Summary
We investigated risk factors associated with HIV infection in women who accepted voluntary counselling and testing (VCT) intrapartum. A survey questionnaire containing information on sociodemographic characteristics was administered to parturients at the Central Hospital Kigali after informed consent had been obtained. Participants were then offered VCT for HIV, and those who accepted were informed of their results. Of the 427 eligible participants, 317 accepted VCT (74.2%). The results of 312 (98.4%) of these women were obtained and 50 tested positive for HIV, yielding an HIV seroprevalence of 16.0% intrapartum. Women who had been pregnant three or more times were three times as likely to test positive for HIV in comparison to those of lower parity (OR = 2.9; 95% confidence interval (CI) = 1.1 – 8.0). This finding contradicts earlier studies performed antenatally among women of childbearing age and pregnant women in general. This may be attributable to some inadequacy in the existing health-care infrastructure to effectively detect HIV in multiparous women antenatally, or may represent a signal that a change in the nature of the epidemic in Rwanda is occurring.
Introduction
Rwanda is a country with a high burden of HIV/AIDS. About 5.1% of the Rwandan population are HIV-positive, and approximately 2.5% have AIDS (United Nations, 2001), making it one of the countries with the highest rates in the world. The prevalence is 29% (Allen et al., 1991) among women of childbearing age and 20% (Nkowane et al., 1991) among pregnant women attending antenatal clinics in Kigali, the capital of Rwanda. This has serious implications, not just for maternal health but also for the health of the child. Studies have shown that HIV seropositive status in the pregnant mother is associated with adverse pregnancy outcomes (Leroy et al., 1998). There is a serious possibility that the child may become infected with HIV, and the leading cause of HIV infection in children is mother to child transmission (Falloon et al., 1989).
New research reveals that single-dose Nevirapine therapy to the mother while in labour (intrapartum) and a dose to the child after birth can reduce the rate of mother to child transmission of HIV (Guay et al., 1999). Hence the spread of HIV to the child can be reduced in women presenting in labour regardless of whether or not they have had any prenatal care. This is a relatively inexpensive intervention that could save lives of children born to HIV-positive women.
To our knowledge, however, there has not been any study looking at the risk factors associated with HIV positivity specifically in women in labour (intrapartum) in Rwanda. In order to reduce mother to child transmission of HIV in a developing country such as Rwanda, one must take into account the fact that many women present intrapartum or very late in pregnancy without any previous prenatal care. Various studies have discussed reasons for poor usage of antenatal care clinics (McCaw-Binns et al., 1995; Adamu et al., 2002). Studies have also revealed that there are certain socio-economic and behavioral differences between women who attend antenatal clinics intrapartum or late in pregnancy (third trimester) and women who attend earlier (Adamu et al., 2002).
It is also probable that women who start attending antenatal clinics early in their pregnancy may not be offered voluntary counselling and testing (VCT) earlier in the course of their pregnancy and hence may be missed, underscoring the importance of investigating factors associated with HIV seropositivity in women intrapartum.
In this study, we sought to determine factors predictive of HIV-seropositivity identified among women during labour and delivery at the Central Hospital, in Kigali, Rwanda.
Methods
Study design and participants
Our study involved a cross-sectional survey of pregnant women in labour who attended the Central Hospital Kigali (CHK). Study participants were 19 – 45 years age. They were admitted to the delivery ward over a 2-month period in 2001. After obtaining informed consent, a pilot-tested questionnaire was administered to women with the assistance of the nurses at the hospital. The nurses translated and administered the questionnaire in the Rwandan local language of Kinyarwanda. The questionnaire obtained information on various sociodemographic factors. These included age, number of children living, parity, marital status, educational level and employment of the woman and her current partner.
After administration of the questionnaire, each participant was given the opportunity to receive confidential HIV testing, counselling and treatment by the hospital staff. All blood samples were screened for antibodies to HIV by the HIV determine test (Abbott, Abbott Park, IL, USA). Confirmatory tests were performed on samples that were positive using the HIV spot test (Genelabs Diagnostics, Singapore). Parturients were informed of their HIV status while they waited to deliver their babies. The study protocol was approved by the Institutional Review Board, University Alabama at Birmingham and the Ethics Committee in Rwanda.
