ABSTRACT
Background
Studies on the impact of counterfactual scenarios of physical activity on premature deaths from non-communicable diseases (NCDs) are sparse in the literature. We estimated preventable premature deaths from NCDs (diabetes, ischemic heart disease, stroke, and breast and colon cancers) in Brazil by increasing population-wide physical activity (i) to theoretical minimum risk exposure levels; (ii) reaching the physical activity recommendation; (iii) reducing insufficient physical activity by 10%; and (iv) eliminating the gender differences in physical activity.
Methods
Preventable fractions were estimated using data from a nationally representative survey, relative risks from a meta-analysis and number of premature deaths (30–69 years) from the Brazilian Mortality Information System.
Results
Physical activity could potentially avoid up to 16 700 premature deaths from NCDs in Brazil, corresponding to 5.75 and 3.23% of premature deaths from major NCDs and of all-causes, respectively. Other scenarios suggested the following impact on premature deaths: reaching physical activity recommendation (5000 or 1.74% of major NCDs); 10% reduction in insufficient physical activity (500 or 0.17% of major NCDs); eliminating gender differences in physical activity (1000 or 0.33% of major NCDs).
Conclusions
Physical activity may play an important role to reduce premature deaths from NCD in Brazil.
Keywords: epidemiology, non-communicable diseases, physical activity, population attributable fraction, premature mortality
Introduction
‘Death in old age is inevitable, but death before old age is not’.1 Under-70 age-standardized mortality rates decreased by 20% in the last decade, but it is still a major concern.2 Currently, more than half of global deaths under the age 70 years were from non-communicable diseases (NCDs).3 Individuals in low- to middle-income countries face a 1.5 time higher risk of premature mortality from NCD than individuals in high-income countries.4 In Brazil, for instance, 40% of all deaths in 2015 occurred between the ages of 30 and 69 years, of which 56% were from major NCDs, namely cardiovascular diseases (CVD), diabetes, cancer and chronic respiratory diseases.5
Most of these premature deaths from NCD could be avoided by tackling their major causes.6 In 2012, the World Health Organization (WHO) launched the Global Plan for 2025 (hereafter referred to as ‘WHO 25 × 25’) aimed to reduce by 25% premature deaths from NCDs.3 To achieve this goal, nine voluntary global targets focusing on some determinants of NCDs (tobacco, alcohol, obesity, physical activity, salt/sodium, hypertension, access to CVD prevention programs and NCD treatments)3 were agreed upon.
Physical activity may have an important role for reducing premature deaths from NCDs as it is consistently associated with type 2 diabetes mellitus, ischemic heart disease, stroke, breast cancer and colon cancer.7–9 The WHO 25 × 25 target aims a 10% relative reduction in the prevalence of insufficient physical activity (i.e. <600 metabolic equivalent task-minute per week (MET-min/week), usually translated as <150 min per week of moderate to vigorous intensity physical activity).3 Reducing the gender differences in the prevalence of insufficient physical activity by increasing physical activity in women has been argued to be an important means toward this WHO target.10–12 However, the impact of reaching these physical activity goals on premature deaths from NCDs is unclear.
Herein, we estimated the proportion and number of premature deaths from NCDs that could be avoided in Brazil by increasing physical activity (i) to theoretical minimum risk exposure levels; (ii) to at least 600 MET-min/week; (iii) reducing insufficient physical activity by 10%; and (iv) eliminating the gender differences in physical activity by increasing total physical activity in women to levels observed in men.
Methods
Data input
Assessment of physical activity
We obtained data on the distribution of physical activity from the National Health Survey (Pesquisa Nacional de Saúde—PNS), 2013.13,14 PNS included a nationally representative sample of adult population aged 18 years and over. The PNS sample was randomly selected in three stages: census tracts (primary sampling units), households (second units) and household members 18 years or older (tertiary units). In the final sample, 62 202 adults aged 18 years or over were interviewed (response rate: 86%). In this study, we used information from 55 263 adults aged 18–69 years that responded the physical activity questionnaire. Further information about PNS has been described elsewhere.13,14
Physical activity level was assessed using self-reported data of weekly frequency (0–7 days) and duration (hours and minutes) of recreational, occupational, household and commuting activities (walking or cycling to and/or from work; walking or cycling to and/or from other daily activities) in a typical week. Additionally, for individuals engaged in recreational physical activity at least once a week, the most frequent type of recreational activity (e.g. walking, cycling, running, soccer) was asked. The PNS physical activity questionnaire is available in the Supplementary material. We used the compendium of physical activities to assign metabolic equivalent of task (MET) considering the most frequent type of recreational physical activity as well as the average MET for each of the other domains of physical activity (Table S1).15 Finally, we estimated total physical activity level by summing up MET-minutes per week (MET-min/week) across domain of physical activity.
