Abstract
Food insecurity affects 1 in 8 US households and has clear implications for population health disparities. We present a person-centered, multilevel framework for understanding how individuals living in food-insecure households cope with inadequate access to food themselves and within their households, communities, and broader food system. Many of these coping strategies can have an adverse impact on health, particularly when the coping strategies are sustained over time; others may be salutary for health. There exist multiple opportunities for aligning programs and policies so that they simultaneously support food security and improved diet quality in the interest of supporting improved health outcomes. Improved access to these programs and policies may reduce the need to rely on individual- and household-level strategies that may have negative implications for health across the life course.
Keywords: ecological frameworks, food insecurity, health disparities
INTRODUCTION
Food insecurity is defined by the US Department of Agriculture as a “household-level economic and social condition of limited or uncertain access to adequate food” (121). In the way that it is tracked and measured in the United States, food insecurity refers to the inability to afford adequate food, rather than other barriers to access that frequently occur with food insecurity. These other barriers include physical inability (as from medical disability) or geographic inability (as from poor neighborhood availability) to access adequate food. In 2017, 11.8% of US households were food insecure, continuing a decline from the height of the Great Recession but not yet returning to the baseline prevalence of approximately 11% seen prior to the recession (37). Recent analyses suggest that those households that remain food insecure as the economy has recovered have greater depth and breadth of food insecurity, meaning that the severity of food insecurity is greater and the duration of food insecurity is longer (7). The sociodemographic characteristics of these food-insecure households have remained consistent as the economy has changed; data have shown food insecurity rates higher than the national average for households with children (particularly households with children under age six years), households headed by a single adult (particularly if that adult is a woman), adults living alone, non-White households, and low-income households (37). Across the United States, food insecurity rates are also particularly high in rural and urban communities (compared with suburban and exurban communities) and in the South.
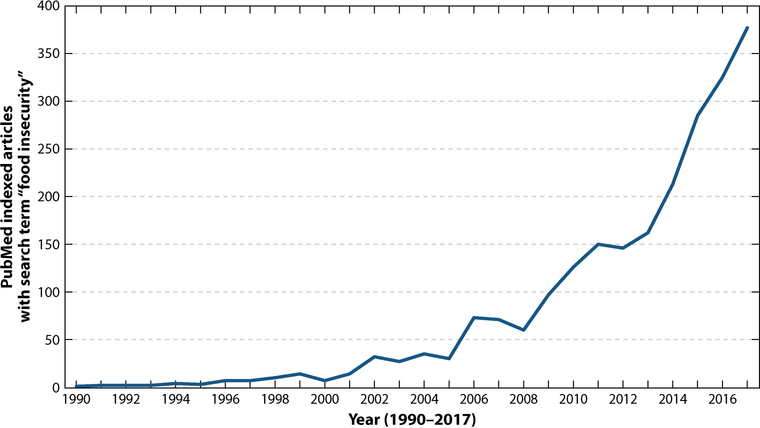
The last decade has witnessed increased attention to food insecurity from the public health and medical communities. This increased attention is demonstrated by the exponential growth in academic articles (Figure 1). Greater alignment between the antihunger and public health communities has partially fueled this growth in attention. Historically, these communities have emphasized different goals. The antihunger community sought to assure access to adequate calories, while the public health community sought to assure access to appropriate nutrition. Because interventions designed specifically to meet one of these goals often exacerbated the other, tensions between the antihunger and public health communities frequently ran high, and few opportunities for collaboration were identified or exploited.
Figure 1.
Rising medical and public health interest in food insecurity.
In recent years, these conflicts have largely resolved owing to two shifts in the way that the interplay between food insecurity and nutrition is understood. First, increasing evidence demonstrating that food insecurity is an important risk factor for poor health has made it virtually incontrovertible that dietary quality, not just calories, is an essential component of supporting food security. Second, there has been broad recognition that antihunger interventions can support healthier dietary intake and reduce food insecurity simultaneously if they are well designed and adequately resourced.
Food insecurity in low- and middle-income countries has historically been conceptualized differently than food insecurity in the United States and other high-income countries. In the latter, calories are often cheap and highly accessible, but nutrition is relatively more expensive and inaccessible, conditions that create simultaneous food insecurity and obesity (42, 99). Low- and middle-income countries have historically experienced inadequate access to both calories and nutrition (at least for certain vulnerable subpopulations), creating an imperative to focus on mal-nourishment and childhood stunting as consequences of undernutrition and lack of calories (50). Globalization of food economies, however, has created increasing similarities in the ways that food insecurity is experienced around the world (87, 94). Insights into how countries such as the United States are simultaneously addressing food insecurity and nutrition through programs and policies may therefore provide a model for addressing challenges that are increasingly being addressed globally.
This manuscript considers three topics critical to addressing food insecurity as a public health priority. The first is a review of evidence to support associations between food insecurity and poor health. The second is a person-centered framework for understanding how individuals living in food-insecure households cope with inadequate access to food themselves and within their households, communities, and broader food system. Finally, we explore opportunities for aligning programs and policies so that they simultaneously support food security and improved diet quality.
FOOD INSECURITY AND POOR HEALTH
A large and growing body of literature reveals food insecurity to be a risk factor for poor health across the life course. Earlier research focused on associations between food insecurity and specific micronutrient deficiencies, such as the well-documented association between food insecurity and iron deficiency anemia among children (47, 93, 111). However, clinically apparent micronutrient deficiencies are rare consequences of food insecurity in the United States. In the last decade, more frequent attention has focused on understanding food insecurity as a risk factor for common metabolic diseases associated with poor dietary intake. These studies have revealed associations between food insecurity and numerous chronic conditions, including diabetes mellitus type 2, hypertension, coronary heart disease and congestive heart failure, dyslipidemia, and chronic kidney disease (63).
Viewed through the lens of food insecurity as a pure manifestation of inadequate access to calories, the association between food insecurity and diabetes appears paradoxical. This paradox may be partially understood by attention to a similar relationship observed between food insecurity and obesity. Indeed, the earliest literature on food insecurity and risk for chronic disease focused on the development of obesity, the so-called “obesity-hunger paradox” (11). In general, studies conducted among adult women consistently demonstrate an association between food insecurity and higher body mass index (BMI), risk of overweight, and risk of obesity (45). Studies conducted among children and adult men show less consistent associations between food insecurity and obesity; most studies fail to show any association at all. These differences may be explained several ways, all of which have been inadequately explored in the literature. First, patterns of occupational physical activity are infrequently accounted for in studies that focus on food insecurity among men, but this physical activity may counterbalance some of the obesogenic effects of poor dietary intake associated with food insecurity. Similarly, some comorbid conditions more common in men than women (such as substance abuse) may increase their risk for weight loss in the context of food insecurity. Second, food insecurity is highly stressful. Differential ways in which women and men cope with such household stress may increase predisposition for women to become obese in the context of food insecurity (78). Third, food insecurity during pregnancy is a risk factor for infants born small-for-gestational-age (5, 28, 67). The growth trajectories of these children could lag, counterbalancing tendencies for some food-insecure children to become obese.
Finally, and perhaps most importantly, existing studies are problematic because the vast majority of those examining associations between food insecurity and obesity are cross-sectional. Individuals often cycle through periods of very low food security (the hallmark of which is decreased calorie consumption), low food security (the hallmark of which is decreased dietary quality, without changes in calorie consumption), and food security (during which time individuals with lived experience of food insecurity may overeat to compensate for past deprivation) (106). Indeed, numerous studies conducted among women have suggested that it is specifically the experience of low food security (but not very low food security) that predisposes to obesity (105).
