Abstract
Men who have sex with men (MSM) disproportionately experience childhood sexual abuse (CSA) compared to heterosexual men, often resulting in continued trauma related sequelae, including symptoms of Post-Traumatic Stress Disorder (PTSD) such as avoidance. The variability in trauma related sequelae may be associated with chronicity or duration of CSA. The relationship between duration of CSA and later PTSD symptom severity is not well understood, including the extent coping strategies account for these relationships. We used linear regression to examine these relationships and to assess the indirect effects of avoidance (behavioral disengagement and denial) and adaptive coping strategies on the relationship between CSA duration and adult PTSD symptom severity on a diverse sample included 290 MSM with a history of CSA. In adjusted models, CSA duration was significantly associated with adult PTSD symptom severity (standardized β =0.23, p <0.000) and with avoidance coping (standardized β = 0.19, p=0.002). Separating this out, behavioral disengagement was significantly associated with CSA duration (standardized β =0.20, p=0.001) but denial was not. In adjusted analyses assessing indirect effects, avoidance coping partially accounted for the relationship between CSA duration and total trauma symptom severity (standardized β reduced from 0.23 to 0.17; Sobel=2.90, p=0.004). Similarly, behavioral disengagement partially accounted for the association between CSA duration and total symptoms (standardized β reduced from 0.23 to 0.18; Sobel=2.68, p=0.007). Avoidance coping, and behavioral disengagement specifically, may play a role in the severity of PTSD symptoms experienced by MSM with CSA histories. This work emphasizes the need for clinicians to consider behavioral disengagement in understanding PTSD symptom severity among MSM with histories of CSA.
Keywords: trauma, coping, childhood sexual abuse, avoidance
Introduction
Experiencing childhood sexual abuse (CSA) increases risk for negative mental health outcomes that last into adulthood (Anda et al., 2006) and has been associated with anxiety, major depression, and posttraumatic stress disorder (PTSD; Neumann, Houskamp, Pollock, & Briere, 1996; Fergusson, Boden, & Horwood, 2008; Boroughs et al., 2015; Fergusson, McLeod, & Horwood, 2013) during childhood and adulthood. Rates of PTSD among children who have experienced sexual abuse are high, and are often comorbid with other mental disorders (Ackerman, Newton, McPherson, Jones, & Dykman, 1998; Boroughs et al., 2015; Deblinger, McLeer, Atkins, Ralphe, & Foa, 1989). Further, research suggests that children who have been sexually abused develop specific maladaptive coping patterns, including greater avoidance and dissociative symptoms than non-abused children, consistent with PTSD (Deblinger et al., 1989; Van Den Bosch, Verheul, Langeland, & Van Den Brink, 2003).
Compared to heterosexual men, men who have sex with men (MSM) report significantly higher rates of CSA, which is associated with psychological and behavioral ramifications throughout adulthood. Estimates of CSA among MSM ranges from 10–50%, compared to 7.9% of men in the general population (Lloyd & Operario, 2012; Pereda, Guilera, Forns, & Gómez-Benito, 2009). A review of the literature indicates that MSM with histories of abuse during childhood or assaults in adulthood display higher levels of psychological distress and greater endorsement of suicidal ideation and suicidal behavior compared to those without histories of violence (Arreola, Neilands, Pollack, Paul, & Catania, 2008), and these negative outcomes can pervade throughout the lifespan. Many MSM with histories of CSA report diagnostic levels of PTSD into adulthood, which the literature suggests is a predictor of sexual risk behaviors and substance use disorders (Boroughs et al., 2015; El-Bassel, Gilbert, Vinocur, Chang, & Wu, 2011; Reisner, Mimiaga, Safren, & Mayer, 2009). Further, CSA among MSM has been linked to sexual assault in adulthood (Pantalone, Horvath, Hart, Valentine, & Kaysen, 2015; Balsam, Lehavot, & Beadnell, 2011).
Research suggests that victims of CSA may utilize avoidance coping strategies, including behavioral disengagement and denial, to manage distress after the abuse, which may decrease in effectiveness in adulthood and lead to or perpetuate PTSD symptoms (Brewin & Holmes, 2003; Holahan & Moos, 1987; Roth & Cohen, 1986; Walsh, Fortier, & Dilillo, 2010). While avoidance coping strategies frequently appear to be correlated with adverse long-term mental health outcomes, such as psychological distress, among adults with a history of CSA and related PTSD symptoms, there are inconsistencies in the literature (e.g., Brand & Alexander, 2003; Cantón-Cortés & Cantón, 2010; Hébert, Tremblay, Parent, Daignault, & Piché, 2006; Leitenberg, Greenwald, & Cado, 1992; Steel, Sanna, Hammond, Whipple, & Cross, 2004). Some evidence suggests that avoidant coping, including experiential avoidance and denial, mediate the relationship between CSA-related PTSD symptoms and emotional distress in adults (Whiffen & MacIntosh, 2005; Shapiro & Levendosky, 1999; Rosenthal, Rasmussen Hall, Palm, Batten, & Follette, 2005). Others have unexpectedly found that distancing, or avoidance, coping was associated with less social dysfunction and among adolescents, while more approach oriented coping was associated with increased sexual concerns (Brand & Alexander, 2003; Daigneault, Hébert, & Tourigny, 2006). Still others have found no relationship between avoidance and adaptive coping and behavioral and interpersonal functioning in survivors of CSA (Cantón-Cortés & Cantón, 2010; Chaffin, Wherry, & Dykman, 1997; Filipas & Ullman, 2006; Hébert et al., 2006; Shapiro & Levendosky, 1999; Tremblay, Hébert, & Piché, 1999; Wright, Crawford, & Sebastian, 2007). The variability in findings indicate that healthy recovery from CSA-related PTSD symptoms may involve a more nuanced understanding of the relationships between CSA and avoidance coping strategies (Phanichrat & Townshend, 2010).
