Abstract
Background:
Recent evidence indicates increased use of urgent care centers (UCCs) for sexually transmitted disease (STD) testing. We sought to learn more about STD services in UCCs in a large metropolitan area.
Method:
Using a modified rapid gap assessment approach, we interviewed staff from 19 UCCs in metro Atlanta, GA. The UCCs were identified using two online search engines. We focused on a 50-mile radius around Atlanta. We then excluded duplicates and closed UCCs, and the ones outside Atlanta’s five contiguous counties. Using a prioritization process, we visited UCCs in or adjacent to areas with mid to high local STD morbidity, or facilities from which STD cases were reported the year prior. We collected checklist-based data on STD testing, treatment, and preventive services, as well as supportive services (eg, substance use/mental health referrals). Checklist data, notes, and open-ended questions were summarized and analyzed descriptively.
Results:
All UCCs (n = 19) reported offering basic to comprehensive STD testing. Although most could treat on-site for chlamydia and gonorrhea, most relied on referrals, or prescriptions and “return to facility” practices to treat syphilis. Sources for STD information/management included the health department/Centers for Disease Control and Prevention, online medical sites, and electronic medical record embedded information. Challenges UCCs acknowledged included staying up-to-date with treatment guidance and laboratory reporting requirements, inadequate time for sexual risk reduction counseling, and linking patients with extended care needs (eg, HIV+ case management, supportive services), or following up with patients.
Conclusions:
Urgent cares are STD testing resources. Service availability varies, but opportunities exist to enhance STD services in UCC settings and in communities.
Over 2.2 million cases of chlamydia (CT), gonorrhea (GC), and primary and secondary (P&S) syphilis cases were reported in the United States in 2017.1 Family planning providers and sexually transmitted disease (STD) clinics continue to be a resource for patients seeking STD services, even with declines in cases identified.2–4 Settings, such as urgent care centers (UCCs), have seen an increase in STD-related visits in recent years, at a time when STD clinics are closing.5,6 Defining characteristics of a UCC include: capacity to address non–life-threatening illnesses and injuries, provide on-site Clinical Laboratory Improvement Amendments-waived laboratory testing, licensed physicians on staff, and walk-in service provision with extended hours and days.7,8
Unlike safety-net providers, which reach underserved communities, UCCs often operate in areas with higher income levels and health insurance rates.9 An analysis of 2010 to 2014 medical claims data showed an increase in UCC visits for STD services among privately insured individuals.5 Nevertheless, UCCs also see patients without insurance or regular providers, or with lower incomes; with reasons for use including availability of timely care and convenience.10 In a 2013 survey of patients attending 21 US STD clinics, 24.4% of males and 25.8% of females responded they would have gone to the UCC or emergency room for care if the local STD clinic were unavailable.11 Results from a 2014 to 2015 survey of colleges/universities showed institutions referred approximately 30% of their students to UCCs for STD care.12
Little is known about the range of STD services offered in UCCs. In collaboration with the Georgia Department of Public Health’s (GA-DPH), State Office of STDs, we conducted an exploratory, yet seminal assessment of STD services in UCCs in a metropolitan area. Specifically, we sought to learn more about STD testing and treatment availability, preventive services and resources offered to STD patients, and challenges associated with providing STD services in UCC settings.
MATERIALS AND METHODS
Sample
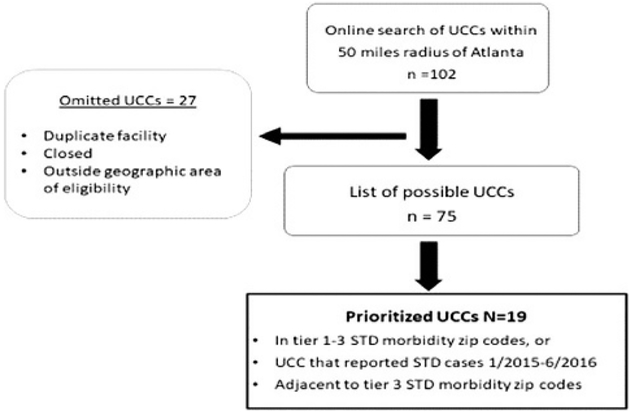
We used purposive sampling to develop a list of prioritized UCCs (Fig. 1). We reviewed January 2015 to June 2016 STD morbidity data by zip code for the Atlanta metropolitan area. We generated a list of 102 self-identified UCCs within a 50-mile radius of downtown Atlanta using online search engines from an urgent care organization.13 We excluded duplicate UCCs, ones permanently closed, or located outside Atlanta’s contiguous counties (eg, Cobb, Fulton, Dekalb, Gwinnett, Clayton). We then matched these 75 UCCs to STD morbidity by zip code (5 tiers) using GA-DPH data and selected UCCs in higher morbidity areas (tiers 1–3). We cross-walked this list with: (1) UCCs located in/or adjacent to tier 1 to 3 zip codes, and (2) facilities reporting STD cases to GA-DPH under the category Urgent Care/Emergency room. The final sample was 19 UCCs: 16 prioritized UCCs in tier 1–3 areas and 3 UCCs adjacent to tier 3.
