Abstract
Background
Peroxisome proliferator‐activated receptor gamma (PPAR‐γ) agonists are insulin‐sensitising drugs used for the treatment of insulin resistance. In addition to lowering glucose in diabetes, these drugs may also protect against hyperlipidaemia and arteriosclerosis, which are risk factors for stroke. This is an update of a review first published in January 2014 and subsequently updated in December 2017.
Objectives
To assess the efficacy and safety of PPAR‐γ agonists in the secondary prevention of stroke and related vascular events for people with stroke or transient ischaemic attack (TIA).
Search methods
We searched the Cochrane Stroke Group Trials Register (30 July 2019), the Cochrane Central Register of Controlled Trials (CENTRAL; 2019, Issue 7), MEDLINE (1949 to 30 July 2019), Embase (1980 to 30 July 2019), CINAHL (1982 to 30 July 2019), AMED (1985 to 30 July 2019), and 11 Chinese databases (30 July 2019). In an effort to identify further published, unpublished, and ongoing trials, we searched ongoing trials registers, reference lists, and relevant conference proceedings, and contacted authors and pharmaceutical companies. We did not impose any language restrictions.
Selection criteria
We included randomised controlled trials (RCTs) evaluating PPAR‐γ agonists versus placebo for the secondary prevention of stroke and related vascular events in people with stroke or TIA, with the outcomes of recurrent stroke, vascular events, and adverse events.
Data collection and analysis
Two review authors independently screened the titles and abstracts of identified records, selected studies for inclusion, extracted eligible data, cross‐checked the data for accuracy, and assessed methodological quality and risk of bias. We evaluated the quality of evidence for each outcome using the GRADE approach.
Main results
We identified five RCTs with 5039 participants; two studies had a low risk of bias for all domains. Four studies evaluated the drug pioglitazone, and one study evaluated rosiglitazone. The participants in different studies were heterogeneous.
Recurrent stroke
Three studies evaluated the number of participants with recurrent stroke (4979 participants, a single study contributing 3876 of these). Peroxisome proliferator‐activated receptor gamma agonists probably reduce the recurrence of stroke compared with placebo (risk ratio (RR) 0.66, 95% confidence interval (CI) 0.44 to 0.99; moderate‐quality evidence).
Adverse events
Evidence that adverse events occurred more frequently in participants treated with PPAR‐γ agonists when compared with placebo was uncertain due to wide confidence interval and high levels of statistical heterogeneity: risk difference 10%, 95% CI ‐8% to 28%; low‐quality evidence).
Data were available on additional composite outcomes reflecting serious vascular events (all‐cause death and other major vascular events; all‐cause mortality, non‐fatal myocardial infarction or non‐fatal stroke) from one study in 984 people. This study provided low‐quality evidence that PPAR‐γ agonists led to fewer events (data not meta‐analysed).
Vascular events
Peroxisome proliferator‐activated receptor gamma agonists given over a mean duration of 34.5 months in a single trial of 984 participants may reduce serious vascular events expressed as a composite outcome of total events of cardiovascular death, non‐fatal myocardial infarction or non‐fatal stroke (RR 0.73, 95% CI 0.54 to 0.99; low‐quality evidence).
Other outcomes
One study in 20 people measured insulin sensitivity, and one study in 40 people measured the ubiquitin‐proteasome activity in carotid plaques. Our confidence in the improvements observed with PPAR‐γ agonists were limited by small sample sizes and risk of bias. None of the studies reported the number of participants with disability due to vascular events or improvement in quality of life.
Authors' conclusions
Peroxisome proliferator‐activated receptor gamma agonists probably reduce recurrent stroke and total events of cardiovascular death, non‐fatal myocardial infarction or non‐fatal stroke, and may improve insulin sensitivity and the stabilisation of carotid plaques. Their effects on adverse events are uncertain. Our conclusions should be interpreted with caution considering the small number and the quality of the included studies. Further well‐designed, double‐blind RCTs with large samples are required to assess the efficacy and safety of PPAR‐γ agonists in the secondary prevention of stroke and related vascular events in people with stroke or TIA.
Plain language summary
Diabetes drugs for preventing stroke and other blood vessel disease in people who have had a previous stroke or transient ischaemic attack
Question
We wanted to evaluate the effectiveness and safety of new diabetes drugs (peroxisome proliferator‐activated receptor gamma (PPAR‐γ) agonists) in the prevention of stroke and related blood vessel disease in people who have already had a stroke or transient ischaemic attack.
Background
Peroxisome proliferator‐activated receptor gamma agonists are drugs that improve the way insulin works in the human body. They are widely used in the treatment of adult type diabetes (type 2 diabetes). Moreover, they may also protect against the presence of excess fats in the blood and disease of the artery walls, which are both risk factors for stroke.
Study characteristics
We identified five studies to 30 July 2019 including a total of 5039 participants. Four studies evaluated the drug pioglitazone, and one study evaluated rosiglitazone. Four studies included participants who had no history of diabetes, and one study included only participants with diabetes.
Key results
Compared with placebo tablets, PPAR‐γ agonists reduced recurrent strokes and other blood vessel disease, improved the body's response to insulin, and stabilised fatty deposits in artery walls. The drugs also appeared to be well tolerated, but the evidence for this was inconclusive.
Quality of the evidence
Our conclusions should be interpreted with caution considering the small number of included studies and the limited quality of some of the studies. Further well‐designed randomised controlled trials with large sample sizes are required.
Summary of findings
Summary of findings for the main comparison. Peroxisome proliferator‐activated receptor gamma agonists for preventing recurrent stroke and other vascular events in people with stroke or transient ischaemic attack.
| Peroxisome proliferator‐activated receptor gamma (PPAR‐γ) agonists for preventing recurrent stroke and other vascular events in people with stroke or transient ischaemic attack | ||||||
|
Patient or population: people with stroke or transient ischaemic attack Settings: inpatients Intervention: PPAR‐γ agonists Comparison: placebo | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Placebo | PPAR‐γ agonists | |||||
|
Recurrence of stroke Follow‐up: 25 to 57.6 months |
85 per 1000 | 56 per 1000 (37 to 84) |
RR 0.66 (0.44 to 0.99) | 4979 (3 studies) | ⊕⊕⊕⊝ Moderate¹ | |
|
Reported adverse events Follow‐up: 3 to 34.5 months |
492 per 1000 | 502 per 1000 (412 to 530) |
RD 0.10 (‐0.08 to 0.28) | 1044 (3 studies) | ⊕⊕⊝⊝ Low² | |
| Serious vascular events | For the total events of all‐cause death, non‐fatal myocardial infarction, acute coronary syndrome and cardiac intervention, stroke, major leg amputation, or bypass surgery or leg revascularisation, there were 126 of 498 (25%). For the total events of all‐cause death, non‐fatal myocardial infarction or non‐fatal stroke, there were 98 of 498 (20%). | For the total events of all‐cause death, non‐fatal myocardial infarction, acute coronary syndrome and cardiac intervention, stroke, major leg amputation, or bypass surgery or leg revascularisation, there were 98 of 486 (20%). For the total events of all‐cause death, non‐fatal myocardial infarction or non‐fatal stroke, there were 76 of 486 (16%). | For the total events of all‐cause death, non‐fatal myocardial infarction, acute coronary syndrome and cardiac intervention, stroke, major leg amputation, or bypass surgery or leg revascularisation (RR 0.80, 95% CI 0.63 to 1.01). For the total events of all‐cause death, non‐fatal myocardial infarction or non‐fatal stroke (RR 0.79, 95% CI 0.61 to 1.04). Pioglitazone reduced fatal or non‐fatal stroke (RR 0.54, 95% CI 0.35 to 0.85) and total events of cardiovascular death, non‐fatal myocardial infarction or non‐fatal stroke (RR 0.73, 95% CI 0.54 to 0.99). | 984 (1 study) | ⊕⊕⊝⊝ Low³ | Pioglitazone reduced fatal or non‐fatal stroke and total events of cardiovascular death, non‐fatal myocardial infarction or non‐fatal stroke. |
| Deaths due to vascular events | Not reported | Not reported | — | — | — | |
| Disability due to vascular events | Not reported | Not reported | — | — | — | |
| Improvement in quality of life | Not reported | Not reported | — | — | — | |
|
Insulin sensitivity Assessed with composite insulin sensitivity index |
The change in the composite index was ‐0.1 ± 0.6. The C‐reactive protein concentration increased from 0.41 to 0.45 mg/L. | The change in the composite index was 1.2 ± 0.6. The C‐reactive protein concentration declined from 0.30 to 0.20 mg/L. | The change in the composite index was significantly increased in the pioglitazone group in comparison with the placebo group (P = 0.0003). | 20 (1 study) | ⊕⊕⊝⊝ Low³ | |
| Ubiquitin‐proteasome activity in carotid plaques | Ubiquitin 468.7 ± 89 ng/mg; proteasome 20S 79.8 ± 25 pmol/mg; nitrotyrosine 3.5 ± 0.42 nmol/pg; superoxide anion production 6.26 ± 1.4 pmol/L | Ubiquitin 322 ± 79 ng/mg; proteasome 20S 46.8 ± 10 pmol/mg; nitrotyrosine 2.2 ± 0.21 nmol/pg; superoxide anion production 3.57 ± 1.1 pmol/L | Compared with the placebo group, symptomatic carotid plaques in the rosiglitazone group showed fewer inflammatory cells (P < 0.01) with less ubiquitin (P < 0.01), proteasome 20S (P < 0.01), nuclear factor kappa B (P < 0.01), nitrotyrosine (P < 0.01), superoxide anion production (P < 0.01), and more collagen content (P < 0.01). | 40 (1 study) | ⊕⊕⊝⊝ Low³ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RD: risk difference; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Downgraded one level due to risk of bias. 2Downgraded one level due to risk of bias and one level due to inconsistency of results. 3Downgraded one level due to risk of bias and one level due to imprecision (small number of participants).
