Abstract
Abstract
The European Union member states received about 385,000 asylum applications from children and adolescents below 18 years in 2015, and 398,000 in 2016. The latest political crises and war have led to an upsurge in refugee movements into European countries, giving rise to a re-evaluation of the epidemiology of psychiatric disorders and mental health problems among young refugees and asylum seekers. We systematically searched five electronic databases and reference lists of pertinent review articles. We then screened the results of forward citation tracking of key articles for relevant studies in the field for the period from January 1990 to October 2017. We dually reviewed citations and assessed risk of bias. We reported the results narratively, as meta-analyses were impeded due to high heterogeneity. We included 47 studies covered in 53 articles. Overall, the point prevalence of the investigated psychiatric disorders and mental health problems varied widely among studies (presenting interquartile ranges): for posttraumatic stress disorder between 19.0 and 52.7%, for depression between 10.3 and 32.8%, for anxiety disorders between 8.7 and 31.6%, and for emotional and behavioural problems between 19.8 and 35.0%. The highly heterogeneous evidence base could be improved by international, methodologically comparable studies with sufficiently large sample sizes drawn randomly among specific refugee populations. The prevalence estimates suggest, nevertheless, that specialized mental health care services for the most vulnerable refugee and asylum-seeking populations are needed.
Registration
The systematic review protocol was registered in PROSPERO on October 19th, 2017 with the number: CRD42017080039 and is available from: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=80039
Electronic supplementary material
The online version of this article (10.1007/s00787-018-1215-z) contains supplementary material, which is available to authorized users.
Keywords: Accompanied refugee minors, Unaccompanied refugee minors, Posttraumatic stress disorder, Depression, Systematic review, Mental health
Introduction
European countries faced unusually high arrivals of asylum seekers mainly from Syria, Afghanistan, and Iraq in 2015 and 2016, with Austria, France, Germany, Greece, Italy, Sweden, and United Kingdom as main destination countries [1]. With 1.3 million arrivals in both 2015 and 2016, the number of asylum applications in the European Union (EU) far exceeded the previous peak of about 672,000 in 1992, when the EU member states received many asylum seekers from former Yugoslavia [2].
Within this group, the most vulnerable asylum seekers and refugees are children and adolescents. In legal terms, asylum seekers are individuals who have applied for asylum on an individual basis and whose claim is pending. Refugees are individuals recognized based on the United Nations Refugee Convention, which gives them a legal residence status [3]. During the last years, increasing numbers of unaccompanied refugee minors (URM) (i.e. children under the age of 18, who came to the host country without a parent or other caregiver) as well as children and adolescents accompanied by their parents or caregivers, were seeking asylum in different countries worldwide [4], as well as in the EU. Overall, unaccompanied or accompanied minors represent one-third of all asylum seekers in the EU [1]. In the year 2015, around 385,000 children and adolescents below 18 years sought asylum in the EU. In the year 2016, this number rose to 398,000, and in 2017, the number rose again to 213,000 [5].
Forced migration sets children and adolescents under increased challenges that compound the usual developmental challenges of childhood. For example, before or during the forced migration, minors might have experienced war or death of relatives and friends and might have been exposed to violence. Furthermore, these children and adolescents might be confronted with different challenges such as adaptation processes to the new setting, racial discrimination, and complex legal immigration processes [6]. These stressors experienced in the country of origin, during migration as well as in the host country, may lead to strong psychological pressure and physical challenges and therefore affect children’s and adolescents’ physical health and well-being [7]. Studies show that traumatic and ongoing adverse experiences as well as social risk factors can lead to mental stress disorders, in specific posttraumatic stress disorders (PTSD), depression, anxiety disorders or psychological distress (e.g. unspecified mental disorders, externalizing behaviour) [8–11]. In addition, long-lasting asylum procedures with uncertain outcomes represent high psychological burdens [6]. Even after a long period in the host country, mental stress remains high [12].
These findings highlight the special vulnerability of both accompanied and unaccompanied refugee children and adolescents in terms of mental health. To take planning steps for guaranteeing an effective mental health care, it is important to be aware of the mental health status of refugee populations in general [13, 14]. The two most recent systematic reviews on the prevalence of psychiatric disorders in asylum-seeking or refugee children and adolescents included studies up to 2008 [15] and 2015, respectively [16]. Since then, new or re-emerging political crises and war have led to an upsurge in refugee movements into European countries, giving rise to a re-evaluation of the prevalence of mental disorders among young refugees. Furthermore, both systematic reviews have methodological limitations that could have had an impact on the completeness of the included evidence base and the results.
Therefore, the goal of our project was to conduct an up-to-date systematic review guided by the Joanna Briggs Institute Reviewers’ Manual for protocols and systematic reviews as this is—to our best knowledge—the only available guideline for systematic reviews on prevalence data [17], addressing the following research question: What is the prevalence of mental health disorders among asylum-seeking or refugee children and adolescents (either accompanied or unaccompanied) in European countries?
Methods
We developed a systematic review protocol according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis for Protocols (PRISMA-P) reporting guidelines [18]. The research question laid out in this article was part of a systematic review registered in PROSPERO (an international database of prospectively registered systematic reviews in health and social care) on October 19th, 2017 under the number: CRD42017080039. Throughout this manuscript, we followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement [19] to report this systematic review.
Eligibility criteria
In accordance with the research question, we specified a priori a list of inclusion and exclusion criteria following the recommended Condition-Context-Population-Framework (CoCoPop) for prevalence data [17]. We included studies if they (1) were published in peer-reviewed journal articles, (2) investigated the prevalence of psychiatric disorders (as primary outcomes) or other psychological problems (as secondary outcomes), (3) examined unaccompanied or accompanied asylum-seeking children and adolescents or refugee minors (≤ 21 years, to allow for some outliers in the age group), (4) and were conducted in European countries. We excluded studies, which provided data on internally displaced children only or on children and adolescents that were invited to participate in the study after their attendance of a mental health clinic. The detailed inclusion and exclusion criteria are depicted in Table 1. We are not reporting on differences between refugees and asylum seekers because most studies included mixed populations or did not state explicitly the legal status of the included children and adolescents.
Table 1.
Eligibility criteria according to Condition-Context-Population-Framework (CoCoPop) for prevalence data [17]
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Condition |
Primary outcomes: anxiety disorder (general anxiety disorder, social phobia, panic disorder), bipolar disorder, eating disorder, major depressive disorder, posttraumatic stress disorder, schizophrenia, somatoform disorders, substance abuse of illicit drugs, alcohol and tobacco, suicidal ideation and behaviour Secondary outcomes: Other psychological problems: psychological distress, behaviour problems, mental health problems, emotional problems, emotional well-being |
All other mental disorders, such as personality disorder |
|
Assessment process: With a reliable, validated self-assessment or proxy-assessment tool or with a structured clinical interview Assessment time: When the assessment happened over several time points we took the first available data point |
Self-developed questionnaire without reporting on psychometric properties | |
| Context | European Countries (Albania, Andorra, Armenia, Austria, Azerbaijan, Belarus, Belgium, Bosnia and Herzegovina, Bulgaria, Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Georgia, Germany, Greece, Hungary, Iceland, Ireland, Italy, Kazakhstan, Kosovo, Latvia, Liechtenstein, Lithuania, Luxembourg, Macedonia [FYROM], Malta, Moldova, Monaco, Montenegro, Netherlands, Norway, Poland, Portugal, Romania, Russia, San Marino, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Turkey, Ukraine, United Kingdom [UK], Vatican City [Holy See]) see list: https://www.countries-ofthe-world.com/countries-of-europe.html | |
| Population | Unaccompanied or accompanied asylum-seeking children and adolescents or refugee minors (≤ 21 years) [including adolescents up to 23 years, if the age group 21–23 years comprised < 50% of the study population] |
Internally displaced children and adolescents (i.e. people who have not crossed a boarder to find safety); Study participation is based on the attendance of a mental health department/clinic |
Literature search strategy
We conducted a systematic literature search of Ovid MEDLINE, PsycINFO (via Ebsco), CINAHL (The Cumulative Index to Nursing and Allied Health Literature, via Ebsco), PubMed (for non-MEDLINE content) and Scopus for the period from January, 1st 1990 to October, 17th 2017. An experienced information specialist developed a search strategy using a combination of different MeSH (Medical subject headings) terms and variations of free-text key words (consisting of search terms for ‘refugees’ AND ‘minors’ AND ‘mental disorders’ AND ‘Europe’). We did not limit the search to any specific languages. The search strategy was developed in Ovid MEDLINE and adapted for the other databases. The detailed search strategy, which we tested using known relevant articles, is available in Additional Material 1. Additionally, we complemented electronic searches by checking reference lists of pertinent review articles and using forward citation tracking of key articles in the field. We further conducted grey literature searches considering government surveillance data, reports from World Health Organization (WHO), United Nations High Commissioner for Refugees (UNHCR), the European Council on Refugees and Exiles (ECRE) and Médecins Sans Frontières (MSF).
Study selection and data extraction
We imported all references into the Systematic Review Software Covidence [20] and used this program throughout the review process. Two reviewers independently screened abstracts and full-texts against pre-specified criteria. They resolved discrepancies about inclusion or exclusion by consensus or by involving a third reviewer. The abstract and full-text review forms were pilot-tested and the review form was adapted according to feedback of the pilot review participants.
Next, we pilot-tested and used standardized data extraction forms to gather relevant information systematically from each study. One investigator extracted data relating to study information, study method, population, and outcomes/condition. A second investigator checked all extracted data for completeness and accuracy. If the publications did not report the necessary information for relevant outcomes, we contacted authors to request additional data.