Figure 1.
Sampling frame of UCCs included in assessment.
Notes: UCCs = Urgent Care Centers. The Georgia Department of Public Health divides morbidity by zip code into five tiers (tier 1 = highest; tier 5 = lowest). Sixteen UCCs were located in tiers 1–3; 3 UCCs were adjacent to tier 3 zip codes.
Procedure
We used a team-based, modified rapid assessment14 approach for this activity. An interviewer and note taker team travelled to each prioritized UCC location to speak with staff familiar with the facilities’ STD services. Before the interviews, the knowledge-building intent of the assessment was described. Verbal consent was obtained; respondents had opportunities to ask or not answer questions. Interviews took 30 to 45 minutes. The team recorded notes by hand or laptop only (no audio), close to verbatim. After completion, the team offered respondents information packets containing GA-DPH notifiable disease posters,15 GA-DPH STD 2009 to 2013 data summaries,16 and Centers for Disease Control and Prevention (CDC) STD treatment guidelines resources.17 The National Center for HIV/AIDS, viral hepatitis, STD, and TB prevention at CDC provided an ethics review and determined the project to be nonresearch.
Data Collection and Analysis
We adapted the STD Preventive Services Gap Assessment Tool18 by modifying the services checklist for UCCs and adding seven open-ended questions. The services checklist included questions about availability of on-site typical STD testing, extragenital site testing and treatment; as well as prescriptions or referrals for GC/CT, P&S, genital herpes simplex virus 2 (HSV2), Trichomonas vaginalis (Trich), and bacterial vaginosis (BV), HIV, and hepatitis B virus (HBV) and hepatitis C virus (HCV). We asked about on-site and outside laboratory specimen processing, and about the STD laboratory reporting procedure. For patients testing STD positive, we asked UCCs if they provided prevention information, behavioral counseling, and linkage-to-care referrals, as well as if they did patient or partner follow-up, or engaged with the state and/or local health department (HD). We asked about on-site provision of, or referrals to, support services (eg, substance use/mental health SU/MH), and asked open-ended questions to elicit more in-depth information related to the checklist.
After each interview, note takers reviewed completed checklists/notes for completeness. Interviewers reviewed for concurrence. We descriptively analyzed and summarized checklist data in Microsoft (MS) Excel. Checklist notes and responses were transcribed in MS Word, organized by question, and then categorized by response options, content theme or similarities. Emergent data were descriptively analyzed, and associated with available quotes. Open-ended questions were transcribed and imported into QSR NVIVO 10. Transcripts were reviewed for initial trends. Structural codes were developed and used to code and analyze open-ended questions’ content. In-depth analyses of the checklist data, notes, and open-ended questions guided the identification and presentation of overall findings.
RESULTS
Sample Characteristics (n = 19)
All UCCs accepted walk-in patients and had weekday hours. Most UCCs had weekend (n = 17) and evening hours (n = 16). All 19 UCCs accepted private insurance and self-pay; 11 accepted Medicaid and 15 Medicare. Four UCCs had a sliding payment scale arrangement. All 19 UCCs had at least one physician on-site during operating hours. Most UCCs had medical assistants (n = 16) and administrative staff (n = 14). Other on-site staff included physician assistants (n = 6), nurse practitioners (n = 5), and registered (n = 1), or licensed practical nurses (n = 3). Also mentioned, were X-ray and laboratory technicians.
Testing for STDs
Testing for CT/GC/P&S was available at all 19 facilities (see table 1). All 19 UCCs provided STD testing per patient request, with most reporting the use of bundled tests referred to as “STD panels.” Respondents referred to panels offered as “simple,” “complete” or “comprehensive,” depending on the number of panel tests (1 to 10). An STD panel typically included testing for Chlamydia trachomatis, Neisseria gonorrhoeae (CT/GC), syphilis and HIV, with more “complete” or “comprehensive” panels also including tests for HSV2, HBV, and HCV.
