Abstract
Objective:
To estimate the percentage of young, sexually active Medicaid-insured women who were tested for chlamydia by age, race/ethnicity, and history of sexually transmitted disease (STD) diagnosis.
Methods:
We used the medical diagnostic and procedural codes from Truven Health MarketScan Medicaid claims data from 10 states in 2012 and 2013 to estimate the rates of chlamydia testing in 2013 and previous STD diagnosis (diagnosed in 2012) among Medicaid-insured women aged 15–25 years who were sexually active in 2013. We also used a logit model to assess the association between chlamydia testing and women’s age, race/ethnicity, and previous STD diagnosis.
Results:
Overall, among approximately 261,000 Medicaid-insured women aged 15–25 years in 2013 who were classified as sexually active, 50.2% were tested for chlamydia in 2013. The chlamydia testing rate was 45.6% for white women and 57.5% for black women. The chlamydia testing rate was 63.5% for women diagnosed as having an STD in 2012 and 46.8% for women not diagnosed as having an STD in 2012. The chlamydia testing rate was significantly (P < 0.05) associated with previous STD diagnosis, age, and race/ethnicity in our logit model.
Conclusions:
Higher chlamydia testing rates among black women can be explained in part by higher rates of previous STD diagnoses. Our finding that black women have the highest chlamydia testing rates is encouraging, as improved access to STD prevention services among racial/ethnic minorities can help to reduce racial/ethnic disparities in STDs. However, chlamydia screening remains an underused preventive health service for young women of all racial and ethnic groups.
Chlamydia is the most prevalent and most costly bacterial sexually transmitted disease (STD) in the United States, with an estimated 2.9 million cases occurring annually with direct medical costs of more than $500 million.1,2 Approximately two-thirds of reported chlamydial infections occur among persons aged 15 to 24 years.3 Among females in this age group, the reported chlamydia rate among blacks was more than 4 times that of whites in 2013.3 Chlamydia rates are typically higher in women with Medicaid insurance than in women with private insurance.4 If left untreated, chlamydial infection can lead to serious and costly sequelae including pelvic inflammatory disease, ectopic pregnancy, infertility, and chronic pelvic pain.5–7
Chlamydia is easily diagnosed as having highly sensitive and specific tests that use genital or urine specimens and can be effectively treated with inexpensive single- or multiple-dose oral therapies.8,9 Because chlamydial infection is asymptomatic in up to 70% of women,10,11 annual chlamydia screening for sexually active women 24 years and younger has been recommended by many health organizations, such as the American College of Obstetricians and Gynecologists, the US Preventive Services Task Force, and the Centers for Disease Control and Prevention.8,11,12 The Centers for Disease Control and Prevention’s guidelines have recently been revised; previously, screening sexually active women 25 years and younger was recommended.13 To monitor national chlamydia screening practices, the National Committee for Quality Assurance added chlamydia testing as one of the performance measures in the Healthcare Effectiveness Data and Information Set (HEDIS) in 2000.14 Chlamydia testing rates increased from 40.4% in 2001 to 57.5% in 2010 among sexually active women aged 16 to 24 years who were enrolled in a Medicaid program.15 Despite this increase, chlamydia screening in women younger than 25 years remains an underused preventive health service.16–18
Although HEDIS is a tool used by 90% of US health plans to evaluate the quality of health care services, it does not track chlamydia screening by race/ethnicity and lacks information related to STD diagnosis.14 Studies have shown that women with Medicaid insurance are significantly more likely to report receiving a chlamydia test in the last 12 months compared with women with private or no insurance19 and that chlamydia testing rates are significantly higher among black women than white women.4,16,20 Our study aims to expand and update the existing literature by using the most recently available administrative claims data to examine chlamydia testing among young Medicaid-insured women in 2013. Specifically, the objectives of this study were to (1) estimate annual chlamydia testing rates by race/ethnicity, age, and previous STD diagnosis among sexually active women aged 15–25 years, and (2) examine the association between chlamydia testing rates and race/ethnicity, age, and previous STD diagnosis.
