Abstract
Background:
Recent budget shortfalls may have resulted in decreases in the number of sexually transmissible infections (STIs) reported from sexually transmitted disease clinics (STDCs) in the United States (US). The objective of this study was to examine the proportion of cases reported from STDCs for three non-viral STIs in the last decade.
Methods:
Data from the national surveillance database on primary and secondary (P&S) syphilis, gonorrhoea and chlamydia cases for 2000–10 were extracted. The percentage of cases reported by STDCs for the nation and for each of the 48 contiguous states were then computed. Finally, the χ2 trend test for proportions was used to determine the annual average decrease/increase in the percentage of cases reported by STDCs for the nation and for each state.
Results:
Results demonstrate that the average annual declines in the proportion of P&S syphilis, gonorrhoea, and chlamydia cases reported from STDCs were 1.43% (P < 0.01), 1.31% (P < 0.01), and 0.31% (P < 0.01), respectively. Additionally, most of the states with statistically significant trends (P < 0.05) in the proportion of cases reported by STDCs had negative slopes: 86% (25/29) for P&S syphilis, 89% (34/38) for gonorrhoea, and 63% (27/43) for chlamydia.
Conclusion:
These results document the declining role of STDCs in STI prevention and control efforts in the US. Further studies are needed to assess the direct or indirect impact of the decline in the proportion of cases from STDCs on the overall STI control and prevention efforts in the US and its implications for the future.
Keywords: chlamydia, gonorrhoea, syphilis, trend analyses
Introduction
Sexually transmissible infections (STIs) in the US continue to be a public health challenge. Recent estimates indicate that in 2008, the number of new or newly diagnosed cases of eight STIs in the US was almost 20 million, with an estimated lifetime cost of approximately $16 billion dollars (2010 US dollars).1,2 This suggests an increase of over 1 million new or newly diagnosed cases when compared with the 2000 estimate.3 Thus, more effective prevention and control measures are needed.
The surveillance and monitoring activities for STIs provide vital information for assessing the burden of disease and help to inform the planning, implementation, and evaluation of interventions.4 Thus, annual STI surveillance reports produced and disseminated by the Division of Sexually Transmitted Disease Prevention (DSTDP) at the Centers for Disease Control and Prevention (CDC) provide information that plays a vital role in STI control and prevention efforts.
The US national sexually transmitted disease (STD) case surveillance data consist of case reports of notifiable diseases (i.e. required by law to be reported) that are provided to CDC by state and local STI programs and health departments, with a substantial proportion coming from categorical, publicly funded sexually transmitted disease clinics (STDCs).4 These case reports include those involving syphilis, gonorrhoea and chlamydia. STDCs play a significant role in the prevention and control of STIs by providing rapid detection and treatment.5–8 However, due to budget shortfalls at both the federal and state levels, there has been discontinuation of STI services in several areas, and the number of STDCs in the US has declined by ~10% over the last decade.6,9,10
The 2010 national STD surveillance report4 showed that the total number of cases reported by STDCs for the past decade was somewhat stable [primary and secondary (P&S) syphilis and chlamydia] or decreasing slightly (gonorrhoea).4 However, such numerator data do not provide information on the trends of STDCs contributions to the total number of reported cases. Consequently, the objective of this study is to examine the proportion of cases reported from STDCs in the US at national and state levels for three non-viral STIs over the past decade (2000–10). The STIs examined were P&S syphilis, gonorrhoea and chlamydia.
Methods
We extracted data from the national surveillance database for P&S syphilis, gonorrhoea, and chlamydia cases that were reported for 2000–10 for the nation, and then for each of the 48 contiguous states from all sources. There were a total of 22 broad sources. The sources were: STDC, Private Physician/Health Maintenance Organisation (HMO), Hospital – Other, Other Health Department Clinic, Family Planning Clinic, Missing, Laboratory, Hospital – Emergency Room, Unknown, Other, Correctional Facility, National Job Training Program, Military, HIV Counselling and Testing Sites, Indian Health Service, Prenatal, Drug Treatment, School-Based Clinic, Labour and Delivery, Tuberculosis Clinic, Blood Bank and Mental Health Provider. Invalid source codes were included in the Unknown category. All ages, genders and races were represented in the data.
