26 to 1.64) | 0.71 (0.46 to 0.96) | .06 |
| 41/40 | 1.87 (1.67 to 2.08) | 2.33 (2.07 to 2.58) | 1.54 (1.31 to 1.77) | 0.78 (0.50 to 1.06) | .05 |
| Males | |||||
| 211/12 | 0.93 (0.84 to 1.03) | 1.43 (1.29 to 1.57) | 0.71 (0.62 to 0.81) | 0.72 (0.57 to 0.86) | <.001 |
| 1146/13 | 0.99 (0.92 to 1.06) | 1.44 (1.33 to 1.55) | 0.77 (0.70 to 0.84) | 0.67 (0.54 to 0.79) | <.001 |
| 1947/14 | 1.03 (0.98 to 1.08) | 1.45 (1.36 to 1.53) | 0.82 (0.76 to 0.88) | 0.62 (0.52 to 0.73) | <.001 |
| 2547/15 | 1.06 (1.02 to 1.11) | 1.44 (1.37 to 1.52) | 0.86 (0.81 to 0.92) | 0.58 (0.49 to 0.67) | <.001 |
| 3153/16 | 1.09 (1.05 to 1.13) | 1.44 (1.37 to 1.51) | 0.90 (0.85 to 0.95) | 0.54 (0.46 to 0.62) | <.001 |
| 3241/17 | 1.11 (1.06 to 1.15) | 1.43 (1.37 to 1.50) | 0.93 (0.88 to 0.98) | 0.50 (0.42 to 0.57) | <.001 |
| 2384/18 | 1.12 (1.07 to 1.16) | 1.42 (1.35 to 1.49) | 0.96 (0.90 to 1.01) | 0.46 (0.38 to 0.54) | .002 |
| 1210/19 | 1.12 (1.07 to 1.17) | 1.41 (1.34 to 1.47) | 0.98 (0.92 to 1.03) | 0.43 (0.35 to 0.51) | .01 |
| 892/20 | 1.12 (1.07 to 1.17) | 1.39 (1.32 to 1.46) | 0.99 (0.93 to 1.05) | 0.40 (0.31 to 0.48) | .04 |
| 1020/21 | 1.12 (1.07 to 1.17) | 1.37 (1.30 to 1.44) | 1.00 (0.94 to 1.07) | 0.37 (0.28 to 0.45) | .11 |
| 1296/22 | 1.11 (1.06 to 1.16) | 1.35 (1.28 to 1.43) | 1.01 (0.95 to 1.08) | 0.34 (0.25 to 0.43) | .22 |
| 1328/23 | 1.11 (1.06 to 1.16) | 1.33 (1.26 to 1.41) | 1.02 (0.95 to 1.09) | 0.31 (0.22 to 0.41) | .33 |
| 1097/24 | 1.10 (1.05 to 1.15) | 1.32 (1.24 to 1.39) | 1.03 (0.96 to 1.09) | 0.29 (0.19 to 0.39) | .43 |
| 624/25 | 1.09 (1.03 to 1.14) | 1.30 (1.23 to 1.37) | 1.03 (0.96 to 1.10) | 0.27 (0.17 to 0.37) | .50 |
| 763/26 | 1.08 (1.02 to 1.13) | 1.29 (1.21 to 1.36) | 1.03 (0.96 to 1.11) | 0.25 (0.15 to 0.35) | .53 |
| 923/27 | 1.07 (1.01 to 1.12) | 1.27 (1.20 to 1.35) | 1.04 (0.96 to 1.11) | 0.24 (0.14 to 0.34) | .52 |
| 1222/28 | 1.06 (1.01 to 1.11) | 1.26 (1.19 to 1.34) | 1.04 (0.96 to 1.12) | 0.22 (0.12 to 0.32) | .48 |
| 1311/29 | 1.06 (1.00 to 1.11) | 1.26 (1.18 to 1.33) | 1.05 (0.97 to 1.12) | 0.21 (0.11 to 0.31) | .42 |
| 1282/30 | 1.06 (1.00 to 1.11) | 1.26 (1.18 to 1.33) | 1.05 (0.97 to 1.13) | 0.20 (0.10 to 0.31) | .34 |
| 819/31 | 1.06 (1.00 to 1.12) | 1.26 (1.18 to 1.34) | 1.06 (0.98 to 1.15) | 0.20 (0.09 to 0.30) | .26 |
| 173/32 | 1.07 (1.01 to 1.13) | 1.27 (1.19 to 1.35) | 1.08 (0.99 to 1.17) | 0.19 (0.08 to 0.31) | .19 |
| 46/33 | 1.09 (1.02 to 1.15) | 1.28 (1.20 to 1.37) | 1.09 (0.99 to 1.19) | 0.19 (0.07 to 0.32) | .15 |
| 163/34 | 1.11 (1.04 to 1.18) | 1.31 (1.21 to 1.40) | 1.11 (1.01 to 1.22) | 0.19 (0.05 to 0.33) | .11 |
| 198/35 | 1.14 (1.06 to 1.22) | 1.33 (1.23 to 1.43) | 1.14 (1.02 to 1.26) | 0.20 (0.04 to 0.35) | .09 |
| 256/36 | 1.18 (1.09 to 1.27) | 1.37 (1.26 to 1.48) | 1.17 (1.03 to 1.31) | 0.20 (0.02 to 0.38) | .08 |
| 321/37 | 1.23 (1.13 to 1.34) | 1.42 (1.29 to 1.55) | 1.21 (1.04 to 1.38) | 0.21 (0.00 to 0.41) | .07 |
| 291/38c | 1.30 (1.16 to 1.43) | 1.47 (1.32 to 1.62) | 1.25 (1.06 to 1.45) | 0.22 (−0.02 to 0.45) | .06 |
| 205/39c | 1.37 (1.21 to 1.53) | 1.54 (1.36 to 1.72) | 1.31 (1.07 to 1.54) | 0.23 (−0.04 to 0.50) | .06 |
| 50/40c | 1.45 (1.26 to 1.65) | 1.61 (1.40 to 1.83) | 1.37 (1.09 to 1.65) | 0.24 (−0.06 to 0.55) | .05 |
Abbreviations: Add Health, National Longitudinal Study of Adolescent to Adult Health; CES-D, Center for Epidemiologic Studies–Depression Scale.
