Abstract
Dry eyes is one of the most common complications after laser vision correction. Small incision lenticule extraction (SMILE) is a flapless procedure with a smaller corneal incision, less corneal nerves are transected during, making it theoretically less prone to dry eyes. Both SMILE and femtosecond-laser-assisted in situ keratomileusis (FS-LASIK) induce a transient worsening in dry eye parameters, but there is evidence showing that SMILE holds promises to have fewer negative impacts on the ocular surface parameters and allow an earlier recovery. SMILE-treated eyes may also have shown less corneal denervation and better corneal sensitivity compared with FS-LASIK eyes. This review summarizes the mechanisms of dry eyes after laser vision correction, the short-term (≤6 months) and long-term (>6 months) results in changes to dry eyes signs and symptoms, and corneal sensitivity of SMILE, as compared with FS-LASIK. Limitation of the studies and reasons accounting for their discrepancies will be discussed. Future randomized controlled trials with standardized postoperative regime are needed for better evaluation of dry eyes after SMILE.
Keywords: dry eyes, refractive surgery, SMILE
Dry eyes is one of the most frequent complications of refractive surgery.1 Among patients having laser in situ keratomileusis (LASIK), including microkeratome LASIK and FS-LASIK, 28% without previous dry eye symptoms developed new symptoms 3 months after surgery.2 Although the majority of postLASIK dry eye symptoms is temporary, some patients may experience longer disturbances. Bower et al estimated that 0.8% of patients who underwent LASIK experienced chronic postoperative dry eye lasting >12 months.3 Frequent tear supplement, anti-inflammatory agent, management of meibomian gland disease, punctal plug, and autologous serum may be required in patients with postLASIK dry eyes. Improper management could result in sight-threatening condition owing to chronic corneal surface complications.
Refractive lenticule extraction (ReLEx) is a relatively new technique to correct myopia and mild-to-moderate myopic astigmatism. Femtosecond lenticule extraction (FLEX) involves lifting a hinged flap, whereas SMILE is an all-in-one procedure without corneal flap creation. SMILE offers a novel and minimal invasive technique of using femtosecond laser to create an intrastromal lenticule that can be removed through a small incision of 3 to 4 mm, which is smaller than a standard 8- to 9-mm diameter LASIK flap. Involvement of the anterior cornea is spared in SMILE. With the absence of corneal flap and a smaller incision site, there is less damage to the subbasal nerve plexus and corneal stromal nerves. This could partially account for the higher levels of corneal sensitivity after SMILE, and theoretically reduce the incidence of dry eye after the procedure.
This review provides a summary of the mechanisms of dry eyes after SMILE and a comparison in the postoperative dry eye and corneal sensitivity changes between SMILE and FS-LASIK. We will also explore the reasons that could account for the discrepancies in the literature.
MECHANISM OF DRY EYES AFTER SMILE
The mechanism for the dry eye syndrome after corneal refractive surgery is multifactorial: decreased trophic influence on the corneal epithelium, impaired corneal sensation affecting blink reflex, damage to the limbal goblet cells during suction, inflammation, and the side effects of medication.4 Disruption of corneal innervation plays an important role in postrefractive surgery dry eye. The corneal nerve bundles enter from the periphery toward the center in a radial fashion to form a subepithelial nerve plexus beneath the Bowman membrane. The nerve bundles penetrate the Bowman membrane to form a subbasal nerve plexus, giving rise to the terminal nerves in the deep epithelium. The vertical incision in LASIK transects the subbasal nerve plexus beneath the corneal epithelium except for those at the hinge. LASIK damages both the dense subbasal nerve plexus and corneal stromal nerves in the creation of the anterior stromal flap and excimer laser photoablation, which could result in corneal and conjunctival hypersensitivity.5 This is known as neuropathic dry eyes with disproportionate dry eye sensation yet minimal clinical signs.6 Corneal nerve damage also affects the cornea-blink reflex and tear production reflex loop, leading to a reduction in tear secretion and tear film instability.7 Lee et al reported that the number of reinnervated corneal fibers at 1 year postLASIK remains at less than half of the baseline value.8 Contrary to LASIK, the all-in-one femtosecond SMILE no longer requires the use of excimer laser or a large flap cut. The smaller incision length in SMILE theoretically better preserves the subbasal nerve compared with LASIK.
Induced Corneal Inflammatory Response
Refractive surgeries also induce low-to-mild inflammatory response, which was shown to be involved in the postoperative wound-healing process.9 As a constituent in the normal tear fluid, interleukin-6 (IL-6) is a proinflammatory cytokine synthesized by keratocytes and endothelial cells. Upregulated IL-6 concentrations are observed in dry eye patients.10 Gao et al studied the tear inflammatory mediator levels after both SMILE and LASIK, and found that they both demonstrated upregulation of tear IL-6.11 However, there was a lower IL-6 level in SMILE group compared with FS-LASIK group at 1 week and 1 month postoperatively. SMILE group had a faster recovery to preoperative IL-6 level 1 month after surgery, compared with that 3 months after FS-LASIK.
