Abstract
Background and Purpose
It is essential to develop a reliable predictive serum biomarker for Parkinson's disease (PD). The accumulation of alpha-synuclein (αSyn) and up-regulated expression of Rab35 participate in the etiology of PD. The purpose of this investigation was to determine whether the combined assessment of serum αSyn and Rab35 is a useful predictive biomarker for PD.
Methods
Serum levels of αSyn or Rab35 were determined in serum samples from 59 sporadic PD patients, 19 progressive supranuclear palsy (PSP) patients, 20 multiple system atrophy (MSA) patients, and 60 normal controls (NC). Receiver operating characteristics (ROC) curves were calculated to determine the diagnostic accuracy of αSyn or/and Rab35 in discriminating PD patients from NC or atypical parkinsonian patients.
Results
The levels of αSyn and Rab35 were increased in PD patients. The serum level of Rab35 was positively correlated with that of αSyn in PD patients. Compared to analyzing αSyn or Rab35 alone, the combined analysis of αSyn and Rab35 produced a larger area under the ROC curve and performed better in discriminating PD patients from NC, MSA patients, or PSP patients. When age was dichotomized at 55, 60, 65, or 70 years, the combined assessment of αSyn and Rab35 for classifying PD was better in the group below the cutoff age than in the group above the cutoff age.
Conclusions
Combined assessment of serum αSyn and Rab35 is a better biomarker for discriminating PD patients from NC or atypical parkinsonian patients, and is a useful predictive biomarker for younger sporadic PD patients.
Keywords: Parkinson's disease, serum, biomarker, alpha-synuclein, Rab35
INTRODUCTION
The death of substantia nigra pars compacta (SNpc) dopaminergic neurons causes Parkinson's disease (PD), which is a common neurodegenerative disorder. PD has a prevalence of 1–2% in the elderly population,1 and its motor symptoms include resting tremor, bradykinesia, rigidity, and postural disturbance.2 Because clinical symptoms of PD fluctuate at the time of diagnosis, identifying reliable biomarkers is important for the early diagnosis and management of PD.
The pathological hallmark of PD is Lewy bodies that consist mainly of alpha-synuclein (αSyn).3 αSyn participates physiologically in the regulation of dopamine synthesis, synaptic plasticity, and neural differentiation.4 The accumulation or aggregation of αSyn contributes to the pathogenesis of PD.5 αSyn exists not only intracellularly but is also found in the blood and the CSF.6,7 Previous studies have showed that the level of αSyn, especially oligomeric αSyn, is elevated in plasma and CSF samples obtained from PD patients.6,8 αSyn is therefore considered the therapeutic target of PD and a potential biomarker for diagnosing PD.9
Ras-related protein (Rab protein) regulated by GTPase-activating proteins and guanine–nucleotide exchange factors are involved in signaling transduction, endocytic recycling, intracellular vesicular trafficking, and endosomal recycling.10 There are many lines of evidence indicating that αSyn aggregates directly bind with Rab proteins.11 Dysregulated expression of Rab GTPases is believed to participate in the etiology of PD.12 Loss-of-function mutations in Rab39B cause young-onset PD.13 The level of phosphorylated Rab10 is increased in neutrophils from PD patients and can be used as an enrichment biomarker for PD patients.14,15 It has been reported that Rab proteins interact with PD genes, including LRRK2, PINK1, and Parkin, and are involved in the pathogenic mechanism of PD.16,17 Endosomal Rab proteins including Rab5 and Rab7A participate in Parkin-mediated mitophagy.18 LRRK2 phosphorylates many Rab proteins, including Rab7L1, Rab8A, Rab10, Rab29, and Rab35.19,20,21,22,23 LRRK2 kinase regulates the propagation of αSyn by phosphorylating Rab35.20 Injecting the phosphomutant Rab35 into the substantia nigra causes the death of dopaminergic neurons.24 Moreover, Rab proteins regulate the homeostasis and aggregation of αSyn.11,25 Our previous study demonstrated that the expression of Rab35 increases the secretion and accumulation of (A53T) αSyn in dopaminergic neurons.26 Moreover, PD patients exhibit elevated levels of serum Rab35. The serum level of Rab35 might therefore be of clinical value in discriminating parkinsonism and might participate in the etiology of PD.26
While detecting a biomarker in CSF represents valuable information, it is invasive and expensive to obtain CSF samples from PD patients; in contrast, it is much more convenient and inexpensive to collect serum samples. The early diagnosis of PD using a serum biomarker would therefore facilitate early treatments of PD and help to improve the progression of PD.27 It is difficult to differentiate early-stage PD from atypical parkinsonism disorders, including progressive supranuclear palsy (PSP) and multiple system atrophy (MSA),28 which makes it essential to identify a reliable predictive serum marker for PD. Both the accumulation of αSyn and the up-regulated expression of Rab35 are believed to participate in the etiology of PD.5,26 Overexpression of Rab35 has been shown to cause neurotoxicity of dopaminergic cells by promoting the aggregation and secretion of αSyn,26 suggesting that the expression level of Rab35 is correlated with that of αSyn. The aim of the present study was to determine whether the combined assessment of serum αSyn and Rab35 is a useful predictive biomarker for PD.
METHODS
Human participants
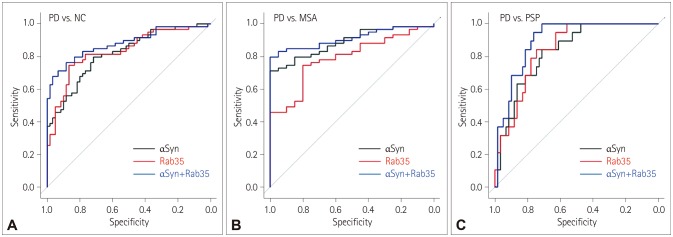
The Institutional Review Board of Chang Gung Memorial Hospital approved this investigation (IRB No. 201600663B0). All participants provided informed consent. The present study included 59 idiopathic PD patients, 19 PSP patients, 20 MSA patients, and 60 normal controls (NC). The clinical diagnoses of PD, MSA, and PSP were confirmed as described previously.26 The demographic characteristics of NC and patients with parkinsonian disorders are listed in Table 1.