Estimated CES-D scores were calculated from the unconditional growth curve model (ie, model 1 in eTable 4 in the Supplement for females and eTable 5 in the Supplement for males).
Estimated CES-D scores were calculated by low and high family cohesion (from growth curve model 3 in eTable 4 in the Supplement for females and eTable 5 in the Supplement for males).
The Wald test showed that the difference in CES-D scores by levels of family cohesion was not significant at α = .05.
The Wald test P value for the comparison of female CES-D score difference by low-high family cohesion to male CES-D score difference by low-high cohesion (results derived from equation 3 in the eMethods in the Supplement).
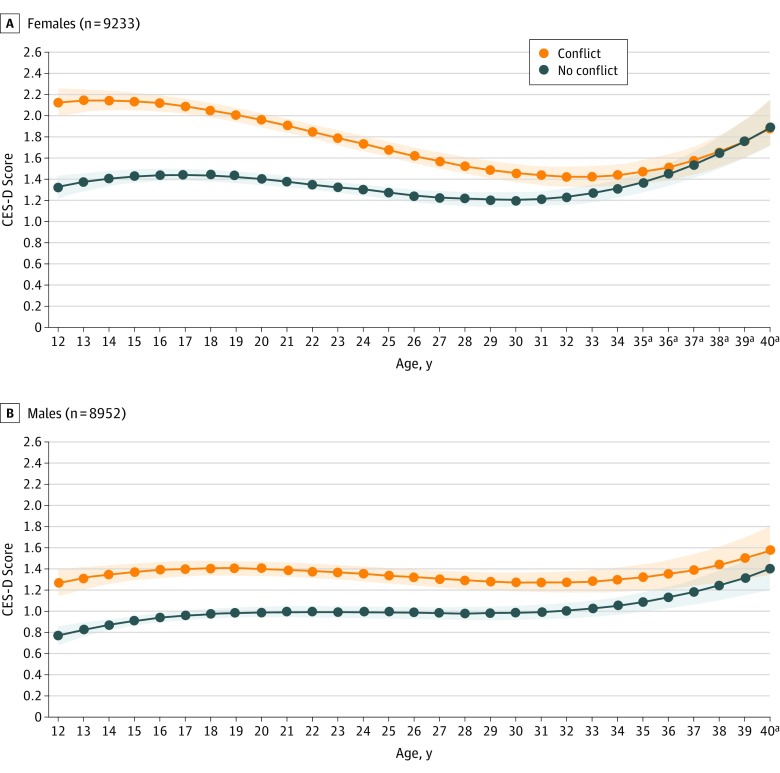
Results from the conditional growth curve models (Table 2 and Table 3) suggest that positive family relationships were associated with lower depressive symptoms across the life course for both females and males. For example, depressive symptoms at 12 years of age were significantly lower among females in highly cohesive families (difference in mean CES-D scores, −1.26; 95% CI, −1.42 to −1.10) (Table 2) and among females without parent-child conflict (difference in mean CES-D scores, −0.80; 95% CI, −0.92 to −0.69) (Table 3) compared with females with less positive family relationships. Depressive symptoms were significantly lower at 12 years of age among males in highly cohesive families (difference in mean CES-D scores, −0.72; 95% CI, −0.86 to 0.57) (Table 2) and males without parent-child conflict (difference in mean CES-D scores, −0.50; 95% CI, −0.61 to −0.39) (Table 3) compared with males with less positive relationships.
Table 3. Age-Specific CES-D Growth Curve Scores by Levels of Parent-Child Conflict in Add Health (1995-2017).