In addition to avoidance coping, adaptive coping strategies including emotion-oriented and problem-oriented coping strategies (e.g., acceptance, religion, active coping, etc.) have been identified as influencing trajectories of recovery and can be a critical component in long-term functioning in adults with histories of CSA. Early trauma, such as CSA, is thought to disrupt adaptive coping mechanisms, making it difficult to recover from traumatic experiences, potentially resulting in greater PTSD symptom severity throughout the lifespan. In contrast to avoidance coping, which has been linked to greater PTSD symptoms (Filipas & Ullman, 2006; Huang, Zhang, Momartin, Huang, & Zhao, 2008; Johnson, Sheahan, & Chard, 2003; Ullman & Filipas, 2005; Ullman & Peter-Hagene, 2014), adaptive coping following CSA may help to manage negative thoughts and emotions associated with CSA-related PTSD symptoms, thereby reducing distress (Walsh et al., 2010). The literature also indicates that adaptive versus avoidance coping strategies evolve over time among adult survivors of CSA, and are differentially associated with long-term psychological functioning (Walsh et al., 2010).
However, the extent that specific coping strategies account for the relationship between varying durations of CSA and later overall PTSD symptom severity, as well as specific PTSD symptom clusters, is not well understood among MSM, a population disproportionately affected by CSA. The exploration of indirect relationships between CSA duration and adult psychological distress, including overall PTSD symptom severity and symptom clusters, may assist us in better understanding the mechanisms at play to more effectively develop strategies to cope with CSA experiences and related psychological distress, and ultimately to encourage resilience in survivors of CSA (Walsh et al., 2010). This study examines the relationships between duration of CSA, severity of adult PTSD symptoms (including specific PTSD symptom clusters), and avoidance and adaptive coping strategies among MSM who endorsed CSA.
Method
Participants
Data from 290 HIV-uninfected MSM with histories of CSA were collected as part of a comprehensive psychiatric baseline assessment from a multi-site randomized clinical trial aimed at reducing sexual risk behaviors associated with HIV in Boston, MA and Miami, FL from 2011–2016 (Batchelder et al., 2017; Boroughs et al., 2015). Of the 827 individuals who completed phone screens across both sites, 421 were deemed eligible, and 290 completed the assessment used in the presented analyses. All participants reported more than one episode of unprotected anal sex or vaginal intercourse within the past 3 months and a history of CSA before age 17. The average age of participants was 38, SD=12 (range 18–67). The sample self-identified as 68% White, 22% Black or African American, and 10% other. Twenty-nine percent of the sample identified as Latino. One quarter of the sample reported having up to a high school education, 36% some college, 24% some graduate school, and 13% reported completing a graduate degree.
Procedures
recruitment.
Participants were recruited through advertising and via outreach to bars, clubs, cruising areas, community venues, and social media. To protect individuals’ privacy and minimize stigma associated with endorsing childhood sexual abuse, recruitment efforts were combined with other ongoing behavioral and biomedical HIV prevention studies and health promotion initiatives.
study procedure.
Prospective participants were screened by trained clinical staff using a structured questionnaire. Enrollment criteria included: 1) identifying as a cisgender birth sex males who have sex with adult men; 2) endorsing sexual contact before 13 years of age with a person 5 or more years older, or sexual contact between 13–16 years of age with a person 10 years older or any age if threat of force or harm; 3) reporting more than one episode of unprotected anal or vaginal intercourse within the past three months; and 4) being HIV uninfected. HIV-negative status was confirmed via rapid testing. Participants were excluded if all episodes of unprotected anal or vaginal intercourse occurred with a single, primary, HIV-negative partner. All participants completed a comprehensive baseline assessment that included HIV and other STI testing, a psychiatric evaluation, and computer-based psychosocial assessments. Given the substantial evidence indicating participants are more likely to disclose sensitive information via computer questionnaire compared to a face-to-face interview, computer-based assessment was used to obtain and confirm verbally reported information (Des Jarlais et al., 1999; Metzger et al., 2000; Millstein, 1987; Navaline et al., 1994; O’Reilly, Hubbard, Lessler, Biemer, & Turner, 1994; Turner et al., 1998; Wilson, Genco, & Yager, 1985). All procedures were IRB approved.
Measures
demographics.
Participants self-reported age, race, ethnicity, educational attainment, income, and sexual orientation. Age was treated as continuous. We disaggregated race into White, Black, and other categories for analyses. Ethnicity was a dichotomous variable: Latino versus non-Latino. Education was disaggregated into 4 categories based on distribution. These categories were: some high school- high school diploma or GED, some college, college degree (BA or BS)-some graduate school, and graduate degree.
assessment of childhood sexual abuse.
Childhood sexual abuse (CSA) was assessed through a clinician-administered interview adapted from an assessment of sexual abuse used with a variety of medical populations (Leserman et al., 1997; Leserman, Li, Drossman, & Hu, 1998), including people living with HIV (Lesserman, Ironson, & O’Cleirigh, 2006). Unwanted sexual contact was assessed using an adaptation from earlier research (Kilpatrick, 1992; Leserman, 2005). The interview included 20 closed-ended standardized questions predominately requiring yes/no answers. CSA was assessed across two age ranges: 0 through 12 years old and 13 through 16 years old. CSA in the younger age range included any unwanted sexual contact reported with someone 5 or more years older. In the older age range, CSA included any sexual contact with someone 10 years older or with someone of any age if there was threat of force or harm. CSA was indicated if any of the following occurred: genital touching, being touched, or penetrative intercourse (i.e., oral or anal penetration). CSA duration was defined as the time in years from the first episode to the last episode of CSA prior to age 17 and was calculated as age at the last reported episode minus age of the first reported episode, plus one. For example, if a participant reported his first CSA episode at 5 years old and the last episode at 10 years old, his CSA duration would be 6 years (inclusive of age 5 through age 10 years old). Additionally, frequency of CSA was asked (0–15+) episodes before 13 years old and between 13 and 16 years old. We created a variable using these two questions to estimate frequency of CSA.
coping strategies.