Table 1. Demographic data and serum αSyn and Rab35 levels of patients and NC.
Data are n or mean±SEM values.
αSyn: alpha-synuclein, MSA: multiple system atrophy, NC: normal controls, PD: Parkinson's disease, PSP: progressive supranuclear palsy.
Serum specimens
Blood specimens were collected in Vacutainer tubes and coagulated at 25℃. Serum samples were obtained by centrifugation and then divided into aliquots.
ELISA determination of serum Rab35 level
The level of serum Rab35 was measured using the Rab35 ELISA kit (CUSABIO; Wuhan, China). Briefly, 100-µL serum samples were added to the wells of the microplate coated with anti-Rab35 antibody. The liquid was removed, and the wells were incubated with biotin antibody. Horseradish peroxidase (HRP)-avidin solution was then applied to the well, followed by the tetramethylbenzidine substrate. The absorbance was then measured at 450 nm, from which the level of serum Rab35 was calculated with the aid of a standard curve.
Quantification of serum αSyn level by IMR
The ultrasensitive immunomagnetic reduction (IMR) immunoassay was performed as described by Yang et al.29 In brief, Fe3O4 magnetic nanoparticles conjugated with anti-αSyn antibody were used to determine the interaction between αSyn and magnetic nanoparticles, which resulted in IMR. An IMR analyzer (XacPro-S, MagQu; Taipei, Taiwan) was used to detect the IMR signal.29
Statistical analysis
Statistical analysis was performed using SPSS version 23 (IBM Corp., Armonk, NY, USA) and GraphPad Prism software (GraphPad Software, San Diego, CA, USA). Data were summarized as mean±SEM error of the mean or 95% CI values. One-way ANOVA and the Tukey test were used to detect significant differences among multiple study groups. The correlation between two variables was analyzed based on Pearson correlation coefficients. Scatter plots with fitted regression lines are presented. A p value less than 0.05 was considered statistically significant. Receiver operating characteristics (ROC) curves were used to determine the diagnostic performance of serum αSyn or/and Rab35 in differentiating PD patients from NC or atypical parkinsonian patients. The accuracy of a biomarker in predicting PD was assessed by calculating the area under the ROC curve (AUC).
RESULTS
Serum samples from PD patients have increased levels of αSyn and Rab35
Sixty NC, 59 PD patients, 19 PSP patients, and 20 MSA patients were enrolled. Because atypical parkinsonism disorders, including MSA and PSP, are clinically indistinguishable from early-stage PD and are pathologically distinct, MSA and PSP patients were chosen as disease controls. The demographic characteristics of the study populations are summarized in Table 1.
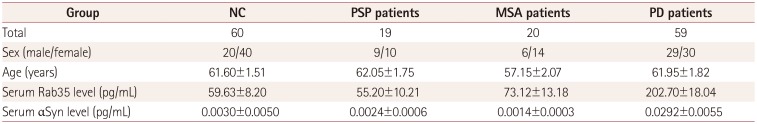
The ultrasensitive IMR immunoassay was performed to determine the serum level of αSyn. A quantitative ELISA assay was performed to calculate the level of serum Rab35. The serum levels of αSyn in NC and MSA, PSP, and PD patients were 0.0030±0.0050, 0.0014±0.0003, 0.0024±0.0006, and 0.0292±0.0055 pg/mL, respectively (Table 1, Fig. 1A); Table 1 and Fig. 1B indicate that the corresponding Rab35 levels were 59.63±8.20, 73.12±13.18, 55.20±10.21, and 202.70±18.04 pg/mL, respectively. Compared to NC, the serum levels of αSyn and Rab35 were elevated by 9.73-fold and 3.40-fold in serum samples from PD patients, respectively.
Fig. 1. The serum levels of αSyn and Rab35 are elevated in PD patients. The ultrasensitive IMR immunoassay and ELISA were used to analyze the levels of αSyn and Rab35 in serum samples, respectively, which were higher in PD patients than in NC, MSA patients, and PSP patients (A and B). Scatter plot of natural-logarithm values of the serum αSyn and Rab35 levels. The fitted regression line shows that there was a positive correlation between these levels (r=0.357, p=0.0055) in PD patients (C). Compared to age-matched controls, the serum levels of αSyn and Rab35 were not significantly altered in DIP patients (D and E). *p<0.001 compared with NC. αSyn: alpha-synuclein, DIP: drug-induced parkinsonism, IMR: immunomagnetic reduction, Ln: natural logarithm, MSA: multiple system atrophy, NC: normal controls, PD: Parkinson's disease, PSP: progressive supranuclear palsy.
The correlation between serum levels of αSyn and Rab35 was examined using the Pearson correlation coefficient. The scatter plot with fitted regression line in Fig. 1C indicates that there was a positive correlation between the serum levels of Rab35 and αSyn (r=0.357, p=0.0055) (Fig. 1C).
Drug-induced parkinsonism (DIP), which is the second-most-common parkinsonian disorder, is caused by the use of antidopaminergic drugs including antipsychotic medications.30 Parkinsonism phenotypes of DIP can be reversed by stopping such medication. It is difficult to distinguish PD patients from DIP patients based on their clinical phenotypes. The serum level of αSyn (0.0076±0.0026 pg/mL) in patients with antipsychotic DIP (age=42.80±4.82 years) did not differ significantly (p=0.5750) from that (0.0058±0.0018 pg/mL) in age-matched controls (age=43.50±4.78 years). The level of serum Rab35 in DIP patients (59.15±2.44 pg/mL) was similar to that in NC (56.37±1.64 pg/mL).
