Abstract
Background
There are significant geographic disparities in the delivery of IBD healthcare in Ontario which may ultimately impact health outcomes. Telemedicine-based health services may potentially bridge gaps in access to gastroenterologists in remote and underserved areas.
Methods
We conducted a needs assessment for IBD specialist care in Ontario using health administrative data. As part of a separate initiative to address geographic disparities in access to care, we described the development and implementation of our Promoting Access and Care through Centres of Excellence (PACE) Telemedicine Program. Over the first 18 months, we measured wait times and potential cost savings.
Results
We found substantial deficiencies in specialist care early in the course of IBD and continuous IBD care in regions where the number of gastroenterologists per capita were low. The PACE Telemedicine Program enabled new IBD consultations within a median time of 17 days (interquartile range [IQR], 7–32 days) and visits for active IBD symptoms with a median time of 8.5 days (IQR, 4–14 days). Forty-five percent of new consultations and 83% of patients with active IBD symptoms were seen within the target wait time of two weeks. Telemedicine services resulted in an estimated cost savings of $47,565 among individuals who qualified for Ontario’s Northern Travel Grant.
Conclusions
The implementation of telemedicine services for IBD is highly feasible and can reduce wait times to see gastroenterologists that meet nationally recommended targets and can lead to cost savings.
Keywords: Crohn's disease, Inflammatory bowel disease, Specialist, Telemedicine, Ulcerative colitis
Telemedicine is changing healthcare delivery in an attempt to provide practical, cost-effective, and high-quality care to patients. The Promoting Access and Care through Centres of Excellence (PACE) Inflammatory Bowel Disease (IBD) Telemedicine Program at Mount Sinai Hospital System (MSH) in Toronto provides telemedicine consultations for patients who reside in underserviced areas of Ontario. In addition to newly referred patients to telemedicine, our program serves current patients from our IBD centre who live in geographically remote regions.
In Ontario, there is substantial geographic variation in access to gastroenterologists who primarily care for IBD patients. There is evidence to suggest that specialist care early in the course of disease may improve IBD outcomes (1). However, lack of access to specialists may significantly delay wait times. Though the recommended wait times to see a specialist for IBD is two weeks, national audits suggest that the wait time is closer to 126 days (2, 3). Telemedicine has the potential to bridge gaps in access to gastroenterology care by connecting gastroenterologists who practice in areas with surplus of specialists with patients in areas where there is poorer access.
For more than three decades, several studies have investigated the use of telecommunication to advance health outcomes (4–7). Telemedicine, in its simplest definition, is the use of electronic information and communication technologies to provide health care for patients who are not seen in person but rather at distance. With constantly evolving information and communication technologies, the World Health Organization (WHO) anticipates telemedicine will help to address health access and equity issues. According to the WHO, telemedicine programs must aim to provide clinical support and intend to overcome geographical barriers using information and communication technologies with the objective to enhance health outcomes.
With the current financial constraints facing our healthcare system, telemedicine can be utilized in nonurban settings to save on unnecessary utilization of emergent health services and other costs that accrue from travelling to see a gastroenterologist for medical services that do not necessarily require a physical presence. In this context, telemedicine has the potential to reshape health care and fundamentally alter the in-person, face-to-face relationship that has been the model for medical care for generations. We are fortunate to be in a time characterized by rapidly advancing technology and innovative approaches to care. Therefore, it is necessary that we utilize the available technology to deliver specialized care to marginalized populations due to geographic location.
In reviewing the literature, telemedicine in rheumatology reportedly enhances access to care and the patient-rheumatologist partnership (4). In fact, tele-rheumatology was found to be a feasible and acceptable mode of care delivery by patients (7). Diagnostic accuracy of televisual consultation reached 97%, a level that was acceptable to physicians and general practitioners (6). Clinicians have also studied telemedicine among IBD patients. In one example, Home Automated Telemanagement, which is a patient-centred, computerized disease management program, was found to increase patients’ awareness and control over their IBD symptoms (8). Telemedicine was also considered to be critical for improving adherence, self-efficacy, and patient knowledge in IBD (9). Finally, in a pilot study, IBD telemedicine for outpatient service resulted in a high level of patient satisfaction similar to that achieved in regular clinical consultations (10).
Rigorous evaluation of telemedicine programs is just as necessary for telemedicine development as it is for other health care technologies. The Institute of Medicine (IOM) has determined critical evaluative criteria of a telemedicine program. The evaluative criteria include factors such as quality of care, accessibility to services, cost and acceptability of the model of care by both healthcare providers and patients. Responding to the evaluative criteria of the report, we are addressing the following two questions that evaluate telemedicine programs:
1. What is the difference in the cost of the telemedicine program for patients and families compared with alternative(s)?