To the extent that the association between food insecurity and obesity is driven by poor dietary quality in the context of adequate (or superadequate) calories, the association between low food security and obesity among women appears to make sense. However, this subtlety can be problematic in cross-sectional studies where a single assessment of food security status may fail to fully capture an individual’s long-term experiences. The resulting miscategorization of individuals can bias associations to the null. Nuanced, longitudinal studies that track both food security and weight over time and are designed to examine the effects that exposure to food insecurity may have, even after a return to food security, are sorely needed. However, from the perspective of public health, whether food insecurity and obesity are causally linked may be less important than the understanding that these two conditions frequently coexist.
This rich, conceptual understanding of the association between food insecurity and obesity is important for two reasons. First, it provides a preliminary understanding of how the apparently paradoxical relationship between food insecurity and diabetes (or other chronic diseases) may be understood. That is, temporal variability in adequate access to calories and healthy food alternatives may result in an individual being at increased risk for diabetes long term, even if in a particular moment in time that same individual is unable to afford adequate food to maintain caloric needs (48). Second, it calls attention to the critical need to understand food insecurity as a predisposing factor for both lack of adequate nutrition and lack of adequate calories, conditions which can exist simultaneously or consecutively. The alignment between public health and antihunger communities on the need to support food security using interventions that can increase access to both nutrition and calories makes sense in this framework.
Food insecurity is highly associated with health among children as well (62); food-insecure children generally experience 2–4 times as many health problems as do other children within the same income bracket (40). These health problems are broad and include iron deficiency anemia, frequent infections (upper respiratory infections, ear infections), nonspecific symptoms (headaches, abdominal pain), lower bone mineral density, and poorer overall health status (63). Food insecurity among children is also associated with higher utilization of health care services, including hospitalizations and mental health care (2, 41). An area of increasingly important research is understanding the extent to which food insecurity impacts educational outcomes, through impaired cognitive function, physical and mental disability, and challenging classroom behaviors (2, 72). Limited educational attainment has downstream implications for public health as well (109).
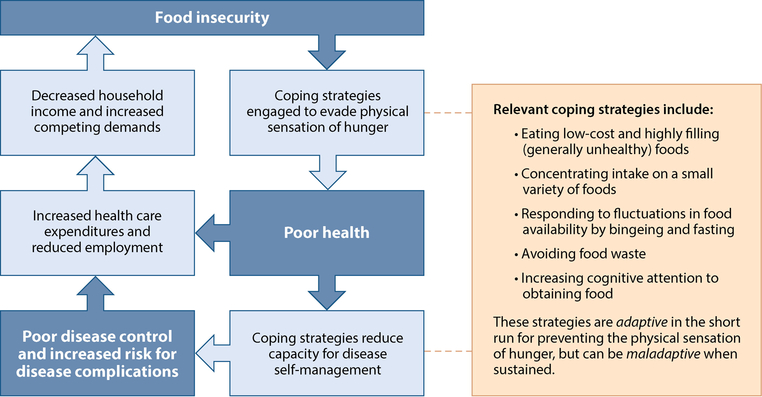
Similarly, food insecurity among adults is associated with a broad range of health conditions, some of which are associated with dietary intake and some of which are not. To understand conceptually the links between food insecurity and heterogeneous poor health outcomes, it is critical to recognize that food insecurity likely acts as a risk factor for poor health, but also that poor health—by increasing out-of-pocket health care expenditures and reducing capacity for maintaining employment—acts as a risk factor for food insecurity (Figure 2).
Figure 2.
Interwoven pathways connecting food insecurity and poor health.
Researchers have now explored each of these pathways, some superficially and others in greater depth. Chronic disease burden and food insecurity have been linked in multiple studies (63, 71, 108). In one study, as severity of food insecurity increased the prevalence of chronic disease increased from 37% to 53%, after adjusting for other demographic and socioeconomic factors (59). Each of the individual-level coping strategies for food insecurity described in the next section can divert cognitive bandwidth from other priorities and activities, including parenting children, obtaining or maintaining employment, and fulfilling basic health needs. Food insecurity also has an important psychological dimension. The insecurity aspect is highly aversive and associated with increased depressive and anxiety symptoms (31). This stress may both lead to physiologic changes (e.g., increased allostatic load) and further reduce cognitive bandwidth and motivation, in turn undermining efforts at behavior change or disease self-management (15, 69). These psychological dimensions may persist long after periods of food inadequacy resolve (112). Adults who experienced food shortages as children sometimes describe lifelong patterns of disordered eating practice, such as bingeing when food is available or food hoarding (91).
Across multiple studies in diverse clinical and nonclinical contexts and different disease states, food-insecure adults with chronic illness also demonstrate worse disease control than do food-secure adults with chronic illness, increasing their risk of disease complications. For example, food-insecure individuals with diabetes show poorer control of their blood sugar (17, 19, 20, 84, 107), and food-insecure individuals with HIV/AIDS show poorer viral suppression (1). These findings may be partially attributable to the need to delay medication refills in order to afford food [known as cost-related medication underuse (or nonadherence) (21, 66)]. Chronic disease also increases out-of-pocket medical expenditures in the United States for most households. Consider diabetes, for example. Mean individual out-of-pocket health care expenditures associated with diabetes average almost $1,400 annually in the United States (110). Diabetes is also associated with absenteeism from work (6, 120). Increased household expenditures and decreased employment have clear economic consequences for the household (32, 54), further increasing the risk of food insecurity. It is clear, therefore, that food insecurity increases one’s risk of chronic disease and that chronic disease increases one’s risk of food insecurity.
There has been recent interest in the possibility that the effect of food insecurity on poor health outcomes may manifest in a very short timeframe, a timeframe that would be relevant for health care payors in addition to public health and health care practitioners (12). For example, administrative data on hospital admissions for low blood sugar (hypoglycemia) suggest that admissions are 27% higher during the last week of the month compared with the first week of the month in low-income populations (106). This observation is attributed to the tendency of low-income households to exhaust food budgets at the end of the month, resulting in lower food intake and increased risk of hypoglycemia among individuals with diabetes. These hospital admissions are costly. According to one estimate, eliminating this end-of-month increase in hospital admissions for hypoglycemia would be expected to avert approximately $54.1 million per year in emergency department and inpatient hospitalization costs for nonelderly, commercially insured adults alone (12).
Other studies in the United States and Canada have shown that adults in food-insecure households have higher health care utilization and costs compared with food-secure households (16, 24, 81, 117). These studies have prompted interest in understanding the accumulation of health care costs associated with food insecurity. A recent study used nationally representative sampling to determine annual health care expenditures in the 24 months after assessing the food security status of an individual’s household. The study found that mean health care expenditures were $1,863 higher annually for food-insecure adults compared with food-secure adults, resulting in an estimated cost of $77.5 billion to the health care sector associated with adult food insecurity (16).