Background
Description of the condition
Stroke is one of the most common neurological diseases and one of the most common causes of mortality worldwide (WHO 2010). On average 80% of strokes are caused by ischaemia, and recurrent strokes account for around 30% of all events (Goldstein 2006; Simon 2009). Significantly higher mortality was found in recurrent stroke compared with first‐ever stroke (Jørgensen 1997). Secondary prevention therefore plays an important role in reducing stroke recurrence and other related vascular events. Diabetes is an important risk factor for ischaemic stroke. It has been estimated that around one in eight or nine strokes in people with a history of stroke or transient ischaemic attack (TIA) could be attributed to diabetes (Emerging Risk Factors Collaboration 2010). Management of blood glucose can therefore be regarded as one possible target for stroke prevention.
Description of the intervention
Peroxisome proliferator‐activated receptor gamma (PPAR‐γ) agonists are insulin‐sensitising drugs used for the treatment of hyperglycaemia with insulin resistance. To date, PPAR‐γ agonists such as rosiglitazone and pioglitazone have been widely recommended in the treatment of people with type 2 diabetes (Mooradian 2002). In certain cases PPAR‐γ agonists can be used in combination with insulin or other hypoglycaemic agents. In view of their effect on lowering glucose, PPAR‐γ agonists are believed to be beneficial for stroke prevention. Common adverse events associated with PPAR‐γ agonists include oedema, anaemia, liver dysfunction, and cardiac failure (Fogg 2009). Moreover, an increased risk of mortality and vascular events was found with rosiglitazone compared with pioglitazone in people with diabetes older than 65 years of age (Graham 2010).
How the intervention might work
The mechanisms of hyperglycaemia and stroke have been widely discussed. Blood flow and vascular reactivity can be affected by hyperglycaemia due to the abnormal metabolism of endothelium‐derived nitric oxide (Melikian 2009). Hyperglycaemia is also associated with reduced penumbral salvage in the large‐vessel thromboembolic stroke (Els 2002). Peroxisome proliferator‐activated receptor gamma agonists can therefore prevent these pathological processes by controlling blood glucose. In addition to lowering glucose, PPAR‐γ agonists may also protect against hyperlipidaemia and arteriosclerosis, which are complications of diabetes and risk factors for stroke (Collino 2010; Dasu 2009). Moreover, PPAR‐γ agonists have been shown to reduce inflammation, which may prevent vascular events to some extent (Nakamura 2007).
Why it is important to do this review
Evidence from trials indicates the benefits of aspirin, clopidogrel, ticlopidine, triflusal, and the combination of aspirin and dipyridamole in the secondary prevention of stroke and other vascular events (Costa 2005; De Schryver 2007; Sudlow 2009). Anticoagulants appear to be less effective, at least where the cause is not cardioembolic (Sandercock 2009). Vitamin K antagonists are not more efficacious than antiplatelet therapy (De Schryver 2012). Peroxisome proliferator‐activated receptor gamma agonists have been tested in clinical trials focusing on the prevention of stroke and other vascular events, particularly for people with diabetes. We thus aimed to evaluate the efficacy and safety of PPAR‐γ agonists for preventing recurrent stroke and other vascular events in people with stroke or TIA. To our knowledge, no other systematic review or meta‐analysis on this topic exists in the literature.
Objectives
To assess the efficacy and safety of PPAR‐γ agonists in the secondary prevention of stroke and related vascular events for people with stroke or TIA.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials and excluded quasi‐randomised or confounded studies.
Types of participants
We included studies of people over the age of 18 years with a history of stroke or TIA. We used the definition of TIA as provided in the original publications. We excluded studies of people with diabetes who lacked a clear history of stroke or TIA.
Types of interventions
We included trials comparing PPAR‐γ agonists (including pioglitazone, rosiglitazone, glitazone, troglitazone, netoglitazone, rivoglitazone, ciglitazone, balaglitazone, darglitazone, edaglitazone, englitazone, and lobeglitazone) with placebo, regardless of the length of treatment period and dosage of treatment. We included other concomitant therapies providing they were administered to both the intervention and control groups.
Types of outcome measures
We measured all outcomes at the end of follow‐up.
Primary outcomes
The number of participants with recurrent stroke, as defined in the original publications.
The number of participants who experienced any adverse events, such as oedema, anaemia, or cardiac failure.
Secondary outcomes
The number of participants with serious vascular events, such as myocardial infarction, stroke, or vascular death.
The number of deaths due to vascular events.
The number of participants with disability due to vascular events.
Improvement in quality of life.
Insulin sensitivity.
Ubiquitin‐proteasome activity in carotid plaques.
Search methods for identification of studies
See the 'Specialized register' section in the Cochrane Stroke Group module. We searched for trials in all languages and arranged for the translation of relevant articles where necessary.
Electronic searches
We searched the Cochrane Stroke Group Trials Register (30 July 2019) and the following electronic bibliographic databases:
Cochrane Central Register of Controlled Trials (CENTRAL; 2019, Issue 7) in the Cochrane Library (searched 30 July 2019) (Appendix 1);
MEDLINE (Ovid) (1949 to 30 July 2019) (Appendix 2);
Embase (Ovid) (1980 to 30 July 2019) (Appendix 3);
CINAHL (EBSCO) (Cumulative Index to Nursing and Allied Health Literature; 1982 to 30 July 2019) (Appendix 4);
AMED (Ovid) (Allied and Complementary Medicine Database; 1985 to 30 July 2019) (Appendix 5).
We developed all the search strategies with the help of the Cochrane Stroke Group Information Specialist.
We also searched the following ongoing trials registers on 30 July 2019:
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov/) (Appendix 6);
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch) (Appendix 7).
Searching other resources
We searched the following resources with the Chinese equivalents of keywords (Appendix 8):
Chinese Clinical Trials Registry (searched on 30 July 2019);
CBM‐disc (China Biological Medicine Databases) (1979 to 30 July 2019);
CNKI (China National Knowledge Infrastructure) (1979 to 30 July 2019);
Chinese MD and DD Dissertations in CNKI (searched on 30 July 2019);
CACP (Chinese Academic Conference Papers Database) (1998 to 30 July 2019);
CDDB (Chinese Dissertations Database) (1977 to 30 July 2019);
Chinese Evidence‐Based Medicine Database (searched on 30 July 2019);
CMAC (China Medical Academic Conferences) (1994 to 30 July 2019);
CMCC (Chinese Medical Current Contents) (1994 to 30 July 2019);
Chinese Science and Technique Journals Database (VIP) (1989 to 30 July 2019);
Wanfang Data (www.wanfangdata.com/) (1984 to 30 July 2019).
We also:
used Science Citation Index Cited Reference Search for forward tracking of important articles;
searched reference lists of relevant reviews and retrieved articles;
searched relevant conference proceedings, including the 6th to 27th European Stroke Conference (from 1997 to 2018), the 5th European Stroke Organisation Conference (2019) and the 4th to 11th World Stroke Congress (from 2000 to 2018);
contacted authors where necessary for missing information;
contacted the manufacturers (Takeda Pharmaceutical Company and GlaxoSmithKline Pharmaceuticals) for updated information.
Data collection and analysis
Selection of studies
Two review authors (JL, LW) independently screened titles and abstracts of the references identified by the search and excluded obviously irrelevant reports. We retrieved the full‐text articles for the remaining references, and the same two review authors independently screened the full‐text articles and identified studies for inclusion, and also identified and recorded reasons for exclusion of the ineligible studies. We resolved any disagreements through discussion or, if required, we consulted an external third party. We collated multiple reports of the same study so that each study, not each reference, was the unit of interest in the review. We recorded the selection process and completed a PRISMA flow diagram (Figure 1).
1.
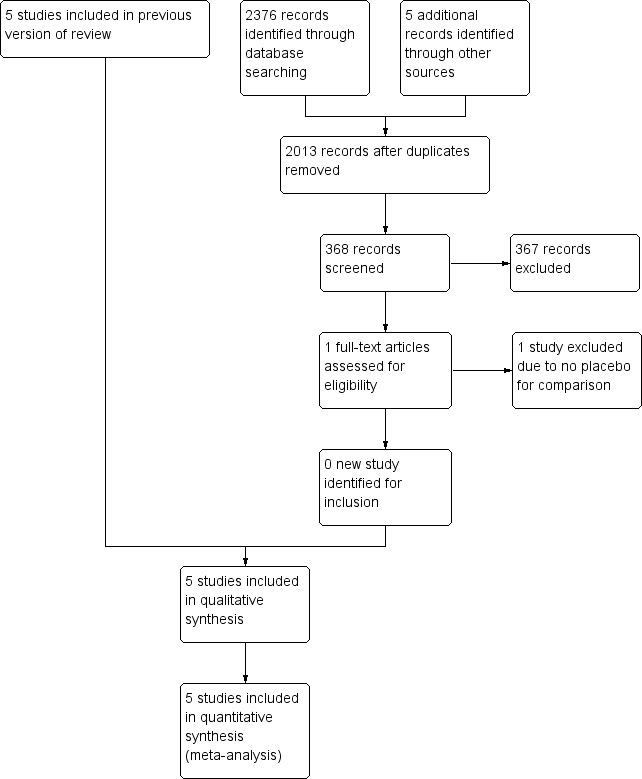
Study flow diagram.
Data extraction and management
Two review authors (JL, LW) independently extracted data from the published reports onto standardised forms, and cross‐checked the data for accuracy. We used checklists to independently record details including methods of generating the randomisation schedule, method of concealment of allocation, blinding of assessors, intention‐to‐treat analysis, adverse events and dropouts for all reasons, important imbalance in prognostic factors, participants (socio‐demographic and related clinical information), interventions (medications and non‐pharmacological interventions), and outcomes. We resolved disagreements with an external third party.
Assessment of risk of bias in included studies
Two review authors (JL, LW) independently assessed the risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved any disagreements by discussion or by involving an external third party. We assessed the risk of bias according to the following domains.
Random sequence generation.
Allocation concealment.
Blinding of participants and personnel.
