Abstract
In 1998 a Tolerable Upper Intake Level (UL) for folic acid was established based on case reports from the 1940s suggesting that high-dosage folic acid intake, used to treat patients with pernicious anemia, had the potential to precipitate or speed-up the development of neurological problems. This UL has been employed in the decision-making process used by more than 80 countries to establish programs to fortify staple foods with folic acid to prevent neural tube birth defects. Some have claimed that this UL is flawed and has become an obstacle to the wider adoption of neural tube defect prevention programs and have called for re-evaluation of the scientific validity of this UL. Case reports cannot establish causality, but they can reveal patterns in the timing of the onset and treatment of patients with pernicious anemia. These patterns can be compared with secular trends of usual medical practice for the treatment of pernicious anemia and with the changes in usage of folic acid preparations, including recommended therapeutic dosage and precautions for its usage surrounding the synthesis of folic acid in 1945 and vitamin B12 in 1948. Folic acid package inserts, early editions of hematology textbooks, and international expert reports provide valuable historical information. The recommended therapeutic daily dosage for folic acid of 5–20 mg was unchanged from 1946 through to 1971. The likely cause of the neurological problems encountered is the development of vitamin B12 neuropathy when pernicious anemia was treated with high-dosage folic acid before vitamin B12 was widely available in the early 1950s. Thus, the historical record does not provide compelling evidence that folic acid can potentially cause neurologic complications among those with low vitamin B12 status and lends support for reconsidering the basis for the UL of folic acid.
Keywords: pernicious anemia, folic acid, vitamin B12, neuropathy, folate, neural tube defects, public health, fortification
Introduction
Since the 1990s we have irrefutable evidence that the maternal intake of folic acid before and during early pregnancy prevents spina bifida and other neural tube birth defects (1–3). In 1992, the US Public Health Service recommended that women take 0.4 mg folic acid daily to reduce the risk of having a neural tube defect-affected pregnancy (4). In 1996, the Food and Drug Administration (FDA) approved mandatory folic acid fortification of enriched cereal grain products to prevent neural tube defect-affected pregnancies (5). In 1998, the Institute of Medicine (IOM) revised the Dietary Reference Intakes for folate and other B-vitamins (6). The IOM evaluated the efficacy of folic acid in preventing neural tube defect-affected pregnancies as well as evidence for the safety of folic acid fortification in the general population. Among case reports of patients with pernicious anemia, the IOM found more than 100 cases reporting neurological problems when taking ≥5 mg of folic acid daily compared with only 8 cases that reported neurological problems when taking ≥5 mg of folic acid daily (6). The IOM concluded from their review that there was “no clear evidence of folate-induced neurotoxicity in humans,” but established a Lowest Observed Adverse Effect Level of 5 mg of folic acid daily, because, “the weight of the limited but suggestive evidence that excessive folate intake may precipitate or exacerbate neuropathy in vitamin B12-deficient individuals justifies the selection of this end point as the critical end point for the development of a Tolerable Upper Intake Level (UL) for folate (6).” A UL for adults, which was set as 1 mg of folic acid daily from fortified foods or supplements, has been adopted by countries and organizations and is being used to set concentrations of folic acid added to staple food products in mandatory folic acid fortification programs to prevent neural tube defect-affected pregnancies (7, 8).
Concerns that high folic acid intake could precipitate or speedup the occurrence of the neurological manifestations of vitamin B12 deficiency have informed decisions regarding whether to recommend mandatory folic acid fortification of staple foods to prevent neural tube defects (8, 9). In 1995 Dickinson reviewed the neurological evidence from early case reports of the treatment of patients with pernicious anemia and found that the speed of progression of neurological problems was similar between those treated with and without folic acid. Dickinson also correctly pointed out that problems associated with the incorrect treatment of vitamin B12 deficiency anemia with folic acid should not be considered evidence that folic acid is toxic (10). A 2018 review in Public Health Reviews by Wald et al. re-evaluated the dosage evidence used by the IOM to create the UL in 1998 and found that “the rate of disease progression was no greater in patients taking higher doses of folic acid (11).” Wald et al. concluded that the IOM analysis was a flawed analysis of uncontrolled observational studies without evidential value and suggested that the scientific basis for the UL be reconsidered and called for the abandonment of the UL for folic acid. The situation was labeled a public health failure because the UL has been an obstacle to the wider adoption of mandatory fortification programs to prevent neural tube defects throughout the world (11). In countries that have adopted folic acid fortification, the UL has constrained the concentration of folic acid added to food, which results in a lower usual intake of folic acid. In other countries that have considered folic acid fortification, the presence of the UL creates concerns regarding potential adverse effects from folic acid fortification and delays or inhibits the adoption of mandatory fortification programs (8, 11).
This review adds historical information from the 1940s and 1950s that allows a more detailed assessment of the evidence that was derived from the case reports used by the IOM in 1998 to create the UL for folic acid. The historical information includes folic acid package inserts, which contain the recommended folic acid therapeutic dosage (including precautions), and descriptions of contemporaneous medical practice from early hematology textbooks and international reports (12, 13). Although other historical reviews have told the story of the people and events involved in the discoveries of folic acid and vitamin B12 (14, 15), this review uses newly obtained documents from the 1940s and subsequent decades to describe recommended medical practice on the use of folic acid. These documents enable a new examination of the timing of the diagnosis and treatment of the IOM case reports and finds little evidence to support the current concern that folic acid might precipitate or aggravate the neurological manifestations of vitamin B12 deficiency.