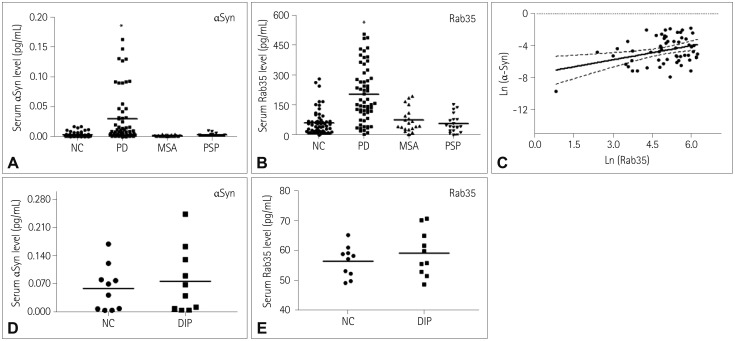
Our previous study showed that 6- or 9-month-old homozygous (D331Y) PLA2G6 knockin mice, which is an animal model of PARK14, exhibited the degeneration of SNpc dopaminergic neurons.31 Treating mice with 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) for 2 weeks resulted in a significant death rate of SNpc dopaminergic neurons.32 The level of serum αSyn or Rab35 was determined in three groups of mice: control, MPTP treatment for 1 week, and MPTP treatment for 2 weeks (Fig. 2A and B). Compared to control mice (αSyn=0.0758±0.0098 pg/mL; Rab35=84.96±1.63 pg/mL), the serum levels of αSyn and Rab35 were increased in mice treated with MPTP for 1 week (αSyn=0.1005±0.0063 pg/mL, p=0.059; Rab35=92.94±1.34 pg/mL, p=0.036) (Fig. 2A and B). Compared with the NC group (αSyn=0.0758±0.0098 pg/mL; Rab35=84.96±1.63 pg/mL), the serum levels of αSyn or Rab35 were significantly increased in mice treated with MPTP for 2 weeks (αSyn=0.1443±0.0157 pg/mL, p=0.0041; Rab35=113.3±6.28 pg/mL, p=0.014) (Fig. 2A and B). There was a positive correlation between the serum levels of αSyn and Rab35 in MPTP-treated mice (r=0.6713, p=0.0011) (Fig. 2C). The serum levels of Rab35 and αSyn in mice treated with MPTP for 2 weeks was higher than those in mice injected with MPTP for 1 week (Fig. 2A and B). Therefore, up-regulated serum levels of Rab35 and αSyn are correlated with the disease progression of MPTP-treated mice.
Fig. 2. The levels of serum αSyn and Rab35 are increased in PD mice models. Compared with control mice, the serum levels of αSyn and Rab35 were up-regulated in mice treated with MPTP for either 1 or 2 weeks (A and B). Scatter plot of natural-logarithm values of the serum αSyn and Rab35 levels. The fitted regression line shows that there was a positive correlation between these levels in MPTP-treated mice (r=0.671, p=0.0011) (C). The levels of serum αSyn and Rab35 were increased in 6M and 9M (D331Y) PLA2G6 knockin mice compared to 6M and 9M wild-type mice (D and E). Scatter plot with a fitted regression line demonstrating a positive correlation between these levels in (D331Y) PLA2G6 knockin mice (r=0.7438, p=0.0271) (F). *p<0.05, †p<0.01 compared with NC. 6M: six-month-old, 9M: nine-month-old, αSyn: alpha-synuclein, Ln: natural logarithm, MPTP: 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine, NC: normal controls, PD: Parkinson's disease, WT: wild-type.
The expression levels of Rab35 and αSyn were evaluated in serum samples of wild-type (WT) and mutant (D331Y) PLA2G6 knockin mice. Compared with age-matched WT mice (αSyn and Rab35 levels of 0.0782±0.0015 and 85.17±0.86 pg/mL at 6 months, respectively, and 0.0902±0.0116 and 86.10±2.04 pg/mL at 9 months), the serum levels of αSyn and Rab35 were up-regulated in 6-month-old (αSyn=0.6964±0.1601 pg/mL, p=0.0181; Rab35=96.05±4.33 pg/mL, p=0.0692) and 9-month-old (αSyn=1.135±0.1974 pg/mL, p=0.0061; Rab35=114.90±4.74 pg/mL, p=0.0051) mutant (D331Y) PLA2G6 knockin mice (Fig. 2D and E). In homozygous (D331Y) PLA2G6 mice there was a positive correlation between the serum levels of αSyn and Rab35 (r=0.7438, p=0.0271) (Fig. 2F). The serum levels of αSyn and Rab35 were higher in 9-month-old than in 6-month-old (D331Y) PLA2G6 knockin mice (Fig. 2D and E). The up-regulation of the expression levels of αSyn and Rab35 was therefore correlated with the disease progression of homozygous (D331Y) PLA2G6 knockin mice.
