Background:
The United States Preventive Services Task Force (USPSTF) recommends annual low-dose computed tomography (CT) lung-cancer screening for persons aged 55–80 years, who currently smoke or quit within the past 15 years, and who have accumulated at least 30 pack-years of cigarette smoking (1). The number of U.S. persons meeting USPSTF-criteria for CT screening sharply decreased from 2010 to 2015 (2). However, the USPSTF criteria may miss smokers at high risk of lung-cancer who would have been selected for CT screening by individual risk calculators that more specifically account for demographic, clinical, and smoking characteristics (3).
Objective:
We compared USPSTF eligibility criteria to individualized risk-based eligibility and estimated the effect of eligibility on screen-preventable lung-cancer deaths since 2005.
Methods and Findings:
We used data from 5,460, 5,155, and 6,971 ever-smokers in the nationally-representative National Health Interview Survey (NHIS) (4) in the years 2005, 2010, and 2015, respectively, aged 50–80 years who had no self-reported lung-cancers (2). Individual 5-year risks of lung-cancer incidence and death were estimated using the previously validated Lung Cancer Risk Assessment Tool (LCRAT) and the Lung Cancer Death Risk Assessment Tool (LCDRAT) (3;5). We estimated the number of U.S. smokers, aged 50–80 years, screen-eligible by USPSTF criteria or by exceeding 1.5%, 2%, and 2.5% in individual 5-year risks of lung-cancer incidence using LCRAT (3;5). Using the difference in LCDRAT-estimated individual risks of lung-cancer death in the absence and presence of screening (5), we estimate the number of screen-preventable lung-cancer deaths within each eligibility criteria and in the U.S. population of ever-smokers, aged 50–80 years (3). Lastly, we estimate the number of U.S. smokers in USPSTF screen eligible and ineligible subgroups. Statistical analysis was conducted in the R version 3.4.1 survey package (6).
The number of screen-eligible ever-smokers, by any eligibility criteria, grew from 2005–2010, but declined from 2010–2015. Particularly, the number of USPSTF-eligible was 8.7 million (24.6% of aged 50–80 ever-smokers) in 2005, grew to 9.5 million (22.8%) in 2010, but then declined substantially to 8.0 million (18.4%) in 2015, a decline of 1.5 million ever-smokers (Figure 1a). However, the declines in screen-eligibility over 2010–2015 were much more modest for risk-based criteria. For example, the number of U.S. smokers exceeding a 2.0% 5-year lung-cancer risk-threshold from 2010–2015 declined by only 0.8 million (9.4 to 8.6 million), half the decline based on USPSTF criteria (p=0.048). Similarly, the declines in screening-eligibility over 2010–2015 based on 1.5% and 2.5% 5-year lung cancer risk-thresholds were only 0.7 and 0.8 million, respectively.
Figure 1:
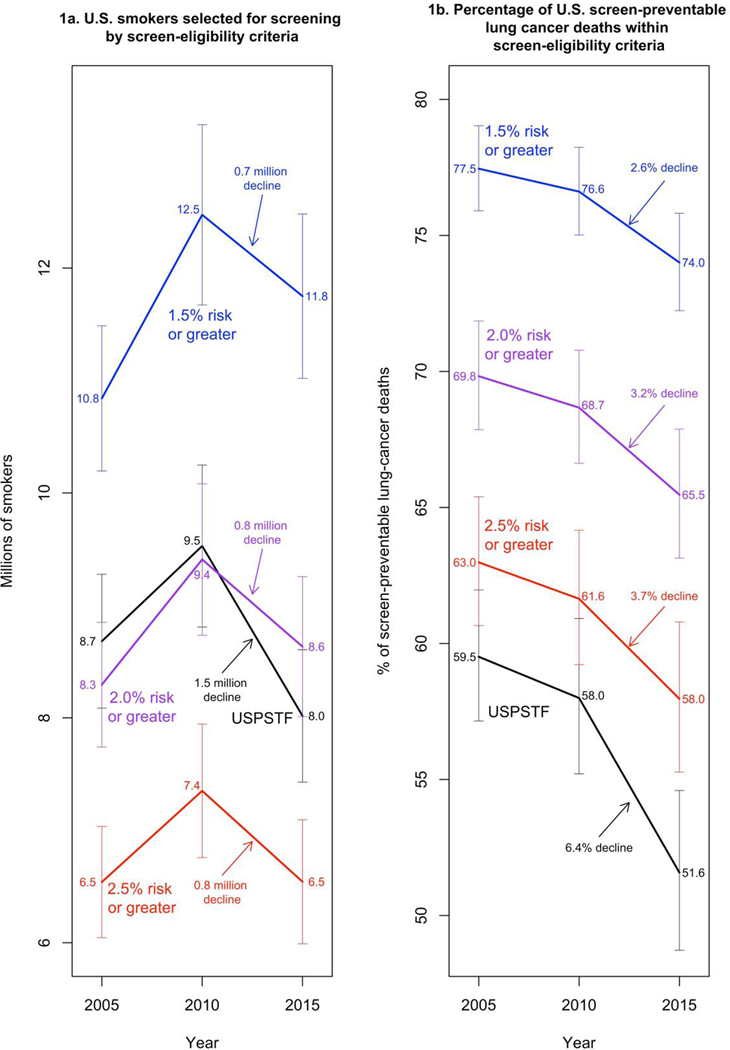
Estimated number of ever-smokers eligible for screening and percentage of all U.S. screen-preventable lung-cancer deaths averted by USPSTF and risk-based screen-eligibility criteria from 2005 to 2015
1a) Number of U.S. ever smokers, aged 50–80, in the years 2005, 2010, and 2015 who would have been eligible for screening with low-dose computed tomography by the United States Preventive Services Task Force (USPSTF) criteria and by 5-year lung-cancer risk-thresholds of 1.5%, 2%, and 2.5%.