Blinding of outcome assessment.
Incomplete outcome data.
Selective outcome reporting.
Other bias.
We graded the risk of bias for each domain as high, low, or unclear and provided information from the study report together with a justification for our judgement in the 'Risk of bias' tables.
Measures of treatment effect
We expected the randomised controlled trials to measure dichotomous data. We expressed dichotomised data as risk ratios (RRs) with their 95% confidence intervals (CI). If a trial (or group within a trial) reported no adverse events or dropouts, we calculated risk differences (RDs) instead of RRs with 95% CI. We entered and analysed data using Review Manager 5 (RevMan 2014).
Unit of analysis issues
We dealt with any unit of analysis issues according to the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Dealing with missing data
We planned to contact the authors of the studies for further details if any data were missing or to establish the characteristics of unpublished trials. According to the intention‐to‐treat principle, all randomised participants should be included. We considered different scenarios (best‐case and worst‐case) to account for missing data.
Assessment of heterogeneity
We used the I² statistic to measure heterogeneity among the trials in each analysis, considering I² values over 50% as suggestive of substantial heterogeneity.
Assessment of reporting biases
We planned to use funnel plots to examine potential publication bias if there was a sufficient number of trials (Egger 1997).
Data synthesis
Where we considered studies to be sufficiently similar, we conducted a meta‐analysis by pooling the appropriate data using Review Manager 5 (RevMan 2014). We expressed dichotomised data as RRs with their 95% CI. If a trial (or group within a trial) reported no adverse events or dropouts, we calculated RDs instead of RRs with 95% CI. We calculated the overall effects using a random‐effects model regardless of the level of heterogeneity. We provided a descriptive summary of the results when substantial heterogeneity between the studies prevented us from combining outcome data.
GRADE and 'Summary of findings'
We included each of the main analyses in a 'Summary of findings' table (Table 1). We determined the quality of the evidence using the GRADE approach and downgraded evidence due to the presence of high risk of bias in at least one study, indirectness of the evidence, unexplained heterogeneity or inconsistency, imprecision of results, high probability of publication bias. We downgraded evidence by one level if we considered the limitation to be serious and by two levels if very serious.
Subgroup analysis and investigation of heterogeneity
We intended to undertake subgroup analyses according to the age and ethnicity of participants, TIA definition, different PPAR‐γ agonists, and dosage and duration of treatment. We intended to use the Chi² test to examine the significance of differences between subgroups.
Sensitivity analysis
We analysed sensitivity by assessing the robustness of results in fixed‐effect versus random‐effects models, and studies at high risk versus low risk of bias. We also examined potential sources of methodological heterogeneity.
Results
Description of studies
Results of the search
The previous version of this review included five studies. On re‐running the searches in 30 July 2019, we identified 315 papers after de‐duplicating the results (Figure 1). We acquired and screened the full text of one article, which did not meet the inclusion criteria. We therefore included a total of five studies with 16 articles in this update. Agreement between the review authors on exclusion was 100%.
Included studies
In accordance with the inclusion criteria, we included five studies with 5039 participants. IRIS investigated the efficacy of pioglitazone in participants with insulin resistance and ischaemic stroke or TIA no less than 14 days and no more than six months before randomisation. J‐SPIRIT tested the effect of pioglitazone on the reduction of recurrent stroke in participants with abnormal glucose metabolisms and insulin resistance after ischaemic stroke. Kernan 2003 evaluated the effect of pioglitazone in improving insulin sensitivity among non‐diabetic patients with a recent TIA or non‐disabling ischaemic stroke. Marfella 2006 investigated the effect of rosiglitazone in participants with symptomatic carotid stenosis by testing ubiquitin‐proteasome activity in carotid plaques. PROactive focused on the efficacy and safety of pioglitazone on the reduction of stroke recurrence and related vascular events in participants with type 2 diabetes. The details of the included studies are provided in the Characteristics of included studies table.
Excluded studies
We excluded 15 studies after full‐text evaluation (CIMT Trial; Erdmann 2015; Forst 2008; Hedblad 2007; ISRCTN54951661; Koshiyama 2001; Lincoff 2014; Meisner 2006; NCT00879970; Schrieks 2018; Sidhu 2004; Tanaka 2015; TART; TRIPOD; Varghese 2009). The reasons for exclusion are provided in the Characteristics of excluded studies table.
Risk of bias in included studies
Information regarding risk of bias is provided in Figure 2 and Figure 3. The data for J‐SPIRIT were only released in abstracts, therefore insufficient information was available for us to judge the risk of bias.
2.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
3.
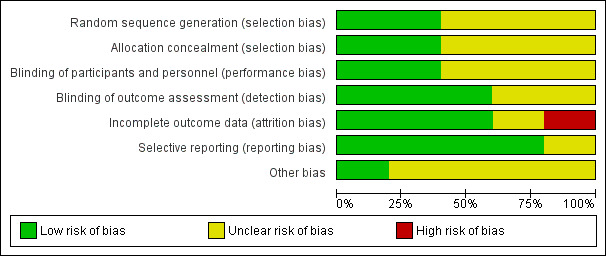
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
Two studies clearly stated the methods of randomisation and allocation concealment (IRIS; Kernan 2003). Information for the remaining studies was insufficient to make a judgement of high or low risk of bias, therefore we judged selection bias as at unclear risk of bias.
Blinding
Information regarding blinding was insufficient in two studies (J‐SPIRIT; PROactive). In Kernan 2003 and IRIS, information about performance bias and detection bias was provided, while only information about detection bias was reported in Marfella 2006. We therefore assessed this as at unclear risk of bias.
Incomplete outcome data
J‐SPIRIT did not report on completeness of outcome data. No dropouts were reported in Kernan 2003 or Marfella 2006. In IRIS, a total of 227 participants (5.9%) withdrew consent and 99 (2.6%) were lost to follow‐up; we assessed this study as at low risk of bias. In PROactive, 882 of 984 participants (90%) completed the final visit: 439/486 (90%) in the pioglitazone group and 443/498 (89%) in the placebo group. We assessed this as at high risk of bias.
Selective reporting
With the exception of J‐SPIRIT, all prespecified outcomes were reported in the included trials. We therefore assessed this as at low risk of bias.
Other potential sources of bias
The role of financial support was clearly stated in Kernan 2003, therefore we judged this study as at low risk of bias. We judged the remaining four studies as at unclear risk of bias (IRIS; J‐SPIRIT; Marfella 2006; PROactive).
Effects of interventions
See: Table 1
Primary outcome measures
Number of participants with recurrent stroke
Three studies with 4979 participants reported the number of recurrent strokes at the end of the study: 156/2483 (6%) participants in the PPAR‐γ agonist group and 212/2496 (8%) participants in the placebo group (risk ratio (RR) 0.66, 95% confidence interval (CI) 0.44 to 0.99; moderate‐quality evidence) (Analysis 1.1) (IRIS; J‐SPIRIT; PROactive). When we conducted a sensitivity analysis with a fixed‐effect model, the results did not vary substantially (RR 0.74, 95% CI 0.61 to 0.90).
1.1. Analysis.
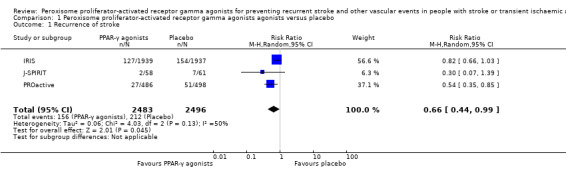
Comparison 1 Peroxisome proliferator‐activated receptor gamma agonists agonists versus placebo, Outcome 1 Recurrence of stroke.
Number of participants who experienced any adverse events
Three studies reported the number of participants with any adverse events (Kernan 2003; Marfella 2006; PROactive). Adverse events were experienced by 247/516 (48%) and 260/528 (49%) participants in the PPAR‐γ agonists and placebo groups, respectively (risk difference (RD) 10%, 95% CI ‐8% to 28%; low‐quality evidence), with strong heterogeneity (test for heterogeneity I² = 86%) (Analysis 1.2). When we conducted a sensitivity analysis with a fixed‐effect model, the result was: RD ‐1%, 95% CI ‐7% to 5%. The RDs of the random‐effects and fixed‐effect models were essentially the same. In Kernan 2003, certain adverse events such as nausea, oedema, muscle aches, sore throat, and dizziness were more common in the pioglitazone group. In Marfella 2006, no clinical events were reported in either group during the study. The proportion of participants who experienced adverse events was the highest in PROactive, with definitions of adverse events including: resulting in death, life‐threatening, needing or prolonging in‐patient admission, resulting in persistent or significant disability, or needing intervention to prevent any of the above. As a result, heart failure requiring hospitalisation was reported in 31 (6.4%) participants in the pioglitazone group versus 20 (4.0%) in the placebo group (P = 0.09). Fatal heart failure was reported in 6 (1.2%) participants in the pioglitazone group versus 4 (0.8%) participants in the placebo group (P = 0.50). IRIS only reported the number of each adverse event. In general, participants in the pioglitazone group had more weight gain, oedema, shortness of breath, and bone fractures than did participants in the placebo group.
1.2. Analysis.

Comparison 1 Peroxisome proliferator‐activated receptor gamma agonists agonists versus placebo, Outcome 2 Reported adverse events.
Secondary outcome measures
Number of participants with serious vascular events
Only one study reported the number of participants with serious vascular events (PROactive). For the total events of all‐cause death, non‐fatal myocardial infarction, acute coronary syndrome and cardiac intervention, stroke, major leg amputation, or bypass surgery or leg revascularisation, there were 98/486 (20%) and 126/498 (25%) participants in the PPAR‐γ agonists and placebo groups, respectively (RR 0.80, 95% CI 0.63 to 1.01; low‐quality evidence). For the total events of all‐cause death, non‐fatal myocardial infarction or non‐fatal stroke, there were 76/486 (16%) and 98/498 (20%) participants in the PPAR‐γ agonists and placebo groups, respectively (RR 0.79, 95% CI 0.61 to 1.04; low‐quality evidence). Pioglitazone reduced fatal or non‐fatal stroke (RR 0.54, 95% CI 0.35 to 0.85; low‐quality evidence) and total events of cardiovascular death, non‐fatal myocardial infarction or non‐fatal stroke (RR 0.73, 95% CI 0.54 to 0.99; low‐quality evidence).