MULTILEVEL STRATEGIES THAT INDIVIDUALS USE TO COPE WITH FOOD INSECURITY
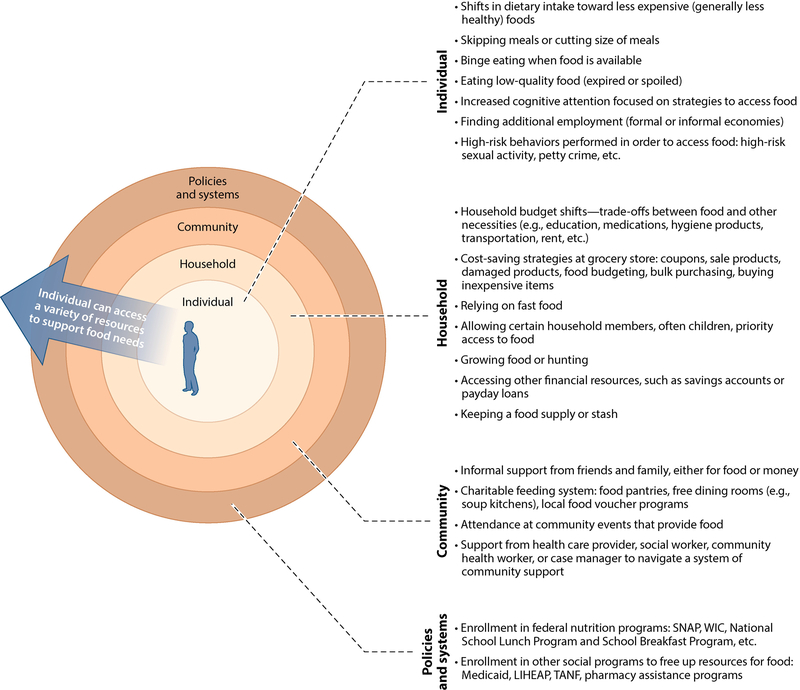
The experience of food insecurity is an individual one shared with members of the household. Understanding the range of coping strategies that may be salient to an individual’s health requires understanding the landscape of support for food security from the perspective of one with lived experience of food insecurity. While many food security frameworks illustrate the primary importance of external resources, such as the Supplemental Nutrition Assistance Program (SNAP) and the charitable feeding system, as primary coping strategies for food insecurity, many individuals access these external resources only after calling upon multiple coping strategies. For organizational purposes, we present a framework for how individuals cope with food insecurity by calling upon resources at the individual, household, community, and systems levels (Figure 3). Some of these coping strategies are likely to worsen health, whereas others may prove salutary. The strategies described in this framework are often complex and, in many cases, may overlap or cross levels. Nonetheless, this simplified framework can help identify opportunities for public health interventions that seek to support individuals in coping with food insecurity in ways that promote health rather than worsen it.
Figure 3.
Food-insecure individuals draw on resources at the individual, household, community, and systems levels. Abbreviations: LIHEAP, Low Income Home Energy Assistance Program; SNAP, Supplemental Nutrition Assistance Program; TANF, Temporary Assistance for Needy Families; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Individual Strategies
Food-insecure adults often rely on their own resources or the resources of their household as an initial strategy for addressing an acute shortage of money for food. Most individual-level strategies involve alterations of behavior. These alterations can include restricting the range of foods consumed, preferentially choosing cheaper foods, and reducing overall food consumption. Although measurement of dietary intake is notoriously challenging, systematic reviews suggest that food insecurity is associated with poorer dietary quality among both adults and children (65), likely because energy-dense, nutritionally poor foods (such as refined grains, saturated fats, and highly processed foods with high sodium content) are cheaper on a per-calorie basis than are whole grains, fresh fruits and vegetables, and lean proteins (42). Reduced overall consumption is observed, particularly among mothers, at the end of the month when food budgets are most likely to be exhausted or during other income shocks (25). In addition to decreased calorie intake, carbohydrate, micronutrient, and fruit and vegetable intake may also decrease over the course of the month (118). Because of its acute attendant health risks, a particularly concerning coping strategy for lack of food is consuming items that would not otherwise be eaten, such as spoiled food.
Individual-level strategies often include focusing additional time and mental effort on the logistics of obtaining food and strategies for accessing other resources available at the level of the household, community, and food system. Individuals seek to find additional food or financial resources for food through secondary employment, gray-market income opportunities, or even risky behaviors (46). Examples of such risky behaviors with particular public health implications include engaging in sexual activity (particularly among adolescent girls) or petty crime in anticipation of being offered food by sexual partners or the justice system (95, 122).
Each of these individual-level strategies serves an important purpose in the immediate term: to maintain caloric needs and escape the physical sensation of hunger. However, particularly when sustained over years or decades, these strategies may also be maladaptive and increase risk for poor health. Leveraging resources available at the household, community, and food system levels may diminish the need to rely on these individual-level strategies.
Household Strategies
In contrast to individual strategies, household strategies for addressing food insecurity can compromise or promote health. Health-compromising strategies include relying on convenience options such as fast food, which can offer extremely high-calorie content for very little money, or delaying purchases of other necessities, such as medications and hygiene products, in order to afford food (102). “Making ends meet” by accessing other financial resources, such as tapping into savings accounts, selling or pawning items, or obtaining short-term loans, may not be immediately detrimental but can have downstream implications for household debt and health (85, 115). Other household-level strategies are implemented when purchasing groceries: using coupons, shopping at multiple stores to take advantage of the best prices, or buying product in bulk. These strategies can be either health promoting or health compromising, depending on how they are operationalized and the environments in which they are implemented. In some cases, outside influences on household spending contribute to making these strategies less health promoting. For example, grocery store coupons may be less frequently available for healthy food options (70, 79, 83), making these foods seem even further out of reach for food-insecure households.
Parents generally attempt to shield their children from acute fluctuations in dietary intake related to the inability to afford food. A strategy of prioritizing young household members for food can only partially protect children. It is instructive that even children in households with marginal food security, for whom neither the quality nor quantity of food is thought to be impacted, suffer worse health outcomes than do children in food-secure households (39). These poorer outcomes may be related to reverse causation (that is, the poor health of the children is the cause of the food insecurity, rather than the food insecurity being the cause of the children’s poor health), the socioeconomic circumstances that led to marginal food security, the toxic nature of household stress associated with food insecurity, or the psychological impact of food insecurity on children (75). Although parents often report that their children are fully shielded from food insecurity, children in these same households report an acute awareness of household need and their own strategies (often hidden from their parents) to alleviate that need (53). Strategies described by children and adolescents include eating less than desired in order to save food for household adults or siblings, strategizing opportunities to eat with family or friends in order to alleviate the pressure for food at home, finding a job, or risky behaviors (such as shoplifting) (53, 95).
Because household-level interventions naturally consider the way food is shared within a household and because they offer the potential for multigenerational benefits, household-level interventions are likely to be useful tools for improving public health related to food security. Strategies that generate greater financial resources for food within the household may reduce the pressure to buy the cheapest foods (often fast food or calorically dense but nutritionally poor food) and reduce the need for household children and adolescents to contribute to the need to meet household food requirements.
Community Strategies
Individuals in food-insecure households often must seek resources from outside the household, particularly after individual- and household-level coping strategies have been strained or exhausted. Local communities offer both informal and formal strategies. Informal strategies include seeking support from friends and family, in the form of either money or food. Parents may send children to a friend’s or relative’s home for dinner, churches or other places of congregation may offer free spaghetti dinners, or individuals may ask for help from other community members (38). Thus, social cohesion and the availability of resources at the community level may be important elements of the capacity of the community to informally support its food-insecure members (82).
The charitable feeding system provides a more formal system for providing free food across the United States, creating a secondary food market that exists in parallel to the retail grocery system. Food banks across the United States source free and low-cost foods in enormous quantities from food growers, manufacturers, wholesalers, and retailers; warehouse that food; and distribute it to food pantries and other meal programs. Food pantries are generally community agencies that partner with the food bank to provide food directly to food-insecure households. These pantries and meal programs may be located in churches and other places of worship, community centers, schools, shelters, and other community locations that reach vulnerable households.
Recently, local communities—sometimes with the support of federal funding—have developed their own formal programs to support food-insecure households in augmenting their food budgets. These community programs have generally taken the form of vouchers redeemable for food. Most frequently, these vouchers are provided for a short period of time to incentivize (not fully subsidize) purchases of fruits and vegetables at local farmer’s markets, although—as with all local programming—much heterogeneity exists (26).
Other community programs exist to fill additional nutritional needs, such as providing food for frail and homebound adults who need cooking support, but may simultaneously address food insecurity. This programming is sometimes divided into home-delivered meal programs, which generally offer precooked meals with limited customization options, and medically tailored meal programs, which generally offer precooked meals customized for specific dietary needs associated with chronic illness (such as HIV, diabetes, or cancer). The overlap between these two kinds of programming is substantial, and their continued separation into different organizations is largely an artifact of how community agencies designed to fill specific community needs were founded and have evolved.
