Abstract
Research into neutrophil biology in the last 10 years has uncovered a number of unexpected aspects of this still mysterious innate immune cell. Advances in technology have allowed visualisation of neutrophil trafficking to sites of inflammation, and, remarkably, neutrophils have been observed to depart from the scene in what has been termed reverse migration. There has also been increasing appreciation of the heterogeneity of neutrophils with ongoing categorisation of neutrophil subsets, including myeloid-derived suppressor cells and low-density granulocytes. Newly recognised neutrophil functions include the ability to release novel immune mediators such as extracellular DNA and microvesicles. Finally, studies of neutrophil cell death, both apoptotic and non-apoptotic, have revealed remarkable differences compared to other cell types. This review will highlight important discoveries in these facets of neutrophil biology and how the new findings will inform treatment of diseases where neutrophils are implicated.
Keywords: Apoptosis, Host defence, Inflammation, Neutrophil
Introduction
The neutrophil has long been recognised as a pivotal player in the innate immune response. Neutrophils employ well-characterised strategies of phagocytosis, reactive oxygen species (ROS) generation and release of pro-inflammatory mediators to provide the critical first-line defence against pathogens. At the end of their lives, neutrophils undergo apoptosis, an orderly programmed dismantling of the cell, are phagocytosed and promote the resolution of inflammation [1]. In the last 10 years, there has been a growing appreciation that neutrophils play roles beyond this relatively simplistic schema (Fig. 1). Investigation of neutrophil trafficking using intravital microscopy has allowed researchers to monitor diapedesis and migration in vivo, leading to novel paradigms in homing and trafficking. Furthermore, within the population of neutrophils, there are subsets that differ in phenotype and functionality, and there has been growing appreciation that neutrophils can modulate the function of other immune cells [2]. This integrated role of neutrophils acting within the immune system is highlighted by their importance in autoimmune diseases [3]. This review will focus on progress in the understanding of several facets of neutrophil biology that reflect these new roles and functions [4].
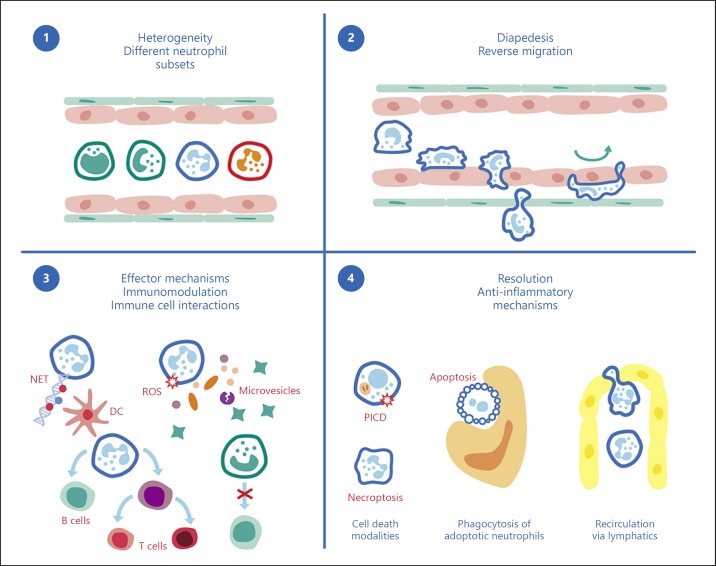
Fig. 1.
Schematic overview of neutrophils. (1) Neutrophil heterogeneity: in inflammatory or pathological conditions, neutrophil subsets have been characterised as including immature neutrophils, hypersegmented neutrophils, low-density granulocytes and granulocyte myeloid-derived suppressor cells. (2) Neutrophil diapedesis: transendothelial migration (rolling, adhesion, crawling and migration to inflamed sites) and reverse migration (returning to the circulation after having migrated into tissues). (3) Effector mechanisms of neutrophils: oxidative burst with production of superoxides, hydrogen peroxide (reactive oxygen species [ROS]) and hypochlorous acid; release of anti-pathogen proteases, defensins, cytokines and chemokines; release of specialised pro-resolving molecules, neutrophil extracellular traps (NETs) and neutrophil microvesicles; and phagocytic clearance of bacterial and cell debris. Neutrophils interact with dendritic cells (DCs), B lymphocytes, natural killer cells, T lymphocytes and endothelial cells and thus influence both the innate and adaptive immune responses. (4) Resolution of inflammation: the modality of cell death (e.g., phagocytosis-induced cell death [PICD], necroptosis and apoptosis) may influence the response of surrounding tissue cells and either perpetuate inflammation or promote resolution. Macrophage efferocytosis of apoptotic neutrophils favours the resolution of inflammation. Recirculation of neutrophils shuttling antigens in lymphatics shapes the adaptive immune response. Interference with or defects in these pro-resolving mechanisms may promote inflammation and autoimmunity.
Neutrophil Trafficking and Homing: No More a One-Way Trip
Neutrophil migration to sites of inflammation has until recently been characterised as a linear progression of intravascular rolling, tethering and adhesion before irreversible diapedesis into tissues [5]. This schema has recently been challenged, particularly in respect to tissue migration. In a number of model systems taking advantage of significant progress in in vivo imaging, reverse migration of neutrophils from tissues back into the circulation has been observed and characterised [6, 7]. The ability to migrate back across the endothelial cell layer is dependent on neutrophil-derived neutrophil elastase-degrading JAM-C, a key endothelial adhesion molecule [8, 9]. The fate of neutrophils after migrating to the site of sterile inflammation was further characterised using similar in vivo two-photon strategies [10]. Once again, moving away from the dogma that neutrophils reach the end of their lifespan at the site of inflammation and either die or are phagocytosed, neutrophils were observed to re-enter the vasculature, migrate to the lungs initially and then home to the bone marrow, where they underwent apoptosis. With this new technology, it remains to be studied whether there is a dominant pattern of neutrophil behaviour in all forms of inflammation or whether the context, in particular sterile and non-sterile, drives different migration patterns. Species-specific effects also need to be considered, although at this time, in the absence of the ability to deeply study neutrophil dynamics in humans, paradigms will continue to be guided by animal models.
At this stage, the importance of this mechanism in the process of inflammation remains to be firmly established. Reverse migration has the potential to be deleterious, allowing localised inflammation to disseminate [9]. Alternatively, encouraging neutrophil egress from sites of inflammation could serve as a pro-resolving mechanism, as demonstrated in a zebra fish model [6]. Answering these key questions in reference to human disease will determine how best to harness reverse migration for therapeutic purposes.