TABLE 1.
STD Services at Sampled UCCs in 5 Metro Atlanta Counties
| STDs | On-Site Services* | Off-Site Offerings | |||
|---|---|---|---|---|---|
| Testing | Treatment | Extra Genital Examinations | Prescriptions† | Referrals | |
| N | n (%) | n (%) | n (%) | n (%) | |
| Syphilis | 19 | 7 (36.8) | NA | 6 (31.6) | 11 (57.9) |
| Gonorrhea | 19 | 18 (94.7) | 11 (57.9) | 7 (36.8) | 1 (5.2) |
| Chlamydia | 19 | 9 (47.4) | 11 (57.9) | 17 (89.5) | 2 (10.5) |
| Herpes | 19 | 2 (10.5) | NA | 17 (89.5) | 4 (21.1) |
| Hepatitis B | 19 | 1 (5.2) | NA | 2 (10.5) | 16 (84.2) |
| Hepatitis C | 18 | 0 | NA | 1 (5.6) | 16 (84.2) |
| Bacterial Vaginosis | 18 | 3 (16.7) | NA | 14 (77.8) | 2 (10.5) |
| Trichomoniasis | 19 | 4 (21.1) | NA | 18 (94.7) | 1 (5.2) |
N = 19 urgent care centers. Rows nor columns equal 100%.
Includes those services done during initial and follow-up visits to complete treatment.
Numbers in Prescription column may overlap with “on-site” treatment column.
NA, not applicable. Respondents indicated syphilis, HSV, HBV, and HCV were conducted as part of STD panels via blood samples.
Although all 19 UCCs reported offering HSV2 testing, three providers commented that they did not recommend HSV2 testing. One provided it only at the patient’s request. As one provider stated, “It opens Pandora’s Box, and it is not helpful.” Another provider expressed that the counseling message for patients with HSV2 was complicated, given that the test does not distinguish recent from old infection.
For patients with limited insurance coverage for STD testing (or self-paying), prices for STD panel tests ranged between US $100 and US $500, exclusive of visit fees. A few (n = 3) UCCs offered a flat rate of US $100 to US $150 for STD panel testing. As one respondent mentioned, “It’s [sometimes] cheaper to pay out of pocket—we are pretty competitive with our self-pay rate. Between copay and laboratory, rates could cost more with insurance.” For patients who found STD testing cost-prohibitive, UCCs often referred them to the local HD’s STD clinic.
Most (n = 11) UCCs said they could perform extragenital testing for CT/GC, if needed. However, providers indicated extragenital testing was rarely performed, and that it was usually triggered by a patient’s concern or a symptom. Nearly all respondents reported testing for Trich (n = 19) and BV (n = 18), with 10 UCCs specifying the use of a point-of-care test, on-site. All other STD specimens were sent to a laboratory. Facilities mentioned sending most STD specimens to one of four commercial laboratory companies.
When asked to recall requests for STD testing in the 3 months before interview. All 19 UCC respondents indicated they had encountered requests for STD testing. Fifteen respondents recalled patients testing positive for CT; and 14 recalled patients testing positive for GC, including what 2 providers referred to as “resistant gonorrhea.”a Nine respondents recalled patients testing positive for P&S, and 4 had patients test positive for HIV. Overall, recall of testing varied, with a couple UCCs recalling periodic requests, but few, if any positive results in the timeframe. However, other UCCs recalled almost daily STD testing requests with positive results seen “several times a week.”
UCCs’ STD (CT/GC/P&S) Treatment and Options
All 19 UCCs tested for GC/CT/P&S (table 1). On-site treatment availability at almost all UCCs (n = 18) was limited to GC, though appropriateness varied. Of the 18 UCCs offering GC treatment, eight reported providing only ceftriaxone, as opposed to the recommended dual therapy (ceftriaxone IM + azithromycin). One facility specifically indicated treating patients using dual therapy.17 Seven facilities also reported providing prescriptions of azithromycin for treating GC; however, the therapeutic purpose (sole or additive treatment) was unclear.