Number of deaths due to vascular events
None of the studies reported the number of deaths due to vascular events. However, PROactive reported all‐cause mortality: 46/486 (9%) and 49/498 (10%) deaths in the PPAR‐γ agonists and placebo groups, respectively (RR 0.96, 95% CI 0.66 to 1.41).
Number of participants with disability due to vascular events
None of the studies reported the number of participants with disability due to vascular events.
Improvement in quality of life
None of the studies reported improvement in quality of life.
Insulin sensitivity
In Kernan 2003, insulin sensitivity was measured with the composite insulin sensitivity index. The change in the composite index was 1.2 ± 0.6 (mean ± standard deviation) in the pioglitazone group and ‐0.1 ± 0.6 in the placebo group (P = 0.0003). The C‐reactive protein concentration declined from 0.30 to 0.20 mg/L in the pioglitazone group, but increased from 0.41 to 0.45 mg/L in the placebo group (P = 0.06).
Ubiquitin‐proteasome activity in carotid plaques
Marfella 2006 examined the ubiquitin‐proteasome activity in carotid plaques. Compared with the placebo group, symptomatic carotid plaques in the rosiglitazone group showed fewer inflammatory cells (P < 0.01); less ubiquitin (322 ± 79 ng/mg in the rosiglitazone group and 468.7 ± 89 ng/mg in the placebo group, P < 0.01), proteasome 20S (46.8 ± 10 pmol/mg in the rosiglitazone group and 79.8 ± 25 pmol/mg in the placebo group, P < 0.01), and nuclear factor kappa B (NFkB) (P < 0.01); less nitrotyrosine (2.2 ± 0.21 nmol/pg in the rosiglitazone group and 3.5 ± 0.42 nmol/pg in the placebo group, P < 0.01) and superoxide anion production (3.57 ± 1.1 pmol/L in the rosiglitazone group and 6.26 ± 1.4 pmol/L in the placebo group, P < 0.01); and more collagen content (P < 0.01), suggesting greater plaque stabilisation.
Discussion
Summary of main results
Five studies with 5039 participants met the inclusion criteria. Four of these studies evaluated the effect of pioglitazone versus placebo (IRIS; J‐SPIRIT; Kernan 2003; PROactive); the fifth focused on rosiglitazone versus placebo (Marfella 2006). Three studies evaluated the number of participants with recurrent stroke (IRIS; J‐SPIRIT; PROactive), where PPAR‐γ agonists reduced the recurrence of stroke compared with placebo (RR 0.66, 95% CI 0.44 to 0.99; moderate‐quality evidence). Moreover, PPAR‐γ agonists reduced total events of cardiovascular death, non‐fatal myocardial infarction or non‐fatal stroke and improved insulin sensitivity and stabilisation of carotid plaques (Kernan 2003; Marfella 2006; PROactive). Regarding safety, evidence was inconclusive of any difference in reported adverse events in the PPAR‐γ agonists group versus the placebo group (RD 10%, 95% CI ‐8% to 28%; low‐quality evidence) in three studies (Kernan 2003; Marfella 2006; PROactive).
Overall completeness and applicability of evidence
All participants had a past history of stroke or TIA; however, none of the randomised controlled trials precisely described stroke type or diagnosis criteria. Kernan 2003 evaluated non‐diabetic participants, IRIS and J‐SPIRIT participants with an abnormal glucose metabolism and insulin resistance, PROactive participants with type 2 diabetes, and Marfella 2006 participants with carotid plaques. The clinical heterogeneity of the participants in the included studies could potentially induce heterogeneity in the results of the meta‐analysis. Four studies evaluated pioglitazone versus placebo (IRIS; J‐SPIRIT; Kernan 2003; PROactive), and one study evaluated rosiglitazone versus placebo (Marfella 2006). Regarding outcomes, three studies recorded recurrent stroke (IRIS; J‐SPIRIT; PROactive). The other two studies investigated insulin sensitivity and ubiquitin‐proteasome activity in carotid plaques, respectively (Kernan 2003; Marfella 2006). Due to insufficient data, we did not undertake any subgroup analyses.
Quality of the evidence
We judged IRIS and Kernan 2003 as of high quality with a low risk of bias for all domains. J‐SPIRIT was only published as abstracts, therefore information was insufficient to judge. We assessed Marfella 2006 and PROactive as at unclear risk of bias forthe method of randomisation, allocation concealment, and blinding., and PROactive as at high risk of bias for incomplete outcome data. In summary, the methodological limitations of the included studies should be considered when interpreting the results. In addition, the sample sizes in Kernan 2003 and Marfella 2006 were relatively small.
Potential biases in the review process
We performed the search strategy as per protocol and identified five completed studies. However, we cannot be certain that we have not missed other unpublished studies. Our contact with relevant authors and manufacturers yielded no additional information. In preparing this review, we independently screened trials for inclusion, extracted data, and assessed the quality of included trials to minimise potential biases. We used the RD as a way of addressing studies with zero events. The event rates of the number of participants with adverse events reported, based on the aggregate event rates for the two groups, were 48% versus 49%, a difference of 1%. With the random‐effects model, the outlying estimate from Kernan 2003 effectively pushed the RD out towards 10%. This might well explain why the difference in the aggregate data of 1% did not translate to a RD of 10% (the fixed‐effect result was much closer to the aggregate events). We found no other potential biases.
Agreements and disagreements with other studies or reviews
To our knowledge, this is the first systematic review of this intervention in the field of secondary prevention of stroke and related vascular events for people with stroke or TIA.
Authors' conclusions
Implications for practice.
Peroxisome proliferator‐activated receptor gamma (PPAR‐γ) agonists appear to reduce recurrent stroke and other vascular events, and improve insulin sensitivity and the stabilisation of carotid plaques. In addition, PPAR‐γ agonists appeared to be relatively well tolerated. However, the conclusions of this review should be interpreted with caution considering the small number of included studies and the quality of some of the studies.
Implications for research.
Further well‐designed, double‐blind randomised controlled trials with large sample sizes are required to test the efficacy and safety of PPAR‐γ agonists in the secondary prevention of stroke and related vascular events for people with stroke or transient ischaemic attack.
What's new
| Date | Event | Description |
|---|---|---|
| 30 July 2019 | New citation required but conclusions have not changed | Conclusions unchanged. |
| 30 July 2019 | New search has been performed | We updated all the searches for this review to 30 July 2019. No new studies were included in the review. The review has five included studies involving 5039 participants. |
History
Protocol first published: Issue 8, 2013 Review first published: Issue 1, 2014
| Date | Event | Description |
|---|---|---|
| 6 May 2017 | New search has been performed | We updated all the searches for this review to 16 May 2017. One previously ongoing study (IRIS; 3876 participants) was completed and has been added to this review; five studies, with a total of 5039 participants, are now included in the review. |
| 6 May 2017 | New citation required but conclusions have not changed | Conclusions unchanged. |
| 24 July 2015 | New search has been performed | We updated all the searches for this review to July 2015 but did not identify any new information for inclusion, therefore our conclusions remain unchanged. We included a 'Summary of findings' table. |
| 24 July 2015 | New citation required but conclusions have not changed | Conclusions unchanged. |
Acknowledgements
The authors acknowledge the help provided by the Cochrane Stroke Group.
Appendices
Appendix 1. Cochrane Central Register of Controlled Trials (CENTRAL)
#1 [mh ^"cerebrovascular disorders"] or [mh "basal ganglia cerebrovascular disease"] or [mh "brain ischemia"] or [mh "carotid artery diseases"] or [mh "cerebrovascular trauma"] or [mh "intracranial arterial diseases"] or [mh "intracranial arteriovenous malformations"] or [mh "intracranial embolism and thrombosis"] or [mh "intracranial hemorrhages"] or [mh ^stroke] or [mh "brain infarction"] or [mh ^"vasospasm, intracranial"]
#2 (stroke or poststroke or "post‐stroke" or cerebrovasc* or brain next vasc* or cerebral next vasc* or cva* or apoplex* or SAH):ti,ab
#3 ((brain* or cerebr* or cerebell* or intracran* or intracerebral) near/5 (isch*mi* or infarct* or thrombo* or emboli* or occlus*)):ti,ab
#4 ((brain* or cerebr* or cerebell* or intracerebral or intracranial or subarachnoid) near/5 (haemorrhage* or hemorrhage* or haematoma* or hematoma* or bleed*)):ti,ab
#5 ((transi* near/3 isch*m* near/3 attack*) or TIA or TIAs):ti,ab
#6 #1 or #2 or #3 or #4 or #5
#7 [mh ^"PPAR gamma"/AG,DE,ME,PD,TU]
#8 [mh ^"Peroxisome Proliferator‐Activated Receptors"/AG,DE,ME,PD,TU] or [mh ^"Transcription Factors"/AG,DE,ME,PD,TU]
#9 [mh ^Thiazolidinediones] or [mh ^Pioglitazone]
#10 (("peroxisome proliferator‐activated receptor gamma" or "PPAR gamma" or "PPAR‐gamma" or "PPARgamma" or PPARG or NR1C3) near/5 (agonist* or modulator* or stimulat* or stimulant* or activat*)):ti,ab
#11 (thiazolidinedione* or glitazone* or pioglitazone or rosiglitazone or troglitazone or netoglitazone or rivoglitazone or ciglitazone or balaglitazone or darglitazone or edaglitazone or englitazone or lobeglitazone):ti,ab
#12 #7 or #8 or #9 or #10 or #11
#13 #6 and #12
Appendix 2. MEDLINE search strategy (Ovid)
1. cerebrovascular disorders/ or exp basal ganglia cerebrovascular disease/ or exp brain ischemia/ or exp carotid artery diseases/ or exp cerebrovascular trauma/ or exp intracranial arterial diseases/ or exp intracranial arteriovenous malformations/ or exp "intracranial embolism and thrombosis"/ or exp intracranial hemorrhages/ or stroke/ or exp brain infarction/ or vasospasm, intracranial/
2. (stroke or poststroke or post‐stroke or cerebrovasc$ or brain vasc$ or cerebral vasc$ or cva$ or apoplex$ or SAH).tw.