Accessing formal resources for food at the levels of both the community and the broader food system can be complex for an individual. For example, even with dozens of food pantries available in a community, an individual may need to navigate the eligibility criteria for each one, the ability to find transportation to and from each location, limited hours of operation, and how those hours may conflict with other commitments such as child care and employment. Individuals may not be aware that they qualify for home-delivered meals; if they do qualify, whether they should be accessing home-delivered meal programs or medically tailored meal programs; and how to obtain a referral for such programs. To take advantage of this complex web of community resources, community-level support from a social worker, community health worker, health care provider, or case manager is often necessary (8, 113). To the extent that these navigators are knowledgeable about local community resources, they may be well positioned to support households in accessing services that provide the greatest support for both food security and nutrition (58).
Policies and Systems Strategies
Thirteen federal nutrition programs represent the largest effort to improve food security in the United States (96). SNAP is by far the largest of the federal nutrition programs; the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) and the National School Lunch Program represent the next two largest. Together, the 13 programs represent ~$100 billion in annual nutrition assistance. Strong evidence indicates that SNAP substantially reduces the rate of food insecurity (80, 89, 97). However, more than half of households receiving SNAP benefits still report being food insecure. Two phenomena contribute to this startlingly high rate of food insecurity among households receiving SNAP benefits. The first is that households self-select into the SNAP program. As already noted, households often do not access SNAP benefits until they have exhausted other coping strategies. Therefore, the most food-insecure households are the most likely to enroll in SNAP. Second, SNAP benefit levels are often not adequate to lift a household over the threshold from food insecurity to food security, even though they may be adequate to reduce the depth and breadth of food insecurity. In a typical household receiving SNAP benefits, for example, 80% of benefits are exhausted by the second week of the month (51).
Because household resources are fungible (i.e., money can easily be moved from one bucket of the household budget to another), participation in other social safety-net programs may also support food security. Households derive financial protection from health insurance, support with utility expenses as provided by LIHEAP (the Low Income Home Energy Assistance Program), and Temporary Assistance for Needy Families. Households that can take advantage of tax policies such as the Earned Income Tax Credit can support their food security by offsetting the relatively larger share of household income spent on food by those with lower incomes (98). Finally, labor policy such as minimum wage laws and overtime regulations may help support food security, although these areas are controversial and inadequately studied. State-level policies that impact implementation of federal nutrition programs, the tax burden on the lowest-income households, housing costs, and labor markets are also clearly associated with food security rates (9).
The degree to which individuals rely on each of these individual, household, community, and systems supports for food security depends on their local availability or accessibility and cultural acceptance. For example, policies that make enrollment in federal nutrition programs easier are associated with increased enrollment rates, communities without access to food pantries (such as many rural communities) cannot rely on the charitable food system as a coping strategy, and generational and cultural differences in preferred strategies can affect how families address food insecurity (10, 29).
INTERVENTION OPPORTUNITIES THAT ALIGN ANTIHUNGER AND NUTRITION GOALS
The clarity of association between food insecurity and poor health has prompted increased interest in understanding the extent to which interventions can simultaneously support an individual’s food security and health. Over the last decade, it has become clear that multiple interventions may be able to do both and that these interventions are clustered primarily at the level of community resources and nutrition policy (4).
Numerous interventions in the community setting are gathering momentum, with varied levels of evidence to support their impact on improved dietary intake or food security. For example, early studies of medically tailored meals for frail, homebound, and/or chronically ill adults suggest that these programs may simultaneously improve food security, disease self-management, intermediate health outcomes, and utilization of health care services (23, 92). These programs may be able to achieve these diverse goals by providing a relatively large dose of food addressing multiple barriers to healthy dietary intake: challenges with food preparation and food access, inconvenience, taste preferences for less healthy food, and affordability of healthy food. Community efforts are currently under way to classify such programs, under specific circumstances, as billable services so that they may be supported by the health care sector (124).
Other examples of emerging community programs that simultaneously support healthier dietary intake and food security occur in food bank settings. Food banks increasingly see their role as not only ending hunger in their communities but also supporting healthier dietary intake to reduce health disparities that disproportionately impact their clients (123). Strategies in place at food bank settings exist along a continuum and include setting operating goals for healthy food sourcing; formal or informal policies to accept any food donations but restrict food bank purchases to healthy foods; and policies to restrict or eliminate the distribution of specific foods, such as sugar-sweetened beverages or junk foods.
Multiple studies show that food pantry clients are interested in receiving healthier foods at the pantry (27, 30). Historically, food pantries offered a box of nonperishable staple food items. Contemporary food pantries often look very different. Perishable food items are often available, including fresh fruits and vegetables, dairy items, and protein. Rather than picking up a preselected box of items, clients can often “shop” at the pantry to choose desired food items. This shift in the way food pantries provide food has created opportunities to use behavioral economics principles to encourage the selection of healthier baskets of goods from choice pantries (125). The reorganization of these food pantries may include fruits and vegetables attractively displayed in full baskets, healthy food options displayed in large quantities at eye level and in multiple places, and unhealthy food options displayed in lower quantities. Preliminary data suggest that these interventions can have a positive impact on client choices in the food pantry setting, just as they can in settings such as school cafeterias and grocery stores, although further studies must be done to confirm these results (126).
Broadscale implementation of voucher and incentive programs for subsidizing the costs of healthier foods, such as fruits and vegetables, is relatively new. However, evidence is beginning to emerge that these programs can support food security and healthier dietary intake. The randomized Healthy Incentives Program offered a 30% incentive for fruit and vegetable purchases made with SNAP benefits. Although the individual-level impact on dietary intake was modest, the benefits observed could have a large population health impact if the intervention impact can be sustained (14, 33). Voucher programs since that trial have been designed to optimize their impact on dietary health. Other randomized and observational studies support the potential of such programs to improve food security and health outcomes.
An additional line of research has focused on increasing the healthfulness of options available for purchase at the grocery store, in addition to nudging individual behavior toward the purchase of these options. These studies provide frameworks for approaches that can make healthful food more accessible (44, 73).
Another growing area of intervention has been linkage programs based in health care settings, which have grown out of the hypothesis that supporting food security, and helping individuals meet other basic needs, can provide health systems with a mechanism to improve population health (3, 55, 56, 58). These programs generally include screening patients for food insecurity at the clinic or hospital using a brief clinical screening tool such as the Hunger Vital Sign© (61, 64). Efforts are then made to link food-insecure patients with community resources or federal nutrition programs. Linking methods can include light touch interventions (such as providing information on operating hours and phone numbers of community food pantries) to more intensive navigation by volunteers, community health workers, social workers, or case managers (8). In some regions, the complexity of these referrals has prompted the creation of formal programs to support health care systems in these referral processes (119). Hunger Free Colorado is an example of such a program (113, 119).
Early results show these linkage programs may hold promise for improving health outcomes, with one study finding clinically important reductions in blood pressure and cholesterol in adult primary care patients (18). Other work in prenatal and pediatric settings has also shown benefit (57, 88). The Accountable Health Communities Model from the Centers for Medicare and Medicaid Services is an ongoing large-scale test of this approach (4). Notably, many linkage programs attempt to address not only food insecurity, but other commonly co-occurring needs such as housing or transportation issues as well.
The recent passage of sugar-sweetened beverage taxes in multiple municipalities in the United States suggests another potential strategy for simultaneously supporting food security and dietary quality. The greatest reductions in sugar-sweetened beverage intake observed as a result of taxation occur in lower-income households (35, 49). To the extent that these sugar-sweetened beverages are not substituted with other unhealthy beverages, they can simultaneously support both lower food costs and better dietary intake. In addition, revenue generated from such taxes is frequently targeted toward supporting the needs of low-income communities in nutrition and physical activity behaviors and food security (114).
Finally, substantial evidence has shown that federal nutrition programs have an important role to play in supporting both food security and dietary intake. For example, WIC supports children’s health in multiple dimensions, including lower infant mortality rates, healthier infant feeding practices (36, 52), increased micronutrients (especially iron, leading to a decreased risk of iron deficiency anemia) (36), and improved school performance. At the same time, WIC likely reduces food insecurity among households with children (77).