Rapid recovery of corneal reinnervation is essential to restore the normal physiological features, tear secretion, and healing properties of the cornea. Trophic substance, such as nerve growth factor (NGF) concentration, is correlated with decreased corneal sensitivity in the early postoperative period.12 NGF was found to accelerate epithelium healing, induce keratocyte migration and facilitate corneal nerve regeneration.5,13 Study from Gao et al also reported increased tear NGF level after both procedures. However, NGF level in SMILE group improved and returned to its preoperative level, whereas the level in FS-LASIK group remained high after 3 months. Tear NGF concentrations were lower in SMILE group compared with FS-LASIK group at any time point during follow-up. However, there was no significant difference in other inflammatory mediators including tumor necrosis factor-α and Intercellular Adhesion Molecule 1. Gao et al reported negative correlations between NGF level and central corneal sensitivity in SMILE and FS-LASIK groups, thus suggesting that tear NGF may play a role in regulating corneal reinnervation after refractive surgeries.11
LITERATURE SEARCH
Two authors (A.W. and R.C.) independently searched the PubMed and MEDLINE for relevant publications from January 1, 2000 to March 31, 2019. Keywords including “small incision lenticule extraction,” “laser in situ keratomileusis,” “dry eye,” and “corneal sensitivity” were used in various and/or logic combinations. We reviewed the abstracts and retrieved full text for articles meeting our selection criteria. We included original studies or meta-analyses to compare both SMILE and FS-LASIK in correction on myopia and myopic astigmatism for discussion. Studies on LASIK procedure using microkeratome, and studies that did not compare SMILE and FS-LASIK in dry eye or corneal sensitivity were excluded. Letters, comments, conference abstracts, animal and laboratory studies, and nonEnglish articles were also excluded. Discrepancies were resolved by discussion with a third author (K.W.). We identified 14 original articles and 6 meta-analyses for discussion (Fig. 1).
FIGURE 1.
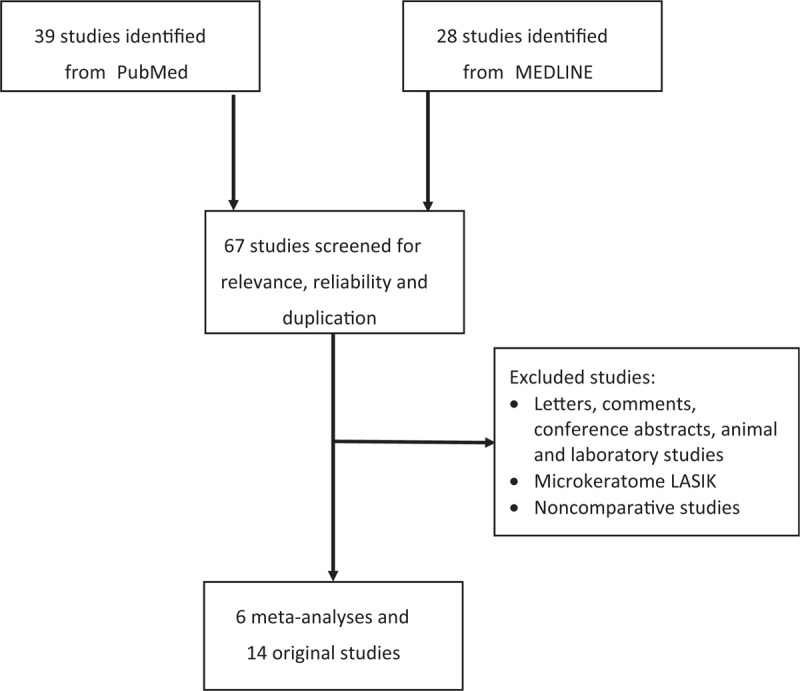
Flowchart showing how the studies were identified.
SHORT-TERM (≤6 MONTHS) DRY EYE OUTCOMES
Several studies compared the short-term results of dry eyes after SMILE and FS-LASIK at different postoperative times with varying results. Demirok et al14 reported similar results between SMILE and FS-LASIK. Their study was conducted in Turkey in 2013 which compared SMILE and FS-LASIK through a paired-eye study design, with 1 eye undergoing SMILE and the fellow eye undergoing FS-LASIK in 28 patients. They reported no significant change from baseline and between both groups in terms of subjective symptoms, Schirmer II test, tear breakup time (TBUT), and tear osmolarity after 1 week, 1 month, 3 months, and 6 months postoperatively.
In contrast, several studies reported better results in SMILE.15–19 Li et al in 2013 conducted a nonrandomized, prospective study on 71 eyes of 71 patients in China undergoing SMILE and FS-LASIK.17 Ocular surface disease index (OSDI) in both groups showed significant increase at 1 week (SMILE 23.95 vs FS-LASIK 18.78) after surgery comparing to baseline (P < 0.0001 and P = 0.010, respectively), but returned to normal at 1 month. No significant difference was found between both groups at 1 week, 1 month, and 3 months. However, SMILE group has better results in TBUT and corneal staining. Decreased TBUT at 1 week, 1 month, and 3 months was reported after SMILE compared with baseline [SMILE: 4.32, 5.68, 5.03 seconds and FS-LASIK: 4.70, 3.77, 4.43 seconds, respectively (P ≤ 0.001 for all)]. These results returned to the baseline level at postoperative 6 months (P = 0.080), but TBUT remained decreased after FS-LASIK throughout the study period at 1 week, 1 month, 3 months, and 6 months (P ≤ 0.002). After 6 months, there was a significant difference in TBUT scores between SMILE (7.06 seconds) and FS-LASIK (4.97 seconds) groups (P = 0.030). Compared with patients undergoing FS-LASIK, patients undergoing SMILE were less likely to have corneal staining (odd ratio 0.50, P = 0.030).