Relative risk estimates
We retrieved relative risks (RRs) and 95% confidence intervals (95% CI) from a recent dose–response meta-analysis of prospective cohort studies7,16 for the association between total physical activity (MET-min/week) and risk of diabetes, ischemic heart disease, stroke, breast cancer and colon cancer. The RRs and 95% CI estimates were related to both sexes (except for breast cancer, women only) and all ages combined for the following categories of total physical activity: <600, 600–3999, 4000–7999 and ≥8000 MET-min/week. The reference group (≥8000 MET-min/week) was intended to represent the theoretical minimum risk exposure level, over which there is no additional benefit of physical activity associated with decreased risk of NCDs.7 The MET-min/week is equivalent to 5 h/day of moderate intensity physical activities (e.g. brisk walking, walking for transportation).
Number of NCD premature deaths
We collected the number of premature deaths (age 30–69 years) from diabetes mellitus (ICD E11, E14), ischemic heart disease (ICD I20-I25), stroke (ICD G45 and I64), breast cancer (ICD C50) for women and colon cancer (ICD C18) in 2015 from the Brazilian Mortality Information System.5 We additionally obtained number of deaths from all-causes (ICD A00-U99) and major NCDs (diabetes (ICD E10-E14), cardiovascular diseases (ICD I00-I99), cancers (ICD C00-C97) and chronic respiratory diseases (ICD J30-J98)). Major NCDs were selected based on the WHO 25 × 25.3
Data management and analysis
We estimated potential impact fractions (PIF), defined as the expected proportional reduction in deaths that would occur by reducing the exposure in the population, with other conditions remaining the same.17 PIF was calculated using the following equation:
where, Pi is the proportion of the population at the level i of total physical activity, P′i is the proportion of the population at the level i of total physical activity in the counterfactual (alternatively proposed) scenarios, and RRi is the relative risk of each outcome (diabetes, ischemic heart disease, stroke, breast cancer and colon cancer) at the level i of total physical activity. Levels i of total physical activity were <600, 600–3999, 4000–7999 and ≥8000 MET-min/week.
In this study, we used the following counterfactual scenarios of total physical activity:
Theoretical minimum risk exposure levels, where everyone reaches at least 8000 MET-min/week. PIF estimates related to this scenario will be hereafter referred as population attributable fraction (PAF), a special case of PIF where the exposure is eliminated.17,18
Physical activity recommendation, where everyone reaches at least 600 MET-min/week.8
10% relative reduction in the prevalence of insufficient physical activity (<600 MET-min/week).6
Gender equality, where total physical activity level is equal between men and women. In this scenario, we increased physical activity in women to levels observed in men (reference group). Men remained with currently observed physical activity level.
To obtain the number of preventable premature deaths from NCDs, we applied PIF estimates to the number of premature deaths from diabetes, ischemic heart disease, stroke, and breast and colon cancers in 2015.5 In addition, we summed up the number of preventable premature deaths from NCDs and divided by total number of premature deaths from major NCD and all-causes.
Finally, we ran a sensitivity analysis considering the current distribution and counterfactual scenarios of recreational and commuting physical activity only. These domains of physical activity have shown the most consistent evidence of preventive effect on NCDs.9,19,20 Indeed, interventions and policies aimed to increase population-wide physical activity have focused on recreational and commuting physical activity.3
Data analysis was performed in Stata version 15.0. Data input and scripts used in our study are available at https://osf.io/5ut4z/.
Results
The sample included mostly middle-age adults (mean age 42 years), women (53%), who completed secondary education (41%), white (47%), and were married (44%). Participant characteristics by time spent in total physical activity are shown in Table 1.
Table 1.