| No. of Participants/Age, y | Conflict (95% CI)a | No Conflict (95% CI)a | Conflict vs No Conflict Difference (95% CI)b | P Valuec |
|---|---|---|---|---|
| Females | ||||
| 276/12 | 2.13 (2.00 to 2.26) | 1.33 (1.22 to 1.44) | 0.80 (0.69 to 0.92) | <.001 |
| 1429/13 | 2.15 (2.04 to 2.25) | 1.38 (1.29 to 1.46) | 0.77 (0.66 to 0.88) | <.001 |
| 2220/14 | 2.15 (2.06 to 2.24) | 1.41 (1.34 to 1.48) | 0.74 (0.64 to 0.84) | <.001 |
| 2792/15 | 2.14 (2.06 to 2.22) | 1.43 (1.37 to 1.49) | 0.71 (0.61 to 0.81) | <.001 |
| 3227/16 | 2.12 (2.05 to 2.19) | 1.44 (1.38 to 1.50) | 0.68 (0.59 to 0.77) | .001 |
| 3227/17 | 2.09 (2.02 to 2.16) | 1.44 (1.39 to 1.50) | 0.65 (0.56 to 0.73) | .001 |
| 2288/18 | 2.05 (1.98 to 2.12) | 1.44 (1.38 to 1.49) | 0.62 (0.54 to 0.70) | .002 |
| 1234/19 | 2.01 (1.94 to 2.08) | 1.42 (1.37 to 1.48) | 0.59 (0.51 to 0.67) | .003 |
| 1093/20 | 1.96 (1.89 to 2.03) | 1.40 (1.35 to 1.46) | 0.56 (0.48 to 0.63) | .007 |
| 1236/21 | 1.91 (1.84 to 1.97) | 1.38 (1.32 to 1.43) | 0.53 (0.45 to 0.60) | .02 |
| 1357/22 | 1.85 (1.78 to 1.92) | 1.35 (1.30 to 1.41) | 0.50 (0.42 to 0.57) | .04 |
| 1397/23 | 1.79 (1.73 to 1.86) | 1.33 (1.27 to 1.38) | 0.47 (0.39 to 0.54) | .10 |
| 1120/24 | 1.73 (1.67 to 1.80) | 1.30 (1.24 to 1.35) | 0.44 (0.36 to 0.51) | .21 |
| 663/25 | 1.68 (1.61 to 1.75) | 1.27 (1.22 to 1.33) | 0.40 (0.33 to 0.48) | .39 |
| 976/26 | 1.62 (1.55 to 1.70) | 1.25 (1.19 to 1.31) | 0.37 (0.29 to 0.46) | .61 |
| 1151/27 | 1.57 (1.50 to 1.65) | 1.23 (1.17 to 1.29) | 0.34 (0.26 to 0.43) | .85 |
| 1419/28 | 1.53 (1.45 to 1.61) | 1.21 (1.15 to 1.28) | 0.31 (0.22 to 0.40) | .92 |
| 1430/29 | 1.49 (1.41 to 1.57) | 1.21 (1.14 to 1.27) | 0.28 (0.19 to 0.38) | .72 |
| 1359/30 | 1.46 (1.37 to 1.55) | 1.21 (1.14 to 1.28) | 0.25 (0.15 to 0.35) | .56 |
| 788/31 | 1.44 (1.35 to 1.53) | 1.22 (1.14 to 1.29) | 0.22 (0.11 to 0.33) | .43 |
| 102/32 | 1.43 (1.33 to 1.52) | 1.24 (1.16 to 1.31) | 0.19 (0.08 to 0.31) | .33 |
| 71/33 | 1.43 (1.33 to 1.53) | 1.27 (1.19 to 1.35) | 0.16 (0.04 to 0.28) | .26 |
| 249/34 | 1.44 (1.34 to 1.55) | 1.31 (1.22 to 1.40) | 0.13 (0.00 to 0.26) | .21 |
| 301/35b | 1.47 (1.36 to 1.58) | 1.37 (1.28 to 1.47) | 0.10 (−0.04 to 0.24) | .17 |
| 369/36b | 1.52 (1.40 to 1.64) | 1.45 (1.34 to 1.56) | 0.07 (−0.07 to 0.21) | .14 |
| 405/37b | 1.58 (1.44 to 1.72) | 1.54 (1.41 to 1.67) | 0.04 (−0.11 to 0.19) | .12 |
| 360/38b | 1.66 (1.50 to 1.82) | 1.65 (1.50 to 1.80) | 0.01 (−0.15 to 0.17) | .10 |
| 289/39b | 1.76 (1.57 to 1.95) | 1.78 (1.60 to 1.96) | −0.02 (−0.19 to 0.14) | .08 |
| 41/40b | 1.88 (1.66 to 2.11) | 1.94 (1.72 to 2.15) | −0.05 (−0.23 to 0.12) | .07 |
| Males | ||||
| 211/12 | 1.27 (1.14 to 1.40) | 0.77 (0.68 to 0.86) | 0.50 (0.39 to 0.61) | <.001 |
| 1146/13 | 1.32 (1.21 to 1.43) | 0.83 (0.76 to 0.90) | 0.49 (0.39 to 0.59) | <.001 |
| 1947/14 | 1.35 (1.26 to 1.44) | 0.87 (0.82 to 0.93) | 0.48 (0.38 to 0.57) | <.001 |
| 2547/15 | 1.38 (1.30 to 1.46) | 0.91 (0.87 to 0.96) | 0.47 (0.38 to 0.56) | <.001 |
| 3153/16 | 1.40 (1.32 to 1.47) | 0.94 (0.90 to 0.99) | 0.46 (0.37 to 0.54) | .001 |
| 3241/17 | 1.41 (1.34 to 1.48) | 0.97 (0.92 to 1.01) | 0.44 (0.36 to 0.52) | .001 |
| 2384/18 | 1.41 (1.34 to 1.48) | 0.98 (0.93 to 1.03) | 0.43 (0.36 to 0.51) | .002 |
| 1210/19 | 1.41 (1.34 to 1.48) | 0.99 (0.94 to 1.04) | 0.42 (0.35 to 0.49) | .003 |
| 892/20 | 1.41 (1.34 to 1.48) | 1.00 (0.95 to 1.05) | 0.41 (0.34 to 0.48) | .007 |
| 1020/21 | 1.40 (1.33 to 1.47) | 1.00 (0.95 to 1.06) | 0.40 (0.33 to 0.47) | .02 |
| 1296/22 | 1.39 (1.32 to 1.46) | 1.00 (0.95 to 1.06) | 0.39 (0.31 to 0.46) | .04 |
| 1328/23 | 1.37 (1.30 to 1.44) | 1.00 (0.95 to 1.05) | 0.37 (0.30 to 0.45) | .10 |
| 1097/24 | 1.36 (1.29 to 1.43) | 1.00 (0.94 to 1.05) | 0.36 (0.29 to 0.44) | .21 |
| 624/25 | 1.34 (1.27 to 1.41) | 0.99 (0.94 to 1.05) | 0.35 (0.27 to 0.43) | .39 |
| 763/26 | 1.33 (1.25 to 1.40) | 0.99 (0.93 to 1.04) | 0.34 (0.25 to 0.42) | .61 |
| 923/27 | 1.31 (1.23 to 1.39) | 0.98 (0.92 to 1.04) | 0.33 (0.24 to 0.42) | .85 |
| 1222/28 | 1.30 (1.21 to 1.38) | 0.98 (0.92 to 1.04) | 0.32 (0.22 to 0.41) | .92 |
| 1311/29 | 1.29 (1.20 to 1.38) | 0.98 (0.92 to 1.05) | 0.30 (0.20 to 0.41) | .72 |
| 1282/30 | 1.28 (1.19 to 1.37) | 0.99 (0.92 to 1.06) | 0.29 (0.18 to 0.40) | .56 |
| 819/31 | 1.28 (1.18 to 1.38) | 1.00 (0.93 to 1.07) | 0.28 (0.16 to 0.40) | .43 |
| 173/32 | 1.28 (1.18 to 1.38) | 1.01 (0.94 to 1.09) | 0.27 (0.15 to 0.39) | .33 |