Background
Before folic acid and vitamin B12 were discovered in the 1940s, patients diagnosed as having “pernicious anemia” could have had macrocytic (megaloblastic) anemia caused by vitamin B12 deficiency, folate deficiency, or another nutritional deficiency. Prior to 1940, these macrocytic anemias were indistinguishable, but were effectively treated with liver and liver extracts, which contained vitamin B12 and folate (16). We now know that both vitamin B12 and folate are required for DNA synthesis necessary for the production of red blood cells. Among patients with vitamin B12 deficiency, high-dosage folic acid intake is able to bypass the vitamin B12 deficiency block and support DNA synthesis to return blood values to normal. In addition, we also know that pernicious anemia develops because of a malabsorption of vitamin B12, which is only effectively treated with vitamin B12 (13, 14). In present-day usage, pernicious anemia refers only to vitamin B12 deficiency anemia.
Discovery of folic acid and vitamin B12
In 1941 Mitchell and Snell purified a growth factor, that they named folic acid, from 4 tons of spinach (17). In 1943, folic acid was isolated from liver (18, 19), and in 1945 was synthetized by Lederle Laboratories (20). The optimal oral and parenteral folic acid dosage was unknown, so initially a wide range of daily dosages up to 600 mg was used (6, 21, 22). In 1946, an editorial in Blood called folic acid a “wonder drug” because a few milligrams daily produced a dramatic improvement in different types of macrocytic anemia (23). Lederle began the commercial production of a 5 mg folic acid tablet in 1946 and added a 20 mg folic acid tablet in 1947. Physicians quickly began to use folic acid instead of liver extracts for the treatment of “pernicious anemia” because it was cheaper, easier to use, and had fewer complications than injections of liver extracts (14).
However, in 1947, case reports of failure of folic acid to adequately treat “pernicious anemias” began to appear; some patients failed to maintain hematological remission when they were switched from liver therapy to folic acid (24–29). Some authors postulated folic acid was precipitating or exacerbating the neurological complications of “pernicious anemia” (24, 25, 30, 31). Scientists quickly recognized that folic acid was not treating the known neurological complications of “pernicious anemia,” and