Coping strategies were assessed using the Brief COPE (Carver, 1997), a 28 item scale that assesses cognitive and behavioral coping strategies (e.g., active coping, behavioral disengagement, and denial). Each coping strategy was assessed by the mean of two items which participants rate on a 4-point scale (0= I haven’t been doing this at all to 3=I’ve been doing this a lot). Avoidance coping mean score included two items assessing behavioral disengagement and two items assessing denial (Chronbach’s alpha = 0.72). Adaptive coping mean score included two items from each of the following subscales: active coping, instrumental support, planning, acceptance, emotional support, positive reframing, and religion (Chronbach’s alpha = 0.88).
post-traumatic stress disorder (PTSD) symptom clusters.
PTSD symptoms were assessed with the Davidson Trauma Scale (DTS; Davidson et al., 1997), a 17-item self-report questionnaire used to evaluate the frequency and severity of PTSD symptoms. Each question is rated on a scale from 0–8 (0–4 for frequency and 0–4 for severity), resulting in a total score range of 0–136. Scores ≥40 are consistent with the presence of PTSD (McDonald, Beckham, Morey, & Calhoun, 2009), which we confirmed in a clinical interview with staff in training for clinical psychology using the Structured Clinical Interview for DSM-IV (SCID, First, Spitzer, Gibbon, & Williams, 1996). The DTS has three subscales that map onto the diagnosis of PTSD: intrusive re-experiencing, avoidance, and hyperarousal.
Data Analysis
We conducted descriptive statistics on demographic variables (see Table 1) and confirmed duration of CSA, coping strategies, and overall PTSD symptoms as well as symptom clusters met assumptions for linear regression. We then conducted preliminary analyses to examine direct relationships between duration of CSA and all study related variables, using linear regression, controlling for age, race, ethnicity, and education which were selected a priori. We subsequently conducted models replacing duration of CSA with CSA frequency. We then followed Baron and Kenny’s (1986) guidelines to assess indirect relationships, consistent with mediation, including conducting a series of linear regression models controlling for chosen demographics (age, race, ethnicity, and education). We used Baron and Kenny’s (1986) rather than other methods given our prioritization of minimizing Type 1 error over increased power (Fritz, Taylor, & MacKinnon, 2012).
Table 1.
Sample Characteristics
| Variable | n=290 |
|---|---|
| Age (mean(SD)) | 37.95 (11.68) range 18–67 |
| Race | |
| White | 201 (67.9%) |
| Black | 66 (22.3%) |
| Other | 29 (9.8%) |
| Ethnicity | |
| Hispanic | 87 (29.4%) |
| Education | |
| ≤High school or GED | 73 (24.7%) |
| Some college | 106 (35.8%) |
| College degree (BA/BS)-Some graduate school | 71 (24.0%) |
| Graduate degree | 39 (13.2%) |
| Income | |
| ≤ $10,000 | 88 (29.7%) |
| $10,001-$20,000 | 66 (22.3%) |
| $20,001-$40,000 | 53 (17.9%) |
| ≥$40,001 | 83 (28.0%) |
| PTSD | |
| Total (mean(SD)) | 34.5 (26.2) range 0–122 |
| CSA Duration (mean(SD)) | 6.6 (4.7) years |
| Estimated CSA Frequency (mean(SD)) | 12.7 (10.0) events |
Results
Background Characteristics
A total of 290 men who endorsed having sex with men were included in the final sample (demographics described in Table 1). Sixty-seven percent (n=199) identified as gay or homosexual, 22% (n=64) identified as bisexual, 2% (n=7) identified as straight or heterosexual, 5% (n=14) reported being unsure, and another 2% identified as other when asked about sexual orientation. Participants’ mean (SD) score for avoidance coping was 0.77 (0.72), with behavioral disengagement being 0.82 (0.85) and denial being 0.72 (0.85). Participants’ mean (SD) score for adaptive coping was 1.52 (0.64). Total PTSD symptom mean (SD) score was 34.55 (26.22) with intrusive-re-experiencing subscale mean (SD) being 7.43 (7.78), avoidance subscale being 13.57 (11.94), and hyperarousal subscale being 13.63 (10.29). Thirty-nine percent of the samples’ Davidson Trauma Scale total score indicated likely PTSD (score of ≥40; McDonald, Beckham, Morey, & Calhoun, 2009).
Direct Relationships
We identified a significant bivariate relationship between CSA duration and avoidance coping in adjusted models (standardized β = 0.16, p=0.007; table 3, step 2 path a) but not between CSA duration and adaptive coping. The only significant direct association between CSA duration and a specific coping strategy in adjusted models was found between CSA duration and behavioral disengagement (standardized β =0.04, p=0.001). All other specific coping strategies were not significantly associated with CSA duration.
Table 3.