Risk of bias assessment of selected studies
We evaluated the risk of bias of included studies using a modified version of the standardized critical appraisal tool (AXIS tool) to assess the quality and risk of bias in cross-sectional studies [21]. Risk of bias was assessed at the outcome level by two independent reviewers. Again, the reviewers solved disagreement by discussion or by involving a third reviewer. We collapsed the information into a final risk of bias rating for each individual included study using three distinct categories: low, unclear, or high risk of bias.
Synthesis and analysis
We performed exploratory random effect meta-analyses based on a logit transformation to calculate weighted summary proportions using generic inverse variance models to synthesise prevalence estimates of studies that were similar with respect to outcome measurement [17]. We pooled studies when there were at least three different studies reporting on the same outcome. We tested for heterogeneity with Cochrane’s Q test and quantified its magnitude using I2 and τ2. We conducted all statistical analyses using Comprehensive Meta-Analysis version 3.0.
Because of high heterogeneity for all outcomes of interest, we conducted subgroup analyses to explore heterogeneity: (i) accompanied vs. unaccompanied refugees/asylum seekers, (ii) type of assessment of mental disorders (structured clinical interview vs. self-report questionnaires), and (iii) sampling procedure (random sampling or census survey vs. non-random sampling). As we did not identify enough similar studies—contrary to what we stated in the protocol—we could not analyse differences between host countries and between placement types (refugee camps vs. non-refugee camps). We carried out sensitivity analyses to assess the effect of high risk of bias studies on the overall effect. Because of very high, unexplained heterogeneity for all outcomes of interest, we do not report pooled effects of prevalence estimates. Throughout the manuscript, we present prevalence estimates as medians and interquartile ranges. Interquartile ranges reflect estimates between the 25th and the 75th percentiles of a range of estimates and eliminate extreme values at both ends of a spectrum.
Confidence in cumulative evidence
For assessing the confidence in available evidence for the prevalence of psychiatric disorders, we followed the guidance of the Project on a Framework for Rating Evidence in Public Health (PRECEPT) [22]. This project adapted the GRADE scheme (Grading of Recommendations Assessment, Development and Evaluation) [23] to prevalence data [22]. We only considered the defined primary outcomes but not the secondary outcomes stated in the protocol (see Table 1). No decision-makers were involved in the selection of outcomes. Criteria for downgrading the quality of evidence according to GRADE are risk of bias, inconsistency, indirectness, imprecision and publication bias using four grades: high, moderate, low, and very low. For each outcome, the quality of evidence is initially rated as “high” and not as “low” as in other observational studies [22]. We dually evaluated both the overall quality of evidence for each outcome and solved disagreement through discussion.
Results
Results of the search strategy
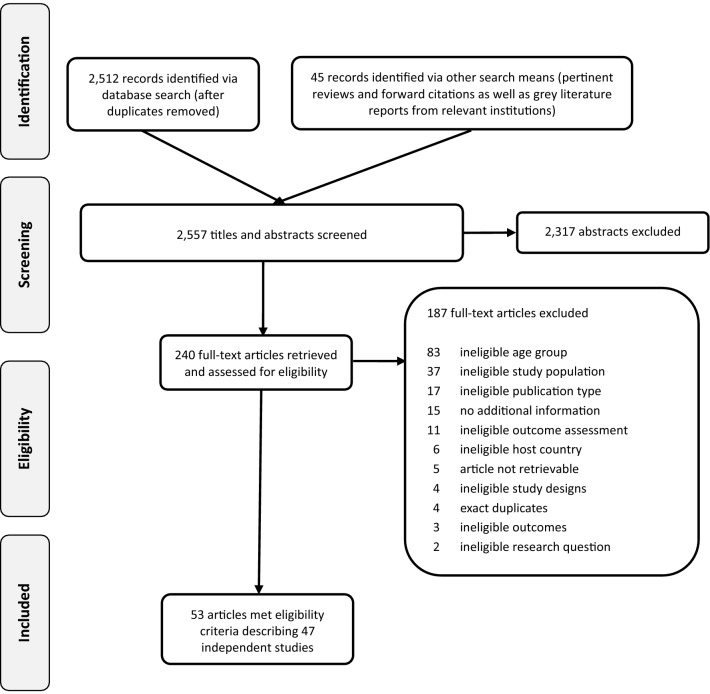
Overall, we identified 2557 citations from searches and reviews of reference lists after removal of duplicates. Of these, we assessed 240 full-texts for eligibility. Finally, we included 47 studies reported in 53 articles [24–76] (see Fig. 1). 15 additional articles were accompanying articles, but did not reveal any further information relevant for our research question and were therefore excluded [8, 9, 11, 77–88]. We obtained additional data for eleven studies after contacting authors [28, 48, 53, 60, 62, 64, 66, 67, 73–75]. Seven studies were published in other languages than English: Danish [55, 69], German [48, 59, 75, 76] and Italian [65]. We translated the relevant information into English. Overall, ten studies [26, 31, 40, 45, 47, 51, 58, 68, 70, 73] reported mean and standard deviation for relevant outcomes. These results are presented in Additional Material 2.
Fig. 1.
PRISMA flow diagram of the study selection process
Description of included studies
Table 2 provides an overview of the included studies summarizing population characteristics, data collection methods and outcomes. Studies reported information on 24,786 refugee or asylum-seeking children and adolescents living in 14 European countries (Austria, Belgium, Croatia, Denmark, Finland, Germany, Greece, Italy, Netherlands, Norway, Slovenia, Sweden, Turkey, and United Kingdom). One large register-based study already contributed data on 15,264 children and adolescents [26]. Overall, the studies included more boys than girls. The mean age of the participants varied between 5.9 and 18.6 years (range 2–23 years). Seven studies assessed the children’s and adolescent’s mental health after 2010, 13 studies were conducted between 2000 and 2010 and eight studies were conducted earlier. The length of stay in the host country ranged from 4 months to 9 years. The countries of origin varied widely with the majority of study participants coming from Africa, Afghanistan, Iran, Iraq, and countries from former Yugoslavia. Two studies [26, 57] received a low risk of bias rating and 29 studies [24, 25, 27, 30, 33–39, 41, 42, 44–51, 54, 56, 61, 62, 66, 68, 75, 76] received an unclear risk of bias rating (see Table 2). Reasons for unclear risk of bias ratings were mainly because the sample was a convenience sample, the sample size was not justified and rather small, or the survey’s response rate was not reported. Sixteen studies showed high risk of bias [29, 32, 52, 55, 58–60, 63, 65, 67, 69–74], because of low response rates (< 30%), inconsistent results, or the lack of informed consent or ethical approval (as rated by the AXIS tool).
Table 2.
Study characteristics of included studies
| Study | Country of study | Region of origin: n (%)† | Sample size, n | Sampling procedure | Year of assessment | Mean age in years, M (SD) | Gender—female, n (%) | u/a | Outcome | RoB |
|---|---|---|---|---|---|---|---|---|---|---|
| Adam and Klasen [67] | Germany |
ME: NR (80.9%) EE: NR (19.1%) |
215 | NRS | 2002–2003 | 14.8 (2.1) | NR (41.4%) | a | A, D, EBP, PTSD | High |
| Almqvist et al. [24] | Sweden | ME: 50 (100%) | 50 | NRS | NR | M: 5.8 (1.1) | 14 (28%) | a | PTSD | Uncl |
| F: 5.8 (1.1) | ||||||||||
| Angel et al. [25] | Sweden | EE: 99 (100%) | 99 | NRS | 1994–1995 | 11.3 (NR) | NR | a | A, EBP, PTSD | Uncl |
| Barghadouch et al. [26] | Denmark |
AS: 2349 (15.4%) EE: 6505 (42.6%) |
15,264 | Census | NR | 9.1 (NR) | 6909 (45.3%) | u and a | AD*, ND*, PD* | Low |
| Bean et al. [27, 28] | Netherlands |
AF: NR (53%) AS: NR (8%) ME: NR (4%) |
1110 | NRS/RS | 2002 | 15.8 (NR) | 329 (29.8%) | u | A, D, EBP, PTSD | Uncl |
| Begovac et al. [29] | Germany/Croatia | EE: 133 (100%) | 133 | NRS | 1997–1999 | NR | 160 (49.7%) | NR | D, PTSD | High |
| Bronstein et al. [30] | UK | ME: 222 (100%) | 222 | NRS | NR | 16.3 (1.0) | 0 (0%) | u | A, D, PTSD | Uncl |
| Derluyn et al. [32] | Belgium |
AF: NR (59%) AS: NR (25.3%) EE: NR (14.3%) SA: 2 (1.2%) |
142 | NRS | NR |
