Abstract
Background
People with HIV-1 (PWH) exhibit a high fall incidence and increased fracture risk. As little is known about fall frequency and associated factors in PWH residing in lower-middle-income countries (LMIC), we investigated fall frequency, bone quality, and factors associated with fall history in a South African cohort.
Methods
Fifty PWH without obvious predisposing factors for mobility impairments attending 2 public primary care clinics in the Western Cape region participated. Demographic, clinical, and physical performance data were collected. Falls were assessed retrospectively over 12 months. Mobility and balance were evaluated using a physical performance battery. Bone mineral density was screened using quantitative ultrasound (QUS). Associations between variables and falls grouping were analyzed using chi-square tests, t tests, and Mann-Whitney U tests, and effect sizes (ES) were calculated.
Results
Thirty-four percent of PWH (median age, 36.6 years) reported falling during the past year, and 41.2% of fallers reported multiple falls. Fallers had more mobility problems (P = .013), higher fear of falling (P = .007), higher fracture history (P = .003), worse balance performance (P < .001), higher proportions of detectable viral loads (P = .021), and poorer bone quality (P = .040). Differences were of medium to large ES.
Conclusions
This exploratory study is the first to show that relatively young South African PWH without obvious predisposing factors for gait and balance impairments experience falls. The observed fall-associated factors warrant further research using larger samples and longitudinal designs to ascertain fall predictors within this population.
Keywords: bone quality, falls, HIV infection, South Africa
Falls are common in people with HIV-1 (PWH) [1, 2]. Falls pose a particular concern in PWH because of reduced bone mineral density (BMD), owing to metabolic changes, bone cell infection, and highly active antiretroviral therapy (ART)–induced bone loss [3, 4]. Many factors associated with falls and BMD coexist (eg, sarcopenia, balance problems), translating to a compounded high fracture risk [5, 6]. The aggregate effect of such factors may partly explain the 4-fold increased hip fracture risk in PWH relative to seronegative individuals [7]. Findings from high-income countries (HICs) indicate that 18%–41% of middle-aged PWH have a history of at least 1 fall in the prior year [5, 8, 9]. Evidence from lower-middle-income countries (LMICs) is, however, lacking—despite the fact that most PWH reside in these regions.
Although HIV-related factors are associated with low BMD [3], published information suggests that HIV-specific variables may not be associated with fall risk [1, 5, 10]. Similarly, substance abuse–related factors (alcohol use, illegal drugs) have not shown an association with falls in PWH [2]. However, PWH have a high prevalence of various factors traditionally associated with falls. For example, the first study to report the rate and risk of falls among PWH [5] found multimorbidity, polypharmacy, and functional impairment (especially balance) to be significant fall predictors among PWH aged 45 to 65. Subsequent studies have also cited medication use [10–12], subjective imbalance symptoms [5, 10, 13], objective functional impairment (slowed walking, impaired balance, impaired sit-to-stand) [9, 10, 14], frailty [9, 15], obesity [8, 10], peripheral neuropathy [1, 9], depression [1, 8], smoking [5, 10] and increasing age [1, 8] as fall risk factors in PWH.
Some inconsistencies in fall-associated factors have, however, been noted between study populations from HICs and LMICs. For example, protease inhibitor (PI) use has demonstrated both a harmful (LMIC) [15] and protective (HIC) [10] association with falls, and polypharmacy was a fall risk factor in HIC studies [5, 10–12], whereas the only study from sub-Saharan Africa found no association [15]. These contrasting observations may be explained by factors unique to the study location. In South Africa, specifically, some individuals have limited access to ART or present late for treatment due to the stigma of the disease or cultural reasons. No or delayed treatment leads to faster disease progression and associated functional decline [16]. Furthermore, the selection of essential prescription medicine may differ in LMICs with limited medication access, resulting in a different risk–benefit ratio relative to HICs [15, 17]. There is a need to identify and understand fall-associated factors in PWH in the distinct local context of LMICs.
Understanding and addressing the profile of fall-associated factors in PWH, especially in LMICs, could reduce fall incidence, should these factors be modifiable. However, as existing data regarding associated factors are derived from HICs, these may not be applicable to LMICs, where socioeconomics, nutrition, and HIV-specific characteristics likely differ. The relatively younger, working-age profile of most PWH in sub-Saharan Africa (new infections being focused in young adults) [18] implies that falls (and related injuries) may occur at an earlier age and require long-term management. The majority of these young PWH are on new-generation highly active ART [19]. Although these drugs, if taken as prescribed, may reduce the risk of developing impairments such as peripheral neuropathy [20], a growing concern is the phenomenon of accelerated or accentuated aging. This may lead to the development of fall risk factors at younger-than-expected ages [2]. Early screening, before the onset of gross impairment, is thus important—1 example being the fact that early balance impairments have been noted in PWH even before the onset of neuropathic signs [21].