Next, the percentage of cases reported by STDCs was computed for the nation and for each state. The χ2 test for trends in proportions was used to determine the annual average decrease/increase (slope) in the percentage of cases reported by STDCs for the nation and for each state. Next, we mapped the estimated average annual decrease/increase for each state. Finally, given the closure of STDCs in Massachusetts (MA) as a consequence of the passage of universal healthcare legislation in 2006,9 we separately examined trends of the proportion of reported cases from STDCs for MA. In particular, we performed and compared trend tests for the proportion of STI cases from STDCs in MA for two periods, namely 2000–08 and 2008–10. This was done to compare the estimated rate of decline (slope) before and after the enactment of the universal healthcare law in MA.
We used Microsoft Excel, version 2010 (Microsoft Corporation, Redmond, WA, USA) for extracting the data, computing the final proportion (%) of the cases reported from STDCs, and for producing the trend charts. All the χ2 tests for trends in proportions were conducted using STATA version 11.2 (StataCorp LP, College Station, TX, USA). Finally, the maps showing the estimated average annual decrease/increase in the proportion of reported cases from STDCs for the states were created with ArcGIS version 10 (ESRI, Redland, CA, USA).
Results
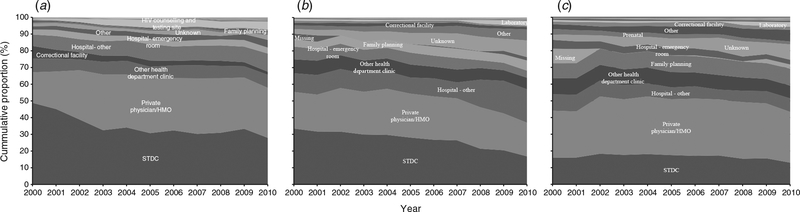
Figure 1 shows the trends in the decline in the proportion of cases of non-viral STIs reported from STDCs. Because our focus was on the proportions reported by STDCs, the proportions from STDCs are provided at the bottom of each figure followed by the remaining sources in decreasing order of their 2000 proportions. From 2000 to 2010, we estimated that the proportion of cases reported by STDCs nationwide declined from 48.9% to 28.0% (P&S syphilis; Fig. 1a), 33.5% to 18.6% (gonorrhoea; Fig. 1b) and 16.0% to 13.0% (chlamydia; Fig. 1c). The trend analysis demonstrates an average annual decline in the proportion of P&S syphilis, gonorrhoea, and chlamydia cases reported by STDCs of 1.4% (P < 0.01), 1.3% (P < 0.01), and 0.3% (P < 0.01), respectively.
Fig. 1.
(a) Cumulative proportion of reported cases of primary and secondary syphilis by source, 2000–10. Note: The following sources (Prenatal, Laboratory, Military, Drug Treatment, Blood Bank, National Job Training Program, Indian Health Services, Missing, Tuberculosis Clinic, Labour and Delivery, School-Based Clinic and Mental Health Provider) were not labelled because they were ≤2% in all the years examined. STDC, sexually transmitted disease clinics; HMO, health maintenance organisation. (b) Cumulative proportion of reported cases of gonorrhoea by source, 2000–10. Note: The following sources (Prenatal, Military, HIV Counselling and Testing Sites, Indian Health Services, National Job Training Program, Drug Treatment, Labour and Delivery, Tuberculosis Clinic, Blood Bank, School-Based Clinic and Mental Health Provider) were not labelled because they were ≤2% in all the years examined. (c) Cumulative proportion of reported cases of chlamydia by source, 2000–10. Note: The following sources (Military, HIV Counselling and Testing Sites, Indian Health Services, National Job Training Program, Drug Treatment, School-Based Clinic, Labour and Delivery, Tuberculosis Clinic, Blood Bank and Mental Health Provider) were not labelled because they were ≤2% in all the years examined.
State-level
P&S syphilis
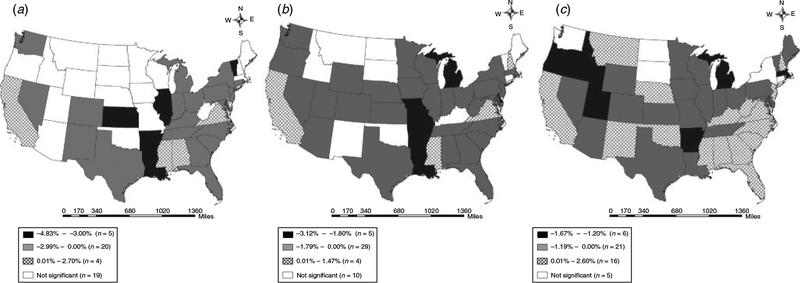
Figure 2a depicts the summary results of the trend tests performed for all the 48 contiguous states in the US for the proportion of P&S syphilis cases from STDCs, 2000–10. Based on our analysis, the estimated slopes of the trends in 19 of the 48 states were not statistically significant. Of the remaining 29 that had statistically significant (P < 0.05) slope estimates, 86% (n = 25) were negative. The states with the highest estimated annual average declines included Arkansas (−4.8%), Kansas (−4.4%), Louisiana (−4.2%), Illinois (−3.2%) and Vermont (−3.1%). The four states that had statistically significant positive slopes included Virginia (2.7%), Mississippi (2.4%), Alabama (0.7%) and California (0.6%).