<14 y: 9.6% 15–17 y: 52.9% >18 years 37.3% |
NR (37.3%) | u | A, D, EBP | High |
| Derluyn et al. [33] | Belgium |
AF: 517 (43.4%) AS: 267 (22.4%) EE: 349 (29.3%) SA: 59 (4.9%) |
1234 | RS | 2002–2003 | 16.6 (1.31) |
U: 43 (35.8%) A: 516 (46.5%) |
u and a | A, D, PTSD | Uncl |
| Elklit et al. [34] | Denmark | EE: 119 (100%) | 119 | NRS | NR | 18.5 (1.8) | NR (33.3%) | u and a | PTSD | Uncl |
| Fazel et al. [35] | UK |
EE: NR (48%) AS: NR (16%) ME: NR (10%) |
101 | NRS | NR | NR | 40 (40%) | u and a | EBP | Uncl |
| Gavranidou et al. [68] | Germany |
EE: 32 (NR) ME: 11 (NR) |
55 | NRS | NR | 13.4 (NR) | 23 (41.8%) | u and a | A*, EBP* | Uncl |
| Goldin et al. [36] | Sweden | EE: NR | 48 | NRS | 1994–1995 | NR | 24 (50%) | a | A, D, PTSD, HYP, PSYCom | Uncl |
| Gusic et al. [72] | Sweden | ME: 26 (60%) | 42 | NRS | NR | 16.1 (1.5) | 16 (38%) | u and a | DP, PTSD | High |
| Hjern et al. [37] | Sweden |
SA: 43 (68%) ME 20 (32%) |
63 | NRS | 1986–1987 | 5.9 (NR) | NR | a | EBP | Uncl |
| Hodes et al. [38] | UK |
~EE: 34 (28.8%) AF: 52 (44.1%) ME: 26 (22.0%) AS: 3 (2.5%) SA: 3 (2.5%) |
113 | NRS | 2002–2003 | 17.0 (NR) | 44 (38.9%) | u and a | D, PTSD | Uncl |
| Hollins et al. [71] | UK | EE: 99 (100%) | 99 | NRS | NR | 16 (1.2) | 12 (NR) | u | A, EBP | High |
| Huemer et al. [39] | Austria | AF: 41 (100%) | 41 | NRS | NR | 17.0 (0.8) | 6 (15%) | u | A*, D, PTSD, S | Uncl |
| Jakobsen et al. [61] | Norway |
ME: 105 (76%) AF: 33 (24%) |
138 | NRS | 2009–2011 | 16.2 (0.8) | 0 (0%) | u | A, D, EBP, OPD, PTSD | Uncl |
| Jensen et al. [41] | Norway |
~AS: 59 (63%) AF: 34 (37%) EE: 1 (1%) |
93 | Census | 2010–2012 | 13.8 (1.4) | 28 (19%) | u | A, D, EBP, PTSD | Uncl |
| Kocijan-Hercigonja et al. [70] | Croatia | EE: 35 (100%) | 35 | NRS | NR | NR | NR | a | A*, D*, PSYCom* | High |
| Longobardi et al. [74] | Italy |
AF: 12 (63.2%) EE: 5 (26.3%) AS: 1 (5.3%) |
23 | NRS | NR | NR | 1 (5%) | u | A, D, PTSD | High |
| Möhrle et al. [75] | Germany |
ME: NR (51.6%) AF: NR (16.8%) |
191 | NRS | 2015–201 | 17.1 (1.2) | 0 (0%) | u | EBP | Uncl |
| Montgomery [42] | Denmark | ME: 131 (96.24%) | 131 | NRS | 2000–2001 | 15.3 (NR) | 76 (58%) | u and a | EBP | Uncl |
| Nasiroglu and Ceri [60] | Turkey | ME: 55 (100%) | 55 | NRS | NR | 11 (3.7) | 25 (45.6%) | NR | A, D, HYP, NE, PTSD | High |
| Nielsen et al. [44] | Denmark |
EE: 118 (48%) ME: 67 (27%) |
246 | NRS | 2006 | 9.6 (NR) | 104 (42%) | a | EBP | Uncl |
| Oppedal and Idsoe [45] | Norway | ME: NR (70%) | 948 | NRS | 2000–2010 | 18.6 (2.5) | NR (15.8%) | u | D*, PTSD | Uncl |
| Papageorgiou et al. [46] | Greece | EE: NR | 95 | NRS | NR | 9.6 (NR) | 54 (57%) | u | A, D, EBP, OPD, PTSD | Uncl |
| Reijneveld et al. [47] | Netherlands |
EE: 6 (4.9%) AS: 9 (7.4%) AF: 107 (87.7%) |
122 | NRS | 2002 –2003 | 16.1 (0.7) | 40 (32.8%) | u | A*, D*, EBP*, PTSD* | Uncl |
| Reis et al. [48] | Germany | ME: 40 (80%) | 58 | NRS | 2007–2009 | 12 (NR) | 25 (43%) | a | EBP | Uncl |
| Rücker et al. [59] | Germany |
ME: 45 (86.5%) OC: 7 (13.5%) |
52 | NRS | 2016 | 16.2 (1.4) | 1 (1.9%) | u | EBP | High |
| Ruf et al. [76] | Germany | EE: 47 (45.2%) | 98 | NRS | 2003–2004 | 10.6 (2.6) | 56 (53.8%) | a | D, S, PTSD | Uncl |
| Sabuncuoglu and Berkem [73] | Turkey | EE: 19 (100%) | 19 | NRS | NR | Range 13–73 (NR) | 10 (53%) | u and a | D* | High |
| Salari et al. [49] | Sweden | ME: NR (100%) | 208 | NRS | 2015–2016 | 15.4 (1.3) | NR (2.4%) | u | PTSD | Uncl |
| Sanchez-Cao et al. [50] | UK |
EE: 25 (35%) AF: 36 (51%) |
71 | NRS | 2003–2004 | NR | 23 (32.4%) | u | D, EBP, PTSD | Uncl |
| Sikic et al. [51] | Croatia | EE: NR | 669 | NRS | 1994–1995 | 12.03 (2.5) | 989 (48%) | NR | A*, D* | Uncl |
| Sleijpen et al. [62] | Netherlands |
ME: 52 (46.8%) AS: 15 (13.5%) AF: 6 (5.4%) OC: 37 (33.3%) |
111 | RS | 2014–2015 | 14.5 (1.8) | 57 (51%) | NR | PTSD | Uncl |
| Slodnjak et al. [52] | Slovenia | EE: NR | 265 | NRS | 1994 | NR | 140 (52.8%) | u and a | D, S, PTSD | High |
| Sourander et al. [54] | Finland | AF: 42 (91.3%) | 46 | NRS | NR | 14.1 (2.3) | 12 (NR) | u | EBP | Uncl |
| Staehr [69] | Denmark | EE: NR | 232 | NRS | 1999 | NR | NR | NR | PTSD | High |
| Staehr et al. [55] | Denmark | NR | 780 | NRS | 2001 –2003 | NR | NR | u and a | S | High |
| Stotz et al. [63] | Germany | NR | 32 | NRS | 2011 | 15.6 (2.2) | 0 (0%) | u and a | PTSD | High |
| Taurino et al. [65] | Italy | AF: 29 (87%) | 34 | NRS | NR | 18.1 (0.6) | 0 (0%) | u | A, D, PTSD | High |
| Thommessen et al. [66] | Italy |
AF: 16 (NR) ME: 15 (NR) AS: 29 (NR) |
60 | NRS | NR | NR | 0 (0%) | u | EBP | Uncl |
| Vervliet et al. [56] | Belgium/Norway |
ME: 212 (69.1%) AF: 92 (30.0%) AS: 2 (0.6%) EE: 1 (0.3%) |
307 | Census | NR | 16.1 (0.8) | 16 (5.2%) | u | A, D, PTSD | Uncl |
| Wiegersma et al. [57] | Netherlands |
ME: NR (37%) EE: NR (39%) AF: NR (24%) |
267 | NRS | 2003 | 9.9 (3.5) | NR (50%) | a | EBP | Low |
| Yurtbay et al. [58] | Turkey | EE: 250 (100%) | 250 | NRS | 1999 |
Children: 10.8 (1.47) Adolescents: 15.4 (1.43) |
125 (50%) | NR | A, D* | High |
A anxiety, a accompanied, AD affective disorder, AF Africa, AS Asia, D depression, DP dissociative psychopathology, EBP emotional and behavioural problems, EE Eastern Europe, HYP hyperactiveness, M mean, ME Middle East, n sample size, NE nocturnal enuresis, ND neurotic disorder, NR not reported, NRS non-random sampling, OPD overall psychiatric disorder, PD psychotic disorder, PSYCom psychiatric complaints, PTSD posttraumatic stress disorder, RoB risk of bias, RS random sampling, S suicidal ideation and behaviour, SA South America, SD standard deviation, u unaccompanied, Uncl unclear
*mean and standard deviation but no point prevalences are reported
~overall sample size differed from n of distribution of countries of origin
†we grouped the reported countries of origin into Asia, Africa, Eastern Europe, Middle East and South America
Unexplained high heterogeneity hampered the conduct of meta-analyses for all outcomes (PTSD: I2 = 96%; depression: I2 = 94%; anxiety disorder: I2 = 96%; suicidal ideation and behaviour: I2 = 90%; emotional and behavioural problems: I2 = 87%;). See Additional Material 3 for point prevalence and confidence interval (CI) for outcomes of individual studies.
Figure 2 presents an overview of the median point prevalence and the interquartile ranges of the relevant outcomes. These results are described in more detail below.
Fig. 2.
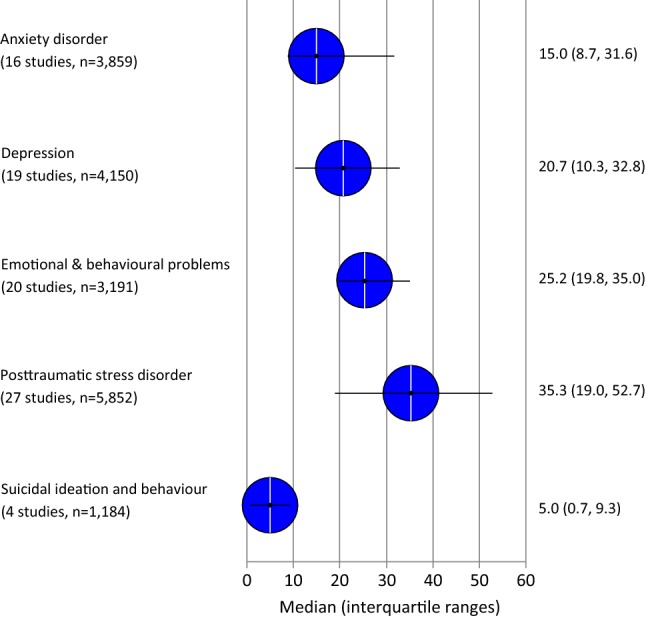
Median and interquartile ranges of point prevalences of psychiatric disorders and mental problems in young refugees and asylum seekers. n sample size
Posttraumatic stress disorder
Twenty-seven studies reported on the prevalence of PTSD, providing data on a total of 5852 young refugees or asylum seekers [24, 25, 27, 29, 30, 33, 34, 36, 38, 39, 41, 45, 46, 49, 50, 52, 56, 60–63, 65, 67, 69, 72, 74, 76]. The interquartile range (IQR) for refugees and asylum seekers screening positive for PTSD was 19.0–52.7% and the median was 35.3%. The two largest studies rated with unclear risk of bias reported a PTSD prevalence of 42.3% (95% CI 39.1%, 45.6%, n = 875) [53] and 52.0% (95% CI 48.7%, 55.2%, n = 895) [45]. PTSD was screened via self-report questionnaires (Impact of War-related Trauma Events [IWRITE], Reactions of Adolescents to Traumatic Stress Questionnaire [RATS]).