2. Is the telemedicine program able to enhance the timeliness of care compared with the alternative(s)?
In this article, we describe two related studies: (1) a needs assessment of IBD specialty care in Ontario using health administrative data and (2) the implementation of an IBD-focused telemedicine program in Ontario to address gaps in specialty care.
METHODS
Data Sources for Specialist Needs Assessment
We used Ontario health administrative databases that included the Ontario Health Insurance Plan (OHIP) database, the Canadian Institute for Health Information Discharge Abstract Database (CIHI-DAD), the Registered Person’s Database (RPDB) and the ICES Physician Database (IPDB). These datasets were linked using unique encoded identifiers and analyzed at the Institute for Clinical Evaluative Sciences (ICES). We evaluated the healthcare utilization patterns of the Ontario Crohn’s and Colitis Cohort, a population-based inception cohort of IBD patients in Ontario. This cohort was derived from health administrative data using algorithms validated specifically in Ontario that have been previously described (11). We differentiated newly diagnosed IBD (incident cases) from prevalent cases by using an eight-year look-back period to ensure there were no diagnosis codes for IBD in that time window. This algorithm was more than 95% accurate in distinguishing prevalent from incident cases (11). We included adults (>18 years) diagnosed between 1999 and 2008 and followed healthcare utilization through March 31, 2013.
We measured three key indicators of IBD healthcare services: number of gastroenterologists per capita (from 2013), early gastroenterology care and continuous gastroenterology care. Gastroenterologists were identified using the specialty code (41) in the IPDB. Early gastroenterology care was defined as having at least one IBD-related visit to a gastroenterologist within the first 12 months of diagnosis. Continuous IBD care was defined as having at least one gastroenterologist visit every 12 ± 3 months for the first five years among patients with at least five years of follow-up. This analysis of continuous IBD was restricted to individuals with IBD with at least five years of follow-up in the OCCC by March 31, 2013. These indicators were measured for 13 of Ontario’s 14 local health integration networks (LHINs). Kingston (LHIN 10) was excluded from analysis because physicians in that LHIN are not fee-for-service but instead perform “shadow billing.” We also determined the number of gastroenterologists per 100,000 capita for the 13 LHINs.
Description of PACE Telemedicine Program
The Promoting Access to Centres of Excellence (PACE) IBD program was developed in collaboration with Crohn’s and Colitis Canada to improve access to and quality of care for IBD patients. This $2.6 million initiative funds five of the largest IBD centres in the country (McGill University, McMaster University, University of Toronto, University of Alberta and University of Calgary) over a four-year period that ends in 2020. The PACE Telemedicine Program, more specifically, was developed to improve access to IBD specialists for patients living in remote and underserviced areas in Ontario. Launched on June 1, 2016, it operates from Mount Sinai Hospital’s IBD Centre of Excellence. The telemedicine team includes six gastroenterologists specializing in IBD care, a colorectal surgeon, two registered nurses and a dietitian. Telemedicine consultations are conducted through a secure online platform hosted by the Ontario Telemedicine Network (OTN). The program aims to reduce the cost and burden associated with long distance travel to an IBD specialist. However, when patients require an endoscopic procedure or specialized testing that is not available in smaller communities, travel to our IBD centre may be necessary.
For patients to be eligible for the program, they must reside at least 100 kilometers away from our IBD centre. Our telemedicine program accepts referrals (a) for the diagnosis of IBD, (b) for the ongoing management of IBD or (c) as a second opinion regarding the treatment of medically complex IBD patients. Primary care providers or specialists can initiate the referral by completing a one-page referral form that can be downloaded from the following website: www.zanecohencentre.com/pdfs/IBD/PACE/PACE_IBD_REFERRAL_AUG2016.pdf and asked to prioritize the referral as urgent (within 14 days), expedited (within one month) or a standard appointment (up to three months). Along with completing the referral form, the referring health care provider is requested to forward recent medical imaging results, endoscopy reports, surgical notes and lab results.