| 46/33 | 1.29 (1.18 to 1.40) | 1.03 (0.95 to 1.11) | 0.26 (0.13 to 0.39) | .26 |
| 163/34 | 1.30 (1.19 to 1.42) | 1.06 (0.98 to 1.14) | 0.25 (0.11 to 0.38) | .21 |
| 198/35 | 1.33 (1.20 to 1.45) | 1.09 (1.00 to 1.19) | 0.23 (0.09 to 0.38) | .17 |
| 256/36 | 1.36 (1.22 to 1.50) | 1.14 (1.03 to 1.24) | 0.22 (0.07 to 0.38) | .14 |
| 321/37 | 1.40 (1.25 to 1.55) | 1.19 (1.07 to 1.31) | 0.21 (0.05 to 0.37) | .12 |
| 291/38 | 1.45 (1.27 to 1.62) | 1.25 (1.11 to 1.39) | 0.20 (0.03 to 0.37) | .10 |
| 205/39 | 1.51 (1.31 to 1.71) | 1.32 (1.15 to 1.49) | 0.19 (0.01 to 0.37) | .08 |
| 50/40b | 1.58 (1.35 to 1.82) | 1.41 (1.21 to 1.61) | 0.18 (−0.01 to 0.36) | .07 |
Abbreviations: Add Health, National Longitudinal Study of Adolescent to Adult Health; CES-D, Center for Epidemiologic Studies–Depression Scale.
Estimated CES-D scores were calculated by levels of conflict (from growth curve model 3 in eTable 6 in the Supplement for females and eTable 7 in the Supplement for males).
The Wald test showed that the difference in CES-D scores by levels of family conflict was not significant at α = .05.
The Wald test P value for the comparison of female CES-D score difference by levels of conflict to male CES-D score difference by levels of conflict (results derived from equation 3 in eMethods in the Supplement).
The association between positive family relationships and the trajectory of depressive symptoms was best seen by the growth curves across ages 12 to 40 years by family cohesion (Figure 1) and parent-child conflict (Figure 2) for females and males. The small cell sizes at ages 41 to 42 years preclude showing these estimates in the tables and figures. Females who experienced high levels of family cohesion had significantly fewer depressive symptoms across all observed ages from 12 to 40 years compared with females with low family cohesion (Figure 1). The difference in CES-D scores by levels of family cohesion was greatest in adolescence, beginning at 12 years of age (difference in mean CES-D score, 1.26; 95% CI, 1.10-1.42) (Table 2), decreased during the late 20s (eg, at 30 years of age; difference in mean CES-D score, 0.38; 95% CI, 0.28-0.48), and increased again during the 30s until 40 years of age (difference in mean CES-D score, 0.78; 95% CI, 0.50-1.06), when the difference reached a level similar to the one at the age of 18 years (difference in mean CES-D score, 0.74; 95% CI, 0.65-0.82).
Figure 1. Center for Epidemiologic Studies–Depression Scale (CES-D) Growth Curve by Levels of Family Cohesion Across Ages 12 to 40 Years.
The CES-D scores were calculated from propensity score weighting conditional growth curve models.
aThe CES-D scores by 2 levels of family cohesion were not significantly different at α = .05.
Figure 2. Center for Epidemiologic Studies–Depression Scale (CES-D) Growth Curve by Levels of Parent-Child Conflict Across Ages 12 to 40 Years.
The CES-D scores were calculated from propensity score weighting conditional growth curve models.
aThe CES-D scores by 2 levels of family conflict were not significantly different at α = .05.
Among males, high levels of family cohesion were also associated with lower levels of depressive symptoms between 12 and 37 years of age compared with low levels of cohesion (Figure 1). The difference in CES-D scores among males by levels of family cohesion was greatest in adolescence, beginning at 12 years of age (difference in mean CES-D score, 0.72; 95% CI, 0.57-0.86) (Table 2), gradually decreased in early adulthood, and remained stable in the late 20s and 30s.
Females with little parent-child conflict in adolescence had significantly lower levels of depressive symptoms from 12 to 34 years of age, whereas the significant association of low parent-child conflict with lower levels of depression lasted longer for males, from 12 to 39 years of age (Figure 2). In contrast, adolescents who had low-quality family relationships (low cohesion and high parent-child conflict) were more likely to experience early onset of depressive symptoms, with the highest CES-D scores during the ages of 12 to 15 years, especially among females. Adolescents with poor family relationships continued to experience high levels of depressive symptoms during late adolescence (ages 15-18 years) and the transition to adulthood (ages 19-22 years) and had high risk of depression in their late 30s as they approached midlife.