Characteristics of participants by time spent in total physical activity: National Health Survey, 2013, Brazil
| Characteristics | Total physical activity (MET-min/week) | |||
|---|---|---|---|---|
| <600 | 600–3999 | 4000–7999 | ≥8000 | |
| (n = 29 482) | (n = 22 408) | (n = 4051) | (n = 3169) | |
| Mean age (years) | 41.8 | 38.7 | 38.7 | 36.9 |
| Sex/Gender (%) | ||||
| Men | 43.5 | 44.5 | 60.5 | 77.8 |
| Women | 56.5 | 55.5 | 39.5 | 22.2 |
| Education (%) | ||||
| None or incomplete primary | 21.0 | 13.9 | 17.5 | 16.8 |
| Complete primary or incomplete secondary | 27.7 | 25.9 | 33.1 | 45.6 |
| Complete secondary or incomplete university | 38.6 | 44.2 | 39.7 | 33.3 |
| University graduate | 12.6 | 15.9 | 9.6 | 4.4 |
| Race/Ethnicity (%) | ||||
| White | 48.4 | 47.4 | 42.2 | 37.0 |
| Black | 8.8 | 8.9 | 9.7 | 14.5 |
| Asian | 0.9 | 0.9 | 0.9 | 0.9 |
| Brown | 41.7 | 42.2 | 46.9 | 46.9 |
| Native Indian | 0.3 | 0.6 | 0.3 | 0.7 |
| Marital status | ||||
| Married | 46.8 | 43.1 | 41.6 | 35.8 |
| Separated/Divorced | 7.2 | 6.4 | 6.4 | 4.9 |
| Widow/widower | 5.0 | 3.3 | 2.5 | 3.0 |
| Single | 41.1 | 47.2 | 49.5 | 56.4 |
| Domain-specific physical activity (mean MET-min/week) | ||||
| Leisure | 30 | 612 | 1131 | 937 |
| Occupational | 4 | 224 | 2667 | 9182 |
| Commuting | 88 | 536 | 1059 | 1049 |
| Household | 10 | 295 | 747 | 837 |
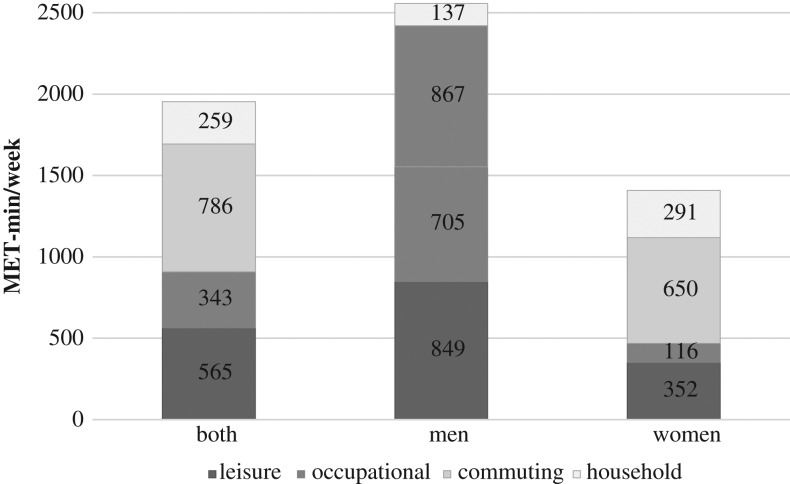
Only 6.5% of participants reported at least 8000 MET-min/week in total physical activity. This proportion was around 4-fold higher in men (10.6%) than in women (2.7%). Nearly 45% of participants spent <600 MET-min/week in total physical activity, with a higher proportion in women (47.9%) than in men (40.9%) (Table 2). Commuting physical activity (34% men, 46% women) contributed most to total physical activity, followed by recreational (33% men, 25% women), occupational (28% men, 8% women) and household (5% men, 21% women) activities (Fig. 1).
Table 2.