Upon triage of the referral, an IBD telemedicine nurse coordinator then arranges the appointment and contacts the patient to gather additional IBD-related health information. Based on the patient’s residential address, the nurse coordinator identifies the nearest telemedicine hosting site, which is often located at a hospital or within a family health team and books the telemedicine consultation or follow-up visit through OTN’s online platform. Before the start of the consultation, a physical assessment is completed by an OTN nurse at the remote site, and the results are communicated to the consulting gastroenterologist. These nurses at remote sites are requested to review an instructional video and primer on how to complete an abdominal exam. The consultation then follows the same procedures as an in-office appointment. After the consultation, the IBD telemedicine coordinator provides the patient with a brief written summary of their plan of care. She also follows up with patients to help coordinate elements of their care plan, such as arranging lab tests, diagnostic imaging and referrals to other health related services. The PACE Telemedicine Program has also expanded its services to include inpatient consultations for hospitalized IBD patients who require expertise in medical management or, in some cases, consideration for transfer to Mount Sinai Hospital for surgery.
Several systematic reviews supported the benefits of remote patient monitoring (RPM), as it was found to enhance patient outcomes by providing continuous self-monitoring for patients and enabling clear communication with health care professionals (12). Since February 2018, the PACE Telemedicine Program has piloted the use of RPM to better monitor patients in-between clinical visits. All telemedicine patients have been invited to download the HealthPROMISE app (healthpromise.org) and log in using user-specific credentials. HealthPROMISE has been customized to query patients on disease activity, quality of life and psychological distress using standardized instruments: Harvey-Bradshaw Index (for CD), partial Mayo score (for UC), short inflammatory bowel disease questionnaire (SIBDQ) and the Patient Health Questionnaire (PHQ-2, depression screening). Patients are prompted to complete these questionnaires every two weeks, and the summary scores are reported on a medical provider dashboard that is reviewed by the PACE Telemedicine coordinator. If there is worsening of disease activity or quality of life, the coordinator then contacts the patient to determine whether an earlier clinic appointment is warranted.
Telemedicine Outcomes
Though the PACE program is funded for four years, we report on PACE outcomes between June 1, 2016, and November 30, 2017. We collected data on wait times for seeing a specialist defined as the time interval between when the referral was first received to the time of the IBD clinical visit. A subgroup analysis was performed for wait times among those waiting for their first IBD consultation and those who had active symptoms at the time they made the appointment.
Cost savings from use of telemedicine were solely in respect to the Northern Travel Grant (NTG). To ensure quality health care for underserviced areas, the Ministry of Health and Long-Term Care provides travel reimbursement from the NTG for patients who need to travel at least 100 kilometers one-way to access the closest medical specialist that is unavailable locally. This grant is provided for only 10 districts throughout Ontario. In Ontario on a yearly basis, 200,000 people apply for assistance through the NTG which costs the province approximately $53 million. Patients are reimbursed 41 cents per kilometer after deducting the initial 100 kilometers. Patients are also reimbursed with $100 if the site is more than 200 kilometers away to help cover hotel expenses. If deemed medically necessary for travel, a companion for the patient can also apply for the grant.
In order to calculate cost savings to the NTG program, we determined the average kilometers traveled from an eligible district within which a telemedicine patient resides to our IBD centre and whether the patient was eligible for hotel reimbursement based on the distance. For each telemedicine patient eligible for the NTG, we estimated the round-trip distance based on their district of residence and multiplied that by $0.41 per kilometer and also added the costs of lodging of $100 for patients residing more than 200 kilometers away.
Research Ethics
ICES is a prescribed entity under section 45 of Ontario’s Personal Health Information Protection Act. Section 45 authorizes ICES to collect personal health information, without consent, for the purpose of analysis or compiling statistical information with respect to the management of, evaluation or monitoring of, the allocation of resources to or planning for all or part of the health system. Projects conducted under section 45, by definition, do not require review by a Research Ethics Board. This project was conducted under section 45 and approved by ICES’ Privacy and Compliance Office.
Research protocols for the PACE Telemedicine Program were approved by the Mount Sinai Hospital Research Ethics Board.