Females’ mental health tended to benefit more from positive family relationships than males’ mental health (Table 2 and Table 3 and eTables 4-7 in the Supplement). For example, at 12 years of age (ie, the intercept), the absolute values of the coefficients were significantly higher among females than males (2.13 [95% CI, 1.95-2.31] for females in the family-cohesion model 3 of eTable 4 in the Supplement and 1.21 [95% CI, 1.05-1.38] for males in model 3 of eTable 5 in the Supplement; Wald test for female-male intercept difference, P < .001; 2.03 [95% CI, 1.87-2.20] for females in the conflict model 3 of eTable 6 in the Supplement and 1.16 [95% CI, 1.01-1.32] for males in model 3 of eTable 7 in the Supplement; Wald test, P < .001), suggesting that exposure to positive family relationships had a stronger association with lowering the initial level of depressive symptoms among females than among males.
Discussion
Few studies have used a longitudinal approach to examine the association between early adolescent family relationships and long-term development of depression into midlife. Our study was, to our knowledge, the first to examine how family relationships during the sensitive period of adolescence are associated with mental health trajectories through adulthood, providing a new contribution to the research on early family experiences and lifetime depression. We highlight several key findings from our longitudinal, developmental, and life-course study based on results from growth curve models that account for potential selection effects of family relationships. First, levels of depressive symptoms changed during a 30-year life course from early adolescence to midlife among both females and males. Second, females experienced significantly higher levels of depressive symptoms than males between early adolescence and the fourth decade of life through the beginning of their 40s. Third, females’ highest levels of depression occurred during the middle to late adolescent years, whereas males experienced a shorter period of high depressive symptoms during late adolescence but increasing depression levels during the 30s to the start of midlife. Fourth, family cohesion and the absence of parent-child conflict were associated with lower risk of depression, not only in the short term during adolescence but also throughout young adulthood and into midlife. Fifth, affective emotions and positive feelings that derive from being a part of a cohesive family were more important for females than for males and were more strongly associated with improved mental health through the transition to adulthood in females. Similarly, parental support and approval reflected by low parent-child conflict was more strongly associated with improved mental health among females than among males during adolescence and into the early 20s. Once females and males were in their middle 20s, the associations of cohesive and low-conflict adolescent family relationships with improved mental health were equal into their 30s, with the association lasting longer for males with low parent-child conflict.
Although high-quality family relationships in adolescence buffer the stresses of teenage life,48,49 our findings suggest that positive adolescent family relationships continue to be associated with benefits for mental health throughout the transition to adulthood and into midlife as individuals face various challenges that involve peer networking, continuing education, managing romantic relationships, building careers, climbing the social ladder, and starting new families.50,51 These sources of social and emotional support in early family life likely encourage the development of skills for coping with changing and cumulative stressors,24,25,26 promoting mental health throughout the life course from early adolescence to midlife and helping to prevent negative outcomes and premature deaths due to suicide, alcohol, or drugs in middle age.
Our findings emphasize the need for early preventive interventions of depression in adolescent family life. Given the profound transformations in neurologic, biological, cognitive, and social development during adolescence when the onset of depression occurs and its rates increase,52,53,54,55,56,57,58 mental health and other health education professionals should target this life stage for interventions in family settings. Public health initiatives that teach and encourage parents and family members to nurture positive family relationships with their adolescents will be most effective in fostering healthy mental development.12,13,14,59 Our research shows that this approach may not only promote mental health during the sensitive and vulnerable period of adolescence but also may be associated with lower risk of adult mental illness and potentially midlife premature deaths due to alcohol addiction, drug abuse, or suicide. Research is needed to better understand the mechanisms by which family cohesion promotes mental health outcomes for youth and young adults. Although theory suggests key mechanisms involve social support, help in working out problems, coping skills, and knowing there is someone to rely on in times of emotional need, research designs are needed to measure these family processes and test for their effectiveness.15,17,20,25 The skills and coping strategies that youth learn to cope with emotional problems may last across the life course and continue to promote mental health well into adulthood.
Limitations
There are some limitations to this study. First, our research focused on family relationships during adolescence and the development of depression into midlife. As such, specific measures of preadolescent family relationships were not examined (or available in our data source), which might also be associated with depression. However, we controlled for physical and sexual abuse before 12 years of age as a proxy to capture an overall picture of family interactions and risks before adolescence. Second, we did not use mother- or father-specific relational measures. Compared with measures from previous research based on retrospective reports with recollection errors,60,61,62 we believe that we improved the operationalization of adolescent family relationships by using prospective reports and comprehensive measures to capture several dimensions, such as emotional affection, bonding, and parental approval. Third, the measure of depressive symptoms in our study was self-reported and does not represent a clinical diagnosis. Future research should attempt to replicate our findings using a clinical measure in a longitudinal study.
Conclusions
In this study, females experienced higher levels of depressive symptoms than males throughout the life course from early adolescence to 40 years of age. During this life stage, females had the highest risks of depression during middle to late adolescence, whereas males had the highest risks of depression later, during their 30s and 40s. Positive adolescent family relationships were associated with better mental health among both females and males from early adolescence to midlife, with the association being stronger for females than males during adolescence and the transition to adulthood. Our findings appear to provide new understanding of the long-term association between early family relationships and lifetime development of depression.