Fig. 2.
Map of the estimated average annual change in the proportion of reported cases of (a) primary and secondary syphilis, (b) gonorrhoea and (c) chlamydia from sexually transmitted disease clinics (STDCs) by state, 2000–10.
Gonorrhoea
Figure 2b depicts the summary results of the trend tests performed for all the 48 contiguous states in the US for the proportion of chlamydia cases from STDCs, 2000–10. Based on our analysis, the estimated slopes in 10 of the 48 states were not statistically significant. Of the remaining 38 that had statistically significant (P < 0.05) slope estimates, 89% (n = 34) were negative. The states with the highest estimated annual average declines included Michigan (−3.1%), Louisiana (−2.5%), Arkansas (−2.2%), Missouri (−2.1%) and Delaware (−1.8%). The remaining four states that had statistically significant positive slopes included Mississippi (1.5%), Virginia (0.9%), New Hampshire (0.4%) and California (0.3%).
Chlamydia
Figure 2c depicts the summary results of the trend tests performed for all the 48 contiguous states in the US for the proportion of chlamydia cases from STDCs, 2000–10. Based on our analysis, the estimated slopes in five of the 48 states were not statistically significant. Of the remaining 43 that had statistically significant (P < 0.05) slope estimates, 63% (n = 27) were negative. The states with the highest estimated annual average declines included Idaho (−1.7%), Michigan (−1.6%), Massachusetts (−1.6%), Utah (−1.4%), Arkansas (−1.3%) and Oregon (−1.2%). Additionally, the states with the highest estimated annual average increases included Mississippi (2.6%), Alabama (1.5%), New Mexico (1.4%), Kentucky (1.1%) and West Virginia (0.9%).
Massachusetts
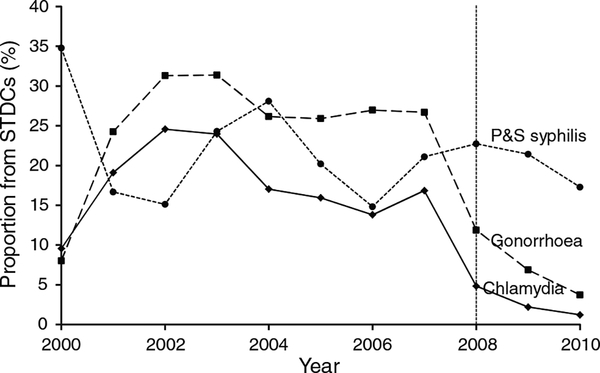
Figure 3 shows the trends in the decline in the proportion of cases of non-viral STIs reported from STDCs for Massachusetts (MA). From 2000 to 2010, we estimated that the proportion of cases reported from STDCs for MA declined from 34.8% to 17.3% (P&S syphilis), 8.0% to 3.7% (gonorrhoea) and 9.6% to 1.2% (chlamydia). The trend analysis indicated that the proportion of gonorrhoea and chlamydia cases reported by STDCs from 2000 to 2010 declined by 1.0% (P < 0.01) and 1.6% (P < 0.01) on average annually, respectively (P&S syphilis was not significant). When looking at 2008–10 data, the estimated proportion of cases from STDCs declined from 23% to 17% (P&S syphilis), from 12% to 4% (gonorrhoea), and from 5% to 1% (chlamydia).
Fig. 3.
Chart of the annual proportion of non-viral sexually transmissible infections (STIs) reported from sexually transmitted disease clinics (STDCs) for Massachusetts, 2000–10. P&S syphilis, primary and secondary syphilis.
When we performed the trend analysis for the two periods separately (2000–08 vs 2008–10), our results indicated that estimated average annual decline (slope) was substantially steeper for 2008–10 when compared with the estimated slope for 2000–08 for gonorrhoea [3.5% (P < 0.01) vs 0.2% (P < 0.05)] and chlamydia [1.7% (P < 0.01) vs 0.9% (P < 0.01)]. However, the estimated slopes for the proportion of P&S syphilis cases from STDCs were not statistically significant for either periods (i.e. 2000–08 and 2008–10).