3. ((brain$ or cerebr$ or cerebell$ or intracran$ or intracerebral) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$)).tw.
4. ((brain$ or cerebr$ or cerebell$ or intracerebral or intracranial or subarachnoid) adj5 (haemorrhage$ or hemorrhage$ or haematoma$ or hematoma$ or bleed$)).tw.
5. ((transi$ adj3 isch?em$ adj3 attack$) or TIA$1).tw.
6. 1 or 2 or 3 or 4 or 5
7. PPAR gamma/ag, de, me, pd, tu
8. Peroxisome Proliferator‐Activated Receptors/ag, de, me, pd, tu or Transcription Factors/ag, de, me, pd, tu
9. Thiazolidinediones/ or Pioglitazone/
10. ((peroxisome proliferator‐activated receptor gamma or PPAR gamma or PPAR‐gamma or PPARgamma or PPARG or NR1C3) adj5 (agonist$ or modulator$ or stimulat$ or stimulant$ or activat$)).tw.
11. (thiazolidinedione$ or glitazone$ or pioglitazone or rosiglitazone or troglitazone or netoglitazone or rivoglitazone or ciglitazone or balaglitazone or darglitazone or edaglitazone or englitazone or lobeglitazone).tw,nm.
12. 7 or 8 or 9 or 10 or 11
13. Randomized Controlled Trials as Topic/
14. random allocation/
15. Controlled Clinical Trials as Topic/
16. control groups/
17. clinical trials as topic/ or clinical trials, phase i as topic/ or clinical trials, phase ii as topic/ or clinical trials, phase iii as topic/ or clinical trials, phase iv as topic/
18. double‐blind method/
19. single‐blind method/
20. Placebos/
21. placebo effect/
22. Drug Evaluation/
23. Research Design/
24. randomized controlled trial.pt.
25. controlled clinical trial.pt.
26. (clinical trial or clinical trial phase i or clinical trial phase ii or clinical trial phase iii or clinical trial phase iv).pt.
27. random$.tw.
28. (controlled adj5 (trial$ or stud$)).tw.
29. (clinical$ adj5 trial$).tw.
30. ((control or treatment or experiment$ or intervention) adj5 (group$ or subject$ or patient$)).tw.
31. (quasi‐random$ or quasi random$ or pseudo‐random$ or pseudo random$).tw.
32. ((singl$ or doubl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).tw.
33. placebo$.tw.
34. controls.tw.
35. (RCT or RCTs).tw. or trial.ti.
36. or/13‐35
37. 6 and 12 and 36
38. exp animals/ not humans.sh.
39. 37 not 38
Appendix 3. Embase search strategy (Ovid)
1. cerebrovascular disease/ or exp basal ganglion hemorrhage/ or exp brain hematoma/ or exp brain hemorrhage/ or exp brain infarction/ or exp brain ischemia/ or exp carotid artery disease/ or cerebral artery disease/ or exp cerebrovascular accident/ or exp intracranial aneurysm/ or exp occlusive cerebrovascular disease/ or vertebrobasilar insufficiency/ or stroke/ or stroke patient/ or stroke unit/
2. (stroke or poststroke or post‐stroke or cerebrovasc$ or brain vasc$ or cerebral vasc$ or cva$ or apoplex$ or SAH).tw.
3. ((brain$ or cerebr$ or cerebell$ or intracran$ or intracerebral) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$)).tw.
4. ((brain$ or cerebr$ or cerebell$ or intracerebral or intracranial or subarachnoid) adj5 (haemorrhage$ or hemorrhage$ or haematoma$ or hematoma$ or bleed$)).tw.
5. ((transi$ adj3 isch?em$ adj3 attack$) or TIA$1).tw.
6. 1 or 2 or 3 or 4 or 5
7. peroxisome proliferator activated receptor gamma agonist/
8. peroxisome proliferator activated receptor gamma/ct, ad, dt [Clinical Trial, Drug Administration, Drug Therapy]
9. peroxisome proliferator activated receptor gamma 2/dt [Drug Therapy]
10. peroxisome proliferator activated receptor/ct, ad, dt [Clinical Trial, Drug Administration, Drug Therapy]
11. transcription factor/ct, ad, dt [Clinical Trial, Drug Administration, Drug Therapy]
12. peroxisome proliferator activated receptor gamma coactivator 1alpha/ct, dt [Clinical Trial, Drug Therapy]
13. peroxisome proliferator activated receptor gamma coactivator 1beta/dt [Drug Therapy]
14. exp glitazone derivative/
15. ((peroxisome proliferator‐activated receptor gamma or PPAR gamma or PPAR‐gamma or PPARgamma or PPARG or NR1C3) adj5 (agonist$ or modulator$ or stimulat$ or stimulant$ or activat$)).tw.
16. (thiazolidinedione$ or glitazone$ or pioglitazone or rosiglitazone or troglitazone or netoglitazone or rivoglitazone or ciglitazone or balaglitazone or darglitazone or edaglitazone or englitazone or lobeglitazone).tw.
17. 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16
18. 6 and 17
19. Randomized Controlled Trial/
20. Randomization/
21. Controlled Study/
22. control group/
23. clinical trial/ or phase 1 clinical trial/ or phase 2 clinical trial/ or phase 3 clinical trial/ or phase 4 clinical trial/ or controlled clinical trial/
24. Double Blind Procedure/
25. Single Blind Procedure/ or triple blind procedure/
26. placebo/
27. "types of study"/
28. random$.tw.
29. (controlled adj5 (trial$ or stud$)).tw.
30. (clinical$ adj5 trial$).tw.
31. ((control or treatment or experiment$ or intervention) adj5 (group$ or subject$ or patient$)).tw.
32. (quasi‐random$ or quasi random$ or pseudo‐random$ or pseudo random$).tw.
33. ((singl$ or doubl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).tw.
34. placebo$.tw.
35. (RCT or RCTs).tw. or trial.ti.
36. or/19‐35
37. 18 and 36
38. (exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/) not (human/ or normal human/ or human cell/)
39. 37 not 38
Appendix 4. CINAHL search strategy (EBSCO)
S16. S11 AND S15
S15. S12 OR S13 OR S14
S14. TI thiazolidinedione* or glitazone* or pioglitazone or rosiglitazone or troglitazone or netoglitazone or rivoglitazone or ciglitazone or balaglitazone or darglitazone or edaglitazone or englitazone or lobeglitazone or AB thiazolidinedione* or glitazone* or pioglitazone or rosiglitazone or troglitazone or netoglitazone or rivoglitazone or ciglitazone or balaglitazone or darglitazone or edaglitazone or englitazone or lobeglitazone
S13. ( TI peroxisome proliferator‐activated receptor gamma or PPAR gamma or PPAR‐gamma or PPARgamma or PPARG or NR1C3 or AB peroxisome proliferator‐activated receptor gamma or PPAR gamma or PPAR‐gamma or PPARgamma or PPARG or NR1C3 ) AND ( TI agonist* or modulator* or stimulat* or stimulant* or activat* or AB agonist* or modulator* or stimulat* or stimulant* or activat* )
S12. (MH "Thiazolidinediones") OR (MH "Troglitazone") OR (MH "Rosiglitazone") OR (MH "Pioglitazone")
S11. S1 OR S2 OR S3 OR S6 OR S9 OR S10
S10. TI transient ischaemic attack* or TI transient ischemic attack* or AB transient ischaemic attack* or AB transient ischemic attack* or TI TIA or TI TIA s or AB TIA or AB TIAs
S9. S7 and S8
S8. TI ( haemorrhage* or hemorrhage* or haematoma* or hematoma* or bleed* ) or AB ( haemorrhage* or hemorrhage* or haematoma* or hematoma* or bleed* )
S7. TI ( brain* or cerebr* or cerebell* or intracerebral or intracranial or subarachnoid ) or AB ( brain* or cerebr* or cerebell* or intracerebral or intracranial or subarachnoid )
S6. S4 and S5
S5. TI ( ischemi* or ischaemi* or infarct* or thrombo* or emboli* or occlus* ) or AB ( ischemi* or ischaemi* or infarct* or thrombo* or emboli* or occlus* )
S4. TI ( brain* or cerebr* or cerebell* or intracran* or intracerebral ) or AB ( brain* or cerebr* or cerebell* or intracran* or intracerebral )
S3. TI ( stroke or poststroke or post‐stroke or cerebrovasc* or brain vasc* or cerebral vasc or cva or apoplex or SAH ) or AB ( stroke or poststroke or post‐stroke or cerebrovasc* or brain vasc* or cerebral vasc or cva or apoplex or SAH )
S2. (MH "Stroke Patients") OR (MH "Stroke Units")
S1. (MH "Cerebrovascular Disorders") OR (MH "Basal Ganglia Cerebrovascular Disease+") OR (MH "Carotid Artery Diseases+") OR (MH "Cerebral Ischemia+") OR (MH "Cerebral Vasospasm") OR (MH "Intracranial Arterial Diseases+") OR (MH "Intracranial Embolism and Thrombosis") OR (MH "Intracranial Hemorrhage+") OR (MH "Stroke") OR (MH "Vertebral Artery Dissections")
Appendix 5. AMED search strategy (Ovid)
1. cerebrovascular disorders/ or cerebral hemorrhage/ or cerebral infarction/ or cerebral ischemia/ or cerebrovascular accident/ or stroke/
2. (stroke or poststroke or post‐stroke or cerebrovasc$ or brain vasc$ or cerebral vasc$ or cva$ or apoplex$ or SAH).tw.