Xu et al18 in 2014 compared SMILE with FS-LASIK in a prospective nonrandomized study of 338 eyes in 176 patients in China. Both groups had significant lower TBUT at 1 month (6.79 vs 6.41 seconds, respectively) and 3 months (5.79 vs 5.67 seconds, respectively), with a modest improvement by 6 months postoperatively (7.39 vs 7.13 seconds). McMonnies questionnaire scores from both groups increased significantly at 1 month as compared with baseline (SMILE: 9.09–12.75 and FS-LASIK 8.60–12.48, P < 0.010 for both). However, SMILE group took 3 months (P = 0.080), whereas FS-LASIK group took 6 months (P = 0.170) to return to preoperative value. Ganesh and Gupta19 in India performed a single-center, randomized, prospective study in 50 patients undergoing bilateral SMILE or FS-LASIK in 2014. Three months after surgery as compared with the preoperative values, both groups demonstrated a reduction in Schirmer I test (SMILE: 33.04–31.94 mm, FS-LASIK: 33.96–26.84 mm), Schirmer II test (SMILE: 26.4–23.28 mm, FS-LASIK: 27.14–15.82 mm), and TBUT (SMILE: 12.32–10.92 seconds, FS-LASIK: 12.5–8.54 seconds). However, these postoperative values were significantly lower in FS-LASIK group (P < 0.001 for all parameters). Similarly, both groups showed increased tear osmolarity compared with baseline (SMILE: 300.3–314.67 mOsm/L and FS-LASIK: 302.3–321.18 mOsm/L), but the increase was significantly higher in the LASIK group (P < 0.001). Despite having a similar satisfactory score (an arbitrary score defined by the investigators) in patients with SMILE, patients in FS-LASIK group had more dry eye complaints including eye pain, watering, pricking.
Furthermore, Denoyer et al16 in 2015 conducted a similar but nonrandomized study with longer follow-up period on 30 patients in France. In addition, they performed corneal esthesiometry and in vivo confocal microscopy to correlate the function and structure of corneal innervation to the severity of postoperative dry eyes symptoms. One month after surgery, FS-LASIK group had a significantly higher incidence of mild-to-moderate dry eye disease, which remained similar after 6 months. 80% of SMILE patients versus 57% of FS-LASIK patients remained artificial tear-free. Among those requiring lubricants, 20% of FS-LASIK patients but none in SMILE group required daily or frequent use of lubricants after surgery. FS-LASIK group also had higher tear osmolarity 1 month after surgery, significantly high OSDI score, TBUT, and tear osmolarity 6 months after surgery. Corneal sensitivity was found to be negatively correlated to dry eye corneal staining (R2 = 0.48, P < 0.010). Long finer nerve density was reported to be independently correlated with OSDI score (R2 = 0.50, P < 0.010) and Schirmer test (R2 = 0.21, P < 0.010) 6 months after surgery. Xia et al15 in 2016 performed a larger study in China involving 128 eyes in 65 patients which showed favorable results toward SMILE. Decreased Schirmer test, TBUT, and higher OSDI were observed in both SMILE and FS-LASIK groups at 1 week, 1 month, 3 months, and 6 months. However, FS-LASIK group showed lower Schirmer test value (1 week: 5.6 vs 9.1 mm; 1 month: 7.6 vs 9.7 mm; 3 months: 10.4 vs 12.6 mm; 6 months: 9.3 vs 9.5 mm; P = 0.016), reduced TBUT (1 week: 4.5 vs 6.4 seconds; 1 month: 4.2 vs 9.7 seconds; 3 months: 5.1 vs 6.0 seconds; 6 months: 6.6 vs 6.3 seconds; P < 0.001), and higher OSDI (1 month: 26.03 vs 20.34; 3 months: 20.63 vs 14.91; 6 months: 16.00 vs 12.11; P < 0.001) than SMILE group.
LONG-TERM (>6 MONTHS) DRY EYE OUTCOMES
There is only 1 study comparing the dry eye parameters >6 months postoperatively. Elmohamady et al20 compared 35 eyes after SMILE and 35 eyes after FS-LASIK in Egypt with a follow-up period up to 3 years. By comparing their preoperative values, both groups had transient worsening in dry eye parameters including higher OSDI score and reduction in TBUT starting from the first month. SMILE took 3 months and 6 months, whereas FS-LASIK needed 6 months and 12 months for recovery from dry eye symptoms and TBUT reductions, respectively. No recurrence of dry eye was seen from 12 months onwards to 3 years among the groups.