later in 1947, an editorial in the New England Journal of Medicine stated that folic acid provided “no new benefit but only risk to the patient” (32). The editorial added the strong recommendation that folic acid should not be used as the only treatment of “pernicious anemia,” which was confirmed by others (33). In 1948, vitamin B12 was isolated and purified and quickly became accepted as the appropriate treatment of vitamin B12 deficiency anemia (34, 35). In the early 1950s, pure vitamin B12, which was produced using bacterial culture production methods, became available in large enough quantities to” allow routine use for treating patients with this deficiency (36, 37).
Changes in recommended folic acid therapeutic dosages, tablet dose, and precautions
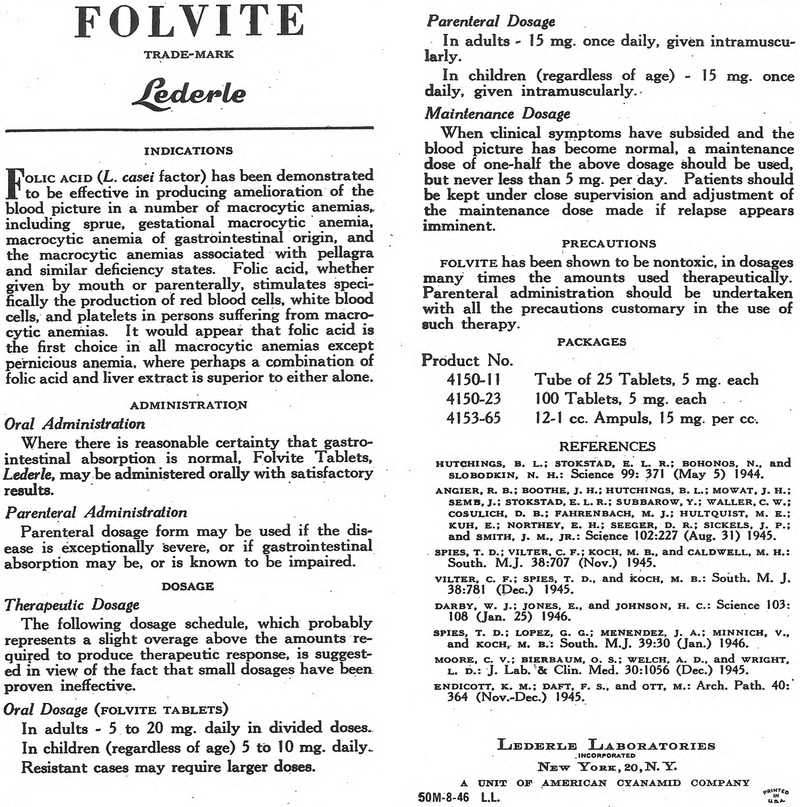
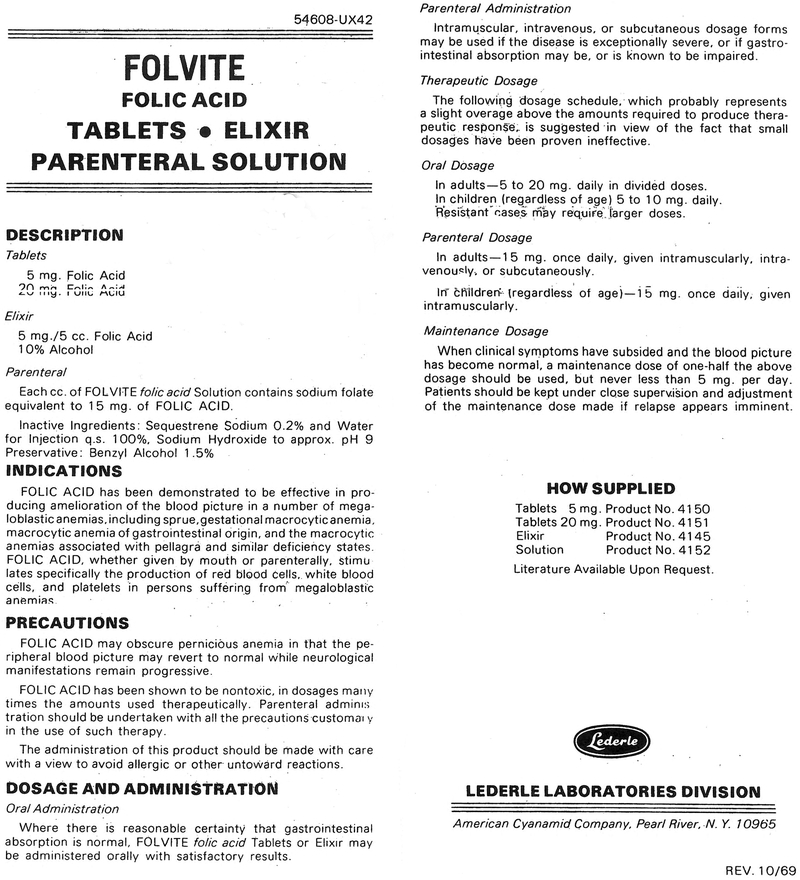
When Lederle Laboratories began production of folic acid tablets in 1946, the recommended daily therapeutic dosage to treat macrocytic anemias in adults was 5–20 mg of folic acid. Comparing the Folvite (folic acid) package insert from 1946 (Figure 1) with the insert from 1969 (Figure 2) confirms there were no changes in the wording describing the dose of available folic acid tablets, the recommended therapeutic dosage, or precautions regarding the potential adverse effects of folic acid. Production of these tablets was high; for example, Lederle reported that from January 1969 until 1971, when production of high-dosage tablets was stopped, over 31 million 5 mg and 846,000 20 mg tablets were produced (38). In 1971, the FDA changed the recommended daily therapeutic dosage to 0.25–1.0 mg of folic acid and lowered the dose of folic acid tablets allowed to 0.25 mg and 1.0 mg (39). The FDA made these changes to implement recommendations from an expert panel from the FDA’s Drug Efficacy Study, which was conducted during the 1960s (40). The FDA had concluded that “there is no evidence that doses of folic acid greater than 1 mg daily have greater efficacy than do those of 1 mg (39).” In 1974, a prominent hematology textbook confirmed the rationale for these changes: “Prior to 1971, the standard oral folic acid tablet contained 5 mg, an amount that is not only excessive, but also wasteful since much of it is excreted (13).”
FIGURE 1.
Package insert for Folvite revised August 1946.
FIGURE 2.
Package insert for Folvite revised October 1969.