This study therefore aimed to assess a cohort of South African PWH by focusing on the frequency of any fall occurring during the prior 12 months and also fall-associated factors. It is envisaged that the results of this study will provide preliminary evidence to address the knowledge gap regarding falls among PWH in an LMIC setting. Considering the high burden of disease, long-term care, and consequent cost, our aim was to focus on an important segment of the relatively young population of PWH in South Africa, namely adults who may not necessarily be screened for falls, despite potentially already manifesting with fall frequencies of which health care practitioners should be aware of. We thus included a cohort without obvious predisposing factors to gait/balance impairments and related falls. For example, peripheral neuropathy [1, 5, 8, 9] and obesity [8, 10, 22] may cause functional gait and balance impairments and have been associated with falls in PWH. Increased awareness of fall frequency within a relatively young population of PWH without obvious risk factors could contribute to regular screening, which may be useful for reducing fall risk or injury severity.
METHODS
Participants
This was an exploratory analysis of cross-sectional data from a study of locomotor impairments in PWH. The locomotor study was part of a larger ongoing study (Cape Winelands HAART to HEART Study [CWH2H]). The study population primarily consisted of male and female adults (patients and family or friends) residing in and around the Cape Winelands District, Western Cape, South Africa, and visiting 2 public primary care Community Health Centers (CHCs). PWH were recruited between June 2016 and December 2017 by research nurses or HIV counselors who approached adults either already participating in the parent study or attending the CHC. Eligibility criteria included (1) age 18–65 years, (2) body mass index (BMI) <25 kg/m2, (3) independent ambulation, and (4) ability to consent and participate in study procedures. Exclusion criteria were (1) pregnancy or <3 months postpartum, (2) acute opportunistic infection/illness, (3) peripheral neuropathy, (4) major neurological conditions, (5) neuromusculoskeletal impairments/injury affecting normal gait, (6) visual impairment, or (7) alcohol intoxication. A confirmatory laboratory test result of HIV-1 infection was required for participation. The study conformed to the Helsinki Declaration and was approved by the Stellenbosch University Health Research Ethics Committee. Participants signed informed consent and received compensation for research activities. Specific consent was obtained for HIV testing, and pre- and post-test counseling was supplied where necessary.
Procedures
All procedures were performed at the local CHC or an adjacent venue. During a single study visit, participants completed questionnaires and underwent instrumented motion analysis (results reported elsewhere) [23] and clinical measurements including functional performance tests. The order of physical testing procedures was randomized. BMD screening was introduced later during the course of data collection, after amendments to the original study protocol.
Measures
A fall was defined as “an unexpected event in which the participant comes to rest on the ground, floor, or lower level” [24]. Fall history assessment over the prior 12 months (using retrospective recall at a single time point) was comprised of questions previously used in a South African Western Cape population [25]. Only falls not resulting from a major external (eg, pedestrian accident) or medical (eg, stroke) event were considered. Participants were asked whether they ever sustained a fracture. Fear of falling was assessed using a single question with a dichotomous response [26]. This approach is less sensitive than psychological indicators of fear or balance confidence but was a practical option during data collection and provides similar information [26].
BMD was screened via calcaneal quantitative ultrasound (QUS) using the SONOST 3000 ultrasound bone densitometer (OsteoSys, Korea). This device has proven useful for BMD screening in resource-limited settings, and the utility of QUS was demonstrated in PWH [27]. QUS estimates different parameters (bone quality, including density, structure, and elasticity) than dual energy x-ray absorptiometry (DEXA; BMD as bone quantity). Although QUS is not currently recommended for the diagnosis of osteoporosis, it can be used to screen and identify high-risk individuals, based on device-specific cutoffs previously validated in populations of intended use [28]. Bone quality was expressed using the Bone Quality Index (BQI), calculated by the device from the QUS parameters Speed of Sound (SOS; indicating bone density/elasticity) and Broadband Ultrasound Attenuation (BUA; indicating bone structure). BQI has a lower precision error and better predicts fractures than BUA or SOS and positively correlates with femoral/lumbar BMD values from DEXA in PWH [27]. The SONOST classifies results as normal (>–1), osteopenic (–1 to –2.5), or osteoporotic (≤–2.5) using T-scores, which represent BQI in standard deviation units from the mean in healthy young adults of the same sex. QUS T-scores correlate well with DEXA in PWH (rs = .43–.55; all P < .001) [29]. Three QUS measurements of the nondominant foot were performed to obtain an average.
Other potential fall-related variables included demographic and clinical characteristics, self-reported measures, and physical performance tests. Variables were selected from available participant data (from the parent study) based on fall-associated factors cited previously [5, 6, 8–11, 13, 30] or considered potentially important in the local context. Data extracted from the CWH2H study included age, sex, tobacco smoking, alcohol use, medication use, and comorbidities. Participants not enrolled in the CWH2H study were subjected to additional questions extracted from the CWH2H questionnaire. Polypharmacy was defined as chronic use of ≥2 non-ART medications, complementary medications, or supplements. Multimorbidity was defined as the presence of ≥2 chronic comorbidities over and above HIV infection. Extracted HIV-related data included HIV duration, most recent CD4+ cell count, viral load, and ART history. When these data were not available from the CWH2H database, results were obtained confidentially from medical records. ART nonadherence (defined as missing >2 prescribed ART dosages per week) was assessed using self-report.