CORNEAL SENSITIVITY
Demirok et al evaluated the corneal sensitivity at 3 locations of the cornea, including the superior, central, and inferior cornea.14 The study involved 56 eyes of 28 patients, prospectively randomized to have FS-LASIK in one eye and SMILE in the other eye. Mean corneal sensation was decreased at 1 week, 1 month, and 3 months (P < 0.050 for both groups at each follow-up period); significant changes compared with the preoperative value were no longer detected by 6 months. Corneal sensation at each corneal location was lower in the FS-LASIK group compared with the SMILE group up to 3 months postoperatively and was comparable by 6 months. Limitations of this study include its small sample size and lack of consideration of subjective dry eye symptoms in data collection.
Studies by Li et al also included a 6-month follow-up.17,21 One of their studies recruited 71 consecutive patients who had undergone SMILE or FS-LASIK with one eye randomly selected for analysis in the study. The other study included 32 eyes of 18 patients receiving SMILE and 42 eyes of 22 patients receiving FS-LASIK, with all the surgeries being performed by one surgeon. Both studies found that the central corneal sensitivity remained lower than its preoperative value by 6 months, with a trend of increasing corneal sensitivity toward the 6 months for both SMILE and FS-LASIK; however, SMILE achieved a sensitivity closer to its preoperative value.17,21 Li et al observed a higher mean central corneal sensitivity in the SMILE group compared with FS-LASIK group at all postoperative follow-up including 1 week (29.59 vs 20.61 mm, P = 0.030), 1 month (30.00 vs 21.45 mm, P = 0.040), 3 months (37.92 vs 27.50 mm, P = 0.010), and 6 months (46.94 vs 39.17 mm, P = 0.030).17 The reduction in subbasal nerve density in the SMILE group was less than that in the FS-LASIK group at 1 week (7608.3 vs 9431.0 μm/mm2, P = 0.015), 1 month (7642.1 vs 9316.7 μm/mm2, P = 0.024), and 3 months (6736.0 vs 8375.8 μm/mm2, P < 0.05); differences were not detected at the 6-month visit (5588.8 vs 5874.6 μm/mm2, P = 0.528). Greater decrease of subbasal nerve density after FS-LASIK up to 3 months postoperatively could be a result of more severe corneal nerve during the procedure. However, the undetectable differences between the 2 groups by 6 months may be because of factors that contribute to corneal nerve reinnervation. Correlation analysis demonstrated a moderate correlation between the subbasal nerve density and corneal sensitivity in the SMILE group (r = 0.42, P < 0.001) and a mild correlation in the FS-LASIK group (r = 0.26, P = 0.004).21
In the study by Gao et al11 with a follow-up of 3 months of 47 patients, the central corneal sensitivity returned to its preoperative level 3 months after SMILE, but remained significantly lower after FS-LASIK. Furthermore, the central corneal sensitivity of FS-LASIK group was significantly lower compared with that of SMILE at 1 week, 1 month, and 3 months postoperatively.
Wei et al compared the corneal sensitivity at the central cornea and the other 4 quadrants between FS-LASIK, ReLEx FLEX, and SMILE at 1 week, 1 month, and 3 months after surgery; they included 54 eyes of 27 subjects, 40 eyes of 22 subjects, and 61 eyes of 32 subjects for each procedure respectively.22 All corneal sensitivity parameters were reduced for the FS-LASIK group at each follow-up time points, wherein the corneal sensitivity was lowest at 1 week postoperatively and improved with time. In contrast, at 1 month after SMILE, there were no statistical differences in the superior and temporal quadrants’ corneal sensitivities compared with preoperative values; by 3 months, all regions returned to their baseline values. A limitation of this study includes the lack of a randomized study design, and further evaluation may require confocal microscopy studies and studies of pathological mechanisms.
FINDINGS FROM THE PUBLISHED META-ANALYSES
Six meta-analyses, which evaluated the differences in dry eyes and corneal sensitivity outcomes after SMILE and FS-LASIK, were published between 2015 and 2017.23–28 Characteristics of these meta-analyses are summarized in Table 1. The meta-analysis pooled results from 5 to 12 original articles, ranging from 1 to 3 randomized controlled trials. Kobashi et al,23 Cai et al,24 and Shen et al26 studied dry eye after SMILE and FS-LASIK as a primary outcome, whereas Zhang et al27 and Shen et al25 reported postoperative dry eye as secondary outcome. He et al28 focused on corneal sensitivity after the procedures. All articles included follow-up periods up to 6 months after the procedures. No significant difference was reported in the preoperative dry eye parameters among the 2 groups.
TABLE 1.