As described earlier, SNAP is highly effective at reducing food insecurity. Recent evidence also suggests that SNAP, though not designed as a health-promotion program, may also improve health (86). Individuals of all ages receiving SNAP benefits are more likely to report excellent or very good health (after adjusting for other characteristics), compared with low-income nonparticipants in SNAP, and decreased psychological distress (90); pregnant women receiving SNAP benefits have improved birth outcomes and their babies have better health outcomes as they grow (5, 68); and older adults receiving SNAP benefits are less likely to put off paying for medications because of cost and more likely to avoid hospitalizations and maintain independence in the community (60, 68, 74, 76, 86, 101, 116). Although numerous studies have shown associations between SNAP and obesity, well-conducted studies consistently demonstrate that SNAP does not cause obesity; rather, it is likely that more obese populations are more likely to enroll in SNAP (100). SNAP is also associated with a reduction in health care costs; low-income adults who participate in SNAP incur an average of $1,400 per year less in health care expenditures compared with matched nonparticipants (22). For adults with chronic disease, the cost savings associated with SNAP benefits may be even higher. Thus, a program that is proven to reduce food insecurity is also likely to support improved health.
Although policy changes could increase the extent to which SNAP benefits can support healthy dietary behaviors (13), strong concerns persist on the part of the antihunger community that such changes—such as restricting purchases of sugar-sweetened beverages—could increase program stigma, decrease ease of operations, reduce public support for the program, and thus weaken SNAP (34, 43), which would ultimately increase food insecurity rates. Thus, opportunities to leverage SNAP for health promotion may be tempered by long-held tensions between improving food access and improving food quality (103, 104).
CONCLUSIONS
Individuals living in food-insecure households engage many coping strategies to meet their food needs. Maintenance of some of these coping strategies over long durations decreases health and increases health care expenditures. Close attention to these coping strategies and their potential to support or undermine healthy behaviors suggests areas of intervention (often policy-oriented) that may be particularly impactful by supporting food security and better health outcomes simultaneously. Evidence already suggests that some of these interventions, such as medically tailored meals, healthier food pantries, SNAP, and WIC, can do just that.
SUMMARY POINTS.
Food insecurity is common and associated with a wide range of poor health outcomes across the life course.
Studies with longitudinal designs and a specific focus on understanding how food insecurity leads to poor health are needed.
Coping strategies used to address food insecurity at the level of the individual, household, community, and broader food system may have positive or negative implications for health outcomes.
There exist household-, community-, and policy-level opportunities to align antihunger and public health goals.
ACKNOWLEDGMENTS
The authors’ role in the research reported in this publication was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under award K23DK109200 (S.A.B.) and P30DK092924 (H.K.S.) and by the Centers for Disease Control and Prevention under award 3U48DP004998 (H.K.S.).
Footnotes
DISCLOSURE STATEMENT
H.K.S. serves as Senior Medical Advisor for Feeding America, a nonprofit organization. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the Centers for Disease Control and Prevention, or Feeding America.
LITERATURE CITED
- 1.Aibibula W, Cox J, Hamelin AM, McLinden T, Klein MB, Brassard P. 2017. Association between food insecurity and HIV viral suppression: a systematic review and meta-analysis. AIDS Behav. 21:754–65 [DOI] [PubMed] [Google Scholar]
- 2.Alaimo K, Olson CM, Frongillo EA Jr. 2001. Food insufficiency and American school-aged children’s cognitive, academic, and psychosocial development. Pediatrics 108:44–53 [PubMed] [Google Scholar]
- 3.Alderwick HAJ, Gottlieb LM, Fichtenberg CM, Adler NE. 2018. Social prescribing in the U.S. and England: emerging interventions to address patients’ social needs. Am. J. Prev. Med 54:715–18 [DOI] [PubMed] [Google Scholar]
- 4.Alley DE, Asomugha CN, Conway PH, Sanghavi DM. 2016. Accountable health communities—addressing social needs through Medicare and Medicaid. N. Engl. J. Med 374:8–11 [DOI] [PubMed] [Google Scholar]
- 5.Almond D, Hoynes HW, Schanzenbach DW. 2011. Inside the War on Poverty: the impact of food stamps on birth outcomes. Rev. Econ. Stat 93:387–403 [Google Scholar]
- 6.Asay GRB, Roy K, Lang JE, Payne RL, Howard DH. 2016. Absenteeism and employer costs associated with chronic diseases and health risk factors in the US workforce. Prev. Chronic Dis 13:150503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Balistreri KS. 2016. A decade of change: measuring the extent, depth and severity of food insecurity. J. Fam. Econ. Issues 37:373–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barnidge E, Stenmark S, Seligman HS. 2017. Clinic-to-community models to address food insecurity. JAMA Pediatr. 171:507–8 [DOI] [PubMed] [Google Scholar]
- 9.Bartfeld J, Dunifon R. 2006. State-level predictors of food insecurity among households with children. J. Policy Anal. Manag 25:921–42 [Google Scholar]
- 10.Bartfeld J, Dunifon R, Nord M, Carlson S. 2006. What factors account for state-to-state differences in food security? Econ. Inf. Bull 20, US Dep. Agric., Washington, DC: https://idph.iowa.gov/Portals/1/Files/WIC/state_to_state_fs.pdf [Google Scholar]
- 11.Basiotis PP, Lino M. 2002. Food insufficiency and prevalence of overweight among adult women. Nutr. Insights 26:1–2 [Google Scholar]
- 12.Basu S, Berkowitz SA, Seligman H. 2017. The monthly cycle of hypoglycemia: an observational claims-based study of emergency room visits, hospital admissions, and costs in a commercially insured population. Med. Care 55:639–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Basu S, Seligman H, Bhattacharya J. 2013. Nutritional policy changes in the supplemental nutrition assistance program: a microsimulation and cost-effectiveness analysis. Med. Decis. Making 33:937–48 [DOI] [PubMed] [Google Scholar]
- 14.Basu S, Seligman HK, Gardner C, Bhattacharya J. 2014. Ending SNAP subsidies for sugar-sweetened beverages could reduce obesity and type 2 diabetes. Health Aff. 33:1032–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berkowitz SA, Baggett TP, Wexler DJ, Huskey KW, Wee CC. 2013. Food insecurity and metabolic control among U.S. adults with diabetes. Diabetes Care 36:3093–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berkowitz SA, Basu S, Meigs JB, Seligman HK. 2018. Food insecurity and health care expenditures in the United States, 2011–2013. Health Serv. Res 53:1600–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berkowitz SA, Gao X, Tucker KL. 2014. Food-insecure dietary patterns are associated with poor longitudinal glycemic control in diabetes: results from the Boston Puerto Rican Health study. Diabetes Care 37:2587–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berkowitz SA, Hulberg AC, Standish S, Reznor G, Atlas SJ. 2017. Addressing unmet basic resource needs as part of chronic cardiometabolic disease management. JAMA Intern. Med 177:244–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berkowitz SA, Karter AJ, Corbie-Smith G, Seligman HK, Ackroyd SA, et al. 2018. Food insecurity, food “deserts,” and glycemic control in patients with diabetes: a longitudinal analysis. Diabetes Care 41:1188–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berkowitz SA, Meigs JB, DeWalt D, Seligman HK, Barnard LS, et al. 2015. Material need insecurities, control of diabetes mellitus, and use of health care resources: results of the Measuring Economic Insecurity in Diabetes study. JAMA Intern. Med 175:257–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berkowitz SA, Seligman HK, Choudhry NK. 2014. Treat or eat: food insecurity, cost-related medication underuse, and unmet needs. Am. J. Med 127:303–10.e3 [DOI] [PubMed] [Google Scholar]