Discussion
The IOM’s evaluation of high-dosage folic acid causing neurological manifestations
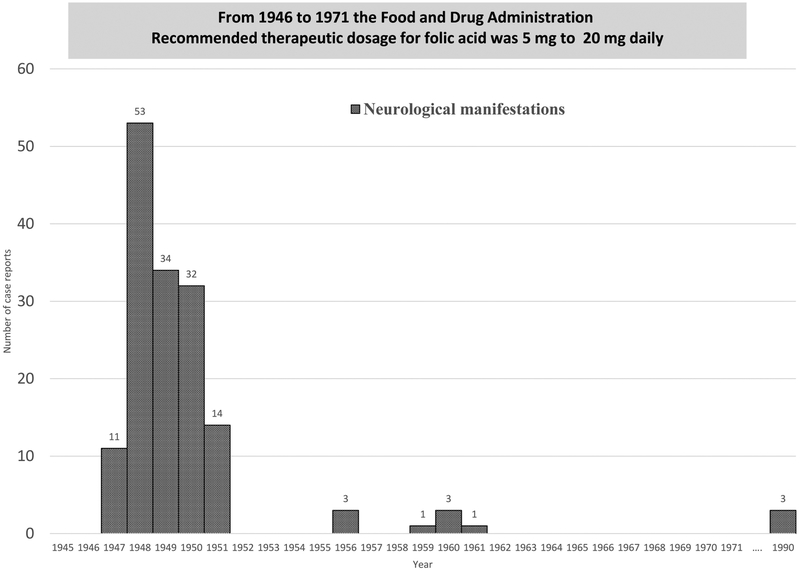
Concerns regarding high folic acid intake began in the 1940s during the period when the treatment of “pernicious anemia” changed from liver extracts to folic acid and later to vitamin B12. The 1998 IOM report identified 284 individual case reports, which were contained in 23 publications between 1947 and 1990. In 155 of these case reports, the IOM identified neurological manifestations (6). Table 1 shows the 23 publications sorted by approximate year of treatment with folic acid, which was determined by the year of publication (16 case reports from the 1940s, which were included in a 1959 review, were assigned to 1949) (41). Figure 3 shows that the number of case reports with neurological manifestations increased sharply in 1947 and decreased rapidly in 1951. Almost all of the 155 case reports, which were identified by the IOM as having neurological manifestations, were diagnosed and treated during the period of 1947–1951.
TABLE 1.
Case reports identified by the Institute of Medicine describing patients having neurological manifestations associated with high-dosage folic acid sorted by approximate year of treatment with folic acid, which was determined by the year of publication
| Year | Number of subjects | ||||
|---|---|---|---|---|---|
| Publication | Treatment | All | Neurological manifestations | Daily dosage (mg) | |
| Hall and Watkins (42) | 1947 | 1947 | 14 | 3 | 10–15 |
| Heinle and Welch (27) | 1947 | 1947 | 1 | 1 | 10–100 |
| Heinle et al. (43) | 1947 | 1947 | 16 | 2 | 10–40 |
| Spies and Stone (28) | 1947 | 1947 | 1 | 1 | 10 |
| Vilter et al. (26) | 1947 | 1947 | 21 | 4 | 50–500 |
| Berk et al. (31) | 1948 | 1948 | 12 | 3 | 10 |
| Bethell and Sturgis (44) | 1948 | 1948 | 15 | 4 | 5–20 |
| Jacobson et al. (45) | 1948 | 1948 | 1 | 1 | 10–65 |
| Ross et al. (30) | 1948 | 1948 | 4 | 1 | 1.25 |
| Ross et al. (30) | 1948 | 1948 | 15 | 8 | 5–45 |
| Spies et al. (46) | 1948 | 1948 | 38 | 28 | 10 |
| Wagley (22) | 1948 | 1948 | 10 | 8 | 5–600 |
| Fowler and Hendricks (47) | 1949 | 1949 | 2 | 2 | 15–20 |
| Israels and Wilkinson (48) | 1949 | 1949 | 20 | 16 | 5–40 |
| Will et al. (41)1 | 1959 | 1949 | 36 | 16 | 5–10 |
| Schwartz et al. (49) | 1950 | 1950 | 48 | 32 | 5 |
| Chodos and Ross (50) | 1951 | 1951 | 4 | 3 | 1.25 |
| Chodos and Ross (50) | 1951 | 1951 | 12 | 8 | 5–30 |
| Conley and Krevans (51) | 1951 | 1951 | 3 | 3 | 4.5–8 |
| Victor and Lear (52) | 1956 | 1956 | 3 | 3 | 1.5–2.55 |
| Best (53) | 1959 | 1959 | 1 | 1 | 10 |
| Crosby (54) | 1960 | 1960 | 1 | 1 | 0.35 |
| Ellison (55) | 1960 | 1960 | 2 | 2 | 0.33–6.4 |
| Baldwin and Dalessio (56) | 1961 | 1961 | 1 | 1 | 0.5 |
| Allen et al. (57) | 1990 | 1990 | 3 | 3 | 0.4–1 |
| Grand total | 284 | 155 | |||
Article includes 16 case reports from the 1940s that were assigned to 1949.
FIGURE 3.
Case reports identified by the Institute of Medicine that describe patients having neurological manifestations associated with high-dosage folic acid by the approximate year of treatment with folic acid, which was determined by the year of publication or treatment (16 case reports from the 1940s, which were included in a 1959 review, were assigned to 1949), N = 155.
Strength of evidence regarding folic acid dosage
Does the strength of evidence from the IOM case reports justify the concern that a relatively small daily intake of folic acid from fortification might aggravate neurological problems among seniors with low vitamin B12 status? Importantly, the IOM case reports were associated with folic acid dosages that are more than 10 times higher than the daily 0.4 mg that is currently recommended in the US (6), and even higher than the amount typically provided by the mandatory fortification of food staples (0.140 mg daily) (58). The IOM identified only 6 patients with neurological manifestations who reported taking a daily folic acid dosage of < 1 mg (54–57).