Characteristics of Published Meta-analyses in Dry Eyes After SMILE
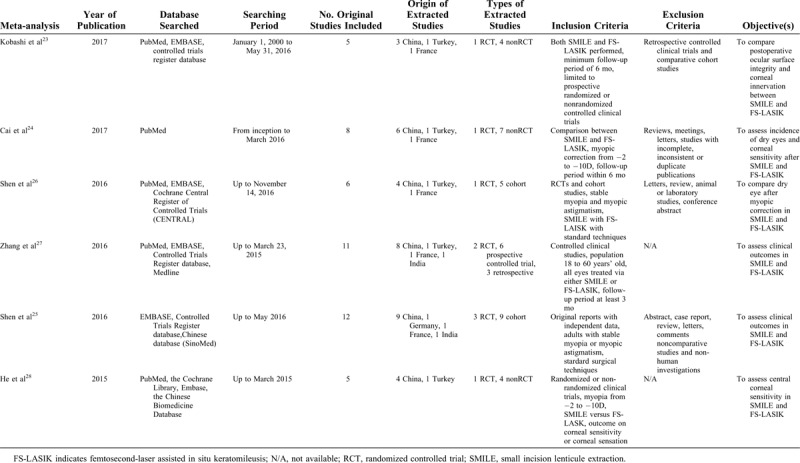
Results for postoperative dry eye from the above meta-analyses are shown in Tables 2 and 3. Mixed conclusions were drawn on postoperative dry eye parameters. Shen et al reported no obvious superiority of SMILE over FS-LASIK, but SMILE may have milder subjective symptoms.26 Kobashi et al23 and Cai et al24 drew a more favorable conclusion on SMILE over FS-LASIK.23,24 Kobashi et al23 concluded with the superiority of SMILE over FS-LASIK in having less postoperative dry eye, less negative impact on the ocular surface, and less damage on corneal innervation. Cai et al24 looked into a shorter period of the first 3 months and concluded that patients with SMILE recovered better from dry eye and corneal sensitivity after surgery.24 Both Zhang et al and Shen et al25,27 commented on postoperative dry eye as secondary outcome and both reached a similar conclusion that SMILE has fewer dry eye and less loss of corneal sensitivity than FS-LASIK. He et al focused on corneal sensitivity and reported smaller decrease and faster recovery in corneal sensitivity in the first 3 months in SMILE.28 Different dry eye parameters were studied among these meta-analyses (Table 2). Quantity of tear secretion23–27 and tear osmolarity23,26 were comparable at different time points between SMILE and FS-LASIK. However, more patients reported dry eye symptoms by having significantly higher OSDI score in FS-LASIK.23–26 Mixed results were shown for TBUT among both procedures, but more meta-analyses concluded that the reduction in TBUT was greater in FS-LASIK at certain time points. The difference in dry eye parameters leads to the conclusion that SMILE has less dry eye symptoms23,25–27 and loss of corneal sensation23–25,27,28 after SMILE than FS-LASIK.
TABLE 2.
Results from Meta-analyses in Postoperative Dry Eye Parameters Between SMILE and FS-LASIK
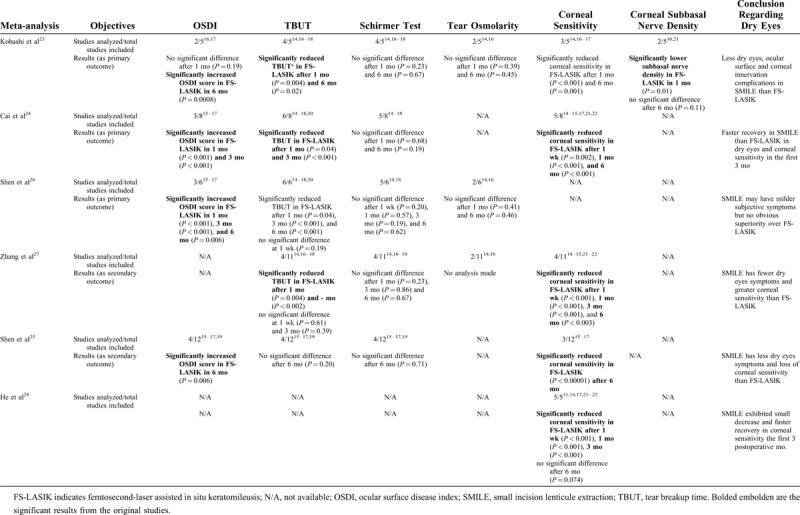
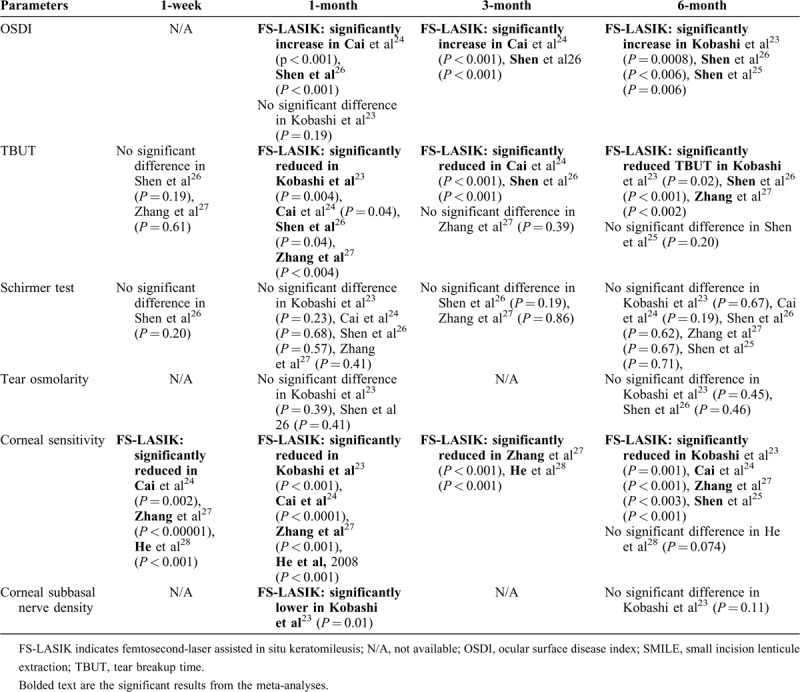
TABLE 3.