3. ((brain$ or cerebr$ or cerebell$ or intracran$ or intracerebral) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$)).tw.
4. ((brain$ or cerebr$ or cerebell$ or intracerebral or intracranial or subarachnoid) adj5 (haemorrhage$ or hemorrhage$ or haematoma$ or hematoma$ or bleed$)).tw.
5. ((transi$ adj3 isch?em$ adj3 attack$) or TIA$1).tw.
6. 1 or 2 or 3 or 4 or 5
7. ((peroxisome proliferator‐activated receptor gamma or PPAR gamma or PPAR‐gamma or PPARgamma or PPARG or NR1C3) adj5 (agonist$ or modulator$ or stimulat$ or stimulant$ or activat$)).tw.
8. (thiazolidinedione$ or glitazone$ or pioglitazone or rosiglitazone or troglitazone or netoglitazone or rivoglitazone or ciglitazone or balaglitazone or darglitazone or edaglitazone or englitazone or lobeglitazone).tw.
9. 7 or 8
10. 6 and 9
Appendix 6. ClinicalTrials.gov (www.clinicaltrials.gov)
( PPAR OR thiazolidinedione OR pioglitazone OR rosiglitazone OR glitazone OR troglitazone OR netoglitazone OR rivoglitazone OR ciglitazone OR balaglitazone OR darglitazone OR edaglitazone OR englitazone OR lobeglitazone ) AND ( Vertebral Artery OR Brain Infarction OR Intracranial Hemorrhages OR Carotid Artery Diseases OR Brain Ischemia OR Cerebral Hemorrhage OR Cerebrovascular Disorders OR Stroke ) [DISEASE]
Appendix 7. World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch)
rosiglitazone AND stroke OR glitazone AND stroke OR troglitazone AND stroke OR netoglitazone AND stroke OR rivoglitazone AND stroke OR ciglitazone AND stroke OR balaglitazone AND stroke OR darglitazone AND stroke OR edaglitazone AND stroke OR englitazone AND stroke OR lobeglitazone AND stroke
Phases are: ALL
Appendix 8. Chinese databases search strategy
1. 脑卒中 OR 脑血管病 OR 缺血性卒中 OR 脑梗塞 OR 脑梗死 OR 出血性卒中 OR 脑出血 OR 短暂性脑缺血发作
2. 主题词="脑梗死"[不加权:扩展] OR "脑血管障碍"[不加权:扩展] OR "脑出血"[不加权:扩展]
3. 中风 OR CVD OR 脑血管意外
4. 过氧化物酶体增殖物激活受体γ激动剂 OR PPRA受体γ激动剂 OR 罗格列酮 OR 吡格列酮 OR 胰岛素增敏剂 OR 格列酮 OR 噻唑烷二酮
5. (#3) OR (#2) OR (#1)
6. (#5) AND (#4) AND ( 临床试验[文献类型] OR 随机对照试验[文献类型])
Data and analyses
Comparison 1. Peroxisome proliferator‐activated receptor gamma agonists agonists versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Recurrence of stroke | 3 | 4979 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.44, 0.99] |
| 2 Reported adverse events | 3 | 1044 | Risk Difference (M‐H, Random, 95% CI) | 0.10 [‐0.08, 0.28] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
IRIS.
| Methods | A multicentre, double‐blind, placebo‐controlled clinical trial to test the effectiveness of pioglitazone for insulin resistant, non‐diabetic patients with a recent ischaemic stroke or TIA | |
| Participants | People aged at least 40 years with qualifying ischaemic stroke or TIA during the 6 months before randomisation, as well as insulin resistance, defined as a value of more than 3.0 on the homeostasis model assessment of insulin resistance index. 3876 participants were randomised. | |
| Interventions | Pioglitazone or matching placebo. The initial dose was 15 mg of pioglitazone daily or placebo. The dose was increased to 2 pills daily (30 mg of pioglitazone or placebo) at 4 weeks and to 3 pills daily (45 mg of pioglitazone or placebo) at 8 weeks. At 12 weeks, participants were started on 1 x 45 mg pioglitazone tablet or placebo tablet daily. | |
| Outcomes | Fatal or non‐fatal stroke; fatal or non‐fatal myocardial infarction; heart failure resulting in hospitalisation or death; death from any cause; diabetes; and cognitive decline | |
| Notes | Participants were contacted every 4 months with a median follow‐up of 4.8 years. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was performed using a random permuted block design with variable block sizes stratified by site. |
| Allocation concealment (selection bias) | Low risk | To conceal the allocation sequence, randomisation lists were kept only at the central pharmacy and the statistical centre. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The Investigational Drug Service prepared medication bottles, including starter supplies, which were stored at the research sites. At the baseline visit, a structured interview was administered and the starter bottle with the participant's assigned randomisation number was dispensed. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Reviewers were blinded to treatment allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | During a median follow‐up of 4.8 years, a total of 227 participants (5.9%) withdrew consent and 99 participants (2.6%) were lost to follow‐up. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes were reported. |
| Other bias | Unclear risk | This study was supported by the National Institute of Neurological Disorders and Stroke (NINDS) and monitored by an independent data and safety monitoring board appointed by NINDS. Pioglitazone and placebo were provided by Takeda Pharmaceuticals International. |
J‐SPIRIT.
| Methods | A multicentre, randomised, double‐blind, placebo‐controlled trial to test the effect of pioglitazone on the reduction of recurrent stroke in people with abnormal glucose metabolism and insulin resistance after ischaemic stroke | |
| Participants | People aged 35 to 85 years with symptomatic ischaemic stroke and no history of diabetes and no evidence of diabetes by initial blood test were included. 119 eligible people from 3 hospitals in Tokyo or neighbouring cities in Japan were randomised. |
|
| Interventions | Pioglitazone or matching placebo | |
| Outcomes | Recurrence of stroke; recurrence of ischaemic stroke | |
| Notes | Mean observation periods were 25 ± 19.9 months in the pioglitazone group and 30 ± 16 months in the control group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of random sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to judge |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to judge |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to judge |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge |
| Other bias | Unclear risk | Information about financial support was not provided. |
Kernan 2003.
| Methods | A randomised, double‐blind, placebo‐controlled trial to test the effect of pioglitazone compared with placebo for improving insulin sensitivity among non‐diabetic patients with a recent TIA or non‐disabling ischaemic stroke | |
| Participants | Non‐diabetic men and women aged > 45 years with TIA or non‐disabling ischaemic stroke were included. 20 eligible patients from 3 hospitals were randomised as 1:1 into the trial. | |
| Interventions | Pioglitazone 45 mg per day or placebo was given for 3 months. | |
| Outcomes | Mean proportional changes in insulin sensitivity; mean C‐reactive protein concentration; adverse events | |
| Notes | A repeated oral glucose tolerance test was done at the endpoint of the 3 months of therapy. The mean age was 66 years among participants assigned to pioglitazone and 67 years among participants assigned to placebo. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A master schedule of computer‐generated random treatment assignments (placebo or pioglitazone) was stored at the investigational pharmacy at Yale‐New Haven hospital. |
| Allocation concealment (selection bias) | Low risk | After screening for eligibility, a research associate contacted the investigational pharmacist, who assigned the participant to the next available treatment as specified by the master schedule. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were blinded to treatment assignment throughout the study. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Research staff and investigators were blinded to treatment assignment throughout the study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participant permanently discontinued the treatment. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes were reported. |
| Other bias | Low risk | The study was funded by an investigator‐initiated grant from Takeda Pharmaceuticals North America. Takeda had no involvement in data collection, data analysis, or report composition. By contract, Takeda could not suppress publication of this report. |
Marfella 2006.
| Methods | A randomised, placebo‐controlled trial | |
| Participants | 40 people who presented with symptoms of cerebral ischaemic attack were included and randomised as 1:1 into the trial. | |
| Interventions | Rosiglitazone 8 mg per day or placebo was given for 4 months. | |
| Outcomes | Ubiquitin‐proteasome activity | |
| Notes | We did not include 38 people with asymptomatic carotid stenosis in this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of random sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to judge |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The specimens were analysed by an expert pathologist blinded to the participant's diagnosis. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participant in either group discontinued the treatment. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes were reported. |
| Other bias | Unclear risk | Information about financial support was not provided. |
PROactive.
| Methods | A multicentre, randomised, double‐blind, placebo‐controlled trial | |
| Participants | People aged 35 to 75 years with type 2 diabetes and a previous stroke (6 months before randomisation) were included. 984 eligible people were randomised into the trial, with 486 in the pioglitazone group and 498 in the placebo group. | |
| Interventions | Pioglitazone titration from 15 mg to 45 mg per day depending on tolerability or placebo was given until the first occurrence of any of the events described in the primary outcomes. The mean duration was 34.5 months. | |
| Outcomes | Primary outcomes: all‐cause mortality, non‐fatal myocardial infarction (including silent myocardial infarction), stroke, acute coronary syndrome, cardiac intervention (including coronary artery bypass graft surgery or percutaneous coronary intervention), leg revascularisation, and amputation above the ankle Secondary outcomes: all‐cause death, non‐fatal myocardial infarction or non‐fatal stroke; adverse events |
|
| Notes | We did not include data for participants without previous stroke. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of random sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to judge |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to judge |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 882/984 (90%) participants completed the final visit: 439/486 (90%) in the pioglitazone group and 443/498 (89%) in the placebo group. Intention‐to‐treat analysis was used. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes were reported. |
| Other bias | Unclear risk | This study was funded by Takeda Pharmaceuticals and Eli Lilly, and designed by the international steering committee, who also approved the protocol and amendments. The sponsors had 2 representatives on the international steering committee; the same 2 were also members of the executive committee. Data analysis, data interpretation, and writing of the report was done by the executive committee, with contributions from the international steering committee, the data and safety monitoring committee, and the endpoint adjudication committee. All the authors had full access to all the data in the study and had final responsibility for the decision to submit for publication. |
TIA: transient ischaemic attack
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| CIMT Trial | The intervention was not PPAR‐γ agonist. |
| Erdmann 2015 | The participants were not eligible. |
| Forst 2008 | There was no subgroup of stroke patients for whom separate results were available. |
| Hedblad 2007 | The participants were not eligible. |
| ISRCTN54951661 | The participants were not eligible. |
| Koshiyama 2001 | The participants were not eligible. |
| Lincoff 2014 | The participants were not eligible. |
| Meisner 2006 | The participants were not eligible. |
| NCT00879970 | There was no subgroup of stroke patients for whom separate results were available. |
| Schrieks 2018 | There was no placebo for comparison. |
| Sidhu 2004 | The participants were not eligible. |
| Tanaka 2015 | There was no placebo for comparison. |
| TART | The participants were not eligible. |
| TRIPOD | The participants were not eligible. |
| Varghese 2009 | The participants were not eligible. |
PPAR‐γ: peroxisome proliferator‐activated receptor gamma
Differences between protocol and review
Some of the subgroup and sensitivity analyses specified were not conducted due to insufficient data.