- 22.Berkowitz SA, Seligman HK, Rigdon J, Meigs JB, Basu S. 2017. Supplemental Nutrition Assistance Program (SNAP) participation and health care expenditures among low-income adults. JAMA Intern. Med 177:1642–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berkowitz SA, Terranova J, Hill C, Ajayi T, Linsky T, et al. 2018. Meal delivery programs reduce the use of costly health care in dually eligible Medicare and Medicaid beneficiaries. Health Aff. 37:535–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bhargava V, Lee JS. 2016. Food insecurity and health care utilization among older adults in the United States. J. Nutr. Gerontol. Geriatr 35:177–92 [DOI] [PubMed] [Google Scholar]
- 25.Bhattacharya J, DeLeire T, Haider S, Currie J. 2003. Heat or eat? Cold-weather shocks and nutrition in poor American families. Am. J. Public Health 93:1149–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blondin K, Orta-Aleman D, Woodward-Lopez G. 2016. Review of the evidence: health promotion strategies for retail food shopping venues. Rep., Nutr. Educ. Obesity Prev. Res. Eval. Unit, Nutr. Policy Inst., Berkeley, CA: http://npi.ucanr.edu/files/263765.pdf [Google Scholar]
- 27.Bomberg EM, Neuhaus J, Hake MM, Engelhard EM, Seligman HK. 2018. Food preferences and coping strategies among diabetic and nondiabetic households served by US food pantries. J. Hunger Environ. Nutr 10.1080/19320248.2018.1512926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Borders AE, Grobman WA, Amsden LB, Holl JL. 2007. Chronic stress and low birth weight neonates in a low-income population of women. Obstet. Gynecol 109:331–38 [DOI] [PubMed] [Google Scholar]
- 29.Borjas GJ. 2004. Food insecurity and public assistance. J. Public Econ. 88:1421–43 [Google Scholar]
- 30.Campbell E, Hudson H, Webb K, Crawford PB. 2011. Food preferences of users of the emergency food system. J. Hunger Environ. Nutr 6:179–87 [Google Scholar]
- 31.Canales MK, Coffey N, Moore E. 2015. Exploring health implications of disparities associated with food insecurity among low-income populations. Nurs. Clin. North Am 50:465–81 [DOI] [PubMed] [Google Scholar]
- 32.Cawley J, Rizzo JA, Haas K. 2008. The association of diabetes with job absenteeism costs among obese and morbidly obese workers. J. Occupat. Environ. Med 50:527–34 [DOI] [PubMed] [Google Scholar]
- 33.Choi SE, Seligman H, Basu S. 2017. Cost effectiveness of subsidizing fruit and vegetable purchases through the Supplemental Nutrition Assistance Program. Am. J. Prev. Med 52:e147–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.CHW (Children’s HealthWatch). 2018. Children’s HealthWatch statement on the 2018 House Farm Bill. Statement, April 13, CHW, Boston: http://childrenshealthwatch.org/childrens-healthwatch-statement-on-the-2018-farm-bill/ [Google Scholar]
- 35.Colchero MA, Rivera-Dommarco J, Popkin BM, Ng SW. 2017. In Mexico, evidence of sustained consumer response two years after implementing a sugar-sweetened beverage tax. Health Aff. 36:564–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Colman S, Nichols-Barrer IP, Redline JE, Devaney BL, Ansell SV, Joyce T. 2012. Effects of the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC): a review of recent research. Rep. WIC-12-WM, Food Nutr. Serv., US Dep. Agric., Alexandria, VA: https://fns-prod.azureedge.net/sites/default/files/WICMedicaidLitRev.pdf [Google Scholar]
- 37.Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. 2018. Household food security in the United States in 2017. Rep. ERR-256, US Dep. Agric., Econ. Res. Serv., Washington, DC: https://www.ers.usda.gov/webdocs/publications/90023/err-256.pdf [Google Scholar]
- 38.Connell CL, Lofton KL, Yadrick K, Rehner TA. 2005. Children’s experiences of food insecurity can assist in understanding its effect on their well-being. J. Nutr 135:1683–90 [DOI] [PubMed] [Google Scholar]
- 39.Cook JT, Black M, Chilton M, Cutts D, Ettinger de Cuba S, et al. 2013. Are food insecurity’s health impacts underestimated in the U.S. population? Marginal food security also predicts adverse health outcomes in young U.S. children and mothers. Adv. Nutr 4:51–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cook JT, Frank DA, Berkowitz C, Black MM, Casey PH, et al. 2004. Food insecurity is associated with adverse health outcomes among human infants and toddlers. J. Nutr 134:1432–38 [DOI] [PubMed] [Google Scholar]
- 41.Cook JT, Frank DA, Levenson SM, Neault NB, Heeren TC, et al. 2006. Child food insecurity increases risks posed by household food insecurity to young children’s health. J. Nutr 136:1073–76 [DOI] [PubMed] [Google Scholar]
- 42.Darmon N, Drewnowski A. 2015. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr. Rev 73:643–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dean S 2018. President’s budget would cut and radically restructure SNAP food benefits. Cent. Budg. Policy Prior. Blog, Feb. 12. https://www.cbpp.org/blog/presidents-budget-would-cut-and-radically-restructure-snap-food-benefits [Google Scholar]
- 44.DeWeese RS, Todd M, Karpyn A, Yedidia MJ, Kennedy M, et al. 2016. Healthy store programs and the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), but not the Supplemental Nutrition Assistance Program (SNAP), are associated with corner store healthfulness. Prev. Med. Rep 4:256–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dinour LM, Bergen D, Yeh MC. 2007. The food insecurity-obesity paradox: a review of the literature and the role food stamps may play. J. Am. Diet. Assoc 107:1952–61 [DOI] [PubMed] [Google Scholar]
- 46.Edin KJ, Shaefer HL. 2016. $2.00 a Day: Living on Almost Nothing in America. New York: N.Y. First Mariner [Google Scholar]
- 47.Eicher-Miller HA, Mason AC, Weaver CM, McCabe GP, Boushey CJ. 2009. Food insecurity is associated with iron deficiency anemia in US adolescents. Am. J. Clin. Nutr 90:1358–71 [DOI] [PubMed] [Google Scholar]
- 48.Essien UR, Shahid NN, Berkowitz SA. 2016. Food insecurity and diabetes in developed societies. Curr. Diabetes Rep 16:79. [DOI] [PubMed] [Google Scholar]
- 49.Falbe J, Thompson HR, Becker CM, Rojas N, McCulloch CE, Madsen KA. 2016. Impact of the Berkeley excise tax on sugar-sweetened beverage consumption. Am. J. Public Health 106:1865–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.FAO (Food Agric. Organ.), IFAD (Int. Fund Agric. Dev.), UNICEF (UN Child. Fund), WFP (World Food Progr.), WHO (World Health Organ.). 2017. The state of food security and nutrition in the world 2017: building resilience for peace and food security. Rep., FAO, Rome: http://www.fao.org/3/a-I7695e.pdf [Google Scholar]
- 51.FNS (Food Nutr. Serv.). 2006. An analysis of Food Stamp benefit redemption patterns. Rep., US Dep. Agric., Washington, DC: https://fns-prod.azureedge.net/sites/default/files/EBTRedemption.pdf [Google Scholar]
- 52.Fox MK, Hamilton W, Lin B, eds. 2004. Effects of food assistance and nutrition programs on nutrition and health. Food Assist. Nutr. Res. Rep. 19–3, US Dep. Agric., Washington, DC: https://www.ers.usda.gov/webdocs/publications/46556/30240_fanrr19-3_002.pdf?v=0 [Google Scholar]