Postoperative Dry Eyes Parameters and Corneal Sensation Changes Over Time After SMILE and FS-LASIK
Corneal sensitivity was remarkably compromised in FS-LASIK lasting from the first week to 3 months, as shown by a meta-analysis by He et al28 that reported on the reduction of corneal sensitivity among SMILE and FS-LASIK as a primary outcome. The other 4 meta-analyses also showed similar result of significant reduction in corneal sensation in FS-LASIK than that in SMILE.23–25,27 However, these meta-analyses differ in the conclusion of recovery time. He et al28 showed that FS-LASIK recovered in corneal sensitivity to the extent of SMILE at 6 months, but other meta-analyses concluded a difference in corneal sensitivity persists between both groups 6 months postoperatively.23–25,27 However, Kobashi et al reviewed corneal subbasal nerve density in their meta-analysis and reported that the significantly low nerve density in FS-LASIK was only seen in the first month.23 Based on the conclusions drawn from these meta-analyses, it seems that SMILE has a less decrease in corneal sensation loss in the early postoperative time, but the rate of recovery among SMILE and FS-LASIK is still inconclusive.
By summarizing the results from these meta-analyses into different follow-up time frame, as shown in Table 3, we can compare the chronological change of dry eye parameters among SMILE and FS-LASIK. The first change that differed among SMILE and FS-LASIK is the loss in corneal sensitivity. This loss in corneal sensation after FS-LASIK was observed as early as the first week. The second difference is that FS-LASIK resulted in more corneal subbasal nerve damage, greater reduction in TBUT, and higher OSDI score at the first postoperative month. At the third month, patients still experienced more dry eye symptoms and lower corneal sensation in FS-LASIK group, although some authors suggested that rate of recovery in TBUT reduction in FS-LASIK is similar to that in FS-LASIK. At the sixth month, the significant loss in corneal sensitivity, OSDI score, and TBUT remained in FS-LASIK. The change in dry eye parameters at different time leads to the conclusion that SMILE has faster recovery in dry eye corneal sensitivity than FS-LASIK.24,28
DISCUSSION
The field of refractive surgeries has evolved rapidly in recent years. SMILE, as a relatively new procedure, is gaining more popularity especially after its FDA approval in 2016 for myopia and that in 2018 for the addition of astigmatism. Meta-analysis supports SMILE for having similar safety, efficacy, and predictability by comparing with FS-LASIK in the correction of myopia.25 The current literature of dry eye after SMILE showed that both SMILE and LASIK induced a transient worsening in dry eye parameters, but the majority of the studies supported that SMILE has less negative impacts on the ocular surface parameters, faster recovery in corneal sensitivity, and short term and long term by comparing with LASIK.
LASIK disrupts the corneal nerves in the creation of the corneal flap and during stromal ablation. Involvement of the anterior cornea is spared in SMILE, and with the absence of corneal flap and a smaller incision site, there is less damage to the subbasal nerve plexus and corneal stromal nerves. This could partially account for the higher levels of corneal sensitivity after SMILE. Corneal nerve damage may affect the reflex loops between cornea-blink and cornea-lacrimal gland, resulting in reduced tear secretion and tear film instability. SMILE also demonstrated raised but lower inflammatory mediators including IL-6 and NGF11 on ocular surface with faster recovery compared with FS-LASIK. Corneal inflammation may play a role in postoperative dry eyes after SMILE and FS-LASIK, but more evidence is needed to support this hypothesis.
The influence of incision size on dry eyes in SMILE also warrants further evaluation. Cetinkaya et al evaluated the influence of incision size (2 mm, 3 mm, or 4 mm) on dry eye symptoms in SMILE with a decrease in incision size during the course of the surgeon's learning curve.29 All 3 groups had a similar trend with early deterioration followed by improvement in dry eye parameters during the 6 months’ follow-up. For all 3 groups, TBUT and Schirmer test reached their preoperative values 1 month after SMILE, whereas OSDI and corneal staining score returned to their preoperative level after 3 months. No significant differences among the different incision size groups with respect to OSDI scores, TBUT, Schirmer test, and staining grade values were observed. These results signify that the variation in incision size between 2 and 4 mm in SMILE does not influence the dry eye parameters after SMILE. Therefore, larger incision sites can facilitate the procedure for the beginning surgeons during their learning curve.