Current and counterfactual scenarios of physical activity among Brazilian adults between 18 and 69 years of age, by sex
| Physical activity (MET-min/week) | ||||
|---|---|---|---|---|
| <600 | 600–3999 | 4000–7999 | >8000 | |
| Both | ||||
| Current distribution (%) | 44.6 | 41.3 | 7.6 | 6.5 |
| Counterfactual scenarios (%) | ||||
| Theoretical minimum risk exposure level (≥8000 MET-min/week) | 0.0 | 0.0 | 0.0 | 100.0 |
| Physical activity recommendation (≥600 MET-min/week) | 0.0 | 85.9 | 7.6 | 6.5 |
| 10% reduction in insufficient physical activity | 40.2 | 45.7 | 7.6 | 6.5 |
| Gender equality in physical activity | 40.9 | 38.7 | 9.7 | 10.6 |
| Men | ||||
| Current distribution (%) | 40.9 | 38.7 | 9.7 | 10.6 |
| Counterfactual scenarios (%) | ||||
| Theoretical minimum risk exposure level (≥8000 MET-min/week) | 0.0 | 0.0 | 0.0 | 100.0 |
| Physical activity recommendation (≥600 MET-min/week) | 0.0 | 79.6 | 9.7 | 10.6 |
| 10% reduction in insufficient physical activity | 36.8 | 42.8 | 9.7 | 10.6 |
| Gender equality in physical activity | 40.9 | 38.7 | 9.7 | 10.6 |
| Women | ||||
| Current distribution (%) | 47.9 | 43.6 | 5.7 | 2.7 |
| Counterfactual scenarios (%) | ||||
| Theoretical minimum risk exposure level (≥8000 MET-min/week) | 0.0 | 0.0 | 0.0 | 100.0 |
| Physical activity recommendation (≥600 MET-min/week) | 0.0 | 91.5 | 5.7 | 2.7 |
| 10% reduction in insufficient physical activity | 43.2 | 48.4 | 5.7 | 2.7 |
| Gender equality in physical activity | 40.9 | 38.7 | 9.7 | 10.6 |
Fig. 1.
Current physical activity level in metabolic equivalent tasks per min per week (MET-min/week) among Brazilian adults between 18 to 69 years of age, by domain of physical activity and sex.
The current distribution and counterfactual scenarios of total physical activity by sex are also presented in Table 2. By assuming a 10% relative reduction in insufficient physical activity, the proportion of adults spending <600 MET-min/week would change from 44.6% (40.9% men, 47.9% women) to 40.2% (36.8% men, 43.2% women). If gender-equality scenario were achieved, the prevalence of insufficient physical activity would decrease 15% (absolute difference: 7.0 percentage points) in women and, consequently, 8% (absolute difference: 3.7 percentage points) in both sexes.
In the theoretical minimum risk exposure level scenario, we estimated that around 16 714 premature deaths from NCDs could be avoided by increasing population-wide physical activity. Estimates ranged from 1236 (11.9%) preventable deaths from breast cancer to 4548 (20.2%) preventable deaths from diabetes. Indeed, around 16% or 10 022 premature deaths from CVD (ischemic heart disease and stroke) could be avoided in this scenario. Preventable deaths from all five outcomes (diabetes, ischemic heart disease, stroke, breast cancer and colon cancer) accounted for 5.75% of premature deaths form major NCDs and 3.23% of premature deaths from all-causes (Table 3).
Table 3.