Neutrophil Heterogeneity - Not All Neutrophils Are Equal
Recent research suggests that the neutrophil population is not made up of homogeneous innate effector cells. On the contrary, analogous to subsets identified amongst lymphoid cells and myeloid cells [11], there may be subsets of neutrophils with potentially important differences in function.
Neutrophil phenotype analysis has been investigated in various conditions including inflammation, autoimmune disease and malignancy. Agreement remains to be reached on the exact nature of these neutrophil subtypes, particularly in regard to cell surface phenotype and whether these subtypes are conserved across species. However, the data are clear that neutrophils do not comprise one uniform population and that this heterogeneity is reflected not only in differences in cell surface marker phenotype but more importantly in function.
One neutrophil subtype of interest is the granulocyte myeloid-derived suppressor cell (G-MDSC). MDSCs comprise a heterogeneous population of cells possessing suppressive capacity and may be derived from both granulocytes and monocytes [12]. Suppression of T cells has been most extensively studied, and potential mechanisms include the release of ROS, nitric oxide and arginase and contact-mediated suppression. The suppressive function of G-MDSCs has been most extensively studied in the context of cancer. In different studies, tumour-infiltrating neutrophils have been found to both promote and inhibit malignancy through mechanisms targeting other immune cells, stromal cells and the tumour itself [13]. In particular tumours, a high circulating neutrophil-to-lymphocyte ratio and the number of neutrophils within the tumour have been identified as poor prognostic indicators suggesting that granulocytes may play a role in cancer progression [14]. The relative role in cancer pathogenesis of subpopulations of granulocytes, and MDSCs in particular, is the subject of ongoing studies.
Low-Density Granulocytes
Over many years, it has been noted that under certain inflammatory conditions, neutrophils can be found in the mononuclear cell fraction of Ficoll gradient separation [15]. These cells, so-called low-density granulocytes (LDGs) or low-density neutrophils, have been better characterised over the last decade, but further research is needed to fully understand their role in various diseases. One study investigated the nature of these cells in humans treated with granulocyte colony-stimulating factor (G-CSF), conducted to mobilise haemopoietic stem cells [16]. Under these conditions, a large percentage of granulocytes are found in the polymorphonuclear cell fraction of Ficoll-separated blood. Intriguingly, both the low-density and normal-density neutrophils demonstrated heterogeneity, primarily in relation to the presence of immature neutrophils characterised in this study by the absence of the surface marker CD10. The mature neutrophils released by G-CSF treatment demonstrated T-cell suppressive activity, whereas the immature cells promoted T-cell survival and proliferation. The pathologic relevance of these cells remains to be established, but G-CSF appears responsible for the mobilisation of neutrophils in certain tumours to promote metastases [17].
In sepsis, LDGs are expanded and have been found to exhibit MDSC characteristics [18]. High levels of G-MDSCs in sepsis predicted subsequent secondary infections, providing one hypothesis for the relative immune suppression that is seen in sepsis. The other scenario in which LDGs are present in significant numbers is in inflammatory diseases, best characterised in systemic lupus erythematosus (SLE) [19]. The LDGs in SLE patients express pro-inflammatory genes driven by type 1 interferons and undergo more rapid cell death than healthy control neutrophils [20, 21]. This cell death, possibly triggered by immune complexes, results in the extracellular release of both nuclear DNA and oxidised mitochondrial DNA [22] in conjunction with neutrophil proteins including LL-37 and HMGB1. These structures in turn are bound by autoantibodies, commonly found in the blood of SLE patients, and this leads to their uptake by plasmacytoid dendritic cells and stimulation of interferon production. This vicious cycle of interferon-driven neutrophil activation is proposed to be a potential target of therapeutic intervention in SLE [23].
LDGs have also been found in the circulation of patients with rheumatoid arthritis (RA). In the case of RA, LDGs are an immature subset with prolonged survival but relatively low rates of NETosis and lower response to cytokine stimulation. Of note, exogenous G-CSF as described above induces LDGs, and G-CSF may play an important role in RA, with antagonism to G-CSF being considered as a therapeutic target [24].
These studies suggest that the phenotype of LDGs may vary depending on the disease context. Describing LDGs in other contexts will be important in order to understand their role and whether they may serve as therapeutic targets in inflammation and other diseases. Future study will be facilitated by finding other markers of LDGs, which can currently only be assessed using Ficoll gradient separation.
Age as a Source of Neutrophil Heterogeneity
Young Neutrophils
Release of immature neutrophil forms into the circulation during infection leading to the appearance of band forms during haematological testing is well known, termed left shift by Joseph Arneth in 1904 [25]. Some recent studies have characterised these cells. A study of bone marrow neutrophils in mice using advanced cell cytometric techniques identified a dedicated pre-neutrophil population capable of differentiating into mature and immature neutrophils (based on CXCR2 status) [26]. This pre-neutrophil responded to systemic stressors of inflammation and malignancy by proliferating and providing a sustained neutrophil response in blood and tissues. This population were also present in the spleen and markedly expanded under the same stressors. Notably no immature neutrophils were present in the blood under steady-state conditions, but they were present in malignancy. CD101 was identified as a positive marker of immature murine neutrophils. Immature neutrophils were also mobilised with G-CSF.
Another study employed a human in vivo model of sepsis coupled with deuterium labelling of neutrophils to establish the timing of release of neutrophils from the bone marrow following cell division, at which time the deuterium is incorporated into DNA. With lipopolysaccharide treatment, an immature banded neutrophil population was identified and two separate mature populations were released into the circulation [27]. The immature cells released under systemic lipopolysaccharide treatment were demonstrated to be 2 days younger than the mature population. The mature neutrophil subsets were separated based on CD62L labelling, and the differences were validated by demonstration of significantly different proteomic profiles, pointing towards important functional differences that remain to be demonstrated.
Old Neutrophils
Ageing neutrophils are also present in the circulation, and increasing evidence suggests they behave differently from their younger counterparts. A paper by Casanova-Acebes et al. [28] demonstrated this ageing of neutrophils in mice in vivo. Ageing neutrophils expressed high levels of CXCR4, previously identified as being upregulated during in vitro ageing of neutrophils. The neutrophils were also CD62lo and are eliminated from the circulation in a circadian fashion by bone marrow macrophages. This clearance in turn provides the impetus to the further release of neutrophils.