Generally, studies relying on clinical interviews for the diagnosis of PTSD showed a lower PTSD prevalence than studies using self-report or proxy-questionnaires (IQR 19.2–36.0% vs. 25.6–62.7%). Three studies directly compared differences between unaccompanied and accompanied children and adolescents. They reported a higher prevalence for being screened positive for PTSD or to be diagnosed with PTSD among unaccompanied than accompanied children and adolescents (Study 1 [different accompanied groups]: 36.7% vs. 5.7–12.7% [33]; Study 2 [gender]: 61.5–73.1% vs 14.3–35.3% [38]; and Study 3: 50% vs. 0% [63]).
Overall, the quality of evidence regarding the prevalence of PTSD in refugee and asylum-seeking children and adolescents is low. This is because the evidence relies mainly on studies that used convenience sampling strategies (downgraded for risks of bias), and the studies’ results varied considerably (downgraded for inconsistency).
Depression
Nineteen studies, including 4150 children and adolescents, analysed the prevalence of depression [27, 29, 31–33, 36, 38, 39, 41, 46, 50, 52, 56, 60, 61, 65, 67, 74, 76]. The IQR for depression prevalence was 10.3–32.8% and the median was 20.7%. As for PTSD, studies using a structured clinical interview (e.g. M.I.N.I Kid) as assessment method reported lower percentages of depression 3.1% to 9.4% [39, 61, 76] compared to the median of all assessments (20.7%).
The two largest studies both using the Hopkins Symptom Checklist-37A [HSCL-37A] (a self-report questionnaire for the screening for depression) revealed very different results. In a sample of 650 accompanied refugees and asylum seekers in Belgium, the study reported a depression prevalence of 8.2% (95% CI 6.3%, 10.5%) [33]. By contrast, a study on 827 unaccompanied children and adolescents in the Netherlands [28] reported a prevalence for depression of 38.8% (95% CI 35.6%, 42.2%). The Belgian study used a higher cut-off-point (90th percentile instead of the 60th percentile), which resulted in a lower prevalence. Two studies directly comparing differences between unaccompanied and accompanied children and adolescents tended to show higher point prevalence for depression for unaccompanied children and adolescents than for accompanied children (30.2% vs. 8.2–32.8% [different accompanied groups] [33] and 11.5–23.1% vs. 5.9–52.9% [gender] [38]).
Overall, the quality of evidence regarding the prevalence of depression in refugee and asylum-seeking children and adolescents is low (downgraded for risk of bias and inconsistency).
Anxiety disorder
We identified 16 studies including 3804 children and adolescents that assessed the point prevalence of anxiety disorders [25, 27, 30, 32, 33, 36, 41, 46, 56, 58, 60, 61, 65, 67, 71, 74]. The IQR for the anxiety disorder prevalence was 8.7–31.6% and the median was 15.0%. The largest study investigating 852 unaccompanied minors in the Netherlands [28] reported a point prevalence of anxiety disorder of 46.0% (95% CI 42.7%, 49.4%). Bronstein et al. [31] applied the same questionnaire (HSCL-37A with the same cut-off point) as Bean et al. [28] in a similar war-affected unaccompanied population from Afghanistan living in the UK (n = 214), but reported a lower prevalence of anxiety disorder, 34.6% (95% CI 28.5%, 41.2%). The differences in these results could be due to differences in the host country, sampling errors or gender differences; while Bronstein et al. [31] included only boys, Bean et al. [28] included boys (70%) and girls (30%). One study directly comparing differences between unaccompanied and accompanied children and adolescents, showed higher anxiety disorder prevalence in unaccompanied children (20.2%; 95% CI 14.0%, 28.1%) than in accompanied children (8.8%; 95% CI 6.8%, 11.2%) [33].
Overall, the quality of evidence regarding the prevalence of anxiety disorder in refugee and asylum-seeking children and adolescents is low (downgraded for risk of bias and inconsistency).
Suicidal ideation and behaviour
Four studies [39, 52, 55, 76] reported on suicidal ideation and behaviour of 1184 children and adolescents revealing a median of 5.0% and an IQR of 0.7–9.3%. Unclear risk of bias studies [39, 76] relying on the assessment of 139 children and adolescents using a clinical interview (M.I.N.I. Kid) revealed higher prevalence (9.2% and 9.8%) than the two high risk of bias studies. A Danish register-based study [55] assessed suicide attempts (0.9%, 95% CI 0.4%, 1.9%) and a Slovenian study investigated “the intention to kill oneself” (0.8%, 95% CI 0.2%, 3.0%) in a sample of refugee adolescents [52].
Overall, the quality of the evidence regarding the prevalence of suicidal ideation and behaviour of refugee and asylum-seeking children and adolescents is very low (due to risk of bias, imprecision and inconsistency).
Emotional and behavioural problems
Overall, 20 studies covering 3191 refugee or asylum-seeking children and adolescents reported on emotional and behavioural problems assessed with eight different self-report or proxy-questionnaires [25, 27, 30, 32, 35, 37, 41, 42, 44, 46, 48, 50, 54, 57, 59, 61, 66, 67, 71, 75]. The IQR of the point prevalence of emotional and behavioural problems is 19.8–35.0% and the median is 25.2%. The largest study [28] reported on prevalence of emotional and behavioural problems in 41.2% (95% CI 37.9%, 44.6%) of the participating unaccompanied children and adolescents living in the Netherlands.
Other outcomes
Few studies [36, 60] reported on point prevalence of other outcomes, such as hyper activeness (1.8–6%) or psychosomatic complaints (13%) [36], any psychiatric disorders as an overall category (13.4–41.9%) [46, 61], nocturnal enuresis (10.9%) [60], and dissociative psychopathology (36%) [72]. We could not identify any studies reporting on the prevalence of bipolar disorder, eating disorder, schizophrenia, and substance abuse of illicit drugs, alcohol and tobacco.
Discussion
Overall, the point prevalence of the investigated psychiatric disorders and mental health problems varied widely and showed that up to a third of refugee and asylum-seeking minors could be affected by either a depression or anxiety disorder or by any other emotional or behavioural problem. Furthermore, up to half of refugee and asylum-seeking minors could be affected by PTSD (IQR: 19.0–52.7%). In general, in comparison to the most up-to-date systematic review on this topic [16], we were able to identify ten additional studies. Nevertheless, the results were within a comparable range [15, 16].
In comparison to the general population, the prevalence of psychiatric disorders and mental health problems is substantially higher. As reported in a systematic review including 48 studies conducted in 27 countries and published from 1985 to 2012 and including a sample size of approximately 90,000 children and adolescents, the estimated worldwide point prevalence of diverse psychiatric disorders for children and adolescents [89] were reported to be lower than the above-mentioned results: The prevalence of any depressive disorder was 2.6% (95% CI 1.7%, 3.9%) and any anxiety disorder was 6.5% (95% CI 4.7%, 9.1%). The prevalence of suicidal behaviour (as a lifetime prevalence) in an Austrian mental health study was 1.8% (95% CI 0.6%, 3.0%) [90]. Furthermore, direct comparisons in our included studies showed that in general, refugee and asylum-seeking children and adolescents were to a greater extent affected by depression, anxiety, and emotional and behavioural problems [27, 40, 51, 68, 70] than native children and adolescents. These differences may be influenced by the different traumatizing experiences in the home country or during migration and diverse challenges or problems in the host country [6]. The literature highlights several pre-migration (e.g. exposure to poverty, violence, war and war-like conditions, but also acquired education, family, social and cultural values), peri-migration (e.g. exposure to traumatic events such as separation, sexual abuse, and trafficking) and post-migration (e.g. access to schooling, social support, stable settlement, parents mental health, insecurity during legal aspects of the immigration process, cultural adaptation) factors influencing the point prevalence of psychiatric disorders in children and adolescents [6, 47, 91].
Participants from most studies came from countries with wars (e.g. African states such as Somalia, Afghanistan, Balkan states), which could explain why prevalence estimates of PTSD (median: 35.5%, range 19.0–52.7%) were higher than for the other disorders. Our analyses also showed that unaccompanied minors revealed a higher risk of suffering from PTSD, depression, and anxiety disorders [33, 38, 63] than accompanied minors, which highlights the need for a special protection of this group. The association and complex interplay of migration factors with mental health disorders does, however, require an in-depth understanding which cannot be provided by the results of this review. The review rather provides a snapshot on mental health prevalence of different periods (over 30 years) in the younger European history.
Our systematic review showed a high heterogeneity of individual studies. This high variability of results was also found in other systematic reviews [92] and may be the result of several influencing methodological and clinical factors. From a methodological perspective, the included studies varied according to sample sizes, sampling strategies (random sampling or census studies versus non-random sampling), and assessment procedures. Structured clinical interviews relying on standard diagnostic criteria (DSM in different versions) tended to result in lower point prevalence in comparison with self-report or proxy-report questionnaires [93] (see Additional Material 4 for a list of the included instruments). These questionnaires may rather be seen as screening instruments that give an indication of a potential problem requiring further psychological or psychiatric investigation [15]. Furthermore, self-report questionnaires were sometimes used with different cut-off-values (e.g. SDQ [35, 44, 75] or the RATS [30, 33, 53]. From a clinical perspective, the studies comprised individuals from diverse social and cultural backgrounds residing in different host countries with varying legal and official support systems and asylum polices. It has recently been shown that the Western-based approach to psychiatric assessment simplifies the complex issue of migration [94].