Summary of analyses examining indirect effects of duration of childhood sexual abuse on PTSD symptom profiles by coping strategies
| Predictor | Mediator | Outcome | Step 1 Path c |
Step 2 Path a |
Step 3 Path b |
Step 3 Path c’ |
Sobel |
|---|---|---|---|---|---|---|---|
| CSA duration | Avoidant Coping1 | Davidson Total | 0.23 p<0.000 |
0.19 p=0.002 |
0.29 p<0.000 |
0.17 p=0.004 |
2.90 p=0.004 |
| CSA duration | Avoidant Coping1 | Davidson Intrusive Re-experiencing | 0.22 p<0.000 |
0.19 p=0.002 |
0.22 p<0.000 |
0.12 p=0.001 |
2.54 p=0.011 |
| CSA duration | Avoidant Coping1 | Davidson Avoidance | 0.26 p<0.000 |
0.19 p=0.002 |
0.28 p<0.000 |
0.19 p=0.001 |
2.85 p=0.004 |
| CSA duration | Avoidant Coping1 | Davidson Hyperarousal | 0.13 p=0.036 |
0.19 p=0.002 |
0.29 p<0.000 |
0.05 p=0.410 |
2.86 p=0.004 |
| CSA duration | Behavioral Disengagement | Davidson Total | 0.23 p<0.000 |
0.20 p=0.001 |
0.24 p<0.000 |
0.18 p=0.002 |
2.68 p=0.007 |
| CSA duration | Behavioral Disengagement | Davidson Intrusive Re-experiencing | 0.22 p<0.000 |
0.20 p=0.001 |
0.14 p=0.019 |
0.19 p=0.002 |
1.96 p=0.051 |
| CSA duration | Behavioral Disengagement | Davidson Avoidance | 0.26 p<0.000 |
0.20 p=0.001 |
0.24 p<0.000 |
0.21 p<0.000 |
2.68 p=0.007 |
| CSA duration | Behavioral Disengagement | Davidson Hyperarousal | 0.13 p=0.036 |
0.20 p=0.001 |
0.26 p<0.000 |
0.07 p=0.237 |
2.73 p=0.006 |
Table shows standardized coefficients. All models control for age, race (white, black, other), ethnicity, and education.
Avoidant coping includes denial and behavioral disengagement.
We also identified a significant direct association in adjusted models between CSA duration and Davidson total PTSD score (standardized β =0.23, p<0.000). Additionally, we identified significant associations between CSA duration and all three Davidson symptom clusters in adjusted models: intrusive re-experiencing (standardized β =0.22, p<0.000), avoidance (standardized β =0.26, p<0.000), and hyperarousal (standardized β =0.13, p=0.036).
Indirect Relationships
To further understand the complex associations between CSA duration, avoidance coping, and PTSD symptoms we conducted analyses in which we examined if avoidance coping accounted for the relationship between CSA duration and PTSD symptom severity scores. As CSA duration was also associated with the three symptom clusters (intrusive re-experiencing, avoidance, and hyperarousal), we conducted four regression models with Davidson total and all three symptom clusters as outcome variables. As the only specific coping strategy significantly associated with CSA duration was behavioral disengagement, we subsequently conducted similar models, with behavioral disengagement replacing avoidance coping.
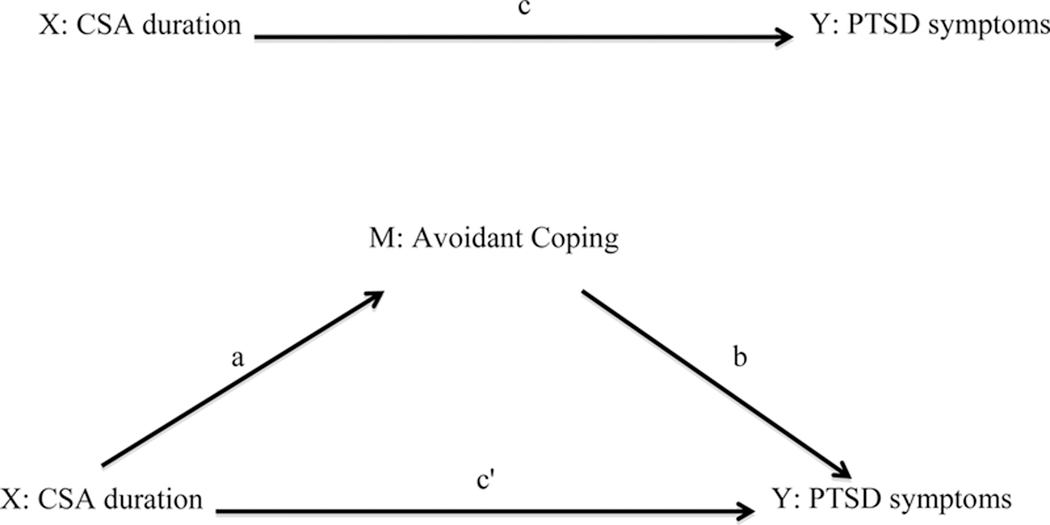
Table 3 summarizes the results for each step in assessing indirect relationships (see Figure 1). Step 1 estimates the c paths by examining the impact of CSA duration directly on PTSD scores. Step 2 estimates the a paths by examining the association of CSA duration on coping. Step 3 estimates the b paths by examining the association of coping scales on PTSD scores over and above effects of CSA duration. Step 4 estimates c’ path. This step differentiates whether the “mediator” partially or completely accounts for the relationship between independent (X) and dependent variable (Y) by examining the effects of CSA duration on PTSD scores. Specifically, if the relationship between the independent (CSA duration) and dependent variable (PTSD score) is reduced, but the direct relationship remains significant, when the “mediator” (type of coping) is included in the model the relationship would be considered partially mediated. In contrast, in full mediation the relationship between the independent (CSA duration) and dependent variable (PTSD score) is insignificant when the “mediator” (type of coping) is included as a predictor in the model. Steps 3 and 4 are tested in the same regression models. To assess the significance of the indirect effects (c-c’) we conducted Sobel tests (Fritz, Taylor, & MacKinnon, 2012; MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002; Sobel, 1982; see Table 3).
Figure 1.