We added insulin sensitivity and ubiquitin‐proteasome activity in carotid plaques as secondary outcomes, which were not included in the protocol.
We calculated the overall effects using a random‐effects model regardless of the level of heterogeneity. If heterogeneity was 0%, then the results using a random‐effects model would be the same as the results from a fixed‐effect model.
Contributions of authors
Liu J and Wang L conceived and developed the review. Liu J was in charge of searching, identifying and assessing studies, data extraction and analyses, and writing the draft of the review. Wang L gave general advice on the review, identified and assessed studies, extracted data, and revised the draft. Liu J supervised the quality of the methodology and statistics. Liu J will be responsible for future review updates.
Declarations of interest
Jia Liu: none known. Lu‐Ning Wang: none known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
IRIS {published data only}
- Inzucchi SE, Viscoli CM, Young LH, Furie KL, Gorman M, Lovejoy AM, et al. Pioglitazone prevents diabetes in patients with insulin resistance and cerebrovascular disease. Diabetes Care 2016;39:1684‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kernan WN, Viscoli CM, Furie KL, Young LH, Inzucchi SE, Gorman M, et al. Pioglitazone after ischemic stroke or transient ischemic attack. New England Journal of Medicine 2016;374:1321‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viscoli CM, Brass LM, Carolei A, Conwit R, Ford GA, Furie KL, et al. Pioglitazone for secondary prevention after ischemic stroke and transient ischemic attack: rationale and design of the Insulin Resistance Intervention after Stroke Trial. American Heart Journal 2014;168:823‐9.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
J‐SPIRIT {published data only}
- Tanaka R, Okuma Y, Miyamoto N, Tanaka Y, Yamashiro K, Watada H, et al. Effects of pioglitazone in patients with impaired glucose tolerance after stroke; progress report from J‐SPIRIT study. International Journal of Stroke 2010;5:195 (Abst.PO10427). [Google Scholar]
- Tanaka R, Yamashiro K, Tanaka Y, Miyamoto N, Ueno Y, Watanabe M, et al. Effects of pioglitazone in patients with abnormal glucose metabolism after stroke. The J‐SPIRIT study. Stroke 2013;44:Abst.ATP416. [Google Scholar]
Kernan 2003 {published data only}
- Kernan WN, Inzucchi SE, Viscoli CM, Brass LM, Bravata DM, Shulman GI, et al. Pioglitazone improves insulin sensitivity among nondiabetic patients with a recent transient ischemic attack or ischemic stroke. Stroke 2003;34:1431‐6. [DOI] [PubMed] [Google Scholar]
Marfella 2006 {published data only}
- Marfella R, D'Amico M, Filippo C, Baldi A, Siniscalchi M, Sasso FC, et al. Increased activity of the ubiquitin‐proteasome system in patients with symptomatic carotid disease is associated with enhanced inflammation and may destabilize the atherosclerotic plaque: effects of rosiglitazone treatment. Journal of the American College of Cardiology 2006;47:2444‐55. [DOI] [PubMed] [Google Scholar]
PROactive {published data only}
- PROactive study shows reduced heart attacks and strokes in type 2 diabetics on pioglitazone HCI (Actos) therapy. Cardiovascular Journal of South Africa 2005; Vol. 16:286‐7. [PubMed]
- Charbonnel B, Dormandy J, Erdmann E, Massi‐Benedetti M, Skene A, on behalf of the PROactive Study Group. The Prospective Pioglitazone Clinical Trial in Macrovascular Events (PROactive). Diabetes Care 2004;27:1647‐53. [DOI] [PubMed] [Google Scholar]
- Dormandy JA, Betteridge DJ, Schernthaner G, Pirags V, Norgren L, on behalf of the PROactive investigators. Impact of peripheral arterial disease in patients with diabetes ‐ results from PROactive (PROactive 11). Atherosclerosis 2009;202:272‐81. [DOI] [PubMed] [Google Scholar]
- Dormandy JA, Charbonnel B, Eckland DJA, Erdmann E, Massi‐Benedetti M, Moules IK, et al. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet 2005;366:1279‐89. [DOI] [PubMed] [Google Scholar]
- Erdmann E, Dormandy J, Wilcox R, Massi‐Benedetti M, Charbonnel B. PROactive 07: Pioglitazone in the treatment of type 2 diabetes: results of the PROactive study. Vascular Health and Risk Management 2007;3:355‐70. [PMC free article] [PubMed] [Google Scholar]
- Erdmann E, Harding S, Lam H, Perez A. Ten‐year observational follow‐up of PROactive: a randomized cardiovascular outcomes trial evaluating pioglitazone in type 2 diabetes. Diabetes, Obesity and Metabolism 2016;18:266‐73. [DOI] [PubMed] [Google Scholar]
- Erdmann E, Spanheimer R, Charbonnel B. Pioglitazone and the risk of cardiovascular events in patients with type 2 diabetes receiving concomitant treatment with nitrates, renin‐angiotensin system blockers, or insulin: results from the PROactive study (PROactive 20). Journal of Diabetes 2010;2:212‐20. [DOI] [PubMed] [Google Scholar]
- Wilcox R, Bousser MG, Betteridge J, Schernthaner G, Pirags V, Kupfer S, et al. Effects of pioglitazone in patients with type 2 diabetes with or without previous stroke. Results from PROactive (PROspective pioglitAzone Clinical Trial In macroVascular Events 04). Stroke 2007;38:865‐73. [DOI] [PubMed] [Google Scholar]
- Wilcox R, Kupfer S, Erdmann E. Effects of pioglitazone on major adverse cardiovascular events in high‐risk patients with type 2 diabetes: results from PROspective pioglitAzone Clinical Trial In macro Vascular Events (PROactive 10). American Heart Journal 2008;155:712‐7. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
CIMT Trial {published data only}
- Lundby Christensen L, Almdal T, Boesgaard T, Breum L, Dunn E, Gade‐Rasmussen B, et al. Study rationale and design of the CIMT trial: the Copenhagen Insulin and Metformin Therapy trial. Diabetes, Obesity and Metabolism 2009;11:315‐22. [DOI] [PubMed] [Google Scholar]
Erdmann 2015 {published data only}
- Erdmann E, Califf R, Gerstein HC, Malmberg K, Ruilope L, Schwartz GG, et al. Effects of the dual peroxisome proliferator‐activated receptor activator aleglitazar in patients with type 2 diabetes mellitus or prediabetes. American Heart Journal 2015;170:117‐22. [DOI] [PubMed] [Google Scholar]
Forst 2008 {published data only}
- Forst T, Wilhelm B, Pfützner A, Fuchs W, Lehmann U, Schaper F, et al. Investigation of the vascular and pleiotropic effects of atorvastatin and pioglitazone in a population at high cardiovascular risk. Diabetes and Vascular Disease Research 2008;5:298‐303. [DOI] [PubMed] [Google Scholar]
Hedblad 2007 {published data only}
- Hedblad B, Zambanini A, Nilsson P, Janzon L, Berglund G. Rosiglitazone and carotid IMT progression rate in a mixed cohort of patients with type 2 diabetes and the insulin resistance syndrome: main results from the Rosiglitazone Atherosclerosis Study. Journal of Internal Medicine 2007;261:293‐305. [DOI] [PubMed] [Google Scholar]
ISRCTN54951661 {unpublished data only}
- ISRCTN54951661. A 52 week double blind randomized controlled trial comparing the effect of rosiglitazone versus placebo on the prevention of progression of atherosclerosis in high risk patients without diabetes. http://www.isrctn.com/ISRCTN54951661 (accessed May 2017).
Koshiyama 2001 {published data only}
- Koshiyama H, Shimono D, Kuwamura N, Minamikawa J, Nakamura Y. Inhibitory effect of pioglitazone on carotid arterial wall thickness in type 2 diabetes. Journal of Clinical Endocrinology and Metabolism 2001;86:3452‐6. [DOI] [PubMed] [Google Scholar]
Lincoff 2014 {published data only}
- Lincoff AM, Tardif JC, Schwartz GG, Nicholls SJ, Rydén L, Neal B, et al. Effect of aleglitazar on cardiovascular outcomes after acute coronary syndrome in patients with type 2 diabetes mellitus: the AleCardio randomized clinical trial. JAMA 2014;311:1515‐25. [DOI] [PubMed] [Google Scholar]
Meisner 2006 {published data only}
- Meisner F, Walcher D, Gizard F, Kapfer X, Huber R, Noak A, et al. Effect of rosiglitazone treatment on plaque inflammation and collagen content in nondiabetic patients: data from a randomized placebo‐controlled trial. Arteriosclerosis Thrombosis and Vascular Biology 2006;26:845‐50. [DOI] [PubMed] [Google Scholar]
NCT00879970 {published data only}
- NCT00879970. Thiazolidinedione intervention with vitamin D evaluation (TIDE). https://clinicaltrials.gov/ct2/show/NCT00879970 (accessed May 2017).