Assessment and diagnosis difficulties could also explain why our review identified only very limited evidence on psychosomatic complaints. Questionnaires assessing psychosomatic complaints have shown to have moderate agreement with interviews, which are in themselves hampered by difficulties of patients to locate the discomfort or pain [95] and expectations to be treated for somatic symptoms on both patient’s and physician’s side [96]. Various symptoms have reportedly been associated with mental health disorders including constipation, amenorrhea or a dry mouth with depression, diarrhoea or hyperhidrosis with anxiety disorders, and quick respiration, palpitations, hyperhidrosis, and pain with PTSD [96]. Future studies should address the under-researched issue of psychosomatic complaints among asylum-seeking and refugee children and adolescents [6, 33, 38, 47, 63].
Overall, results of our study highlight the special attention that should be given to the mental health problems of refugee and asylum-seeking children and adolescents upon arrival, despite the fact that aspects of physical health tend to push themselves into the foreground [97]. As many young people are expected to show high levels of resilience, it is crucial to not only focus on therapeutic but also preventative actions to reduce psychological distress and promote social function and well-being [98]. These preventative actions range from a collaborative, political efforts to resolve conflict and war, to the training of professionals for work with refugees, and the respect of existing relationships, e.g. between parents and children [91]. Unaccompanied minors should receive special attention as they constitute a high-risk group. Upon arrival in the host country, rapid resolution of asylum claims as well as educational and employment opportunities are seen as important policy measures [6, 91]. Programs should further focus on family cohesion and peer and social support [99]. For therapeutic actions, facilitating an easier access to mental and physical health services may be essential by adapting to the refugees’ help-seeking behaviour, offering practical support and using interpreters [100–102]. Western-based approaches of care should shift to a more ecological culturally sensitive approach, accounting for the complexity of mental distress of refugee and asylum-seeking children and adolescents [94]. Effective core strategies for psychotherapeutic interventions with refugee minors are developing coping strategies, improving self-esteem, and rebuilding identity [103]. Where language barriers are prevalent, art-based interventions should be considered as they have proved to be equally effective as verbal interventions in reducing PTSD symptoms in refugee and asylum-seeking children and adolescents [104].
Our systematic review has several strengths. The greatest strength of our review is the comprehensive search strategy, including hand-searching of reference lists and contacting authors to receive additional data to calculate point prevalence. Moreover, we applied a rigorous methodologically sound systematic review process to address the review question. Nonetheless, we cannot be sure that we have detected every study on prevalence of psychiatric disorders in this population. Upon completion of this review, a new study on Syrian refugee children settled in Turkey was published, with prevalences of 47.9% for depression and 53.2% for anxiety disorders having only a slight impact on the prevalence ranges found for anxiety disorders (3.8–53.2% instead of 3.8–50.5%) [105]. The main weakness of our study is that we did not analyse the results considering gender and age differences or the legal status of children and adolescents (i.e. no differentiation between asylum seekers and refugees). Gender differences in psychiatric disorders were reported to be age-dependant: higher point prevalence was seen in boys than in girls younger than 13 years [90, 106]. Generally, the point prevalence of psychiatric disorders was not reported specifically regarding age and gender as well as the asylum status/immigration label [15] impeding additional analyses.
A considerably large problem is that the evidence base relies mainly on convenience samples not providing information if the investigated population is comparable to a countries young refugee and asylum-seeker population. Further effort needs to be undertaken to conduct representative studies. Currently, we are faced with a dearth of relevant prevalence data for several European countries (e.g. Austria, France, Germany, Hungary, Sweden, Switzerland, and Turkey), leaving the varying legal situations in host countries out of sight. Furthermore, there is an ongoing debate on whether mental illnesses and their symptomatology can be seen as a transcultural phenomenon and if levels of distress are expressed differently in different cultures [11, 107–109]. Some authors called for cautiousness [15]. To investigate potential cultural differences among five different linguistic groups, a large study in the Netherlands used the Harvard Trauma Questionnaire (HTQ) and the Hopkins Symptom Checklist (HSCL-25) for assessing PTSD and anxiety and depression [110]. The results showed good construct validity, indicating that different ways of expressing mental illnesses and their symptomatology might be less a problem than assumed.
Nevertheless, to take planning steps for guaranteeing an effective mental health care, it is important to improve the evidence base on refugees’ mental health in general and in particular for children and adolescents, as they are the most vulnerable group [13, 14, 16]. Research should continue to assess the cultural validity of often applied screening instruments for psychiatric disorders. Further steps should be undertaken to assess the screening instruments sensitivity and specificity to detect psychiatric disorders. To gain more precise estimates of the psychiatric disorder point prevalence, large studies using the same methodology (questionnaires, cut-off-values) based on similar samples regarding age, gender, asylum/immigration status, and countries of origin should be conducted.
In conclusion, the investigated refugee and asylum-seeking children and adolescents were affected by high levels of PTSD, but also by anxiety and depression disorders. As the results were highly heterogeneous, the evidence base could be improved by international methodologically comparable studies with sufficiently large sample sizes drawn randomly among specified refugee populations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We are very grateful to the authors of the studies for their time to provide additional data and further explanations. We also would like to thank Marlene Spatt for her administrative support. Open access funding provided by Danube University Krems University for Continuing Education.
Author contributions
CK, IS and GG devised the protocol for the review. CK coordinated the reviewing and data extraction process. IK conducted the literature search. AF, BK, CK, EK, IS, LG, MaS, MoS, PB, and RJ conducted the screening of articles and extracted data. CK performed the statistical analysis and drafted the manuscript; AF supported the writing of the introduction section, and IS supported the writing of the discussion section. All authors read, critically revised, and approved the final manuscript.
Funding
The research was funded by an internal grant of the University for Continuing Education (Danube-University Krems).
Compliance with ethical standards
Conflict of interest
The authors declare that they have no competing interests.
Contributor Information
Christina Kien, Phone: +43 2732 893 2917, Email: christina.kien@donau-uni.ac.at.
Isolde Sommer, Email: isolde.sommer@donau-uni.ac.at.
Anna Faustmann, Email: anna.faustmann@donau-uni.ac.at.
Lacey Gibson, Email: lag357@mail.harvard.edu.
Martha Schneider, Email: martha.schneider@uni-graz.at.
Eva Krczal, Email: eva.krczal@donau-uni.ac.at.
Robert Jank, Email: robert.jank@donau-uni.ac.at.
Irma Klerings, Email: irma.klerings@donau-uni.ac.at.
Monika Szelag, Email: monika.szelag@donau-uni.ac.at.
Bernd Kerschner, Email: bernd.kerschner@donau-uni.ac.at.
Petter Brattström, Email: petterbrattstrom@gmail.com.
Gerald Gartlehner, Email: gerald.gartlehner@donau-uni.ac.at.