Self-reported mobility function (walking problems) and anxio-depressive symptoms were assessed using relevant domains from the 5-level European Quality of Life Five-Dimensions questionnaire (EQ-5D-5L). The EQ-5D-5L is available in South African English, Afrikaans, and isiXhosa. It has been validated in PWH [31] and applied in South Africans [32]. Responses were captured on a 5-point Likert scale and subsequently dichotomized (“problems”/”no problems”).
Functional movement and balance were assessed using the Health ABC Physical Performance Battery (PPB) [33]. The battery is scored according to standing balance (30-second positions held in semitandem, tandem, and single-leg standing), time taken for 5 sit-to-stand repetitions without arm assistance, walking speed (time to ambulate 6 usual-paced meters), and a narrow-walk test of dynamic balance (time to ambulate a 6-meter-long, 20-cm wide walkway). Ratio scores from the 4 individual tests (each ranging from 0 to 1) were summed to generate a continuous score ranging from 0 to 4. This approach aims to minimize ceiling effects and maximize overall dispersion on each measure [33]. Total PPB score and component ratio scores were statistically analyzed for fall association.
Statistical Analysis
Analyses were performed using SPSS (version 25.0; IBM Corp.). Summary statistics included frequencies and percentages, medians and interquartile ranges (IQRs), or means and standard deviations. Associations between categorical variables and falls grouping (fallers vs nonfallers) were analyzed using chi-square tests. For continuous data, differences between fallers and nonfallers were evaluated using independent t tests (normal data) and Mann-Whitney U tests (skewed data). The significance level was set at P <.05. Effect sizes (ES) were expressed as Cramer's phi (φ), Pearson's r, or Cohen's d, as appropriate. ES interpretation was according to Cohen's guidelines for the d-family ES index (.2 = small; .5 = medium; .8 = large) or for the r-family measure of association (.1 = small; .3 = medium; .5 = large) [34].
RESULTS
Of 100 PWH screened, 21 refused or were unavailable after CWH2H participation, 13 had a BMI >25 kg/m2, 5 did not arrive for testing procedures, 3 had active pulmonary tuberculosis, 2 were feeling unwell, and 2 were aged >65. Four data sets were additionally excluded due to corrupted motion analysis data. Thus 50 data sets were analyzed.
Participants had a median age (IQR) of 36.6 (32.0–45.6) years. More than half were female (58.0%) and current tobacco smokers (52.0%). Most PWH (44.0%) had an HIV duration of 5 to 15 years. On average, the CD4+ count was <500 cells/μL, and 45.7% of PWH had undetectable viral loads (data missing for 4 PWH who were not enrolled in the CWH2H study and had no values recorded in medical records). Almost all PWH (90.0%) were using ART (median duration, ~2.3 years). Nonadherence was reported by 22.2% of ART users. Non-ART polypharmacy and multimorbidity were present in 32.0% and 8.0%, respectively.
Fear of falling was reported by 20.0% of PWH. Two PWH had missing data for anxio-depressive symptoms (1 omitted the question; another completed all domains incorrectly). Among 48 PWH with available data, 25.0% reported anxio-depressive symptoms. Among 49 PWH, 22.4% reported mobility problems. Fracture questioning was introduced, along with BMD screening, and thus data were available for 44 PWH, of whom 29.5% reported previous fractures.
The median total PPB score (IQR) was 2.4/4 (2.2–2.7). Best performance was evident for the balance domain (including achievement of maximum domain score), and worst performance for the chair stand domain.
Thirty-four percent of PWH reported falling in the past year. A single fall was reported by 20.0% of PWH (58.8% of fallers), whereas 14.0% (41.2% of fallers) reported multiple falls. The most common reasons reported for falling were tripping (n = 7; 41.2%), legs giving way/dizziness (n = 5; 29.4%), and slipping (n = 2; 11.8%). Fallers were more likely to have detectable viral loads, worse self-reported mobility function, higher fear of falling, fracture history, and worse PPB balance score (all P < .050). Age, gender, time since HIV diagnosis, current CD4+ count, ART use (including PI), ART duration, polypharmacy, multimorbidity, smoking, and depression were not associated with falls (all P > .050). Differences between fallers and nonfallers were moderate to large based on ES for detectable viral load (φ = .340), mobility problems (φ = .355), fear of falling (φ = .380), fracture history (φ = .454), and PPB balance score (r = .508) (Table 1).
Table 1.