eMethods. Supplementary Methods
eReferences
eTable 1. Sample Demographics and Study Characteristics - Weighted and Unweighted Results
eTable 2. Percentage of Selected Demographic and Socioeconomic Characteristics From Full, Analytical, and Non-Analytical Samples
eTable 3. Odds Ratios of Two Logistic Regressions on Positive Family Relation Measures - PWS Models
eTable 4. Weighted Coefficients of Gender-Specific Growth Curve Models Predicting CES-D by Levels of Family Cohesion, Female Sample (N = 9233), Add Health (1995 - 2017)
eTable 5. Weighted Coefficients of Gender-Specific Growth Curve Models Predicting CES-D by Levels of Family Cohesion, Male Sample (N = 8952), Add Health (1995 - 2017)
eTable 6. Weighted Coefficients of Gender-Specific Growth Curve Models Predicting CES-D by Levels of Parent-Child Conflict, Female Sample (N = 9233), Add Health (1995 - 2017)
eTable 7. Weighted Coefficients of Gender-Specific Growth Curve Models Predicting CES-D by Levels of Parent-Child Conflict, Male Sample (N = 8952), Add Health (1995 - 2017)
eFigure 1. Growth Curve of Standardized CES-D by Levels of Family Cohesion Across Ages 12-40 - Female
eFigure 2. Growth Curve of Standardized CES-D by Levels of Family Cohesion Across Ages 12-40 - Male
eFigure 3. Growth Curve of Standardized CES-D by Levels of Parent-Child Conflict Across Ages 12-40 - Female
eFigure 4. Growth Curve of Standardized CES-D by Levels of Parent-Child Conflict Across Ages 12-40 - Male
References
- 1.World Health Organization Depression. 2017. https://www.who.int/mediacentre/factsheets/fs369/en/. Accessed December 15, 2018.
- 2.Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):-. doi: 10.1016/S0140-6736(13)61611-6 [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Avenevoli S, Ries Merikangas K. Mood disorders in children and adolescents: an epidemiologic perspective. Biol Psychiatry. 2001;49(12):1002-1014. doi: 10.1016/S0006-3223(01)01129-5 [DOI] [PubMed] [Google Scholar]
- 4.Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH. Psychosocial functioning of young adults who have experienced and recovered from major depressive disorder during adolescence. J Abnorm Psychol. 2003;112(3):353-363. doi: 10.1037/0021-843X.112.3.353 [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC, Angermeyer M, Anthony JC, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6(3):168-176. [PMC free article] [PubMed] [Google Scholar]
- 6.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112(49):15078-15083. doi: 10.1073/pnas.1518393112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meara E, Skinner J. Losing ground at midlife in America. Proc Natl Acad Sci U S A. 2015;112(49):15006-15007. doi: 10.1073/pnas.1519763112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kochanek KD, Arias E, Bastian BA. The effect of changes in selected age-specific causes of death on non-Hispanic white life expectancy between 2000 and 2014. NCHS Data Brief. 2016;(250):1-8. [PubMed] [Google Scholar]
- 9.Stein EM, Gennuso KP, Ugboaja DC, Remington PL. The epidemic of despair among white Americans: trends in the leading causes of premature death, 1999-2015. Am J Public Health. 2017;107(10):1541-1547. doi: 10.2105/AJPH.2017.303941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Masters RK, Tilstra AM, Simon DH. Explaining recent mortality trends among younger and middle-aged white Americans. Int J Epidemiol. 2018;47(1):81-88. doi: 10.1093/ije/dyx127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Andrews G, Issakidis C, Sanderson K, Corry J, Lapsley H. Utilising survey data to inform public policy: comparison of the cost-effectiveness of treatment of ten mental disorders. Br J Psychiatry. 2004;184:526-533. doi: 10.1192/bjp.184.6.526 [DOI] [PubMed] [Google Scholar]
- 12.Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: a global public-health challenge. Lancet. 2007;369(9569):1302-1313. doi: 10.1016/S0140-6736(07)60368-7 [DOI] [PubMed] [Google Scholar]
- 13.Hogan P, Hogan BK. The family treatment of depression In: Flach FF, Draghi SC, eds. The Nature and Treatment of Depression. New York, NY: Wiley; 1978:197-228. [Google Scholar]
- 14.Young JF, Mufson L. Interpersonal psychotherapy for treatment and prevention of adolescent depression In: Abela JR, Hankin BL, eds. Handbook of Depression in Children and Adolescents. New York, NY: Guilford Press; 2008:288-306. [Google Scholar]
- 15.Allen JP, Porter M, McFarland C, McElhaney KB, Marsh P. The relation of attachment security to adolescents’ paternal and peer relationships, depression, and externalizing behavior. Child Dev. 2007;78(4):1222-1239. doi: 10.1111/j.1467-8624.2007.01062.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eberhart NK, Shih JH, Hammen CL, Brennan PA. Understanding the sex difference in vulnerability to adolescent depression: an examination of child and parent characteristics. J Abnorm Child Psychol. 2006;34(4):495-508. doi: 10.1007/s10802-006-9020-4 [DOI] [PubMed] [Google Scholar]