METHODS
We analyzed Truven Health MarketScan Medicaid claims data for 2012 and 2013. The MarketScan Medicaid database integrates administrative claims data of approximately 7 million beneficiaries from 10 US states in 2013 and includes person-specific enrollment and use information such as places of service, physician or hospital visits, diagnosis codes, procedure codes, retail or mail order of prescription drugs, other billing-related information, and carve-out services. The Medicaid claims data we used included information regarding the length of patient enrollment, patient demographics, service provision dates, and diagnostic codes (International Classification of Disease, Ninth Revision) and procedural codes (Physician’s Current Procedural Terminology). The geographic identifying information (including region or state) was unavailable to us due to confidentiality agreements between state Medicaid programs and Truven Health Analytics. Because the database involves de-identified medical claims of patient encounter data, institutional review board review was not required for this study.
From the database, we selected a study population consisting of Medicaid-insured women aged 15 to 25 years who were continuously enrolled in 2013 and had at least 1 claim in 2012. We excluded women not continuously enrolled, as defined by having a gap in coverage of 60 days or more in the database. Using previously adopted methods to calculate the HEDIS measure of chlamydia screening,14 we classified women as sexually active if they had any claim in the inpatient services, outpatient claims, or prescription claims data that specified a diagnosis, procedure, or prescription code for a Papanicolaou test or pelvic examination, a pregnancy-related service, a contraceptive service, an infertility-related service, or an STD-related service during 2013.14,20 We classified women as having a previously diagnosed STD if they had any claim in 2012 indicating a diagnosis code for chlamydia, syphilis, gonorrhea, HIV, herpes, HPV, chancroid, and trichomoniasis. In addition to classifying women according to previous STD diagnosis in 2012, we also examined 2 subclassifications: women diagnosed as having chlamydia in 2012 and women diagnosed as having other STDs (but not chlamydia) in 2012. We identified chlamydia testing in the 2013 administrative claims data using the same Physician’s Current Procedural Terminology codes that are used to define chlamydia testing in the HEDIS measure.14 Race/ethnicity in the data set we used has been precoded with 4 categories: Hispanics, white, black, and other. Using χ2 tests, we compared these 2 outcomes (percent sexually active, percent tested for chlamydia, and percent with a previous STD diagnosis) by age and race/ethnicity. Using a logit model, we assessed the association between chlamydia testing rates and race/ethnicity, age, and previous STD diagnosis. Statistically significant differences were defined as those with a 2-tailed probability less than 0.05. We used SAS software version 9.3 (SAS Institute, Cary, NC) for all statistical analyses.
RESULTS
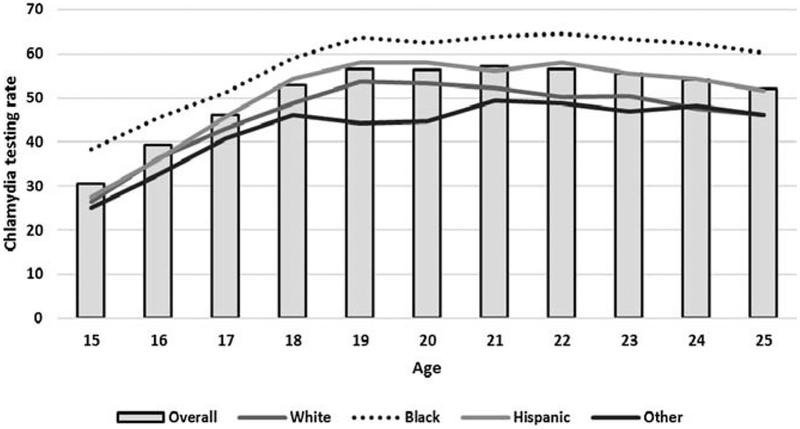
Of approximately 410,000 Medicaid-insured women aged 15 to 25 years who were enrolled in Medicaid program without a gap of 60 days of coverage in 2013 and who had at least 1 medical claim in 2012, 64% were classified as sexually active in 2013 (Table 1). The chlamydia testing rate among sexually active women aged 15 to 25 years was 50.2% overall but varied significantly by race/ethnicity, age, and previous STD diagnosis (Table 1 and Fig. 1). Black women were most likely to be tested for chlamydia, as the chlamydia testing rate was 57.5% in black women, 45.6% in white women, 47.8% in Hispanic women, and 42.7% in other women (P < 0.05).
TABLE 1.