RESULTS
Unmet Needs for IBD Specialist Care
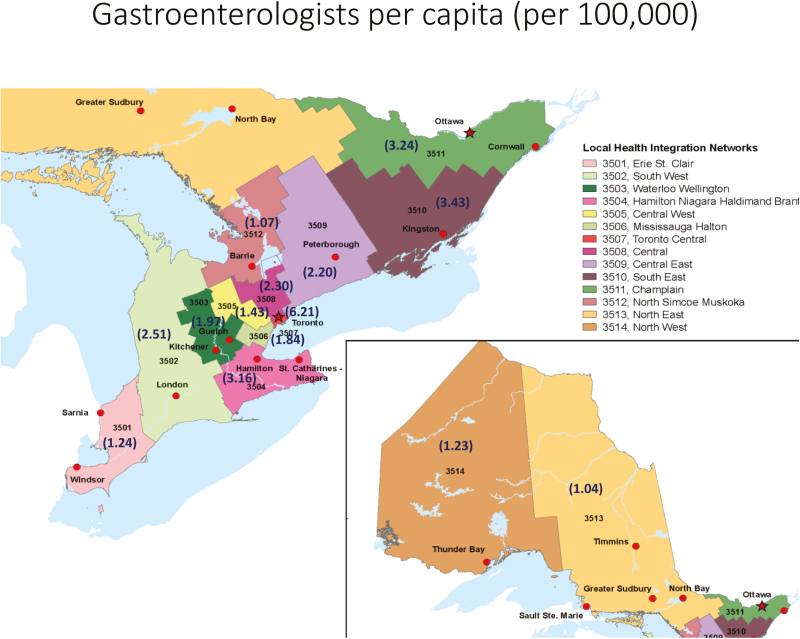
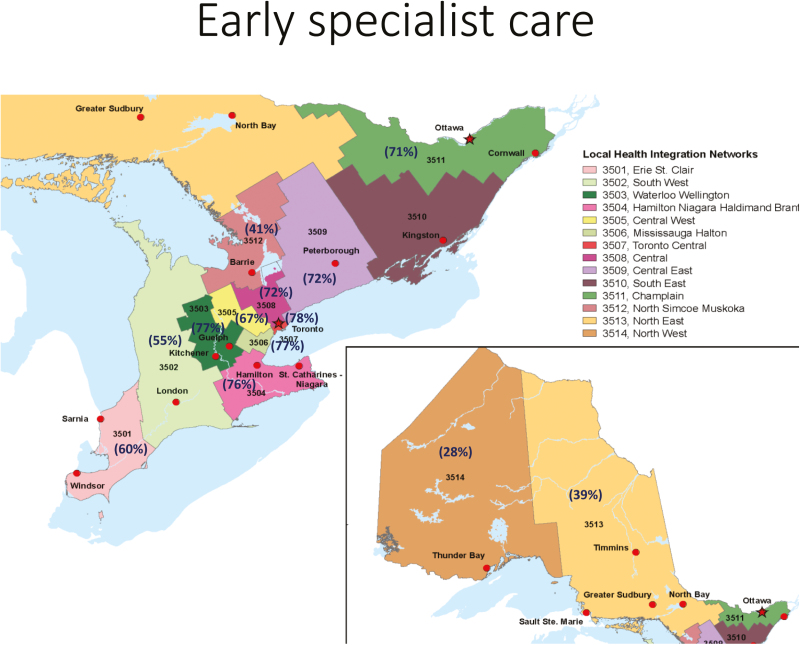
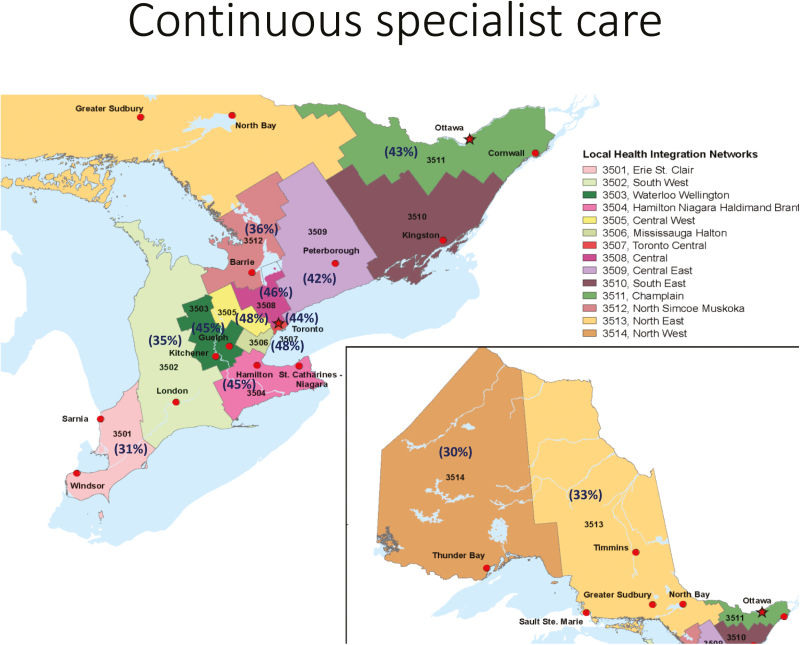
There was substantial geographic variation in the proportion of patients who received early gastroenterology care among Ontario’s 13 local health integration networks (LHINs)(Figure 1 and Appendix 1). Early gastroenterology care was particularly low in the North East (38%), North West (28%) and North Simcoe Muskoka (41%) LHINs compared with the Toronto Central LHIN (78%) and those immediately surrounding it (67%–77%). Continuous IBD care also varied across LHINs (Figure 2 and Appendix 1) and was lowest in the North East (31%), North West (30%) and Erie St. Claire (31%) compared with 48% in Toronto Central. The health regions with lowest implementation of early specialist and continuous IBD care were also the same ones where the fewest gastroenterologists practiced per 100,000 capita, which also varied substantially across Ontario’s LHINs, ranging from 1.04 to 6.21 per 100,000 (Figure 3 and Appendix 1). Thus, the North East, North West, Erie St. Claire, and North Simcoe Muskoka LHINs were designated as areas that could potentially benefit from telemedicine services to bridge geographic disparities in access to gastroenterologists.