Masking the anemia of vitamin B12 deficiency
When the FDA reduced the recommended therapeutic dosage and the dose of folic acid tablets allowed in 1971, they also added a precaution to the package insert (Figure 2) that “folic acid may obscure pernicious anemia in that the peripheral blood picture may revert to normal whereas neurological manifestations remain progressive,” this precaution describes what has become known as masking (39). In the 1940s, the only routine diagnostic hematological tests available to clinicians were hemoglobin, hematocrit, and microscopic examination of stained blood smears (16). Mean corpuscular volume and red blood cell count were laborious research methods performed manually; blood folate and vitamin B12 assays were not yet developed. If masking of the anemia of vitamin B12 deficiency were to occur today, one would expect to find less anemia among adults with newly diagnosed vitamin B12 deficiency. Both Mills and Qi have searched for and found no such evidence to support the occurrence of masking (59, 60). Although it is possible that masking of the anemia of vitamin B12 deficiency could occur today from inappropriate treatment of vitamin B12 deficiency with high-dosage folic acid, dramatic improvements in clinical laboratory testing and the practice of medicine over the past 70 y makes the occurrence of such masking highly unlikely. In addition, others have concluded that masking does not exist (61–63). Consequently, masking of the anemia of vitamin B12 deficiency should not be considered a potential adverse effect resulting from mandatory fortification with folic acid.
Could high-dosage folic acid have caused neurological manifestations?
We now know that severe vitamin B12 deficiency disease is associated with signs and symptoms that eventually might include severe macrocytic (megaloblastic) anemia, diarrhea, loss of appetite, glossitis, and severe neurological complications including confusion, depression, and sensory changes (14, 64, 65). This disease has a varied clinical presentation and might present with neurological signs and symptoms even in the absence of anemia (65–67). In addition, rapid progression of the neuropathy of “pernicious anemia” was described well before folic acid became available (68). From 1946 to 1971, the recommended daily therapeutic dosage for folic acid was 5–20 mg for adults; therefore, exposure to high-dosage folic acid continued for 20 y until 1971, with only 11 sporadic case reports detailing neurological manifestations being reported after 1951 (52–57). If high-dosage folic acid had directly caused neurological manifestations among patients with “pernicious anemia,” then additional case reports would have been expected to occur throughout the 1950s and 1960s until the FDA lowered the folic acid therapeutic recommendations in 1971. The fact that case reports of neurological manifestations virtually disappeared after vitamin B12 became commercially available in the early 1950s suggests that the case reports with neurological manifestations identified by the IOM were due to the unavoidable error of treating vitamin B12 deficiency with folic acid alone for months or years.
The historical evidence regarding the timing of case reports of neurological manifestations and the lack of changes in recommendations and usage of folic acid does not support the idea that folic acid directly causes neurological problems among adults with low vitamin B12 status. Despite the weakness of this evidence, in a recent British Medical Journal Head to Head on the safety of folic acid fortification, Reynolds used this evidence to argue that folic acid fortification had the potential to cause neurological damage (69).
Strength of evidence
Modern evidence-based scientific practice has dictated that, where possible, randomized trials, as well as systematic reviews and meta-analyses, which utilize high-quality studies, are required to establish scientifically valid assertions of causality and that only these sources of evidence be used in formulating recommendations and public health policy (70). As highlighted by Wald et al. (11), case reports provide very poor evidence for establishing causality because of serious methodological limitations such as lack of control/comparison groups. However, case reports were the primary scientific methodology used in clinical publications during the 1940s. A recent evidence-based review conducted by the UK’s Scientific Advisory Committee on Nutrition identified no studies with high-quality evidence that could be used to evaluate the risk of folic acid masking or exacerbating vitamin B12 deficiency in adults (9). It is unlikely that a systematic review of the evidence could ever resolve these concerns because the only available data for such a review are historical case reports, and generating new evidence by conducting a randomized trial of treating patients with vitamin B12 deficiency with high-dosage folic acid alone would be unethical.
Conclusions
This review of historical information suggests that the most likely explanation for the neurological manifestations associated with the use of high-dosage folic acid to treat “pernicious anemia” is that folic acid restored normal hematological blood values, but did not prevent the neuropathy of vitamin B12 deficiency. This therapeutic error occurred because of the gap between folic acid becoming available to treat macrocytic anemia in the early 1940s and vitamin B12 becoming widely available for clinical use in the early 1950s. The most likely explanation for the sharp decline in case reports with neurological manifestations in the early 1950s is that clinicians stopped using folic acid alone to treat “pernicious anemia.” During the 1950s, textbooks confirmed that there were no changes in recommended folic acid therapeutic dosage, the dose of folic acid tablets, or precautions that could account for the rapid decline in case reports of high-dosage folic acid associated with neurological manifestations.
Even as late as 1988, an FAO/WHO expert consultation found no evidence of folate toxicity stating, “no toxicity has been reported at the concentration of the doses of folate discussed in the preceding sections of this report” and “in the past, concern has been expressed that folate supplementation (as in pregnancy) given to a person with early vitamin B12 deficiency, could precipitate neuropathy. However, no such cases have been reported (12).” Thus, the historical record does not provide compelling evidence that current folic acid food fortification has the potential to cause neurologic complications among those with low vitamin B12 status and lends support for reconsidering the basis for the UL as proposed by Wald et al. In summary, findings from the historical record support the value of promoting folic acid fortification as a safe and effective intervention that could, if more fully implemented, annually prevent thousands of additional neural tube defect-affected pregnancies worldwide.