References
- 1.Eurostat. Asylum and managed migration database (2018) http://ec.europa.eu/eurostat/web/asylum-and-managed-migration/data/database. Accessed 22 Mar 2018
- 2.Eurostat. Asylum statistics (2018) http://ec.europa.eu/eurostat/statistics-explained/index.php/Asylum_statistics. Accessed 19 Mar 2018
- 3.European Migration Network (EMN). Asylum and Migration Glossary 3.0 (2014) https://ec.europa.eu/home-affairs/sites/homeaffairs/files/what-we-do/networks/european_migration_network/docs/emn-glossary-en-version.pdf. Accessed 22 Mar 2018
- 4.United Nations Children´s Fund (UNICEF). A child is a child. Protecting children on the move from violence, abuse and exploitation. UNICEF, New York. 2017. Accessed 19 Mar 2018
- 5.Eurostat (2018) Asylum and first time asylum applicants. http://appsso.eurostat.ec.europa.eu/nui/submitViewTableAction.do. Accessed 22 Mar 2018
- 6.Fazel M, Reed RV, Panter-Brick C, Stein A. Mental health of displaced and refugee children resettled in high-income countries: risk and protective factors. Lancet. 2012;379(9812):266–282. doi: 10.1016/S0140-6736(11)60051-2. [DOI] [PubMed] [Google Scholar]
- 7.Spallek J, Razum O. Erklärungsmodelle für die gesundheitliche Situation von Migrantinnen und Migranten. In: Bauer U, Bittlingmayer UH, Richter M, editors. Health Inequalities. Wiesbaden: VS Verlag für Sozialwissenschaften; 2008. pp. 271–288. [Google Scholar]
- 8.Seglem KB, Oppedal B, Raeder S. Predictors of depressive symptoms among resettled unaccompanied refugee minors. Scand J Psychol. 2011;52(5):457–464. doi: 10.1111/j.1467-9450.2011.00883.x. [DOI] [PubMed] [Google Scholar]
- 9.Jensen TK, Skardalsmo EM, Fjermestad KW. Development of mental health problems—a follow-up study of unaccompanied refugee minors. Child Adolesc Psychiatry Ment Health. 2014;8:29. doi: 10.1186/1753-2000-8-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Walg M, Fink E, Großmeier M, Temprano M, Hapfelmeier G. The proportion of unaccompanied refugee minors suffering from psychiatric disorders in Germany (Häufi gkeit psychischer Störungen bei unbegleiteten minderjährigen Flüchtlingen in Deutschland) Zeitschrift für Kinder- und Jugendpsychiatrie und Psychotherapie. 2017;45(1):58–68. doi: 10.1024/1422-4917/a000459. [DOI] [PubMed] [Google Scholar]
- 11.Seglem KB, Oppedal B, Roysamb E. Daily hassles and coping dispositions as predictors of psychological adjustment: a comparative study of young unaccompanied refugees and youth in the resettlement country. Int J Behav Dev. 2014;38(3):293–303. doi: 10.1177/0165025414520807. [DOI] [Google Scholar]
- 12.Witt A, Rassenhofer M, Fegert JM, Plener PL. Demand for help and provision of services in the care of unaccompanied refugee minors: a systematic review (Hilfebedarf und Hilfsangebote in der Versorgung von unbegleiteten minderjährigen Flüchtlingen: eine systematische Übersicht) Kindheit und Entwicklung: Zeitschrift für Klinische Kinderpsychologie. 2015;24(4):209–224. doi: 10.1026/0942-5403/a000177. [DOI] [Google Scholar]
- 13.Hodes M, Vasquez MM, Anagnostopoulos D, Triantafyllou K, Abdelhady D, Weiss K, et al. Refugees in Europe: national overviews from key countries with a special focus on child and adolescent mental health. Eur Child Adolesc Psychiatry. 2017 doi: 10.1007/s00787-017-1094-8. [DOI] [PubMed] [Google Scholar]
- 14.Hebebrand J, Anagnostopoulos D, Eliez S, Linse H, Pejovic-Milovancevic M, Klasen H. A first assessment of the needs of young refugees arriving in Europe: what mental health professionals need to know. Eur Child Adolesc Psychiatry. 2016;25(1):1–6. doi: 10.1007/s00787-015-0807-0. [DOI] [PubMed] [Google Scholar]
- 15.Bronstein I, Montgomery P. Psychological distress in refugee children: a systematic review. Clin Child Fam Psychol Rev. 2011;14(1):44–56. doi: 10.1007/s10567-010-0081-0. [DOI] [PubMed] [Google Scholar]
- 16.van Os EC, Kalverboer ME, Zijlstra AE, Post WJ, Knorth EJ. Knowledge of the unknown child: a systematic review of the elements of the best interests of the child assessment for recently arrived refugee children. Clin Child Fam Psychol Rev. 2016;19(3):185–203. doi: 10.1007/s10567-016-0209-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Chapter 5: systematic reviews of prevalence and incidence. In: Aromatoris E, Munn Z, editors. Joanna Briggs Institute reviewer’s manual. Adelaide: The Joanna Briggs Institute; 2017. [Google Scholar]
- 18.Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647. doi: 10.1136/bmj.g7647. [DOI] [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Babineau J. Product review: covidence (Systematic Review Software). 2014. J Can Health Libr. 2014;35(2):4. doi: 10.5596/c14-016. [DOI] [Google Scholar]
- 21.Downes MJ, Brennan ML, Williams HC, Dean RS. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS) BMJ Open. 2016;6(12):e011458. doi: 10.1136/bmjopen-2016-011458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harder T, Takla A, Eckmanns T, Ellis S, Forland F, James R, et al. PRECEPT: an evidence assessment framework for infectious disease epidemiology, prevention and control. Euro Surveill. 2017 doi: 10.2807/1560-7917.es.2017.22.40.16-00620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Langer G, Meerpohl JJ, Perleth M, Gartlehner G, Kaminski-Hartenthaler A, Schunemann H. [GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables]. Zeitschrift fur Evidenz, Fortbildung und Qualitat im. Gesundheitswesen. 2012;106(5):357–368. doi: 10.1016/j.zefq.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 24.Almqvist K, Brandell-Forsberg M. Refugee children in Sweden: post-traumatic stress disorder in Iranian preschool children exposed to organized violence. Child Abuse Negl. 1997;21(4):351–366. doi: 10.1016/S0145-2134(96)00176-7. [DOI] [PubMed] [Google Scholar]
- 25.Angel B, Hjern A, Ingleby D. Effects of war and organized violence on children: a study of Bosnian refugees in Sweden. Am J Orthopsychiatry. 2001;71(1):4–15. doi: 10.1037/0002-9432.71.1.4. [DOI] [PubMed] [Google Scholar]
- 26.Barghadouch A, Carlsson J, Norredam M. Psychiatric disorders and predictors hereof among refugee children in early adulthood: a register-based cohort study. J Nerv Ment Dis. 2016;01:01. doi: 10.1097/NMD.0000000000000576. [DOI] [PubMed] [Google Scholar]
- 27.Bean T, Derluyn I, Eurelings-Bontekoe E, Broekaert E, Spinhoven P. Comparing psychological distress, traumatic stress reactions, and experiences of unaccompanied refugee minors with experiences of adolescents accompanied by parents. J Nerv Ment Dis. 2007;195(4):288–297. doi: 10.1097/01.nmd.0000243751.49499.93. [DOI] [PubMed] [Google Scholar]
- 28.Bean T, Eurelings-Bontekoe E, Mooijaart A, Spinhoven P. Factors associated with mental health service need and utilization among unaccompanied refugee adolescents. Adm Policy Ment Health. 2006;33(3):342–355. doi: 10.1007/s10488-006-0046-2. [DOI] [PubMed] [Google Scholar]
- 29.Begovac I, Rudan V, Begovac B, Vidovic V, Majic G. Self-image, war psychotrauma and refugee status in adolescents. Eur Child Adolesc Psychiatry. 2004;13(6):381–388. doi: 10.1007/s00787-004-0423-x. [DOI] [PubMed] [Google Scholar]
- 30.Bronstein I, Montgomery P, Dobrowolski S. PTSD in asylum-seeking male adolescents from Afghanistan. J Trauma Stress. 2012;25(5):551–557. doi: 10.1002/jts.21740. [DOI] [PubMed] [Google Scholar]
- 31.Bronstein I, Montgomery P, Ott E. Emotional and behavioural problems amongst Afghan unaccompanied asylum-seeking children: results from a large-scale cross-sectional study. Eur Child Adolesc Psychiatry. 2013;22(5):285–294. doi: 10.1007/s00787-012-0344-z. [DOI] [PubMed] [Google Scholar]
- 32.Derluyn I, Broekaert E. Different perspectives on emotional and behavioural problems in unaccompanied refugee children and adolescents. Ethn Health. 2007;12(2):141–162. doi: 10.1080/13557850601002296. [DOI] [PubMed] [Google Scholar]
- 33.Derluyn I, Mels C, Broekaert E. Mental health problems in separated refugee adolescents. J Adolesc Health. 2009;44(3):291–297. doi: 10.1016/j.jadohealth.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 34.Elklit A, Ostergard Kjaer K, Lasgaard M, Palic S. Social support, coping and posttraumatic stress symptoms in young refugees. Torture. 2012;22(1):11–23. [PubMed] [Google Scholar]
- 35.Fazel M, Stein A. Mental health of refugee children: comparative study. BMJ. 2003;327(7407):134. doi: 10.1136/bmj.327.7407.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goldin S, Hagglof B, Levin L, Persson LA. Mental health of Bosnian refugee children: a comparison of clinician appraisal with parent, child and teacher reports. Nord J Psychiatry. 2008;62(3):204–216. doi: 10.1080/08039480801983604. [DOI] [PubMed] [Google Scholar]
- 37.Hjern A, Angel B, Jeppson O. Political violence, family stress and mental health of refugee children in exile. Scand J Soc Med. 1998;26(1):18–25. doi: 10.1177/14034948980260010701. [DOI] [PubMed] [Google Scholar]
- 38.Hodes M, Jagdev D, Chandra N, Cunniff A. Risk and resilience for psychological distress amongst unaccompanied asylum seeking adolescents. J Child Psychol Psychiatry. 2008;49(7):723–732. doi: 10.1111/j.1469-7610.2008.01912.x. [DOI] [PubMed] [Google Scholar]
- 39.Huemer J, Karnik N, Voelkl-Kernstock S, Granditsch E, Plattner B, Friedrich M, et al. Psychopathology in African unaccompanied refugee minors in Austria. Child Psychiatry Hum Dev. 2011;42(3):307–319. doi: 10.1007/s10578-011-0219-4. [DOI] [PubMed] [Google Scholar]