Physiologic neutrophil ageing appears to be governed by the microbiome [29]. In sickle cell disease, a chronic inflammatory condition, numbers of circulating aged neutrophils were significantly elevated in both a mouse model and in affected patients. These aged neutrophils unexpectedly possess a pro-inflammatory phenotype, in contrast to neutrophils aged in vitro, which exhibit a downregulated functionality [30]. Aged neutrophils have enhanced integrin activation and release neutrophil extracellular traps under inflammatory conditions. Of note, antibiotic treatment abrogated the increase in aged neutrophils under these conditions and consequently reduced the impact of inflammation reflected by less vascular occlusion and fibrosis.
New Ways to Die - Neutrophil Cell Death
Neutrophils have a relatively short lifespan in the circulation, estimated at 5 days [31]. The rate and mode of neutrophil death has been studied intensively over the last decade. New insights have been gained into the mechanisms of neutrophil apoptosis and the potential anti- inflammatory consequences of promoting accelerated apoptosis. Furthermore, non-apoptotic forms of neutrophil cell death have been identified that may lead to pro-inflammatory consequences in both infective and autoimmune diseases [32].
Neutrophil Apoptosis
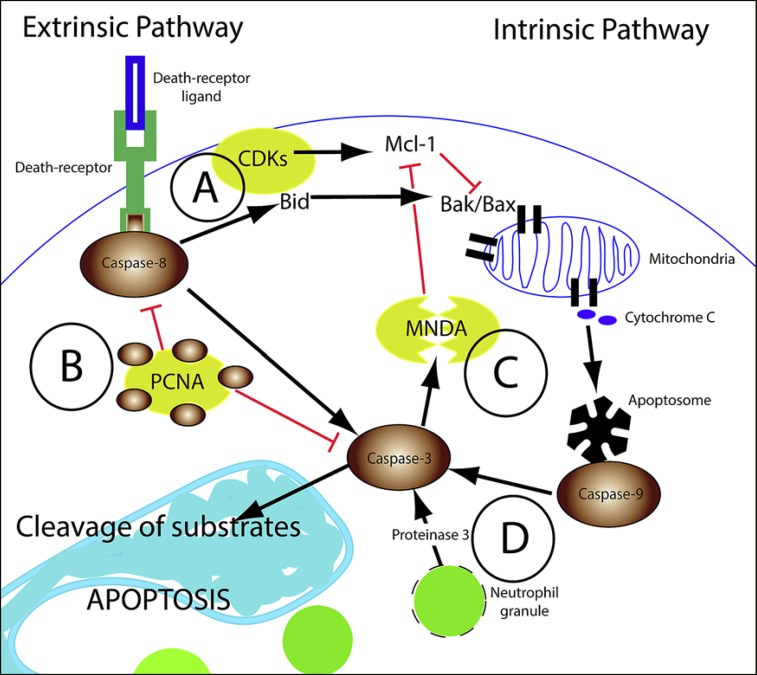
The exact mechanisms behind spontaneous neutrophil apoptosis have not yet been defined, although a number of recent studies have highlighted unexpected pathways to apoptosis (Fig. 2). Neutrophils do not appear to employ the same cell death pathways characterised by other cell types [33]. The anti-apoptotic protein Mcl-1 is abundantly expressed in neutrophils and may play a role in governing the timing of apoptosis [34], whereas Bcl2, the founding member of this family of anti-apoptotic proteins and widely expressed in other cell types, is not expressed in mature neutrophils [35].
Fig. 2.
Neutrophil apoptotic pathways. A simplified schematic of the intrinsic and extrinsic pathways of apoptosis with specific emphasis on the main factors involved in neutrophil apoptosis. Novel mediators of neutrophil apoptosis are: (A) cyclin-dependent kinases (CDKs) that inhibit Mcl-1 degradation and reduce apoptosis; (B) proliferating cell nuclear antigen (PCNA), which sequesters pro-caspases to prevent their activation; (C) myeloid cell nuclear differentiation antigen (MNDA), which is cleaved by caspase-3 and the cleaved product promotes Mcl-1 proteasomal degradation; and (D) proteinase 3, which leaks from the granules of aging neutrophils to directly cleave caspase-3 and activate the apoptotic programme.
Caspases are important in the execution phase of spontaneous apoptosis, but the mechanism by which they become cleaved and activated in neutrophils is not clear. A recent paper highlighted a novel role for the neutrophil serine protease proteinase 3 (PR3) as a mediator of spontaneous neutrophil apoptosis. With neutrophil ageing, the study found that PR3, normally sequestered within neutrophil granules, is released into the cytoplasm, where it is able to cleave caspase 3, inducing apoptosis. The role of PR3 was demonstrated in vivo using adoptive transfer of PR3-deficient and -sufficient neutrophils in the inflammatory context of thioglycolate peritonitis. PR3-deficient neutrophils survived longer than wild-type PR3-sufficient neutrophils [36]. In contrast, our recent study using novel transgenic mice expressing human PR3 (whose enzymatic activity is different from its murine counterpart) showed a defect in the resolution of inflammation associated with an increased survival of neutrophils expressing human PR3. Furthermore, transgenic mice expressing human PR3 have an increased mortality during sepsis [37].
Ingestion of apoptotic neutrophils by macrophages has the ability to downregulate the inflammatory response through modification of macrophage function [38]. However, when PR3 is expressed at the neutrophil membrane in an inflammatory context, it alters the nature of phagocytosis by macrophages, promoting a pro-inflammatory rather than anti-inflammatory response [39]. This mechanism appears to be of relevance in anti-neutrophil cytoplasmic antibody-associated vasculitis, a severe inflammatory disorder characterised by the presence of circulating autoantibodies against neutrophil granule enzymes including PR3 [40].
Along with PR3, a number of other unexpected mediators of neutrophil apoptosis have been identified that had not previously been characterised in other cell types. Myeloid cell nuclear differentiation antigen (MNDA) is a protein with roles in cell differentiation that has been discovered to influence neutrophil apoptosis [41]. Nuclear MNDA is cleaved by caspases early during apoptosis and translocates to the cytoplasm, where it promotes proteasomal degradation of Mcl-1, accelerating apoptosis. Knockdown of MNDA in HL-60 granulocytic cells decreased susceptibility to apoptosis.