Figure 1.
Early specialist care among Ontario’s Local Health Integration Networks (LHINs). The proportion of inflammatory bowel disease patients who received a visit to gastroenterologist within the first year of IBD diagnosis is shown in parentheses.
Figure 2.
Continuous inflammatory bowel disease care among Ontario’s Local Health Integration Networks (LHINs). The proportion of inflammatory bowel disease patients who received at least one gastroenterology visit every 12 ± 3 months during the first five years of diagnosis is shown in parentheses.
Figure 3.
Number of gastroenterologists per capita among Ontario’s Local Health Integration Networks (LHINs). The number of gastroenterologists per 100,000 IBD capita is shown in parentheses for each LHIN.
Patient Population and Outcomes of PACE Telemedicine Program
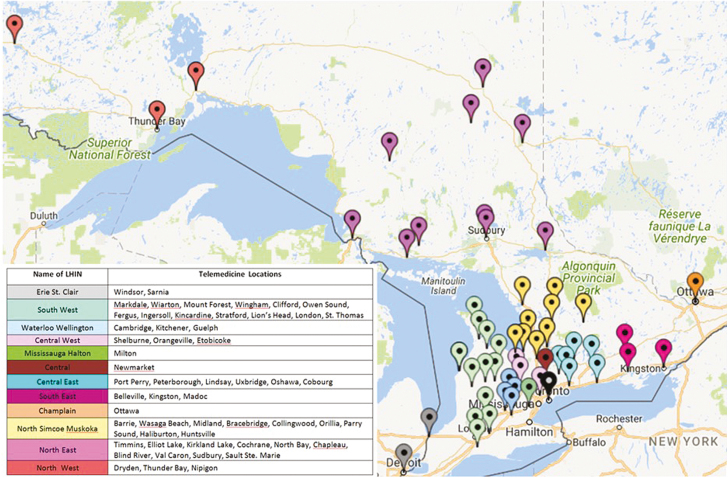
During the first 18 months since its inception, the telemedicine team accepted 99 patients to our telemedicine program and completed 186 telemedicine visits utilizing the resources of the Ontario Telemedicine Network. We provided new consultations for 47 patients newly referred to our program, and we transitioned 52 patients who were currently being cared for at our centre but living in remote areas who requested to be seen via telemedicine. A total of 12 out of the 47 new patients were referred for a second opinion, mainly due to the medically complex nature of their illness. Four hospitalized inpatients underwent a telemedicine consultation: three of them were newly referred to our program, and one was a current patient of MSH living at a distance. Telemedicine activity by month showed an increasing trend of total visits and increasing number of visits with three patients reaching the fifth visit in the 18-month period (See Table 1). During the course of these visits, we established a hosting relationship at 61 remote OTN sites throughout Ontario (Figure 4). The average number of visits per patient was 1.87.
Table 1.
Telemedicine PACE IBD Activity by Month Since Inception
| Telemedicine Activity by Month and Year | ||||||
|---|---|---|---|---|---|---|
| Month & Year | Total Visits | 1 st visit | 2 nd visit | 3 rd visit | 4 th visit | 5 th visit |
| June 2016 | 1 | 1 | ||||
| July 2016 | 0 | 0 | ||||
| August 2016 | 5 | 5 | ||||
| September 2016 | 3 | 3 | ||||
| October 2016 | 6 | 5 | 1 | |||
| November 2016 | 4 | 3 | 1 | |||
| December 2016 | 6 | 3 | 3 | |||
| January 2017 | 7 | 5 | 1 | 1 | ||
| February 2017 | 8 | 4 | 3 | 1 | ||
| March 2017 | 9 | 8 | 1 | |||
| April 2017 | 12 | 11 | 1 | |||
| May 2017 | 15 | 8 | 4 | 2 | 1 | |
| June 2017 | 26 | 7 | 15 | 4 | ||
| July 2017 | 11 | 7 | 1 | 2 | 1 | |
| August 2017 | 9 | 4 | 1 | 3 | 1 | |
| September 2017 | 15 | 6 | 3 | 3 | 2 | 1 |
| October 2017 | 17 | 8 | 5 | 1 | 2 | 1 |
| November 2017 | 33 | 12 | 9 | 6 | 5 | 1 |
| Total Visits | 186 | 99 | 49 | 23 | 12 | 3 |
Figure 4.