- 17.Meadows SO, Brown JS, Elder GH. Depressive symptoms, stress, and support: gendered trajectories from adolescence to young adulthood. J Youth Adolesc. 2006;35(1):89-99. doi: 10.1007/s10964-005-9021-6 [DOI] [Google Scholar]
- 18.Field T, Diego M, Sanders C. Adolescent depression and risk factors. Adolescence. 2001;36(143):491-498. [PubMed] [Google Scholar]
- 19.MacPhee AR, Andrews JJW. Risk factors for depression in early adolescence. Adolescence. 2006;41(163):435-466. [PubMed] [Google Scholar]
- 20.Makri-Botsari E. Risk/protective effects on adolescent depression: role of individual, family and peer factors. Psychol Stud (Mysore). 2005;50(1):50-61. [Google Scholar]
- 21.Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74(1):5-13. doi: 10.1016/S0165-0327(02)00426-3 [DOI] [PubMed] [Google Scholar]
- 22.Hyde JS, Mezulis AH, Abramson LY. The ABCs of depression: integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychol Rev. 2008;115(2):291-313. doi: 10.1037/0033-295X.115.2.291 [DOI] [PubMed] [Google Scholar]
- 23.Landman-Peeters KMC, Hartman CA, van der Pompe G, den Boer JA, Minderaa RB, Ormel J. Gender differences in the relation between social support, problems in parent-offspring communication, and depression and anxiety. Soc Sci Med. 2005;60(11):2549-2559. doi: 10.1016/j.socscimed.2004.10.024 [DOI] [PubMed] [Google Scholar]
- 24.Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;51(6):843-857. doi: 10.1016/S0277-9536(00)00065-4 [DOI] [PubMed] [Google Scholar]
- 25.Thoits PA. Mechanisms linking social ties and support to physical and mental health. J Health Soc Behav. 2011;52(2):145-161. doi: 10.1177/0022146510395592 [DOI] [PubMed] [Google Scholar]
- 26.Umberson D, Montez JK. Social relationships and health: a flashpoint for health policy. J Health Soc Behav. 2010;51(suppl):S54-S66. doi: 10.1177/0022146510383501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gariépy G, Honkaniemi H, Quesnel-Vallée A. Social support and protection from depression: systematic review of current findings in Western countries. Br J Psychiatry. 2016;209(4):284-293. doi: 10.1192/bjp.bp.115.169094 [DOI] [PubMed] [Google Scholar]
- 28.Mirowsky J, Ross CE. Social Causes of Psychological Distress. 2nd ed New York, NY: Aldine de Gruyter; 2003. [Google Scholar]
- 29.Sutin AR, Terracciano A, Milaneschi Y, An Y, Ferrucci L, Zonderman AB. The trajectory of depressive symptoms across the adult life span. JAMA Psychiatry. 2013;70(8):803-811. doi: 10.1001/jamapsychiatry.2013.193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cyranowski JM, Frank E, Young E, Shear MK. Adolescent onset of the gender difference in lifetime rates of major depression: a theoretical model. Arch Gen Psychiatry. 2000;57(1):21-27. doi: 10.1001/archpsyc.57.1.21 [DOI] [PubMed] [Google Scholar]
- 31.Harris KM, Halpern CT, Whitsel EA, et al. Cohort profile: the National Longitudinal Study of Adolescent to Adult Health (Add Health) [published online June 29, 2019]. Int J Epidemiol. doi: 10.1093/ije/dyz115 [DOI] [PMC free article] [PubMed]
- 32.Harris KM, Halpern CT, Hussey J, et al. Social, behavioral, and genetic linkages from adolescence into adulthood. Am J Public Health. 2013;103(suppl 1):S25-S32. doi: 10.2105/AJPH.2012.301181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385-401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- 34.Perreira KM, Deeb-Sossa N, Harris KM, Bollen K. What are we measuring? an evaluation of the CES-D across race/ethnicity and immigrant generation. Soc Forces. 2005;83(4):1567-1601. doi: 10.1353/sof.2005.0077 [DOI] [Google Scholar]
- 35.Radloff LS. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. J Youth Adolesc. 1991;20(2):149-166. doi: 10.1007/BF01537606 [DOI] [PubMed] [Google Scholar]
- 36.Jensen TM, Harris KM. Stepfamily relationship quality and stepchildren’s depression in adolescence and adulthood. Emerg Adulthood. 2017;5(3):191-203. doi: 10.1177/2167696816669901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Harris KM, Gerken K, Chen P, Yang YC Social integration and health from adolescence into adulthood. Presented at the: DeJong Lecture in Social Demography; November 12, 2016; Pennsylvania State University, University Park, Pennsylvania. [Google Scholar]
- 38.Chow GC. Tests of equality between sets of coefficients in two linear regressions. Econometrica. 1960;28(3):591. doi: 10.2307/1910133 [DOI] [Google Scholar]
- 39.Gould W. Can You Explain Chow Tests? https://www.stata.com/support/faqs/statistics/chow-tests/. Accessed March 23, 2019.