Another protein better characterised as a mediator of cell proliferation, proliferating cell nuclear antigen (PCNA), has been identified as a novel mediator of neutrophil apoptosis [42]. Normally expressed primarily in the nucleus in the majority of cell types, PCNA is expressed in the cytoplasm of mature neutrophils, where it sequesters pro-caspases, limiting their activation and delaying apoptosis [43]. Peptides derived from the endogenously expressed cyclin-dependent kinase (CDK) inhibitor p21 displace the pro-caspases from PCNA and facilitate activation to trigger neutrophil apoptosis [44].
A related group of cell proliferation proteins, the CDKs (in particular CDK9 [45]), have been identified to modulate neutrophil apoptosis. The CDK inhibitor roscovitine induces neutrophil apoptosis and has been demonstrated to have an anti-inflammatory effect in vivo, harnessing the pro-resolving capabilities of apoptotic neutrophils [46, 47]. Finally, the long non-coding RNA Morrbid has been identified as a novel regulator of myeloid cell life span, including that of neutrophils [48]. The mechanism involves regulation of the transcription of Bim, a pro-apoptotic molecule.
Following apoptosis, neutrophils that are not phagocytosed in a timely manner may undergo secondary necrosis, spilling the neutrophil contents into the surrounding tissues and possibly contributing to exacerbated inflammation. One recent study found that during apoptosis, neutrophils processed the pro-form of the cytokine IL-16C through the action of caspase 3 but were only able to release this cytosolic protein once the membrane had been compromised [49]. Secondary necrosis also leads to release of other pre-formed molecules such as pleiotropic migration inhibitory factor [49]. This parallels work on macrophages describing the release of IL-1β, which is cytosolic and does not possess export sequences, necessitating cell death for release [50].
Immune complexes, implicated in the pathogenesis of a number of inflammatory diseases, have been found to induce neutrophil apoptosis through a non-canonical PI3K-Cdc42-Pak-Mek-Erk pathway, resulting in alterations in the proportions of pro- and anti-apoptotic molecules [51].
Non-Apoptotic Cell Death
The field of cell death has expanded greatly in the last decade to embrace newly described forms of non-apoptotic cell death including newly uncovered forms of “programmed” cell death. Whether or not neutrophils can undergo these forms of death, or indeed whether there are neutrophil-specific forms of cell death, is a field of on going study, with recent findings highlighted below.
NETosis - NET Release
One form of non-apoptotic neutrophil cell death has been termed NETosis or neutrophil extracellular trap release-associated cell death [52]. The central characteristics of this form of neutrophil demise are caspase-independent cell death and the release of DNA coated in neutrophil granule proteins. The exact mechanisms and clinical relevance of this form of cell death have been the focus of a large amount of research, with many questions remaining [53]. Key questions about NETosis and NET release remain, including whether DNA release can occur without triggering neutrophil death, as has been described in vitro for the release of mitochondrial DNA [54] and in vivo using two-photon microscopy in mice [55]. The physiologic and pathologic stimuli that induce NETosis need to be better defined, as a number of studies describing the mechanistic pathways of NETosis have been performed using the potent non-physiologic cell stimulant PMA [53, 56].
One scenario that appears to trigger this process is the attempted phagocytosis of large pathogens such as fungal hyphae [57]. As a consequence of the size of the hyphae, instead of forming a discrete pathogen-containing phagosome, the neutrophil granule enzymes are released into the cytoplasm in a ROS-dependent manner to enter the nucleus, degrade histones and allow the chromatin to decondense prior to cell membrane compromise. Intriguingly, neutrophils also respond to large particles by producing IL-1β [58]. In comparison to the phagocytosis of small particles where intracellularly generated ROS leads to oxidation of NF-κB and inhibition of IL-1β generation, ROS are instead directed extracellularly. These two neutrophil responses create a strategy of amplified neutrophil recruitment and local deposition of DNA and neutrophil granule proteins to ensnare the large hyphae and control growth.
As discussed above, one important consequence of apoptosis in neutrophils is that it triggers orderly dismantling of the cell and labelling of the cells for phagocytosis by macrophages, such that the potentially toxic neutrophil contents are sequestered during cell death. Furthermore, ingestion of apoptotic neutrophils triggers an anti-inflammatory response in the macrophages themselves [59]. Cell death with release of intracellular contents has the potential to circumvent this process. DNA release in the context of neutrophil cell death has been found to prime macrophages to release IL-1β in the context of atherosclerotic disease [60] both in vitro and in vivo.
The interaction of dead neutrophils with clearing phagocytes may be further perturbed by bacteria. Staphylococcus aureus was found to degrade the extracellular DNA structures released by neutrophils, not only dismantling their net-like properties, but converting the nucleic acids into deoxyadenosine, which resulted in caspase- mediated cell death of macrophages in proximity [61].
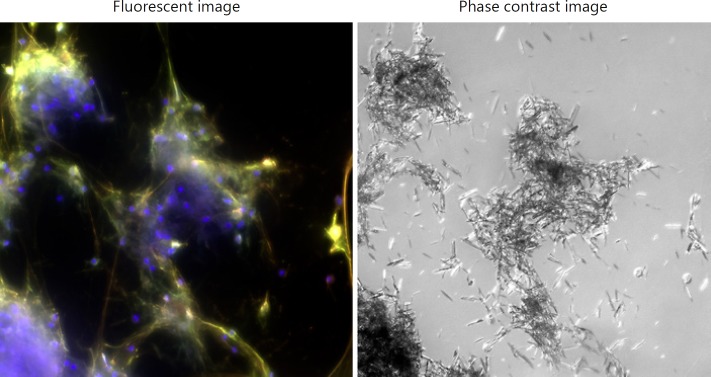
Another scenario where neutrophil cell death and DNA release may be of physiologic importance is in the human inflammatory joint disease gout. In vitro, monosodium urate (MSU) crystals are phagocytosed by neutrophils and, unlike hyphae, are encased in a maturing phagosome. Neutrophils subsequently undergo rapid cell death with post-mortem decondensation of the chromatin [62] (Fig. 3). This raises the question whether this form of cell death is programmed or a form of unregulated cell disruption occurring in the context of neutrophil granule release, resulting in dismantling of the chromatin. Extracellular DNA structures associated with neutrophil granule proteins are found to be associated with MSU crystals taken from the joints of gout patients, suggesting the process is occurring in this context. Using an in vivo model of MSU peritonitis, release of DNA leads to the formation of large aggregates of crystals that not only sequester the crystals but also actively degrade pro- inflammatory cytokines, leading to downregulation of inflammation [63]. This is in keeping with the clinical observations that gout attacks are self-limited and large aggregates of MSU crystals form around the joints of gout patients but remain largely uninflamed.