Of the 19 UCCs that tested for syphilis, only 1 UCC indicated treating P&S on-site (same-day) using benzathine penicillin (Bicillin).17 Six additional UCCs offered “on-site” treatments involving a return to the facility. Patients were either given a prescription to obtain the treatment (n = 5; 1 UCC had an in-house pharmacy), or the Bicillin was ordered as needed (n = 1). “We can order Bicillin and get [it] within 48 hours but do not keep on-site. Once it comes in, we can administer it. We can also send [people] to the HD.” Eleven of the UCCs referred patients suspected of, or diagnosed with syphilis to the HD for treatment. “[We] do not keep Bicillin, [we] refer to the HD.” One UCC did not respond. They may be similar to a UCC that acknowledged testing, then referring patients testing positive for an STD. “[We] refer to HD. [We] do not treat here. Do not keep Bicillin.” Reasons for prescription and referral protocols, outside of low incidence, included Bicillin’s costs, treatment administration discomforts, and syphilis complications.
Some UCCs treated BV (n = 3) and trichomoniasis (n = 4) on-site, with most providing patients with a prescription for treatment (table 1). Most (n = 17) UCCs provided prescriptions for HSV2 treatment, particularly for patients with symptoms. For HBV and HCV, the majority (n = 16) of UCCs referred patients to an infectious disease specialist, primary care provider, or to the HD.
For STD diagnosis and treatment, 11 (58%) respondents reported using the CDC STD Treatment Guidelines.17 “The CDC. I’m trusting those guys. I’m assuming their [information] is accurate.” Other treatment sources mentioned included electronic medical record (EMR)/system embedded resources, the state/local HD, and nonspecific websites.
Posttest Resources for Patients Testing STD Positive
Most UCCs (n = 15) provided STD prevention information to patients (table 2), and used other resources. One third were from HDs/CDC (n = 5), or medical information websites (n = 2), but most used information embedded in the EMR system, or incorporated into the discharge instructions (n = 8). Most UCCs (n = 10) offered some type of behavioral counseling to STD patients for risk reduction (table 2), but they also found it to be a challenge. One respondent mentioned the difficulty providers had with delivering counseling, “80% of the providers try but it’s really hard.” Six UCCs reported not conducting any counseling and referring patients to primary care providers or specific providers they knew.
TABLE 2.
UCC On-Site and Referred Services for Patients Testing Positive for an STD
| UCC Offered On-site | UCC Offered Referral | Unavailable | |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| STD Resources/Services | |||
| Offer STD prevention written guidance, brochures | 15 (78.9) | 3 (15.8) | 1 (5.2) |
| Behavioral risk reduction counseling | 10 (52.6) | 6 (32.4) | 3 (15.8) |
| Counsel to notify sex partners | 18 (94.7) | 0 | 1 (5.2) |
| Patient-delivered partner therapy was available | 1 (5.2) | 1 (5.2) | 17 (89.5) |
| Provide STD services to partners | 19 (100) | 1 (5.2) | 0 |
| HIV case management linkage/relinkage to care | 1 (5.2) | 13 (68.4) | 5 (26.3) |
| Social/supportive services* | |||
| WIC/EBT | 0 | 5 (26.3) | 14 (73.7) |
| Health insurance enrollment | 4 (21.1) | 0 | 15 (78.9) |
| Substance use and/or mental health programs | 1 (5.2) | 14 (73.7) | 4 (21.1) |
N = 19 urgent care centers.
Services may have been available to any UCC patient.
EBT, Electronic Benefits Transfer Card; SNAP, Supplemental Nutrition Assistance Program; WIC, Women, Infants and Children Nutrition Program.
Patients testing STD-positive were encouraged to have partners visit the UCC or a provider for testing. Almost all respondents (n = 18) reported informing patients to notify sex partners about the potential exposure. Although 1 respondent was unclear of the facility’s protocol, all of the UCCs were willing to provide STD services to patients’ partners. However, the partners were required to come to the office to have a fee-for-service examination. Expedited/patient-delivered partner therapy (EPT) was not available at the majority of sites (n = 17), primarily because the provider wanted to see, test and treat the patient’s sex partner. Of the two UCCs that acknowledged EPT, one indicated its provision depended on specific circumstances.