Conceptual Model of Indirect Effects
As indicated in Table 3, avoidance coping partially accounted for the relationship between CSA duration and Davidson total (standardized β reduced from 0.23 to 0.17; Sobel=2.90, p=0.004), Davidson intrusive re-experiencing (standardized β reduced from 0.22 to 0.12; Sobel=2.54, p=0.011), and Davidson avoidance (standardized β reduced from 0.26 to 0.19; Sobel=2.85, p=0.004) in that the relationships between CSA duration and Davidson scores were smaller in the presence of avoidance coping. Avoidance coping fully mediated the relationship between CSA duration and Davidson hyperarousal (standardized β reduced from 0.13 to 0.05; Sobel=2.86, p=0.004), in that the direct relationship between CSA duration and Davidson hyperarousal was insignificant when avoidance coping was included in the model.
Similarly, behavioral disengagement partially accounted for the association between CSA duration and Davidson total (standardized β reduced from 0.23 to 0.18; Sobel=2.68, p=0.007) and Davidson avoidance (standardized β reduced from 0.26 to 0.21; Sobel=2.68, p=0.007). Behavioral disengagement only partially accounted for the relationship between CSA duration and Davidson intrusive re-experiencing (standardized β reduced from 0.22 to 0.19; Sobel=1.96, p=0.051). Resembling the effect of avoidance coping, behavioral disengagement fully accounted for the association between CSA duration and Davidson hyperarousal (standardized β reduced from 0.13 to 0.07; Sobel=2.73, p=0.006).
As post-hoc analyses, we completed similar models replacing CSA duration with estimated CSA frequency, based on the number of incidents of CSA endorsed by participants, rather than the span of time between the first and last incident. The significance of the relationships did not change in these models, compared to the reported models.
Discussion
This study is the first we are aware of to investigate the relationship between duration of CSA, avoidance coping strategies, and severity of adult PTSD symptoms in MSM with histories of CSA. Thirty-nine percent of this sample endorsed PTSD symptoms consistent with a PTSD diagnoses, confirmed with SCID interviewing. As expected, and consistent with existing theory (Walsh et al., 2010), our results indicate that longer duration of CSA was associated with greater avoidance coping, but CSA duration was not associated with adaptive coping. Behavioral disengagement, or the reduction in effortful engagement with a stressor, including potentially giving up on pursuit of stressor-related goals (Carver, Scheier, & Weintraub, 1989), was the only specific avoidance coping strategy associated with CSA duration. Consistent with findings in other populations (Filipas & Ullman, 2006; Huang, Zhang, Momartin, Huang, & Zhao, 2008; Johnson, Sheahan, & Chard, 2003; Ullman & Filipas, 2005; Ullman & Peter-Hagene, 2014), we identified relationships between longer CSA duration and higher current overall PTSD symptom severity, as well as all three symptom clusters: intrusive re-experiencing, avoidance, and hyperarousal.
When we examined whether avoidance coping strategies mediated the relationships between CSA duration and PTSD symptom severity, our results were more nuanced than, but consistent with, earlier investigations (e.g., Choi et al., 2015; Whiffen & MacIntosh, 2005; Shapiro & Levendosky, 1999). Specifically, avoidance coping fully accounted for the relationship between CSA and the hyperarousal symptoms in our sample of MSM. However, avoidance coping only partially accounted the relationship between CSA duration and overall PTSD symptom severity, as well as intrusive re-experiencing and avoidance symptom clusters. Together, these findings give us new insights into potential mechanisms of action that may lead to or perpetuate PTSD symptoms, including potentially varying relationships between coping strategies and PTSD symptom clusters among adult survivors of CSA, particularly MSM. Specifically, these findings indicate that among MSM with histories of CSA, an emphasis on engagement-focused coping, including behavioral activation, may be helpful in reducing adult PTSD symptomology. Longitudinal research is needed to investigate whether avoidance coping, particularly behavioral disengagement, mediates the relationship between CSA duration and PTSD symptom severity, both overall and specific symptom clusters. Additionally, behavioral disengagement, a type of avoidance coping that involves the reduction in engagement with a stressor or a stressor-related goal, was the only coping strategy directly associated with CSA duration. It fully mediated the relationship between CSA duration and hyperarousal and partially mediated the relationships between CSA duration and overall trauma symptom severity as well as intrusive re-experiencing and avoidance symptom clusters. These findings are consistent with evidence suggesting that victims of repeated CSA may initially utilize avoidance coping strategies to manage distress shortly after the abuse and continue through adulthood (Brewin & Holmes, 2003). However, this avoidance coping strategy may then decrease in effectiveness in adulthood thereby perpetuating PTSD symptoms (Brewin & Holmes, 2003).
Unlike previous work, we did not find that denial, the second component in the avoidance coping subscale along with behavioral disengagement, was associated with PTSD symptom severity (Whiffen & MacIntosh, 2005; Shapiro & Levendosky, 1999; Rosenthal, Rasmussen Hall, Palm, Batten, & Follette, 2005). Our finding demonstrating that behavioral disengagement mediated the relationship between CSA duration and PTSD symptom severity may be attributable to longer exposure to CSA. For example, prolonged effortful attempts to extricate oneself from abuse may lead to overgeneralization of behavioral disengagement as a coping strategy, and perpetuation of PTSD symptoms. Further, as behavioral disengagement involves a reduction in one’s effortful engagement with a stressor, potentially including the goal with which the stressor is interfering, it can be conceptualized as helplessness (Carver et al., 1989; Kaholokula et al., 2017). This maladaptive coping strategy offers temporary symptomatic relief; however, over time the increased passivity and effortful withdrawal may be detrimental to the recovery process.