Data analysis
Data were entered into Microsoft access and subsequently exported to SAS for analysis. We generated 2 × 2 contingency tables to compare sociodemographic attributes between women who accepted and those who did not accept VCT. We then constructed a logistic regression model to determine sociodemographic predictors of HIV seropositivity intrapartum using adjusted odds ratio estimates. Based on our findings that there was a significant relationship between parity and HIV seropositivity, we then generated a probability curve showing the dose-dependent relationship between parity and probability of HIV seropositive status. To generate this curve, we used the formula:
where eβx is the adjusted odds ratio for parity (considered here as a continuous variable). The generated probabilities were then used to construct the curve of parity vs. probability of testing positive for HIV intrapartum.
All tests of hypothesis were two-tailed, with a type 1 error rate fixed at 5%.
Results
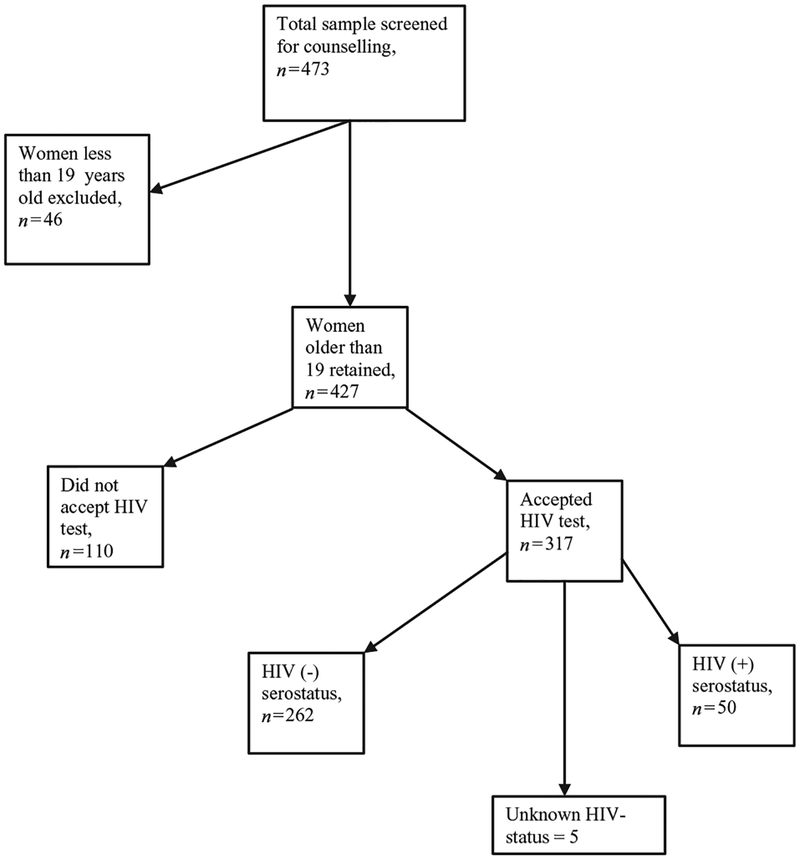
Figure 1 provides a schematic diagram of the eligibility and exclusion criteria of our study. Of the 473 women screened, 46 (9.7%) were excluded because they were teenagers, a subgroup that was a priori not qualified for enrolment according to the study protocol. Table I shows a breakdown of the sociodemographic characteristics of the 427 mothers retained in the study. Most of our study participants were below 35 years of age (92.5%), married (89.4%), had no formal education or only primary school education (70.3%) and the majority were unemployed housewives (63.7%). In contrast, only a small proportion of their partners were uneducated, although more than a third of them were unemployed.
Figure 1.
Eligibility criteria for the study.
Table I.
Socio-demographic characteristics of study population
| Variable | No. | No. (%) |
|---|---|---|
| Age (years) | 427 | |
| < 35 | 395 (92.5%) | |
| > 35 | 32 (7.5%) | |
| Children (living) | 427 | |
| 0–2 | 352 (82.4%) | |
| 3 or more | 72 (16.9%) | |
| Missing | 3 (0.7%) | |
| Parity | 427 | |
| 0–2 | 325 (76.1%) | |
| 3 or more | 102 (23.9%) | |
| Marital status | 427 | |
| Single | 37 (8.7%) | |
| Married | 382 (89.4%) | |
| Missing | 8 (1.9%) | |
| Education of mother | 427 | |
| No formal education | 28 (6.6%) | |
| Primary education | 272 (63.7%) | |
| Secondary education | 115 (26.9%) | |
| Missing | 12 (2.8%) | |
| Profession of mother | 427 | |
| Housewife | 272 (63.7%) | |
| Employed | 141 (33.0%) | |
| Missing | 14 (3.3%) | |
| Education of partner | 427 | |
| No formal education | 17 (4.0%) | |
| Primary education | 250 (58.5%) | |
| Secondary education and above | 131 (30.7%) | |
| Missing | 29 (6.8%) | |
| Profession of partner | 427 | |
| Unemployed | 167 (39.1%) | |
| Employed | 235 (55.0%) | |
| Missing | 25 (5.9%) |
When offered voluntary counseling and testing (VCT), 317 women accepted while 110 refused. Table II shows the results of a comparison of sociodemographic characteristics of those who accepted testing vs. those who refused. Both groups were similar except with respect to age and employment status of participants. Those who accepted VCT were more likely to be older (35 years and above) compared to those that did not accept testing (P = 0.05). Also women who accepted VCT were more likely to be employed compared to those who did not accept VCT (P = 0.04).