Preventable premature deaths (from 30 to 69 years) from cancer (breast and colon), diabetes and cardiovascular disease (IHD and stroke) by increasing population-wide physical activity in Brazil
| Outcomes | Total premature deaths (n)a | TMREL (≥8000 MET-min/week) | PA recommendation (≥600 MET-min/week) | 10% reduction in insufficient physical activityb | Gender equality | ||||
|---|---|---|---|---|---|---|---|---|---|
| PAF | Preventable premature deaths (n) | PIF | Preventable premature deaths (n) | PIF | Preventable premature deaths (n) | PIF | Preventable premature deaths (n) | ||
| Breast cancer | |||||||||
| Both | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Men | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Women | 10 480 | 11.79 | 1236 | 1.65 | 173 | 0.16 | 17 | 1.18 | 124 |
| Colon cancer | |||||||||
| Both | 5313 | 17.14 | 908 | 4.47 | 237 | 0.45 | 24 | 1.15 | 58 |
| Men | 2624 | 16.18 | 425 | 4.15 | 109 | 0.42 | 11 | 0.00 | 0 |
| Women | 2689 | 17.99 | 484 | 4.76 | 128 | 0.48 | 13 | 2.16 | 58 |
| Diabetes | |||||||||
| Both | 22 618 | 20.22 | 4548 | 7.05 | 1583 | 0.70 | 158 | 1.47 | 299 |
| Men | 11 748 | 19.04 | 2236 | 6.56 | 771 | 0.66 | 77 | 0.00 | 0 |
| Women | 10 870 | 21.26 | 2311 | 7.48 | 813 | 0.75 | 81 | 2.75 | 299 |
| IHDc | |||||||||
| Both | 51 566 | 15.96 | 8038 | 4.51 | 2262 | 0.45 | 226 | 1.17 | 375 |
| Men | 34 514 | 14.97 | 5167 | 4.18 | 1444 | 0.42 | 144 | 0.00 | 0 |
| Women | 17 048 | 16.84 | 2871 | 4.79 | 817 | 0.48 | 82 | 2.20 | 375 |
| Stroke | |||||||||
| Both | 11 817 | 17.00 | 1984 | 7.04 | 819 | 0.70 | 82 | 1.11 | 102 |
| Men | 6917 | 16.07 | 1111 | 6.53 | 452 | 0.65 | 45 | 0.00 | 0 |
| Women | 4899 | 17.82 | 873 | 7.49 | 367 | 0.75 | 37 | 2.08 | 102 |
| Major NCDs | |||||||||
| Both | 290 874 | 5.75 | 16 714 | 1.74 | 5073 | 0.17 | 507 | 0.33 | 958 |
| Men | 163 881 | 5.45 | 8939 | 1.69 | 2775 | 0.17 | 278 | 0.00 | 0 |
| Women | 126 963 | 6.12 | 7775 | 1.81 | 2298 | 0.18 | 230 | 0.75 | 958 |
| All-cause mortality | |||||||||
| Both | 517 134 | 3.23 | 16 714 | 0.98 | 5073 | 0.10 | 507 | 0.19 | 958 |
| Men | 325 583 | 2.75 | 8939 | 0.85 | 2775 | 0.09 | 278 | 0.00 | 0 |
| Women | 191 477 | 4.06 | 7775 | 1.20 | 2298 | 0.12 | 230 | 0.50 | 958 |
Abbreviation: IHD, Ischemic heart disease. Major NCDs: non-communicable diseases targeted by the World Health Organization (WHO) Global Action Plan for 2025 were diabetes (ICD E10-E14), cardiovascular diseases (ICD I00-I99), cancer (ICD C00-C97) and chronic respiratory diseases (ICD J30-J98); PA, physical activity; TMREL, theoretical minimum risk exposure level; PIF, potential impact fraction.
aNationwide deaths in 2015 among people aged 30–69.
bInactivity defined as ≤600 MET-min/week.
cBoth sex category does not sum-up sex-specific number of deaths due to missing information about sex (4 deaths for IHD; 1 death for stroke; 74 deaths for all-cause mortality).
Achieving at least the physical activity recommendation (≥600 MET-min/week) could potentially avoid 1.65% (173 deaths) premature deaths from breast cancer and 7.05% (1 583 deaths) from diabetes. Overall, around 5 073 premature deaths could be potentially avoided in this scenario, corresponding to 1.74 and 0.98% of premature deaths from major NCD and all-causes, respectively.
A 10% relative reduction in insufficient physical activity could reduce <1% of all five outcomes, with a total of 507 preventable premature deaths (Table 3).
Increasing physical activity in women to levels observed in men (gender-equality scenario) could potentially avoid, on average, 2% of premature deaths from breast, colon, diabetes, ischemic heart disease and stroke (Table 3).
Sensitivity analysis
Sensitivity analysis considering only recreational and commuting physical activities suggested slightly higher preventable premature death from NCDs. In these two domains, ~60% of participants spent less than 600 MET-min/week, with a higher proportion in women (62.5%) than in men (56.2%). Only 0.9% of men and 0.2% of women achieved at least 8000 MET-min/week in recreational and commuting physical activities. We estimated that increasing recreational and commuting physical activity could potentially avoid up to 19 259 premature deaths from NCDs in Brazil. Preventable premature deaths represented 6.6% of premature deaths from NCDs and 3.7% of premature deaths from all-causes in Brazil in 2015 (Tables S2–S4).