- 53.Fram MS, Frongillo EA, Jones SJ, Williams RC, Burke MP, et al. 2011. Children are aware of food insecurity and take responsibility for managing food resources. J. Nutr 141:1114–19 [DOI] [PubMed] [Google Scholar]
- 54.Fu AZ, Qiu Y, Radican L, Wells BJ. 2009. Health care and productivity costs associated with diabetic patients with macrovascular comorbid conditions. Diabetes Care 32:2187–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gold R, Cottrell E, Bunce A, Middendorf M, Hollombe C, et al. 2017. Developing electronic health record (EHR) strategies related to health center patients’ social determinants of health. J. Am. Board Fam. Med 30:428–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gottlieb L, Tobey R, Cantor J, Hessler D, Adler NE. 2016. Integrating social and medical data to improve population health: opportunities and barriers. Health Aff. 35:2116–23 [DOI] [PubMed] [Google Scholar]
- 57.Gottlieb LM, Hessler D, Long D, Laves E, Burns AR, et al. 2016. Effects of social needs screening and in-person service navigation on child health: a randomized clinical trial. JAMA Pediatr. 170:e162521. [DOI] [PubMed] [Google Scholar]
- 58.Gottlieb LM, Wing H, Adler NE. 2017. A systematic review of interventions on patients’ social and economic needs. Am. J. Prev. Med 53:719–29 [DOI] [PubMed] [Google Scholar]
- 59.Gregory CA, Coleman-Jensen A. 2017. Food insecurity, chronic disease, and health among working-age adults. Econ. Res. Rep. 235, Econ. Res. Serv., US Dep. Agric., Washington, DC: https://www.ers.usda.gov/webdocs/publications/84467/err-235.pdf?v=0 [Google Scholar]
- 60.Gregory CA, Deb P. 2015. Does SNAP improve your health? Food Policy 50:11–19 [Google Scholar]
- 61.Gundersen C, Engelhard EE, Crumbaugh AS, Seligman HK. 2017. Brief assessment of food insecurity accurately identifies high-risk US adults. Public Health Nutr. 20:1367–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gundersen C, Kreider B. 2009. Bounding the effects of food insecurity on children’s health outcomes. J. Health Econ 28:971–83 [DOI] [PubMed] [Google Scholar]
- 63.Gundersen C, Ziliak JP. 2015. Food insecurity and health outcomes. Health Aff. 34:1830–39 [DOI] [PubMed] [Google Scholar]
- 64.Hager ER, Quigg AM, Black MM, Coleman SM, Heeren T, et al. 2010. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics 126:e26–32 [DOI] [PubMed] [Google Scholar]
- 65.Hanson KL, Connor LM. 2014. Food insecurity and dietary quality in US adults and children: a systematic review. Am. J. Clin. Nutr 100:684–92 [DOI] [PubMed] [Google Scholar]
- 66.Herman D, Afulani P, Coleman-Jensen A, Harrison GG. 2015. Food insecurity and cost-related medication underuse among nonelderly adults in a nationally representative sample. Am. J. Public Health 105:e48–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hobel CJ. 2004. Stress and preterm birth. Clin. Obstet Gynecol 47:856–80 [DOI] [PubMed] [Google Scholar]
- 68.Hoynes H, Schanzenbach DW, Almond D. 2016. Long-run impacts of childhood access to the safety net. Am. Econ. Rev 106:903–34 [Google Scholar]
- 69.Ippolito MM, Lyles CR, Prendergast K, Marshall MB, Waxman E, Seligman HK. 2017. Food insecurity and diabetes self-management among food pantry clients. Public Health Nutr. 20:183–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jahns L, Payne CR, Whigham LD, Johnson LK, Scheett AJ, et al. 2014. Foods advertised in US weekly supermarket sales circulars over one year: a content analysis. Nutr. J 13:95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jih J, Stijacic-Cenzer I, Seligman HK, Boscardin WJ, Nguyen TT, Ritchie CS. 2018. Chronic disease burden predicts food insecurity among older adults. Public Health Nutr. 21:1737–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jyoti DF, Frongillo EA, Jones SJ. 2005. Food insecurity affects school children’s academic performance, weight gain, and social skills. J. Nutr 135:2831–39 [DOI] [PubMed] [Google Scholar]
- 73.Karpyn A, Manon M, Treuhaft S, Giang T, Harries C, McCoubrey K. 2010. Policy solutions to the ‘grocery gap’. Health Aff. 29:473–80 [DOI] [PubMed] [Google Scholar]
- 74.Kim J 2015. Are older adults who participate in the Supplemental Nutrition Assistance Program healthier than eligible nonparticipants? Evidence from the Health and Retirement Study. Gerontologist 55:672 [Google Scholar]
- 75.Knowles M, Rabinowich J, Ettinger de Cuba S, Cutts DB, Chilton M. 2016. “Do you wanna breathe or eat?”: parent perspectives on child health consequences of food insecurity, trade-offs, and toxic stress. Matern. Child Health J 20:25–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kreider B, Pepper JV, Gundersen C, Jolliffe D. 2012. Identifying the effects of SNAP (Food Stamps) on child health outcomes when participation is endogenous and misreported. J. Am. Stat. Assoc 107:958–75 [Google Scholar]
- 77.Kreider B, Pepper JV, Roy M. 2016. Identifying the effects of WIC on food insecurity among infants and children. South. Econ. J 82:1106–22 [Google Scholar]
- 78.Laraia BA. 2013. Food insecurity and chronic disease. Adv. Nutr 4:203–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lopez A, Seligman HK. 2014. Online grocery store coupons and unhealthy foods, United States. Prev. Chronic Dis 11:130211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mabli J, Ohls J, Dragoset L, Castner L, Santos B. 2013. Measuring the effect of Supplemental Nutrition Assistance Program (SNAP) participation on food security. Nutr. Assist. Progr. Rep., Food Nutr. Serv., US Dep. Agric., Alexandria, VA: https://fns-prod.azureedge.net/sites/default/files/Measuring2013.pdf [Google Scholar]
- 81.Mangurian C, Sreshta N, Seligman H. 2013. Food insecurity among adults with severe mental illness. Psychiatr. Serv 64:931–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Martin KS, Rogers BL, Cook JT, Joseph HM. 2004. Social capital is associated with decreased risk of hunger. Soc. Sci. Med 58:2645–54 [DOI] [PubMed] [Google Scholar]
- 83.Martin-Biggers J, Yorkin M, Aljallad C, Ciecierski C, Akhabue I, et al. 2013. What foods are US supermarkets promoting? A content analysis of supermarket sales circulars. Appetite 62:160–65 [DOI] [PubMed] [Google Scholar]
- 84.Mayer VL, McDonough K, Seligman H, Mitra N, Long JA. 2016. Food insecurity, coping strategies and glucose control in low-income patients with diabetes. Public Health Nutr. 19:1103–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Melzer BT. 2011. The real costs of credit access: evidence from the payday lending market. Q. J. Econ 126:517–55 [Google Scholar]
- 86.Miller DP, Morrissey T. 2017. Using natural experiments to identify the effects of SNAP on child and adult health. Discuss. Pap. Ser. 105, Univ. Ky. Cent. Poverty Res., Lexington: https://uknowledge.uky.edu/ukcpr_papers/105 [Google Scholar]
- 87.Monteiro CA, Moubarac JC, Cannon G, Ng SW, Popkin B. 2013. Ultra-processed products are becoming dominant in the global food system. Obes. Rev 14(Suppl. 2):21–28 [DOI] [PubMed] [Google Scholar]
- 88.Morales ME, Epstein MH, Marable DE, Oo SA, Berkowitz SA. 2016. Food insecurity and cardiovascular health in pregnant women: results from the Food for Families program, Chelsea, Massachusetts, 2013–2015. Prev. Chronic Dis 13:160212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nord M, Prell M. 2011. Food security improved following the 2009 ARRA increase in SNAP benefits. Econ. Res. Rep. 116, Econ. Res. Serv., US Dep. Agric., Washington, DC: https://www.ers.usda.gov/webdocs/publications/44837/7469_err116.pdf?v=0 [Google Scholar]
- 90.Oddo VM, Mabli J. 2015. Association of participation in the Supplemental Nutrition Assistance Program and psychological distress. Am. J. Public Health 105:e30–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Olson CM, Bove CF, Miller EO. 2007. Growing up poor: long-term implications for eating patterns and body weight. Appetite 49:198–207 [DOI] [PubMed] [Google Scholar]