Map of remote telemedicine sites within the Ontario Telemedicine Network that have serviced patients in the PACE Telemedicine Program.
Cost Savings
The average distance of travel avoided by our telemedicine cohort was 818 kilometers per visit. However, the distance saved varied dramatically between the different LHINs, with the North East LHIN saving an average of 1137 kilometers and the North West LHIN saving an average of 2791 kilometers.
Thirty-five of 99 telemedicine patients resided in designated areas eligible for the Northern Travel Grant and qualified for government reimbursement for their transportation expenses. Among these eligible patients, the average cost savings per telemedicine consultation was $767.18. Total cost savings for patients who were already established in our clinics and transferred to telemedicine care was $15,410.21, whereas overall total cost savings for new telemedicine program patients was $32,155.06. The breakdown of total travel distance avoided and total cost savings to the NTG program are shown by location in Table 2.
Table 2.
Distance of Travel Avoided and Cost Savings to the Northern Travel Grant by Location of Residence
| Location | Total Travel Distance Avoided (km) | Total Cost Savings (Canadian dollars) |
|---|---|---|
| Blind River | 1,108 | $513.28 |
| Chapleau | 8,450 | $3,759.50 |
| Cochrane | 4,302 | $1,940.83 |
| Dryden | 3,428 | $1,464.48 |
| Elliot Lake | 2,160 | $1,003.60 |
| Kirkland Lake | 1,172 | $539.52 |
| Nipigon | 7,602 | $3,293.82 |
| North Bay | 1,380 | $624.80 |
| Parry Sound | 916 | $493.56 |
| Sault Ste. Marie | 15,114 | $6,847.74 |
| Sudbury | 9,552 | $4,624.32 |
| Thunder Bay | 49,716 | $21,445.56 |
| Timmins | 1,382 | $625.62 |
| Val Caron | 804 | $388.64 |
| TOTAL | 107,086 | $47,565.27 |
Wait Times
We recently evaluated the wait times for new patients from the receipt of the referral to the first telemedicine consultation. The median wait time from time of referral to initial telemedicine consultation was 17 days (interquartile range [IQR], 7–32 days). Overall, 45% of patients attended their telemedicine appointment within 14 days of the referral, thus meeting our target wait times of two weeks or less. Of those who did not undergo consultation within 14 days, the reasons for the delay were the availability of the remote OTN site to host the appointment (16%), patient preference for delaying the appointment (26%) and office scheduling (42%).
We also evaluated the wait time between the request by a patient to be seen for active IBD symptoms and the office visit. In total, 18 patients requested a follow-up telemedicine visit for active IBD symptoms. Among the 18 patients with active IBD symptoms, the median wait time for a telemedicine visit was 8.5 days (IQR, 4–14 days). Overall, 83% of patients who required a telemedicine visit for active IBD symptoms were seen within the 2-week target wait time. Among the three patients who were not seen within 14 days, two were due to scheduling conflicts, and the other was because of patient’s preference for delay.
Discussion
Our needs assessment of IBD healthcare delivery in Ontario highlights geographic disparities in access to and utilization of specialist care. Our analysis was limited by its inability to account for migration of gastroenterologists and patients between geographic regions over time. Moreover, our analysis was limited by the relatively short follow-up period and did not directly assess the clinical impact of gaps in specialty care. However, indirect evidence from other Canadian studies suggest that specialist care is associated with improved clinical outcomes. If rendered within the first year of diagnosis, it was associated with up to one-third reduction in risk of surgery among CD patients most pronounced after two years of diagnosis (1). Moreover, gastroenterology care delivered within the first six months following CD surgery was associated with reduction in IBD-related hospitalizations (13). Finally, inpatient care by a gastroenterologist during a hospitalization for acute-severe ulcerative colitis was associated with lower in-hospital and 12-month mortality (14). Given the potential of gastroenterology care to improve clinical outcomes in IBD, we developed a telemedicine program under the auspices of the PACE network to improve access to specialist care in underserved areas.