Discussion
Physical activity could potentially avoid up to 16 700 premature deaths from NCDs, which correspond to 5.75% of premature deaths from major NCDs and 3.23% of premature deaths from all-causes per year in Brazil. Reaching at least the physical activity recommendation (600 MET-min/week) could potentially avoid 5 000 premature deaths from NCDs per year in Brazil. A 10% relative reduction in insufficient physical activity showed limited impact on premature deaths from NCDs. On the other hand, eliminating gender differences in physical activity showed moderate benefit, estimated to prevent 1000 premature deaths from NCDs.
PAF estimates gained momentum in the physical activity epidemiology literature after the seminal paper published by Lee and colleagues in the first Lancet Physical Activity Series, in 2012.21 This study suggested that around 9% or 5.3 million premature deaths worldwide were attributable to physical inactivity.21 In the same year, estimates from Global Burden of Disease (GBD) suggested that physical inactivity was responsible for around 6% (3.2 million premature deaths) per year.22 In Brazil, PAF estimates were 13.2% by Lee et al.21 and 2.8% by GBD,22 whereas we found that 3.2% of all deaths could be potentially avoided. Differences in PAF estimates could be due to several methodological issues, such as the equations used, source of physical activity data, exposure definition, and RR estimates.23,24 In addition, both GBD and our estimates considered cause-specific RR, whereas Lee et al. considered all-cause relative risks, to compute the total number of attributable deaths.23,24 It is worth noting that all these estimates reflect the theoretical minimum risk exposure level, which despite being informative, is unfeasible in the real world.
Studies on the impact of plausible counterfactual scenarios of physical activity on premature deaths from NCDs are sparse in the literature, despite its clear importance to inform policy makers. We found that achieving the physical activity recommendation may substantially reduce the proportion and number of premature deaths from NCDs, but this recommendation may not be achievable for the entire population.25,26 On the other hand, reaching the WHO 25 × 25 target for physical activity (a 10% relative reduction in insufficient physical activity) is likely to have a limited impact on premature deaths from NCDs in Brazil. These results do not necessarily suggest that physical activity should be neither neglected, nor quantitative recommendations ignored. It does, however, reinforce the need for a multisector effort to make physical activity convenient, pleasurable and meaningful,27 so more audacious (but feasible) targets could be reached. In addition, the expected net benefit of interventions promoting population-wide physical activity could be substantial given that few negative side effects and non-responders are likely to occur.28,29 Finally, these results highlight the importance of concomitantly tackling other determinants of NCDs (e.g. smoking) to reach the 25% reduction in premature deaths from NCDs by 2025.6
Gender inequality in physical activity is also an important concern. Activity inequality between countries has been highly driven by the gender gap in physical activity.12 Globally, relative and absolute differences in the prevalence of insufficient physical activity are 20% and 7.5 percentage points, respectively, in favor of men.11 We found similar figures of gender inequality in the prevalence of insufficient physical activity in Brazil (relative difference: 20%; absolute difference: 7.9 percentage points), and showed that these differences are even more pronounced among those reaching 8000 MET-min/week (relative difference: 390%; absolute difference: 7 percentage points). Yet, most of these differences are driven by occupational physical activity. In Brazil, for instance, 28% of men’s and 8% of women’s total physical activity are occupational activities. Obligatory occupational physical activity has shown less consistent benefit on reduced risk of deaths from NCDs than other domains of physical activity.9,19,20 However, heterogeneity in effect sizes between domains of physical activity could be due to residual confounding by socioeconomic status.30 We argue that promotion of physical activity should be focused on recreational and commuting physical activity. Currently, recreational physical activity contributes to 33 and 25% of total physical activity in men and women, respectively. Although commuting physical activity contributes to a higher proportion of total physical activity in women (46%), relative to men (34%), there is still absolute differences in the volume of commuting physical activity favoring men (423 MET-min/week in men versus 397 MET-min/week in women). Considering only recreational and commuting physical activity, ~60% of adults spent less than 600 MET-min/week in Brazil. Eliminating gender differences in recreational and commuting physical activity should be considered an important target for increasing physical activity levels and, therefore, preventing premature deaths from NCDs in Brazil.