Fig. 3.
Neutrophil death with DNA release and decondensation triggered by monosodium urate crystals. Healthy control neutrophils incubated with monosodium urate crystals (0.2 mg/mL) for 4 h. Maximum-intensity projection of a z-stack. The fluorescent image is a merge of blue (DAPI), green (neutrophil elastase) and red (myeloperoxidase). DNA colocalised with neutrophil granule proteins aggregates the crystals.
Other Forms of Non-Apoptotic Cell Death
Other forms of programmed, non-apoptotic cell death have been characterised in the last decade, including necroptosis and pyroptosis. The majority of studies on these forms of death have been undertaken in cells other than neutrophils. In one study [64], Staphylococcus aureus triggered a non-apoptotic form of lytic cell death that involved RIPK3, a key component of the necroptotic death pathway, but did not involve RIPK1, the upstream component, and the death was not accompanied by MLKL membrane translocation, the critical downstream step leading to cell lysis in necroptosis. This study cautioned against relying on the results of experiments using chemical inhibitors of the necroptosis pathway, such as necrostatin-1, as evidence of necroptosis.
Neutrophil phagocytosis-induced cell death has been difficult to characterise and may depend on ROS generation and rapid caspase activation [65]. The phagocytosed pathogen plays an active role in the death pathway, exemplified by bacteria such as Francisella novicida that inhibit phagocytosis-induced cell death. This adaptation may serve as a survival advantage for this intracellular organism [66]. Another organism, Salmonella, induces macrophage pyroptosis, a form of programmed non-apoptotic cell death mediated by caspase 1 cleavage of gasdermin and accompanied by IL-1β release [67]. Neutrophils, on the other hand, despite containing the machinery to respond to Salmonella including the inflammasome NLRC4, resist pyroptosis whilst retaining the capacity to release active IL-1β. This heterogeneity in cell death and response to different pathogens reveals the complexity of neutrophil function [68].
Neutrophil-Derived Microvesicles - Novel Messengers That Modulate Inflammation
Microvesicles are tiny membrane-bound structures released by leukocytes or endothelial cells that can circulate throughout the body, carrying with them various immunomodulatory molecules that allow them to remotely modify inflammation [69]. Microvesicles are surrounded by a membrane containing high levels of phosphatidylserine, a lipid that is normally located inside the cell. Interestingly, using a unique hydrophobic patch, neutrophil-derived PR3 can bind to phosphatidylserine, a major component of microvesicles, thereby affecting both their production and their function to ultimately promote inflammation [70]. Conversely, microvesicles can have potent anti-inflammatory effects. As an example, a recent report has shown that neutrophil-derived microvesicles can enter cartilage and protect the joint in inflammatory arthritis [71]. In this setting, the anti-inflammatory protein annexin A1, which is also a phosphatidylserine-binding protein, bound to microvesicles. Annexin A1 could next interact with its receptor FPR2 (formyl peptide receptor 2)/ALX, increasing transforming growth factor-β production by chondrocytes, ultimately leading to cartilage protection. Microvesicles are emerging as a novel means for neutrophils to deliver proteins remotely to other cells with an impact on inflammation. Harnessing the pro-resolving effects of microvesicles may serve as a future therapeutic opportunity.
Conclusions
The last decade has uncovered some surprising aspects to neutrophil biology. Neutrophil heterogeneity at multiple levels, from neutrophil maturity, functionality and ultimately demise, has led to a reconsideration of the role of neutrophils in many diseases ranging from inflammatory disorders over cardiovascular and thrombotic diseases to cancer. The future of neutrophil research looks bright, but challenges remain. Translating discoveries into neutrophil-targeting therapeutics is the next critical step.
Disclosure Statement
The authors declare no financial or commercial conflict of interest.
Acknowledgements
The authors greatly acknowledge the Investissements d'Avenir programme ANR-11-IDEX-0005-02, Sorbonne Paris Cité, Labex INFLAMEX, the DHU AUTHORS (AP-HP and Paris Descartes University), the Chancellerie des Universités de Paris (Legs Poix) and charities including the Arthritis Foundation, Vaincre la Mucoviscidose (VLM) and ABCF Mucoviscidose.
References
- 1.Nauseef WM, Borregaard N. Neutrophils at work. Nat Immunol. 2014 Jul;15((7)):602–11. doi: 10.1038/ni.2921. [DOI] [PubMed] [Google Scholar]
- 2.Mantovani A, Cassatella MA, Costantini C, Jaillon S. Neutrophils in the activation and regulation of innate and adaptive immunity. Nat Rev Immunol. 2011 Jul;11((8)):519–31. doi: 10.1038/nri3024. [DOI] [PubMed] [Google Scholar]
- 3.Thieblemont N, Wright HL, Edwards SW, Witko-Sarsat V. Human neutrophils in auto-immunity. Semin Immunol. 2016 Apr;28((2)):159–73. doi: 10.1016/j.smim.2016.03.004. [DOI] [PubMed] [Google Scholar]
- 4.Soehnlein O, Steffens S, Hidalgo A, Weber C. Neutrophils as protagonists and targets in chronic inflammation. Nat Rev Immunol. 2017 Apr;17((4)):248–61. doi: 10.1038/nri.2017.10. [DOI] [PubMed] [Google Scholar]