Some (n = 5) UCCs offered specific supportive services (eg, health insurance enrollment); most offered referrals (table 2). The most frequently mentioned referral was to supportive services (n = 14). Most UCCs referred patients to specific facilities, and others more actively linked patients to referral. As one provider explained, “We provide resources; [we] partner with the local hospital and county crisis team.” Some UCCs that were part of larger hospital systems referred to programs within the system. One UCC had a partnering clinical therapist in the same building. Other types of referrals were to safety-net programs, such as Women, Infants and Children, or to the Georgia Health Insurance Marketplace. One facility offered patients an alternative option in the form of a concierge health program with a monthly membership fee.
Needs and Challenges Associated With Providing STD Services in UCCs
When asked about patients’ STD clinical or preventive needs that were beyond their facility’s scope, 26% of UCCs responded they did not have specific challenges. Their approach was to refer patients to resources based on needs. Among the remaining UCCs, 68% (n = 13) indicated HIV case management was the most frequently mentioned unmet patient need. The UCCs typically referred to specialty care providers (eg, infectious disease), or the HD. As one provider stated, “We want to send patients to the most appropriate place to get proper management. It would be irresponsible to manage when we are not the most appropriate place.”
Other patient-level challenges included having inadequate time to provide behavioral counseling, difficulties following-up with patients beyond their initial visit, and delivering patient test results once labs were received after visit. Facility-related challenges included having or being familiar with STD screening and treatment protocols, and difficulties (both technology and protocol-related) for reporting STD laboratories to the HD. Collectively, these challenges represented what one respondent summarized as challenges for UCCs to provide “good” STD services to patients, especially repeat cases: “Because we are an urgent care facility, and clients often come in wanting a full workup, I do not think that is good medicine. We do not have the ability to follow the clients beyond the appointment. There is no system for follow up the way a primary provider’s office can. If there are active symptoms we can treat, and I believe that is good medicine, but primary care is much better about client follow up.”
Reporting Practices and Health Department Engagement
Laboratory reporting varied; most (n = 13) UCCs had reporting procedures. Those that did not (n = 5) indicated relying on other systems to report. One respondent was unsure. The 13 UCCs with procedures reported directly to the HD using electronic methods or faxing. The respondents without protocols were unclear about reporting requirements, or did not consistently report, as with one facility in which a part-time clinical staff person reported laboratories when they were on-site. Reasons included lack of awareness of reporting requirements, but more specifically, and most often, a reliance on the laboratory facilities to report cases. For example, one respondent mentioned that, with the advent of EMR, they were not aware that it was still a facility requirement. Incidentally, the five UCCs that did not submit laboratory reports also had previous STD cases from the facility report and area.
When asked how the STD program could assist UCCs, suggestions fell into three main categories: 1) provision of direct resources to the facility in the form of medication assistance (eg, Bicillin/ceftriaxone), condoms and lubricant samples, educational brochures and other STD-related information for patients; 2) improve visibility of HD program resources for UCC patients and staff awareness, local STD clinics locations, and hours; 3) communication and engagement between the HD and UCCs. Respondents at one UCC suggested active linkages with the HD, like a liaison to review current STD reporting requirements, guidance which other respondents also welcomed. Such engagement could assist with enhancing patient follow-up, partner services, linkages to HIV care and case management, and referrals to supportive resources, as well as overall service provision.
DISCUSSION
Sampled UCCs exhibited characteristics similar to those cited in the literature.7,8 All UCCs had the capacity to test for common STDs. The STD services were focused on relatively uncomplicated testing and treatment procedures that were managed in 1 or 2 visits. Although UCCs were in or adjacent to zip codes with STD morbidity, testing frequency was qualitatively “rare” to “several times a week,” and some respondents could not recall a positive STD test in the prior 3 months. Patient needs that were more difficult to address in the UCC context included sexual risk counseling, HIV case management, and supportive services. The UCCs interviewed want to provide a quality service that is accessible. Below, we highlight gaps and challenges in STD management with potential opportunities to address them.
Gaps and Challenges
The principal challenges related to STD management concerned providing or assuring adequate treatment. Although almost all UCCs treated patients testing positive for GC with ceftriaxone, only one specifically indicated treating patients using dual therapy.17 Moreover, seven UCCs provided prescriptions and so did not treat directly. Appropriate treatment availability was a more common issue for syphilis. All UCCs offered syphilis testing, but only seven offered treatment. The other 11 UCCs offered referrals for treatment elsewhere, mainly the HD. Consistent with prior research,19 UCCs’ challenges to syphilis treatment included buying, keeping, or storing Bicillin on-site (cost prohibitive); provider discomfort with administering Bicillin and complexity of syphilis management (possibly due to rarity in UCCs). Patients were also typically responsible for STD testing costs and were referred to the HD for services when they did not have the ability to pay.