Classification of Women Aged 15 to 25 Years Enrolled in Medicaid Program, MarketScan Medicaid Data 2012–2013
| No. Women, 2013* | Sexually Active Women, 2013 | % | No. Tested for Chlamydia, 2013 | % | Had Chlamydia Diagnosis, 2012 | % | Had Other STD Diagnosis, 2012 | % | Had any STD Diagnosis, 2012 | % | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 410,052 | 260,881 | 63.6 | 131,012 | 50.2 | 11,820 | 4.5 | 47,279 | 18.1 | 53,980 | 20.7 |
| Age group†, y | |||||||||||
| 15–19 | 271,913 | 140,840 | 51.8 | 64,606 | 45.9 | 6573 | 4.7 | 16,823 | 11.9 | 21,173 | 15.0 |
| 20–25 | 138,139 | 120,041 | 86.9 | 66,406 | 55.3 | 5247 | 4.4 | 30,456 | 25.4 | 32,807 | 27.3 |
| Race/Ethnicity‡ | |||||||||||
| White | 183,524 | 118,056 | 64.3 | 53,847 | 45.6 | 4732 | 4.0 | 16,042 | 13.6 | 19,422 | 16.5 |
| Black | 157,755 | 105,791 | 67.1 | 60,881 | 57.5 | 5668 | 5.4 | 25,744 | 24.3 | 28,153 | 26.6 |
| Hispanics | 20,367 | 9467 | 46.5 | 4522 | 47.8 | 323 | 3.4 | 1148 | 12.1 | 1376 | 14.5 |
| Other | 48,406 | 27,567 | 56.9 | 11,762 | 42.7 | 1097 | 4.0 | 4345 | 15.8 | 5029 | 18.2 |
The number of sexually active women was used as the denominator to calculate the percent tested for chlamydia and the percent with chlamydia diagnosis, other STD diagnosis, and any STD diagnosis.
Women aged 15 to 25 years who had at least 1 claim in 2012 and had no gap of at least 60 days in coverage in 2013.
P < 0.05 for comparison of age groups for all columns in table.
P < 0.05 for comparison of race/ethnicity for all columns in table.
FIGURE 1.
Chlamydia testing rate (percent of women tested in 2013) among women aged 15 to 25 years who were classified as sexually active by race/ethnicity.
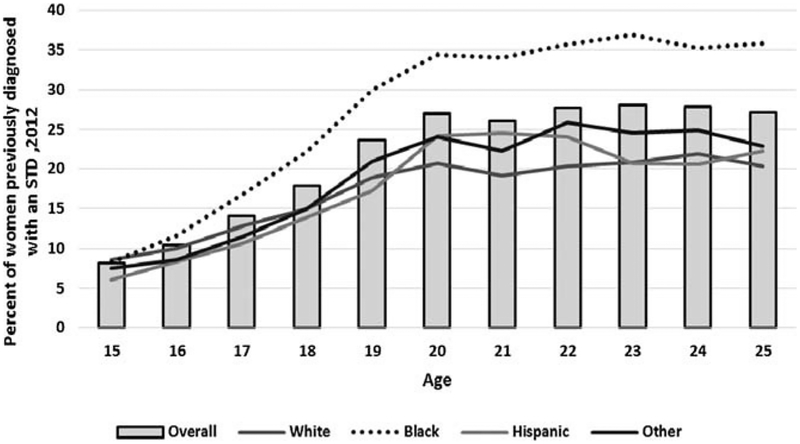
The previous STD diagnosis rate was 20.7% overall, 26.6% for blacks, 16.5% for whites, and 14.5% for Hispanics. Black women were significantly more likely (P < 0.05) to be diagnosed as having a previous STD than white women (Fig. 2). Among sexually active women with a previous STD diagnosis, 37% were not tested for chlamydia overall, and specifically 31% in black and 43% in white (Table 2).
FIGURE 2.
Previous STD diagnosis rate (percent of women previously diagnosed as having an STD in 2012) among women aged 15 to 25 years who were classified as sexually active in 2013 by race/ethnicity.
TABLE 2.
