Abstract
A 55-year-old man was admitted to the trauma center after a car accident. Cardiac tamponade, traumatic aortic injury, and hemoperitoneum were diagnosed by ultrasonography. The trauma surgeon, cardiac surgeon, and interventional radiologist discussed the prioritization of interventions. Multi-detector computed tomography was carried out first to determine the severity and extent of the injuries, followed by exploratory sternotomy to repair a left auricle rupture. A damage control laparotomy was then performed to control mesenteric bleeding. Lastly, a descending thoracic aorta injury was treated by endovascular stenting. These procedures were performed in the hybrid-angio room. The patient was discharged on postoperative day 135, without complications.
Keywords: Trauma, Hybrid operation, Endovascular procedure, stent, Resuscitation, Shock
Case report
A 55-year-old man was admitted to the emergency room of our level I trauma center, suffering from severe chest and abdominal pain as a result of a car traffic accident, during which he had worn a seat belt. His initial vital signs were stable. His blood pressure was 120/70 mm Hg, and he had a heart rate of 82 beats per minute and a respiration rate of 20 breaths per minute. He scored 15 on the Glasgow Coma Scale.
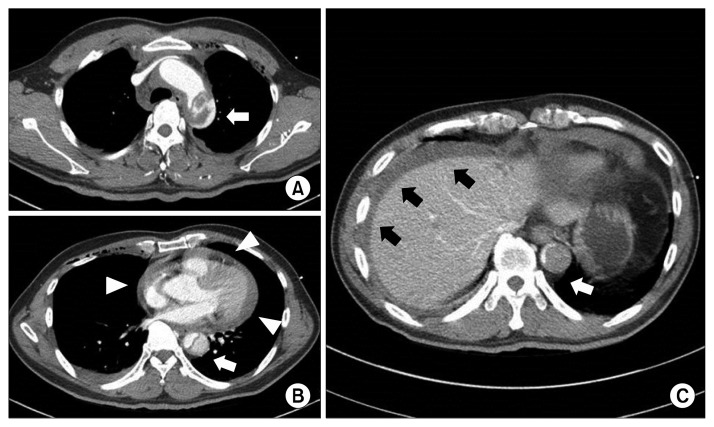
At the primary examination, focused assessment by sonography for trauma (FAST) was performed and revealed fluid collection in the pericardial, pleural, perihepatic, and peripelvic spaces. In addition, a descending thoracic aortic injury was strongly suspected. In order to confirm the injury and perform the necessary surgical intervention, we moved the patient to the hybrid-angio room, where surgery, angiography, and multi-detector computed tomography (MDCT, Aquilion ONE; Toshiba Medical System Corp., Otawara, Japan) could all be performed. MDCT demonstrated multiple hemorrhagic lesions, including hemopericardium, with suspicion of cardiac rupture and rupture of the proximal descending thoracic aorta, combined with a dissection, sternal fracture, and suspicion of a mesenteric injury (Fig. 1). The Estimated Injury Severity Score, Revised Trauma Score, and probability of survival were 26, 7.841 and 87.8%, respectively.
Fig. 1.
(A) Chest CT shows a traumatic aortic injury of the proximal descending thoracic aorta (white arrow). (B) Hemopericardium (white arrowheads) and dissection of the descending thoracic aorta are shown on CT. (C) Abdominal CT shows hemoperitoneum (black arrows) and dissection of the abdominal aorta (white arrow). CT, computed tomography.
The traumatologist, cardiac surgeon, general surgeon, and interventionist were assembled, and they discussed the serial order of treatment for the patient. The patient’s vital signs gradually began worsening. An exploratory sternotomy was first carried out, with the option of cardiopulmonary bypass on standby. A copiously bleeding injury to the left atrial auricle (LA) was found. The rupture site was easily clamped without the need for bypass and repaired with simple over-sewing. The patient’s vital signs then stabilized and an exploratory laparotomy was commenced. This revealed injuries of the mesenteric arteries, which were corrected, as well as a partial tear of the duodenum, which was also repaired. Lastly, endovascular treatment via both femoral arteries was employed to correct traumatic dissection of the descending thoracic aorta. An 8F sheath was introduced via the left superficial femoral artery and a stent graft was inserted through it. Thoracic endovascular aortic repair (TEVAR) with a 36×32×180 mm SEAL thoracic stent graft (S&G Biotech, Seongnam, Korea) was successfully performed at zone II, with intentional coverage of the left subclavian artery (LSCA). We planned embolization of the LSCA orifice and a debranching procedure from the left carotid artery to the LSCA, but decided to postpone it until possible complications such as type II endoleak, arm ischemia, pain, or neurological symptoms occurred. Fortunately, no endoleak occurred during the postoperative period, the collateral blood flow was maintained, and this procedure was not necessary. All of the crucial treatments outlined above, including the imaging diagnosis, were performed sequentially at a single location.