Table II.
Comparison of sociodemographic characteristics for those who accepted and those who refused to be tested for HIV (total number = 427)
| Variable | Accepted, n (%) | Did not accept, n (%) | P-value |
|---|---|---|---|
| Age (years) | |||
| < 35 | 289 (73.2%) | 106 (26.8%) | |
| > 35 | 28 (87.5%) | 4 (12.5%) | 0.05 |
| No. of living children | |||
| 0–2 | 264 (75.0%) | 88 (25.0%) | |
| 3 or more | 51 (70.8%) | 21 (29.2%) | |
| Missing | 2 (66.7%) | 1 (33.3%) | 0.72 |
| Parity | |||
| 0–2 | 244 (75.1%) | 81 (24.9%) | |
| 3 or more | 73 (71.6%) | 29 (28.4%) | 0.48 |
| Marital Status | |||
| Single | 30 (81.1%) | 7 (18.9%) | |
| Married | 280 (73.3%) | 102 (26.7%) | |
| Missing | 7 (87.5%) | 1 (12.5%) | 0.40 |
| Education of mother | |||
| No formal education | 22 (78.6%) | 6 (21.4%) | |
| Primary education | 200 (73.5%) | 72 (26.5%) | |
| Secondary education | 85 (73.9%) | 30 (26.1%) | |
| Missing | 10 (83.3%) | 2 (16.7%) | 0.70 |
| Profession of mother | |||
| Housewife | 191 (70.2%) | 81 (29.8%) | |
| Employed | 115 (81.6%) | 26 (18.4%) | |
| Missing | 11 (78.6%) | 3 (21.4%) | 0.04 |
| Education of partner | |||
| No formal education | 13 (76.5%) | 4 (23.5%) | |
| Primary education | 191 (76.4%) | 59 (23.6%) | |
| Secondary and beyond | 94 (71.8%) | 37 (28.2%) | |
| Missing | 19 (65.5%) | 10 (34.5%) | 0.52 |
| Profession of partner | |||
| Unemployed | 122 (73.1%) | 45 (26.9%) | |
| Employed | 177 (75.3%) | 58 (24.7%) | |
| Missing | 18 (72.0%) | 7 (28.0%) | 0.84 |
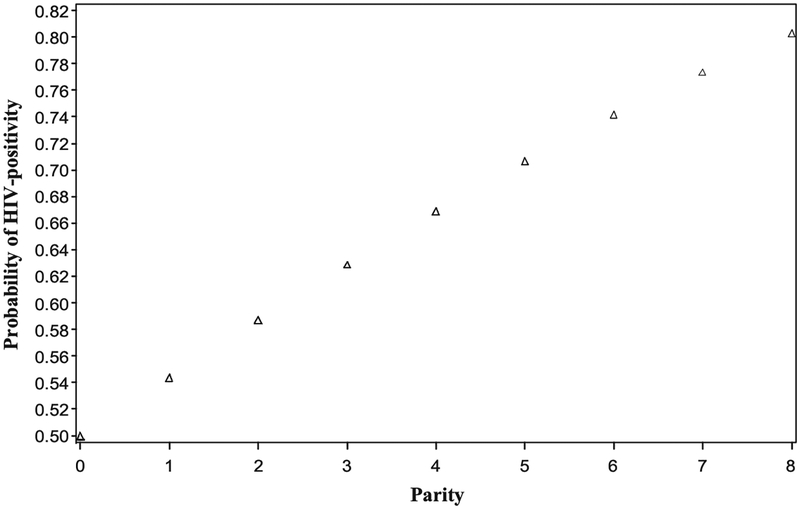
Of the 317 who accepted VCT, the results of five women remained unknown, while 50 tested positive for HIV, yielding an HIV-seroprevalence of 16% (Figure 1). Table III presents adjusted odds ratio estimates measuring the association between the various sociodemographic factors and HIV seropositivity. The only significant association was the relationship between parity and HIV seropositivity. Women who had been pregnant three or more times were three times as likely to test positive for HIV compared to those who had been pregnant two or fewer times (OR = 2.9; 95% CI = 1.1 – 8.0). Figure 2 displays a graph of parity vs. probability of testing positive for HIV. The positive slope of the line indicates that as parity increases, the probability of testing positive for HIV intrapartum also increases.