Schrieks 2018 {published data only}
- Schrieks IC, Nozza A, Stähli BE, Buse JB, Henry RR, Malmberg K, et al. Adiponectin, free fatty acids, and cardiovascular outcomes in patients with type 2 diabetes and acute coronary syndrome. Diabetes Care 2018;41:1792‐800. [DOI] [PubMed] [Google Scholar]
Sidhu 2004 {published data only}
- Sidhu JS, Kaposzta Z, Markus HS, Kaski JC. Effect of rosiglitazone on common carotid intima‐media thickness progression in coronary artery disease patients with diabetes mellitus. Arteriosclerosis Thrombosis and Vascular Biology 2004;24:930‐4. [DOI] [PubMed] [Google Scholar]
Tanaka 2015 {published data only}
- Tanaka R, Yamashiro K, Okuma Y, Shimura H, Nakamura S, Ueno Y, et al. Effects of pioglitazone for secondary stroke prevention in patients with impaired glucose tolerance and newly diagnosed diabetes: the J‐SPIRIT Study. Journal of Atherosclerosis and Thrombosis 2015;22:1305‐16. [DOI] [PubMed] [Google Scholar]
TART {published data only}
- Hodis HN, Mack WJ, Zheng L, Li Y, Torres M, Sevilla D, et al. Effect of peroxisome proliferator‐activated receptor gamma agonist treatment on subclinical atherosclerosis in patients with insulin‐requiring type 2 diabetes. Diabetes Care 2006;29:1545‐53. [DOI] [PubMed] [Google Scholar]
- Karim R, Buchanan TA, Hodis HN, Li Y, Mack WJ. The association of smoking and subclinical atherosclerosis in type 2 diabetes: modification by duration of diabetes. Diabetic Medicine 2005;22:81‐7. [DOI] [PubMed] [Google Scholar]
- Zheng L, Buchanan TA, Hodis HN, Li Y, Torres M, Mack WJ. Time from diagnosis of type 2 diabetes to initiation of insulin therapy is related to carotid artery intima‐media thickness. Atherosclerosis 2003;170:293‐9. [DOI] [PubMed] [Google Scholar]
- Zheng L, Hodis HN, Buchanan TA, Li Y, Mack WJ. Effect of antihypertensive therapy on progression of carotid intima‐media thickness in patients with type 2 diabetes mellitus. American Journal of Cardiology 2007;99:956‐60. [DOI] [PubMed] [Google Scholar]
TRIPOD {published data only}
- Azen SP, Peters RK, Berkowitz K, Kjos S, Xiang A, Buchanan TA. TRIPOD (TRoglitazone In the Prevention Of Diabetes): a randomized, placebo‐controlled trial of troglitazone in women with prior gestational diabetes mellitus. Controlled Clinical Trials 1998;19:217‐31. [DOI] [PubMed] [Google Scholar]
- Xiang AH, Hodis HN, Kawakubo M, Peters RK, Kjos SL, Marroquin A, et al. Effect of pioglitazone on progression of subclinical atherosclerosis in non‐diabetic premenopausal Hispanic women with prior gestational diabetes. Atherosclerosis 2008;199:207‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang AH, Peters RK, Kjos SL, Ochoa C, Marroquin A, Goico J, et al. Effect of thiazolidinedione treatment on progression of subclinical atherosclerosis in premenopausal women at high risk for type 2 diabetes. Journal of Clinical Endocrinology and Metabolism 2005;90:1986‐91. [DOI] [PubMed] [Google Scholar]
Varghese 2009 {published data only}
- Varghese A, Yee MS, Chan CF, Crowe LA, Keenan NG, Johnston DG, et al. Effect of rosiglitazone on progression of atherosclerosis: insights using 3D carotid cardiovascular magnetic resonance. Journal of Cardiovascular Magnetic Resonance 2009;11:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Collino 2010
- Collino M, Aragno M, Castiglia S, Miglio G, Tomasinelli C, Boccuzzi G, et al. Pioglitazone improves lipid and insulin levels in overweight rats on a high cholesterol and fructose diet by decreasing hepatic inflammation. British Journal of Pharmacology 2010;160:1892‐902. [DOI] [PMC free article] [PubMed] [Google Scholar]
Costa 2005
- Costa J, Ferro JM, Matias‐Guiu J, Alvarez‐Sabin J, Torres F. Triflusal for preventing serious vascular events in people at high risk. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD004296.pub2] [DOI] [PubMed] [Google Scholar]
Dasu 2009
- Dasu MR, Park S, Devaraj S, Jialal I. Pioglitazone inhibits toll‐like receptor expression and activity in human monocytes and db/db mice. Endocrinology 2009;150:3457‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
De Schryver 2007
- Schryver ELLM, Algra A, Gijn J. Dipyridamole for preventing stroke and other vascular events in patients with vascular disease. Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD001820.pub3] [DOI] [PubMed] [Google Scholar]
De Schryver 2012
- Schryver EL, Algra A, Kappelle LJ, Gijn J, Koudstaal PJ. Vitamin K antagonists versus antiplatelet therapy after transient ischaemic attack or minor ischaemic stroke of presumed arterial origin. Cochrane Database of Systematic Reviews 2012, Issue 9. [DOI: 10.1002/14651858.CD001342.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple graphical test. BMJ 1997;315:629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Els 2002
- Els T, Klisch J, Orszagh M, Hetzel A, Schulte‐Mönting J, Schumacher M, et al. Hyperglycemia in patients with focal cerebral ischemia after intravenous thrombolysis: influence on clinical outcome and infarct size. Cerebrovascular Diseases 2002;13:89‐94. [DOI] [PubMed] [Google Scholar]
Emerging Risk Factors Collaboration 2010
- Emerging Risk Factors Collaboration, Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta‐analysis of 102 prospective studies. Lancet 2010;375:2215‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fogg 2009
- Fogg C, Kasliwal R, Shakir SA. Risk management and outcomes of adverse events to pioglitazone in primary care in the UK: an observational study. Drug Safety 2009;32:229‐37. [DOI] [PubMed] [Google Scholar]
Goldstein 2006
- Goldstein LB, Adams R, Alberts MJ, Appel LJ, Brass LM, Bushnell CD, et al. Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council: cosponsored by the Atherosclerotic Peripheral Vascular Disease Interdisciplinary Working Group; Cardiovascular Nursing Council; Clinical Cardiology Council; Nutrition, Physical Activity, and Metabolism Council; and the Quality of Care and Outcomes Research Interdisciplinary Working Group: the American Academy of Neurology affirms the value of this guideline. Stroke 2006;37:1583‐633. [DOI] [PubMed] [Google Scholar]
Graham 2010
- Graham DJ, Ouellet‐Hellstrom R, MaCurdy TE, Ali F, Sholley C, Worrall C, et al. Risk of acute myocardial infarction, stroke, heart failure, and death in elderly Medicare patients treated with rosiglitazone or pioglitazone. JAMA 2010;304:411‐8. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Jørgensen 1997
- Jørgensen HS, Nakayama H, Reith J, Raaschou HO, Olsen TS. Stroke recurrence: predictors, severity, and prognosis. The Copenhagen Stroke Study. Neurology 1997;48:891‐5. [DOI] [PubMed] [Google Scholar]
Melikian 2009
- Melikian N, Seddon MD, Casadei B, Chowienczyk PJ, Shah AM. Neuronal nitric oxide synthase and human vascular regulation. Trends in Cardiovascular Medicine 2009;19:256‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mooradian 2002
- Mooradian AD, Chehade J, Thurman JE. The role of thiazolidinediones in the treatment of patients with type 2 diabetes mellitus. Treatments in Endocrinology 2002;1:13‐20. [DOI] [PubMed] [Google Scholar]
Nakamura 2007
- Nakamura T, Yamamoto E, Kataoka K, Yamashita T, Tokutomi Y, Dong YF, et al. Pioglitazone exerts protective effects against stroke in stroke‐prone spontaneously hypertensive rats, independently of blood pressure. Stroke 2007;38:3016‐22. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Sandercock 2009
- Sandercock PA, Gibson LM, Liu M. Anticoagulants for preventing recurrence following presumed non‐cardioembolic ischaemic stroke or transient ischaemic attack. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD000248.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Simon 2009
- Simon RP, Greenberg DA, Aminoff MJ. Stroke. Clinical Neurology. 7th Edition. New York: McGraw‐Hill, 2009:292‐327. [Google Scholar]
Sudlow 2009
- Sudlow CL, Mason G, Maurice JB, Wedderburn CJ, Hankey GJ. Thienopyridine derivatives versus aspirin for preventing stroke and other serious vascular events in high vascular risk patients. Cochrane Database of Systematic Reviews 2009, Issue 4. [DOI: 10.1002/14651858.CD001246.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2010
- World Health Organization. The atlas of heart disease and stroke. www.who.int/cardiovascular_diseases/resources/atlas/en (accessed 12 May 2013).
References to other published versions of this review
Liu 2013
- Liu J, Wang LN. Peroxisome proliferator‐activated receptor gamma agonists for preventing recurrent stroke and other vascular events in patients with stroke or transient ischaemic attack. Cochrane Database of Systematic Reviews 2013, Issue 8. [DOI: 10.1002/14651858.CD010693] [DOI] [Google Scholar]
Liu 2014
- Liu J, Wang LN. Peroxisome proliferator‐activated receptor gamma agonists for preventing recurrent stroke and other vascular events in patients with stroke or transient ischaemic attack. Cochrane Database of Systematic Reviews 2014, Issue 1. [DOI: 10.1002/14651858.CD010693.pub2] [DOI] [PubMed] [Google Scholar]
Liu 2015
- Liu J, Wang LN. Peroxisome proliferator‐activated receptor gamma agonists for preventing recurrent stroke and other vascular events in patients with stroke or transient ischaemic attack. Cochrane Database of Systematic Reviews 2015, Issue 10. [DOI: 10.1002/14651858.CD010693.pub3] [DOI] [PubMed] [Google Scholar]