Demographic, Clinical, and Physical Performance Characteristics in PWH and Association With Falls
| Characteristic | All PWH (n = 50) | Nonfallers (n = 33) | Fallers (n = 17) | P | Effect Size |
|---|---|---|---|---|---|
| Age, median (IQR), y | 36.6 (32.0–45.6) | 35.6 (31.8–43.1) | 44.0 (33.9–51.3) | .087 | r = .242 small |
| Women, No. (%) | 29 (58.0) | 19 (57.6) | 10 (58.8) | .933 | φ = .012 small |
| Time since HIV diagnosis, No. (%) | .873 | φ = 0.118 small | |||
| <2 y | 9 (18.0) | 7 (21.2) | 2 (11.8) | - | - |
| 2–5 y | 16 (32.0) | 10 (30.3) | 6 (35.3) | - | - |
| 5–15 y | 22 (44.0) | 14 (42.4) | 8 (47.1 ) | - | - |
| >15 y | 3 (6.0) | 2 (6.1) | 1 (5.9) | - | - |
| Current CD4+ T-cell count, median (IQR), cells/μL | 442.0 (245.0–675.5) | 465.0 (270.0–685.0) | 394.0 (242.0–558.0) | .582 | r = .078 |
| Detectable HIV-1 RNA (≥50 cp/mL; n = 46), No. (%) | 25 (54.3) | 12 (41.4) | 13 (76.5) | .021 | φ = .340 medium |
| On ART | 45 (90.0) | 29 (87.9) | 16 (94.1) | .486 | φ = .099 |
| ART duration (n = 44), median (IQR), wk | 119.0 (62.0–312.0) | 109.0 (62.0–312.0) | 134.5 (48.0–496.8) | .641 | r = .066 small |
| PI use (n = 45) | 9 (18.0) | 6 (18.2) | 3 (17.6) | .963 | φ = .007 small |
| Non-ART polypharmacy (≥2 non-ART medications), No. (%) | 16 (32.0) | 9 (27.3) | 7 (41.2) | .318 | φ = .141 small |
| Multimorbidity (≥2 comorbidities), No. (%) | 4 (8.0) | 2 (6.1) | 1 (5.9) | .980 | φ = .004 small |
| Current tobacco smoker, No. (%) | 26 (52.0) | 16 (48.5) | 10 (58.8) | .488 | φ = .098 small |
| Alcohol use ≥8 d/mo | 8 (16) | 4 (12.1) | 4 (23.5) | .297 | φ = .147 small |
| Depression/anxiety (n = 48), No. (%) | 12 (25.0) | 6 (18.8) | 6 (37.5) | .157 | φ = .204 small |
| Self-reported function: mobility problems (n = 49), No. (%) | 11 (22.4) | 4 (12.1) | 7 (43.8) | .013 | φ = .355 medium |
| Fear of falling, No. (%) | 10 (20.0) | 3 (9.1) | 7 (41.2) | .007 | φ = .380 medium |
| Previous fracture (n = 44), No. (%) | 13 (29.5) | 5 (16.1) (n = 31) | 8 (61.5) (n = 13) | .003 | φ = .454 medium |
| PPB total score, median (IQR) | 2.4 (2.2–2.7) | 2.4 (2.2–2.7) | 2.5 (1.9–2.8) | .927 | r = .013 small |
| PPB balance ratio score, median (IQR) | 1.0 (1.0–1.0) | 1.0 (1.0–1.0) | 0.9 (0.8–1.0) | <.001 | r = .508 large |
| PPB 6mW ratio score, mean ± SD | 0.5 ± 0.1 | 0.5 ± 0.1 | 0.5 ± 0.1 | .434 | d = .235 small |
| PPB narrow walk ratio score, mean ± SD | 0.5 ± 0.1 | 0.5 ± 0.1 | 0.5 ± 0.2 | .299 | d = .315 small |
| PPB chair stand ratio score, median (IQR) | 0.4 (0.4–0.5) | 0.4 (0.4–0.5) | 0.4 (0.3–0.5) | .260 | r = .159 small |
Bold formatting indicates statistical significance at 5%.
Abbreviations: ART, antiretroviral therapy; HIV-1 RNA, viral load; IQR, interquartile range; PPB, Health ABC Physical Performance Battery; PWH, people with HIV-1 infection.