Behavioral disengagement accounting for the relationship between CSA duration and PTSD symptom severity may be explained by a learned avoidance response. Those who experienced CSA over a longer duration may have learned to disengage or avoid, as they anticipated recurring negative outcomes, which may have resulted in a pattern that perpetuated the trauma-related symptoms (Brewin & Holmes, 2003). Notably, behavioral disengagement may have been adaptive in the context of CSA, including experiences a lack of control or power while potentially being dependent on the abuser (e.g., for food, shelter, etc.). Further, behavioral disengagement may be detrimental over time due to lack of active engagement in trauma recovery (Ullman & Peter-Hagene, 2014). Specifically, behavioral disengagement may fully account for the association between CSA duration and the hyperarousal symptom cluster due to the internalization of the experience of CSA being unavoidable, resulting in psychological distress eliciting heightened anxiety (Karakurt & Silver, 2014).
This work has several limitations and should therefore be considered an incremental contribution to the field. First, the sample included HIV-uninfected MSM who all reported recent sexual risk in addition to a history of CSA, limiting the generalizability of the findings. The measure of duration of CSA does not capture frequency or chronicity of abuse, rather the span of years between in the first and last episodes. To minimize triggering participants, participants were asked about a limited range of CSA episode frequency (up to “>15 times” before 13 years old and between 13 and 16 years old), resulting in a limited range of CSA episode frequency (1–30). Therefore, the frequency of CSA episode variable was truncated, which may not have captured the full range across participants. However, when we looked at the capped frequency measure, our findings did not significantly differ from analyses including the CSA duration variable (results not shown). Further, CSA was retrospectively reported and the data was collected cross-sectionally.
In conclusion, this is the first study we are aware of to demonstrate a relationship between duration of CSA and avoidance coping in a sample of MSM with histories of CSA, a population disproportionately affected by CSA. Further, in this sample CSA duration was associated with overall PTSD symptom severity, as well as all three symptom clusters: intrusive re-experiencing, avoidance, and hyperarousal. Finally, our findings emphasize the role of behavioral disengagement, possibly indicative of learned avoidance, in the relationship between CSA duration and PTSD symptom severity among MSM with histories of CSA. Ultimately, this work emphasizes the need for clinicians to consider the role avoidance coping, specifically behavioral disengagement, in understanding the relationship between duration or severity of CSA and current PTSD symptom severity among MSM living with histories of CSA.
Table 2.
Correlations between duration of childhood sexual abuse and coping strategies
| Coping Strategy | CSA Duration (0–16 years) |
|---|---|
| Avoidant Coping Composite | 0.204 (p=0.001) |
| Specific Coping Strategies | |
| Denial | 0.062 (p=0.297) |
| Behavioral Disengagement | 0.185 (p=0.002) |
Acknowledgments:
This work was support by a grant from the National Institute of Mental Health (R01MH095624, PI Dr. Conall O’Cleirigh) and by a grant from National Institute of Drug Abuse (K23DA043418, PI Dr. Abigail Batchelder).
References
- Ackerman PT, Newton JE, McPherson WB, Jones JG, & Dykman RA (1998). Prevalence of post traumatic stress disorder and other psychiatric diagnoses in three groups of abused children (sexual, physical, and both). Child Abuse & Neglect, 22(8), 759–774. [DOI] [PubMed] [Google Scholar]
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, … Giles WH (2006). The enduring effects of abuse and related adverse experiences in childhood: A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience, 256(3), 174–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arreola S, Neilands T, Pollack L, Paul J, & Catania J (2008). Childhood sexual experiences and adult health sequelae among gay and bisexual men: Defining childhood sexual abuse. Journal of Sex Research, 45(3), 246–252. [DOI] [PubMed] [Google Scholar]
- Balsam KF, Lehavot K, & Beadnell B (2011). Sexual revictimization and mental health: A comparison of lesbians, gay men, and heterosexual women. Journal of Interpersonal Violence, 26(9), 1798–1814. [DOI] [PubMed] [Google Scholar]
- Baron RM & Kenny D (1986). The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51, 1173–1182. [DOI] [PubMed] [Google Scholar]
- Batchelder AW, Ehlinger PP, Boroughs MS, Shipherd JC, Safren SA, Ironson GH, & O’Cleirigh C (2017). Psychological and behavioral moderators of the relationship between trauma severity and HIV transmission risk behavior among MSM with a history of childhood sexual abuse. Journal of Behavioral Medicine, 40(5), 794–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boroughs MS, Valentine SE, Ironson GH, Shipherd JC, Safren SA, Taylor SW, … O’Cleirigh C (2015). Complexity of childhood sexual abuse: predictors of current post-traumatic stress disorder, mood disorders, substance use, and sexual risk behavior among adult men who have sex with men. Archives of Sexual Behavior, 44(7), 1891–1902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand BL & Alexander PC (2003). Coping with incest: The relationship between recollections of childhood coping and adult functioning in female survivors of incest. Journal of Traumatic Stress, 16(3), 285–293. [DOI] [PubMed] [Google Scholar]
- Brewin CR & Holmes EA (2003). Psychological theories of posttraumatic stress disorder. Clinical Psychology Review, 23(3), 339–376. [DOI] [PubMed] [Google Scholar]