Acknowledgments
The author reported no funding received for this study.
Abbreviations used:
- FDA
Food and Drug Administration
- IOM
Institute of Medicine
- UL
Tolerable Upper Intake Level
References
- 1.MRC Vitamin Study Research Group. Prevention of neural tube defects: Results of the Medical Research Council Vitamin Study. Lancet 1991;338:131–7. [PubMed] [Google Scholar]
- 2.Czeizel AE, Dudas I. Prevention of the first occurrence of neural-tube defects by periconceptional vitamin supplementation. N Engl J Med 1992;327(26):1832–5. [DOI] [PubMed] [Google Scholar]
- 3.Berry RJ, Li Z, Erickson JD, Li S, Moore CA, Wang H, Mulinare J, Zhao P, Wong LY, Gindler J, et al. Prevention of neural-tube defects with folic acid in China. China-U.S. Collaborative Project for Neural Tube Defect Prevention. N Engl J Med 1999;341(20):1485–90. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Recommendations for the use of folic acid to reduce the number of cases of spina bifida and other neural tube defects. MMWR Recomm Rep 1992;41(RR-14):1–7. [PubMed] [Google Scholar]
- 5.Food US and Administration Drug. Food standards: Amendment of standards of identity for enriched grain products to require addition of folic acid Final Rule. 21 CFR Parts 136, 137, and 139. Fed Reg; 1996;61:8781–9. [Google Scholar]
- 6.Institute of Medicine. Folate Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington, DC: National Academy Press; 1998:196–305. [PubMed] [Google Scholar]
- 7.Berry RJ, Mulinare J, Hamner HC. Folic acid fortification: Neural tube defect risk reduction - A global perspective In: Bailey LB, ed. Folate in Health and Disease. Boca Raton, Fl: CRC Press; 2010:179–204. [Google Scholar]
- 8.Crider KS, Bailey LB, Berry RJ. Folic acid food fortification–its history, effect, concerns, and future directions. Nutrients 2011;3:370–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scientific Advisory Committee on Nutrition. Update Report on Folic Acid. Norwich, England: The Stationery Office; 2017. [Google Scholar]
- 10.Dickinson CJ. Does folic acid harm people with vitamin B12 deficiency? QJM 1995;88(5):357–64. [PubMed] [Google Scholar]
- 11.Wald NJ, Morris JK, Blakemore C. Public health failure in the prevention of neural tube defects: Time to abandon the tolerable upper intake level of folate. Public Health Rev 2018;39(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Food and Agriculture Organization. Folate Requirements of Vitamin A, Iron, Folate and Vitamin B12 Report of a Joint FAO/WHO Expert Consultation. Rome, Italy: Food and Agriculture Organization; 1988:51–61. [Google Scholar]
- 13.Wintrobe MM. Macrocytosis and Macrocytic Anemias Clinical Hematology. Philadelphia: Lea & Febiger; 1974:566–601. [Google Scholar]
- 14.Chanarin I Historical review: A history of pernicious anaemia. Br J Haematol 2000;111(2):407–15. [DOI] [PubMed] [Google Scholar]
- 15.Hoffbrand AV, Weir DG. The history of folic acid. Br J Haematol 2001;113(3):579–89. [DOI] [PubMed] [Google Scholar]
- 16.Wintrobe MM. Pernicious Anemia Clinical Hematology. Philadelphia: Lea & Febiger; 1942:310–38. [Google Scholar]
- 17.Mitchell HK, Snell EE, Williams RJ. The concentration of “folic acid”. J Am Chem Soc 1941;63(8):2284. [Google Scholar]
- 18.Pfiffner JJ, Binkley SB, Bloom ES, Brown RA, Bird OD, Emmett AD, Hogan AG, O’Dell BL. Isolation of the antianemia factor (Vitamin Bc) in crystalline form from liver. Science 1943;97(2522): 404–5. [DOI] [PubMed] [Google Scholar]
- 19.Stokstad ELR. Some properties of a growth factor for Lactobacillus casei. J Biol Chem 1943;149:573–4. [Google Scholar]
- 20.Angier RB, Boothe JH, Hutchings BL, Mowat JH, Semb J, Stokstad EL, Subbarow Y, Waller CW, Cosulich DB, Fahrenbach MJ, et al. Synthesis of a compound identical with the L. casei factor isolated from liver. Science 1945;102(2644):227–8. [DOI] [PubMed] [Google Scholar]
- 21.Spies TD, Vilter CF, Koch MB, Caldwell MH. Observations of the anti-anemic properties of synthetic folic acid. South Med J 1945;38(11):707–9. [Google Scholar]
- 22.Wagley PF. Neurologic disturbances with folic acid therapy. N Engl J Med 1948;238(1):11–5. [DOI] [PubMed] [Google Scholar]
- 23.Dameshek W Editorial. Blood 1946;1(4):357. [Google Scholar]
- 24.Sargent F Folic acid: Pteroylglutamic acid and related substances. N Engl J Med 1947;237(18):667–72. [DOI] [PubMed] [Google Scholar]