- 5.Voisin MB, Nourshargh S. Neutrophil transmigration: emergence of an adhesive cascade within venular walls. J Innate Immun. 2013;5((4)):336–47. doi: 10.1159/000346659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robertson AL, Holmes GR, Bojarczuk AN, Burgon J, Loynes CA, Chimen M, et al. A zebrafish compound screen reveals modulation of neutrophil reverse migration as an anti-inflammatory mechanism. Sci Transl Med. 2014 Feb;6((225)):225ra29. doi: 10.1126/scitranslmed.3007672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nourshargh S, Renshaw SA, Imhof BA. Reverse Migration of Neutrophils: Where, When, How, and Why? Trends Immunol. 2016 May;37((5)):273–86. doi: 10.1016/j.it.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 8.Woodfin A, Voisin MB, Beyrau M, Colom B, Caille D, Diapouli FM, et al. The junctional adhesion molecule JAM-C regulates polarized transendothelial migration of neutrophils in vivo. Nat Immunol. 2011 Jun;12((8)):761–9. doi: 10.1038/ni.2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Colom B, Bodkin JV, Beyrau M, Woodfin A, Ody C, Rourke C, et al. Leukotriene B4-Neutrophil Elastase Axis Drives Neutrophil Reverse Transendothelial Cell Migration In Vivo. Immunity. 2015 Jun;42((6)):1075–86. doi: 10.1016/j.immuni.2015.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang J, Hossain M, Thanabalasuriar A, Gunzer M, Meininger C, Kubes P. Visualizing the function and fate of neutrophils in sterile injury and repair. Science. 2017 Oct;358((6359)):111–6. doi: 10.1126/science.aam9690. [DOI] [PubMed] [Google Scholar]
- 11.Auffray C, Sieweke MH, Geissmann F. Blood monocytes: development, heterogeneity, and relationship with dendritic cells. Annu Rev Immunol. 2009;27((1)):669–92. doi: 10.1146/annurev.immunol.021908.132557. [DOI] [PubMed] [Google Scholar]
- 12.Bronte V, Brandau S, Chen SH, Colombo MP, Frey AB, Greten TF, et al. Recommendations for myeloid-derived suppressor cell nomenclature and characterization standards. Nat Commun. 2016 Jul;7:12150. doi: 10.1038/ncomms12150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou J, Nefedova Y, Lei A, Gabrilovich D. Neutrophils and PMN-MDSC: their biological role and interaction with stromal cells. Semin Immunol. 2018 Feb;35:19–28. doi: 10.1016/j.smim.2017.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ocana A, Nieto-Jiménez C, Pandiella A, Templeton AJ. Neutrophils in cancer: prognostic role and therapeutic strategies. Mol Cancer. 2017 Aug;16((1)):137. doi: 10.1186/s12943-017-0707-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hacbarth E, Kajdacsy-Balla A. Low density neutrophils in patients with systemic lupus erythematosus, rheumatoid arthritis, and acute rheumatic fever. Arthritis Rheum. 1986 Nov;29((11)):1334–42. doi: 10.1002/art.1780291105. [DOI] [PubMed] [Google Scholar]
- 16.Marini O, Costa S, Bevilacqua D, Calzetti F, Tamassia N, Spina C, et al. Mature CD10+ and immature CD10- neutrophils present in G-CSF-treated donors display opposite effects on T cells. Blood. 2017 Mar;129((10)):1343–56. doi: 10.1182/blood-2016-04-713206. [DOI] [PubMed] [Google Scholar]
- 17.Coffelt SB, Kersten K, Doornebal CW, Weiden J, Vrijland K, Hau CS, et al. IL-17-producing γδ T cells and neutrophils conspire to promote breast cancer metastasis. Nature. 2015 Jun;522((7556)):345–8. doi: 10.1038/nature14282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uhel F, Azzaoui I, Grégoire M, Pangault C, Dulong J, Tadié JM, et al. Early Expansion of Circulating Granulocytic Myeloid-derived Suppressor Cells Predicts Development of Nosocomial Infections in Patients with Sepsis. Am J Respir Crit Care Med. 2017 Aug;196((3)):315–27. doi: 10.1164/rccm.201606-1143OC. [DOI] [PubMed] [Google Scholar]
- 19.Smith CK, Kaplan MJ. The role of neutrophils in the pathogenesis of systemic lupus erythematosus. Curr Opin Rheumatol. 2015 Sep;27((5)):448–53. doi: 10.1097/BOR.0000000000000197. [DOI] [PubMed] [Google Scholar]
- 20.Garcia-Romo GS, Caielli S, Vega B, Connolly J, Allantaz F, Xu Z, et al. Netting neutrophils are major inducers of type I IFN production in pediatric systemic lupus erythematosus. Sci Transl Med. 2011 Mar;3((73)):73ra20. doi: 10.1126/scitranslmed.3001201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Villanueva E, Yalavarthi S, Berthier CC, Hodgin JB, Khandpur R, Lin AM, et al. Netting neutrophils induce endothelial damage, infiltrate tissues, and expose immunostimulatory molecules in systemic lupus erythematosus. J Immunol. 2011 Jul;187((1)):538–52. doi: 10.4049/jimmunol.1100450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lood C, Blanco LP, Purmalek MM, Carmona-Rivera C, De Ravin SS, Smith CK, et al. Neutrophil extracellular traps enriched in oxidized mitochondrial DNA are interferogenic and contribute to lupus-like disease. Nat Med. 2016 Feb;22((2)):146–53. doi: 10.1038/nm.4027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grayson PC, Schauer C, Herrmann M, Kaplan MJ. Review: Neutrophils as Invigorated Targets in Rheumatic Diseases. Arthritis Rheumatol. 2016 Sep;68((9)):2071–82. doi: 10.1002/art.39745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cornish AL, Campbell IK, McKenzie BS, Chatfield S, Wicks IP. G-CSF and GM-CSF as therapeutic targets in rheumatoid arthritis. Nat Rev Rheumatol. 2009 Oct;5((10)):554–9. doi: 10.1038/nrrheum.2009.178. [DOI] [PubMed] [Google Scholar]
- 25.Henson GE. A Study of the Arneth Formula. J Am Med Assoc. 1914;LXIII((11)):922–5. [Google Scholar]
- 26.Evrard M, Kwok IW, Chong SZ, Teng KW, Becht E, Chen J, et al. Developmental Analysis of Bone Marrow Neutrophils Reveals Populations Specialized in Expansion, Trafficking, and Effector Functions. Immunity. 2018 Feb;48((2)):364–379. doi: 10.1016/j.immuni.2018.02.002. e8. [DOI] [PubMed] [Google Scholar]
- 27.Tak T, Wijten P, Heeres M, Pickkers P, Scholten A, Heck AJ, et al. Human CD62Ldim neutrophils identified as a separate subset by proteome profiling and in vivo pulse-chase labeling. Blood. 2017 Jun;129((26)):3476–85. doi: 10.1182/blood-2016-07-727669. [DOI] [PubMed] [Google Scholar]