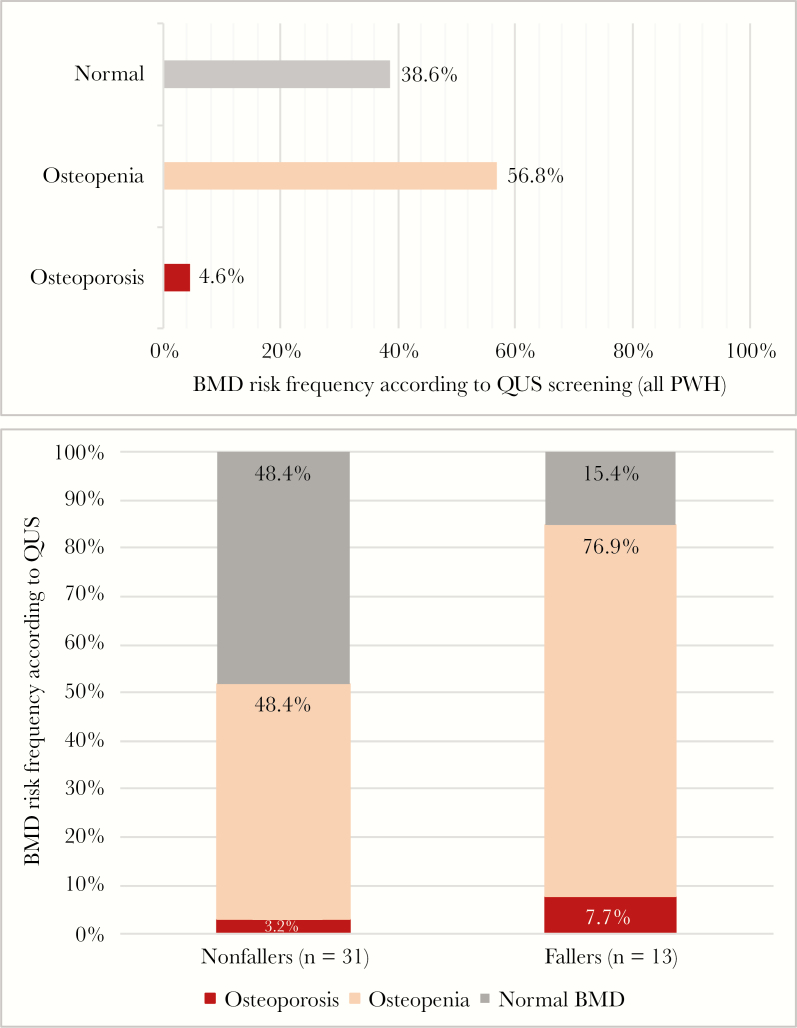
Forty-four PWH (88.0%) were screened for risk of reduced BMD. This subsample had similar demographics to the overall sample and comprised 31 nonfallers and 13 fallers. The median BQI (IQR) was significantly lower (medium ES; r = .310) in fallers than in nonfallers (77.8 [67.9–82.9] vs 84.1 [78.4–89.0]; P = .040). According to QUS screening, 27 (61.4%) PWH with available data were at risk of reduced BMD: 25 (56.8%; 92.6% of those with decreased BMD) were classified as potentially osteopenic, and 2 (4.5%; 7.4% of those with decreased BMD) as potentially osteoporotic. Relative to nonfallers, a significantly larger proportion of fallers were at risk of abnormal BMD, a difference with medium ES (P = .045; φ = .317). One faller (7.7%) and 1 nonfaller (3.2%) were classified as potentially osteoporotic (Figure 1).
Figure 1.
Bone mineral density (BMD) screening results in people with HIV (PWH) with available data (n = 44), classified according to quantitative ultrasound (QUS) T-score in all PWH (top chart) and stratified by fall status (bottom chart).
DISCUSSION
This is the first study to assess fall frequency and associated factors in a sample of South African PWH. Our findings, although preliminary, suggest that fall screening and prevention may be important in this population at relatively young ages, given that a large proportion of PWH (median age, <40 years) reported previous falls and demonstrated reduced bone quality. These observations were in a cohort without obvious predisposing factors for mobility or balance impairments.
The fall frequency in our study is higher than that observed in the general population of young to middle-aged (HIC) adults [35]. Data from this age bracket are lacking for LMICs, but our results resemble rates in a sample of 837 community-dwelling South African older adults [36], which (although not reported) may have included PWH, given South Africa's large prevalence. Statistics in PWH from HICs also resemble our results [5, 30], although these cohorts were ~20 years older than our sample. The high rate noted in our young cohort may be explained by a different HIV profile to that of PWH in HIC studies. Although most HIC studies found no association between falls and viral load, these studies included cohorts with mostly undetectable viral loads [1, 5, 8, 12, 30]. The discordance noted between ART use and virologic suppression in our sample may be reflective of South African PWH [37], where poor ART adherence or virological failure may be common [16]. Increased viral load may be associated with impaired neuromotor performance in PWH [38] or a frailty phenotype associated with falls [9], and even low levels of detectable virus have been associated with higher immune activation levels, virological failure, and poorer clinical outcomes [39]. It may be worth further investigating the association between viral load and falls, especially in LMICs.
Although the prevalence of reduced BMD in PWH seems generally higher in LMICs relative to HICs [4] and may be doubled in PWH relative to HIV-seronegative controls (at least in HICs) [3], no studies have investigated associations between BMD and falls in PWH. We found that a large proportion of PWH, especially fallers, may be eligible for DEXA to confirm/exclude osteopenia/osteoporosis. Our results emphasize the importance of screening and modifying risks for both falls and fractures in younger-than-expected PWH [3]. Given that the relationships between BMD, functional impairment, and falls may be multidirectional [2], interventions that simultaneously reduce fall risk, improve function, and increase BMD may hold the most benefit.