Combined assessment of serum αSyn and Rab35 is a better biomarker for discriminating PD patients from NC or patients with atypical parkinsonian disorders
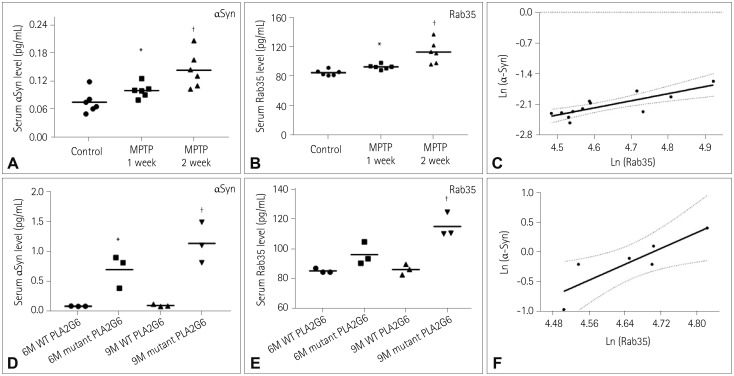
To explore the diagnostic application of serum αSyn and Rab35 levels in discriminating PD patients from NC or atypical parkinsonism disorders, the natural-logarithm values of these levels were analyzed using ROC curves. The area above the reference line in the ROC curve was >0.5, which suggested that the serum levels of αSyn and Rab35 may be used as a biomarker for the diagnosis of PD. Compared with the NC group, the AUCs for the serum levels of αSyn and Rab35 in PD patients were 0.8175 (95% CI=0.7429–0.8921) (Fig. 3A) and 0.8314 (95% CI=0.7569–0.9058) (Fig. 3A), respectively. Moreover, the AUC was higher for the combined assessment of serum αSyn and Rab35 in PD patients, at 0.8794 (95% CI=0.8161–0.9427) (Fig. 3A). This finding suggests that compared to analyzing serum αSyn or Rab35 alone, the combined assessment of serum αSyn and Rab35 has a better performance in discriminating PD patients from NC (Fig. 3A).
Fig. 3. The combined assessment of serum αSyn and Rab35 levels has a better accuracy in differentiating PD from NC and other parkinsonian disorders. ROC curves of serum αSyn (black line), serum Rab35 (red line), and combined assessment of serum αSyn and Rab35 (αSyn+Rab35, blue line) were examined in serum samples from NC and PD, MSA, and PSP patients. The AUCs for serum αSyn, serum Rab35, and the combined assessment of serum αSyn and Rab35 when comparing PD patients with NC were 0.8175 (95% CI=0.7429–0.8921), 0.8314 (95% CI=0.7569–0.9058), and 0.8794 (95% CI=0.8161–0.9427), respectively (A). The AUCs for serum αSyn, serum Rab35, and the combined assessment of serum αSyn and Rab35 when comparing PD and MSA patients were 0.8890 (95% CI=0.8191–0.9589), 0.7907 (95% CI=0.6870–0.8944), and 0.9110 (95% CI=0.8490–0.9731), respectively (B). The AUCs for serum αSyn, serum Rab35, and the combined assessment of serum αSyn and Rab35 when comparing PD and PSP patients were 0.8305 (95% CI=0.7362–0.9248), 0.8421 (95% CI=0.7548–0.9294), and 0.8983 (95% CI=0.8312–0.9655), respectively (C). αSyn: alpha-synuclein, AUC: area under the ROC curve, IMR: immunomagnetic reduction, MSA: multiple system atrophy, NC: normal controls, PD: Parkinson's disease, PSP: progressive supranuclear palsy, ROC: receiver operating characteristics.
When PD patients were compared with MSA patients, the AUCs for serum αSyn and Rab35 were 0.8890 (95% CI=0.8191–0.9589) and 0.7907 (95% CI=0.6870–0.8944), respectively (Fig. 3B). The AUC for the combined measurement of serum αSyn and Rab35 in PD patients was 0.9110 (95% CI=0.8490–0.9731) (Fig. 3B). Compared to PSP patients, the AUCs for serum αSyn and Rab35 in PD patients were 0.8305 (95% CI=0.7362–0.9248) and 0.8421 (95% CI=0.7548–0.9294), respectively (Fig. 3C). The AUC for the combined assessment of serum αSyn and Rab35 in PD patients was 0.8983 (95% CI=0.8312–0.9655) (Fig. 3C). All of these data suggest that the combined assessment of serum αSyn and Rab35 is a better biomarker for differentiating PD patients from atypical parkinsonian patients.
Combined assessment of serum αSyn and Rab35 is a predictive biomarker for younger sporadic PD patients
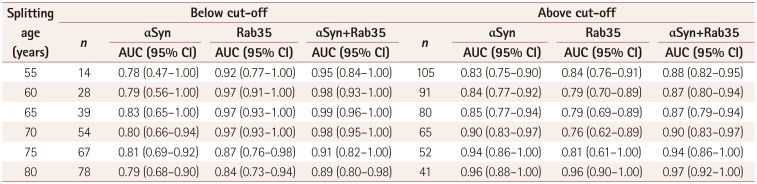
We further examined the diagnostic accuracy of using combined serum αSyn and Rab35 to differentiate PD from NC. One hundred and nineteen cases, including 50 NC and 59 sporadic PD patients, were dichotomized into pairs of groups by age (<55 and ≥55 years, <60 and ≥60 years, <65 and ≥65 years, <70 and ≥70 years, <75 and ≥75 years, and <80 and ≥80 years), and then the diagnostic accuracy of PD was analyzed by using the AUC in the pairs of cutoff age groups (Table 2). When the age cutoff was 55, 60, 65, or 70 years, the combined assessment of serum αSyn and Rab35 for classifying sporadic PD was better for the group below the cutoff age than for the group above the cutoff age (Table 2). The AUCs for combined αSyn and Rab35 in PD patients aged <55 and ≥55 years were 0.95 (95% CI=0.84–1.00) and 0.88 (95% CI=0.82–0.95), respectively; the corresponding values were 0.98 (95% CI=0.93–1.00) and 0.87 (95% CI=0.80–0.94) for PD patients aged <60 and ≥60 years, respectively, 0.99 (95% CI=0.96–1.00) and 0.87 (95% CI=0.79–0.94) for those aged <65 and ≥65 years, respectively, and 0.98 (95% CI=0.95–1.00) and 0.90 (95% CI=0.83–0.97) for those aged <70 and ≥70 years, respectively. These findings suggest that the combined assessment of serum αSyn and Rab35 is more accurate in predicting younger sporadic PD patients.
Table 2. Summary of AUC results when the age groups were dichotomized.
αSyn: alpha-synuclein, AUC: area under the receiver operating characteristics curve.