Discussion
In this study, we analysed trends in the proportion of non-viral STI (i.e. primary and secondary [P&S] syphilis, gonorrhoea and chlamydia) cases reported from STDCs in the US at the national and state levels over the last decade. We found that overall, the proportion of P&S syphilis cases reported from STDCs declined by almost half (48.9% to 28.0%) at an estimated average annual rate of 1.4%; the proportion of gonorrhoea cases reported from STDCs declined from just over one-third to less than one-fifth (33.5% to 18.6%) at an estimated average annual rate of 1.3%; and the proportion of chlamydia cases reported from STDCs declined from 16.0% to 13.0% at an estimated average annual rate of 0.3%. Estimated average annual declines at the state level indicated that the majority of states had statistically significant declines in the proportion of cases reported from STDCs for all three STIs: 86% (25/29) for P&S syphilis, 89% (34/38) for gonorrhoea, and 63% (27/43) for chlamydia.
We also found a substantial decline in the proportion of gonorrhoea and chlamydia cases from STDCs in MA after 2008; the estimated annual rate of decline increased by at least twofold. At the national level, as the proportion of cases reported from STDCs declined, the cases reported from other sources (i.e. non-STDCs sources) picked up the slack. This is more evident for the STIs that experienced high declines in the proportion of cases reported from STDCs (syphilis and gonorrhoea). In particular, there were substantial increases in the proportion of cases reported from Private Physician/HMO (18% to 27%), Hospital – Other (7% to 10%) and HIV Counselling and Testing Sites (1% to 4%) for syphilis (Fig. 1a). For gonorrhoea, there were substantial increases in the proportion of cases reported from Hospital – Other (11% to 20%), Other (2% to 7%) and Laboratory (1% to 3%), as well as a considerable increase in the cases reported from sources coded as Unknown (3% to 10%; Fig. 1b). Shifting care to non-speciality providers could be helpful in some ways but harmful in others; providers who do not routinely diagnose or treat STIs may have more variability in quality of care (including treatment and partner services).6,11,12
No previous trend data showing the proportion of STI cases reported from STDCs in the US at the national and state levels have been published, thus, comparison with previous studies is not possible. Nonetheless, our results are consistent with what might be expected given the recent cuts in STI prevention funding at the state and local levels,6 and given that the number of STDCs has declined over the past decade.10 In MA, the corollary to the enacted universal healthcare law was an increase in access to private physicians and other health providers for STI services, thereby gradually eliminating the need for stand-alone STDCs. In fact, funding for STDCs was terminated in 2009.9 As a result, the sharp decline after 2008 was expected.
Limitations
This study has some limitations primarily associated with the surveillance data. In general, the surveillance data depend largely on medical providers testing and reporting practises.1 Thus, for chlamydia, inconsistencies associated with (or difference in) the nature of annual screening and reporting is more pronounced due to its asymptomatic nature.4 Consequently, some states (or jurisdictions) may focus testing on target populations and might potentially report higher rates among those populations. However, to the extent that these different testing and reporting practises are specific to individual jurisdictions, the inconsistencies might not be as much of a limitation as one would expect when looking at trends.4 It is also possible that the definition of STDC may vary, leading to inconsistent classification over time. Also, for each of the years examined, we found records where the source of the reported cases was coded missing/unknown (<11%). However, it is difficult to assess how these missing/unknown sources or other factors might impact our results. Finally, although we provided state-level results, we did not discuss specific reasons for the results we found for each state. This is because that would require more data (such as information on their STI reporting systems, adherence to reporting protocols, STDC location and their spatial distribution across the state, and STDC funding) from each state. Thus, analysis (and discussion) of the specific reasons for the increase/decrease in the proportion of STIs reported from STDCs for each state is beyond the scope of this study.
It is plausible that the decline in the number of cases reported from STDCs was a direct consequence of a decline in the volume of visits (or the volume of STI tests performed) at the STDCs, an actual decline in the number of patients with STIs who visited STDCs, or a combination of both. However, due to the lack of data on attendance (or the volume of tests conducted) at the different sources, information on positivity cannot be provided. Thus, it is important to note that this study analysed and provided information on the relative size of the ‘reported cases’ but does not provide any information on the relative volume of attendance (or testing) done at the different sources. More data is needed to examine the trends in the relative volume of visits (or volume of tests) and the related positivity outcomes for the different sources.