2b) Percentage of screen-preventable lung cancer deaths among U.S. ever-smokers, aged 50–80, averted by United States Preventive Services Task Force (USPSTF) criteria or by 5-year lung-cancer risk-thresholds of 1.5%, 2%, and 2.5% in the years 2005, 2010, and 2015.
For each NHIS survey year, we used 5 multiple imputation datasets to account for missing information on race, education, BMI, quit years, cigarettes smoked per day, years smoked, emphysema and family history of lung cancer (3). The following number of respondents were missing data for these items and are shown in parentheses: race (50/92/128), education (29/17/27), BMI (151/127/202), quit years (33/12/25), cigarettes smoked per day (252/366/512), years smoked (28/9/20), emphysema (5/9/13), and family history of lung cancer (146/102/846) for years 2005, 2010, and 2015, respectively.
Horizontal lines indicate 95% confidence intervals.
Likewise, the percentage of U.S. screen-preventable lung-cancer deaths within each eligibility criteria, declined from 2005–2015 (Figure 1b). From 2010–2015, the USPSTF criteria had a percentage decline of 6.4% (8,122 fewer deaths averted). However, the percentage declines were much more modest for risk-based criteria: 2.6%, 3.2%, and 3.7%, based on exceeding 1.5%, 2%, and 2.5% 5-year lung cancer risk-thresholds, respectively (approximately 6,000 fewer deaths averted for each, p<0.001 compared to USPSTF criteria, for all). Using a 2.5% 5-year lung cancer risk-threshold instead of USPSTF criteria in 2005 would have prevented 2,617 more lung-cancer deaths (percentage increase of 3.5%) over 5 years (p<0.001), but in 2015, the difference in prevented deaths grew to 5,115 (6.4%) (p<0.001).
From 2010–2015, the 1.5 million decline in the number of U.S. ever-smokers screen-eligible by USPSTF criteria is offset by a 1.3 million increase in the number of U.S. ever-smokers with 20–29 pack-years who otherwise meet USPSTF criteria (Figure 2). These smokers may have sufficiently high individual risk of lung-cancer (7) to be screen-eligible under risk-based criteria.
Figure 2:
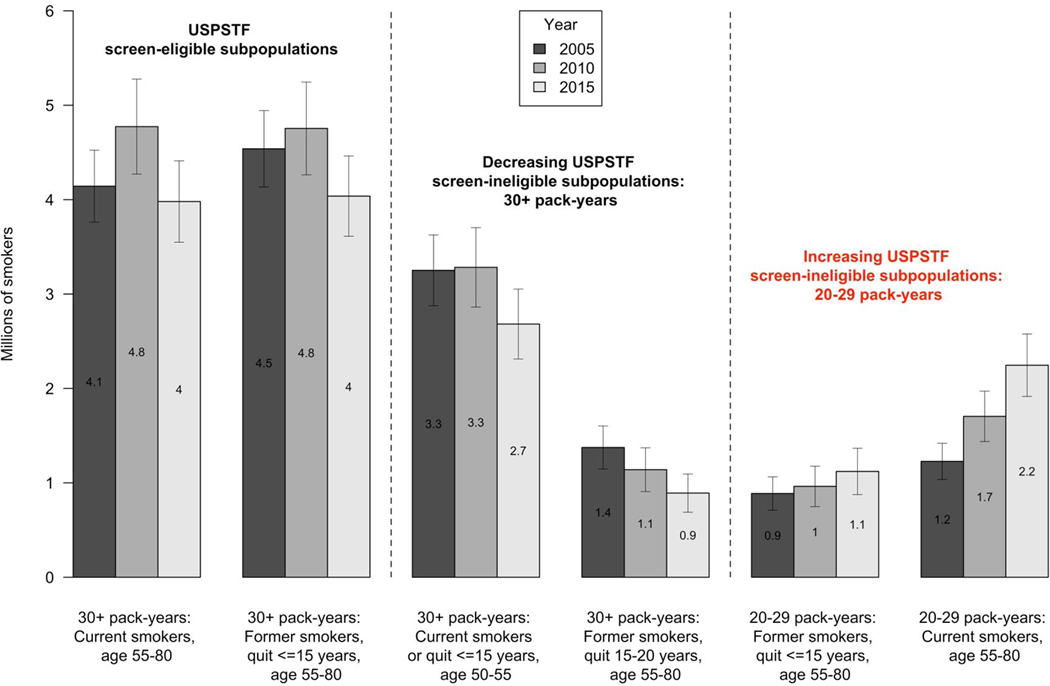
Number of U.S. ever smokers in USPSTF screen eligible and ineligible subgroups from 2005–2015
USPSTF = U.S. Preventive Services Task Force
Horizontal lines indicate 95% confidence intervals
Median and interquartile range (IQR) of 5-year individual lung-cancer incidence and death risks, in the absence of CT screening, for smoking subgroups in 2015 are as followed:
30+ pack-years: Current smokers, age 55–80: 3.6% (2.2–6.4%) incidence / 2.2% (1.3–4.1%) death
30+ pack-years: Former smokers, age 55–80: 2.0% (1.2–3.4%) incidence / 1.2% (0.7–2.3%) death
30+ pack-years: Current smokers or quit<=15 years, age 50–55: 1.0% (0.7–1.4%) incidence / 0.4% (0.3–0.7%) death
30+ pack-years: Former smokers, quit 15–20 years, age 55–80: 1.4% (1.0–2.6%) incidence / 1.0% (0.6–1.9%) death
20–29 pack-years: Former smokers, quit <=15 years, age 55–80: 1.0% (0.4–1.5%) incidence / 0.5% (0.2–0.9%) death
20–29 pack-years: Current smokers, age 55–80: 1.8% (1.1–3.0%) incidence / 1.0% (0.6–1.7%) death
Medians risks within subgroups in 2005 and 2010 are all within 0.2% of the 2015 estimates.