- 92.Palar K, Napoles T, Hufstedler LL, Seligman H, Hecht FM, et al. 2017. Comprehensive and medically appropriate food support is associated with improved HIV and diabetes health. J. Urban Health 94:87–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Park K, Kersey M, Geppert J, Story M, Cutts D, Himes JH. 2009. Household food insecurity is a risk factor for iron-deficiency anaemia in a multi-ethnic, low-income sample of infants and toddlers. Public Health Nutr. 12:2120–28 [DOI] [PubMed] [Google Scholar]
- 94.Popkin BM, Adair LS, Ng SW. 2012. Global nutrition transition: the pandemic of obesity in developing countries. Nutr. Rev 70:3–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Popkin SJ, Scott MM, Galvez MM. 2016. Impossible choices: teens and food insecurity in America. Res. Rep., Urban Inst., Washington, DC: https://www.urban.org/research/publication/impossible-choices-teens-and-food-insecurity-america [Google Scholar]
- 96.Rada R 2018. Chart of federal nutrition programs. National Conference of State Legislatures. http://www.ncsl.org/research/human-services/federal-nutrition-programs-chart.aspx [Google Scholar]
- 97.Ratcliffe C, McKernan S-M, Zhang S. 2011. How much does the Supplemental Nutrition Assistance Program reduce food insecurity? Am. J. Agric. Econ 93:1082–98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Rehkopf DH, Strully KW, Dow WH. 2014. The short-term impacts of Earned Income Tax Credit disbursement on health. Int. J. Epidemiol 43:1884–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rehm CD, Monsivais P, Drewnowski A. 2015. Relation between diet cost and Healthy Eating Index 2010 scores among adults in the United States 2007–2010. Prev. Med 73:70–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Rigdon J, Berkowitz SA, Seligman HK, Basu S. 2017. Re-evaluating associations between the Supplemental Nutrition Assistance Program participation and body mass index in the context of unmeasured confounders. Soc. Sci. Med 192:112–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Samuel LJ, Szanton SL, Cahill R, Wolff JL, Ong P, et al. 2018. Does the Supplemental Nutrition Assistance Program affect hospital utilization among older adults? The case of Maryland. Popul. Health Manag 21:88–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Santos R, Waxman E, Engelhard E. 2013. In short supply: American families struggle to secure everyday essentials. Rep., Feed. Am., Chicago [Google Scholar]
- 103.Schwartz MB. 2017. Moving beyond the debate over restricting sugary drinks in the Supplemental Nutrition Assistance Program. Am. J. Prev. Med 52:S199–205 [DOI] [PubMed] [Google Scholar]
- 104.Seligman HK, Basu S. 2018. In an unhealthy food system, what role should SNAP play? PLOS Med. 15:e1002662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. 2007. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. J. Gen. Intern. Med 22:1018–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Seligman HK, Bolger AF, Guzman D, López A, Bibbins-Domingo K. 2014. Exhaustion of food budgets at month’s end and hospital admissions for hypoglycemia. Health Aff. 33:116–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Seligman HK, Jacobs EA, López A, Tschann J, Fernandez A. 2012. Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care 35:233–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Seligman HK, Laraia BA, Kushel MB. 2010. Food insecurity is associated with chronic disease among low-income NHANES participants. J. Nutr 140:304–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Shankar P, Chung R, Frank DA. 2017. Association of food insecurity with children’s behavioral, emotional, and academic outcomes: a systematic review. J. Dev. Behav. Pediatr 38:135–50 [DOI] [PubMed] [Google Scholar]
- 110.Simmons M, Bishu KG, Williams JS, Walker RJ, Dawson AZ, Egede LE. 2018. Racial and ethnic differences in out-of-pocket expenses among adults with diabetes. J. Natl. Med. Assoc 10.1016/j.jnma.2018.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Skalicky A, Meyers AF, Adams WG, Yang Z, Cook JT, Frank DA. 2006. Child food insecurity and iron deficiency anemia in low-income infants and toddlers in the United States. Matern. Child Health J 10:177–85 [DOI] [PubMed] [Google Scholar]
- 112.Smith C, Klosterbuer A, Levine AS. 2009. Military experience strongly influences post-service eating behavior and BMI status in American veterans. Appetite 52:280–89 [DOI] [PubMed] [Google Scholar]
- 113.Stenmark S, Steiner JF, Marpadga S, Debor M, Underhill K, Seligman K. 2018. Lessons learned from implementation of the food insecurity screening and referral program at Kaiser Permanente, Colorado. Permanente J. 22:18–093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Stier M 2016. Who Benefits from the Philadelphia Soda Tax? Harrisburg: Pa. Budg. Policy Cent. [Google Scholar]
- 115.Sweet E, Nandi A, Adam EK, McDade TW. 2013. The high price of debt: household financial debt and its impact on mental and physical health. Soc. Sci. Med 91:94–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Szanton SL, Samuel LJ, Cahill R, Zielinskie G, Wolff JL, et al. 2017. Food assistance is associated with decreased nursing home admissions for Maryland’s dually eligible older adults. BMC Geriatr. 17:162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Tarasuk V, Cheng J, de Oliveira C, Dachner N, Gundersen C, Kurdyak P. 2015. Association between household food insecurity and annual health care costs. CMAJ 187:E429–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Tarasuk V, McIntyre L, Li J. 2007. Low-income women’s dietary intakes are sensitive to the depletion of household resources in one month. J. Nutr 137:1980–87 [DOI] [PubMed] [Google Scholar]
- 119.Torres J, De Marchis E, Fichtenberg C, Gottlieb L. 2017. Identifying food insecurity in health care settings: a review of the evidence. Res. Brief, Soc. Interv. Res. Eval. Netw., San Francisco: https://hungerandhealth.feedingamerica.org/wp-content/uploads/2017/11/SIREN_FoodInsecurity_Brief.pdf [Google Scholar]
- 120.Tunceli K, Bradley CJ, Lafata JE, Pladevall M, Divine GW, et al. 2007. Glycemic control and absenteeism among individuals with diabetes. Diabetes Care 30:1283–85 [DOI] [PubMed] [Google Scholar]
- 121.USDA (US Dep. Agric.). 2018. Definitions of food security. US Department of Agriculture. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/definitions-of-food-security.aspx [Google Scholar]
- 122.Vogenthaler NS, Kushel MB, Hadley C, Frongillo EA Jr., Riley ED, et al. 2013. Food insecurity and risky sexual behaviors among homeless and marginally housed HIV-infected individuals in San Francisco. AIDS Behav. 17:1688–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wetherill MS, White KC, Rivera C, Seligman HK. 2018. Challenges and opportunities to increasing fruit and vegetable distribution through the US charitable feeding network: increasing food systems recovery of edible fresh produce to build healthy food access. J. Hunger Environ. Nutr 10.1080/19320248.2018.1484315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Willink A, DuGoff EH. 2018. Integrating medical and nonmedical services—the promise and pitfalls of the CHRONIC Care Act. New Engl. J. Med 378:2153–55 [DOI] [PubMed] [Google Scholar]
- 125.Wilson N 2016. When the cupboards are bare: nudging food pantry clients to healthier foods. J. Assoc. Con. Res 1:125–33 [Google Scholar]
- 126.Wilson NLW, Just DR, Swigert J, Wansink B. 2017. Food pantry selection solutions: a randomized controlled trial in client-choice food pantries to nudge clients to targeted foods. J. Public Health 39:366–72 [DOI] [PubMed] [Google Scholar]