- 40.Huemer J, Volkl-Kernstock S, Karnik N, Denny KG, Granditsch E, Mitterer M, et al. Personality and psychopathology in African unaccompanied refugee minors: repression, resilience and vulnerability. Child Psychiatry Hum Dev. 2013;44(1):39–50. doi: 10.1007/s10578-012-0308-z. [DOI] [PubMed] [Google Scholar]
- 41.Jensen TK, Fjermestad KW, Granly L, Wilhelmsen NH. Stressful life experiences and mental health problems among unaccompanied asylum-seeking children. Clin Child Psychol Psychiatry. 2015;20(1):106–116. doi: 10.1177/1359104513499356. [DOI] [PubMed] [Google Scholar]
- 42.Montgomery E. Long-term effects of organized violence on young Middle Eastern refugees’ mental health. Soc Sci Med. 2008;67(10):1596–1603. doi: 10.1016/j.socscimed.2008.07.020. [DOI] [PubMed] [Google Scholar]
- 43.Montgomery E. Trauma and resilience in young refugees: a 9-year follow-up study. Dev Psychopathol. 2010;22(2):477–489. doi: 10.1017/S0954579410000180. [DOI] [PubMed] [Google Scholar]
- 44.Nielsen SS, Norredam M, Christiansen KL, Obel C, Hilden J, Krasnik A. Mental health among children seeking asylum in Denmark–the effect of length of stay and number of relocations: a cross-sectional study. BMC Public Health. 2008;8:293. doi: 10.1186/1471-2458-8-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Oppedal B, Idsoe T. The role of social support in the acculturation and mental health of unaccompanied minor asylum seekers. Scand J Psychol. 2015;56(2):203–211. doi: 10.1111/sjop.12194. [DOI] [PubMed] [Google Scholar]
- 46.Papageorgiou V, Frangou-Garunovic A, Iordanidou R, Yule W, Smith P, Vostanis P. War trauma and psychopathology in Bosnian refugee children. Eur Child Adolesc Psychiatry. 2000;9(2):84–90. doi: 10.1007/s007870050002. [DOI] [PubMed] [Google Scholar]
- 47.Reijneveld SA, de Boer JB, Bean T, Korfker DG. Unaccompanied adolescents seeking asylum: poorer mental health under a restrictive reception. J Nerv Ment Dis. 2005;193(11):759–761. doi: 10.1097/01.nmd.0000185870.55678.82. [DOI] [PubMed] [Google Scholar]
- 48.Reis O, Jung P, Hasler F. Mental health in children from families seeking asylum in Mecklenburg-Western Pomerania 2007–2009: personal and contextual risk factors. Prax Kinderpsychol Kinderpsychiatr. 2016;65(10):729–743. doi: 10.13109/prkk.2016.65.10.729. [DOI] [PubMed] [Google Scholar]
- 49.Salari R, Malekian C, Linck L, Kristiansson R, Sarkadi A. Screening for PTSD symptoms in unaccompanied refugee minors: a test of the CRIES-8 questionnaire in routine care. Scand J Public Health. 2017;45(6):605–611. doi: 10.1177/1403494817715516. [DOI] [PubMed] [Google Scholar]
- 50.Sanchez-Cao E, Kramer T, Hodes M. Psychological distress and mental health service contact of unaccompanied asylum-seeking children. Child Care Health Dev. 2013;39(5):651–659. doi: 10.1111/j.1365-2214.2012.01406.x. [DOI] [PubMed] [Google Scholar]
- 51.Sikic N, Javornik N, Stracenski M, Bunjevac T, Buljan-Flander G. Psychopathological differences among three groups of school children affected by the war in Croatia. Acta Med Croatica. 1997;51(3):143–149. [PubMed] [Google Scholar]
- 52.Slodnjak V, Kos A, Yule W. Depression and parasuicide in refugee and Slovenian adolescents. Crisis. 2002;23(3):127–132. doi: 10.1027//0227-5910.23.3.127. [DOI] [PubMed] [Google Scholar]
- 53.Smid GE, Lensvelt-Mulders GJ, Knipscheer JW, Gersons BP, Kleber RJ. Late-onset PTSD in unaccompanied refugee minors: exploring the predictive utility of depression and anxiety symptoms. J Clin Child Adolesc Psychol. 2011;40(5):742–755. doi: 10.1080/15374416.2011.597083. [DOI] [PubMed] [Google Scholar]
- 54.Sourander A. Behavior problems and traumatic events of unaccompanied refugee minors. Child Abuse Negl. 1998;22(7):719–727. doi: 10.1016/S0145-2134(98)00053-2. [DOI] [PubMed] [Google Scholar]
- 55.Staehr MA, Munk-Andersen E. Suicide and suicidal behavior among asylum seekers in Denmark during the period 2001–2003. A retrospective study. Ugeskr Laeger. 2006;168(17):1650–1653. [PubMed] [Google Scholar]
- 56.Vervliet M, Meyer Demott MA, Jakobsen M, Broekaert E, Heir T, Derluyn I. The mental health of unaccompanied refugee minors on arrival in the host country. Scand J Psychol. 2014;55(1):33–37. doi: 10.1111/sjop.12094. [DOI] [PubMed] [Google Scholar]
- 57.Wiegersma PA, Stellinga-Boelen AA, Reijneveld SA. Psychosocial problems in asylum seekers’ children: the parent, child, and teacher perspective using the strength and difficulties questionnaire. J Nerv Ment Dis. 2011;199(2):85–90. doi: 10.1097/NMD.0b013e31820446d2. [DOI] [PubMed] [Google Scholar]
- 58.Yurtbay T, Alyanak B, Abali O, Kaynak N, Durukan M. The psychological effects of forced emigration on Muslim Albanian children and adolescents. Community Ment Health J. 2003;39(3):203–212. doi: 10.1023/A:1023386122344. [DOI] [PubMed] [Google Scholar]
- 59.Rucker S, Buttner P, Lambertz B, Karpinski N, Petermann F. Resilient or risk group? Psychological burden at unaccompanied refugee minors (URM) in Germany. Prax Kinderpsychol Kinderpsychiatr. 2017;66(4):242–258. doi: 10.13109/prkk.2017.66.4.242. [DOI] [PubMed] [Google Scholar]
- 60.Nasiroglu S, Ceri V. Posttraumatic stress and depression in Yazidi refugees. Neuropsychiatr Dis Treat. 2016;12:2941–2948. doi: 10.2147/NDT.S119506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jakobsen M, Meyer DeMott MA, Wentzel-Larsen T, Heir T. The impact of the asylum process on mental health: a longitudinal study of unaccompanied refugee minors in Norway. BMJ Open. 2017;7(6):e015157. doi: 10.1136/bmjopen-2016-015157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sleijpen M, Haagen J, Mooren T, Kleber RJ. Growing from experience: an exploratory study of posttraumatic growth in adolescent refugees. Eur J Psychotraumatol. 2016;7:28698. doi: 10.3402/ejpt.v7.28698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Stotz SJ, Elbert T, Muller V, Schauer M. The relationship between trauma, shame, and guilt: findings from a community-based study of refugee minors in Germany. Eur J Psychotraumatol. 2015;6:25863. doi: 10.3402/ejpt.v6.25863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jakobsen M, Demott MA, Heir T. Prevalence of psychiatric disorders among unaccompanied asylum-seeking adolescents in norway. Clin Pract Epidemol Ment Health. 2014;10:53–58. doi: 10.2174/1745017901410010053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Taurino A, Vergatti LV, Colavitto MT, Bastianoni P, Godelli S, Del Castello E. The unaccompanied foreign minors between trauma and repair interventions. A study on post-traumatic stress disorder, anxiety, depression and dissociative tendencies in young migrants living in community health centers (I minori stranieri non accompagnati tra trauma e riparazione. Uno studio su disturbo post-traumatico da stress, ansia, depressione e tendenze dissociative in giovani migranti residenti in comunità) Infanzia e Adolescenza. 2012;11(1):47–64. [Google Scholar]
- 66.Thommessen S, Laghi F, Cerrone C, Baiocco R, Todd BK. Internalizing and externalizing symptoms among unaccompanied refugee and Italian adolescents. Child Youth Ser Rev. 2013;35(1):7–10. doi: 10.1016/j.childyouth.2012.10.007. [DOI] [Google Scholar]
- 67.Adam H, Klasen F. Trauma and reconciliation: child refugees in Hamburg (Trauma und Versöhnung: Versöhnungsbereitschaft bei traumatisierten. Flüchtlingskindern) Trauma Gewalt. 2011;5(4):356–369. [Google Scholar]
- 68.Gavranidou M, Niemiec B, Magg B, Rosner R. Traumatic experiences, current living conditions, and psychological distress symptoms among adolescent refugees (Traumatische erfahrungen, aktuelle lebensbedingungen im exil und psychische belastung junger flüchtlinge) Kindheit und Entwicklung: Zeitschrift für Klinische Kinderpsychologie. 2008;17(4):224–231. doi: 10.1026/0942-5403.17.4.224. [DOI] [Google Scholar]
- 69.Staehr MA. Psychoeducation with Kosovo Albanian refugee children (Psykoedukation med Kosovo Albanske flygtningebørn: en effektundersøgelse af et program til forebyggelse af alvorlige psykiske belastningsreaktioner) Psyke Logos. 2001;22(1):127–146. [Google Scholar]
- 70.Kocijan-Hercigonja D, Rijavec M, Maruŝić A, Hercigonja V. Coping strategies of refugee, displaced, and non-displaced children in a war area. Nord J Psychiatry. 1998;52(1):45–50. doi: 10.1080/080394898422562. [DOI] [Google Scholar]
- 71.Hollins K, Heydari H, Grayson K, Leavey G. The mental health and social circumstances of Kosovan Albanian and Albanian unaccompanied refugee adolescents living in London. Divers Health Soc Care. 2007;4(4):277–285. [Google Scholar]
- 72.Gušić S, Cardeña E, Bengtsson H, Søndergaard HP. Dissociative experiences and trauma exposure among newly arrived and settled young war refugees. J Aggress Maltreat Trauma. 2017;26:1–18. doi: 10.1080/10926771.2017.1365792. [DOI] [Google Scholar]
- 73.Sabuncuoǧlu O, Berkem M. Emotional state of Bosnian refugee and immigrant children in Turkey. Marmara Med J. 2002;15(2):103–107. [Google Scholar]
- 74.Longobardi C, Veronesi TG, Prino LE. Abuses, resilience, behavioural problems and post-traumatic stress symptoms among unaccompanied migrant minors: an Italian cross-sectional exploratory study. Psychiatria i Psychologia Kliniczna. 2017;17(2):87–92. doi: 10.15557/PiPK.2017.0009. [DOI] [Google Scholar]