- 28.Casanova-Acebes M, Pitaval C, Weiss LA, Nombela-Arrieta C, Chèvre R, A-González N, et al. Rhythmic modulation of the hematopoietic niche through neutrophil clearance. Cell. 2013 May;153((5)):1025–35. doi: 10.1016/j.cell.2013.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang D, Chen G, Manwani D, Mortha A, Xu C, Faith JJ, et al. Neutrophil ageing is regulated by the microbiome. Nature. 2015 Sep;525((7570)):528–32. doi: 10.1038/nature15367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Whyte MK, Meagher LC, MacDermot J, Haslett C. Impairment of function in aging neutrophils is associated with apoptosis. J Immunol. 1993 Jun;150((11)):5124–34. [PubMed] [Google Scholar]
- 31.Pillay J, den Braber I, Vrisekoop N, Kwast LM, de Boer RJ, Borghans JA, et al. In vivo labeling with 2H2O reveals a human neutrophil lifespan of 5.4 days. Blood. 2010 Jul;116((4)):625–7. doi: 10.1182/blood-2010-01-259028. [DOI] [PubMed] [Google Scholar]
- 32.Brinkmann V. Neutrophil Extracellular Traps in the Second Decade. J Innate Immun. 2018 Jun;•••:1–8. doi: 10.1159/000489829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Geering B, Simon HU. Peculiarities of cell death mechanisms in neutrophils. Cell Death Differ. 2011 Sep;18((9)):1457–69. doi: 10.1038/cdd.2011.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Murphy MP, Caraher E. Mcl-1 is vital for neutrophil survival. Immunol Res. 2015 Jun;62((2)):225–33. doi: 10.1007/s12026-015-8655-z. [DOI] [PubMed] [Google Scholar]
- 35.Iwai K, Miyawaki T, Takizawa T, Konno A, Ohta K, Yachie A, et al. Differential expression of bcl-2 and susceptibility to anti-Fas-mediated cell death in peripheral blood lymphocytes, monocytes, and neutrophils. Blood. 1994 Aug;84((4)):1201–8. [PubMed] [Google Scholar]
- 36.Loison F, Zhu H, Karatepe K, Kasorn A, Liu P, Ye K, et al. Proteinase 3-dependent caspase-3 cleavage modulates neutrophil death and inflammation. J Clin Invest. 2014 Oct;124((10)):4445–58. doi: 10.1172/JCI76246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Martin KR, Pederzoli-Ribeil M, Pacreau E, Burgener SS, Dahdah A, Candalh C, et al. Transgenic Mice Expressing Human Proteinase 3 Exhibit Sustained Neutrophil-Associated Peritonitis. J Immunol. 2017 Dec;199((11)):3914–24. doi: 10.4049/jimmunol.1601522. [DOI] [PubMed] [Google Scholar]
- 38.Thieblemont N, Witko-Sarsat V, Ariel A. Regulation of macrophage activation by proteins expressed on apoptotic neutrophils: subversion towards autoimmunity by proteinase 3. Eur J Clin Invest. 2018 Jul;•••:e12990. doi: 10.1111/eci.12990. [DOI] [PubMed] [Google Scholar]
- 39.Kantari C, Pederzoli-Ribeil M, Amir-Moazami O, Gausson-Dorey V, Moura IC, Lecomte MC, et al. Proteinase 3, the Wegener autoantigen, is externalized during neutrophil apoptosis: evidence for a functional association with phospholipid scramblase 1 and interference with macrophage phagocytosis. Blood. 2007 Dec;110((12)):4086–95. doi: 10.1182/blood-2007-03-080457. [DOI] [PubMed] [Google Scholar]
- 40.Millet A, Martin KR, Bonnefoy F, Saas P, Mocek J, Alkan M, et al. Proteinase 3 on apoptotic cells disrupts immune silencing in autoimmune vasculitis. J Clin Invest. 2015 Nov;125((11)):4107–21. doi: 10.1172/JCI78182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fotouhi-Ardakani N, Kebir DE, Pierre-Charles N, Wang L, Ahern SP, Filep JG, et al. Role for myeloid nuclear differentiation antigen in the regulation of neutrophil apoptosis during sepsis. Am J Respir Crit Care Med. 2010 Aug;182((3)):341–50. doi: 10.1164/rccm.201001-0075OC. [DOI] [PubMed] [Google Scholar]
- 42.Witko-Sarsat V, Mocek J, Bouayad D, Tamassia N, Ribeil JA, Candalh C, et al. Proliferating cell nuclear antigen acts as a cytoplasmic platform controlling human neutrophil survival. J Exp Med. 2010 Nov;207((12)):2631–45. doi: 10.1084/jem.20092241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Witko-Sarsat V, Ohayon D. Proliferating cell nuclear antigen in neutrophil fate. Immunol Rev. 2016 Sep;273((1)):344–56. doi: 10.1111/imr.12449. [DOI] [PubMed] [Google Scholar]
- 44.Martin C, Ohayon D, Alkan M, Mocek J, Pederzoli-Ribeil M, Candalh C, et al. Neutrophil-Expressed p21/waf1 Favors Inflammation Resolution in Pseudomonas aeruginosa Infection. Am J Respir Cell Mol Biol. 2016 May;54((5)):740–50. doi: 10.1165/rcmb.2015-0047OC. [DOI] [PubMed] [Google Scholar]
- 45.Hoodless LJ, Lucas CD, Duffin R, Denvir MA, Haslett C, Tucker CS, et al. Genetic and pharmacological inhibition of CDK9 drives neutrophil apoptosis to resolve inflammation in zebrafish in vivo. Sci Rep. 2016 Nov;5((1)):36980. doi: 10.1038/srep36980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rossi AG, Sawatzky DA, Walker A, Ward C, Sheldrake TA, Riley NA, et al. Cyclin-dependent kinase inhibitors enhance the resolution of inflammation by promoting inflammatory cell apoptosis. Nat Med. 2006 Sep;12((9)):1056–64. doi: 10.1038/nm1468. [DOI] [PubMed] [Google Scholar]
- 47.Meijer L, Nelson DJ, Riazanski V, Gabdoulkhakova AG, Hery-Arnaud G, Le Berre R, et al. Modulating Innate and Adaptive Immunity by (R)-Roscovitine: Potential Therapeutic Opportunity in Cystic Fibrosis. J Innate Immun. 2016;8((4)):330–49. doi: 10.1159/000444256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kotzin JJ, Spencer SP, McCright SJ, Kumar DB, Collet MA, Mowel WK, et al. The long non-coding RNA Morrbid regulates Bim and short-lived myeloid cell lifespan. Nature. 2016 Sep;537((7619)):239–43. doi: 10.1038/nature19346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Roth S, Solbach W, Laskay T. IL-16 and MIF: messengers beyond neutrophil cell death. Cell Death Dis. 2016 Jan;7((1)):e2049–2042. doi: 10.1038/cddis.2015.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Martín-Sánchez F, Diamond C, Zeitler M, Gomez AI, Baroja-Mazo A, Bagnall J, et al. Inflammasome-dependent IL-1β release depends upon membrane permeabilisation. Cell Death Differ. 2016 Jul;23((7)):1219–31. doi: 10.1038/cdd.2015.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chu JY, Dransfield I, Rossi AG, Vermeren S. Non-canonical PI3K-Cdc42-Pak-Mek-Erk Signaling Promotes Immune-Complex-Induced Apoptosis in Human Neutrophils. Cell Reports. 2016 Oct;17((2)):374–86. doi: 10.1016/j.celrep.2016.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Brinkmann V, Reichard U, Goosmann C, Fauler B, Uhlemann Y, Weiss DS, et al. Neutrophil extracellular traps kill bacteria. Science. 2004 Mar;303((5663)):1532–5. doi: 10.1126/science.1092385. [DOI] [PubMed] [Google Scholar]