DISCUSSION
Patients do not display symptoms of PD before 70–80% of SNpc dopaminergic neurons have degenerated,33 which indicates that a reliable serum biomarker for the early detection of PD is urgently needed. Many potential serum biomarkers have been identified in PD patients. The level of serum uric acid is decreased in PD patients, and a high serum uric acid is correlated with a slower progression of PD.34 Serum levels of inflammatory cytokines and interleukins, including interleukin-2 (IL-2), IL-4, IL-6, IL-10, and interferon-gamma, are up-regulated in PD patients.35 The serum level of IL-6 is increased in PD patients and is correlated with the physical disability associated with PD.36 The serum level of tumor necrosis factor-alpha is up-regulated in PD patients 35. The serum level of insulin-like growth factor-1 is higher in PD patients than in NC.37 The serum level of lymphocyte activation gene-3 is increased in patients with PD.38 The difference in the serum level of neurofilament light chain is used to discriminate PD from atypical parkinsonian disorders.39 The level of serum CXCL12 is up-regulated in PD patients and can be used as a biomarker.40 Finally, an increased activity of β-galactosidase is observed in serum from PD patients.41
Rab proteins participate in membrane trafficking of neurons and are implicated in the pathogenic mechanisms of several neurodegenerative disorders.16 The Rab proteins Rab3 and Rab27B are found in neuronal synapses and regulate the exocytosis of synaptic vesicles,42 while Rab4, Rab8, Rab11, Rab17, and Rab39B regulate neurotransmitter trafficking and turnover,43,44,45 and Rab5 interacts with LRRK2 and is involved in the endocytosis of synaptic vesicles.46 It has been reported that dysfunction of membrane trafficking leads to neurodegeneration.16 Mutations in Rab proteins are likely to be involved in the neuronal death that occurs in neurodegenerative diseases.16 The loss of Rab39B function leads to early-onset PD.13 Expression of the phosphomutant Rab35 results in the loss of SNpc dopaminergic neurons.24 Moreover, Rab proteins could play a role in the etiology of PD by interacting with several PD genes, including the LRRK2, PINK1, and αSyn genes.47
Increased levels of αSyn and Rab35 are likely to participate in the etiology of PD.26 Consistent with the results of previous investigations,48 the present study has demonstrated that the level of serum αSyn is up-regulated in sporadic PD patients. As we reported previously,26 the level of serum Rab35 is also up-regulated in patients with PD. A particularly interesting aspect of our results is the suggestion that compared with measuring the serum level of αSyn or Rab35 alone, the combined assessment of serum αSyn and Rab35 has a better performance in discriminating PD patients from NC. Furthermore, compared to analyzing serum αSyn or Rab35 alone, the combined assessment of serum αSyn and Rab35 is more effective in differentiating PD patients from MSA or PSP patients. Therefore, our study provides evidence that the combined assessment of serum αSyn and Rab35 is a better biomarker for discriminating PD patients from NC or patients affected with atypical parkinsonian disorders.
The findings of this study indicate that in contrast to sporadic PD patients, the serum level of Rab35 or αSyn is not significantly altered in patients with DIP. It is difficult to distinguish PD and DIP by their clinical phenotypes.49 Our results suggest that the absence of an increased serum Rab35 or αSyn level can be used to differentiate DIP patients from sporadic PD patients.
Nonmotor symptoms of PD, such as olfactory dysfunction, REM sleep-behavior disorder, or autonomic malfunction, are believed to be symptomatic biomarkers and can be used to predict the prodromal stage of PD,50,51 However, the reported sensitivity of symptomatic markers has ranged widely, from 27.6% to 90%.52,53 SPECT, PET, and fMRI are neuroimaging techniques that have been used to diagnose early-stage PD.50,51,54 However, neuroimaging biomarkers for detecting PD are more expensive and time-consuming to acquire compared to obtaining serum samples from PD patients.54 In addition to detecting PD, altered serum levels of biomarkers could also be used differentiate younger sporadic PD patients from older sporadic PD patients, and be used for the early diagnosis of PD. The results from the present study demonstrate that when using an age cutoff of 55, 60, 65, or 70 years, the combined assessment of serum αSyn and Rab35 for predicting sporadic PD performs better for the group below the cutoff age than for the group above the cutoff age. Therefore, the present study is the first to provide evidence that the combined assessment of serum αSyn and Rab35 is a useful predictive biomarker for younger sporadic PD patients.
Acknowledgements
This work was supported by the Ministry of Science and Technology, Taiwan (grant MOST107-2320-B-182-036-MY3 to H.L.W. and grant MOST106-2314-B-182A-012-MY3 to C.C.C.) and the Chang Gung Medical Foundation (grants CMRPD1C0623, CRRPD1C0013, CMRPD180433, CMRPD1B0332, EMRPD1G0171, and CMRPD1H0281 to H.L.W., and grants CMRPG3F1823 and CMRPG3J0761 to C.C.C.).
Footnotes
- Conceptualization: Chin-Song Lu, Tu-Hsueh Yeh, Yi-Hsin Weng, Ying-Zu Huang, Rou-Shayn Chen, Yi-Chuan Cheng, Ching-Chi Chiu.
- Data curation: Hung-Li Wang, Yu-Ming Shen, Yu-Chuan Liu, Hsiu-Chen Chang, Ying-Ling Chen, Yu-Jie Chen, Yan-Wei Lin, Chia-Chen Hsu, Chi-Han Chiu.
- Formal analysis: Yu-Ming Shen.
- Funding acquisition: Hung-Li Wang, Ching-Chi Chiu.
- Investigation: Yu-Jie Chen, Yan-Wei Lin, Chia-Chen Hsu, Chi-Han Chiu, Ching-Chi Chiu.
- Methodology: Yi-Hsin Weng, Rou-Shayn Chen, Ying-Zu Huang, Yi-Chuan Cheng.