Table III.
Association of various factors with HIV seropositivity intrapartum
| Variable | Adjusted odds ratios (95% CI) |
|---|---|
| Age group | |
| < 35 | 1.0 |
| > 35 | 1.9 (0.7–5.2) |
| Parity | |
| 0–2 | 1.0 |
| 3 or more | 2.9 (1.1 −8.0) |
| Marital status | |
| Single | 1.0 |
| Married | 0.4 (0.2–1.1) |
| Number of living children | |
| 0–2 | 1.0 |
| 3 or more | 0.4 (0.1 −1.3) |
| Educational status of the mother | |
| No formal education | 1.0 |
| At least primary education | 1.3 (0.4–4.4) |
| At least secondary education | 1.9 (0.4–8.1) |
| Educational status of partner | |
| No formal education | 1.0 |
| At least primary education | 0.5 (0.1 −1.6) |
| At least secondary education | 0.4 (0.1 −1.7) |
| Profession of mother | |
| Housewife | 1.0 |
| Employed | 1.1 (0.5–2.2) |
| Profession of partner | |
| Unemployed | 1.0 |
| Employed | 1.1 (0.6–2.2) |
CI = confidence interval. Adjusted odds ratios were generated by loading all the variables in the table into the logistic regression model.
Figure 2.
Dose – response relationship between parity and HIV-positivity intrapartum.
Discussion
This study provides strong evidence to suggest that there is a significant relationship between parity and HIV serostatus intrapartum. Women who had been pregnant three or more times were three times as likely to test positive for HIV compared to those of lower parity. Our findings also provide evidence of a dose – response relationship between parity and probability of testing positive for HIV. The greater the number of pregnancies a woman has had, the higher the likelihood of testing positive to HIV intrapartum.
Previous studies performed in Rwanda on women of childbearing age (Allen et al., 1991) and pregnant women (Chao et al., 1994) reported findings that were contrary to the results in this study. Those reports showed that parity was associated inversely with probability of testing positive for HIV. There are several possible explanations for this difference in results. Our study differs remarkably from previous ones because those studies offered VCT to pregnant women antenatally while we conducted VCT during labour and delivery. It is likely, therefore, that the group of mothers detected to be HIV seropositive represented pregnant women who did not have the opportunity of coming into contact with VCT during the antenatal period.
Another possible explanation for our findings is that limited resources in Rwanda may be forcing care providers to be selective in the conduct of VCT antenatally by focusing on high-risk women, including those with low parity, as numerous studies have linked low parity to increased adverse pregnancy outcomes (Prazuck et al., 1993; Tsu et al., 1993; Ibrahim et al., 1994). Consequently, multiparous women with underlying HIV infection might be missed during the antenatal period. This might explain their preponderance among HIV seropositive cases detected in our study intrapartum. While it may be true that low parity is associated with adverse pregnancy outcome, it is important that multiparous women be given quality care as well, including an equal opportunity of receiving VCT.
A third possible reason for our findings is that the HIV epidemic in Rwanda may be beginning to change from being an infection associated more with nulliparous women to one that afflicts multiparous women to the same proportion. Those studies that investigated the epidemiological profiles of HIV seropositive women and identified low parity as a risk factor were conducted about a decade ago. There may have been a shifting of the epidemic during this time. Health promotion messages have often been targeted towards younger, nulliparous women. In our campaign to increase public awareness about HIV/AIDS we may be neglecting multiparous women. There have been studies looking at the efficacy of HIV/AIDS messages targeted toward adolescents and young adults, truck drivers as well as other high-risk groups (Wolf et al., 2000; Tambashe et al., 2003). However, because multiparous women are often considered as low risk, prevention messages are often not targeted to this group. This may be causing the pattern of the epidemic to change.
The findings of our study raise some important issues as the world continues to fight the battle against the HIV/AIDS pandemic. Multiparous women need to be considered equally as a high-risk population for HIV infection. Our results also underscore the need to conduct more studies to clearly discern the relationship between parity and HIV infection. Such studies may look at the feasibility and cost-effectiveness of intrapartum VCT, as this may be an important component in the strategy to prevent mother-to-child transmission of HIV.