- Cantón-Cortés D & Cantón J (2010). Coping with child sexual abuse among college students and post-traumatic stress disorder: the role of continuity of abuse and relationship with the perpetrator. Child Abuse & Neglect, 34(7), 496–506. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, & Weintraub JK (1989). Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology, 56(2), 267–283. [DOI] [PubMed] [Google Scholar]
- Carver CS (1997). You want to measure coping but your protocol’ too long: Consider the brief cope. International Journal of Behavioral Medicine, 4(1), 92–100. [DOI] [PubMed] [Google Scholar]
- Chaffin M, Wherry JN, & Dykman R (1997). School age children’s coping with sexual abuse: Abuse stresses and symptoms associated with four coping strategies. Child Abuse & Neglect, 21(2), 227–240. [DOI] [PubMed] [Google Scholar]
- Choi KW, Sikkema KJ, Velloza J, Marais A, Jose C, Stein DJ, … Joska JA (2015). Maladaptive coping mediates the influence of childhood trauma on depression and PTSD among pregnant women in South Africa. Archives of Women’s Mental Health, 18(5), 731–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daigneault I, Hébert M, & Tourigny M (2006). Attributions and coping in sexually abused adolescents referred for group treatment. Journal of Child Sexual Abuse, 15(3), 35–59. [DOI] [PubMed] [Google Scholar]
- Davidson JR, Book SW, Colket JT, Tupler LA, Roth S, David D, … Feldman ME (1997). Assessment of a new self-rating scale for post-traumatic stress disorder. Psychological Medicine, 27(1), 153–160. [DOI] [PubMed] [Google Scholar]
- Deblinger E, McLeer SV, Atkins MS, Ralphe D, & Foa E (1989). Post-traumatic stress in sexually abused, physically abused, and nonabused children. Child Abuse & Neglect, 13(3), 403–408. [DOI] [PubMed] [Google Scholar]
- Des Jarlais DC, Paone D, Milliken J, Turner CF, Miller H, Gribble J, … Friedman SR (1999). Audio-computer interviewing to measure risk behaviour for HIV among injecting drug users: a quasi-randomised trial. Lancet (London, England), 353(9165), 1657–1661. [DOI] [PubMed] [Google Scholar]
- El-Bassel N, Gilbert L, Vinocur D, Chang M, & Wu E (2011). Posttraumatic stress disorder and HIV risk among poor, inner-city women receiving care in an emergency department. American Journal of Public Health, 101(1), 120–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, & Horwood LJ (2008). Exposure to childhood sexual and physical abuse and adjustment in early adulthood. Child Abuse & Neglect, 32(6), 607–619. [DOI] [PubMed] [Google Scholar]
- Filipas HH & Ullman SE (2006). Child sexual abuse, coping responses, self-blame, posttraumatic stress disorder, and adult sexual revictimization. Journal of Interpersonal Violence, 21(5), 652–672. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (1996). Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version (SCID-CV). Washington, D.C.: American Psychiatric Press, Inc. [Google Scholar]
- Fritz MS, Taylor AB, & MacKinnon DP (2012). Explanation of two anomalous results in statistical mediation analysis. Multivariate Behavioral Research, 47(1), 61–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hébert M, Tremblay C, Parent N, Daignault IV, & Piché C (2006). Correlates of behavioral outcomes in sexually abused children. Journal of Family Violence, 21(5), 287–299. [Google Scholar]
- Holahan CJ & Moos RH (1987). Personal and contextual determinants of coping strategies. Journal of Personality and Social Psychology, 52(5), 946–955. [DOI] [PubMed] [Google Scholar]
- Huang G, Zhang Y, Momartin S, Huang X, & Zhao L (2008). Child sexual abuse, coping strategies and lifetime posttraumatic stress disorder among female inmates. International Journal of Prisoner Health, 4(1), 54–63. [DOI] [PubMed] [Google Scholar]
- Johnson DM, Sheahan TC, & Chard KM (2003). Personality disorders, coping strategies, and posttraumatic stress disorder in women with histories of childhood sexual abuse. Journal of Child Sexual Abuse, 12(2), 19–39. [DOI] [PubMed] [Google Scholar]
- Kaholokula JK, Antonio MCK, Ing CKT, Hermosura A, Hall KE, Knight R, & Wills TA (2017). The effects of perceived racism on psychological distress mediated by venting and disengagement coping in Native Hawaiians. BMC Psychology, 5(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karakurt G, & Silver KE (2014). Therapy for childhood sexual abuse survivors using attachment and family systems theory orientations. The American Journal of Family Therapy, 42(1), 79–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick AC (1992). Long-range effects of child and adolescent sexual experiences: myths, mores, and menaces. Hillsdale, N.J: L. Erlbaum Associates. [Google Scholar]
- Leitenberg H, Greenwald E, & Cado S (1992). A retrospective study of long-term methods of coping with having been sexually abused during childhood. Child Abuse & Neglect, 16(3), 399–407. [DOI] [PubMed] [Google Scholar]
- Leserman J, Li Z, Drossman DA, Toomey TC, Nachman G, & Glogau L (1997). Impact of sexual and physical abuse dimensions on health status: development of an abuse severity measure. Psychosomatic Medicine, 59(2), 152–160. [DOI] [PubMed] [Google Scholar]
- Leserman J, Li Z, Drossman DA, & Hu YJ (1998). Selected symptoms associated with sexual and physical abuse history among female patients with gastrointestinal disorders: The impact on subsequent health care visits. Psychological Medicine, 28(2), 417–425. [DOI] [PubMed] [Google Scholar]
- Leserman J (2005). Sexual abuse history: Prevalence, health effects, mediators, and psychological treatment. Psychosomatic Medicine, 67, 906–915. [DOI] [PubMed] [Google Scholar]
- Leserman J, Ironson G, & O’Cleirigh C (2006). Preliminary results of a randomized controlled trial of an emotional disclosure intervention in patients with HIV. Presented at the Annual Meeting of the International Society of Behavioral Medicine, Bangkok, Thailand. [Google Scholar]