- Project administration: Hung-Li Wang, Chin-Song Lu, Tu-Hsueh Yeh, Ying-Zu Huang, Ching-Chi Chiu.
- Resources: Chin-Song Lu, Yi-Hsin Weng, Ying-Zu Huang, Rou Shayn Chen, Yu-Chuan Liu, Huang-Li Lin.
- Software: Yu-Ming Shen, Ching-Chi Chiu.
- Supervision: Chin-Song Lu, Tu-Hsueh Yeh, Yi-Hsin Weng, Rou-Shayn Chen, Ying-Zu Huang, Yi-Chuan Cheng, Ching-Chi Chiu.
- Validation: Hung-Li Wang, Ying-Ling Chen, Ching-Chi Chiu.
- Visualization: Hung-Li Wang, Yu-Ming Shen, Ching-Chi Chiu.
- Writing—original draft: Hung-Li Wang, Ching-Chi Chiu.
- Writing—review & editing: Chin-Song Lu, Yu-Ming Shen, Ying-Zu Huang, Ching-Chi Chiu.
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
References
- 1.De Lau LM, Breteler MM. Epidemiology of Parkinson's disease. Lancet Neurol. 2006;5:525–535. doi: 10.1016/S1474-4422(06)70471-9. [DOI] [PubMed] [Google Scholar]
- 2.Jankovic J. Parkinson's disease: clinical features and diagnosis. J Neurol Neurosurg Psychiatry. 2008;79:368–376. doi: 10.1136/jnnp.2007.131045. [DOI] [PubMed] [Google Scholar]
- 3.Spillantini MG, Schmidt ML, Lee VM, Trojanowski JQ, Jakes R, Goedert M. Alpha-synuclein in Lewy bodies. Nature. 1997;388:839–840. doi: 10.1038/42166. [DOI] [PubMed] [Google Scholar]
- 4.Burré J. The synaptic function of α-synuclein. J Parkinsons Dis. 2015;5:699–713. doi: 10.3233/JPD-150642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karpinar DP, Balija MB, Kügler S, Opazo F, Rezaei-Ghaleh N, Wender N, et al. Pre-fibrillar alpha-synuclein variants with impaired beta-structure increase neurotoxicity in Parkinson's disease models. EMBO J. 2009;28:3256–3268. doi: 10.1038/emboj.2009.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.El-Agnaf OM, Salem SA, Paleologou KE, Curran MD, Gibson MJ, Court JA, et al. Detection of oligomeric forms of alpha-synuclein protein in human plasma as a potential biomarker for Parkinson's disease. FASEB J. 2006;20:419–425. doi: 10.1096/fj.03-1449com. [DOI] [PubMed] [Google Scholar]
- 7.Mollenhauer B, Locascio JJ, Schulz-Schaeffer W, Sixel-Döring F, Trenkwalder C, Schlossmacher MG. α-Synuclein and tau concentrations in cerebrospinal fluid of patients presenting with parkinsonism: a cohort study. Lancet Neurol. 2011;10:230–240. doi: 10.1016/S1474-4422(11)70014-X. [DOI] [PubMed] [Google Scholar]
- 8.Park MJ, Cheon SM, Bae HR, Kim SH, Kim JW. Elevated levels of α-synuclein oligomer in the cerebrospinal fluid of drug-naïve patients with Parkinson's disease. J Clin Neurol. 2011;7:215–222. doi: 10.3988/jcn.2011.7.4.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lashuel HA, Overk CR, Oueslati A, Masliah E. The many faces of α-synuclein: from structure and toxicity to therapeutic target. Nat Rev Neurosci. 2013;14:38–48. doi: 10.1038/nrn3406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stenmark H. Rab GTPases as coordinators of vesicle traffic. Nat Rev Mol Cell Biol. 2009;10:513–525. doi: 10.1038/nrm2728. [DOI] [PubMed] [Google Scholar]
- 11.Dalfó E, Gómez-Isla T, Rosa JL, Nieto Bodelón M, Cuadrado Tejedor M, Barrachina M, et al. Abnormal alpha-synuclein interactions with Rab proteins in alpha-synuclein A30P transgenic mice. J Neuropathol Exp Neurol. 2004;63:302–313. doi: 10.1093/jnen/63.4.302. [DOI] [PubMed] [Google Scholar]
- 12.Gao Y, Wilson GR, Stephenson SEM, Bozaoglu K, Farrer MJ, Lockhart PJ. The emerging role of Rab GTPases in the pathogenesis of Parkinson's disease. Mov Disord. 2018;33:196–207. doi: 10.1002/mds.27270. [DOI] [PubMed] [Google Scholar]
- 13.Wilson GR, Sim JC, McLean C, Giannandrea M, Galea CA, Riseley JR, et al. Mutations in RAB39B cause X-linked intellectual disability and early-onset Parkinson disease with α-synuclein pathology. Am J Hum Genet. 2014;95:729–735. doi: 10.1016/j.ajhg.2014.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Atashrazm F, Hammond D, Perera G, Bolliger MF, Matar E, Halliday GM, et al. LRRK2-mediated Rab10 phosphorylation in immune cells from Parkinson's disease patients. Mov Disord. 2019;34:406–415. doi: 10.1002/mds.27601. [DOI] [PubMed] [Google Scholar]
- 15.Mir R, Tonelli F, Lis P, Macartney T, Polinski NK, Martinez TN, et al. The Parkinson's disease VPS35[D620N] mutation enhances LRRK2-mediated Rab protein phosphorylation in mouse and human. Biochem J. 2018;475:1861–1883. doi: 10.1042/BCJ20180248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kiral FR, Kohrs FE, Jin EJ, Hiesinger PR. Rab GTPases and membrane trafficking in neurodegeneration. Curr Biol. 2018;28:R471–R486. doi: 10.1016/j.cub.2018.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lai YC, Kondapalli C, Lehneck R, Procter JB, Dill BD, Woodroof HI, et al. Phosphoproteomic screening identifies Rab GTPases as novel downstream targets of PINK1. EMBO J. 2015;34:2840–2861. doi: 10.15252/embj.201591593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yamano K, Wang C, Sarraf SA, Münch C, Kikuchi R, Noda NN, et al. Endosomal Rab cycles regulate Parkin-mediated mitophagy. Elife. 