- 25.Sargent F Folic acid; pteroylglutamic acid and related substances. N Engl J Med 1947;237(19):703–7. [DOI] [PubMed] [Google Scholar]
- 26.Vilter CF, Vilter RW, Spies TD. The treatment of pernicious and related anemias with synthetic folic acid; observations on the maintenance of a normal hematologic status and on the occurrence of combined system disease at the end of one year. J Lab Clin Med 1947;32(3): 262–73. [PubMed] [Google Scholar]
- 27.Heinle RW, Welch AD. Folic acid in pernicious anemia; failure to prevent neurologic relapse. JAMA 1947;133(11):739–41. [DOI] [PubMed] [Google Scholar]
- 28.Spies T, Stone R. Liver extract, folic acid, and thymine in pernicious anaemia and subacute combined degeneration. Lancet 1947;249(6440):174–6. [DOI] [PubMed] [Google Scholar]
- 29.Meyer LM. Folic acid in the treatment of pernicious anemia. Blood 1947;2(1):50–62. [PubMed] [Google Scholar]
- 30.Ross JF, Belding H, Paegel BL. The development and progression of subacute combined degeneration of the spinal cord in patients with pernicious anemia treated with synthetic pteroylglutamic (folic) acid. Blood 1948;3(1):68–90. [PubMed] [Google Scholar]
- 31.Berk L, Bauer JL, Castle WB. A report of 12 patients treated with synthetic pteroylglutamic acid with comments on the pertinent literature. S Afr Med J 1948;22:604–11. [Google Scholar]
- 32.Massachusetts Medical Society. Warning regarding the use of folic acid. N Engl J Med 1947;237(19):715. [DOI] [PubMed] [Google Scholar]
- 33.Davidson LS, Girdwood RH. Folic acid as a therapeutic agent. BMJ 1947;1(4504):587–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rickes EL, Brink NG, Koniuszy FR, Wood TR, Folkers K. Crystalline vitamin B12. Science 1948;107(2781):396–7. [DOI] [PubMed] [Google Scholar]
- 35.Smith EL. Purification of anti-pernicious anaemia factors from liver. Nature 1948;161(4095):638. [DOI] [PubMed] [Google Scholar]
- 36.Castle WB. The conquest of pernicious anemia In: Wintrobe MM, ed. Blood, Pure and Eloquent. New York: McGraw-Hill; 1980: 283–317. [Google Scholar]
- 37.Martens JH, Barg H, Warren M, Jahn D. Microbial production of vitamin B12. Appl Microbiol Biotechnol 2002;58(3): 275–85. [DOI] [PubMed] [Google Scholar]
- 38.Lederle Laboratories. Annual report to FDA on products containing folic acid covered by NDA 5897. Food and Drug Administration, 1971. [Google Scholar]
- 39.Food and Drug Administration. Folic acid preparations, oral and parenteral for therapeutic use. Fed Reg 1971;36: 6843–4. [Google Scholar]
- 40.Massachusetts Medical Society. The drug efficacy study. N Engl J Med 1969;280(21):1177–9. [DOI] [PubMed] [Google Scholar]
- 41.Will JJ, Mueller JF, Brodine C, Kiely CE, Friedman B, Hawkins VR, Dutra J, Vilter RW. Folic acid and vitamin B12 in pernicious anemia; studies on patients treated with these substances over a ten year period. J Lab Clin Med 1959;53(1):22–38. [PubMed] [Google Scholar]
- 42.Hall BE, Watkins CH. Experience with pterolyglutamic (synthetic folic) acid in the treatment of pernicious anemia. J Lab Clin Med 1947;32(6):622–34. [PubMed] [Google Scholar]
- 43.Heinle RW, Dingle JT, Weisberger AS. Folic acid in the maintenance of pernicious anemia. J Lab Clin Med 1947;32(8):970–81. [PubMed] [Google Scholar]
- 44.Bethell FH, Sturgis CC. The relation of therapy in pernicious anemia to changes in the nervous system; early and late results in a series of cases observed for periods of not less than ten years, and early results of treatment with folic acid. Blood 1948;3(1):57–67. [PubMed] [Google Scholar]
- 45.Jacobson SD, Berman L, Axelrod AR, Vonder Heide EC. Folic acid therapy; its effect as observed in two patients with pernicious anemia and neurologic symptoms. JAMA 1948;137(10):825–7. [DOI] [PubMed] [Google Scholar]
- 46.Spies TD, Stone RE. The association between gastric achlorhydria and subacute combined degeneration of the spinal cord. Postgrad Med 1948;4(2):89–95. [DOI] [PubMed] [Google Scholar]
- 47.Fowler WM, Hendricks AB. Folic acid and the neurologic manifestations of pernicious anemia. Am Pract Dig Treat 1949;3(10):609–13. [PubMed] [Google Scholar]
- 48.Israels MC, Wilkinson JF. Risk of neurological complications in pernicious anaemia treated with folic acid. BMJ 1949;2(4636):1072–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schwartz SO, Kaplan SR, Armstrong BE. The long-term evaluation of folic acid in the treatment of pernicious anemia. J Lab Clin Med 1950;35(6):894–8. [PubMed] [Google Scholar]