Discussion:
Although the number of U.S. ever-smokers eligible for lung-cancer screening according to USPSTF criteria declined by 1.5 million from 2010–2015, the number of screen-eligible ever-smokers based on exceeding risk-threshold criteria declined by only half as much. Because of U.S. population changes in relation to smoking from 2010–2015, the USPSTF criteria leads to fewer ever-smokers eligible for CT screening and fewer lung cancer deaths averted by screening. Individual risk-based criteria would screen high-risk smokers currently screen-ineligible using USPSTF criteria, resulting in more modest declines in the numbers screened and deaths averted. To better capture high-risk smokers and prevent premature deaths from lung-cancer, eligibility for lung-cancer screening should be based on exceeding a cost-effective risk-threshold that balances CT-screening benefits and harms, using a lung-cancer risk tool validated in the U.S. population. The gap in screening effectiveness between risk-based and USPSTF screening criteria may continue to increase in the future.
Acknowledgements:
This research was supported by the Intramural Research Program of the NIH/National Cancer Institute.
Funding/Support: This study was supported by the Intramural Research Program of the US National Institutes of Health/National Cancer Institute.
Role of the sponsor: The NIH had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
Footnotes
Conflicts of Interest: Dr. Christine Berg receives consulting fees from Medial ES, LLC, a company that is developing algorithms from routine blood tests that may indicate an increased risk of malignancy. Dr. Christine Berg has also received consulting fees from GRAIL, a company that is planning a clinical trial to evaluate their early stage cancer detection products. All other authors have no conflict of interests.
References:
- 1.Moyer VA; US Preventive Services Task Force. Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2014;160(5):330–338. [DOI] [PubMed] [Google Scholar]
- 2.Jemal A, Fedewa SA. Lung cancer screening with low-dose computed tomography in the United States – 2010 to 2015. JAMA Oncol Published online February 02, 2017. doi: 10.1001/jamaoncol.2016.6416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katki HA, Kovalchik SA, Berg CD, Cheung LC, Chaturvedi AK. Development and validation of risk models to select ever-smokers for CT lung cancer screening. JAMA 2016;315(21):2300–2311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC). National Health Interview Survey. CDC website; http://www.cdc.gov/nchs/nhis. 2017. Accessed October 30, 2017. [Google Scholar]
- 5.Cheung LC, Kovalchik SA, Katki HA. lcrisks: lung cancer risk models for screening. R package version 0.1.0. https://dceg.cancer.gov/tools/risk-assessment/lcrisks. 2017. Accessed October 30, 2017.
- 6.Lumley T. Analysis of complex survey samples. J Stat Softw 2004; 9(1): 1–19. [Google Scholar]
- 7.Pinsky PF, Kramer BS. Lung cancer risk and demographic characteristics of current 20–29 pack-year smokers: implications for screening. JNCI 2015; 107(11): djv226. [DOI] [PMC free article] [PubMed] [Google Scholar]