During the first 18 months of its operation, we have demonstrated that the PACE Telemedicine Program provided a feasible approach to bridging regional disparities in access to specialist care for IBD. The telemedicine program’s median wait times for new consultations and visits for active IBD symptoms of 17 days and 8.5 days, respectively, were considerably lower than the median 126 days reported by historical controls obtained through national audits. One of the study’s limitations is that we do not have recent wait time data for in-person consultations at our centre with which to compare. However, it is important to note that for patients with active IBD symptoms, the telemedicine program was able to achieve the target wait time of less than two weeks.
Telemedicine also has the potential to yield significant cost savings. The operating costs for the telemedicine program during its first year was $92,000, which was allocated toward the salary of the telemedicine nurse coordinator. The OTN provided in-kind support for other infrastructural operating costs (e.g., telemedicine hardware and software and nursing, physical space, and administrative costs at remote sites). The program saved the provincial government nearly $50,000 based only on individuals who qualified for the Northern Travel Grant. Our analysis underestimated savings from indirect costs due to missed work for the patient and family member and for out-of-pocket travel expenses among those did not qualify for the NTG. As the telemedicine program grows, we would expect an increase in the number of patients who qualify for the NTG and an increase in cost savings that could offset the operating costs of the telemedicine program. Currently, Crohn’s and Colitis Canada funds the operating costs of the telemedicine program. We hope to demonstrate by the end of the four-year funding period that the IBD telemedicine program is at least cost-neutral to the provincial government in order to make a case for a business model in which the latter assumes these costs. A formal cost analysis that integrates indirect and patient out-of-pocket costs would be warranted at the conclusion of PACE’s four-year funding period.
In order to improve the program’s outreach, our team is actively addressing barriers to its implementation. These challenges include the limited availability of telemedicine sites, especially in the beginning stages of our program, which delayed some appointment times. The piloting of infrastructural enhancements that enable patients to receive video consultation from their own homes will likely mitigate this issue. The other limitation experienced by our program has been a lack of awareness of our program within Northern Ontario areas that were designated as underserved “target” communities, which resulted in an initial slow uptake of referrals. Over the past 18 months, the PACE program has conducted webinars with key stakeholders in these underserved areas and liaised with OTN to extend its referral base.
One of the key advantages of our program is its multidisciplinary nature. Having an IBD surgeon available to provide consultation for cases that may require surgery facilitated access to surgical services at our high-volume IBD centre. This is important as IBD centres with high surgical volume have demonstrated improved clinical outcomes (15). Consultation with a registered dietitian is also valuable because such services are often not available in many of the remote, underserved communities. As the program moves forward, we hope to integrate other key specialties including psychiatry, rheumatology and dermatology.
Prior studies in other fields suggest telemedicine systems are associated with improved quality of life, patient satisfaction, decreased health resource utilization and indirect costs (16). In addition to demonstrating telemedicine’s capacity to reduce wait times, we are currently measuring other performance metrics that include patient satisfaction, quality of care and quality of life using validated questionnaires, the results of which were not yet available for this analysis. We will also compare these performance measures in our telemedicine cohort with those of a matched cohort of our IBD patients seen in-person at our centre. We also plan to measure indicators of IBD healthcare utilization using data from ICES to see if the telemedicine initiative has reduced geographic disparity.
In conclusion, the PACE telemedicine program has tapped into OTN’s well-developed infrastructure to address deficiencies in access to IBD care. However, these issues are not unique to Ontario. Many other provinces have the technology to adopt telemedicine-based health services, and our program can serve as a prototype for other IBD centres, particularly those in the PACE network, to establish similar telemedicine programs. Moreover, the multidisciplinary nature of our program can serve as a model for the development of telemedicine programs for other chronic diseases in Ontario.
Acknowledgements
The needs assessment study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results and conclusions reported in this article are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred.
Authorship Contributions: GCN, PH and SB conceived and designed the study. GCN drafted the manuscript, and all authors critically reviewed it.
Funding: This study was supported in part by the Promoting Access and Care through Centres of Excellence (PACE) Network in partnership with Crohn’s and Colitis Canada.
Conflicts of Interest: GCN is supported by a Canadian Institutes of Health Research (CIHR) Embedded Clinician Researcher Award. All other authors report no conflicts of interest.