Acknowledgements
This research was funded by the Minority International Research Training (MIRT) grant no. T37-TW00077 from the Fogarty International Center, National Institutes of Health [NIH], and the Ministry of Health, Rwanda and the Elizabeth Gasler Pediatric AIDS Foundation.
References
- Adamu YM and Salihu HM (2002) Barriers to the use of antenatal and obstetric care services in rural Kano, Nigeria. Journal of Obstetrics and Gynecology, 22, 600 – 603. [DOI] [PubMed] [Google Scholar]
- Allen S, Lindan C, Serufilira A, Van de Perre P, Rundle AC, Nsengumureyi F, Carael M, Schwalbe J and Hulley S (1991) Human immunodeficiency virus infection in urban Rwanda; demographic and behavioral correlates in a representative sample of childbearing women. Journal of the American Medical Association, 266, 1657 – 1663. [PubMed] [Google Scholar]
- Chao A, Bulterys M, Musanganire F, Habimana P, Nawrocki P, Taylor E, Dushimimana A and Saah A (1994) Risk factors associated with prevalent HIV-1 infection among pregnant women in Rwanda. International Journal of Epidemiology, 23, 371 – 380. [DOI] [PubMed] [Google Scholar]
- Falloon J, Eddy J, Wiener L and Pizzo PA (1989) Human immunodeficiency virus infection in children. Journal of Pediatrics, 114, 1 – 30. [DOI] [PubMed] [Google Scholar]
- Guay LA, Musoke P, Flemming T, Bagenda D, Allen M, Nakabiito C and Sherman J (1999) Intrapartum and neonatal single-dose nevirapine compared with zidovudine for prevention of mother-to-child transmission of HIV-1 in Kampala, Uganda: HIVNET 012 randomised trial. Lancet, 354, 795 – 802. [DOI] [PubMed] [Google Scholar]
- Ibrahim SA, Babiker AG, Amin IK, Omer MI and Rushwan H (1994) Factors associated with high risk of perinatal and neonatal mortality: an interim report on a prospective community-based study in rural Sudan. Paediatric Perinatal Epidemiology, 8, 193 – 204. [DOI] [PubMed] [Google Scholar]
- Leroy V, Ladner J, Nyirazirage M, De Clercq A, Bazubagira A, Van de Perre P, Karita E and Dabis F (1998) Effect of HIV-1 infection on pregnancy outcome in women in Kigali, Rwanda, 1992 – 1994. Acquired Immunodeficiency Syndrome, 12, 643 – 650. [DOI] [PubMed] [Google Scholar]
- McCaw-Binns A, Grenade J and Ashley D (1995) Under-users of antenatal care: a comparison of non-attenders and late attenders for antenatal care, with early attenders. Social Science in Medicine, 40, 1003 – 1012. [DOI] [PubMed] [Google Scholar]
- Nkowane BM (1991) Prevalence and incidence of HIV infection in Africa: a review of data published in 1990. Acquired Immunodeficiency Syndrome, 5 (Suppl.1), S7 – S15. [PubMed] [Google Scholar]
- Prazuck T, Tall F, Roisin AJ, Konfe S, Cot M and Lafaix C (1993) Risk factors for preterm delivery in Burkina Faso (West Africa). International Journal of Epidemiology, 22, 489 – 494. [DOI] [PubMed] [Google Scholar]
- Tambashe BO, Speizer IS, Amouzou A and Djangone AM (2003) Evaluation of the PSAMAO ‘Roulez Protégé’ mass media campaign in Burkina Faso. Prevention du SIDA sur les Axes Migratoires de l’Afrique de l’Ouest. AIDS Education and Prevention, 15, 33 – 48. [DOI] [PubMed] [Google Scholar]
- Tsu VD (1993) Postpartum haemorrhage in Zimbabwe: a risk factor analysis. British Journal Obstetrics and Gynaecology, 100, 327 – 333. [DOI] [PubMed] [Google Scholar]
- United Nations Department of Economic and Social Affairs— Population Division: Years of life lost to AIDS, Twenty countries with the highest adult HIV prevalence 2000 – 2005. 12 June 2001. Available at: www.un.org/esa/population/AidsWallChart/chart2.jpg. Accessed: October 8, 2001.
- Wolf RC, Tawfik LA and Bond KC (2000) Peer promotion programs and social networks in Ghana: methods for monitoring and evaluating AIDS prevention and reproductive health programs among adolescents and young adults. Journal of Health Communication, 5 (Suppl.), 61 – 80. [DOI] [PubMed] [Google Scholar]