Chlamydia Testing Rate (Percent of Women Tested in 2013) Among Sexually Active Women Aged 15 to 25 Years Overall and by Previous STD Diagnosis, Age, and Race/Ethnicity, in Logit Model, MarketScan Medicaid Data 2013
| Characteristic | No. Women | % Tested for Chlamydia, 2013 | Odds Ratio | Adjusted Odds Ratio* | Adjusted 95% CI |
|---|---|---|---|---|---|
| Total | 260,881 | 50.2 | |||
| Had any STD diagnosis, 2012 | |||||
| Yes | 53,980 | 63.5 | 1.00 | 1.00 | (Referent) |
| No | 206,901 | 46.8 | 0.51 | 0.56 | 0.55–0.57 |
| Age, y | |||||
| 15–19 | 140,840 | 45.9 | 0.68 | 0.74 | 0.73–0.75 |
| 20–25 | 120,041 | 55.3 | 1.00 | 1.00 | (Referent) |
| Race/Ethnicity | |||||
| White | 118,056 | 45.6 | 1.00 | 1.00 | (Referent) |
| Black | 105,791 | 57.5 | 1.62 | 1.53 | 1.50–1.55 |
| Hispanic | 9467 | 47.8 | 1.09 | 1.16 | 1.11–1.21 |
| Other | 27,567 | 42.7 | 0.89 | 0.87 | 0.85–0.90 |
Logistic regression model included 2012 STD diagnosis status, age group, and race/ethnicity group.
CI indicates confidence interval.
In our logit model, previous STD diagnosis, after adjusting by age and race/ethnicity, was significantly associated with chlamydia testing rate. Women without an STD diagnosis in 2012, compared with those with an STD diagnosis in 2012, were less likely to be tested for chlamydia in 2013 (odds ratios and 95% confidence interval 0.56 [0.55–0.57]). Black women were more likely to be tested for chlamydia than white women (odds ratio and 95% confidence interval 1.53 [1.50–1.55]).
DISCUSSION
Approximately half of sexually active Medicaid-enrolled women aged 15 to 25 years in our sample were tested for chlamydia in 2013, suggesting that chlamydia screening remains an underused preventive health service in this population. We found that the chlamydia testing rate and the STD diagnosis rate for black women enrolled in Medicaid were the highest among all race/ethnicity groups, regardless of age. Among sexually active black women aged 15 to 25 years, 57% were tested for chlamydia and 27% were previously diagnosed as having an STD. Black women were more likely to be tested for chlamydia than white women even after controlling for age and STD diagnosis status (adjusted odds ratio, 1.53). This finding supports survey data based on self-report that have found higher rates of chlamydia testing in non-Hispanic black women than in Hispanic or non-Hispanic white women.4
Our finding of higher previous STD diagnosis rates for black women is consistent with the extensive literature that documents racial and ethnic disparities in the burden of STDs.3,21,22 Our finding of higher chlamydia testing rates for black women is consistent with the relatively few studies that have examined chlamydia testing rates by race/ethnicity.16,20 Given the disproportionate burden of STDs among blacks, the higher chlamydia testing rates among black women are encouraging. These higher testing rates are even more encouraging when considered in light of documented patterns of health care provider performance across a variety of measures, in which providers caring for predominantly minority populations do not perform as well on average compared with their counterparts who care for nonminority populations.23 Addressing the populations at higher risk through screening interventions would eventually help reduce disparities in STD.
Christiansen-Lindquist and colleagues20 showed that Medicaid claims data could be used to assess chlamydia testing rates by race/ethnicity as well as trends in these rates over time. They hypothesized that the higher chlamydia testing rates among black women may be due to different chlamydia prevalence rates across subpopulations, and noted that future research is needed to help understand the reasons for racial/ethnic differences in chlamydia testing rates. Our analysis contributes to this literature by showing that the claims data allow for the comparison of testing rates by race/ethnicity to be adjusted by age and previous STD diagnosis status. By doing so, we can examine whether higher chlamydia testing rates among black women can be explained by higher rates of previous STD diagnoses among black women at the individual level. We found that previous STD diagnosis explained some—but not all—of the differences in chlamydia testing rates by race/ethnicity. Higher chlamydia testing rates among black women might also be explained by higher chlamydia prevalence rates among black women as a group in addition to higher rates of previous STD diagnoses at the individual level. For example, we found that higher chlamydia testing rates among black women were noticeable beginning at age 15 years (Fig. 1) whereas higher rates of previous STD diagnosis among black women were not noticeable until the later teen years (Fig. 2).
