Hypertension remains the single largest modifiable contributor to risk for heart failure with preserved ejection fraction (HFpEF).1 The female versus male predominance of HFpEF remains incompletely understood, but may be related to sex differences in the cardiac response to chronic hypertension. Efforts to explore this possibility have been challenging, largely due to fact that HFpEF typically presents in older age – and older women compared to older men tend to carry a greater burden of certain co-morbid chronic disease traits (e.g. obesity, chronic kidney disease) that can also impact various aspects of cardiac structure and function. Therefore, to minimize potential confounding by comorbid disease, we investigated sex differences in the extent to which subclinical cardiac disease is evident by mid-life among persons whose chronic hypertension began in early life (i.e. hypertension starting at age <35 years).
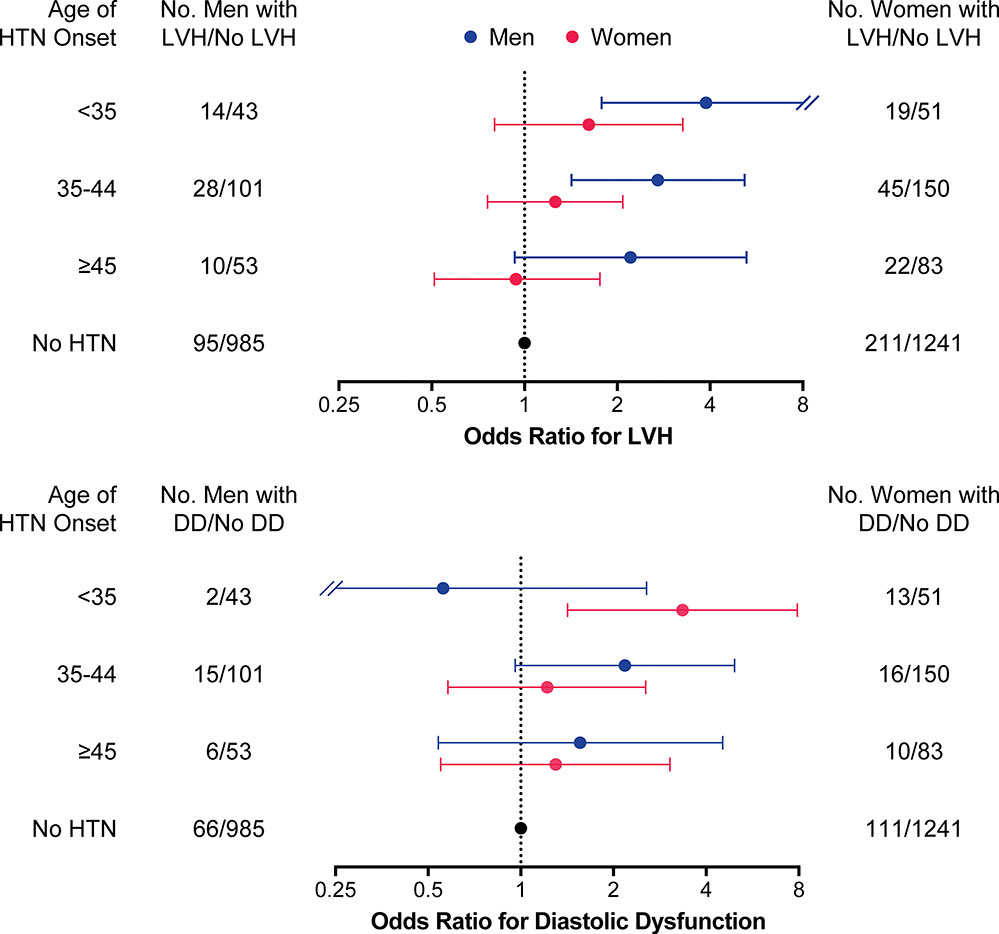
We studied N=2683 participants (mean age 50±4 years, 57% women) of the Coronary Artery Risk Development in Young Adults (CARDIA) cohort,2 who attended up to 8 serial examinations between 1985 and 2011, leading up to and including echocardiography at study cycle 8 (2010–2011), and did not have any key covariate data missing at attended exams. Blood pressure (BP) measurements at each exam were collected and calibrated using standardized methods, as previously described.2 We categorized participants according to the onset age at which hypertension criteria were met (BP ≥140/90 mmHg or use of antihypertensive medication): <35 years, 35–44 years, ≥45 years, or no hypertension.2 Echocardiographic LVH was defined as increased left ventricular mass index >115 g/m2 in males and >95 g/m2 in females;2 left ventricle diastolic dysfunction (DD) was defined as a ratio between peak velocity flow in early and late diastole of >2.0 or <0.8.2 Using multivariable logistic regression models (adjusting for age, sex, body mass index, total serum cholesterol, high-density cholesterol, smoking status, use of antihypertensive medication, and diabetes), we related hypertension onset age group with presence versus absence of LV trait (LVH or DD, prevalent in 16.6% and 9.0% overall). We observed that men with early-onset hypertension (starting at age <35 years) were much more likely to have LVH (odds ratio [OR] 3.88, 95% confidence interval [CI] 1.78–8.45] but not DD, when compared to men without hypertension (Figure). Conversely, women with early-onset hypertension were much more likely to have DD (OR 3.36, 95% CI 1.42–7.93) but not LVH, when compared to women without hypertension.