Our study adds knowledge to estimates of preventable premature deaths from NCDs, especially for policy relevant, plausible counterfactual scenarios of physical activity. We used data from a large nationally representative health survey to estimate the distribution of total physical activity in Brazil and retrieved maximally adjusted RR estimates from a recent dose–response meta-analysis of prospective studies.7,16 Physical activity distribution and RR were consistently used in terms of physical activity construct (total physical activity, in MET-min/week) and cut-offs (<600, 600–3999, 4000–7999 and ≥8000 MET-min/week). Nonetheless, there are several data limitations. The current physical activity level was assessed using questionnaire and did not include information about the intensity of physical activities. However, we used the 2011 compendium of physical activities to assign average METs to self-reported recreational physical activities as well as other domain of physical activity. RR estimates from the dose–response meta-analysis7,16 were derived mainly from USA and European cohort studies and whether they are applicable to the Brazilian population is unknown. These RR estimates were not available by type (e.g. aerobic and resistance), domain (recreational, occupational, commuting and household) and intensity (e.g. moderate and vigorous) of activities. Despite using multiple RR categories of total physical activity, these estimates did not capture potential benefits of shifting from inactivity to low physical activity levels (e.g. 300 MET-min/week) on premature deaths from NCDs. Some RR included in the dose–response meta-analysis were adjusted by potential mediators (e.g. body mass index, systolic blood pressure) through which physical activity may reduce the risk of NCDs. These limitations may have underestimated the impact of physical activity on premature deaths from NCDs. In addition, physical activity was self-reported rather than objectively measured, thus biases arising from measurement error is likely to have occurred. Finally, we restricted our analysis to prevention of premature deaths from NCDs targeted in the WHO 25 × 25, but physical activity may confer further benefits on other NCDs (e.g. dementia)31 as well as overall population health.8
Physical activity may play an important role to reduce premature deaths from NCDs in Brazil. The WHO target for physical activity (10% relative reduction in insufficient physical activity) might be a feasible goal but suggested a limited impact on prevention of premature deaths from NCDs. On the other hand, interventions and policies aiming at tackling structural determinants of gender inequality in physical activity might confer a moderate impact on premature deaths from NCD in Brazil.
Supplementary Material
Acknowledgements
None.
Funding
LFMR receives a doctoral scholarship from Sao Paulo Research Foundation (FAPESP) (Grants 2014/25614-4 and 2016/21390-0). LMTG undertook this work under the auspices of the Centre for Diet and Activity Research (CEDAR), a UKCRC Public Health Research Centre of Excellence which is funded by the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, the National Institute for Health Research, and the Wellcome Trust.
Conflict of interest
None.
References
- 1. Doll R. Foreword In: Peto R, Lopez AD, Boreham J et al. (eds). Mortality From Smoking in Developed Countries 1950–2000. Oxford: Oxford University Press, 1994. [Google Scholar]
- 2. Norheim OF, Jha P, Admasu K et al. Avoiding 40% of the premature deaths in each country, 2010–30: review of national mortality trends to help quantify the UN sustainable development goal for health. Lancet 2015;385:239–52. [DOI] [PubMed] [Google Scholar]
- 3. World Health Organization (WHO). Global Status Report on Noncommunicable Diseases 2014. Geneva: WHO press, 2014. [Google Scholar]
- 4. Allen L, Cobiac L, Townsend N. Quantifying the global distribution of premature mortality from non-communicable diseases. J Public Health 2017;39:698–703. [DOI] [PubMed] [Google Scholar]
- 5. Brasil. Ministério da Saúde. Sistema de Informações Sobre Mortalidade (SIM) de 1996 a 2015 Brasília 2017 [09/11/2017]. http://tabnet.datasus.gov.br/cgi/deftohtm.exe?sim/cnv/obt10uf.def.