However, the results of these original studies and meta-analyses should be interpreted with cautions. The number of trials is limited. The 6 meta-analyses for dry eyes identified only 5 to 11 studies with different designs, outcome measurement, and follow-up period, most of which are not randomized controlled trials. Most of the studies were conducted in China; therefore, the results may not be generalized to other ethnic population. The number of subjects is also limited to variation in baseline dry eye conditions among different interventional groups and studies. Variation in the postoperative regimen of topical lubricants and steroid use were present among the different original studies which were included in the meta-analyses. Some original studies allowed liberal use of lubricant pro re nata, whereas some did not report the frequency, dosage, and regime of lubricants used. Different postoperative regimen, and frequency of lubricants and topical steroid could account for the varying results among the literature. Xu and Yang18 used 0.1% sodium hyaluronate for 2 weeks, whereas Li et al17 used carboxymethylcellulose sodium tear supplement for 1 month. Denoyer et al16 and Xia et al15 prescribed lubricants regularly for 1 month and allowed patients to apply additional eyedrops according to their perceived dry eyes symptoms; however, the extra pro re nata dosage was not documented. In the remaining studies, no specific regime and dosage of lubricants were mentioned. The use of tear supplement could account for the difference in dry eye parameters. Also, the anti-inflammatory property of steroid also plays a role in dry eye signs and symptoms. Topical dexamethasone was used 4 times per day for 1 week in the study by Xia et al,15 but on a tapering regime of 6 to 3 times per day for 1 month in the study reported by Demirok et al14 and Denoyer et al.16 Li et al,17 and Xu and Yang18 used 0.1% fluorometholone for 2 to 3 weeks. Although the above studies concluded that a more favorable outcome of dry eyes in SMILE over FS-LASIK, and a more standardized postoperative drug regime are needed to evaluate dry eye changes after refractive surgeries.
Evolution in technology and technique may also affect the outcome. There is a range of femtosecond and excimer laser machines used among the studies which have different speed and technology. It remains to be elucidated whether these differences among the laser platforms may affect ocular surface and the sequential dry eye condition. Regarding corneal sensation, the assessment of corneal sensitivity by Cochet-Bonnet esthesiometry can be subjective. The assessment of corneal subbasal nerve density by confocal microscopy is operator-dependent. There is insufficient study to correlate loss of sensitivity or subbasal nerve plexus to the postoperative dry eye parameters. The above limitations jeopardize the validity of conclusions reached for postoperative dry eye after SMILE and FS-LASIK. The majority of studies only reported the short-term outcome with a paucity of long-term data. As the worsening of dry eyes can persist for a long period in a minority of patients, longer follow-up would be needed to better understand the changes in dry eyes and its impact on the quality of life after laser refractive surgery.
CONCLUSIONS
In conclusion, both SMILE and FS-LASIK induce or aggregate dry eye symptoms postoperatively; these changes seem to be transient. The evidence in the literature is mixed, but there are more original studies and meta-analyses to support dry eye parameters and recovery in corneal sensitivity after SMILE than that in FS-LASIK in the short term. However, this review highlights the need for more randomized controlled trial with a standardized protocol and postoperative management for better understanding of dry eye after SMILE.
Footnotes
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Toda I. LASIK and the ocular surface. Cornea 2008; 27 (suppl 1):S70–S76. [DOI] [PubMed] [Google Scholar]
- 2.Eydelman M, Hilmantel G, Tarver ME, et al. Symptoms and satisfaction of patients in the patient-reported outcomes with laser in situ keratomileusis (PROWL) studies. JAMA Ophthalmol 2017; 135:13–22. [DOI] [PubMed] [Google Scholar]
- 3.Bower KS, Sia RK, Ryan DS, et al. Chronic dry eye in photorefractive keratectomy and laser in situ keratomileusis: manifestations, incidence, and predictive factors. J Cataract Refract Surg 2015; 41:2624–2634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mian SI, Li AY, Dutta S, et al. Dry eyes and corneal sensation after laser in situ keratomileusis with femtosecond laser flap creation effect of hinge position, hinge angle, and flap thickness. J Cataract Refract Surg 2009; 35:2092–2098. [DOI] [PubMed] [Google Scholar]
- 5.Muller LJ, Marfurt CF, Kruse F, et al. Corneal nerves: structure, contents and function. Exp Eye Res 2003; 76:521–542. [DOI] [PubMed] [Google Scholar]
- 6.Chao C, Golebiowski B, Stapleton F. The role of corneal innervation in LASIK-induced neuropathic dry eye. Ocul Surf 2014; 12:32–45. [DOI] [PubMed] [Google Scholar]
- 7.Toda I. Dry eye after LASIK. Invest Ophthalmol Vis Sci 2018; 59:DES109–DES115. [DOI] [PubMed] [Google Scholar]