- 75.Möhrle B, Dölitzsch C, Fegert JM, Keller F. Emotional and behavioral problems and quality of life in unaccompanied adolescent male refugees residing in institutional care. Kindheit Entwickl. 2016;25(4):204–215. doi: 10.1026/0942-5403/a000206. [DOI] [Google Scholar]
- 76.Ruf M, Schauer M, Elbert T. Prevalence of traumatic stress and mental health problems in children of asylum seekers in Germany. Z Klin Psychol Psychother. 2010;39(3):151–160. doi: 10.1026/1616-3443/a000029. [DOI] [Google Scholar]
- 77.Almqvist K, Broberg AG. Mental health and social adjustment in young refugee children 3 1/2 years after their arrival in Sweden. J Am Acad Child Adolesc Psychiatry. 1999;38(6):723–730. doi: 10.1097/00004583-199906000-00020. [DOI] [PubMed] [Google Scholar]
- 78.Bean TM, Eurelings-Bontekoe E, Spinhoven P. Course and predictors of mental health of unaccompanied refugee minors in the Netherlands: one year follow-up. Soc Sci Med. 2007;64(6):1204–1215. doi: 10.1016/j.socscimed.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 79.Begovac I, Begovac B, Rudan V. Self-image and refugee status in adolescents from Bosnia and Herzegovina and Croatia. Coll Antropol. 2003;27(Suppl 1):135–145. [PubMed] [Google Scholar]
- 80.Hjern A, Angel B. Organized violence and mental health of refugee children in exile: a six-year follow-up. Acta Paediatr. 2000;89(6):722–727. doi: 10.1111/j.1651-2227.2000.tb00372.x. [DOI] [PubMed] [Google Scholar]
- 81.Keles S, Friborg O, Idsoe T, Sirin S, Oppedal B. Depression among unaccompanied minor refugees: the relative contribution of general and acculturation-specific daily hassles. Ethn Health. 2016;21(3):300–317. doi: 10.1080/13557858.2015.1065310. [DOI] [PubMed] [Google Scholar]
- 82.Keles S, Idsoe T, Friborg O, Sirin S, Oppedal B. The longitudinal relation between daily hassles and depressive symptoms among unaccompanied refugees in Norway. J Abnorm Child Psychol. 2016;26:26. doi: 10.1007/s10802-016-0251-8. [DOI] [PubMed] [Google Scholar]
- 83.Montgomery E, Foldspang A. Discrimination, mental problems and social adaptation in young refugees. Eur J Public Health. 2008;18(2):156–161. doi: 10.1093/eurpub/ckm073. [DOI] [PubMed] [Google Scholar]
- 84.Nielsen SS, Norredam M, Christensen KL, Obel C, Krasnik A. The mental health of asylum-seeking children in Denmark. Ugeskr Laeger. 2007;169(43):3660–3665. [PubMed] [Google Scholar]
- 85.Nielsen SS, Norredam M, Christiansen KL, Obel C, Hilden J, Krasnik A. The effect of length of stay and number of relocations on asylum-seeking children’s mental health–secondary publication. Ugeskr Laeger. 2009;171(12):981–984. [PubMed] [Google Scholar]
- 86.Oppedal B, Idsoe T. Conduct problems and depression among unaccompanied refugees: the association with pre-migration trauma and acculturation. Anales de Psicología. 2012;28(3):683–694. doi: 10.6018/analesps.28.3.155981. [DOI] [Google Scholar]
- 87.Vervliet M, Lammertyn J, Broekaert E, Derluyn I. Longitudinal follow-up of the mental health of unaccompanied refugee minors. Eur Child Adolesc Psychiatry. 2014;23(5):337–346. doi: 10.1007/s00787-013-0463-1. [DOI] [PubMed] [Google Scholar]
- 88.Volkl-Kernstock S, Karnik N, Mitterer-Asadi M, Granditsch E, Steiner H, Friedrich MH, et al. Responses to conflict, family loss and flight: posttraumatic stress disorder among unaccompanied refugee minors from Africa. Neuropsychiatrie. 2014;28(1):6–11. doi: 10.1007/s40211-013-0094-2. [DOI] [PubMed] [Google Scholar]
- 89.Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015;56(3):345–365. doi: 10.1111/jcpp.12381. [DOI] [PubMed] [Google Scholar]
- 90.Wagner G, Zeiler M, Waldherr K, Philipp J, Truttmann S, Dur W, et al. Mental health problems in Austrian adolescents: a nationwide, two-stage epidemiological study applying DSM-5 criteria. Eur Child Adolesc Psychiatry. 2017;26(12):1483–1499. doi: 10.1007/s00787-017-0999-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Pejovic-Milovancevic M, Klasen H, Anagnostopoulos D. ESCAP for mental health of child and adolescent refugees: facing the challenge together, reducing risk, and promoting healthy development. Eur Child Adolesc Psychiatry. 2018;27(2):253–257. doi: 10.1007/s00787-017-1064-1. [DOI] [PubMed] [Google Scholar]
- 92.Turrini G, Purgato M, Ballette F, Nose M, Ostuzzi G, Barbui C. Common mental disorders in asylum seekers and refugees: umbrella review of prevalence and intervention studies. Int J Ment Health Syst. 2017;11:51. doi: 10.1186/s13033-017-0156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Fazel M, Wheeler J, Danesh J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. Lancet. 2005;365(9467):1309–1314. doi: 10.1016/S0140-6736(05)61027-6. [DOI] [PubMed] [Google Scholar]
- 94.Villanueva O’Driscoll J, Serneels G, Imeraj L. A file study of refugee children referred to specialized mental health care: from an individual diagnostic to an ecological perspective. Eur Child Adolesc Psychiatry. 2017;07:07. doi: 10.1007/s00787-017-0981-3. [DOI] [PubMed] [Google Scholar]
- 95.Murray AM, Toussaint A, Althaus A, Löwe B. The challenge of diagnosing non-specific, functional, and somatoform disorders: a systematic review of barriers to diagnosis in primary care. J Psychosom Res. 2016;80:1–10. doi: 10.1016/j.jpsychores.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 96.Rohlof HG, Knipscheer JW, Kleber RJ. Somatization in refugees: a review. Soc Psychiatry Psychiatric Epidemiol. 2014;49(11):1793–1804. doi: 10.1007/s00127-014-0877-1. [DOI] [PubMed] [Google Scholar]
- 97.Marquardt L, Kramer A, Fischer F, Prufer-Kramer L. Health status and disease burden of unaccompanied asylum-seeking adolescents in Bielefeld, Germany: cross-sectional pilot study. Trop Med Int Health. 2016;21(2):210–218. doi: 10.1111/tmi.12649. [DOI] [PubMed] [Google Scholar]
- 98.Hodes M, Anagnostopoulos D, Skokauskas N. Challenges and opportunities in refugee mental health: clinical, service, and research considerations. Eur Child Adolesc Psychiatry. 2018;27(4):385–388. doi: 10.1007/s00787-018-1115-2. [DOI] [PubMed] [Google Scholar]
- 99.Horlings A, Hein I. Psychiatric screening and interventions for minor refugees in Europe: an overview of approaches and tools. Eur J Pediatr. 2018;177(2):163–169. doi: 10.1007/s00431-017-3027-4. [DOI] [PubMed] [Google Scholar]
- 100.de Anstiss H, Ziaian T, Procter N, Warland J, Baghurst P. Help-seeking for mental health problems in young refugees: a review of the literature with implications for policy, practice, and research. Transcult Psychiatry. 2009;46(4):584–607. doi: 10.1177/1363461509351363. [DOI] [PubMed] [Google Scholar]
- 101.Betancourt TS, Frounfelker R, Mishra T, Hussein A, Falzarano R. Addressing health disparities in the mental health of refugee children and adolescents through community-based participatory research: a study in 2 communities. Am J Public Health. 2015;105(Suppl 3):S475–S482. doi: 10.2105/ajph.2014.302504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Cheng IH, Drillich A, Schattner P. Refugee experiences of general practice in countries of resettlement: a literature review. Br J Gen Pract. 2015;65(632):e171–e176. doi: 10.3399/bjgp15X683977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Demazure G, Gaultier S, Pinsault N. Dealing with difference: a scoping review of psychotherapeutic interventions with unaccompanied refugee minors. Eur Child Adolesc Psychiatry. 2017 doi: 10.1007/s00787-017-1083-y. [DOI] [PubMed] [Google Scholar]
- 104.Khan K (2017) Evidence on interventions that improve mental health of child refugees and child asylum seekers in Europe: a rapid systematic review [MPH Thesis]. Maastricht University, Maastricht, Netherlands
- 105.Kandemir H, Karatas H, Ceri V, Solmaz F, Kandemir SB, Solmaz A. Prevalence of war-related adverse events, depression and anxiety among Syrian refugee children settled in Turkey. Eur Child Adolesc Psychiatry. 2018 doi: 10.1007/s00787-018-1178-0. [DOI] [PubMed] [Google Scholar]
- 106.Ihle W, Esser G. Epidemiologie psychischer Störungen im Kindes- und Jugendalter: Prävalenz, Verlauf, Komorbidität und Geschlechtsunterschiede. Epidemiology of mental disorders in childhood and adolescence: prevalence, course, comorbidity and gender differences. Psychologische Rundschau. 2002;53(4):159–169. doi: 10.1026//0033-3042.53.4.159. [DOI] [Google Scholar]
- 107.Kleinman A. Anthropology and psychiatry. The role of culture in cross-cultural research on illness. Br J Psychiatry. 1987;151:447–454. doi: 10.1192/bjp.151.4.447. [DOI] [PubMed] [Google Scholar]
- 108.Summerfield D. Childhood, war, refugeedom and ‘trauma’: three core questions for mental health professionals. Transcult Psychiatry. 2000;37(3):417–433. doi: 10.1177/136346150003700308. [DOI] [Google Scholar]
- 109.Silove D, Austin P, Steel Z. No refuge from terror: the impact of detention on the mental health of trauma-affected refugees seeking asylum in Australia. Transcult Psychiatry. 2007;44(3):359–393. doi: 10.1177/1363461507081637. [DOI] [PubMed] [Google Scholar]
- 110.Wind TR, van der Aa N, de la Rie S, Knipscheer J. The assessment of psychopathology among traumatized refugees: measurement invariance of the Harvard trauma questionnaire and the Hopkins symptom checklist-25 across five linguistic groups. Eur J Psychotraumatol. 2017;8(sup2):1321357. doi: 10.1080/20008198.2017.1321357. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.