In accordance with published reports, we found that objective balance impairments are associated with fall frequency. Objective and self-reported balance impairments are well-established and consistent fall predictors in community-dwelling adults of all ages, including PWH [5, 10, 35]. Quantitative balance measures have demonstrated increased center-of-pressure (COP) excursion in PWH under challenging conditions [23, 38], potentially indicating a reduced ability to adapt and shift the body's COP to prevent falling. Our findings indicate that in a South African context, increased awareness of balance problems is important and that screening should be considered in a young population without obvious risk factors. Importantly, balance assessment in a high-functioning population with HIV should be revisited, as we have found high ceiling effects in our sample using a combination of tandem- and single-leg standing tests. Further research to ascertain the most sensitive balance test in a high-functioning group is warranted.
Fear of falling models suggest that such fear directly and negatively affects balance function [40]. It is also suggested that fear of falling stems from judging one's own balance ability, along with contributing factors (eg, fall history) [40]. Falls associated with balance problems may cause further fear of falling, ultimately reducing quality of life [41]. Relationships between fear of falling, balance, and falls are thus likely multidirectional, and risk factors may be shared. Unfortunately, our analysis cannot shed light on whether fear of falling precedes balance impairments or falls; this should be addressed in larger longitudinal studies.
This is the first study to report on an association between self-reported walking function and falls. A significant association existed between walking problems and falls, highlighting the potential clinical utility of using self-report as a simple, no-cost screening tool in an LMIC context. Using a person-centered tool to identify adverse outcomes related to mobility function in PWH is further supported by the fact that self-reported mobility problems have been associated with reduced quality of life, poor ART adherence, and barriers to health care access in PWH [42]. Regarding objectively measured gait, we found that fallers tended to walk faster than nonfallers, although not significantly so. Other fall studies have reported similar nonsignificant trends in PWH [5, 9]. This could suggest a nonlinear relationship between falls and walking speed in PWH, where a greater risk of falls may exist in fast walkers [43].
Many of the previously cited fall risk factors in PWH were not associated with falls in this cohort. This may be explained by the relatively young age and a profile generally free of multimorbidity (including peripheral neuropathy and obesity), along with the study setting. For example, we found no association between polypharmacy (a commonly cited fall risk factor among PWH in HICs [5, 10–12]) and falls. Recently, Ssonko et al. [15] found no association between polypharmacy and falls in an sub-Saharan African cohort of PWH. These authors suggested that persons residing in HICs may be more prone to taking multiple medications, resulting in a higher potential of harm, compared with those from LMICs [15].
Fall prevention is a critical health and prevention issue regarding elderly care in the general population. Although fall risk is usually not a concern in younger persons, fall prevention may be of importance for young to middle-aged South African PWH without obvious predisposing factors for gait or balance impairments. HIV-1 and modern ART have been associated with accelerated or accentuated aging, which may compound fall risks in PWH as they age. It may be worth extrapolating from the high-quality evidence existing for older adults, which has recommended multifactorial risk assessments and screening to identify fall risk. A holistic management model that simultaneously focuses on local contexts and modifiable factors, including balance impairment, along with factors that may impact viral load and overall wellness of PWH, may be valuable in the unique context of LMICs.
This study is limited by a relatively small sample, and the cross-sectional design prohibits causal inferences. The small number of event observations prohibited multivariate analyses; thus we could not assess confounding or independence of association. Although the study sample provides unique insights into relatively young nonobese South African PWH without peripheral neuropathy, the results may not be generalizable to other clinical settings. Finally, fall history was based on a reliance on retrospective self-reporting that may have resulted in inaccurate reporting.
CONCLUSIONS
This is the first study to show that one-third of young to middle-aged South African adults with HIV (<40 years) without known predisposing factors for gait and balance impairments experience falls. Self-reported mobility problems, fear of falling, previous fractures, balance impairments, detectable viral load, and reduced bone quality were associated with falls in univariate analyses. This exploratory study warrants further research with defensible sample sizes and longitudinal designs to ascertain predictors of falls within this population.
Acknowledgments
The authors thank the study participants for their effort and patience, Worcester and Paarl Community Health Clinics and Stellenbosch University Ukwanda Centre for Rural Health for hosting data collection, and the Cape Winelands HAART to HEART team, research nurses, and HIV counselors for assisting with data collection and study logistics throughout.
Financial support. This work was supported by the South African Medical Research Council under a Self-Initiated Research Grant (Q.L.) and the Harry Crossley Foundation (SU-PT-15/10-000005 and SU-PT-16/10-000057 to K.B.). The PhD from which this study emanated was funded by the South African Medical Research Council in terms of the National Health Scholars Programme (K.B.) from funds provided for this purpose by the National Department of Health. Publication of this article was partly funded by the Stellenbosch University Open Access Fund (K.B). The views and opinions expressed are not those of the funders, but of the authors of the material publicized.
Potential conflicts of interest. All authors declare that they have no potential conflicts of interest. The authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Author contributions. K.B., Q.L., and L.M. were involved in the conception and initial design of the study. K.B., Q.L., H.S., M.F.E., and I.W. were involved in study coordination and implementation. I.W. extracted relevant data from the CWH2H database. K.B. conducted data collection and analysis. K.B., Q.L., H.S., M.F.E., I.W., and L.M. were all involved in data interpretation, manuscript writing, revision, and critical comment; all approved the final version for publication.