- 53.Malachowa N, Kobayashi SD, Quinn MT, DeLeo FR. NET Confusion. Front Immunol. 2016 Jun;7:259. doi: 10.3389/fimmu.2016.00259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yousefi S, Mihalache C, Kozlowski E, Schmid I, Simon HU. Viable neutrophils release mitochondrial DNA to form neutrophil extracellular traps. Cell Death Differ. 2009 Nov;16((11)):1438–44. doi: 10.1038/cdd.2009.96. [DOI] [PubMed] [Google Scholar]
- 55.Yipp BG, Petri B, Salina D, Jenne CN, Scott BN, Zbytnuik LD, et al. Infection-induced NETosis is a dynamic process involving neutrophil multitasking in vivo. Nat Med. 2012 Sep;18((9)):1386–93. doi: 10.1038/nm.2847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nauseef WM, Kubes P. Pondering neutrophil extracellular traps with healthy skepticism. Cell Microbiol. 2016 Oct;18((10)):1349–57. doi: 10.1111/cmi.12652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Branzk N, Lubojemska A, Hardison SE, Wang Q, Gutierrez MG, Brown GD, et al. Neutrophils sense microbe size and selectively release neutrophil extracellular traps in response to large pathogens. Nat Immunol. 2014 Nov;15((11)):1017–25. doi: 10.1038/ni.2987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Warnatsch A, Tsourouktsoglou TD, Branzk N, Wang Q, Reincke S, Herbst S, et al. Reactive Oxygen Species Localization Programs Inflammation to Clear Microbes of Different Size. Immunity. 2017 Mar;46((3)):421–32. doi: 10.1016/j.immuni.2017.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Huynh ML, Fadok VA, Henson PM. Phosphatidylserine-dependent ingestion of apoptotic cells promotes TGF-beta1 secretion and the resolution of inflammation. J Clin Invest. 2002 Jan;109((1)):41–50. doi: 10.1172/JCI11638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Warnatsch A, Ioannou M, Wang Q, Papayannopoulos V. Inflammation. Neutrophil extracellular traps license macrophages for cytokine production in atherosclerosis. Science. 2015 Jul;349((6245)):316–20. doi: 10.1126/science.aaa8064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Thammavongsa V, Missiakas DM, Schneewind O. Staphylococcus aureus degrades neutrophil extracellular traps to promote immune cell death. Science. 2013 Nov;342((6160)):863–6. doi: 10.1126/science.1242255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chatfield SM, Grebe K, Whitehead LW, Rogers KL, Nebl T, Murphy JM, et al. Monosodium Urate Crystals Generate Nuclease-Resistant Neutrophil Extracellular Traps via a Distinct Molecular Pathway. J Immunol. 2018 Mar;200((5)):1802–16. doi: 10.4049/jimmunol.1701382. [DOI] [PubMed] [Google Scholar]
- 63.Schauer C, Janko C, Munoz LE, Zhao Y, Kienhöfer D, Frey B, et al. Aggregated neutrophil extracellular traps limit inflammation by degrading cytokines and chemokines. Nat Med. 2014 May;20((5)):511–7. doi: 10.1038/nm.3547. [DOI] [PubMed] [Google Scholar]
- 64.Greenlee-Wacker MC, Kremserová S, Nauseef WM. Lysis of human neutrophils by community-associated methicillin-resistant Staphylococcus aureus. Blood. 2017 Jun;129((24)):3237–44. doi: 10.1182/blood-2017-02-766253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhang B, Hirahashi J, Cullere X, Mayadas TN. Elucidation of molecular events leading to neutrophil apoptosis following phagocytosis: cross-talk between caspase 8, reactive oxygen species, and MAPK/ERK activation. J Biol Chem. 2003 Aug;278((31)):28443–54. doi: 10.1074/jbc.M210727200. [DOI] [PubMed] [Google Scholar]
- 66.Kinkead LC, Fayram DC, Allen LH. Francisella novicida inhibits spontaneous apoptosis and extends human neutrophil lifespan. J Leukoc Biol. 2017 Sep;102((3)):815–28. doi: 10.1189/jlb.4MA0117-014R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Man SM, Kanneganti TD. Gasdermin D: the long-awaited executioner of pyroptosis. Cell Res. 2015 Nov;25((11)):1183–4. doi: 10.1038/cr.2015.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kobayashi SD, Malachowa N, DeLeo FR. Neutrophils and Bacterial Immune Evasion. J Innate Immun. 2018 Apr;•••:1–10. doi: 10.1159/000487756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.van der Pol E, Böing AN, Harrison P, Sturk A, Nieuwland R. Classification, functions, and clinical relevance of extracellular vesicles. Pharmacol Rev. 2012 Jul;64((3)):676–705. doi: 10.1124/pr.112.005983. [DOI] [PubMed] [Google Scholar]
- 70.Martin KR, Kantari-Mimoun C, Yin M, Pederzoli-Ribeil M, Angelot-Delettre F, Ceroi A, et al. Proteinase 3 Is a Phosphatidylserine-binding Protein That Affects the Production and Function of Microvesicles. J Biol Chem. 2016 May;291((20)):10476–89. doi: 10.1074/jbc.M115.698639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Headland SE, Jones HR, Norling LV, Kim A, Souza PR, Corsiero E, Gil CD, Nerviani A, Dell'Accio F, Pitzalis C, Oliani SM, Jan LY, Perretti M. Neutrophil-derived microvesicles enter cartilage and protect the joint in inflammatory arthritis. Science Translational Medicine. 2015;7:315ra190–315ra190. doi: 10.1126/scitranslmed.aac5608. [DOI] [PMC free article] [PubMed] [Google Scholar]