- 6. Peto R, Lopez AD, Norheim OF. Halving premature death. Science 2014;345:1272. [DOI] [PubMed] [Google Scholar]
- 7. Kyu HH, Bachman VF, Alexander LT et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013. Br Med J 2016;354:i3857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. World Health Organization (WHO). Global Recommendations on Physical Activity for Health. Geneva: World Health Organization, 2010. [PubMed] [Google Scholar]
- 9. Rezende LFM, Sa TH, Markozannes G et al. Physical activity and cancer: an umbrella review of the literature including 22 major anatomical sites and 770 000 cancer cases. Br J Sports Med 2018;52:826–33. [DOI] [PubMed] [Google Scholar]
- 10. Brown WJ, Mielke GI, Kolbe-Alexander TL. Gender equality in sport for improved public health. Lancet 2016;388:1257–8. [DOI] [PubMed] [Google Scholar]
- 11. Mielke GI, da Silva ICM, Kolbe-Alexander TL et al. Shifting the physical inactivity curve worldwide by closing the gender gap. Sports Med 2018;48:481–9. [DOI] [PubMed] [Google Scholar]
- 12. Althoff T, Sosic R, Hicks JL et al. Large-scale physical activity data reveal worldwide activity inequality. Nature 2017;547:336–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Szwarcwald CL, Malta DC, Pereira CA et al. [National Health Survey in Brazil: design and methodology of application]. Cien Saude Colet 2014;19:333–42. [DOI] [PubMed] [Google Scholar]
- 14. Instituto Brasileiro de Geografia e Estatística. Pesquisa Nacional de Saúde 2013: Percepção do Estado de Saúde, Estilo de Vida e Doenças Crônicas Brasil, Grandes Regiões e Unidades da Federação. Rio de Janeiro: IBGE; 2013 [cited 2017 03 April]. http://www.ibge.gov.br/home/estatistica/populacao/pns/2013/.
- 15. Ainsworth BE, Haskell WL, Herrmann SD et al. 2011 Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc 2011;43:1575–81. [DOI] [PubMed] [Google Scholar]
- 16. Risk GBD. Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1659–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Murray CJL, Ezzati M, Lopez AD et al. Comparative quantification of health risks: conceptual framework and methodological issues. Popul Health Metr 2003;1:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Poole C. A history of the population attributable fraction and related measures. Ann Epidemiol 2015;25:147–54. [DOI] [PubMed] [Google Scholar]
- 19. Samitz G, Egger M, Zwahlen M. Domains of physical activity and all-cause mortality: systematic review and dose-response meta-analysis of cohort studies. Int J Epidemiol 2011;40:1382–400. [DOI] [PubMed] [Google Scholar]
- 20. Hallman DM, Birk Jorgensen M, Holtermann A. On the health paradox of occupational and leisure-time physical activity using objective measurements: effects on autonomic imbalance. PLoS One 2017;12:e0177042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lee IM, Shiroma EJ, Lobelo F et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 2012;380:219–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lim SS, Vos T, Flaxman AD et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lee IM, Bauman AE, Blair SN et al. Annual deaths attributable to physical inactivity: whither the missing 2 million? Lancet (London, England) 2013;381:992–3. [DOI] [PubMed] [Google Scholar]
- 24. Lim SS, Carnahan E, Danaei G et al. Annual deaths attributable to physical inactivity: whither the missing 2 million?—Authors’ reply. Lancet 2013;381:993. [DOI] [PubMed] [Google Scholar]
- 25. Barreto PS. Why are we failing to promote physical activity globally? Bull World Health Organ 2013;91:390-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Barreto PS. Global health agenda on non-communicable diseases: has WHO set a smart goal for physical activity? Br Med J 2015;350:h23. [DOI] [PubMed] [Google Scholar]
- 27. Silva KS, Garcia LM, Rabacow FM et al. Physical activity as part of daily living: moving beyond quantitative recommendations. Prev Med 2017;96:160–2. [DOI] [PubMed] [Google Scholar]
- 28. Salkever DS, Johnston S, Karakus MC et al. Enhancing the net benefits of disseminating efficacious prevention programs: a note on target efficiency with illustrative examples. Adm Policy Ment Health 2008;35:261–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ross R, de Lannoy L, Stotz PJ. Separate effects of intensity and amount of exercise on interindividual cardiorespiratory fitness response. Mayo Clin Proc 2015;90:1506–14. [DOI] [PubMed] [Google Scholar]
- 30. Wade KH, Richmond RC, Davey Smith G. Physical activity and longevity: how to move closer to causal inference. Br J Sports Med 2018;52:890–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sallis JF, Bull F, Guthold R et al. Progress in physical activity over the Olympic quadrennium. Lancet 2016;388:1325–36. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.