Ethical approval. Study approval was granted by the Stellenbosch University (SU) Human Research Ethics Committee (HREC) and the Western Cape Department of Health.
References
- 1. Sharma A, Hoover DR, Shi Q, et al. . Longitudinal study of falls among HIV-infected and uninfected women: the role of cognition. Antivir Ther 2018; 23:179–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Erlandson KM, Guaraldi G, Falutz J. More than osteoporosis: age-specific issues in bone health. Curr Opin HIV AIDS 2016; 11:343–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Goh SSL, Lai PSM, Tan ATB, Ponnampalavanar S. Reduced bone mineral density in human immunodeficiency virus-infected individuals: a meta-analysis of its prevalence and risk factors: supplementary presentation. Osteoporos Int 2018; 29:595–613. [DOI] [PubMed] [Google Scholar]
- 4. Matovu FK, Wattanachanya L, Beksinska M, et al. . Bone health and HIV in resource-limited settings: a scoping review. Curr Opin HIV AIDS 2016; 11:306–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Erlandson KM, Allshouse AA, Jankowski CM, et al. . Risk factors for falls in HIV-infected persons. J Acquir Immune Defic Syndr 2012; 61:484–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Richert L, Dehail P, Mercié P, et al. ; Groupe d'Epidémiologie Clinique du SIDA en Aquitaine (GECSA) High frequency of poor locomotor performance in HIV-infected patients. AIDS 2011; 25:797–805. [DOI] [PubMed] [Google Scholar]
- 7. Arnsten JH, Freeman R, Howard AA, et al. . Decreased bone mineral density and increased fracture risk in aging men with or at risk for HIV infection. AIDS 2007; 21:617–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sharma A, Hoover DR, Shi Q, et al. . Falls among middle-aged women in the Women's Interagency HIV Study. Antivir Ther 2016; 21:697–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tassiopoulos K, Abdo M, Wu K, et al. . Frailty is strongly associated with increased risk of recurrent falls among older HIV-infected adults. AIDS 2017; 31:2287–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Erlandson KM, Plankey MW, Springer G, et al. . Fall frequency and associated factors among men and women with or at risk for HIV infection. HIV Med 2016; 17:740–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ruiz MA, Reske T, Cefalu C, Estrada J. Falls in HIV-infected patients: a geriatric syndrome in a susceptible population. J Int Assoc Provid AIDS Care 2013; 12:266–9. [DOI] [PubMed] [Google Scholar]
- 12. Kim TW, Walley AY, Ventura AS, et al. . Polypharmacy and risk of falls and fractures for patients with HIV infection and substance dependence. AIDS Care 2018; 30:150–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brown T, Li X, Jacobson L, et al. . Balance confidence predicts falls better than physical function testing in HIV+ men. Paper presented at: Conference on Retroviruses and Opportunistic Infections; February 23–26, 2015; WA: Seattle. Abstract #786. [Google Scholar]
- 14. Richert L, Brault M, Mercié P, et al. ; Groupe d'Epidémiologie Clinique du SIDA en Aquitaine (GECSA) Decline in locomotor functions over time in HIV-infected patients. AIDS 2014; 28:1441–9. [DOI] [PubMed] [Google Scholar]
- 15. Ssonko M, Stanaway F, Mayanja HK, et al. . Polypharmacy among HIV positive older adults on anti-retroviral therapy attending an urban clinic in Uganda. BMC Geriatr 2018; 18:125–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Osler M, Hilderbrand K, Goemaere E, et al. . The continuing burden of advanced HIV disease over 10 years of increasing antiretroviral therapy coverage in South Africa. Clin Infect Dis 2018; 66:118–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mori AT, Kaale EA, Ngalesoni F, et al. . The role of evidence in the decision-making process of selecting essential medicines in developing countries: the case of Tanzania. PLoS One 2014; 9:e84824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Statistics South Africa. Mid-year Population Estimates - P0302. Pretoria, South Africa:Statistics South Africa; 2019. [Google Scholar]
- 19. UNAIDS. Prevention Gap Report: UNAIDS 2016. Geneva, Switzerland: UNAIDS, Joint United Nations Programme on HIV/AIDS; 2016. [Google Scholar]
- 20. Spudich S, Ances B. Neurologic complications of HIV infection: highlights from the 2013 Conference on Retroviruses and Opportunistic Infections. Top Antivir Med 2013; 21:100–8. [PMC free article] [PubMed] [Google Scholar]
- 21. Trenkwalder C, Straube A, Paulus W, et al. . Postural imbalance: an early sign in HIV-1 infected patients. Eur Arch Psychiatry Clin Neurosci 1992; 241:267–72. [DOI] [PubMed] [Google Scholar]
- 22. Bauer LO, Wu Z, Wolfson LI. An obese body mass increases the adverse effects of HIV/AIDS on balance and gait. Phys Ther 2011; 91:1063–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Berner K. Biomechanical Analysis of Specific Motor Impairments Contributing to Early Functional Decline in Adults Living With HIV-1 Infection: A Sub-study to the Cape Winelands HAART to HEART (Prevalence)/EndoAfrica Study [dissertation]. Stellenbosch: Stellenbosch University; 2019. [Google Scholar]