Appendix 1. Indicators of Access to Specialist Care and Health Care Utilization by Local Health Integration Networks
| LHIN | LHIN name | IBD Population |
Gastroenterologists
per 100,000 capita |
Early Specialist Care (%) | Continuous Specialist Care (%) |
|---|---|---|---|---|---|
| 1 | Erie St. Clair | 4,791 | 1.24 | 60% | 31% |
| 2 | South West | 6,504 | 2.51 | 55% | 35% |
| 3 | Waterloo Wellington | 4,828 | 1.97 | 77% | 45% |
| 4 | Hamilton Niagara Haldimand Brant | 9,349 | 3.16 | 76% | 45% |
| 5 | Central West | 4,523 | 1.43 | 67% | 48% |
| 6 | Mississauga Halton | 6,469 | 1.84 | 77% | 48% |
| 7 | Toronto Central | 7,045 | 6.21 | 78% | 44% |
| 8 | Central | 9,441 | 2.3 | 72% | 46% |
| 9 | Central East | 9,431 | 2.2 | 72% | 42% |
| 11 | Champlain | 8,618 | 3.24 | 71% | 43% |
| 12 | North Simcoe Muskoka | 3,392 | 1.07 | 41% | 36% |
| 13 | North East | 4,504 | 1.04 | 39% | 33% |
| 14 | North West | 1,674 | 1.23 | 28% | 30% |
References
- 1. Nguyen GC, Nugent Z, Shaw S, et al. . Outcomes of patients with Crohn’s disease improved from 1988 to 2008 and were associated with increased specialist care. Gastroenterology 2011;141:90–7. [DOI] [PubMed] [Google Scholar]
- 2. Paterson WG, Depew WT, Pare P, et al. . Canadian consensus on medically acceptable wait times for digestive health care. Can J Gastroenterol 2006;20:411–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Leddin D, Armstrong D, Borgaonkar M, et al. . The 2012 SAGE wait times program: Survey of access to GastroEnterology in Canada. Can J Gastroenterol 2013;27:83–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nakamura N, Koga T, Iseki H. A meta-analysis of remote patient monitoring for chronic heart failure patients. J Telemed Telecare 2014;20:11–7. [DOI] [PubMed] [Google Scholar]
- 5. McLean S, Nurmatov U, Liu JL, et al. . Telehealthcare for chronic obstructive pulmonary disease: Cochrane Review and meta-analysis. Br J Gen Pract 2012;62:e739–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. El Miedany Y. e-Rheumatology: Are we ready?Clin Rheumatol 2015;34:831–7. [DOI] [PubMed] [Google Scholar]
- 7. Leggett P, Graham L, Steele K, et al. . Telerheumatology—diagnostic accuracy and acceptability to patient, specialist, and general practitioner. Br J Gen Pract 2001;51:746–8. [PMC free article] [PubMed] [Google Scholar]
- 8. Castro HK, Cross RK, Finkelstein J. Using a Home Automated Telemanagement (HAT) system: Experiences and perceptions of patients with inflammatory bowel disease. AMIA Annu Symp Proc 2006:872. [PMC free article] [PubMed] [Google Scholar]
- 9. Cross RK, Jambaulikar G, Langenberg P, et al. . TELEmedicine for Patients with Inflammatory Bowel Disease (TELE-IBD): Design and implementation of randomized clinical trial. Contemp Clin Trials 2015;42:132–44. [DOI] [PubMed] [Google Scholar]
- 10. Krier M, Kaltenbach T, McQuaid K, et al. . Potential use of telemedicine to provide outpatient care for inflammatory bowel disease. Am J Gastroenterol 2011;106:2063–7. [DOI] [PubMed] [Google Scholar]
- 11. Benchimol EI, Guttmann A, Mack DR, et al. . Validation of international algorithms to identify adults with inflammatory bowel disease in health administrative data from Ontario, Canada. J Clin Epidemiol 2014;67:887–96. [DOI] [PubMed] [Google Scholar]
- 12. Riaz MS, Atreja A. Personalized technologies in chronic gastrointestinal disorders: Self-monitoring and remote sensor technologies. Clin Gastroenterol Hepatol 2016;14:1697–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nguyen GC, Saibil F, Steinhart AH, et al. . Postoperative health-care utilization in Crohn’s disease: The impact of specialist care. Am. J. Gastroenterol 2012;107:1522–9. [DOI] [PubMed] [Google Scholar]
- 14. Murthy SK, Steinhart AH, Tinmouth J, et al. . Impact of gastroenterologist care on health outcomes of hospitalised ulcerative colitis patients. Gut 2012;61:1410–6. [DOI] [PubMed] [Google Scholar]
- 15. Nguyen GC, Steinhart AH. The impact of surgeon volume on postoperative outcomes after surgery for Crohn’s disease. Inflamm Bowel Dis 2014;20:301–6. [DOI] [PubMed] [Google Scholar]
- 16. Patil SA, Cross RK. Current landscape of telemedicine practice in inflammatory bowel disease. Inflamm Bowel Dis 2018, April 28 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]