- Lloyd S & Operario D (2012). HIV risk among men who have sex with men who have experienced childhood sexual abuse: systematic review and meta-analysis. AIDS Education and Prevention: Official Publication of the International Society for AIDS Education, 24(3), 228–241. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, & Sheets V (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7(1), 83–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald SD, Beckham JC, Morey RA, & Calhoun PS (2009). The validity and diagnostic efficiency of the Davidson Trauma Scale in military veterans who have served since September 11th, 2001. Journal of Anxiety Disorders, 23(2), 247–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metzger DS, Koblin B, Turner C, Navaline H, Valenti F, Holte S, … Seage GR (2000). Randomized controlled trial of audio computer-assisted self-interviewing: utility and acceptability in longitudinal studies. HIVNET Vaccine Preparedness Study Protocol Team. American Journal of Epidemiology, 152(2), 99–106. [DOI] [PubMed] [Google Scholar]
- Millstein SG (1987). Acceptability and reliability of sensitive information collected via computer interview. Educational and Psychological Measurement, 47(2), 523–533. [Google Scholar]
- Navaline HA, Snider EC, Petro CJ, Tobin D, Metzger D, Alterman AI, & Woody GE (1994). Preparations for AIDS vaccine trials. An automated version of the Risk Assessment Battery (RAB): Enhancing the assessment of risk behaviors. AIDS Research and Human Retroviruses, 10 Suppl 2, S281–283. [PubMed] [Google Scholar]
- Neumann DA, Houskamp BM, Pollock VE, & Briere J (1996). The long-term sequelae of childhood sexual abuse in women: A meta-analytic review. Child Maltreatment, 1(1), 6–16. [Google Scholar]
- O’Reilly JM, Hubbard ML, Lessler JT, Biemer PP, & Turner CF (1994). Audio and video computer-assisted self interviewing: preliminary tests of new technologies for data collection. Journal of Official Statistics, 10(2), 197–214. [PMC free article] [PubMed] [Google Scholar]
- Pantalone DW, Horvath KJ, Hart TA, Valentine SE, & Kaysen DL (2015). Traumatic revictimization of men who have sex with men living with HIV/AIDS. Journal of Interpersonal Violence, 30(9), 1459–1477. [DOI] [PubMed] [Google Scholar]
- Pereda N, Guilera G, Forns M, & Gómez-Benito J (2009). The prevalence of child sexual abuse in community and student samples: a meta-analysis. Clinical Psychology Review, 29(4), 328–338. [DOI] [PubMed] [Google Scholar]
- Phanichrat T, & Townshend JM (2010). Coping strategies used by survivors of childhood sexual abuse on the journey to recovery. Journal of Child Sexual Abuse, 19(1), 62–78. [DOI] [PubMed] [Google Scholar]
- Reisner SL, Mimiaga MJ, Safren SA, & Mayer KH (2009). Stressful or traumatic life events, post-traumatic stress disorder (PTSD) symptoms, and HIV sexual risk taking among men who have sex with men. AIDS Care, 21(12), 1481–1489. [DOI] [PubMed] [Google Scholar]
- Rosenthal MZ, Rasmussen Hall ML, Palm KM, Batten SV, & Follette V (2005). Chronic avoidance helps explain the relationship between severity of childhood sexual abuse and psychological distress in adulthood. Journal of Child Sexual Abuse, 14(4), 25–41. [DOI] [PubMed] [Google Scholar]
- Roth S, & Cohen LJ (1986). Approach, avoidance, and coping with stress. The American Psychologist, 41(7), 813–819. [DOI] [PubMed] [Google Scholar]
- Shapiro DL, & Levendosky AA (1999). Adolescent survivors of childhood sexual abuse: the mediating role of attachment style and coping in psychological and interpersonal functioning. Child Abuse & Neglect, 23(11), 1175–1191. [DOI] [PubMed] [Google Scholar]
- Sobel ME (1982). Asymptotic confidence intervals for indirect effects in structural equation models. Sociological Methodology, 13, 290. 10.2307/270723 [DOI] [Google Scholar]
- Steel J, Sanna L, Hammond B, Whipple J, & Cross H (2004). Psychological sequelae of childhood sexual abuse: abuse-related characteristics, coping strategies, and attributional style. Child Abuse & Neglect, 28(7), 785–801. [DOI] [PubMed] [Google Scholar]
- Tremblay C, Hébert M, & Piché C (1999). Coping strategies and social support as mediators of consequences in child sexual abuse victims. Child Abuse & Neglect, 23(9), 929–945. [DOI] [PubMed] [Google Scholar]
- Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, & Sonenstein FL (1998). Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science (New York, N.Y.), 280(5365), 867–873. [DOI] [PubMed] [Google Scholar]
- Ullman SE, & Filipas HH (2005). Gender differences in social reactions to abuse disclosures, post-abuse coping, and PTSD of child sexual abuse survivors. Child Abuse & Neglect, 29(7), 767–782. [DOI] [PubMed] [Google Scholar]
- Ullman SE & Peter-Hagene L (2014). Social reactions to sexual assault disclosure, coping, perceived control, and PTSD symptoms in sexual assault victims: Social reactions and PTSD. Journal of Community Psychology, 42(4), 495–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh K, Fortier MA, & Dilillo D (2010). Adult coping with childhood sexual abuse: A theoretical and empirical review. Aggression and Violent Behavior, 15(1), 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiffen VE, & MacIntosh HB (2005). Mediators of the link between childhood sexual abuse and emotional distress: A Critical Review. Trauma, Violence, & Abuse, 6(1), 24–39. [DOI] [PubMed] [Google Scholar]
- Wilson FR, Genco KT, & Yager GG (1985). Assessing the equivalence of paper-and-pencil vs. computerized tests: Demonstration of a promising methodology. Computers in Human Behavior, 1(3–4), 265–275. [Google Scholar]
- Wright MO, Crawford E, & Sebastian K (2007). Positive resolution of childhood sexual abuse experiences: The role of coping, benefit-finding and meaning-making. Journal of Family Violence, 22(7), 597–608. [Google Scholar]