- 24. Lamb SE, Jørstad-Stein EC, Hauer K, Becker C; Prevention of Falls Network Europe and Outcomes Consensus Group Development of a common outcome data set for fall injury prevention trials: the prevention of falls network Europe consensus. J Am Geriatr Soc 2005; 53:1618–22. [DOI] [PubMed] [Google Scholar]
- 25. Kalula SZ, Ferreira M, Swingler GH, Badri M. Ethnic differences in rates and causes of falls in an urban community-dwelling older population in South Africa. J Am Geriatr Soc 2015; 63:403–4. [DOI] [PubMed] [Google Scholar]
- 26. Maki BE. Gait changes in older adults: predictors of falls or indicators of fear. J Am Geriatr Soc 1997; 45:313–20. [DOI] [PubMed] [Google Scholar]
- 27. Fantauzzi A, Floridia M, Ceci F, et al. . Usefulness of calcaneal quantitative ultrasound stiffness for the evaluation of bone health in HIV-1-infected subjects: comparison with dual x-ray absorptiometry. HIV AIDS (Auckl) 2016; 8:109–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Thomsen K, Jepsen DB, Matzen L, et al. . Is calcaneal quantitative ultrasound useful as a prescreen stratification tool for osteoporosis? Osteoporos Int 2015; 26:1459–75. [DOI] [PubMed] [Google Scholar]
- 29. Quiros Roldan E, Brianese N, Raffetti E, et al. . Comparison between the gold standard DXA with calcaneal quantitative ultrasound based-strategy (QUS) to detect osteoporosis in an HIV infected cohort. Braz J Infect Dis 2017; 21:581–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Greene M, Covinsky KE, Valcour V, et al. . Geriatric syndromes in older HIV-infected adults. J Acquir Immune Defic Syndr 2015; 69:161–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Tran BX, Ohinmaa A, Nguyen LT. Quality of life profile and psychometric properties of the EQ-5D-5L in HIV/AIDS patients. Health Qual Life Outcomes 2012; 10:132–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kastien-Hilka T, Rosenkranz B, Sinanovic E, et al. . Health-related quality of life in South African patients with pulmonary tuberculosis. PLoS One 2017; 12:e0174605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Simonsick EM, Newman AB, Nevitt MC, et al. ; Health ABC Study Group Measuring higher level physical function in well-functioning older adults: expanding familiar approaches in the Health ABC study. J Gerontol A Biol Sci Med Sci 2001; 56:M644–9. [DOI] [PubMed] [Google Scholar]
- 34. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- 35. Talbot LA, Musiol RJ, Witham EK, Metter EJ. Falls in young, middle-aged and older community dwelling adults: perceived cause, environmental factors and injury. BMC Public Health 2005; 5:86–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kalula SZ, Ferreira M, Swingler GH, Badri M. Risk factors for falls in older adults in a South African urban community. BMC Geriatr 2016; 16:51–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. George S, McGrath N, Oni T. The association between a detectable HIV viral load and non-communicable diseases comorbidity in HIV positive adults on antiretroviral therapy in Western Cape, South Africa. BMC Infect Dis 2019; 19:348–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Berner K, Morris L, Baumeister J, Louw Q. Objective impairments of gait and balance in adults living with HIV-1 infection: a systematic review and meta-analysis of observational studies. BMC Musculoskelet Disord 2017; 18:325–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Antinori A, Cozzi Lepri A, Ammassari A, et al. . Low-level viremia (LLV) ranging from 50 to 500 copies/mL is associated to an increased risk of AIDS events in the Icona Foundation Cohort. Paper presented at: 15th European AIDS Conference (EACS); October 21–24, 2015; Barcelona, Spain. [Google Scholar]
- 40. Hadjistavropoulos T, Delbaere K, Fitzgerald TD. Reconceptualizing the role of fear of falling and balance confidence in fall risk. J Aging Health 2011; 23:3–23. [DOI] [PubMed] [Google Scholar]
- 41. Schoene D, Heller C, Aung YN, et al. . A systematic review on the influence of fear of falling on quality of life in older people: is there a role for falls? Clin Interv Aging 2019; 14:701–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hanass-Hancock J, Myezwa H, Carpenter B. Disability and living with HIV: baseline from a cohort of people on long term ART in South Africa. PLoS One 2015; 10:e0143936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Quach L, Galica AM, Jones RN, et al. . The nonlinear relationship between gait speed and falls: the maintenance of balance, independent living, intellect, and zest in the elderly of Boston study. J Am Geriatr Soc 2011; 59:1069–73. [DOI] [PMC free article] [PubMed] [Google Scholar]