2018;7:e31326. doi: 10.7554/eLife.31326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rivero-Ríos P, Romo-Lozano M, Madero-Pérez J, Thomas AP, Biosa A, Greggio E, et al. The G2019S variant of leucine-rich repeat kinase 2 (LRRK2) alters endolysosomal trafficking by impairing the function of the GTPase RAB8A. J Biol Chem. 2019;294:4738–4758. doi: 10.1074/jbc.RA118.005008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bae EJ, Kim DK, Kim C, Mante M, Adame A, Rockenstein E, et al. LRRK2 kinase regulates α-synuclein propagation via RAB35 phosphorylation. Nat Commun. 2018;9:3465. doi: 10.1038/s41467-018-05958-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Madero-Pérez J, Fdez E, Fernández B, Lara Ordóñez AJ, Blanca Ramírez M, Gómez-Suaga P, et al. Parkinson disease-associated mutations in LRRK2 cause centrosomal defects via Rab8a phosphorylation. Mol Neurodegener. 2018;13:3. doi: 10.1186/s13024-018-0235-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fujimoto T, Kuwahara T, Eguchi T, Sakurai M, Komori T, Iwatsubo T. Parkinson's disease-associated mutant LRRK2 phosphorylates Rab7L1 and modifies trans-Golgi morphology. Biochem Biophys Res Commun. 2018;495:1708–1715. doi: 10.1016/j.bbrc.2017.12.024. [DOI] [PubMed] [Google Scholar]
- 23.Purlyte E, Dhekne HS, Sarhan AR, Gomez R, Lis P, Wightman M, et al. Rab29 activation of the Parkinson's disease-associated LRRK2 kinase. EMBO J. 2018;37:1–18. doi: 10.15252/embj.201798099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jeong GR, Jang EH, Bae JR, Jun S, Kang HC, Park CH, et al. Dysregulated phosphorylation of Rab GTPases by LRRK2 induces neurode-generation. Mol Neurodegener. 2018;13:8. doi: 10.1186/s13024-018-0240-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chutna O, Gonçalves S, Villar-Piqué A, Guerreiro P, Marijanovic Z, Mendes T, et al. The small GTPase Rab11 co-localizes with α-synuclein in intracellular inclusions and modulates its aggregation, secretion and toxicity. Hum Mol Genet. 2014;23:6732–6745. doi: 10.1093/hmg/ddu391. [DOI] [PubMed] [Google Scholar]
- 26.Chiu CC, Yeh TH, Lai SC, Weng YH, Huang YC, Cheng YC, et al. Increased Rab35 expression is a potential biomarker and implicated in the pathogenesis of Parkinson's disease. Oncotarget. 2016;7:54215–54227. doi: 10.18632/oncotarget.11090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pagan FL. Improving outcomes through early diagnosis of Parkinson's disease. Am J Manag Care. 2012;18:S176–S182. [PubMed] [Google Scholar]
- 28.Tolosa E, Wenning G, Poewe W. The diagnosis of Parkinson's disease. Lancet Neurol. 2006;5:75–86. doi: 10.1016/S1474-4422(05)70285-4. [DOI] [PubMed] [Google Scholar]
- 29.Yang SY, Chiu MJ, Lin CH, Horng HE, Yang CC, Chieh JJ, et al. Development of an ultra-high sensitive immunoassay with plasma biomarker for differentiating Parkinson disease dementia from Parkinson disease using antibody functionalized magnetic nanoparticles. J Nanobiotechnology. 2016;14:41. doi: 10.1186/s12951-016-0198-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shin HW, Chung SJ. Drug-induced parkinsonism. J Clin Neurol. 2012;8:15–21. doi: 10.3988/jcn.2012.8.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chiu CC, Lu CS, Weng YH, Chen YL, Huang YZ, Chen RS, et al. PARK14 (D331Y) PLA2G6 causes early-onset degeneration of substantia nigra dopaminergic neurons by inducing mitochondrial dysfunction, ER stress, mitophagy impairment and transcriptional dysregulation in a knockin mouse model. Mol Neurobiol. 2019;56:3835–3853. doi: 10.1007/s12035-018-1118-5. [DOI] [PubMed] [Google Scholar]
- 32.Chiu CC, Yeh TH, Lai SC, Wu-Chou YH, Chen CH, Mochly-Rosen D, et al. Neuroprotective effects of aldehyde dehydrogenase 2 activation in rotenone-induced cellular and animal models of parkinsonism. Exp Neurol. 2015;263:244–253. doi: 10.1016/j.expneurol.2014.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schapira AH. Science, medicine, and the future: Parkinson's disease. BMJ. 1999;318:311–314. doi: 10.1136/bmj.318.7179.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schlesinger I, Schlesinger N. Uric acid in Parkinson's disease. Mov Disord. 2008;23:1653–1657. doi: 10.1002/mds.22139. [DOI] [PubMed] [Google Scholar]
- 35.Brodacki B, Staszewski J, Toczyłowska B, Kozłowska E, Drela N, Chalimoniuk M, et al. Serum interleukin (IL-2, IL-10, IL-6, IL-4), TNFalpha, and INFgamma concentrations are elevated in patients with atypical and idiopathic parkinsonism. Neurosci Lett. 2008;441:158–162. doi: 10.1016/j.neulet.2008.06.040. [DOI] [PubMed] [Google Scholar]