Our study has several limitations. First, because the claims data do not include information on sexual behavior (e.g., having a new sex partner or multiple sex partners), we could not estimate chlamydia testing rates among women with these behavioral risk factors. Second, because our data are from 10 states and may not be nationally representative (7 million Medicaid enrollees in these 10 states vs. 68 million Medicaid enrollees in the United States), our results cannot be generalized to all women enrolled in Medicaid. However, our estimated chlamydia testing rate (50.2%) in this study was similar to that (54.9%) reported from the State of Health Care Quality Report based on the 2013 HEDIS chlamydia testing measure. Third, a high proportion (44%) of women who experienced a gap or gaps in coverage were excluded due to eligibility criteria, although they might be diagnosed as having chlamydia or other STDs. Fourth, our estimates of chlamydia testing rates could be biased upward or downward. Specifically, we may have overestimated chlamydia testing rates among those sexually active if we underestimated the percentage of women who are sexually active.24,25 For example, women might be sexually active without seeking medical care for sexual health–related services. However, the percentage of women we classified as being sexually active is consistent with the percentages identified by the 2006–2008 National Survey of Family Growth.16,26 Our estimates of chlamydia testing rates might also overestimate the true chlamydia screening rates because the claims data do not provide a clear distinction between chlamydia tests performed on symptomatic versus asymptomatic women. On the other hand, we may have underestimated chlamydia testing rates if the Medicaid claims data did not capture all medical care encounters at which chlamydia testing was performed. Finally, we defined women as having an STD based on diagnosis codes, but the databases do not have test results. Diagnosis codes entered at the time of the initial visit may not correlate with test results.27,28
Consistent with previous studies, we found that chlamydia testing rates in young sexually active Medicaid-insured women remain suboptimal. The potential for improvement in chlamydia testing rates was illustrated by our finding that many women diagnosed as having an STD had not been tested for chlamydia. Current screening recommendations note that more frequent STD testing might be appropriate for those with a history of STD diagnosis.8,12 However, 2 encouraging aspects of our study are (1) the demonstration that many health care providers adhere to chlamydia testing guidelines and (2) the documentation of higher chlamydia testing rates among black women. A review by Guy and colleagues29 reports several effective interventions to increase chlamydia screening rates, such as educational activities (workshops for clinical staff and online continuing medical education programs), provision of free sexual health consultations, and strategies to routinize chlamydia screening (computer prompts for doctors, linking chlamydia screening to routine Papanicolaou testing, and providing patients with a urine specimen jar prior to their examination). Although several effective interventions have been identified, additional interventions are needed. Studies such as ours of chlamydia testing rates can help not only to inform the development and targeting of future interventions but also to assess the impact of these interventions over time by monitoring trends in chlamydia testing rates.
Footnotes
Conflict of interest: None declared.
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Owusu-Edusei K Jr, Chesson HW, Gift TL, et al. The estimated direct medical cost of selected sexually transmitted infections in the United States, 2008. Sex Transm Dis 2013; 40:197–201. [DOI] [PubMed] [Google Scholar]
- 2.Satterwhite CL, Torrone E, Meites E, et al. Sexually transmitted infections among US women and men: Prevalence and incidence estimates, 2008. Sex Transm Dis 2013; 40:187–193. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. 2013 Sexually Transmitted Disease Surveillance: Chlamydia. Atlanta, GA: Department of Health and Human Services; 2014. Available at: http://www.cdc.gov/std/stats13/default.htm. Accessed January 15, 2015. [Google Scholar]
- 4.Tao G, Hoover KW, Leichliter JS, et al. Self-reported Chlamydia testing rates of sexually active women aged 15–25 years in the United States, 2006–2008. Sex Transm Dis 2012; 39:605–607. [DOI] [PubMed] [Google Scholar]
- 5.Haggerty CL, Gottlieb SL, Taylor BD, et al. Risk of sequelae after Chlamydia trachomatis genital infection in women. J Infect Dis 2010; 201 (suppl 2):S134–S155. [DOI] [PubMed] [Google Scholar]
- 6.Oakeshott P, Kerry S, Aghaizu A, et al. Randomised controlled trial of screening for Chlamydia trachomatis to prevent pelvic inflammatory disease: the POPI (Prevention Of Pelvic Infection) trial. BMJ 2010; 340:c1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Westrom L, Joesoef R, Reynolds G, et al. Pelvic inflammatory disease and fertility. A cohort study of 1,844 women with laparoscopically verified disease and 657 control women with normal laparoscopic results. Sex Transm Dis 1992; 19:185–192. [PubMed] [Google Scholar]
- 8.Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 2015; 64:1–137. [PMC free article] [PubMed] [Google Scholar]
- 9.Recommendations for the laboratory-based detection of Chlamydia trachomatis and Neisseria gonorrhoeae—2014. MMWR Recomm Rep 2014; 63:1–19. [PMC free article] [PubMed] [Google Scholar]
- 10.Stamm W, ed. Chlamydia Trachomatis Infections of the Adult. 4th ed: Mc Graw Hill Medical, 2008. [Google Scholar]
- 11.American College of Obstetricians and Gynecologists. Spotlight on Chlamydia: Annual Screenings a Must for Young Women. San Diego, CA: American College of Obstetricians and Gynecologists, 2007. [Google Scholar]
- 12.Meyers D, Wolff T, Gregory K, et al. USPSTF recommendations for STI screening. Am Fam Physician 2008; 77:819–824. [PubMed] [Google Scholar]
- 13.Workowski KA, Berman S. Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep 2010; 59:1–110. [PubMed] [Google Scholar]
- 14.HEDIS 2013: Technical Specifications. National Committee for Quality Assurance 2013.