Although referring patients to the HD (ie, unable to pay) or to a health care provider (ie, linkage-to-care) for treatment is responsible, informational-only referrals, without a warm linkage, contact, or follow-up can be insufficient or ineffective.20,21 Because we did not ascertain the precise nature of referrals, we do not know how likely patients could be successfully treated via referrals. Some UCCs indicated they had a referral list they shared with patients, but this information was more often mentioned when responding to questions about supportive services.
Consistent laboratory reporting procedures, across UCCs, was a service gap. Most UCCs reported STD positive tests to HDs. Those that did not relied on laboratories to submit reportable STD positive tests. Several UCCs acknowledged the unawareness of reporting requirements and were open to knowing more. This is an opportunity to address a gap in laboratory reporting. Incidentally, respondents, who had procedures for reporting STD positives to the HD, were familiar with reporting requirements, and often had relationships with the HDs. This highlighted the important role of HDs as STD prevention experts, and by them providing technical assistance to UCCs, also addressing STD services gaps in the community.
Prospects for Improving STD Services Involving UCCs
Although UCCs were limited in their STD management ability, several appeared to have extensive links with hospitals, the HD, and infectious disease providers, including extant referral arrangements for conditions requiring long-term management. The challenge for STD management is therefore to bridge the gap between what UCCs offer (eg, STD testing) and what patients and public health need (ie, appropriate treatment, consistent laboratory reporting), in the UCC context.
If treatment availability, based on CDC Guidelines17 for tested STDs, at all times, is infeasible; UCCs can enhance STD services by confirming their STD-related prevention information and management resources are current and accurate so STD treatment is appropriate and timely. Of the 19 UCCs, 58% use the STD Treatment Guidelines, and all were receptive to the Treatment Guidelines Mobile App.17 If alternative resources are used, then source reliability is important to ensure. Patient information developed in-house, is ideally evidenced/practiced-based that complements treatment recommendations.
Another approach to enhancing STD services in UCCs is to consider STD trainings offered by the National Network of STD Clinical Prevention Training Centers (PTCs).22 The PTCs is a group of regional centers dedicated to increasing the awareness and knowledge of health professionals in sexual and reproductive health care settings. On a facility level, UCC staff can visit PTC online for resources. On a macro level, UCC organizations may explore opportunities with regional PTCs for UCC focused STD trainings.
Another potential step to bridging the gap between what services are offered in UCCs and what is needed, is improved communication between UCCs and state or local HDs. For example, dissemination of treatment guidelines, best practices, and other resources (ie, EPT Legal/Policy Toolkit23), could enhance provision of appropriate STD treatment and basic follow-up instructions (eg, retesting and partner notification), as well as address a barrier to STD services.24 Health departments could also build on existing UCC referral protocols and willingness to engage with public health to set-up simple protocols to improve linkage. For example, patients sent to the HD for treatment could be offered expedited service, and the HD could manage further patient follow-up and confirm treatment with the UCC facility.
These potential efforts and service improvements are largely contingent on the morbidity seen in UCCs and the costs associated with collaboration. Even in a high-morbidity area, a UCC might see few infections, in which case both the HD and the UCC might be better served spending resources otherwise. That noted, UCCs are a source of medical services in many communities. Given evidence of the growing use of UCC for STD services, future assessments might address scope and scale of STD morbidity, as well as approaches to treatment challenges and continuity of care for patients seeking STD testing and care in urgent care settings.
Acknowledgments:
The authors would like to acknowledge Wendasha Hall, PhD, who participated in project discussions; Darlene Davis, who assisted in developing the services checklist; and Penny Loosier, PhD, who reviewed the manuscript.
Footnotes
Conflict of Interest and Sources of Funding: None declared.
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
It is not known whether such references match any formal definition of antimicrobial resistance.