- 36.Scalzo P, Kümmer A, Cardoso F, Teixeira AL. Serum levels of interleukin-6 are elevated in patients with Parkinson's disease and correlate with physical performance. Neurosci Lett. 2010;468:56–58. doi: 10.1016/j.neulet.2009.10.062. [DOI] [PubMed] [Google Scholar]
- 37.Godau J, Herfurth M, Kattner B, Gasser T, Berg D. Increased serum insulin-like growth factor 1 in early idiopathic Parkinson's disease. J Neurol Neurosurg Psychiatry. 2010;81:536–538. doi: 10.1136/jnnp.2009.175752. [DOI] [PubMed] [Google Scholar]
- 38.Cui SS, Du JJ, Liu SH, Meng J, Lin YQ, Li G, et al. Serum soluble lymphocyte activation gene-3 as a diagnostic biomarker in Parkinson's disease: a pilot multicenter study. Mov Disord. 2019;34:138–141. doi: 10.1002/mds.27569. [DOI] [PubMed] [Google Scholar]
- 39.Marques TM, Van Rumund A, Oeckl P, Kuiperij HB, Esselink RAJ, Bloem BR, et al. Serum NFL discriminates Parkinson disease from atypical parkinsonisms. Neurology. 2019;92:e1479–e1486. doi: 10.1212/WNL.0000000000007179. [DOI] [PubMed] [Google Scholar]
- 40.Bagheri V, Khorramdelazad H, Hassanshahi G, Moghadam-Ahmadi A, Vakilian A. CXCL12 and CXCR4 in the peripheral blood of patients with Parkinson's disease. Neuroimmunomodulation. 2018;25:201–205. doi: 10.1159/000494435. [DOI] [PubMed] [Google Scholar]
- 41.Niimi Y, Ito S, Mizutani Y, Murate K, Shima S, Ueda A, et al. Altered regulation of serum lysosomal acid hydrolase activities in Parkinson's disease: a potential peripheral biomarker. Parkinsonism Relat Disord. 2019;61:132–137. doi: 10.1016/j.parkreldis.2018.10.032. [DOI] [PubMed] [Google Scholar]
- 42.Pavlos NJ, Grønborg M, Riedel D, Chua JJ, Boyken J, Kloepper TH, et al. Quantitative analysis of synaptic vesicle Rabs uncovers distinct yet overlapping roles for Rab3a and Rab27b in Ca2+-triggered exocytosis. J Neurosci. 2010;30:13441–13453. doi: 10.1523/JNEUROSCI.0907-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gerges NZ, Backos DS, Esteban JA. Local control of AMPA receptor trafficking at the postsynaptic terminal by a small GTPase of the Rab family. J Biol Chem. 2004;279:43870–43878. doi: 10.1074/jbc.M404982200. [DOI] [PubMed] [Google Scholar]
- 44.Mignogna ML, Giannandrea M, Gurgone A, Fanelli F, Raimondi F, Mapelli L, et al. The intellectual disability protein RAB39B selectively regulates GluA2 trafficking to determine synaptic AMPAR composition. Nat Commun. 2015;6:6504. doi: 10.1038/ncomms7504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mori Y, Fukuda M, Henley JM. Small GTPase Rab17 regulates the surface expression of kainate receptors but not α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors in hippocampal neurons via dendritic trafficking of Syntaxin-4 protein. J Biol Chem. 2014;289:20773–20787. doi: 10.1074/jbc.M114.550632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shin N, Jeong H, Kwon J, Heo HY, Kwon JJ, Yun HJ, et al. LRRK2 regulates synaptic vesicle endocytosis. Exp Cell Res. 2008;314:2055–2065. doi: 10.1016/j.yexcr.2008.02.015. [DOI] [PubMed] [Google Scholar]
- 47.Shi MM, Shi CH, Xu YM. Rab GTPases: the key players in the molecular pathway of Parkinson's disease. Front Cell Neurosci. 2017;11:81. doi: 10.3389/fncel.2017.00081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Williams SM, Schulz P, Sierks MR. Oligomeric α-synuclein and β- amyloid variants as potential biomarkers for Parkinson's and Alzheimer's diseases. Eur J Neurosci. 2016;43:3–16. doi: 10.1111/ejn.13056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brigo F, Erro R, Marangi A, Bhatia K, Tinazzi M. Differentiating drug-induced parkinsonism from Parkinson's disease: an update on non-motor symptoms and investigations. Parkinsonism Relat Disord. 2014;20:808–814. doi: 10.1016/j.parkreldis.2014.05.011. [DOI] [PubMed] [Google Scholar]
- 50.Wu Y, Le W, Jankovic J. Preclinical biomarkers of Parkinson disease. Arch Neurol. 2011;68:22–30. doi: 10.1001/archneurol.2010.321. [DOI] [PubMed] [Google Scholar]
- 51.Sherer TB. Biomarkers for Parkinson's disease. Sci Transl Med. 2011;3:79ps14. doi: 10.1126/scitranslmed.3002488. [DOI] [PubMed] [Google Scholar]
- 52.Haehner A, Boesveldt S, Berendse HW, Mackay-Sim A, Fleischmann J, Silburn PA, et al. Prevalence of smell loss in Parkinson's disease--a multicenter study. Parkinsonism Relat Disord. 2009;15:490–494. doi: 10.1016/j.parkreldis.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 53.Ravina B, Camicioli R, Como PG, Marsh L, Jankovic J, Weintraub D, et al. The impact of depressive symptoms in early Parkinson disease. Neurology. 2007;69:342–347. doi: 10.1212/01.wnl.0000268695.63392.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Delenclos M, Jones DR, McLean PJ, Uitti RJ. Biomarkers in Parkinson's disease: advances and strategies. Parkinsonism Relat Disord. 2016;22 Suppl 1:S106–S110. doi: 10.1016/j.parkreldis.2015.09.048. [DOI] [PMC free article] [PubMed] [Google Scholar]