These results provide more specific information on the suggested declining role (in the area of STI surveillance and monitoring) of STDCs in the STI prevention and control efforts in the US. A recent study used county-level STI data from Texas to demonstrate the association between STI services (i.e. STDCs and family planning clinics) and STI morbidity.8 In their cross-sectional analysis, they found that counties with STDCs and family planning clinic services reported higher STIs rates on average than those without these services.8 However, their longitudinal analysis (i.e. comparing 2000 to 2007 STI rates), found that having these services was associated with a decline in STI rates. Their results suggests that the decline (or termination) of service provision by STDCs might affect the detection and control of STIs at both the local and national levels over time.6,9 More comprehensive research studies are needed to investigate the direct and/or indirect impact of the decline in the contribution of STDCs to the overall STI control and prevention efforts in the US and its implications for the future.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the United States Centers for Disease Control and Prevention (CDC). Mention of company names or products does not imply endorsement by the CDC.
Conflict of interest
None declared.
References
- 1.Owusu-Edusei K Jr, Chesson HW, Gift TL, Tao G, Mahajan R, Ocfemia MC, et al. The estimated direct medical cost of selected sexually transmitted infections in the United States, 2008. Sex Transm Dis 2013; 40: 197–201. doi: 10.1097/OLQ.0b013e318285c6d2 [DOI] [PubMed] [Google Scholar]
- 2.Satterwhite CL, Torrone E, Meitis E, Dunne EF, Mahajan R, Ocfemia MC, et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sex Transm Dis 2013; 40: 187–93. doi: 10.1097/OLQ.0b013e318286bb53 [DOI] [PubMed] [Google Scholar]
- 3.Weinstock H, Berman S, Cates W. Sexually transmitted diseases among American youth: incidence and prevalence estimates, 2000. Perspect Sex Reprod Health 2004; 36: 6–10. doi: 10.1363/3600604 [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Sexually transmitted disease surveillance, 2010. Atlanta, GA: U.S. Department of Health and Human Services; 2011. [Google Scholar]
- 5.Chorba T, Scholes D, BlueSpruce J, Operskalski BH, Irwin K. Sexually transmitted diseases and managed care: an inquiry and review of issues affecting service delivery. Am J Med Qual 2004; 19: 145–56. doi: 10.1177/106286060401900403 [DOI] [PubMed] [Google Scholar]
- 6.Golden MR, Kerndt PR. Improving clinical operations: can we and should we save our STD clinics? Sex Transm Dis 2010; 37: 264–5. [DOI] [PubMed] [Google Scholar]
- 7.Owusu-Edusei K Jr, Doshi SR. Assessing spatial gaps in sexually transmissible infection services and morbidity: an illustration with Texas county-level data from 2007. Sex Health 2012; 9: 334–40. doi: 10.1071/SH11117 [DOI] [PubMed] [Google Scholar]
- 8.Owusu-Edusei K Jr, Doshi SR. County-level sexually transmitted disease detection and control in Texas: do sexually transmitted diseases and family planning clinics matter? Sex Transm Dis 2011; 38: 970–5. doi: 10.1097/OLQ.0b013e3182215615 [DOI] [PubMed] [Google Scholar]
- 9.Felsenstein D A universal health insurance mandate does not equate to universal coverage for STI clinic patients (C3.3). National STD Prevention Conference; 12–15 March 2012, Minneapolis, MN, USA 2012. Available online at: https://cdc.confex.com/cdc/std2012/webprogram/Paper29952.html [verified 10 December 2012]. [Google Scholar]
- 10.Wong W Fact sheet: STD program capacity and preparedness in the United States: results of a National Survey. Washington, DC: National Coalition of STD Directors; 2009. [Google Scholar]
- 11.Eubanks C, Lafferty WE, Kimball AM, MacCornack R, Kassler WJ. Privatization of STD services in Tacoma, Washington: a quality review. Sex Transm Dis 1999; 26: 537–42. doi: 10.1097/00007435-199910000-00010 [DOI] [PubMed] [Google Scholar]
- 12.St. Lawrence JS, Montano DE, Kasprzyk D, Phillips WR, Armstrong K, Leichliter JS. STD screening, testing, case reporting, and clinical and partner notification practices: a national survey of US physicians. Am J Public Health 2002; 92: 1784–8. doi: 10.2105/AJPH.92.11.1784 [DOI] [PMC free article] [PubMed] [Google Scholar]