REFERENCES
- 1.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2017. Atlanta: U.S. Department of Health and Human Services, 2018. [Google Scholar]
- 2.Brackbill RM, Sternberg MR, Fishbein M. Where do people go for treatment of sexually transmitted diseases? Fam Plann Perspect 1999; 31:10–15. [PubMed] [Google Scholar]
- 3.Pathela P, Klingler EJ, Guerry SL, et al. Sexually transmitted infection clinics as safety net providers: Exploring the role of categorical sexually transmitted infection clinics in an era of health care reform. Sex Transm Dis 2015; 42:286–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Owusu-Edusei K, Sayegh BJ, Harvey AJ, et al. Declining trends in the proportion of non-viral sexually transmissible infections reported by STD clinics in the US, 2000–10. Sex Health 2014; 11:340–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pearson WS, Tao G, Kroeger K, et al. Increase in urgent care center visits for sexually transmitted infections, United States, 2010–2014. Emerg Infect Dis 2017; 23:367–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schechter SB, Romo DL, Cohall AT, et al. Approach to human immunodeficiency virus/sexually transmitted infection testing for men at an urban urgent care center. Sex Transm Dis 2017; 44:255–259. [DOI] [PubMed] [Google Scholar]
- 7.Weinick RM, Bristol SJ, DesRoches CM. Urgent care centers in the U.S.: Findings from a national survey. BMC Health Serv Res 2009; 9:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McNeely S. Urgent care center: An overview. Am J Clin Med 2012; 9: 80–81. [Google Scholar]
- 9.Le ST, Hsia RY. Community characteristics associated with where urgent care centers are located: A cross-sectional analysis. BMJ Open 2016; 6:e010663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scott DR, Batal HA, Majeres S, et al. Access and care issues in urban urgent care clinic patients. BMC Health Serv Res 2009; 9:222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoover KW, Parsell BW, Leichliter JS, et al. Continuing need for sexually transmitted disease clinics after the affordable care act. Am J Public Health 2015; 105(Suppl 5):S690–S695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Habel MA, Coor A, Beltran O, et al. The State of Sexual Health Services at U.S. Colleges and Universities. J Am Coll Health 2018; 66:259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Urgent Care Association of America. Find A Center—Urgent Care Association (UCA). Available at: https://www.ucaoa.org/page/centersearch. Accessed June 17, 2019.
- 14.Beebe J. Rapid Assessment Process: An Introduction. Walnut Creek, CA: Alta Mira Press, 2001. [Google Scholar]
- 15.Georgia Department of Public Health. Notifiable Disease/Condition Reporting. Available at: https://dph.georgia.gov/sites/dph.georgia.gov/files/Immunizations/Georgia.DPH.Notifiable.Disease.Poster.FINAL.PRESS.pdf. Accessed January 2017; November 30, 2018 and June 17, 2019.
- 16.Georgia Department of Public Health. STD Data Summary—2009–2013. Available at: https://dph.georgia.gov/sites/dph.georgia.gov/files/MCH/STD/data_summary_2009_2013.pdf. Accessed June 17, 2019.
- 17.CDC 2015. STD Treatment Guidelines. Available at: https://www.cdc.gov/std/tg2015/default.htm. Accessed June 17, 2019.
- 18.Hogben M, Kroeger K, Alexander-Pender C, et al. Sexually Transmitted Diseases (STD) Preventive Services Gap Assessment Toolkit. Atlanta, GA: Centers for Disease Control and Prevention, 2016. Available at: https://www.cdc.gov/std/program/gap/default.htm. Accessed June 17, 2019. [Google Scholar]
- 19.Kroeger KA, Sangaramoorthy T, Loosier PS, et al. Pathways to congenital syphilis prevention: A rapid qualitative assessment of barriers, and the public health response, in Caddo Parish, Louisiana. Sex Transm Dis 2018; 45:442–446. [DOI] [PubMed] [Google Scholar]
- 20.Akbari A, Mayhew A, Al-Alawi MA, et al. Interventions to improve outpatient referrals from primary care to secondary care. Cochrane Database Syst Rev 2008; CD005471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carter MW, Wu H, Cohen S, et al. Linkage and referral to HIV and other medical and social services: A focused literature review for sexually transmitted disease prevention and control programs. Sex Transm Dis 2016; 43(2 Suppl 1):S76–S82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. The National Network of STD Clinical Prevention Training Centers. Available at: https://nnptc.org/about. Accessed June 17, 2019.
- 23.Centers for Disease Control and Prevention. Legal Status of Expedited Partner Therapy (EPT). Available at: https://www.cdc.gov/std/ept/legal/default.htm#a4. Accessed June 6, 2019.
- 24.Jamison CD, Chang T, Mmeje O. Expedited partner therapy: combating record high sexually transmitted infection rates. Am J Public Health 2018; 108:1325–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]