- 40.Imbens GW. Nonparametric estimation of average treatment effects under exogeneity: a review. Rev Econ Stat. 2004;86(1):4-29. doi: 10.1162/003465304323023651 [DOI] [Google Scholar]
- 41.Robins JM. Association, causation, and marginal structural models. Synthese. 1999;121(1-2):151-179. doi: 10.1023/A:1005285815569 [DOI] [Google Scholar]
- 42.Sato T, Matsuyama Y. Marginal structural models as a tool for standardization. Epidemiology. 2003;14(6):680-686. doi: 10.1097/01.EDE.0000081989.82616.7d [DOI] [PubMed] [Google Scholar]
- 43.Harris KM, Chen P The acculturation of parent-child relations in immigrant families. Paper presented at: Annual Meeting of the Population Association of America; April 2, 2004; Boston, Massachusetts. [Google Scholar]
- 44.Chen P, Chantala K. Guidelines for Analyzing Add Health Data. Chapel Hill: Carolina Population Center, University of North Carolina at Chapel Hill; 2014. [Google Scholar]
- 45.Singer JD, John B. Willett. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. London, England: Oxford University Press; 2003. doi: 10.1093/acprof:oso/9780195152968.001.0001 [DOI] [Google Scholar]
- 46.Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. 2nd ed Thousand Oaks, California: Sage Publications, Inc; 2002:512. [Google Scholar]
- 47.Rabe-Hesketh S, Skrondal A. Multilevel and Longitudinal Modeling Using Stata. 3rd ed College Station, TX: Stata Press Publication; 2012. [Google Scholar]
- 48.Stice E, Ragan J, Randall P. Prospective relations between social support and depression: differential direction of effects for parent and peer support? J Abnorm Psychol. 2004;113(1):155-159. doi: 10.1037/0021-843X.113.1.155 [DOI] [PubMed] [Google Scholar]
- 49.Armsden GC, Greenberg MT. The inventory of parent and peer attachment: individual differences and their relationship to psychological well-being in adolescence. J Youth Adolesc. 1987;16(5):427-454. doi: 10.1007/BF02202939 [DOI] [PubMed] [Google Scholar]
- 50.McNeely C, Blanchard J. The Teen Years Explained: A Guide to Healthy Adolescent Development. Baltimore, MD: Johns Hopkins Bloomberg School of Public Health: Center for Adolescent Health; 2009. [Google Scholar]
- 51.Bonnie RJ, Stroud C, Breiner H; Committee on Improving the Health, Safety, and Well-Being of Young Adults, Board on Children, Youth, and Families, Institute of Medicine . National Research Council. Investing in the Health and Well-Being of Young Adults. Washington, DC: National Academies Press; 2015. [PubMed] [Google Scholar]
- 52.Takeuchi Y, Matsushita H, Sakai H, Kawano H, Ochi M. Developmental changes in cerebrospinal fluid concentrations of monoamine-related substances in patients with dentatorubral-pallidoluysian atrophy. J Child Neurol. 2001;16(2):79-82. doi: 10.1177/088307380101600202 [DOI] [PubMed] [Google Scholar]
- 53.Sawyer SM, Afifi RA, Bearinger LH, et al. Adolescence: a foundation for future health. Lancet. 2012;379(9826):1630-1640. doi: 10.1016/S0140-6736(12)60072-5 [DOI] [PubMed] [Google Scholar]
- 54.Spear LP. The adolescent brain and age-related behavioral manifestations. Neurosci Biobehav Rev. 2000;24(4):417-463. doi: 10.1016/S0149-7634(00)00014-2 [DOI] [PubMed] [Google Scholar]
- 55.Case R. Intellectual Development: Birth to Adulthood. Orlando, FL: Academic Press; 1985. [Google Scholar]
- 56.Chalmers D, Lawrence JA. Investigating the effects of planning aids on adults’ and adolescents’ organisation of a complex task. Int J Behav Dev. 1993;16(2):191-214. doi: 10.1177/016502549301600206 [DOI] [Google Scholar]
- 57.Angold A, Costello EJ. Depressive comorbidity in children and adolescents: empirical, theoretical, and methodological issues. Am J Psychiatry. 1993;150(12):1779-1791. doi: 10.1176/ajp.150.12.1779 [DOI] [PubMed] [Google Scholar]
- 58.Abela JR, Hankin BL. Depression in children and adolescents: causes, treatment, and prevention In: Abela JR, Hankin BL, eds. Handbook of Depression in Children and Adolescents. New York, NY: The Guilford Press; 2008:3-5. [Google Scholar]
- 59.Yap MBH, Pilkington PD, Ryan SM, Jorm AF. Parental factors associated with depression and anxiety in young people: a systematic review and meta-analysis. J Affect Disord. 2014;156:8-23. doi: 10.1016/j.jad.2013.11.007 [DOI] [PubMed] [Google Scholar]
- 60.Crook T, Raskin A, Eliot J. Parent-child relationships and adult depression. Child Dev. 1981;52(3):950-957. doi: 10.2307/1129099 [DOI] [PubMed] [Google Scholar]
- 61.Enns MW, Cox BJ, Clara I. Parental bonding and adult psychopathology: results from the US National Comorbidity Survey. Psychol Med. 2002;32(6):997-1008. doi: 10.1017/S0033291702005937 [DOI] [PubMed] [Google Scholar]
- 62.Russek LG, Schwartz GE. Perceptions of parental caring predict health status in midlife: a 35-year follow-up of the Harvard Mastery of Stress Study. Psychosom Med. 1997;59(2):144-149. doi: 10.1097/00006842-199703000-00005 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Supplementary Methods
eReferences
eTable 1. Sample Demographics and Study Characteristics - Weighted and Unweighted Results
eTable 2. Percentage of Selected Demographic and Socioeconomic Characteristics From Full, Analytical, and Non-Analytical Samples
eTable 3. Odds Ratios of Two Logistic Regressions on Positive Family Relation Measures - PWS Models
eTable 4. Weighted Coefficients of Gender-Specific Growth Curve Models Predicting CES-D by Levels of Family Cohesion, Female Sample (N = 9233), Add Health (1995 - 2017)
eTable 5. Weighted Coefficients of Gender-Specific Growth Curve Models Predicting CES-D by Levels of Family Cohesion, Male Sample (N = 8952), Add Health (1995 - 2017)
eTable 6. Weighted Coefficients of Gender-Specific Growth Curve Models Predicting CES-D by Levels of Parent-Child Conflict, Female Sample (N = 9233), Add Health (1995 - 2017)
eTable 7. Weighted Coefficients of Gender-Specific Growth Curve Models Predicting CES-D by Levels of Parent-Child Conflict, Male Sample (N = 8952), Add Health (1995 - 2017)
eFigure 1. Growth Curve of Standardized CES-D by Levels of Family Cohesion Across Ages 12-40 - Female
eFigure 2. Growth Curve of Standardized CES-D by Levels of Family Cohesion Across Ages 12-40 - Male
eFigure 3. Growth Curve of Standardized CES-D by Levels of Parent-Child Conflict Across Ages 12-40 - Female
eFigure 4. Growth Curve of Standardized CES-D by Levels of Parent-Child Conflict Across Ages 12-40 - Male