The treatment of this patient was quick and effective, but his postoperative course was complicated. A massive transfusion was needed due to bleeding from posttraumatic coagulopathy. A minor left middle cerebral artery infarction with hemorrhagic transformation presented in the form of a seizure on postoperative day 2. Infarction caused by an air embolism was suspected. His mental status was initially drowsy, but he soon recovered fully, with no neurological deficit. The patient developed pneumonia caused by Klebsiella pneumoniae, and a tracheostomy was carried out on postoperative day 7. Further problems with infection included sacral sores and bacteremia with Serratia marcescens.
The patient was transferred to the general ward after 67 days in the intensive care unit. After a long period of rehabilitation, he was discharged on postoperative day 135 without any problems. Follow-up MDCT at discharge (Fig. 2) detected no endoleak at the site of the vascular stent/graft, and the remnant dissection of the descending and abdominal aorta was stable.
Fig. 2.
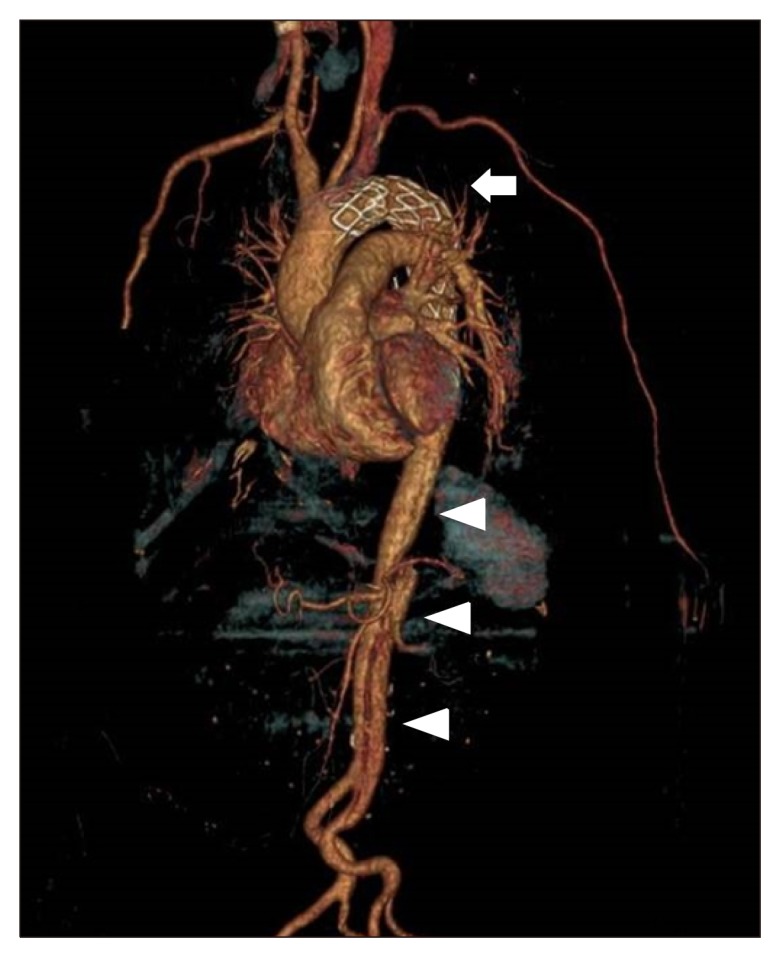
Three-dimensional computed tomography of the aorta shows successful zone II thoracic endovascular aortic repair without endoleak (white arrow) and with remaining, but stable, dissection of the descending thoracic and abdominal aorta (white arrowheads).
The patient provided written informed consent for the publication of clinical details and images.
Discussion
Multiple traumas involving various organs could easily be lethal due to the complexity of the injuries involved. The key steps of treatment in such cases are as follows: (1) vital sign stabilization, (2) early detection of the injured site, and (3) serial treatment including surgery, as well as endovascular treatment using a multidisciplinary approach [1]. Most importantly, these interventions should proceed sequentially, without delay, during the golden hour of survival. We believe that the hybrid-angio room in our trauma center enables us to achieve this goal effectively.