- 15.Chlamydia screening among sexually active young female enrollees of health plans—United States, 2000–2007. MMWR Morb Mortal Wkly Rep 2009; 58:362–365. [PubMed] [Google Scholar]
- 16.Hoover KW, Leichliter JS, Torrone EA, et al. Chlamydia screening among females aged 15–21 years—Multiple data sources, United States, 1999–2010. Mortal Wkly Rep Surveill Summ 2014; 63(suppl 2):80–88. [PubMed] [Google Scholar]
- 17.Hoover K, Tao G. Missed opportunities for chlamydia screening of young women in the United States. Obstet Gynecol 2008; 111:1097–1102. [DOI] [PubMed] [Google Scholar]
- 18.Berman SM, Satterwhite CL. A paradox: Overscreening of older women for chlamydia while too few younger women are being tested. Sex Transm Dis 2011; 38:130–132. [DOI] [PubMed] [Google Scholar]
- 19.Nguyen TQ, Ford CA, Kaufman JS, et al. Infrequent chlamydial testing among young adults: Financial and regional differences. Sex Transm Dis 2008; 35:725–730. [DOI] [PubMed] [Google Scholar]
- 20.Christiansen-Lindquist L, Tao G, Hoover K, et al. Chlamydia screening of young sexually active, Medicaid-insured women by race and ethnicity, 2002–2005. Sex Transm Dis 2009; 36:642–646. [DOI] [PubMed] [Google Scholar]
- 21.Newman LM, Berman SM. Epidemiology of STD disparities in African American communities. Sex Transm Dis 2008; 35:S4–S12. [DOI] [PubMed] [Google Scholar]
- 22.Hogben M, Leichliter JS. Social determinants and sexually transmitted disease disparities. Sex Transm Dis 2008; 35:S13–S18. [DOI] [PubMed] [Google Scholar]
- 23.Blustein J Who is accountable for racial equity in health care? JAMA 2008; 299:814–816. [DOI] [PubMed] [Google Scholar]
- 24.Khosropour CM, Broad JM, Scholes D, et al. Estimating chlamydia screening coverage: A comparison of self-report and health care effectiveness data and information set measures. Sex Transm Dis 2014; 41:665–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tao G, Hua J, Chen JL. Understanding sexual activity and chlamydia testing rate based on linked national survey and medicaid claims data. PLoS One 2015; 10:e0122927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mosher WD, Chandra A, Jones J. Sexual behavior and selected health measures: Men and women 15–44 years of age, United States, 2002. Adv Data; 2005:1–55. [PubMed] [Google Scholar]
- 27.Jenkins WD, Zahnd W, Kovach R, et al. Chlamydia and gonorrhea screening in United States emergency departments. J Emerg Med 2013; 44: 558–567. [DOI] [PubMed] [Google Scholar]
- 28.Andric B, Drowos J, Trepka MJ, et al. High frequencies of negative pretreatment results following presumptive antibiotic treatment for chlamydia and gonorrhea. South Med J 2013; 106:321–326. [DOI] [PubMed] [Google Scholar]
- 29.Guy RJ, Ali H, Liu B, et al. Efficacy of interventions to increase the uptake of chlamydia screening in primary care: A systematic review. BMC Infect Dis 2011; 11:211. [DOI] [PMC free article] [PubMed] [Google Scholar]