- 8.Lee BH, McLaren JW, Erie JC, et al. Reinnervation in the cornea after LASIK. Invest Ophthalmol Vis Sci 2002; 43:3660–3664. [PubMed] [Google Scholar]
- 9.Dong Z, Zhou X, Wu J, et al. Small incision lenticule extraction (SMILE) and femtosecond laser LASIK: comparison of corneal wound healing and inflammation. Br J Ophthalmol 2014; 98:263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Massingale ML, Li X, Vallabhajosyula M, et al. Analysis of inflammatory cytokines in the tears of dry eye patients. Cornea 2009; 28:1023–1027. [DOI] [PubMed] [Google Scholar]
- 11.Gao S, Li S, Liu L, et al. Early changes in ocular surface and tear inflammatory mediators after small-incision lenticule extraction and femtosecond laser-assisted laser in situ keratomileusis. PLoS One 2014; 9:e107370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee HK, Lee KS, Kim HC, et al. Nerve growth factor concentration and implications in photorefractive keratectomy vs laser in situ keratomileusis. Am J Ophthalmol 2005; 139:965–971. [DOI] [PubMed] [Google Scholar]
- 13.Blanco-Mezquita T, Martinez-Garcia C, Proenca R, et al. Nerve growth factor promotes corneal epithelial migration by enhancing expression of matrix metalloprotease-9. Invest Ophthalmol Vis Sci 2013; 54:3880–3890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Demirok A, Ozgurhan EB, Ağca A, et al. Corneal sensation after corneal refractive surgery with small incision lenticule extraction. Optom Vis Sci 2013; 90:1040–1047. [DOI] [PubMed] [Google Scholar]
- 15.Xia L, Zhang J, Wu J, et al. Comparison of corneal biological healing after femtosecond lasik and small incision lenticule extraction procedure. Curr Eye Res 2016; 41:1202–1208. [DOI] [PubMed] [Google Scholar]
- 16.Denoyer A, Landman E, Trinh L, et al. Dry eye disease after refractive surgery: comparative outcomes of small incision lenticule extraction versus LASIK. Ophthalmology 2015; 122:669–676. [DOI] [PubMed] [Google Scholar]
- 17.Li M, Zhao J, Shen Y, et al. Comparison of dry eye and corneal sensitivity between small incision lenticule extraction and femtosecond LASIK for myopia. PLoS One 2013; 8:e77797–e177797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xu Y, Yang Y. Dry eye after small incision lenticule extraction and LASIK for myopia. J Refract Surg 2014; 30:186–190. [DOI] [PubMed] [Google Scholar]
- 19.Ganesh S, Gupta R. Comparison of visual and refractive outcomes following femtosecond laser- assisted lasik with smile in patients with myopia or myopic astigmatism. J Refract Surg 2014; 30:590–596. [DOI] [PubMed] [Google Scholar]
- 20.Elmohamady MN, Abdelghaffar W, Daifalla A, et al. Evaluation of femtosecond laser in flap and cap creation in corneal refractive surgery for myopia: a 3-year follow-up. Clin Ophthalmol 2018; 12:935–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li M, Niu L, Qin B, et al. Confocal comparison of corneal reinnervation after small incision lenticule extraction (SMILE) and femtosecond laser in situ keratomileusis (FS-LASIK). PLoS One 2013; 8:e81435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wei S, Wang Y. Comparison of corneal sensitivity between FS-LASIK and femtosecond lenticule extraction (ReLEx flex) or small-incision lenticule extraction (ReLEx smile) for myopic eyes. Graefes Arch Clin Exp Ophthalmol 2013; 251:1645–1654. [DOI] [PubMed] [Google Scholar]
- 23.Kobashi H, Kamiya K, Shimizu K. Dry eye after small incision lenticule extraction and femtosecond laser-assisted LASIK: meta-analysis. Cornea 2017; 36:85–91. [DOI] [PubMed] [Google Scholar]
- 24.Cai WT, Liu QY, Ren CD, et al. Dry eye and corneal sensitivity after small incision lenticule extraction and femtosecond laser-assisted in situ keratomileusis: a meta-analysis. Int J Ophthalmol 2017; 10:632–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shen Z, Shi K, Yu Y, et al. Small incision lenticule extraction (SMILE) versus femtosecond laser-assisted in situ keratomileusis (FS-LASIK) for myopia: a systematic review and meta-analysis. PLoS One 2016; 11:e0158176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shen Z, Zhu Y, Song X, et al. Dry eye after small incision lenticule extraction (SMILE) versus femtosecond laser-assisted in situ keratomileusis (FS-LASIK) for myopia: a meta-analysis. PLoS One 2016; 11:e0168081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang Y, Shen Q, Jia Y, et al. Clinical outcomes of SMILE and FS-LASIK used to treat myopia: a meta-analysis. J Refract Surg 2016; 32:256–265. [DOI] [PubMed] [Google Scholar]
- 28.He M, Huang W, Zhong X. Central corneal sensitivity after small incision lenticule extraction versus femtosecond laser-assisted LASIK for myopia: a meta-analysis of comparative studies. BMC Ophthalmol 2015; 15:141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cetinkaya S, Gulmez M, Mestan E, et al. Influence of incision size on dry eye symptoms in the small incision lenticule extraction procedure. Cornea 2019; 38:18–23. [DOI] [PubMed] [Google Scholar]
- 30.Wang B, Naidu RK, Chu R, et al. Dry eye disease following refractive surgery: a 12-month follow-up of SMILE versus FS-LASIK in high myopia. J Ophthalmol 2015; 2015:132417. [DOI] [PMC free article] [PubMed] [Google Scholar]