- 50.Chodos RB, Ross JF. The effects of combined folic acid and liver extract therapy. Blood 1951;6(12):1213–33. [PubMed] [Google Scholar]
- 51.Conley CL, Krevans JR. Development of neurologic manifestations of pernicious anemia during multivitamin therapy. N Engl J Med 1951;245(14):529–31. [DOI] [PubMed] [Google Scholar]
- 52.Victor M, Lear AA. Subacute combined degeneration of the spinal cord; current concepts of the disease process; value of serum vitamin B12; determinations in clarifying some of the common clinical problems. Am J Med 1956;20(6):896–911. [DOI] [PubMed] [Google Scholar]
- 53.Best CN. Subacute combined degeneration of spinal cord after extensive resection of ileum in Crohn’s disease: Report of a case. BMJ 1959;2(5156):862–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Crosby WH. The danger of folic acid in multivitamin preparations. Mil Med 1960;125:233–5. [PubMed] [Google Scholar]
- 55.Ellison ABC. Pernicious anemia masked by multivitamins containing folic acid. JAMA 1960;173(3):240–3. [DOI] [PubMed] [Google Scholar]
- 56.Baldwin JN, Dalessio DJ. Folic acid therapy and spinal-cord degeneration in pernicious anemia. N Engl J Med 1961;264:1339–42. [DOI] [PubMed] [Google Scholar]
- 57.Allen RH, Stabler SP, Savage DG, Lindenbaum J. Diagnosis of cobalamin deficiency I: Usefulness of serum methylmalonic acid and total homocysteine concentrations. Am J Hematol 1990;34(2): 90–8. [DOI] [PubMed] [Google Scholar]
- 58.Yang Q, Cogswell ME, Hamner HC, Carriquiry A, Bailey LB, Pfeiffer CM, Berry RJ. Folic acid source, usual intake, and folate and vitamin B-12 status in US adults: National Health and Nutrition Examination Survey (NHANES) 2003–2006. Am J Clin Nutr 2010;91(1): 64–72. [DOI] [PubMed] [Google Scholar]
- 59.Mills JL, Von Kohorn I, Conley MR, Zeller JA, Cox C, Williamson RE, Dufour DR. Low vitamin B-12 concentrations in patients without anemia: The effect of folic acid fortification of grain. Am J Clin Nutr 2003;77(6):1474–7. [DOI] [PubMed] [Google Scholar]
- 60.Qi YP, Do AN, Hamner HC, Pfeiffer CM, Berry RJ. The prevalence of low serum vitamin B-12 status in the absence of anemia or macrocytosis did not increase among older U.S. adults after mandatory folic acid fortification. J Nutr 2014;144(2):170–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Allen LH, Rosenberg IH, Oakley GP, Omenn GS. Considering the case for vitamin B12 fortification of flour. Food Nutr Bull 2010;31(1 Suppl):S36–46. [DOI] [PubMed] [Google Scholar]
- 62.Brouwer I, Verhoef P. Folic acid fortification: Is masking of vitamin B-12 deficiency what we should really worry about? Am J Clin Nutr 2007;86(4):897–8. [DOI] [PubMed] [Google Scholar]
- 63.Morris MS, Jacques PF, Rosenberg IH, Selhub J. Folate and vitamin B-12 status in relation to anemia, macrocytosis, and cognitive impairment in older Americans in the age of folic acid fortification. Am J Clin Nutr 2007;85(1):193–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Savage DG, Lindenbaum J. Neurological complications of acquired cobalamin deficiency: Clinical aspects. Baillieres Clin Haematol 1995;8:657–78. [DOI] [PubMed] [Google Scholar]
- 65.Stabler SP, Allen RH, Savage DG, Lindenbaum J. Clinical spectrum and diagnosis of cobalamin deficiency. Blood 1990;76(5):871–81. [PubMed] [Google Scholar]
- 66.Healton EB, Savage DG, Brust JC, Garrett TJ, Lindenbaum J. Neurologic aspects of cobalamin deficiency. Medicine 1991;70(4):229–45. [DOI] [PubMed] [Google Scholar]
- 67.Lindenbaum J, Healton EB, Savage DG, Brust JCM, Garrett TJ, Podell ER, Marcell PD, Stabler SP, Allen RH. Neuropsychiatric disorders caused by cobalamin deficiency in the absence of anemia or macrocytosis. N Engl J Med 1988;318(26):1720–8. [DOI] [PubMed] [Google Scholar]
- 68.Russell JSR, Batten FE, Collier J. Subacute combined degeneration of the spinal cord. Brain 1900;23(1):39–110. [Google Scholar]
- 69.Mills JL, Molloy AM, Reynolds EH. Do the benefits of folic acid fortification outweigh the risk of masking vitamin B12 deficiency? BMJ 2018;360:k724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Oxman AD. Grading quality of evidence and strength of recommendations. BMJ 2004;328(7454):1490–4. [DOI] [PMC free article] [PubMed] [Google Scholar]