In our case, the patient had severe injuries to the chest and abdomen at the same time. In the field of trauma surgery, it is crucial to prioritize treatment when managing severely injured patients with multiple traumas [1,2]. The concept of damage control surgery is well established for hemodynamically unstable abdominal trauma patients. This is the step-by-step correction of damage over time, to restore the systemic condition of the patient. The first surgery is to eliminate serious bleeding. The abdomen is then kept open in order to perform secondary surgery [3]. However, cardiac or aortic injuries caused by chest trauma have special characteristics. Cardiac rupture commonly occurs due to blunt chest trauma from a traffic accident, and the most common site is the right atrial auricle. Most cases can be simply repaired via sternotomy, but rapid hemodynamic deterioration means that most patients die before surgical repair can be completed [4]. Once cardiac arrest happens, conventional cardiopulmonary resuscitation is not effective because of tamponade.
Previously, our center reported the management of cardiac tamponade in cases of severe chest trauma using extracorporeal membrane oxygenation (ECMO), enabling a secure transfer of the patient to the operating theater and saving time for surgery preparation [5]. In our experience, immediate surgical exploration with ECMO on standby in case of sudden cardiac arrest is essential for saving lives. While a high suspicion of cardiac tamponade is inevitable based on the mechanism of trauma, the extent and severity of the cardiac injury should be precisely identified using FAST and MDCT.
Endovascular repair is the standard treatment for traumatic aortic injuries [6]. We carry out endovascular repair together with surgical repair. In the case of severely injured patients (with an Injury Severity Score above 20), who have a high risk of bleeding from brain or internal organ injuries or require concomitant damage control surgery, we prefer to carry out the endovascular repair as soon as possible, according to the level of priority. In this case, our patient underwent TEVAR after an urgent surgical exploration. No complications related to the endovascular procedure occurred, and the patient recovered well from a seizure due to cerebral infarction. There was no change in near-infrared spectroscopy monitoring during the surgery, but intra-cardiac air from the LA may have flowed into the cerebral circulation during the repair of the ruptured LA. Fortunately, cerebral infarction did not affect the patient’s postoperative course, and the long hospital stay was due to infectious complications, such as pneumonia as bacteremia, and post-traumatic rehabilitation.
Having a hybrid operating room combined with MDCT enables us to save time between making the diagnosis and carrying out treatment. It also reduces the risk of moving patients with unstable pelvic or spinal fractures from one room to another, and the time delays associated with this process. The facility is useful for trauma centers to deal with severely injured patients with multiple trauma.
In conclusion, a hybrid approach by a multi-disciplinary team, with diagnosis and treatment using endovascular as well as surgical methods, is a good option for saving time in the management of patients with severe multiple traumas and improving their outcomes.
Footnotes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Bunya N, Harada K, Kuroda Y, et al. The effectiveness of hybrid treatment for sever multiple trauma: a case of multiple trauma for damage control laparotomy and thoracic endovascular repair. Int J Emerg Med. 2017;10:18. doi: 10.1186/s12245-017-0145-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.D’Amours SK, Rastogi P, Ball CG. Utility of simultaneous interventional radiology and operative surgery in a dedicated suite for seriously injured patients. Curr Opin Crit Care. 2013;19:587–93. doi: 10.1097/MCC.0000000000000031. [DOI] [PubMed] [Google Scholar]
- 3.Ball CG. Damage control resuscitation: history, theory and technique. Can J Surg. 2014;57:55–60. doi: 10.1503/cjs.020312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yun JH, Byun JH, Kim SH, et al. Blunt traumatic cardiac rupture: single-institution experiences over 14 years. Korean J Thorac Cardiovasc Surg. 2016;49:435–42. doi: 10.5090/kjtcs.2016.49.6.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huh U, Song S, Chung SW, et al. Is extracorporeal cardiopulmonary resuscitation practical in severe chest trauma?: a systematic review in single center of developing country. J Trauma Acute Care Surg. 2017;83:903–7. doi: 10.1097/TA.0000000000001680. [DOI] [PubMed] [Google Scholar]
- 6.Agostinelli A, Carino D, Borrello B, et al. Blunt traumatic injury to the thoracic aorta treated with thoracic endovascular aortic repair: a single-centre 20-year experience. Interact Cardiovasc Thorac Surg. 2019;28:17–22. doi: 10.1093/icvts/ivy211. [DOI] [PubMed] [Google Scholar]