Figure. Early-Onset Hypertension and Cardiac Effects by Sex.
While there was an overall trend observed for greater prevalence of left ventricular hypertrophy (LVH) and diastolic dysfunction (DD) among individuals with earlier compared to later onset hypertension, the findings were more specific for greater LVH in men and greater DD for women with early-onset hypertension.
In older-aged cohorts, age-related concentric remodeling without elevation in LV mass (i.e. overt hypertrophy) is seen more commonly in women than men.3 Intriguingly, murine models have not only recapitulated these findings but also suggest that the female heart develops higher LV filling pressure in response to afterload resistance – especially when wall stress is higher than in males but also even when wall stress is similar.4 The current analysis expands from prior observational and experimental reports, and highlights a pronounced divergence between women and men in the cardiac effects that emerge in the setting of a chronic afterload stress that begins well before the menopausal transition in women. In particular, we observed a prominent association of early-onset hypertension with LV diastolic dysfunction (but not hypertrophy) in women, which stands in contrast to a prominent association of early-onset hypertension with increase in LV mass (but not diastolic dysfunction) in men. These results suggest that whereas the men tend to exhibit a cardiac remodeling response to hypertension stress that could serve to delay impaired function, women tend to exhibit a more limited cardiac remodeling response that renders susceptibility to dysfunction – particularly diastolic dysfunction, which is a known precursor to HFpEF. This sexual dimorphism could be related to the more prominent increases in arterial stiffness seen in aging women than aging men5 and, in turn, coupling of vascular-ventricular remodeling processes that may drive HFpEF pathophysiology. Further research is needed to validate and determine the mechanisms underlying our findings, as well as the extent to which they contribute to the consistently observed female predominance of incident HFpEF in later life.
Supplementary Material
ACKNOWLEDGEMENTS
This study was conducted using CARDIA Research Materials obtained from the NHLBI Biologic Specimen and Data Repository Information Coordinating Center and does not necessarily reflect the opinions or views of the cohort study or the NHLBI. We thank all the participants of the CARDIA study for their invaluable contributions to this work.
SOURCES OF FUNDING
This study was funded in part by an unrestricted research grant from Gilead Sciences, contracts from the National Heart, Lung and Blood Institutes N01-HV-68161, N01-HV-68162, N01-HV-68163, N01-HV-68164, grants U01-64829, U01-HL649141, U01-HL649241, R01-HL090957, R01-HL134168, R01-HL131532, R01-HL143227, and R03AG032631 from the National Institute on Aging, GCRC grant MO1-RR00425 from the National Center for Research Resources, the National Center for Advancing Translational Sciences Grant UL1TR000124, the Edythe L. Broad and the Constance Austin Women’s Heart Research Fellowships, Cedars-Sinai Medical Center, Los Angeles, California, the Barbra Streisand Women’s Cardiovascular Research and Education Program, Cedars-Sinai Medical Center, Los Angeles, The Society for Women’s Health Research (SWHR), Washington, D.C., the Linda Joy Pollin Women’s Heart Health Program, the Erika Glazer Women’s Heart Health Project, and the Adelson Family Foundation, Cedars-Sinai Medical Center, Los Angeles, California.
Footnotes
DISCLOSURES
The authors report no relevant conflicts of interest.
REFERENCES
- 1.Andersson C and Vasan RS. Epidemiology of heart failure with preserved ejection fraction. Heart Fail Clin. 2014;10:377–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suvila K, McCabe EL, Lehtonen A, Ebinger JE, Lima JAC, Cheng S and Niiranen TJ. Early Onset Hypertension Is Associated With Hypertensive End-Organ Damage Already by MidLife. Hypertension. 2019:HYPERTENSIONAHA11913069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cheng S, Xanthakis V, Sullivan LM, Lieb W, Massaro J, Aragam J, Benjamin EJ and Vasan RS. Correlates of echocardiographic indices of cardiac remodeling over the adult life course: longitudinal observations from the Framingham Heart Study. Circulation. 2010;122:570–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patrizio M and Marano G. Gender differences in cardiac hypertrophic remodeling. Ann Ist Super Sanita. 2016;52:223–9. [DOI] [PubMed] [Google Scholar]
- 5.Mitchell GF, Gudnason V, Launer LJ, Aspelund T and Harris TB. Hemodynamics of increased pulse pressure in older women in the community-based Age, Gene/Environment Susceptibility-Reykjavik Study. Hypertension. 2008;51:1123–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.